Abstract
Background. Blastocystis spp. is a common protozoan found in the gastrointestinal tract, typically existing as a non-pathogenic organism in humans and other animals. However, it can become pathogenic when the immune system is compromised due to bacterial, viral, fungal, or other parasitic infections, as well as systemic conditions, leading to symptomatic blastocystosis. Methods. Fecal samples were collected from patients at the University Hospital of Campania “Luigi Vanvitelli” and Cotugno Hospital in Naples. Among these samples, those that tested positive for Blastocystis spp. and were associated with other microbial infections were further analyzed. Bacterial co-infections were identified using immunochromatographic tests (ICTs) and matrix-assisted laser desorption/ionization time-of-flight mass spectrometry (MALDI-TOF MS). Viral infections were detected using chemiluminescent immunoassay (CLIA), while fungal infections were diagnosed through microscopic examination and molecular biology techniques. Additionally, co-infections with other parasites were identified through microscopic analysis after Ridley’s concentration and Giemsa staining (O&P). Results. Out of the 2050 stool samples collected, 121 were positive for Blastocystis spp., of which 75 were associated with other infections. We identified the vacuolar form in patients co-infected with bacteria (n = 22), viruses (n = 30), fungi (n = 3), and other parasites (n = 20). Conclusions. Our findings indicated a higher incidence of the vacuolar form of Blastocystis spp. in symptomatic and immunocompromised patients, suggesting that a weakened immune system may increase the risk of contracting Blastocystis and other microbial infections.
1. Introduction
Protozoan infections present various clinical symptoms, including fever, acute watery diarrhea, nausea, abdominal pain, vomiting, and dehydration. The main risk factors for their global prevalence include uncontrolled population growth, low levels of education and sanitation, climate change, and poor nutrition. Blastocystis spp. are common protozoans of the large intestine, causing blastocystosis, and their prevalence ranges from 7 to 20% in developed countries and 40–60% in developing countries [1,2]. Despite their origin dating back to the early part of the 20th century, their potential pathogenicity is still controversial: Blastocystis spp. are usually localized as a commensal in the intestine, where they feed on bacteria and food residues necessary for growth [3]; however, some strains are characterized by certain pathogenicity causing clinical signs and symptoms like abdominal pain, bloating, flatulence, traveler’s diarrhea, rectal bleeding, and irritable bowel syndrome, with extraintestinal cutaneous manifestations [4,5]. According to the World Health Organization (WHO), Blastocystis spp. are classified as neglected pathogens responsible for one of the twenty-one neglected tropical diseases (NTDs) [6,7]. The taxonomic classification of this protozoan is uncertain, but recent studies using sequencing of multiple conserved genes suggest that Blastocystis spp. belongs to the Stramenopiles group of protists.
Currently, 22 subtypes (STs) have been identified based on nucleotide variations in the rRNA gene [8]. Among these, Blastocystis hominis is the species found in human intestines. The predominant subtypes affecting humans include ST1, ST12 [9,10], and ST14, the latter described in 2020 by Khaled et al. Subtypes ST1, ST2, ST3, and ST4 are common in Europe. Notably, ST1, ST2, and ST3 are equally prevalent among healthy and sick individuals, whereas ST4 is epidemiologically linked to acute diarrhea and chronic conditions, such as irritable bowel syndrome, associated with enhanced biomarkers of gut inflammation.
The heterogeneity of Blastocystis spp. accounts for their variable virulence, influenced by factors such as protease secretion, damage to cellular barriers due to actin filament rearrangement, and the production of inflammatory cytokines by colon cells. The infectious forms of Blastocystis spp., likely the cyst and vacuolar forms, are presumed to be transmitted via the fecal–oral route, although they have not yet been definitively identified. The host ingests the cyst through water or food contaminated with fecal material. Once inside the large intestine, the cyst develops, progressing through various stages before being expelled into the environment. In the environment, the cyst can survive in water for up to one month at 25 °C and up to two months at 4 °C [3,11]. According to a study by F. Beghini et al., Blastocystis spp. are common components of the human gut microbiome [12]. However, they are also found in patients with dysbiosis, which is associated with conditions such as colorectal cancer and Crohn’s disease. Additionally, several studies have indicated that Blastocystis spp. are present in immunocompromised individuals, with a prevalence of 30 to 38% in developed countries. This prevalence suggests that they may be an important risk factor, particularly in cases involving viral co-infections, especially among patients infected with human immunodeficiency virus (HIV) [13,14,15].
Blastocystis spp. have also been identified alongside bacterial infections in the gastrointestinal tract. In patients experiencing diarrhea caused by Clostridium difficile, as noted by L. Deng et al. [16], the ST7 subtype of Blastocystis was predominant. Similarly, in an Italian study conducted in northeastern Italy [17], a large number of positive cases for the cagA factor of Helicobacter pylori were observed, highlighting the importance of screening for parasitic infections in such patients.
Further studies have confirmed the co-infection of Blastocystis spp. with other pathogens such as Cryptosporidium spp., Toxocara spp. [18], Giardia spp. [19], and Entamoeba spp. The presence of these other pathogens in the gastrointestinal tract can promote blastocystosis, as the commensal organisms can proliferate and reach higher concentrations in the intestine [20]. As demonstrated by Pielok et al. [18], subjects infected with oocysts of Cryptosporidium spp. [18] who were also co-infected with Toxocara spp. showed a significant presence of blastocystosis, which was further corroborated by cases of giardiasis described by Sánchez et al. Infections caused by bacteria, viruses, and parasites can increase the prevalence of blastocystosis and its most virulent subtype, leading to alterations in gut microbiota. In this context, Blastocystis can act as both a pathogen and a virulent agent. In this work, we analyzed the prevalence of blastocystosis in two hospital settings in southern Italy. Additionally, we reported cases of co-infection with various pathogens, including bacteria, viruses, fungi, and parasites.
2. Materials and Methods
2.1. Sample Collection
A total of 2050 stool samples were collected from the Complex Operative Unit (U.O.C) of Virology and Microbiology of two hospitals in Naples, including the University of Campania “L. Vanvitelli” and Cotugno Hospital. Sampling and identification were conducted between January 2022 and January 2024, following the recommended national and international guidelines [21,22]. Three samples from three different and non-consecutive days were collected from each patient with suspected bacterial, viral, fungal, or parasitic gastroenteritis.
2.2. Direct Microscopic Fresh Examination of Fecal Samples
A few grams of feces was diluted in 1–2 mL NaCl 0.9%; a drop of the diluted sample was placed on a glass slide and microscopic observation was immediately performed to search for the presence of parasites by observing motile structures (cilia or flagella) and the movements of certain parasites (amoebae or larvae). Another direct examination included preparation with Dobell’s solution to stain glycogen vacuoles and nuclei of cysts present.
2.3. Microscopic Examination After Ridley’s Concentration Method
Samples analyzed by Ridley’s method were fixed and concentrated with a Para-Pak® CON-Trate® System stool concentration kit (Meridian Bioscience, Cincinnati, United States). Four distinct phases were visible after the concentration of samples: a layer of ethyl acetate or solvent, a layer of feces debris, a slightly colored aqueous layer (formalin), and a sediment layer. This last phase was collected, and the sample was observed by microscopy.
2.4. Detection of Bacterial Co-Infections
2.4.1. Clostridium Difficile Detection by GDH Immuno-Chromatographic Test: Tox A and Tox B
The stool samples were screened for antigens and toxins (Tox A and Tox B), using the Immunocard Clostridium difficile GDH (Meridian Bioscience, Cincinnati, OH, USA) according to the manufacturer’s instructions [22]. Briefly, the diluent sample and enzyme conjugate were added together with liquid stool. The specimen was mixed and then transferred to the card. After incubation for 15 min at room temperature, the substrate was added, and results were read in 10 min.
2.4.2. Helicobacter Pylori Antigen Detection by Immuno-Chromatographic Test
A Helicobacter pylori Antigen Rapid Test Cassette (Alltest, Hangzhou, China) was used. Labeled antibodies attached to a nitrocellulose membrane were able to recognize and bind to the antigens present in the fecal sample, resulting in the formation of a colored band.
2.4.3. Salmonella spp. Detection
One gram of fecal sample was inoculated in Selenite Broth Base broth (Biolife Italiana, Monza, Italy) and incubated at 35 ± 2 °C for 18–24 h. Subsequently, the turbidity of the broth was assessed, and 1 μL was plated on Hektoen Enteric Agar (H.E.A.; Becton Dickinson, Franklin Lakes, NJ, USA) and Salmonella and Shigella Agar (SS; Becton Dickinson). The plate was incubated at 35 ± 2 °C for 18–24 h, and mass spectrometry using matrix-assisted laser desorption/ionization (MALDI-TOF, Bruker, Biellerica, MA, USA) was executed (KIT Salmonella typhi H Micro 5 × 10 mL; LTA, Bussero, Milano, Italy).
