Extended-Spectrum β-lactamase-Producing Enterobacteriaceae Shedding in Farm Horses Versus Hospitalized Horses: Prevalence and Risk Factors
Abstract
:Simple summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Equine Study Cohorts, Study Design, and Sampling Methods
2.2. Demographic and Medical Data
2.3. ESBL-E Isolation and Species Identification
2.4. Molecular Characterization of ESBL-E
2.5. Sample Size and Statistical Analysis
3. Results
3.1. Characterization of the Equine Study Populations (Table 1)
3.2. Antibiotic Therapy, Surgical Procedures, Length of Stay, and Outcome
3.3. Prevalence of ESBL-E Shedding
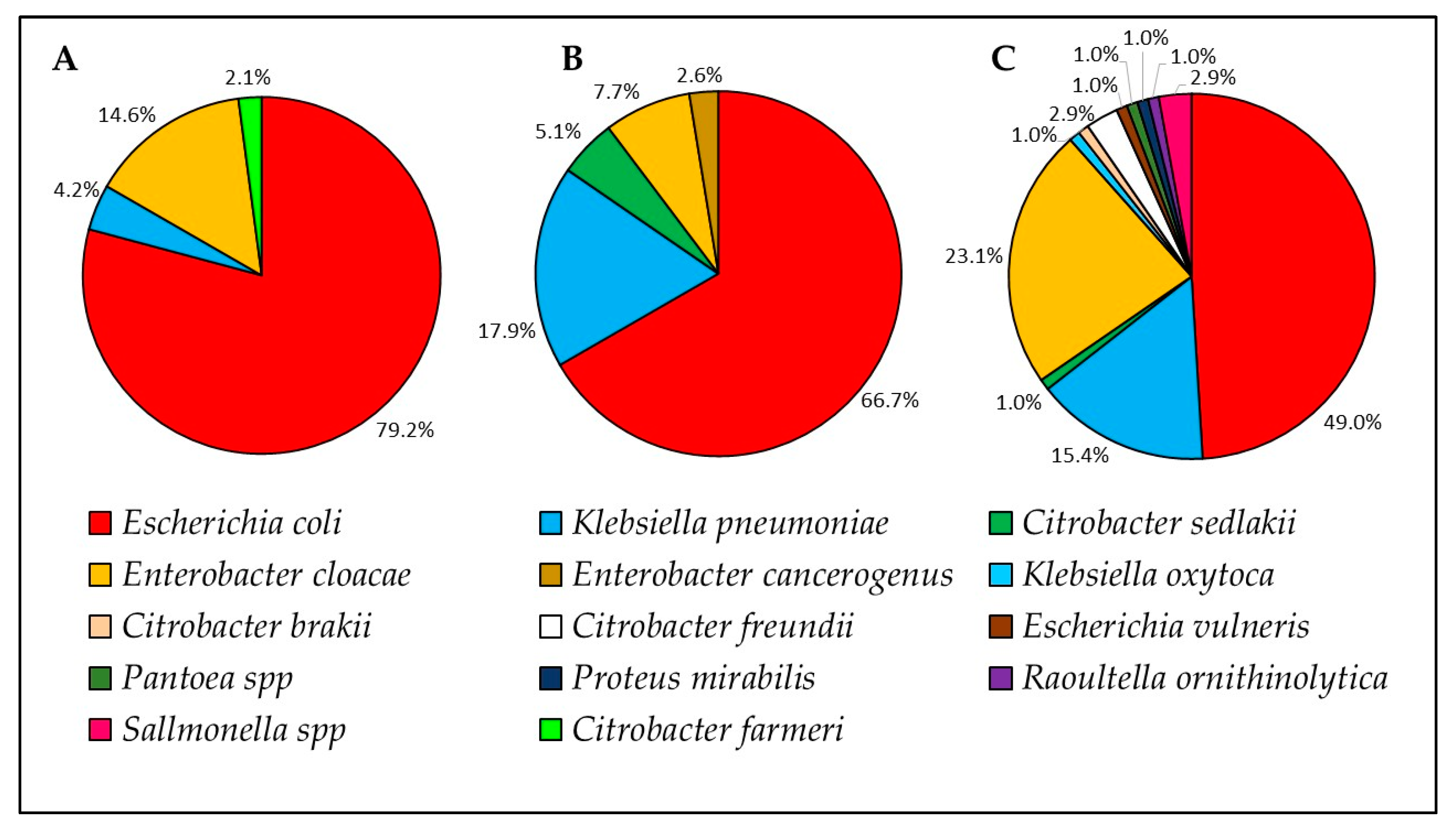
3.4. Distribution of ESBL-E Species and ESBL Genes
3.5. Antibiotic Susceptibility Profiles
3.6. Risk Factor Analysis for ESBL-E Shedding
3.6.1. Farm Horses
3.6.2. Horses on Admission
3.6.3. Horses During Hospitalization
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
| Num. | Horse Serial Number | Isolate | Origin | Bacterial ID | AMC | IMP | ENR | CHL | GEN | AMK | TMS | MDR |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 1 | 1.1.1 | On admission | Escherichia coli | 2 | 0 | 1 | 2 | 2 | 0 | 0 | 1 |
| 2 | 2 | 2.1.1 | Escherichia coli | 2 | 0 | 0 | 2 | 2 | 1 | 2 | 1 | |
| 3 | 3 | 3.1.1 | Escherichia coli | 2 | 0 | 0 | 2 | 2 | 1 | 2 | 1 | |
| 4 | 6 | 6.1.1 | Citrobacter sedlakii | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 5 | 7 | 7.1.1 | Klebsiella pneumoniae | 2 | 0 | 1 | 2 | 2 | 0 | 2 | 1 | |
| 6 | 15 | 15.1.1 | Escherichia coli | 2 | 0 | 1 | 2 | 2 | 1 | 2 | 1 | |
| 7 | 15 | 15.1.2 | Klebsiella pneumoniae | 2 | 0 | 2 | 0 | 2 | 1 | 2 | 1 | |
| 8 | 17 | 17.1.2 | Klebsiella pneumoniae | 2 | 0 | 1 | 0 | 0 | 0 | 2 | 1 | |
| 9 | 22 | 22.1.1 | Escherichia coli | 2 | 0 | 0 | 2 | 2 | 1 | 2 | 1 | |
| 10 | 22 | 22.1.2 | Klebsiella pneumoniae | 2 | 0 | 1 | 0 | 2 | 0 | 2 | 1 | |
| 11 | 31 | 31.1.1 | Escherichia coli | 1 | 0 | 0 | 2 | 2 | 1 | 2 | 1 | |
| 12 | 32 | 32.1.1 | Escherichia coli | 2 | 0 | 1 | 2 | 0 | 0 | 2 | 1 | |
| 13 | 46 | 46.1.1 | Enterobacter cloacae | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 14 | 60 | 60.1.1 | Escherichia coli | 2 | 0 | 1 | 0 | 0 | 0 | 2 | 1 | |
| 15 | 74 | 74.1.2 | Enterobacter cloacae | 2 | 0 | 2 | 2 | 2 | 2 | 2 | 1 | |
| 16 | 77 | 77.1.1 | Escherichia coli | 2 | 0 | 1 | 0 | 0 | 0 | 2 | 1 | |
| 17 | 81 | 81.1.1 | Escherichia coli | 2 | 0 | 1 | 2 | 2 | 0 | 2 | 1 | |
| 18 | 101 | 101.1.1 | Escherichia coli | 2 | 0 | 2 | 2 | 2 | 0 | 2 | 1 | |
| 19 | 101 | 101.1.2 | Klebsiella pneumoniae | 2 | 0 | 1 | 0 | 0 | 0 | 2 | 0 | |
| 20 | 107 | 107.1.1 | Escherichia coli | 2 | 0 | 1 | 0 | 0 | 0 | 2 | 1 | |
| 21 | 112 | 112.1.1 | Enterobacter cloacae | 2 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | |
| 22 | 113 | 113.1.1 | Escherichia coli | 2 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | |
| 23 | 120 | 120.1.1 | Escherichia coli | 1 | 0 | 2 | 2 | 2 | 1 | 2 | 1 | |
| 24 | 121 | 121.1.1 | Escherichia coli | 2 | 1 | 2 | 2 | 0 | 0 | 0 | 1 | |
| 25 | 136 | 136.1.1 | Escherichia coli | 2 | 0 | 2 | 2 | 0 | 0 | 2 | 1 | |
| 26 | 136 | 136.1.2 | Klebsiella pneumoniae | 2 | 0 | 2 | 0 | 2 | 1 | 2 | 1 | |
| 27 | 144 | 144.1.1 | Escherichia coli | 2 | 0 | 1 | 2 | 2 | 1 | 2 | 1 | |
| 28 | 153 | 153.1.1 | Escherichia coli | 2 | 0 | 1 | 0 | 0 | 0 | 2 | 0 | |
| 29 | 162 | 162.1.1 | Escherichia coli | 2 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | |
| 30 | 176 | 176.1.1 | Escherichia coli | 2 | 0 | 1 | 2 | 2 | 1 | 2 | 1 | |
| 31 | 177 | 177.1.1 | Escherichia coli | 1 | 0 | 1 | 2 | 2 | 0 | 2 | 1 | |
| 32 | 179 | 179.1.1 | Escherichia coli | 1 | 0 | 0 | 2 | 2 | 0 | 2 | 1 | |
| 33 | 203 | 203.1.1 | Klebsiella pneumoniae | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | |
| 34 | 239 | 239.1.1 | Enterobacter cancerogenus | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 35 | 244 | 244.1.1 | Citrobacter sedlakii | 0 | 0 | 0 | 0 | 0 | 0 | |||
