Autotransporter-Mediated Display of Complement Receptor Ligands by Gram-Negative Bacteria Increases Antibody Responses and Limits Disease Severity
Abstract
1. Introduction
2. Results
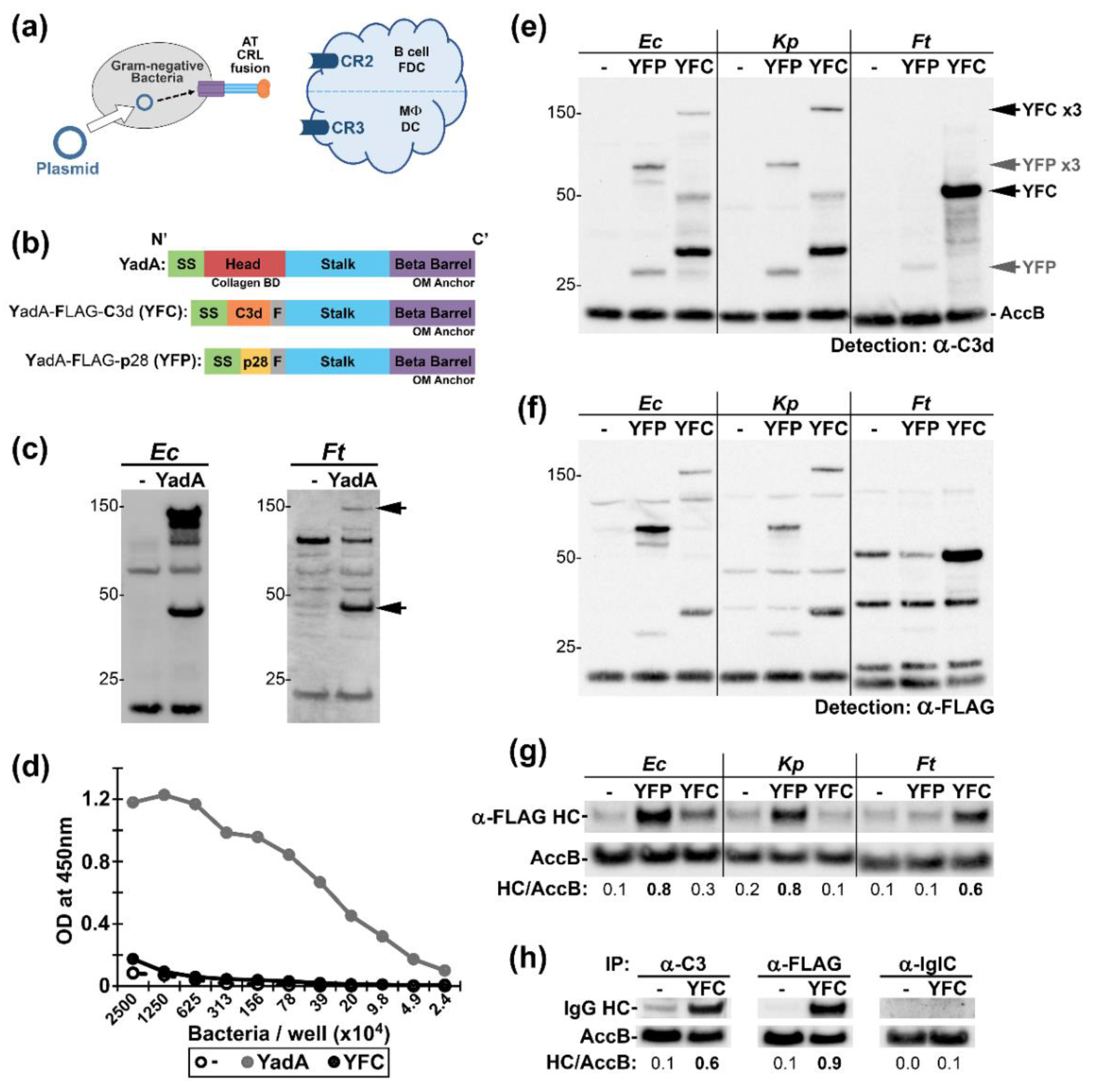
2.1. Conception and Applicability of Autotransporter (AT)—Complement Receptor Ligand (CRL) Fusions to Multiple Gram-Negative Bacteria
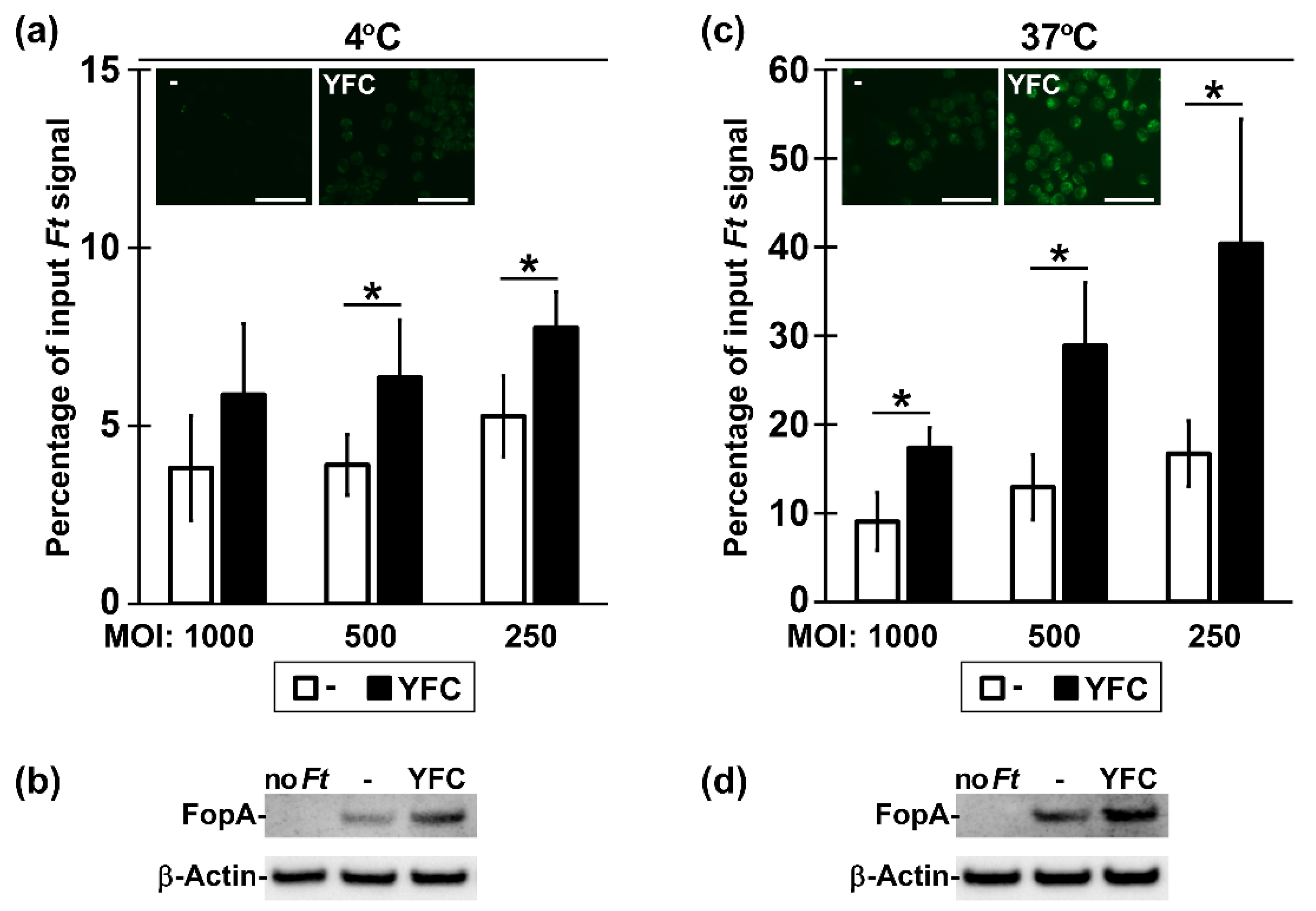
2.2. Bacterial Expression of YFC Enhances Binding and Uptake by Murine Macrophages
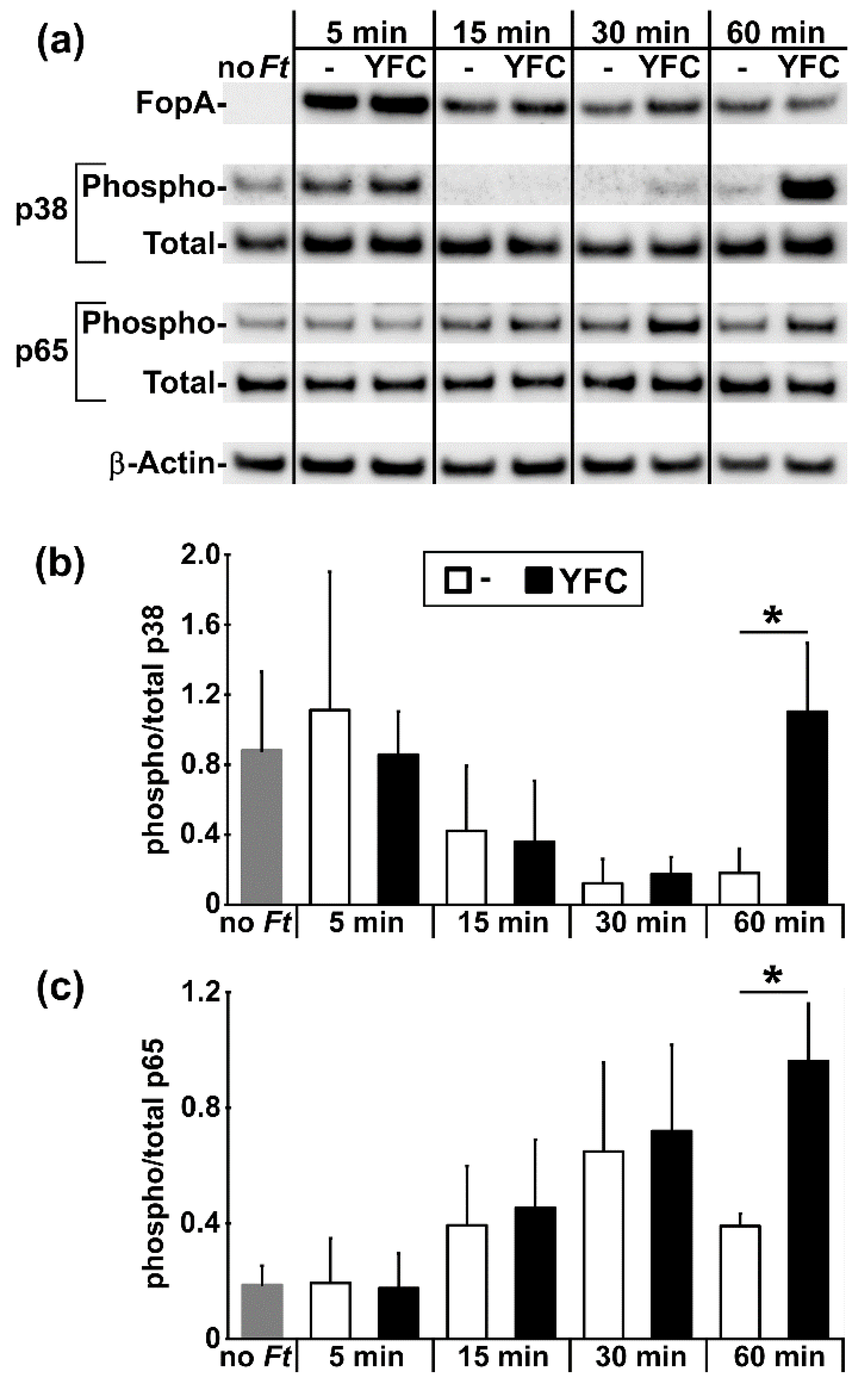
2.3. YFC-Bearing Bacteria Induce Elevated p38 and p65 Phosphorylation in Murine Macrophages
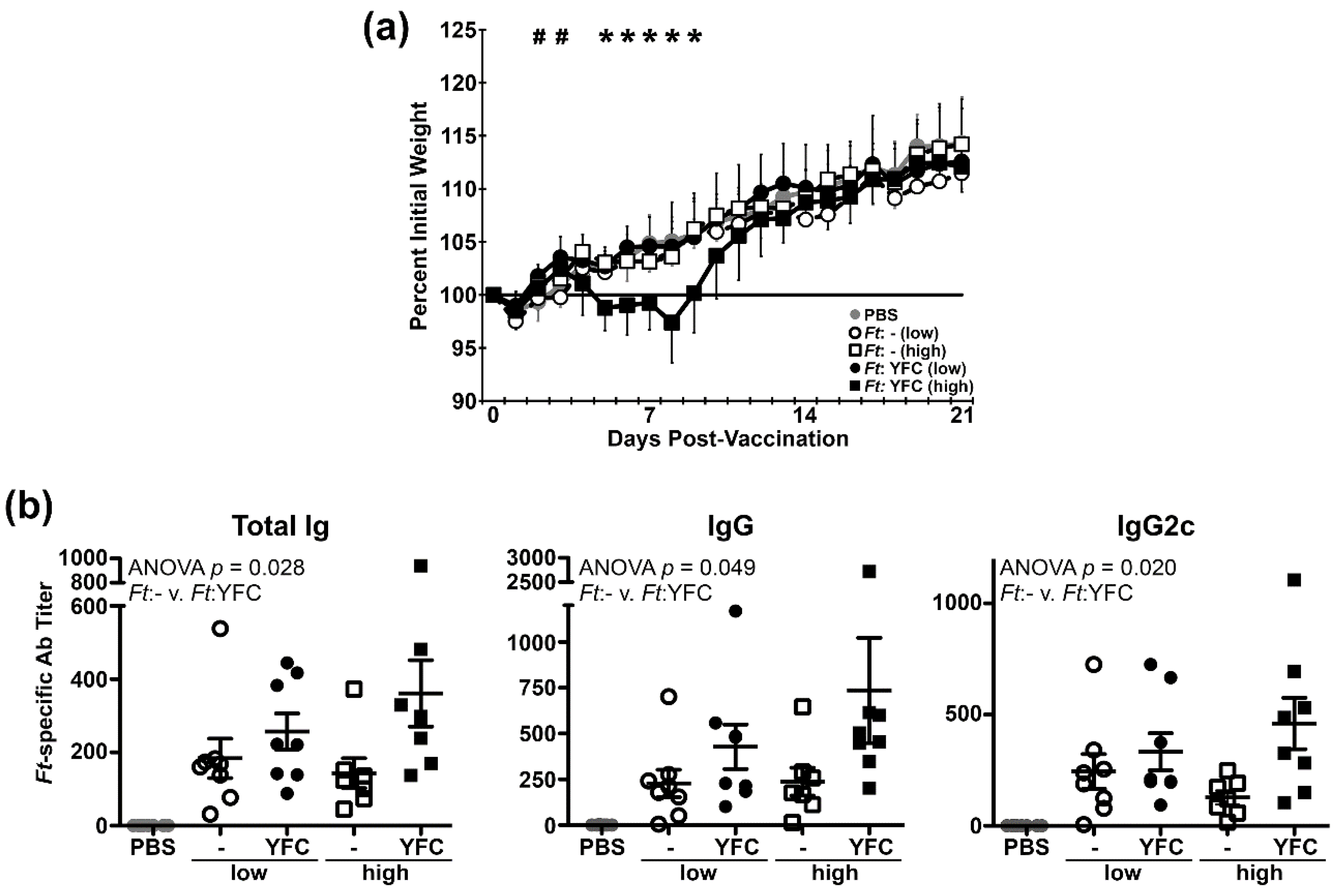
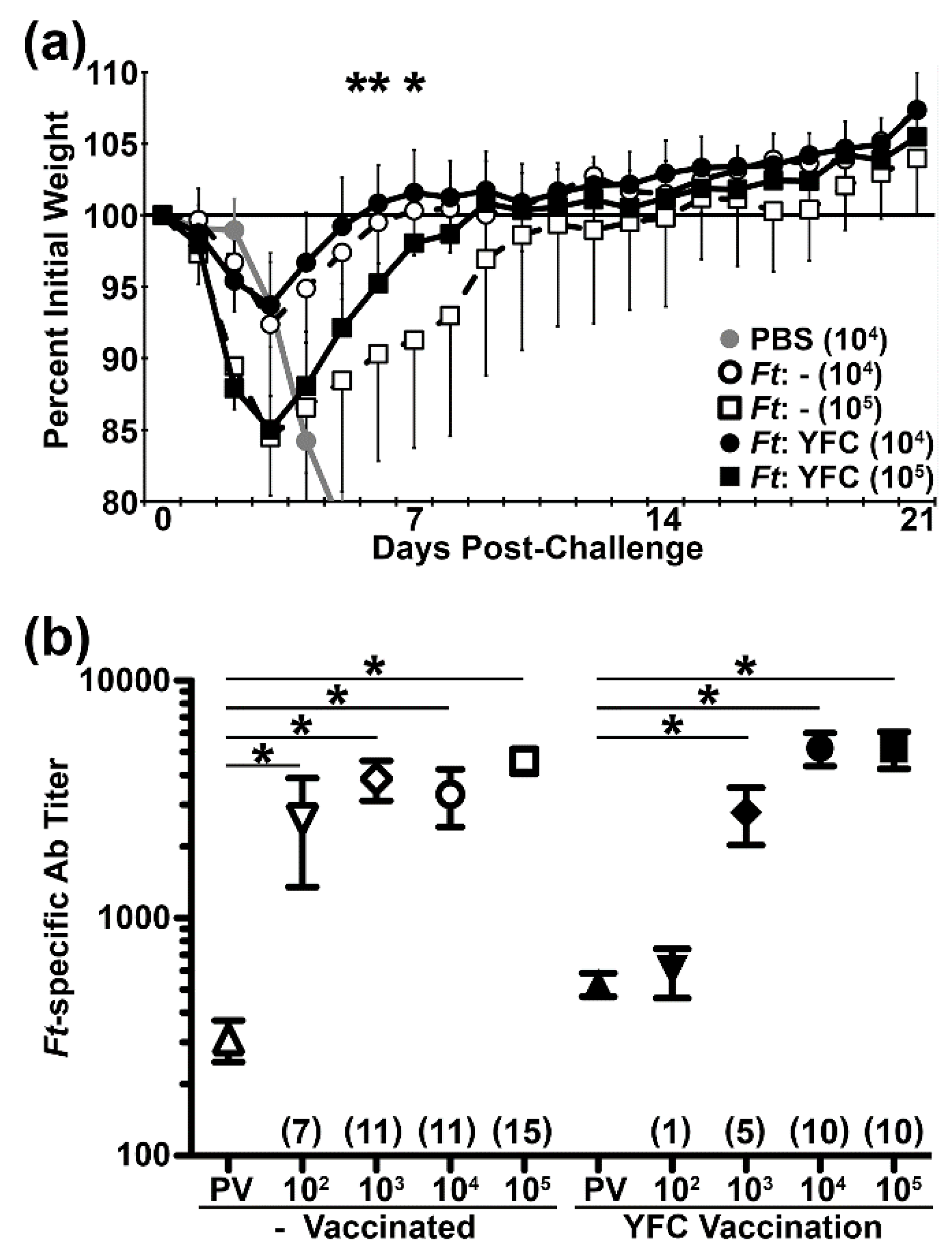
2.4. Infection of Mice with YFC-Bacteria Transiently Limits Weight Gain and Induces Higher Titers of Ab
2.5. Vaccination with YFC-Bacteria Alters Ag Recognition and Limits Morbidity Following Challenge
2.6. Vaccination with YFC-Bacteria Accelerates Recovery Following Challenge with a Heterologous Isolate
3. Discussion
4. Materials and Methods
4.1. Bacteria
4.2. Plasmids
4.3. SDS-PAGE and Western Blots
4.4. Bacterial Fractionation
4.5. Collagen Binding ELISA
4.6. Antibody Immunoprecipitation
4.7. Cell Culture
4.8. Bacteria Staining and Quantification of RAW 264.7 Cell Binding
4.9. RAW 264.7 Cell Signaling Experiments
4.10. Mice and Immunizations
4.11. Antibody Titer Determination
4.12. Statistics
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Del Giudice, G.; Rappuoli, R.; Didierlaurent, A.M. Correlates of adjuvanticity: A review on adjuvants in licensed vaccines. Semin. Immunol. 2018, 39, 14–21. [Google Scholar] [CrossRef] [PubMed]
- Di Pasquale, A.; Preiss, S.; Tavares Da Silva, F.; Garcon, N. Vaccine adjuvants: From 1920 to 2015 and beyond. Vaccines 2015, 3, 320–343. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Wang, Y.; Sun, Y.; Cui, H.; Zhu, S.J.; Qiu, H.J. Mucosal vaccines: Strategies and challenges. Immunol. Lett. 2020, 217, 116–125. [Google Scholar] [CrossRef] [PubMed]
- Rhee, J.H.; Lee, S.E.; Kim, S.Y. Mucosal vaccine adjuvants update. Clin. Exp. Vaccine Res. 2012, 1, 50–63. [Google Scholar] [CrossRef]
- Cohn, L.; Delamarre, L. Dendritic cell-targeted vaccines. Front. Immunol. 2014, 5, 255. [Google Scholar] [CrossRef] [PubMed]
- Tesfaye, D.Y.; Gudjonsson, A.; Bogen, B.; Fossum, E. Targeting conventional dendritic cells to fine-tune antibody responses. Front. Immunol. 2019, 10, 1529. [Google Scholar] [CrossRef]
- Caminschi, I.; Proietto, A.I.; Ahmet, F.; Kitsoulis, S.; Shin Teh, J.; Lo, J.C.; Rizzitelli, A.; Wu, L.; Vremec, D.; van Dommelen, S.L.; et al. The dendritic cell subtype-restricted C-type lectin Clec9A is a target for vaccine enhancement. Blood 2008, 112, 3264–3273. [Google Scholar] [CrossRef]