2.5. Detection of Viral Co-Infections
The viral co-infections were detected by the LIAISON XL (Diasorin S.P.A., Saluggia, Italy). Specific viruses were investigated, including hepatitis viruses A (HAV) and B (HBV); adenovirus (AdV); SARS-CoV-2; cytomegalovirus (CMV); herpes simplex virus type 1 (HSV-1) and type 2 (HSV-2); Epstein–Barr virus (EBV); rubella virus (RuV); influenza viruses A and B; human immunodeficiency virus (HIV).
2.6. Fungal Co-Infections by DNA Identification
Fungal co-infection was assessed based on direct microscopic examination, which revealed the characteristic mycetic pseudohyphae of Candida spp., and by detecting Pneumocystis jirovecii DNA using a PCR assay (ELITE INGENIUS®-ELITechGroup Molecular Diagnostics, Torino, Italy) from a specific bronchoalveolar lavage sample, integrating extraction, amplification, and results interpretation.
2.7. Parasitic Co-Infections by Immuno-Chromatographic Tests and Molecular Confirmation
Chilomastix mesnili, Dientamoeba fragilis, Endolimax nana, Entamoeba coli, Entamoeba histolytica/dispar, Enterocytozoon bieneusi, Giardia duodenalis, and Schistosoma mansoni infections were detected by microscopy analysis as previously described. In addition, two kits were used for Giardia spp. identification: Cryptosporidium and Giardia Card Plus (Mascia Brunelli; Monza, Italy) and immunofluorescence assay (IFA) with Merifluor® Cryptosporidium/Giardia (Meridian Bioscience). Molecular analysis was also conducted by combining the PCR and microarray procedure with the Novadiag molecular biology system (Hologic, Marlborough, MA, USA).
2.8. DNA Extraction, PCR Amplification, and Microarray
The Novodiag molecular biology system (Hologic) was used for the detection of nucleic acids of the most common parasites, including Ancylostoma duodenalis, Ascaris lumbricoides, Balantidium coli, Blastocystis spp., Diphyllobothrium latum, Clonorchis sinensis, Opisthrochis spp., Cryptosporidium spp., Cyclospora cayetanensis, Cystoisospora belli, Dientamoeba fragilis, Entamoeba histolytica, Enterobius vermicularis, Fasciola spp., Giardia intestinalis, Fasciolopsis buski, Hymenolepis nana, Schistosoma mansoni, Strongyloides stercoralsis, Taenia saginata, Taenia solium, Taenia asiatica, and Thricuris spp. The procedure included the adsorption of a certain amount of feces via the eSwab; then, 1 mL of the fecal solution was inoculated into a tube containing agarose beads, and mechanical lysis of cells was carried out by the MagNALyser (Roche Diagnostics, Indianapolis, IN, USA). The cartridge containing specific PCR sequence primers was filled with 600 μL of the lysed cells, and PCR was performed according to manufacturer’s instructions (94 °C for 4 min; 95 °C for 15 s, 60 °C for 15 s, 72 °C for 30 s, repeated for 30 cycles; 72 °C for 5 min). Finally, the amplified sequences were paired with specific sequence microarrays for a qualitative result (absence/presence of parasitic DNA).
2.9. Statistical Analysis
The IBM SPSS software (version 22.0; IBM SPSS Inc., New York, NY, USA) was utilized for data analysis. The data were summarized and described using frequencies and proportions. For categorical variables, descriptive statistics were presented as counts and percentages. The chi-square test was used to compute p-values, with a significance threshold set at <0.05.
3. Results
3.1. Prevalence of Blastocystis spp. by Microscopic Detection
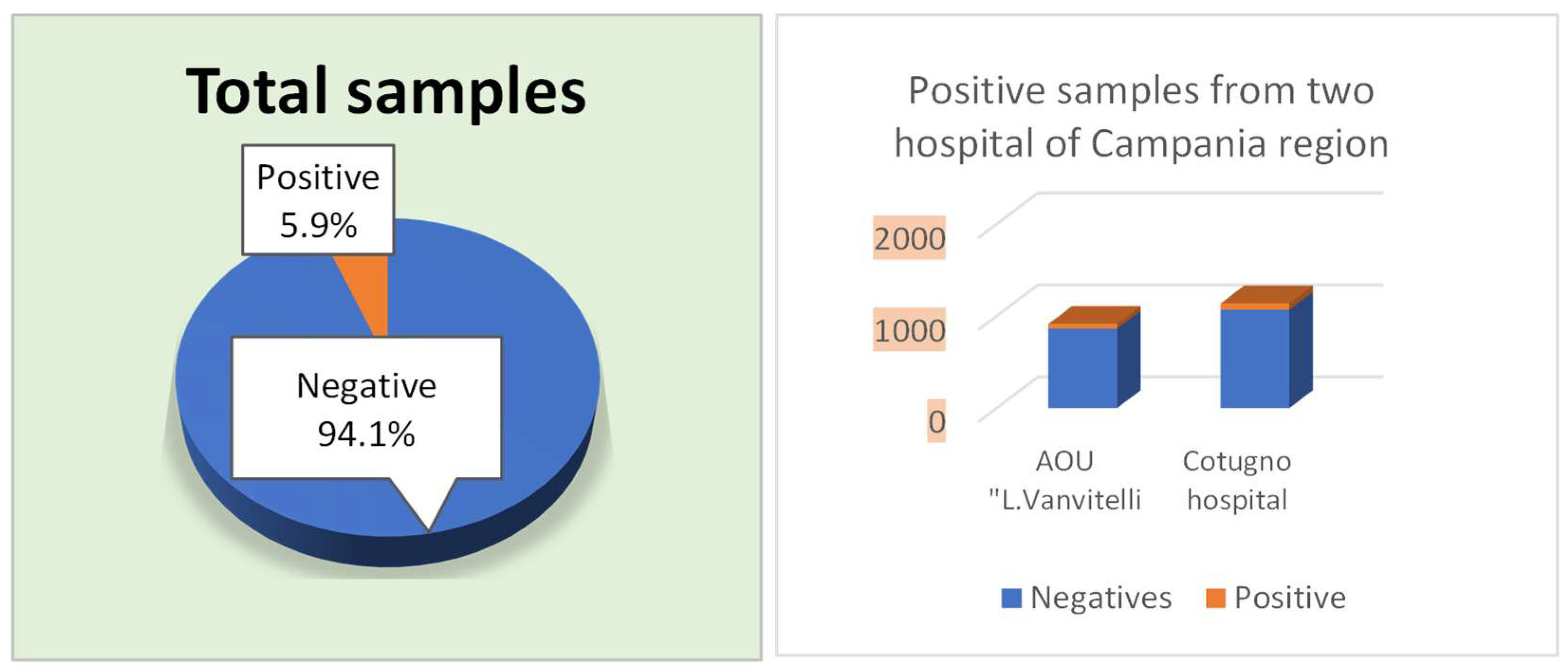
During the period from January 2022 to January 2024, 2050 stool samples were collected in the two hospitals of the Naples area. In detail, 913 (44.5%) samples were isolated from the AOU of the University Hospital of Campania “Luigi Vanvitelli” while 1137 (55.5%) samples were collected from Cotugno Hospital (Figure 1). Among them, 121 (5.9%) were positive for Blastocystis spp.: 51 belonging to the AOU of the University Hospital of Campania “L. Vanvitelli” and 70 patients from Cotugno Hospital.
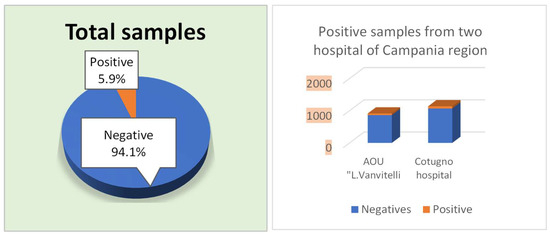
Figure 1.
Total samples, Negative and Positive from AOU “L. Vanvitelli” and Cotugno Hospital. From 2050 samples, 5.9% positives were identified through fresh microscopic analysis after Ridley’s concentration and Giemsa staining (O&P).