| 36 | 267 | 267.1.1 | Escherichia coli | 2 | 0 | 1 | 0 | 0 | 0 | 2 | 1 | |
| 37 | 278 | 278.1.1 | Escherichia coli | 2 | 0 | 1 | 0 | 0 | 0 | 2 | 1 | |
| 38 | 288 | 288.1.1 | Escherichia coli | 2 | 0 | 1 | 0 | 0 | 0 | 2 | 1 | |
| 39 | 290 | 290.1.1 | Escherichia coli | 2 | 0 | 1 | 0 | 0 | 0 | 2 | 1 | |
| 40 | 1 | 1.2.2 | During hospitalization | Klebsiella pneumoniae | 0 | 0 | 1 | 0 | 2 | 0 | 2 | 1 |
| 41 | 5 | 5.2.1 | Escherichia coli | 0 | 0 | 0 | 2 | 2 | 0 | 2 | 1 | |
| 42 | 6 | 6.2.1 | Klebsiella pneumoniae | 1 | 0 | 2 | 0 | 0 | 0 | 2 | 1 | |
| 43 | 6 | 6.2.2 | Escherichia coli | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | |
| 44 | 7 | 7.2.1 | Escherichia coli | 1 | 0 | 0 | 0 | 2 | 0 | 2 | 1 | |
| 45 | 7 | 7.2.2 | Klebsiella pneumoniae | 1 | 0 | 2 | 2 | 2 | 0 | 2 | 1 | |
| 46 | 8 | 8.2.1 | Escherichia coli | 2 | 0 | 1 | 2 | 2 | 1 | |||
| 47 | 8 | 8.2.2 | Enterobacter cloacae | 2 | 0 | 2 | 2 | 2 | 0 | 2 | 1 | |
| 48 | 15 | 15.2.1 | Escherichia coli | 1 | 0 | 2 | 2 | 2 | 0 | 2 | 1 | |
| 49 | 15 | 15.2.2 | Enterobacter cloacae | 2 | 0 | 1 | 2 | 2 | 0 | 2 | 1 | |
| 50 | 16 | 16.2.1 | Escherichia coli | 0 | 0 | 1 | 2 | 0 | 0 | 2 | 1 | |
| 51 | 16 | 16.2.2 | Enterobacter cloacae | 2 | 0 | 2 | 2 | 2 | 0 | 2 | 1 | |
| 52 | 29 | 29.2.1 | Escherichia coli | 1 | 0 | 2 | 2 | 2 | 0 | 2 | 1 | |
| 53 | 29 | 29.2.2 | Escherichia vulneris | 0 | 0 | 1 | 2 | 2 | 0 | 2 | 1 | |
| 54 | 31 | 31.2.1 | Escherichia coli | 1 | 0 | 2 | 2 | 2 | 0 | 2 | 1 | |
| 55 | 35 | 35.2.1 | Klebsiella pneumoniae | 1 | 0 | 1 | 2 | 2 | 0 | 2 | 1 | |
| 56 | 46 | 46.2.1 | Pantoea spp | 1 | 0 | 2 | 2 | 2 | 0 | 1 | ||
| 57 | 46 | 46.2.2 | Escherichia coli | 1 | 0 | 2 | 2 | 2 | 0 | 2 | 1 | |
| 58 | 47 | 47.2.1 | Escherichia coli | 1 | 0 | 2 | 2 | 2 | 0 | 2 | 1 | |
| 59 | 47 | 47.2.2 | Enterobacter cloacae | 2 | 0 | 2 | 2 | 2 | 2 | 2 | 1 | |
| 60 | 49 | 49.2.2 | Enterobacter cloacae | 2 | 0 | 1 | 2 | 2 | 2 | 2 | 1 | |
| 61 | 55 | 55.2.1 | Escherichia coli | 1 | 1 | 2 | 2 | 0 | 2 | 1 | ||
| 62 | 55 | 55.2.2 | Klebsiella pneumoniae | 1 | 0 | 2 | 0 | 2 | 0 | 2 | 1 | |
| 63 | 56 | 56.2.2 | Enterobacter cloacae | 2 | 0 | 2 | 2 | 2 | 1 | 2 | 1 | |
| 64 | 57 | 57.2.1 | Escherichia coli | 0 | 0 | 0 | 0 | 2 | 0 | |||
| 65 | 60 | 60.2.1 | Enterobacter cloacae | 2 | 0 | 2 | 2 | 2 | 0 | 2 | 1 | |
| 66 | 60 | 60.2.3 | Escherichia coli | 1 | 0 | 1 | 2 | 2 | 0 | 2 | 1 | |
| 67 | 72 | 72.2.3 | Salmonella group | 1 | 0 | 0 | 2 | 2 | 2 | 1 | ||
| 68 | 75 | 75.2.3 | Enterobacter cloacae | 2 | 0 | 1 | 2 | 2 | 0 | 2 | 1 | |
| 69 | 84 | 84.2.1 | Escherichia coli | 0 | 0 | 0 | 2 | 2 | 0 | 2 | 1 | |
| 70 | 85 | 85.2.1 | Escherichia coli | 0 | 0 | 1 | 2 | 2 | 0 | 2 | 1 | |
| 71 | 85 | 85.2.2 | Enterobacter cloacae | 2 | 0 | 2 | 2 | 2 | 0 | 2 | 1 | |
| 72 | 87 | 87.2.1 | Escherichia coli | 0 | 0 | 2 | 2 | 0 | 0 | 2 | 1 | |
| 73 | 87 | 87.2.2 | Escherichia coli | 1 | 0 | 2 | 2 | 2 | 0 | 2 | 1 | |
| 74 | 89 | 89.2.1 | Escherichia coli | 1 | 0 | 2 | 2 | 2 | 0 | 2 | 1 | |
| 75 | 89 | 89.2.2 | Klebsiella pneumoniae | 1 | 0 | 2 | 0 | 2 | 0 | 2 | 1 | |
| 76 | 91 | 91.2.1 | Escherichia coli | 1 | 0 | 2 | 2 | 2 | 2 | 2 | 1 | |
| 77 | 91 | 91.2.2 | Enterobacter cloacae | 2 | 0 | 2 | 2 | 2 | 0 | 2 | 1 | |
| 78 | 101 | 101.2.1 | Escherichia coli | 1 | 0 | 2 | 2 | 1 | 0 | 2 | 1 | |
| 79 | 101 | 101.2.2 | Klebsiella pneumoniae | 0 | 0 | 1 | 2 | 0 | 0 | 2 | 1 | |
| 80 | 107 | 107.2.1 | Escherichia coli | 1 | 0 | 2 | 2 | 2 | 0 | 2 | 1 | |
| 81 | 107 | 107.2.2 | Enterobacter cloacae | 2 | 0 | 2 | 2 | 2 | 2 | 2 | 1 | |
| 82 | 107 | 107.2.4 | Enterobacter cloacae | 2 | 0 | 1 | 2 | 2 | 0 | 2 | 1 | |
| 83 | 108 | 108.2.2 | Enterobacter cloacae | 2 | 0 | 1 | 2 | 2 | 0 | 2 | 1 | |
| 84 | 113 | 113.2.1 | Escherichia coli | 2 | 2 | |||||||
| 85 | 115 | 115.2.1 | Escherichia coli | 0 | 0 | 2 | 2 | 2 | 0 | 2 | 1 | |