- Wang, H.; Griffiths, M.N.; Burton, D.R.; Ghazal, P. Rapid antibody responses by low-dose, single-step, dendritic cell-targeted immunization. Proc. Natl. Acad. Sci. USA 2000, 97, 847–852. [Google Scholar] [CrossRef]
- Lysen, A.; Braathen, R.; Gudjonsson, A.; Tesfaye, D.Y.; Bogen, B.; Fossum, E. Dendritic cell targeted Ccl3- and Xcl1-fusion DNA vaccines differ in induced immune responses and optimal delivery site. Sci. Rep. 2019, 9, 1820. [Google Scholar] [CrossRef]
- Park, H.Y.; Light, A.; Lahoud, M.H.; Caminschi, I.; Tarlinton, D.M.; Shortman, K. Evolution of B cell responses to Clec9A-targeted antigen. J. Immunol. 2013, 191, 4919–4925. [Google Scholar] [CrossRef]
- Park, H.Y.; Tan, P.S.; Kavishna, R.; Ker, A.; Lu, J.; Chan, C.E.Z.; Hanson, B.J.; MacAry, P.A.; Caminschi, I.; Shortman, K.; et al. Enhancing vaccine antibody responses by targeting Clec9A on dendritic cells. NPJ Vaccines 2017, 2, 31. [Google Scholar] [CrossRef] [PubMed]
- Layek, B.; Lipp, L.; Singh, J. APC targeted micelle for enhanced intradermal delivery of hepatitis B DNA vaccine. J. Control. Release 2015, 207, 143–153. [Google Scholar] [CrossRef] [PubMed]
- Muhamad, N.; Plengsuriyakarn, T.; Na-Bangchang, K. Application of active targeting nanoparticle delivery system for chemotherapeutic drugs and traditional/herbal medicines in cancer therapy: A systematic review. Int. J. Nanomed. 2018, 13, 3921–3935. [Google Scholar] [CrossRef] [PubMed]
- Goyvaerts, C.; Breckpot, K. Pros and cons of antigen-presenting cell targeted tumor vaccines. J. Immunol. Res. 2015, 2015, 785634. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Liu, S.; Lyu, H.; Riker, A.I.; Zhang, Y.; Liu, B. Development of effective therapeutics targeting HER3 for cancer treatment. Biol. Proced. Online 2019, 21, 5. [Google Scholar] [CrossRef] [PubMed]
- Sancho, D.; Mourao-Sa, D.; Joffre, O.P.; Schulz, O.; Rogers, N.C.; Pennington, D.J.; Carlyle, J.R.; Reis e Sousa, C. Tumor therapy in mice via antigen targeting to a novel, DC-restricted C-type lectin. J. Clin. Investig. 2008, 118, 2098–2110. [Google Scholar] [CrossRef]
- Iglesias, B.V.; Bitsaktsis, C.; Pham, G.; Drake, J.R.; Hazlett, K.R.O.; Porter, K.; Gosselin, E.J. Multiple mechanisms mediate enhanced immunity generated by mAb-inactivated F. tularensis immunogen. Immunol. Cell Biol. 2013, 91, 139–148. [Google Scholar] [CrossRef][Green Version]
- Rawool, D.B.; Bitsaktsis, C.; Li, Y.; Gosselin, D.R.; Lin, Y.; Kurkure, N.V.; Metzger, D.W.; Gosselin, E.J. Utilization of Fc receptors as a mucosal vaccine strategy against an intracellular bacterium, Francisella tularensis. J. Immunol. 2008, 180, 5548–5557. [Google Scholar] [CrossRef]