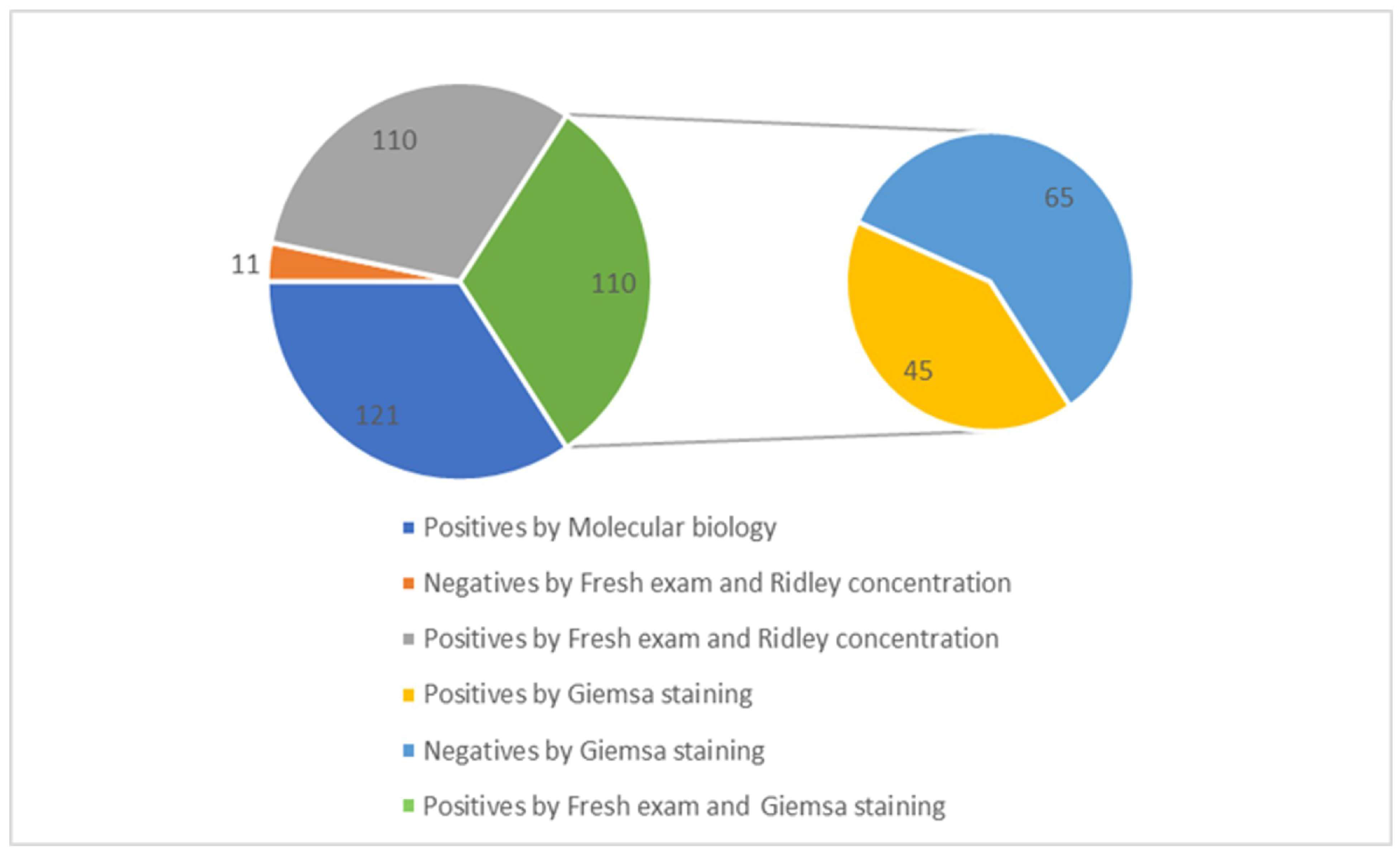
In contrast, 55.5% of the samples (n = 1137) came from Cotugno Hospital, which had 70 positive cases. Additionally, a further identification was performed to test the positive samples for Blastocystis spp. using Giemsa staining. A total of 121 samples were analyzed for Blastocystis spp. using molecular biology techniques, and it was confirmed that 45 of these samples were positive. Specifically, out of the 121 samples, 110 tested positive based on fresh examination and Ridley concentration methods. Among these, 45 samples were also positive when examined using Giemsa staining: 15 from the AOU of the University Hospital of Campania “Luigi Vanvitelli” and 30 from Cotugno Hospital. Additionally, 65 samples were found to be negative using the Giemsa staining method. This discrepancy is because Giemsa staining is less sensitive compared to microscopic observation following fresh examination, Ridley concentration, PCR, and microarray detection (Figure 2).
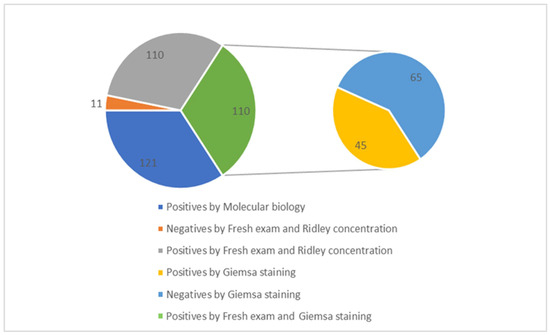
Figure 2.
Correlation between total positive samples for Blastocystis spp. and Giemsa staining.
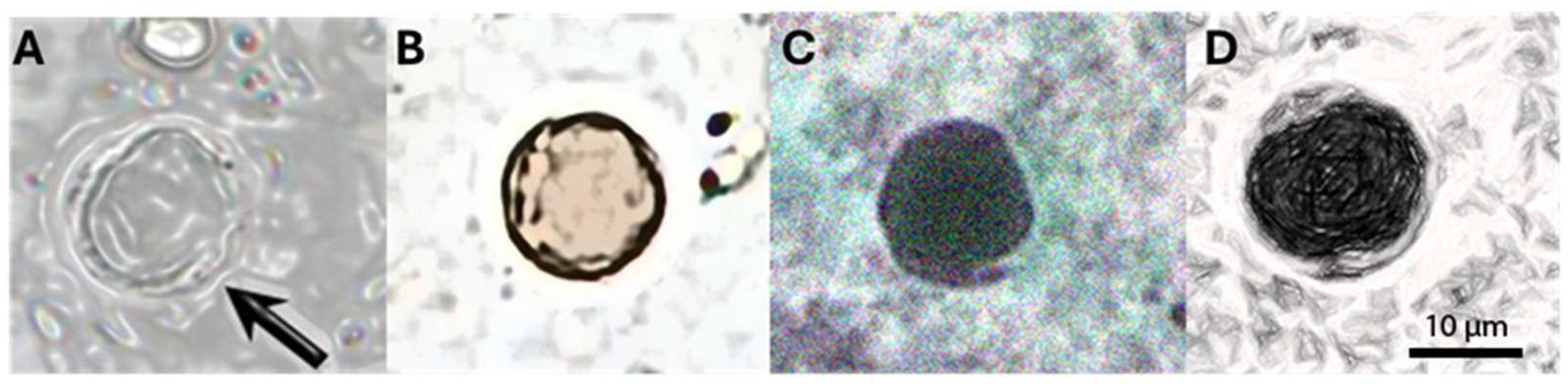
Among the samples that tested positive for Blastocystis spp., at least four major forms were identified through microscopic examination of fresh specimens. As shown in Figure 3, we observed the vacuolar form (Figure 3A), representing the most common form present in the culture and feces of the host. It was spherical and with a variable diameter (2–200 μm, average 4–15 μm). The vacuole occupied most of the cell, while the cytoplasm and nuclei were arranged in a ring at the periphery. As shown in Figure 3B, the granular form with a vacuolar shape is characterized by granulations in the cytoplasm; an amoeboid form (Figure 3C) was rarely observed, characterized by one or more extensions of the cytoplasm (pseudopodia). The cystic form (Figure 3D) is frequently found in the feces and is characterized by variable morphology (spherical to oval) and small size (2–5 μm). A multilayered wall surrounded the cyst and contained small vacuoles, glycogen granules, and one to four nuclei.
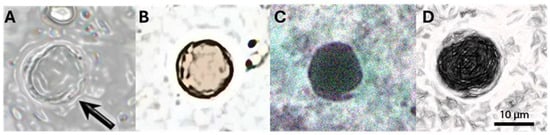
Figure 3.
The most representative forms of Blastocystis spp. (A) The vacuolar form with a central vacuole and peripheric nuclei and cytoplasm; (B) The granular form with the presence of granulation; (C) The ameboid form with rgw presence of pseudopodia by the cytoplasm; (D) The cystic form with small vacuoles, granulation, and peripherical nuclei.