| 86 | 115 | 115.2.2 | Citrobacter freundii | 2 | 0 | 2 | 2 | 2 | 0 | 2 | 1 | |
| 87 | 124 | 124.2.1 | Escherichia coli | 0 | 0 | 2 | 2 | 2 | 0 | 2 | 1 | |
| 88 | 124 | 124.2.3 | Salmonella enterica | 1 | 0 | 2 | 2 | 2 | 1 | |||
| 89 | 126 | 126.2.2 | Citrobacter brakii | 2 | 0 | 2 | 2 | 2 | 1 | 2 | 1 | |
| 90 | 127 | 127.2.1 | Escherichia coli | 1 | 0 | 2 | 2 | 2 | 1 | 2 | 1 | |
| 91 | 127 | 127.2.2 | Enterobacter cloacae | 2 | 0 | 1 | 2 | 2 | 0 | 2 | 1 | |
| 92 | 136 | 136.2.1 | Escherichia coli | 1 | 0 | 2 | 2 | 2 | 1 | 2 | 1 | |
| 93 | 136 | 136.2.2 | Klebsiella pneumoniae | 1 | 0 | 2 | 0 | 2 | 0 | 2 | 1 | |
| 94 | 143 | 143.2.1 | Escherichia coli | 0 | 0 | 0 | 2 | 2 | 0 | 2 | 1 | |
| 95 | 143 | 143.2.2 | Citrobacter freundii | 2 | 0 | 0 | 2 | 2 | 0 | 2 | 1 | |
| 96 | 144 | 144.2.1 | Escherichia coli | 2 | 0 | 1 | 2 | 2 | 0 | 2 | 1 | |
| 97 | 144 | 144.2.2 | Citrobacter freundii | 2 | 0 | 2 | 1 | 2 | 1 | |||
| 98 | 144 | 144.2.3 | Proteus mirabilis | 1 | 0 | 2 | 0 | 0 | 1 | |||
| 99 | 148 | 148.2.1 | Escherichia coli | 2 | 0 | 0 | 0 | 0 | 0 | 2 | 1 | |
| 100 | 149 | 149.2.1 | Escherichia coli | 0 | 0 | 0 | 2 | 2 | 0 | 2 | 1 | |
| 101 | 149 | 149.2.2 | Enterobacter cloacae | 2 | 0 | 1 | 2 | 2 | 2 | 2 | 1 | |
| 102 | 152 | 152.2.2 | Escherichia coli | 1 | 0 | 2 | 0 | 2 | 0 | 2 | 1 | |
| 103 | 156 | 156.2.1 | Enterobacter cloacae | 2 | 0 | 1 | 2 | 2 | 2 | 2 | 1 | |
| 104 | 156 | 156.2.2 | Escherichia coli | 1 | 0 | 2 | 2 | 2 | 0 | 2 | 1 | |
| 105 | 158 | 158.2.2 | Klebsiella pneumoniae | 1 | 0 | 2 | 0 | 2 | 0 | 2 | 1 | |
| 106 | 161 | 161.2.1 | Escherichia coli | 1 | 0 | 2 | 2 | 2 | 0 | 2 | 1 | |
| 107 | 161 | 161.2.2 | Enterobacter cloacae | 2 | 0 | 1 | 2 | 2 | 0 | 2 | 1 | |
| 108 | 167 | 167.2.1 | Klebsiella pneumoniae | 1 | 0 | 1 | 2 | 2 | 0 | 2 | 1 | |
| 109 | 176 | 176.2.1 | Escherichia coli | 1 | 0 | 0 | 2 | 2 | 0 | 2 | 1 | |
| 110 | 177 | 177.2.1 | Escherichia coli | 1 | 0 | 1 | 2 | 2 | 0 | 2 | 1 | |
| 111 | 177 | 177.2.2 | Enterobacter cloacae | 2 | 0 | 1 | 2 | 2 | 0 | 2 | 1 | |
| 112 | 181 | 181.2.1 | Enterobacter cloacae | 2 | 0 | 1 | 2 | 1 | 2 | 1 | ||
| 113 | 181 | 181.2.2 | Escherichia coli | 1 | 0 | 2 | 2 | 2 | 0 | 2 | 1 | |
| 114 | 183 | 183.2.1 | Klebsiella pneumoniae | 1 | 0 | 1 | 2 | 2 | 0 | 2 | 1 | |
| 115 | 183 | 183.2.2 | Escherichia coli | 1 | 0 | 0 | 2 | 2 | 0 | 2 | 1 | |
| 116 | 195 | 195.2.1 | Escherichia coli | 1 | 0 | 1 | 2 | 2 | 0 | 2 | 1 | |
| 117 | 212 | 212.2.1 | Escherichia coli | 0 | 0 | 1 | 2 | 0 | 0 | 0 | ||
| 118 | 216 | 216.2.1 | Escherichia coli | 0 | 0 | 2 | 2 | 0 | 0 | 2 | 0 | |
| 119 | 219 | 219.2.1 | Escherichia coli | 1 | 0 | 2 | 2 | 0 | 2 | 1 | ||
| 120 | 222 | 222.2.1 | Klebsiella pneumoniae | 1 | 0 | 1 | 2 | 2 | 0 | 2 | 1 | |
| 121 | 222 | 222.2.2 | Escherichia coli | 0 | 0 | 2 | 2 | 0 | 0 | 2 | 1 | |
| 122 | 223 | 223.2.1 | Escherichia coli | 1 | 0 | 2 | 2 | 2 | 0 | 0 | 1 | |
| 123 | 224 | 224.2.1 | Escherichia coli | 1 | 0 | 2 | 2 | 2 | 0 | 2 | 1 | |
| 124 | 224 | 224.2.2 | Klebsiella pneumoniae | 1 | 0 | 2 | 2 | 2 | 0 | 2 | 1 | |
| 125 | 228 | 228.2.1 | Klebsiella pneumoniae | 0 | 0 | 2 | 0 | 2 | 0 | 0 | 1 | |
| 126 | 229 | 229.2.1 | Escherichia coli | 1 | 0 | 2 | 2 | 2 | 2 | 2 | 1 | |
| 127 | 229 | 229.2.2 | Salmonella enterica | 1 | 0 | 2 | 2 | 2 | 2 | 2 | 1 | |
| 128 | 234 | 234.2.1 | Raoultella ornithinolytica | 2 | 0 | 1 | 2 | 2 | 2 | 2 | 1 | |
| 129 | 237 | 237.2.1 | Escherichia coli | 0 | 0 | 0 | 2 | 0 | 0 | 2 | 1 | |
| 130 | 238 | 238.2.1 | Klebsiella pneumoniae | 1 | 0 | 1 | 0 | 2 | 0 | 2 | 1 | |
| 131 | 243 | 243.2.1 | Escherichia coli | 0 | 0 | 2 | 2 | 0 | 0 | 2 | 1 | |
| 132 | 243 | 243.2.2 | Enterobacter cloacae | 2 | 0 | 1 | 2 | 2 | 0 | 2 | 1 | |
| 133 | 246 | 246.2.1 | Escherichia coli | 1 | 0 | 1 | 0 | 2 | 1 | |||
| 134 | 246 | 246.2.2 | Enterobacter cloacae | 2 | 0 | 2 | 2 | 2 | 0 | 2 | 1 | |