- Carroll, M.C.; Isenman, D.E. Regulation of humoral immunity by complement. Immunity 2012, 37, 199–207. [Google Scholar] [CrossRef]
- Merle, N.S.; Church, S.E.; Fremeaux-Bacchi, V.; Roumenina, L.T. Complement system part I—Molecular mechanisms of activation and regulation. Front. Immunol. 2015, 6, 262. [Google Scholar] [CrossRef]
- Toapanta, F.R.; Ross, T.M. Complement-mediated activation of the adaptive immune responses: Role of C3d in linking the innate and adaptive immunity. Immunol. Res. 2006, 36, 197–210. [Google Scholar] [CrossRef]
- Dempsey, P.W.; Allison, M.E.; Akkaraju, S.; Goodnow, C.C.; Fearon, D.T. C3d of complement as a molecular adjuvant: Bridging innate and acquired immunity. Science 1996, 271, 348–350. [Google Scholar] [CrossRef] [PubMed]
- De Groot, A.S.; Ross, T.M.; Levitz, L.; Messitt, T.J.; Tassone, R.; Boyle, C.M.; Vincelli, A.J.; Moise, L.; Martin, W.; Knopf, P.M. C3d adjuvant effects are mediated through the activation of C3d-specific autoreactive T cells. Immunol. Cell Biol. 2015, 93, 189–197. [Google Scholar] [CrossRef] [PubMed]
- Bajic, G.; Yatime, L.; Sim, R.B.; Vorup-Jensen, T.; Andersen, G.R. Structural insight on the recognition of surface-bound opsonins by the integrin I domain of complement receptor 3. Proc. Natl. Acad. Sci. USA 2013, 110, 16426–16431. [Google Scholar] [CrossRef] [PubMed]
- Henson, S.E.; Smith, D.; Boackle, S.A.; Holers, V.M.; Karp, D.R. Generation of recombinant human C3dg tetramers for the analysis of CD21 binding and function. J. Immunol. Methods 2001, 258, 97–109. [Google Scholar] [CrossRef]
- Musa, H.H.; Zhang, W.J.; Lv, J.; Duan, X.L.; Yang, Y.; Zhu, C.H.; Li, H.F.; Chen, K.W.; Meng, X.; Zhu, G.Q. The molecular adjuvant mC3d enhances the immunogenicity of FimA from type I fimbriae of Salmonella enterica serovar Enteritidis. J. Microbiol. Immunol. Infect. 2014, 47, 57–62. [Google Scholar] [CrossRef]
- Green, T.D.; Montefiori, D.C.; Ross, T.M. Enhancement of antibodies to the human immunodeficiency virus type 1 envelope by using the molecular adjuvant C3d. J. Virol. 2003, 77, 2046–2055. [Google Scholar] [CrossRef][Green Version]
- Haas, K.M.; Toapanta, F.R.; Oliver, J.A.; Poe, J.C.; Weis, J.H.; Karp, D.R.; Bower, J.F.; Ross, T.M.; Tedder, T.F. Cutting edge: C3d functions as a molecular adjuvant in the absence of CD21/35 expression. J. Immunol. 2004, 172, 5833–5837. [Google Scholar] [CrossRef]
- Test, S.T.; Mitsuyoshi, J.; Connolly, C.C.; Lucas, A.H. Increased immunogenicity and induction of class switching by conjugation of complement C3d to pneumococcal serotype 14 capsular polysaccharide. Infect. Immunol. 2001, 69, 3031–3040. [Google Scholar] [CrossRef]