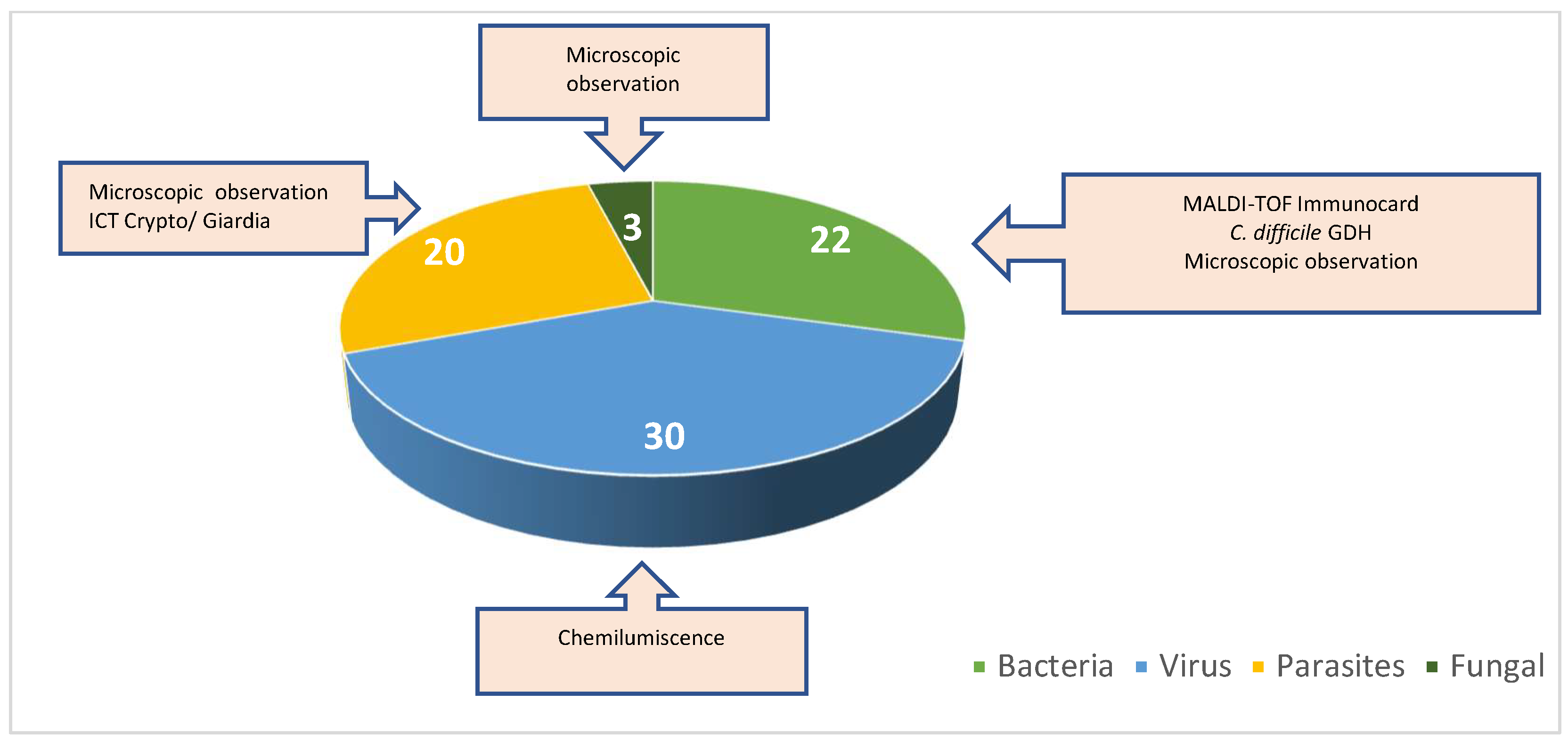
3.2. Detection of Co-Infecting Pathogens
In addition to detecting Blastocystis spp. in the analyzed samples, we also investigated the presence of co-infections among the positive cases. A total of 121 samples were examined for co-infections: 75 samples tested positive for co-infections, while 46 samples tested negative. Among the co-infected samples, 22 (29%) showed bacterial co-infections, 30 (40%) exhibited viral co-infections, 3 (4%) were characterized by fungal co-infections, and 20 (27%) had parasitic co-infections (Figure 4).
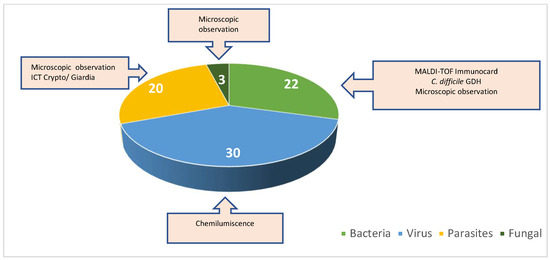
Figure 4.
Percentage of co-infections with bacteria, viruses, parasites, and fungi.
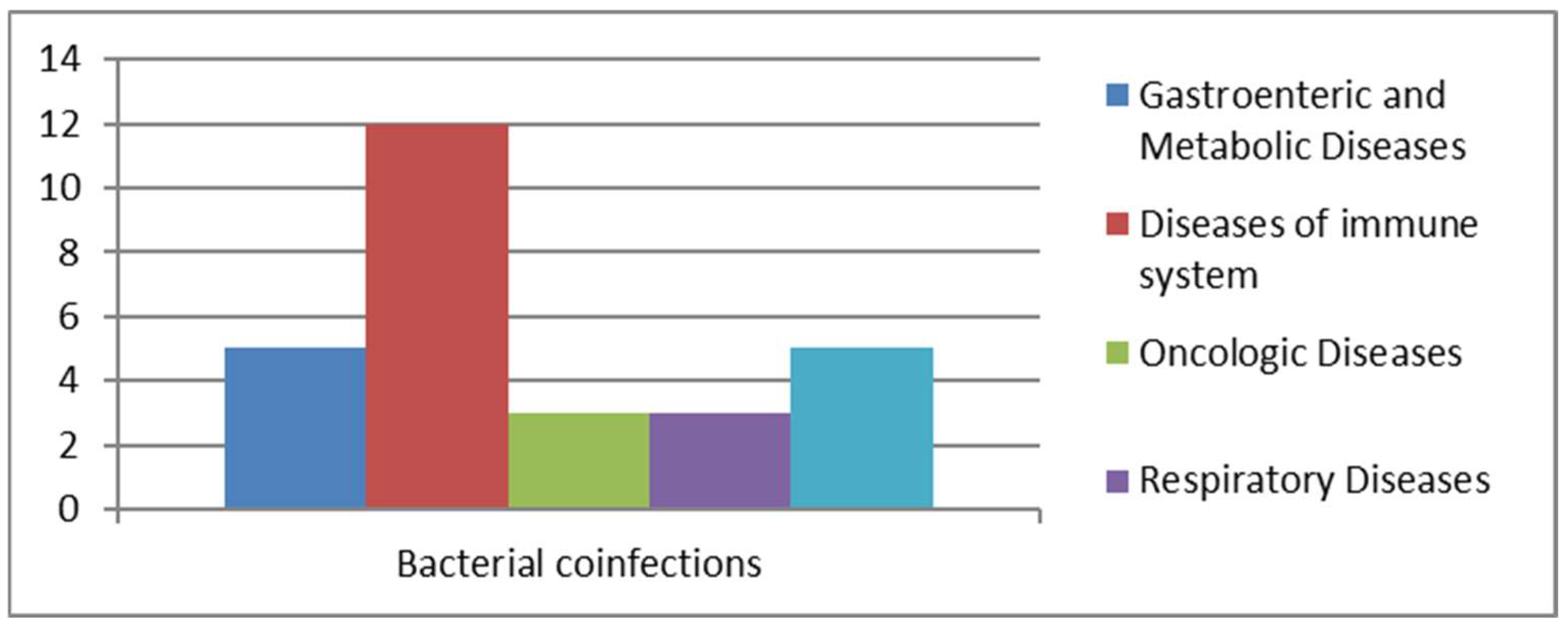
3.2.1. Bacterial Co-Infection
We analyzed cases of Blastocystis spp. infections associated with bacterial co-infections (Figure 5).
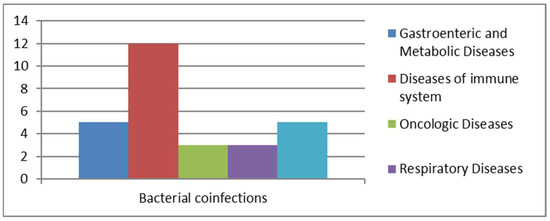
Figure 5.
Bacterial co-infections.
Among the pathogens identified in samples with bacterial co-infections were both Gram-positive and Gram-negative bacteria capable of colonizing various regions of the human body, particularly the urinary and gastrointestinal tracts. Out of 22 positive cases, most showed co-infections with members of the Enterobacteriaceae family (n = 10) (Table 1). A smaller number of cases were caused by Helicobacter pylori (n = 3) and Clostridium difficile. Other pathogens were identified less frequently, including Campylobacter (n = 1), Klebsiella pneumoniae (n = 1), Salmonella spp. (n = 1), Plesiomonas shigelloides (n = 1), and Treponema pallidum (n = 1). The presence of pathogenic bacteria in the gastrointestinal tract, along with immunocompromisation of the immune system, favors the proliferation of commensal protozoa like Blastocystis spp. [18,20]. The total number of patients with bacterial co-infections was 22, which included 3 oncology patients, 3 patients with respiratory diseases, 5 transplant recipients, 5 individuals with gastrointestinal and metabolic issues, and 12 patients suffering from immune system disorders. Among these 12 patients, 2 also had metabolic diseases, while another 2 were oncology patients, and 2 were affected by bacterial pneumonia.

Table 1.
Bacterial co-infection in the University Hospital “Luigi Vanvitelli” and Cotugno Hospital.