| 135 | 265 | 265.2.1 | Enterobacter cloacae | 2 | 0 | 1 | 2 | 2 | 0 | 2 | 1 | |
| 136 | 272 | 272.2.1 | Enterobacter cloacae | 2 | 0 | 1 | 2 | 2 | 0 | 2 | 1 | |
| 137 | 273 | 273.2.1 | Enterobacter cloacae | 2 | 0 | 1 | 2 | 2 | 0 | 2 | 1 | |
| 138 | 278 | 278.2.1 | Escherichia coli | 0 | 0 | 1 | 2 | 0 | 0 | 2 | 1 | |
| 139 | 278 | 278.2.2 | Citrobacter sedlakii | 0 | 0 | 2 | 2 | 0 | 0 | 1 | ||
| 140 | 278 | 278.2.4 | Klebsiella pneumoniae | 0 | 0 | 2 | 2 | 2 | 0 | 0 | 1 | |
| 141 | 279 | 279.2.1 | Klebsiella oxytoca | 2 | 0 | 0 | 0 | 2 | 1 | 2 | 1 | |
| 142 | 279 | 279.2.2 | Escherichia coli | 0 | 0 | 1 | 2 | 0 | 0 | 2 | 1 | |
| 143 | 289 | 289.2.1 | Escherichia coli | 1 | 0 | 2 | 0 | 2 | 0 | 2 | 1 | |
| 144 | H40 | H40.2 | Farms | Escherichia coli | 2 | 0 | 1 | 0 | 0 | 0 | 2 | 1 |
| 145 | H42 | H42.1 | Escherichia coli | 2 | 0 | 1 | 2 | 2 | 1 | 2 | 1 | |
| 146 | H44 | H44.1 | Escherichia coli | 2 | 0 | 1 | 2 | 2 | 1 | 2 | 1 | |
| 147 | H45 | H45.2 | Citrobacter farmeri | 1 | 0 | 1 | 2 | 2 | 0 | 2 | 1 | |
| 148 | H48 | H48.2 | Escherichia coli | 2 | 0 | 2 | 2 | 2 | 0 | 2 | 1 | |
| 149 | H48 | H48.3 | Enterobacter cloacae | 2 | 0 | 1 | 2 | 2 | 1 | 2 | 1 | |
| 150 | H53 | H53.1 | Escherichia coli | 2 | 0 | 1 | 0 | 0 | 0 | 2 | 1 | |
| 151 | H53 | H53.2 | Enterobacter cloacae | 2 | 0 | 1 | 2 | 2 | 1 | 2 | 1 | |
| 152 | H54 | H54.1 | Escherichia coli | 2 | 0 | 2 | 2 | 2 | 0 | 2 | 1 | |
| 153 | H56 | H56.1 | Escherichia coli | 2 | 0 | 1 | 2 | 2 | 1 | 2 | 1 | |
| 154 | H56 | H56.2 | Enterobacter cloacae | 2 | 0 | 1 | 2 | 2 | 1 | 2 | 1 | |
| 155 | H57 | H57.1 | Enterobacter cloacae | 2 | 0 | 1 | 2 | 2 | 1 | 2 | 1 | |
| 156 | H57 | H57.2 | Escherichia coli | 2 | 0 | 1 | 2 | 2 | 1 | 2 | 1 | |
| 157 | H60 | H60.2 | Escherichia coli | 2 | 0 | 1 | 0 | 0 | 0 | 2 | 1 | |
| 158 | H110 | H110.1 | Enterobacter cloacae | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 159 | H138 | H138.1 | Escherichia coli | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | |
| 160 | H140 | H140.1 | Escherichia coli | 2 | 0 | 0 | 2 | 2 | 1 | 2 | 1 | |
| 161 | H154 | H154.2 | Klebsiella pneumoniae | 2 | 0 | 1 | 1 | 2 | 0 | 0 | 1 | |
| 162 | H157 | H157.2 | Klebsiella pneumoniae | 2 | 0 | 2 | 0 | 0 | 0 | 2 | 1 | |
| 163 | H230 | H230.1 | Escherichia coli | 1 | 0 | 1 | 2 | 2 | 0 | 2 | 1 | |
| 164 | H230 | H230.2 | Enterobacter cloacae | 2 | 0 | 1 | 2 | 2 | 0 | 0 | 1 | |
| 165 | H231 | H231.1 | Escherichia coli | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | |
| 166 | H233 | H233.1 | Escherichia coli | 1 | 0 | 1 | 2 | 2 | 0 | 2 | 1 | |
| 168 | H234 | H234.1 | Escherichia coli | 0 | 0 | 1 | 2 | 2 | 0 | 2 | 1 | |
| 169 | H234 | H234.2 | Enterobacter cloacae | 2 | 0 | 1 | 2 | 2 | 0 | 2 | 1 | |
| 170 | H235 | H235.1 | Escherichia coli | 1 | 0 | 1 | 2 | 2 | 0 | 2 | 1 | |
| 171 | H236 | H236.1 | Escherichia coli | 0 | 0 | 1 | 2 | 2 | 0 | 2 | 1 | |
| 172 | H237 | H237.1 | Escherichia coli | 1 | 0 | 1 | 2 | 2 | 0 | 2 | 1 | |
| 173 | H238 | H238.1 | Escherichia coli | 0 | 0 | 1 | 2 | 2 | 0 | 2 | 1 | |
| 174 | H241 | H241.1 | Escherichia coli | 1 | 0 | 1 | 2 | 2 | 0 | 2 | 1 | |
| 175 | H242 | H242.1 | Escherichia coli | 1 | 0 | 1 | 2 | 2 | 0 | 2 | 1 | |
| 176 | H243 | H243.1 | Escherichia coli | 1 | 0 | 1 | 2 | 2 | 0 | 2 | 1 | |
| 177 | H245 | H245.1 | Escherichia coli | 1 | 0 | 1 | 2 | 2 | 0 | 2 | 1 | |
| 178 | H246 | H246.1 | Escherichia coli | 1 | 0 | 1 | 2 | 2 | 0 | 2 | 1 | |
| 179 | H247 | H247.1 | Escherichia coli | 0 | 0 | 1 | 2 | 2 | 0 | 2 | 1 | |
| 180 | H248 | H248.1 | Escherichia coli | 0 | 0 | 1 | 2 | 2 | 0 | 2 | 1 | |
| 181 | H250 | H250.1 | Escherichia coli | 0 | 0 | 1 | 2 | 2 | 0 | 2 | 1 | |
| 182 | H251 | H251.1 | Escherichia coli | 0 | 0 | 1 | 2 | 2 | 0 | 2 | 1 | |
| 183 | H253 | H253.1 | Escherichia coli | 0 | 0 | 1 | 2 | 2 | 0 | 2 | 1 | |