- Pompa-Mera, E.N.; Arroyo-Matus, P.; Ocana-Mondragon, A.; Gonzalez-Bonilla, C.R.; Yepez-Mulia, L. Protective immunity against enteral stages of Trichinella spiralis elicited in mice by live attenuated Salmonella vaccine that secretes a 30-mer parasite epitope fused to the molecular adjuvant C3d-P28. Res. Vet. Sci. 2014, 97, 533–545. [Google Scholar] [CrossRef]
- Tozakidis, I.E.P.; Sichwart, S.; Jose, J. Going beyond E. coli: Autotransporter based surface display on alternative host organisms. New Biotechnol. 2015, 32, 644–650. [Google Scholar] [CrossRef] [PubMed]
- Cotter, S.E.; Surana, N.K.; St Geme, J.W. 3rd. Trimeric autotransporters: A distinct subfamily of autotransporter proteins. Trends Microbiol. 2005, 13, 199–205. [Google Scholar] [CrossRef] [PubMed]
- Emody, L.; Heesemann, J.; Wolf-Watz, H.; Skurnik, M.; Kapperud, G.; O’Toole, P.; Wadstrom, T. Binding to collagen by Yersinia enterocolitica and Yersinia pseudotuberculosis: Evidence for yopA-mediated and chromosomally encoded mechanisms. J. Bacteriol. 1989, 171, 6674–6679. [Google Scholar] [CrossRef] [PubMed]
- Roggenkamp, A.; Ackermann, N.; Jacobi, C.A.; Truelzsch, K.; Hoffmann, H.; Heesemann, J. Molecular analysis of transport and oligomerization of the Yersinia enterocolitica adhesin YadA. J. Bacteriol. 2003, 185, 3735–3744. [Google Scholar] [CrossRef]
- Schulze-Koops, H.; Burkhardt, H.; Heesemann, J.; von der Mark, K.; Emmrich, F. Characterization of the binding region for the Yersinia enterocolitica adhesin YadA on types I and II collagen. Arthritis Rheum. 1995, 38, 1283–1289. [Google Scholar] [CrossRef]
- Gaither, T.A.; Vargas, I.; Inada, S.; Frank, M.M. The complement fragment C3d facilitates phagocytosis by monocytes. Immunology 1987, 62, 405–411. [Google Scholar]
- Jensen, M.R.; Bajic, G.; Zhang, X.; Laustsen, A.K.; Koldso, H.; Skeby, K.K.; Schiott, B.; Andersen, G.R.; Vorup-Jensen, T. Structural basis for simvastatin competitive antagonism of complement receptor 3. J. Biol. Chem. 2016, 291, 16963–16976. [Google Scholar] [CrossRef]
- Bower, J.F.; Ross, T.M. A minimum CR2 binding domain of C3d enhances immunity following vaccination. Adv. Exp. Med. Biol. 2006, 586, 249–264. [Google Scholar]
- Holland, K.M.; Rosa, S.J.; Kristjansdottir, K.; Wolfgeher, D.; Franz, B.J.; Zarrella, T.M.; Kumar, S.; Sunagar, R.; Singh, A.; Bakshi, C.S.; et al. Differential growth of Francisella tularensis, which alters expression of virulence factors, dominant antigens, and surface-carbohydrate synthases, governs the apparent virulence of Ft SchuS4 to immunized animals. Front. Microbiol. 2017, 8, 1158. [Google Scholar] [CrossRef]