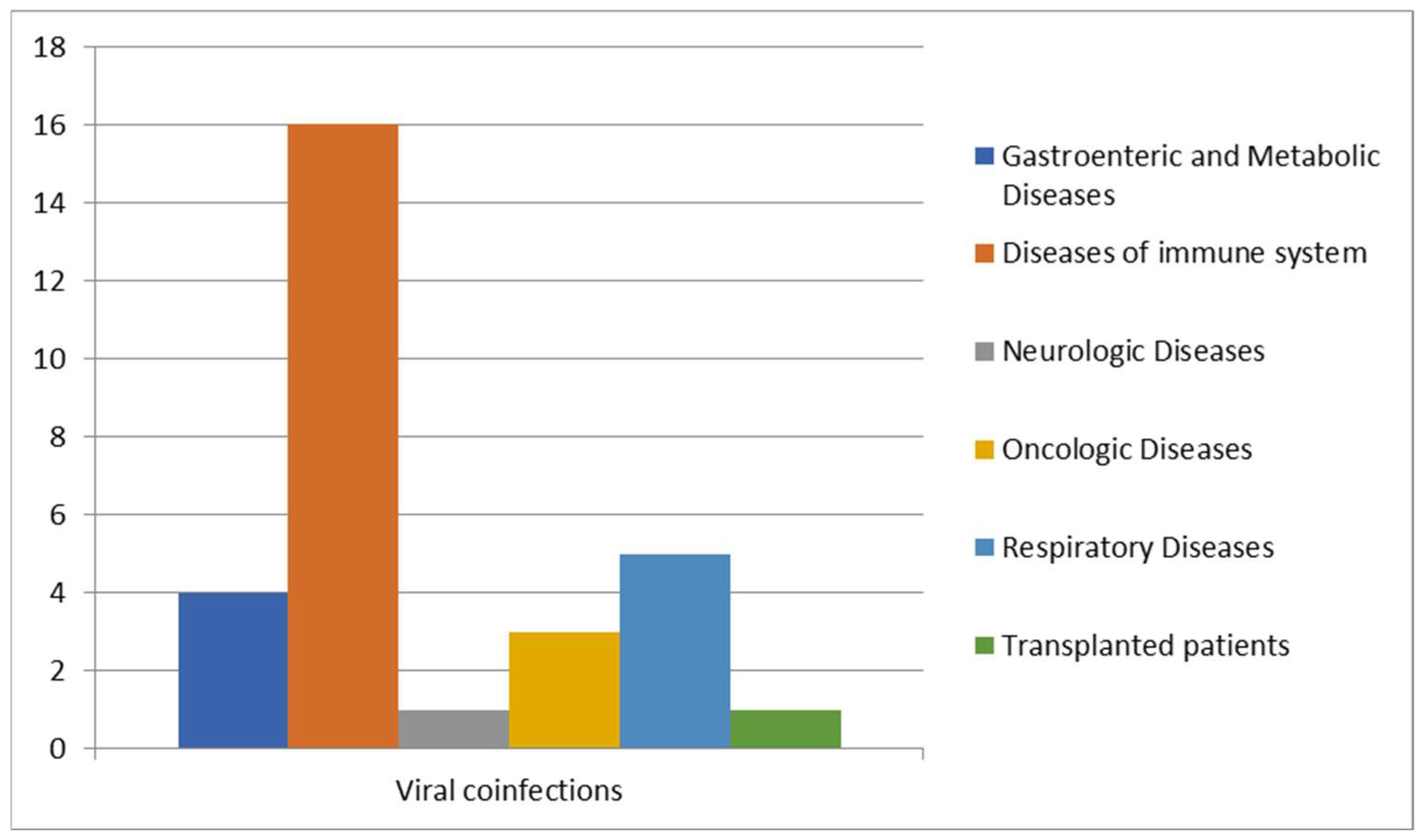
3.2.2. Viral Co-Infections
We further analyzed cases of Blastocystis spp. infection in patients with viral co-infections (Figure 6).
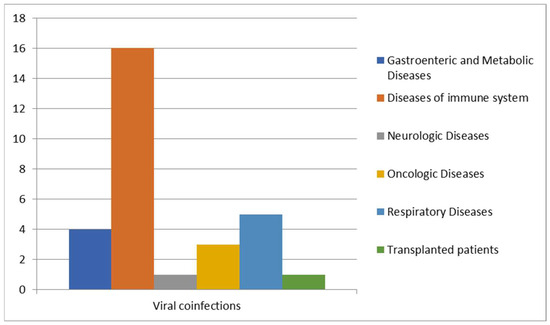
Figure 6.
Correlation between viral infections and other diseases.
Viral co-infections were found in a higher number of the positive samples, with a prevalence of infections caused by members of the Herpesviridae family, retroviruses, and hepatitis viruses (Table 2).

Table 2.
Viral co-infection in University Hospital “Luigi Vanvitelli” and Cotugno Hospital.
A high prevalence of Blastocystis co-infections was observed in patients with problems of the immune system since people with HIV or with several other irreversible viral infections are the most susceptible [14,23]. Of the 30 patients positive for viral co-infections, like HAV, HBV, adenovirus, CMV, HSV-1 and HSV-2, RSV, EBV, influenzas A and B, Coxsackie virus, SARS-CoV-2, and HIV, 16 patients were affected by immune system problems [24], 5 patients by respiratory diseases, 4 patients by metabolic diseases, 3 patients were oncologic patients, 1 patient was affected by neurological disease, and 1 patient was transplanted.
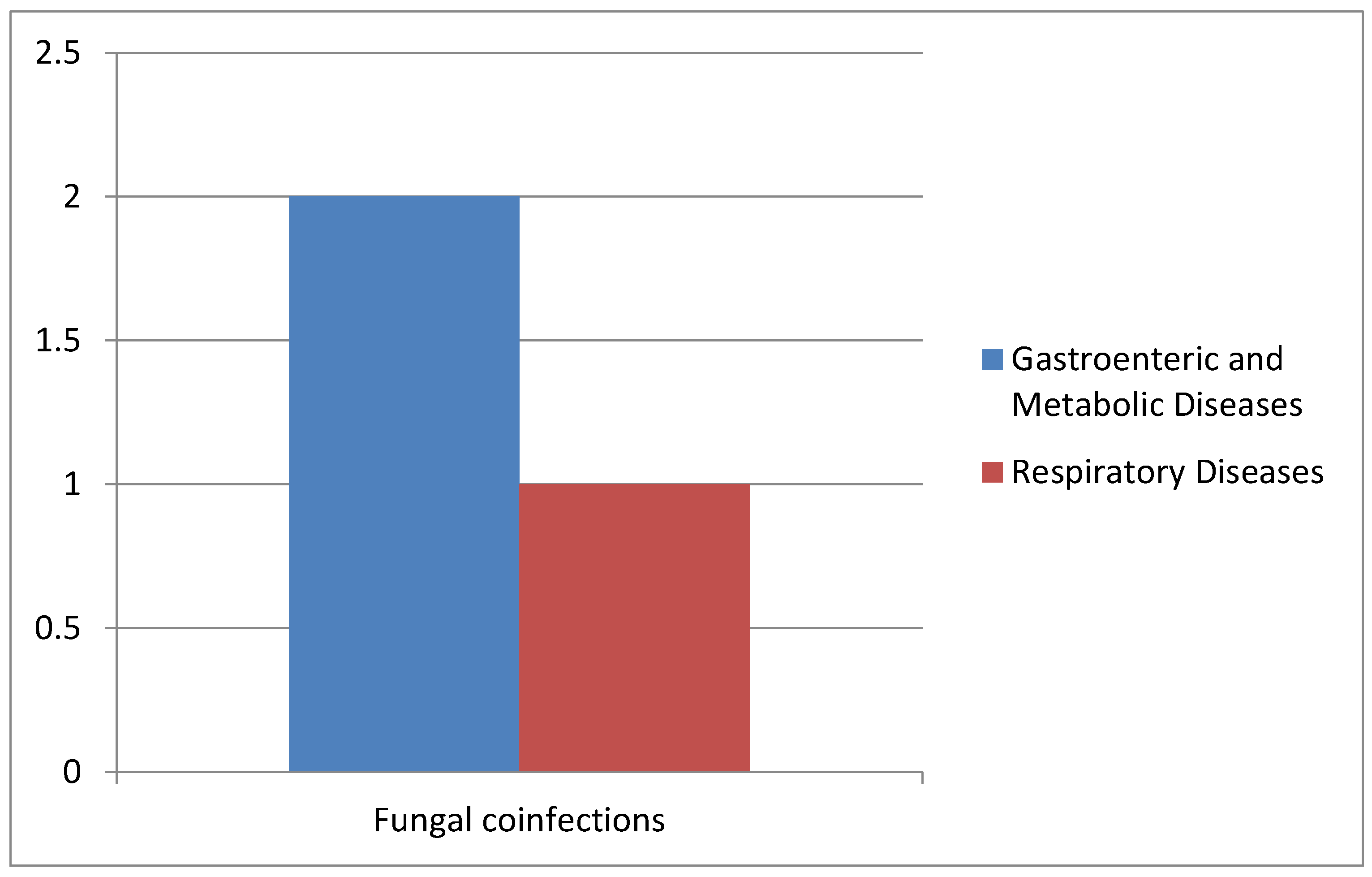
3.2.3. Fungal Co-Infections
In all collected samples, we also evaluated the presence of Blastocystis spp. and fungal infections (Figure 7).