| 184 | H254 | H254.1 | Escherichia coli | 0 | 0 | 1 | 2 | 2 | 0 | 2 | 1 | |
| 185 | H256 | H256.1 | Escherichia coli | 0 | 0 | 1 | 0 | 0 | 0 | 2 | 1 | |
| 186 | H257 | H257.1 | Escherichia coli | 1 | 0 | 0 | 1 | 2 | 0 | 2 | 1 | |
| 187 | H258 | H258.1 | Escherichia coli | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | |
| 188 | H259 | H259.1 | Escherichia coli | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | |
| 189 | H263 | H263.1 | Escherichia coli | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | |
| 190 | H265 | H265.1 | Escherichia coli | 1 | 0 | 0 | 1 | 2 | 0 | 2 | 1 | |
| 191 | H267 | H267.1 | Escherichia coli | 0 | 0 | 1 | 0 | 0 | 0 | 2 | 1 | |
| 192 | H268 | H268.1 | Escherichia coli | 1 | 0 | 0 | 1 | 2 | 0 | 2 | 1 |
| Population Studied | Variable | Classification | p-Value |
|---|---|---|---|
| Farm horses | Breed | Quarter Horse Arabian Pacer Warmblood Pony Local | <0.0001 |
| Sex | Female Male Gelding | 0.027 | |
| Farm | Numbered 1–13 | ||
| Hospitalization within the previous year | Yes/No | 0.018 | |
| Antibiotic treatment within the previous year | Yes/No | <0.0001 | |
| Age | Ranged from 0.1–23 y | <0.0001 | |
| Time in farm | Ranged from 0–23 y | 0.36 | |
| On admission | Breed | Quarter Horse Arabian Tennessee Walking horse Friesian Mangalarga Marchador Warmblood Thoroughbred Miniature horse Haflinger Hannoverian Single footed horse Missouri Fox Trotter | 0.394 |
| Age | Years | 0.259 | |
| Sex | Female Male Gelding | 0.117 | |
| Geographical origin (within the country) | North South Center | 0.879 | |
| Hospitalization within the previous year | Yes/No | 0.295 | |
| Clinical signs on admission | Gastro-intestinal disorder Neonatology disorder Ophthalmic disorder Reproduction Orthopedic disorder Hematological disorder Respiratory disorder Endocrine disorder Healthy (mares of sick hospitalized foals) | 0.587 | |
| Length of illness before admission | Days | 0.618 | |
| Antibiotic treatment within the previous year | Yes/No | 0.587 | |
| Length of stay | Days | 0.169 | |
| Admission charge | - | 0.056 | |
| During hospitalization | Shedding on admission | Yes/No | 0.9 |
| Clinical signs on admission | Gastro-intestinal disorder Neonatology disorder Ophthalmic disorder Reproduction Orthopedic disorder Hematological disorder Respiratory disorder Endocrine disorder Tumor Teeth lesion Healthy (mares of sick hospitalized foals) | 0.428 | |
| Antibiotic treatment during hospitalization | Yes/No | 0.841 | |
| Outcome | Discharged/Died | 0.174 | |
| Length of stay | Days | 0.29 | |
| Admission charge | - | 0.69 |
| Risk Factor | p-Value | OR |
|---|---|---|
| Sex (reference: mare) | 0.647 | |
| Stallion | 0.409 | 0.571 (95% CI 0.151–2.162) |
| Gelding | 0.639 | 0.765 (95% CI 0.25–2.34) |
| Length of stay | 0.766 | 1 (95% CI 0.997–1) |
| Admission charge | 0.184 | 1 (95% 1–1) |
References
- Vo, A.T.T.; van Duijkeren, E.; Fluit, A.C.; Gaastra, W. Characteristics of extended-spectrum cephalosporin-resistant Escherichia coli and Klebsiella pneumoniae isolates from horses. Vet. Microbiol. 2007, 124, 248–255. [Google Scholar] [CrossRef]
- Paterson, D.L.; Bonomo, R.A. Extended-Spectrum β-Lactamases: A Clinical Update. Clin. Microbiol. Rev. 2005, 18, 657–686. [Google Scholar] [CrossRef] [Green Version]
- Denkel, L.A.; Schwab, F.; Kola, A.; Leistner, R.; Garten, L.; von Weizsäcker, K.; Geffers, C.; Gastmeier, P.; Piening, B. The mother as most important risk factor for colonization of very low birth weight (VLBW) infants with extended-spectrum β-lactamase-producing Enterobacteriaceae (ESBL-E). J. Antimicrob. Chemother. 2014, 69, 2230–2237. [Google Scholar] [CrossRef] [Green Version]
- Schwaber, M.J.; Navon-Venezia, S.; Kaye, K.S.; Ben-Ami, R.; Schwartz, D.; Carmeli, Y. Clinical and economic impact of bacteremia with extended- spectrum-beta-lactamase-producing Enterobacteriaceae. Antimicrob. Agents Chemother. 2006, 50, 1257–1262. [Google Scholar] [CrossRef] [Green Version]