- Feng, Y.; Chin, C.Y.; Chakravartty, V.; Gao, R.; Crispell, E.K.; Weiss, D.S.; Cronan, J.E. The atypical occurrence of two biotin protein ligases in francisella novicida is due to distinct roles in virulence and biotin metabolism. MBio 2015, 6, e00591. [Google Scholar] [CrossRef]
- Brock, S.R.; Parmely, M.J. Francisella tularensis confronts the complement system. Front. Cell Infect. Microbiol. 2017, 7, 523. [Google Scholar] [CrossRef]
- McLendon, M.K.; Apicella, M.A.; Allen, L.A. Francisella tularensis: Taxonomy, genetics, and Immunopathogenesis of a potential agent of biowarfare. Annu. Rev. Microbiol. 2006, 60, 167–185. [Google Scholar] [CrossRef]
- Dai, S.; Rajaram, M.V.; Curry, H.M.; Leander, R.; Schlesinger, L.S. Fine tuning inflammation at the front door: Macrophage complement receptor 3-mediates phagocytosis and immune suppression for Francisella tularensis. PLoS Pathog. 2013, 9, e1003114. [Google Scholar] [CrossRef] [PubMed]
- Edwards, M.W.; Aultman, J.A.; Harber, G.; Bhatt, J.M.; Sztul, E.; Xu, Q.; Zhang, P.; Michalek, S.M.; Katz, J. Role of mTOR downstream effector signaling molecules in Francisella tularensis internalization by murine macrophages. PLoS ONE 2013, 8, e83226. [Google Scholar] [CrossRef] [PubMed]
- Medina, E.A.; Morris, I.R.; Berton, M.T. Phosphatidylinositol 3-kinase activation attenuates the TLR2-mediated macrophage proinflammatory cytokine response to Francisella tularensis live vaccine strain. J. Immunol. 2010, 185, 7562–7572. [Google Scholar] [CrossRef] [PubMed]
- Saint, R.J.; D’Elia, R.V.; Bryant, C.; Clark, G.C.; Atkins, H.S. Mitogen-activated protein kinases (MAPKs) are modulated during Francisella tularensis infection, but inhibition of extracellular-signal-regulated kinases (ERKs) is of limited therapeutic benefit. Eur. J. Clin. Microbiol. Infect. Dis. 2016, 35, 2015–2024. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Telepnev, M.; Golovliov, I.; Sjostedt, A. Francisella tularensis LVS initially activates but subsequently down-regulates intracellular signaling and cytokine secretion in mouse monocytic and human peripheral blood mononuclear cells. Microb. Pathog. 2005, 38, 239–247. [Google Scholar] [CrossRef]
- Griffin, A.J.; Crane, D.D.; Wehrly, T.D.; Bosio, C.M. Successful protection against tularemia in C57BL/6 mice is correlated with expansion of Francisella tularensis-specific effector T cells. Clin. Vaccine Immunol. 2015, 22, 119–128. [Google Scholar] [CrossRef]
- Gonzalez, S.F.; Lukacs-Kornek, V.; Kuligowski, M.P.; Pitcher, L.A.; Degn, S.E.; Turley, S.J.; Carroll, M.C. Complement-dependent transport of antigen into B cell follicles. J. Immunol. 2010, 185, 2659–2664. [Google Scholar] [CrossRef]
- Plzakova, L.; Krocova, Z.; Kubelkova, K.; Macela, A. Entry of Francisella tularensis into Murine B Cells: The role of B Cell receptors and complement receptors. PLoS ONE 2015, 10, e0132571. [Google Scholar] [CrossRef]