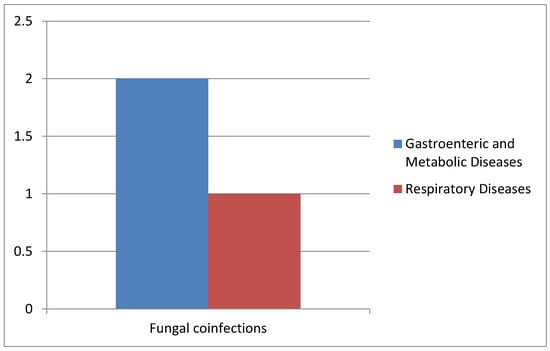
Figure 7.
Correlation of Blastocystis and fungal co-infections with gastrointestinal and metabolic diseases and respiratory diseases.
In detail, two cases of co-infections with Candida spp. were observed in the AOU of the University Hospital of Campania “L. Vanvitelli”, and only one case affected by Pneumocystis jirovecii pneumonia was reported at Cotugno Hospital with the presence of Pneumocystis (Table 3).

Table 3.
Cases of fungal co-infection in the University Hospital “L. Vanvitelli” and Cotugno Hospital.
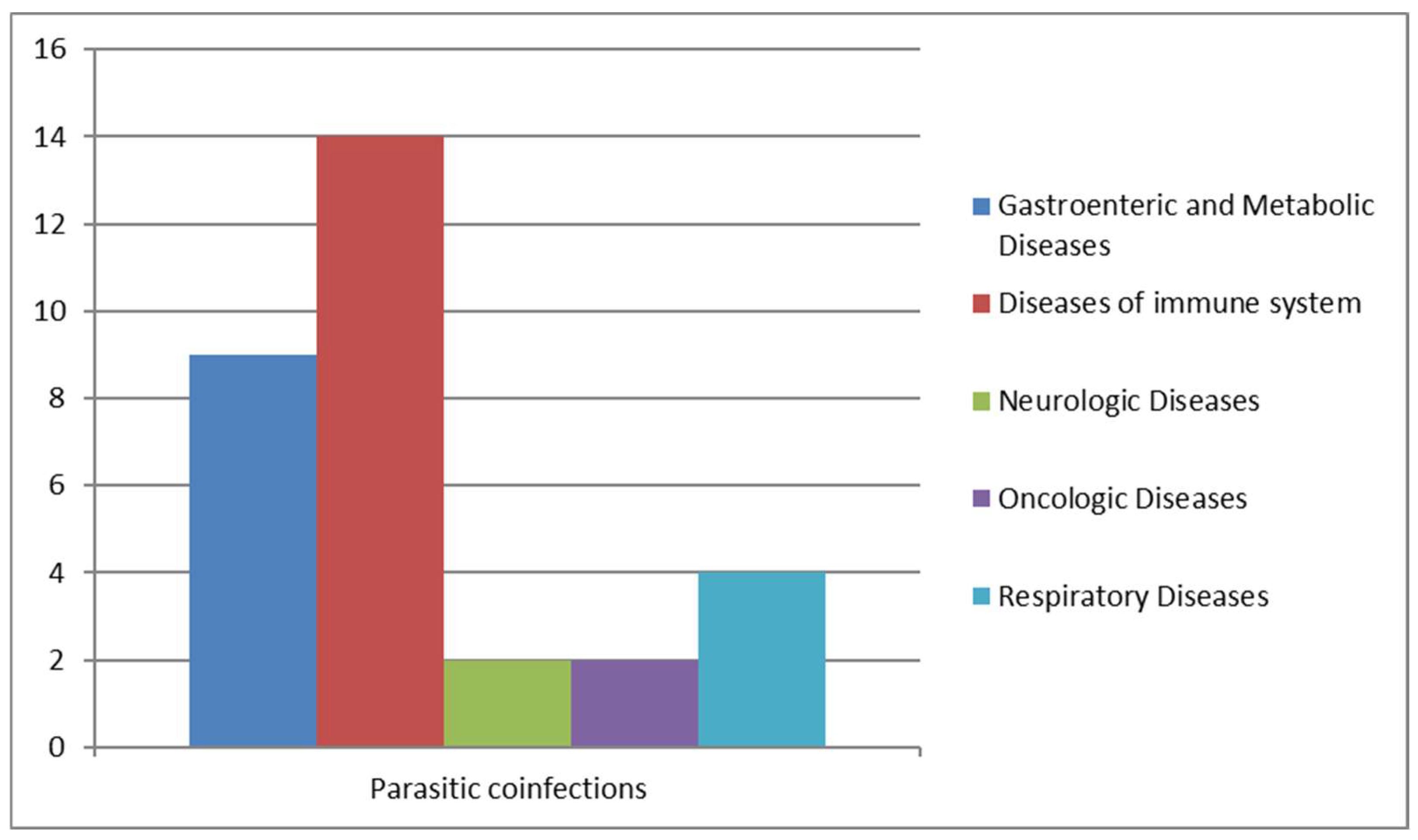
3.2.4. Parasitic Co-Infections
We analyzed cases of Blastocystis infections associated with other parasitic infections: 14 patients with immune system problems, so the most susceptible and fragile to contract blastocystosis, 2 patients were also affected by metabolic diseases, 2 by respiratory diseases, 1 by neurologic diseases, and 1 was an oncologic patient (Figure 8).
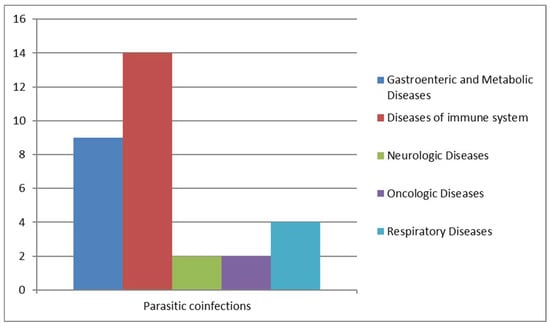
Figure 8.
Parasitic co-infections correlated with other diseases.
As reported in Table 4, parasitic co-infection is detected in 30–69-year-old patients. An imposing incidence has been shown by parasitic co-infections: out of 121 positive samples, 20 were co-infected with parasites, like Chilomastix mesnili, Dientamoeba fragilis, Entamoeba histolytica/dispar, Endolimax nana, Entamoeba coli, Enterocytozoon bieneusi, Giardia duodenalis, and Schistosoma mansoni. Widely, we observed Entamoeba histolytica/dispar with the highest incidence, followed by Giardia duodenalis and Schistosoma mansoni (Table 4).

Table 4.
Cases of parasitic co-infection in the University Hospital “L. Vanvitelli” and Cotugno Hospital.
3.2.5. Prevalence of Blastocystis spp.
We observed Blastocystis spp. and other microbial infections in 62 % of male and 38 % of female patients. Starting from 75 total positive patients with co-infections, four age groups were investigated (0–20; 21–40; 41–60; 61–80). The highest prevalence was observed at 21–40 years with 21% (p-value: 0804) and 41–60 years with 29% (p-value: 0048) (Table 5).

Table 5.
Incidence of Blastocystis spp., analyzing specific age ranges of patients.
The incidence of Blastocystis spp. among various ethnic groups was also analyzed, with the highest values in the Italian population (88%). The most representative form was vacuolar in 88 samples (73%) and granular in 33 (27%). The presence of the first infectious form was significant in the patients with co-infections (Table 6). As reported in Table 6, Blastocystis spp. co-infections were more common in males (59%, p-value: 0.099) than females (41%, p-value: 0.548), with a high incidence (88%) in Italians, and the most frequent form was vacuolar (73%, p-value: <0.005).

Table 6.
Detection of the incidence of Blastocystis spp. co-infections in patients, specifying gender, nationality, and form. N/A: not available.
3.2.6. Molecular Analysis to Characterize Blastocystis spp.
To confirm the presence of positive cases of Blastocystis spp. and other parasites, molecular analysis was performed. A total of 121 patients (6%) tested positive using the Novodiag stool parasite system. Of these, 110 (91%) samples also tested positive upon retesting and after Ridley concentration, while 45 (37%) were confirmed positive by Giemsa staining (Table 7).

Table 7.
Concordance of epidemiological data.
After comparison to standard reference methods, including direct microscopic examination of fresh samples, microscopic examination after Ridley concentration, and Giemsa (O&P) staining, the Novodiag test showed higher sensitivity and specificity, detecting even traces of parasitic DNA. The optimal approach would be a combination of both methods, with the Novodiag test used for initial screening of intestinal parasitic infections and the standard reference techniques used for confirming positive results.