- Ewers, C.; Stamm, I.; Pfeifer, Y.; Wieler, L.H.; Kopp, P.A.; Schønning, K.; Prenger-Berninghoff, E.; Scheufen, S.; Stolle, I.; Günther, S.; et al. Clonal spread of highly successful ST15-CTX-M-15 Klebsiella pneumoniae in companion animals and horses. J. Antimicrob. Chemother. 2014, 69, 2676–2680. [Google Scholar] [CrossRef] [Green Version]
- Ewers, C.; Bethe, A.; Stamm, I.; Grobbel, M.; Kopp, P.A.; Guerra, B.; Stubbe, M.; Doi, Y.; Zong, Z.; Kola, A.; et al. CTX-M-15-D-ST648 Escherichia coli from companion animals and horses: Another pandemic clone combining multiresistance and extraintestinal virulence? J. Antimicrob. Chemother. 2014, 69, 1224–1230. [Google Scholar] [CrossRef] [Green Version]
- Shnaiderman-Torban, A.; Navon-Venezia, S.; Dahan, R.; Dor, Z.; Taulescu, M.; Paitan, Y.; Edery, N.; Steinman, A. CTX-M-15 Producing Escherichia coli Sequence Type 361 and Sequence Type 38 Causing Bacteremia and Umbilical Infection in a Neonate Foal. J. Equine Vet. Sci. 2020, 85, 102881. [Google Scholar] [CrossRef]
- Shnaiderman-Torban, A.; Paitan, Y.; Arielly, H.; Kondratyeva, K.; Tirosh-Levy, S.; Abells-Sutton, G.; Navon-Venezia, S.; Steinman, A. Extended-Spectrum β-Lactamase-Producing Enterobacteriaceae in Hospitalized Neonatal Foals: Prevalence, Risk Factors for Shedding and Association with Infection. Animals 2019, 9, 600. [Google Scholar] [CrossRef] [Green Version]
- Johns, I.; Verheyen, K.; Good, L.; Rycroft, A. Antimicrobial resistance in faecal Escherichia coli isolates from horses treated with antimicrobials: A longitudinal study in hospitalised and non-hospitalised horses. Vet. Microbiol. 2012, 159, 381–389. [Google Scholar] [CrossRef]
- Dolejska, M.; Duskova, E.; Rybarikova, J.; Janoszowska, D.; Roubalova, E.; Dibdakova, K.; Maceckova, G.; Kohoutova, L.; Literak, I.; Smola, J.; et al. Plasmids carrying blaCTX-M-1 and qnr genes in Escherichia coli isolates from an equine clinic and a horseback riding centre. J. Antimicrob. Chemother. 2011, 66, 757–764. [Google Scholar] [CrossRef] [Green Version]
- Maddox, T.W.; Clegg, P.D.; Diggle, P.J.; Wedley, A.L.; Dawson, S.; Pinchbeck, G.L.; Williams, N.J. Cross-sectional study of antimicrobial-resistant bacteria in horses. Part 1: Prevalence of antimicrobial-resistant Escherichia coli and methicillin-resistant Staphylococcus aureus. Equine Vet. J. 2012, 44, 289–296. [Google Scholar] [CrossRef]
- Kaspar, U.; von Lützau, K.; Schlattmann, A.; Rösler, U.; Köck, R.; Becker, K. Zoonotic multidrug-resistant microorganisms among non-hospitalized horses from Germany. One Health 2019, 7, 100091. [Google Scholar] [CrossRef]
- De Lagarde, M.; Larrieu, C.; Praud, K.; Schouler, C.; Doublet, B.; Sallé, G.; Fairbrother, J.M.; Arsenault, J. Prevalence, risk factors, and characterization of multidrug resistant and extended spectrum β-lactamase/AmpC β-lactamase producing Escherichia coli in healthy horses in France in 2015. J. Vet. Intern. Med. 2019, 33, 902–911. [Google Scholar] [CrossRef] [Green Version]
- Maddox, T.W.; Pinchbeck, G.L.; Clegg, P.D.; Wedley, A.L.; Dawson, S.; Williams, N.J. Cross-sectional study of antimicrobial-resistant bacteria in horses. Part 2: Risk factors for faecal carriage of antimicrobial-resistant Escherichia coli in horses. Equine Vet. J. 2012, 44, 297–303. [Google Scholar] [CrossRef]
- Murk, J.-L.A.N.; Heddema, E.R.; Hess, D.L.J.; Bogaards, J.A.; Vandenbroucke-Grauls, C.M.J.E.; Debets-Ossenkopp, Y.J. Enrichment broth improved detection of extended-spectrum-beta-lactamase-producing bacteria in throat and rectal surveillance cultures of samples from patients in intensive care units. J. Clin. Microbiol. 2009, 47, 1885–1887. [Google Scholar] [CrossRef] [Green Version]