- Ulrich, T.; Oberhettinger, P.; Schutz, M.; Holzer, K.; Ramms, A.S.; Linke, D.; Autenrieth, I.B.; Rapaport, D. Evolutionary conservation in biogenesis of beta-barrel proteins allows mitochondria to assemble a functional bacterial trimeric autotransporter protein. J. Biol. Chem. 2014, 289, 29457–29470. [Google Scholar] [CrossRef] [PubMed]
- Hajishengallis, G.; Lambris, J.D. Crosstalk pathways between Toll-like receptors and the complement system. Trends Immunol. 2010, 31, 154–163. [Google Scholar] [CrossRef] [PubMed]
- Harokopakis, E.; Hajishengallis, G. Integrin activation by bacterial fimbriae through a pathway involving CD14, Toll-like receptor 2, and phosphatidylinositol-3-kinase. Eur. J. Immunol. 2005, 35, 1201–1210. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Shakhatreh, M.-A.K.; James, D.; Liang, S.; Nishiyama, S.-I.; Yoshimura, F.; Demuth, D.R.; Hajishengallis, G. Fimbrial proteins of porphyromonas gingivalis mediate in vivo virulence and exploit TLR2 and complement receptor 3 to persist in macrophages. J. Immunol. 2007, 179, 2349–2358. [Google Scholar] [CrossRef]
- Lee, J.O.; Bankston, L.A.; Arnaout, M.A.; Liddington, R.C. Two conformations of the integrin A-domain (I-domain): A pathway for activation? Structure 1995, 3, 1333–1340. [Google Scholar] [CrossRef]
- Oxvig, C.; Lu, C.; Springer, T.A. Conformational changes in tertiary structure near the ligand binding site of an integrin I domain. Proc. Natl. Acad. Sci. USA 1999, 96, 2215–2220. [Google Scholar] [CrossRef]
- Fabrik, I.; Link, M.; Putzova, D.; Plzakova, L.; Lubovska, Z.; Philimonenko, V.; Pavkova, I.; Rehulka, P.; Krocova, Z.; Hozak, P.; et al. The early dendritic cell signaling induced by virulent francisella tularensis strain occurs in phases and involves the activation of extracellular signal-regulated kinases (ERKs) and p38 in the later stage. Mol. Cell Proteom. 2018, 17, 81–94. [Google Scholar] [CrossRef]
- Arbore, G.; Kemper, C.; Kolev, M. Intracellular complement—The complosome—In immune cell regulation. Mol. Immunol. 2017, 89, 2–9. [Google Scholar] [CrossRef]
- Liszewski, M.K.; Elvington, M.; Kulkarni, H.S.; Atkinson, J.P. Complement’s hidden arsenal: New insights and novel functions inside the cell. Mol. Immunol. 2017, 84, 2–9. [Google Scholar] [CrossRef]
- Reichhardt, M.P.; Meri, S. Intracellular complement activation-An alarm raising mechanism? Semin. Immunol. 2018, 38, 54–62. [Google Scholar] [CrossRef]
- Tam, J.C.; Bidgood, S.R.; McEwan, W.A.; James, L.C. Intracellular sensing of complement C3 activates cell autonomous immunity. Science 2014, 345, 1256070. [Google Scholar] [CrossRef] [PubMed]