By the comparison between standard retrieval techniques (O&P) for the search for parasites in feces and molecular diagnosis, it emerged that molecular biology and microarray are more sensitive (standard reference technique sensitivity: 87%/molecular analysis sensitivity: 100%). The specificities of the methods were the same (standard reference technique specificity: 100%, molecular analysis specificity: 100%). In fact, with 100% agreement, molecular biology confirms 121 positive cases of Blastocystis spp. versus 110 positive cases observed only by the microscopic exam (fresh examination and Ridley concentration) and only 45 positive results by a less specific method, Giemsa staining. A large number of positives by molecular biology are also associated with patients in therapy and with DNA in feces, detectable only by molecular analysis but not by direct search for vital microscopic forms.
4. Discussion
Our study investigated the prevalence of Blastocystis spp. infections and their correlation with other infectious diseases in two hospital settings in southern Italy: the University Hospital of Campania “Luigi Vanvitelli” and Cotugno Hospital. Sample collection took place from January 2022 to January 2024. We analyzed a total of 2050 samples using various methods by national and international guidelines. These methods included fresh examination of feces, Ridley’s concentration technique, Giemsa staining (O&P), and molecular biology approaches. Our findings highlighted the significance and prevalence of Blastocystis infections, occurring not only in endemic regions with poor sanitary conditions but also in industrialized countries. As demonstrated by Parija S.C. et al., the incidence of Blastocystis-related diarrhea has increased in recent decades, affecting both impoverished and Western globalized nations [25]. We identified a total of 121 positive samples for Blastocystis spp., with 22 co-infected with bacteria, 30 with viruses, 3 with fungi, and 20 with other parasites. Notably, a significant percentage of cases involved bacterial infections, particularly gastroenteric bacteria such as Campylobacter, Clostridium difficile, Escherichia coli (extended-spectrum β-lactamase), Helicobacter pylori, Salmonella spp., Klebsiella pneumoniae, and Plesiomonas shigelloides. Patients with these co-infections, as indicated by their medical history, exhibited a variety of symptoms related to intestinal diseases, including diarrhea (particularly traveler’s diarrhea), abdominal pain, gastrointestinal discomfort, bloating, flatulence, rectal bleeding, and irritable bowel syndrome.
Some patients exhibited extraintestinal skin manifestations. In contrast, individuals solely infected with Blastocystis spp. generally showed fewer symptoms. A retrospective data analysis was conducted to explore the correlation between Blastocystis spp. and other microorganisms. The analysis revealed a significant positive correlation between the presence of Blastocystis spp. and bacterial and viral infections (p-value: <0.05). This suggests that changes in the gastrointestinal microbiota or systemic viral infections are significantly associated with Blastocystis in the gut. Moreover, we observed that patients with co-infections more frequently exhibited vacuolar forms of Blastocystis spp., with cyst counts exceeding 20 per microscopic field. These patients displayed more pronounced clinical symptoms and had stool types classified as 6–7 on the Bristol stool scale. It is well established that co-infections typically lead to worse overall health outcomes, as they often pose greater treatment challenges. For example, patients who are co-infected with fungal pneumonia (Pneumocystis jirovecii), seasonal respiratory viruses, tuberculosis, and COVID-19 frequently experience intensified dysbiosis symptoms, such as diarrhea, due to compromised immune systems. However, our study did not find a significant correlation between Blastocystis spp. and fungal infections (p-value > 0.05). We recognize that this limitation may be due to the relatively small number of positive fungal samples. Interestingly, the granular form of Blastocystis was only observed in patients who were not co-infected with other pathogens. Several studies have suggested that Blastocystis spp. may have beneficial effects on the host by modulating the immune system. One potential mechanism is through the stimulation of mucus production via the cytokine IL-22, which may help alleviate colitis symptoms and improve gut health. Blastocystis plays a crucial role in modulating bacterial diversity and promoting the abundance of Clostridia species, which produce short-chain fatty acids, ultimately contributing positively to microbiota health [26,27]. Our research also confirmed that the vacuolar form is predominantly observed in the non-co-infected population, as 88 samples showing the vacuolar form were from this group, which appears to validate the proposed opportunistic pathogenic behavior of Blastocystis spp. This was previously emphasized in a study involving patients diagnosed with gastric and colorectal cancer where Blastocystis spp. was found in 11% of cancer-affected patients, who also exhibited diarrhea: the presence of blastocysts is a risk factor for the worsening of colorectal cancer by the alteration of the host immune response and by the increase in oxidative damage of the cells of the gastrointestinal tract; in this case, the subtype ST1 was the most prevalently detected in patients with colorectal cancer, with a significant risk of association (p-value: =0.004). In contrast, it was detected in only 2% of the control group [28] and also in another study involving HIV-positive patients that revealed that Blastocystis hominis infection decreased progressively with increasing CD4+ T-helper cells, while the risk of infection increased with higher HIV viral load. This confirms that an alteration of the immune system can cause a modification of the gastrointestinal tract and the microbiome; viral infections, like HIV, influence the production of cells of the immune response. In detail, T-helper cells regulate the immune response by producing and releasing cytokines that stimulate other cells to activate or suppress immune responses. HIV co-infection and the presence of Blastocystis not only aggravate the clinical signs of the commensal but also accelerate the progression of the acquired immunodeficiency syndrome [23,29,30]. In our study, we observed a correlation between the isolation of the vacuolar form of this parasite and the presence of bacterial, viral, and parasitic co-infections. The vacuolar form is most frequently found in patients with these co-infections. Anamnestic information shows that these patients are more likely to exhibit clinical signs of blastocystosis, such as diarrhea, flatulence, skin rashes, and irritable bowel syndrome. We believe that a diagnosis of Blastocystis spp. requires clinical attention and intervention, particularly in patients with a history of chronic or recurrent illness. The role of this parasite’s isolation is still unclear and warrants further investigation.
Additionally, our analysis of the prevalence of Blastocystis infection in two hospitals in the Campania region indicates that the symptomatology of Blastocystis infection cannot be fully explained by the presence of different subtypes or other microbial co-infections. This highlights the hypothesis that the host’s condition plays a crucial role in influencing the pathogenicity of Blastocystis spp. colonization. Considering the higher prevalence in younger patients, it would be worthwhile to evaluate the association between Blastocystis infection and intestinal microbiota or immunological conditions, as this could enhance our understanding of the parasite’s ability to penetrate the host.
5. Conclusions
Our study, conducted in two hospital settings in the Campania region, provides valuable insights into the incidence of infection and co-infection of Blastocystis spp. with other pathogens. We detected a total of 121 positive cases. A significant correlation was found between Blastocystis spp. and both bacterial and viral infections, suggesting that alterations in the gastrointestinal microbiota or systemic viral infections may be linked to the presence of this parasite. Patients with co-infections displayed more pronounced clinical symptoms, including diarrhea, abdominal pain, and gastrointestinal discomfort. They were also more likely to exhibit the vacuolar form of Blastocystis spp., which is frequently associated with pathogenicity. Our findings emphasize the importance of clinical attention when diagnosing Blastocystis spp., particularly in patients who experience chronic or recurrent gastrointestinal symptoms. Further investigation is necessary to enhance diagnostic and therapeutic strategies for managing co-infections and related health complications.
Author Contributions
Conceptualization, M.G. and M.G.C.; methodology, M.A., A.C., F.F. and L.P.; software, M.A, A.C. and F.F.; validation, A.D.F., C.Z., L.P. and E.F.; formal analysis, A.D.F. and C.Z.; investigation, M.A., A.C., F.F. and L.P.; resources, M.G. and M.G.C.; writing—original draft preparation, M.A. and A.C.; writing—review and editing, A.D.F. and C.Z.; supervision, M.G.; project administration, M.G. and M.G.C.; funding acquisition, M.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was conducted using anonymized fecal samples collected during routine diagnostic procedures, without the use of identifiable personal data, and without any additional interventions involving patients. According to the Italian Legislative Decree 101/2018, which implements EU Regulation 2016/679 (General Data Protection Regulation – GDPR), and the guidelines of the Italian Data Protection Authority (Garante per la Protezione dei Dati Personali), research using fully anonymized biological samples that are not traceable to individual subjects does not fall under the requirement for ethical review.
Informed Consent Statement
The requirement for informed consent for participation does not apply to the present study.
Data Availability Statement
Further inquiries can be directed to the corresponding author.