- Clinical and Laboratory Standards Institute (CLSI). Performance Standards for Antimicrobial Susceptibility Testing, 26th ed.; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2016. [Google Scholar]
- Falagas, M.E.; Karageorgopoulos, D.E. Pandrug Resistance (PDR), Extensive Drug Resistance (XDR), and Multidrug Resistance (MDR) among Gram-Negative Bacilli: Need for International Harmonization in Terminology. Clin. Infect. Dis. 2008, 46, 1121–1122. [Google Scholar] [CrossRef] [Green Version]
- Woodford, N.; Fagan, E.J.; Ellington, M.J. Multiplex PCR for rapid detection of genes encoding CTX-M extended-spectrum β-lactamases. J. Antimicrob. Chemother. 2006, 57, 154–155. [Google Scholar] [CrossRef] [Green Version]
- Lin, S.-P.; Liu, M.-F.; Lin, C.-F.; Shi, Z.-Y. Phenotypic detection and polymerase chain reaction screening of extended-spectrum β-lactamases produced by Pseudomonas aeruginosa isolates. J. Microbiol. Immunol. Infect. 2012, 45, 200–207. [Google Scholar] [CrossRef] [Green Version]
- Tofteland, S.; Haldorsen, B.; Dahl, K.H.; Simonsen, G.S.; Steinbakk, M.; Walsh, T.R.; Sundsfjord, A. Norwegian ESBL Study Group Effects of phenotype and genotype on methods for detection of extended-spectrum-beta-lactamase-producing clinical isolates of Escherichia coli and Klebsiella pneumoniae in Norway. J. Clin. Microbiol. 2007, 45, 199–205. [Google Scholar] [CrossRef] [Green Version]
- Johnson, J.R.; Clermont, O.; Johnston, B.; Clabots, C.; Tchesnokova, V.; Sokurenko, E.; Junka, A.F.; Maczynska, B.; Denamur, E. Rapid and Specific Detection, Molecular Epidemiology, and Experimental Virulence of the O16 Subgroup within Escherichia coli Sequence Type 131. J. Clin. Microbiol. 2014, 52, 1358–1365. [Google Scholar] [CrossRef] [Green Version]
- Ahmed, M.O.; Clegg, P.D.; Williams, N.J.; Baptiste, K.E.; Bennett, M. Antimicrobial resistance in equine faecal Escherichia coli isolates from North West England. Ann. Clin. Microbiol. Antimicrob. 2010, 9, 12. [Google Scholar] [CrossRef] [Green Version]
- Bilavsky, E.; Temkin, E.; Lerman, Y.; Rabinovich, A.; Salomon, J.; Lawrence, C.; Rossini, A.; Salvia, A.; Samso, J.V.; Fierro, J.; et al. Risk factors for colonization with extended-spectrum beta-lactamase-producing enterobacteriaceae on admission to rehabilitation centres. Clin. Microbiol. Infect. Off. Publ. Eur. Soc. Clin. Microbiol. Infect. Dis. 2014, 20, O804–O810. [Google Scholar] [CrossRef] [Green Version]
- Shitrit, P.; Reisfeld, S.; Paitan, Y.; Gottesman, B.-S.; Katzir, M.; Paul, M.; Chowers, M. Extended-spectrum beta-lactamase-producing Enterobacteriaceae carriage upon hospital admission: Prevalence and risk factors. J. Hosp. Infect. 2013, 85, 230–232. [Google Scholar] [CrossRef]
- Ewers, C.; Grobbel, M.; Stamm, I.; Kopp, P.A.; Diehl, I.; Semmler, T.; Fruth, A.; Beutlich, J.; Guerra, B.; Wieler, L.H.; et al. Emergence of human pandemic O25:H4-ST131 CTX-M-15 extended-spectrum-β-lactamase-producing Escherichia coli among companion animals. J. Antimicrob. Chemother. 2010, 65, 651–660. [Google Scholar] [CrossRef] [Green Version]
- Isgren, C.M.; Edwards, T.; Pinchbeck, G.L.; Winward, E.; Adams, E.R.; Norton, P.; Timofte, D.; Maddox, T.W.; Clegg, P.D.; Williams, N.J. Emergence of carriage of CTX-M-15 in faecal Escherichia coli in horses at an equine hospital in the UK; increasing prevalence over a decade (2008–2017). BMC Vet. Res. 2019, 15, 268. [Google Scholar] [CrossRef] [Green Version]
- Maddox, T.W.; Williams, N.J.; Clegg, P.D.; O’Donnell, A.J.; Dawson, S.; Pinchbeck, G.L. Longitudinal study of antimicrobial-resistant commensal Escherichia coli in the faeces of horses in an equine hospital. Prev. Vet. Med. 2011, 100, 134–145. [Google Scholar] [CrossRef]
- European Medicines Agency. Available online: https://www.ema.europa.eu/en/documents/scientific-guideline/reflection-paper-risk-antimicrobial-resistance-transfer-companion-animals_en.pdf (accessed on 15 January 2015).