- Sorbara, M.T.; Foerster, E.G.; Tsalikis, J.; Abdel-Nour, M.; Mangiapane, J.; Sirluck-Schroeder, I.; Tattoli, I.; van Dalen, R.; Isenman, D.E.; Rohde, J.R.; et al. Complement C3 drives autophagy-dependent restriction of cyto-invasive bacteria. Cell Host Microbe 2018, 23, 644–652 e645. [Google Scholar] [CrossRef] [PubMed]
- Steele, S.; Radlinski, L.; Taft-Benz, S.; Brunton, J.; Kawula, T.H. Trogocytosis-associated cell to cell spread of intracellular bacterial pathogens. Elife 2016, 5, e10625. [Google Scholar] [CrossRef] [PubMed]
- Brock, S.R.; Parmely, M.J. Complement C3 as a prompt for human macrophage death during infection with francisella tularensis strain SCHU S4. Infect. Immun. 2017, 85, e00424-17. [Google Scholar] [CrossRef]
- Checroun, C.; Wehrly, T.D.; Fischer, E.R.; Hayes, S.F.; Celli, J. Autophagy-mediated reentry of Francisella tularensis into the endocytic compartment after cytoplasmic replication. Proc. Natl. Acad. Sci. USA 2006, 103, 14578–14583. [Google Scholar] [CrossRef]
- Lai, X.H.; Xu, Y.; Chen, X.M.; Ren, Y. Macrophage cell death upon intracellular bacterial infection. Macrophage 2015, 2, e779. [Google Scholar] [CrossRef]
- Case, E.D.; Chong, A.; Wehrly, T.D.; Hansen, B.; Child, R.; Hwang, S.; Virgin, H.W.; Celli, J. The Francisella O-antigen mediates survival in the macrophage cytosol via autophagy avoidance. Cell Microbiol. 2014, 16, 862–877. [Google Scholar] [CrossRef]
- Bradt, V.; Malafa, S.; von Braun, A.; Jarmer, J.; Tsouchnikas, G.; Medits, I.; Wanke, K.; Karrer, U.; Stiasny, K.; Heinz, F.X. Pre-existing yellow fever immunity impairs and modulates the antibody response to tick-borne encephalitis vaccination. NPJ Vaccines 2019, 4, 38. [Google Scholar] [CrossRef]
- Memoli, M.J.; Czajkowski, L.; Reed, S.; Athota, R.; Bristol, T.; Proudfoot, K.; Fargis, S.; Stein, M.; Dunfee, R.L.; Shaw, P.A.; et al. Validation of the wild-type influenza A human challenge model H1N1pdMIST: An A(H1N1)pdm09 dose-finding investigational new drug study. Clin. Infect. Dis. 2015, 60, 693–702. [Google Scholar] [CrossRef]
- Ndungo, E.; Randall, A.; Hazen, T.H.; Kania, D.A.; Trappl-Kimmons, K.; Liang, X.; Barry, E.M.; Kotloff, K.L.; Chakraborty, S.; Mani, S.; et al. A novel shigella proteome microarray discriminates targets of human antibody reactivity following oral vaccination and experimental challenge. mSphere 2018, 3, e00260-18. [Google Scholar] [CrossRef]
- Park, J.K.; Han, A.; Czajkowski, L.; Reed, S.; Athota, R.; Bristol, T.; Rosas, L.A.; Cervantes-Medina, A.; Taubenberger, J.K.; Memoli, M.J. Evaluation of preexisting anti-hemagglutinin stalk antibody as a correlate of protection in a healthy volunteer challenge with influenza A/H1N1pdm virus. MBio 2018, 9, e02284-17. [Google Scholar] [CrossRef] [PubMed]