Acknowledgments
We thank the Complex Operative Unit of Virology and Microbiology staff members of the University Hospital of Campania “Luigi Vanvitelli”, Italy.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Lepczynska, M.; Bialkowska, J.; Dzika, E.; Piskorz-Ogorek, K.; Korycinska, J. Blastocystis: How do specific diets and human gut microbiota affect its development and pathogenicity? Eur. J. Clin. Microbiol. Infect. Dis. 2017, 36, 1531–1540. [Google Scholar] [CrossRef]
- Stenzel, D.J.; Boreham, P.F. Blastocystis hominis revisited. Clin. Microbiol. Rev. 1996, 9, 563–584. [Google Scholar] [CrossRef] [PubMed]
- Tan, K.S. New insights on classification, identification, and clinical relevance of Blastocystis spp. Clin. Microbiol. Rev. 2008, 21, 639–665. [Google Scholar] [CrossRef]
- Ajjampur, S.S.; Tan, K.S. Pathogenic mechanisms in Blastocystis spp.—Interpreting results from in vitro and in vivo studies. Parasitol. Int. 2016, 65, 772–779. [Google Scholar] [CrossRef] [PubMed]
- Tan, K.S.; Mirza, H.; Teo, J.D.; Wu, B.; Macary, P.A. Current Views on the Clinical Relevance of Blastocystis spp. Curr. Infect. Dis. Rep. 2010, 12, 28–35. [Google Scholar] [CrossRef]
- Kosik-Bogacka, D.; Lepczynska, M.; Kot, K.; Szkup, M.; Lanocha-Arendarczyk, N.; Dzika, E.; Grochans, E. Prevalence, subtypes and risk factors of Blastocystis spp. infection among pre- and perimenopausal women. BMC Infect. Dis. 2021, 21, 1125. [Google Scholar] [CrossRef]
- Parija, S.C. Neglected tropical diseases. Trop. Parasitol. 2022, 12, 67–68. [Google Scholar] [CrossRef]
- Stensvold, C.R.; Clark, C.G. Pre-empting Pandora’s Box: Blastocystis Subtypes Revisited. Trends Parasitol. 2020, 36, 229–232. [Google Scholar] [CrossRef]
- Mohammadpour, I.; Bozorg-Ghalati, F.; Gazzonis, A.L.; Manfredi, M.T.; Motazedian, M.H.; Mohammadpour, N. First molecular subtyping and phylogeny of Blastocystis sp. isolated from domestic and synanthropic animals (dogs, cats and brown rats) in southern Iran. Parasit. Vectors 2020, 13, 365. [Google Scholar] [CrossRef]
- Stensvold, C.R.; Tan, K.S.W.; Clark, C.G. Blastocystis. Trends Parasitol. 2020, 36, 315–316. [Google Scholar] [CrossRef]
- Khaled, S.; Gantois, N.; Ly, A.T.; Senghor, S.; Even, G.; Dautel, E.; Dejager, R.; Sawant, M.; Baydoun, M.; Benamrouz-Vanneste, S.; et al. Prevalence and Subtype Distribution of Blastocystis sp. in Senegalese School Children. Microorganisms 2020, 8, 1408. [Google Scholar] [CrossRef] [PubMed]
- Beghini, F.; Pasolli, E.; Truong, T.D.; Putignani, L.; Caccio, S.M.; Segata, N. Large-scale comparative metagenomics of Blastocystis, a common member of the human gut microbiome. ISME J. 2017, 11, 2848–2863. [Google Scholar] [CrossRef]
- Sanchez-Aguillon, F.; Lopez-Escamilla, E.; Velez-Perez, F.; Martinez-Flores, W.A.; Rodriguez-Zulueta, P.; Martinez-Ocana, J.; Martinez-Hernandez, F.; Romero-Valdovinos, M.; Maravilla, P. Parasitic infections in a Mexican HIV/AIDS cohort. J. Infect. Dev. Ctries. 2013, 7, 763–766. [Google Scholar] [CrossRef]
- Albrecht, H.; Stellbrink, H.J.; Koperski, K.; Greten, H. Blastocystis hominis in human immunodeficiency virus-related diarrhea. Scand. J. Gastroenterol. 1995, 30, 909–914. [Google Scholar] [CrossRef]
- Bednarska, M.; Jankowska, I.; Pawelas, A.; Piwczynska, K.; Bajer, A.; Wolska-Kusnierz, B.; Wielopolska, M.; Welc-Faleciak, R. Prevalence of Cryptosporidium, Blastocystis, and other opportunistic infections in patients with primary and acquired immunodeficiency. Parasitol. Res. 2018, 117, 2869–2879. [Google Scholar] [CrossRef] [PubMed]
- Deng, L.; Tay, H.; Peng, G.; Lee, J.W.J.; Tan, K.S.W. Prevalence and molecular subtyping of Blastocystis in patients with Clostridium difficile infection, Singapore. Parasit. Vectors 2021, 14, 277. [Google Scholar] [CrossRef]
- Pomari, E.; Ursini, T.; Silva, R.; Leonardi, M.; Ligozzi, M.; Angheben, A. Concomitant Infection of Helicobacter pylori and Intestinal Parasites in Adults Attending a Referral Centre for Parasitic Infections in North Eastern Italy. J. Clin. Med. 2020, 9, 2366. [Google Scholar] [CrossRef] [PubMed]
- Pielok, L.A.; Swarcewicz, J.; Frackowiak, K.; Lisiecka, M. Cryptosporidium spp. and Blastocystis spp. coinfection as a reason of an acute diarrhea in a young healthy veterinary Polish student—Case report. Ann. Agric. Environ. Med. 2022, 29, 592–594. [Google Scholar] [CrossRef]
- Sanchez, A.; Munoz, M.; Gomez, N.; Tabares, J.; Segura, L.; Salazar, A.; Restrepo, C.; Ruiz, M.; Reyes, P.; Qian, Y.; et al. Molecular Epidemiology of Giardia, Blastocystis and Cryptosporidium among Indigenous Children from the Colombian Amazon Basin. Front. Microbiol. 2017, 8, 248. [Google Scholar] [CrossRef]
- Matovelle, C.; Tejedor, M.T.; Monteagudo, L.V.; Beltran, A.; Quilez, J. Prevalence and Associated Factors of Blastocystis sp. Infection in Patients with Gastrointestinal Symptoms in Spain: A Case-Control Study. Trop. Med. Infect. Dis. 2022, 7, 226. [Google Scholar] [CrossRef]
- AMCLI. Available online: https://www.amcli.it/wp-content/uploads/2024/02/2022-25_PARASSITOSI-INTESTINALI.pdf (accessed on 12 December 2024).
- Wormser, G.P.; Hanna, B.A. Manual of Clinical Microbiology, 8th Edition. Edited by Patrick R. Murray, Ellen Jo Baron, James H. Jorgensen, Michael A. Pfaller, and Robert H. Yolken Washington, D.C.: American Society for Microbiology Press, 2003. 2322 pp. $189.95 (cloth). Clin. Infect. Dis. 2004, 38, 1199–1200. [Google Scholar] [CrossRef]
- Zhang, S.X.; Kang, F.Y.; Chen, J.X.; Tian, L.G.; Geng, L.L. Risk factors for Blastocystis infection in HIV/AIDS patients with highly active antiretroviral therapy in Southwest China. Infect. Dis. Poverty 2019, 8, 89. [Google Scholar] [CrossRef]
- Duda, A.; Kosik-Bogacka, D.; Lanocha-Arendarczyk, N.; Kolodziejczyk, L.; Lanocha, A. The prevalence of Blastocystis hominis and other protozoan parasites in soldiers returning from peacekeeping missions. Am. J. Trop. Med. Hyg. 2015, 92, 805–806. [Google Scholar] [CrossRef]
- Parija, S.C.; Jeremiah, S. Blastocystis: Taxonomy, biology and virulence. Trop. Parasitol. 2013, 3, 17–25. [Google Scholar] [CrossRef] [PubMed]
- Abdel-Hafeez, E.H.; Sanadeki, M.M.; Abdelgelil, N.H.; Shaban, N.M.; Abd Rabou, R.A.M. Is co-infection of intestinal parasites with COVID-19 virus infection affecting its severity? Minia J. Med. Res. 2023, 34, 113–122. [Google Scholar] [CrossRef]
- Audebert, C.; Even, G.; Cian, A.; Blastocystis Investigation, G.; Loywick, A.; Merlin, S.; Viscogliosi, E.; Chabe, M. Colonization with the enteric protozoa Blastocystis is associated with increased diversity of human gut bacterial microbiota. Sci. Rep. 2016, 6, 25255. [Google Scholar] [CrossRef]
- Leung, J.M.; Davenport, M.; Wolff, M.J.; Wiens, K.E.; Abidi, W.M.; Poles, M.A.; Cho, I.; Ullman, T.; Mayer, L.; Loke, P. IL-22-producing CD4+ cells are depleted in actively inflamed colitis tissue. Mucosal Immunol. 2014, 7, 124–133. [Google Scholar] [CrossRef]
- El Safadi, D.; Gaayeb, L.; Meloni, D.; Cian, A.; Poirier, P.; Wawrzyniak, I.; Delbac, F.; Dabboussi, F.; Delhaes, L.; Seck, M.; et al. Children of Senegal River Basin show the highest prevalence of Blastocystis sp. ever observed worldwide. BMC Infect. Dis. 2014, 14, 164. [Google Scholar] [CrossRef]
- Jones, M.S.; Whipps, C.M.; Ganac, R.D.; Hudson, N.R.; Boorom, K. Association of Blastocystis subtype 3 and 1 with patients from an Oregon community presenting with chronic gastrointestinal illness. Parasitol. Res. 2009, 104, 341–345. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).