- Shimanovich, A.A.; Buskirk, A.D.; Heine, S.J.; Blackwelder, W.C.; Wahid, R.; Kotloff, K.L.; Pasetti, M.F. Functional and antigen-specific serum antibody levels as correlates of protection against shigellosis in a controlled human challenge study. Clin. Vaccine Immunol. 2017, 24, e00412-16. [Google Scholar] [CrossRef] [PubMed]
- Hirschmann, J.V. From squirrels to biological weapons: The early history of tularemia. Am. J. Med. Sci. 2018, 356, 319–328. [Google Scholar] [CrossRef] [PubMed]
- Ramirez, M.S.; Traglia, G.M.; Lin, D.L.; Tran, T.; Tolmasky, M.E. Plasmid-mediated antibiotic resistance and virulence in gram-negatives: The klebsiella pneumoniae paradigm. Microbiol. Spectr. 2014, 2, 459–474. [Google Scholar] [CrossRef]
- Zarrella, T.M.; Singh, A.; Bitsaktsis, C.; Rahman, T.; Sahay, B.; Feustel, P.J.; Gosselin, E.J.; Sellati, T.J.; Hazlett, K.R.O. Host-adaptation of Francisella tularensis alters the bacterium’s surface-carbohydrates to hinder effectors of innate and adaptive immunity. PLoS ONE 2011, 6, e22335. [Google Scholar] [CrossRef][Green Version]

© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Holland-Tummillo, K.M.; Shoudy, L.E.; Steiner, D.; Kumar, S.; Rosa, S.J.; Namjoshi, P.; Singh, A.; Sellati, T.J.; Gosselin, E.J.; Hazlett, K.R. Autotransporter-Mediated Display of Complement Receptor Ligands by Gram-Negative Bacteria Increases Antibody Responses and Limits Disease Severity. Pathogens 2020, 9, 375. https://doi.org/10.3390/pathogens9050375
Holland-Tummillo KM, Shoudy LE, Steiner D, Kumar S, Rosa SJ, Namjoshi P, Singh A, Sellati TJ, Gosselin EJ, Hazlett KR. Autotransporter-Mediated Display of Complement Receptor Ligands by Gram-Negative Bacteria Increases Antibody Responses and Limits Disease Severity. Pathogens. 2020; 9(5):375. https://doi.org/10.3390/pathogens9050375
Chicago/Turabian StyleHolland-Tummillo, Kristen M, Lauren E Shoudy, Donald Steiner, Sudeep Kumar, Sarah J Rosa, Prachi Namjoshi, Anju Singh, Timothy J Sellati, Edmund J Gosselin, and Karsten RO Hazlett. 2020. "Autotransporter-Mediated Display of Complement Receptor Ligands by Gram-Negative Bacteria Increases Antibody Responses and Limits Disease Severity" Pathogens 9, no. 5: 375. https://doi.org/10.3390/pathogens9050375
APA StyleHolland-Tummillo, K. M., Shoudy, L. E., Steiner, D., Kumar, S., Rosa, S. J., Namjoshi, P., Singh, A., Sellati, T. J., Gosselin, E. J., & Hazlett, K. R. (2020). Autotransporter-Mediated Display of Complement Receptor Ligands by Gram-Negative Bacteria Increases Antibody Responses and Limits Disease Severity. Pathogens, 9(5), 375. https://doi.org/10.3390/pathogens9050375