- Dunkel, B.; Johns, I.C. Antimicrobial use in critically ill horses. J. Vet. Emerg. Crit. Care 2015, 25, 89–100. [Google Scholar] [CrossRef]
- Norris, J.M.; Zhuo, A.; Govendir, M.; Rowbotham, S.J.; Labbate, M.; Degeling, C.; Gilbert, G.L.; Dominey-Howes, D.; Ward, M.P. Factors influencing the behaviour and perceptions of Australian veterinarians towards antibiotic use and antimicrobial resistance. PLoS ONE 2019, 14, e0223534. [Google Scholar]
- Van Spijk, J.N.; Schmitt, S.; Schoster, A. Infections caused by multidrug-resistant bacteria in an equine hospital (2012–2015). Equine Vet. Educ. 2019, 31, 653–658. [Google Scholar] [CrossRef]
- Johns, I.C.; Adams, E.-L. Trends in antimicrobial resistance in equine bacterial isolates: 1999–2012. Vet. Rec. 2015, 176, 334. [Google Scholar] [CrossRef]
- Colodner, R.; Rock, W.; Chazan, B.; Keller, N.; Guy, N.; Sakran, W.; Raz, R. Risk factors for the development of extended-spectrum beta-lactamase-producing bacteria in nonhospitalized patients. Eur. J. Clin. Microbiol. Infect. Dis. Off. Publ. Eur. Soc. Clin. Microbiol. 2004, 23, 163–167. [Google Scholar] [CrossRef]
- Vázquez-Martínez, E.R.; García-Gómez, E.; Camacho-Arroyo, I.; González-Pedrajo, B. Sexual dimorphism in bacterial infections. Biol. Sex. Differ. 2018, 9, 27. [Google Scholar] [CrossRef] [Green Version]
- Adler, A.; Sturlesi, N.; Fallach, N.; Zilberman-Barzilai, D.; Hussein, O.; Blum, S.E.; Klement, E.; Schwaber, M.J.; Carmeli, Y. Prevalence, Risk Factors, and Transmission Dynamics of Extended-Spectrum-β-Lactamase-Producing Enterobacteriaceae: A National Survey of Cattle Farms in Israel in 2013. J. Clin. Microbiol. 2015, 53, 3515–3521. [Google Scholar] [CrossRef] [Green Version]
- McGowan, C. Welfare of Aged Horses. Animals 2011, 1, 366–376. [Google Scholar] [CrossRef] [PubMed]
- Monroe, M.; Whitworth, J.D.; Wharton, T.; Turner, J. Effects of an Equine-Assisted Therapy Program for Military Veterans with Self-Reported PTSD. Soc. Amp Anim. 2019, 1, 1–14. [Google Scholar] [CrossRef]
- Borgi, M.; Loliva, D.; Cerino, S.; Chiarotti, F.; Venerosi, A.; Bramini, M.; Nonnis, E.; Marcelli, M.; Vinti, C.; De Santis, C.; et al. Effectiveness of a Standardized Equine-Assisted Therapy Program for Children with Autism Spectrum Disorder. J. Autism Dev. Disord. 2016, 46, 1–9. [Google Scholar] [CrossRef] [PubMed]
- White-Lewis, S.; Johnson, R.; Ye, S.; Russell, C. An equine-assisted therapy intervention to improve pain, range of motion, and quality of life in adults and older adults with arthritis: A randomized controlled trial. Appl. Nurs. Res. 2019, 49, 5–12. [Google Scholar] [CrossRef]
- Linder, D.E.; Mueller, M.K.; Gibbs, D.M.; Siebens, H.C.; Freeman, L.M. The Role of Veterinary Education in Safety Policies for Animal-Assisted Therapy and Activities in Hospitals and Nursing Homes. J. Vet. Med. Educ. 2016, 44, 229–233. [Google Scholar] [CrossRef]
- Royden, A.; Ormandy, E.; Pinchbeck, G.; Pascoe, B.; Hitchings, M.D.; Sheppard, S.K.; Williams, N.J. Prevalence of faecal carriage of extended-spectrum β-lactamase (ESBL)-producing Escherichia coli in veterinary hospital staff and students. Vet. Rec. Open 2019, 6, e000307. [Google Scholar] [CrossRef] [Green Version]
| Equine Cohort | Breeds 1 | Median Age 2 (Years ± SD) | Sex Distribution 3 |
|---|---|---|---|
| Farm horses (n = 192) | 41.1% Arabians (n = 79/192) 25% pacers (n = 48/192) 15.1% Quarter horses (n = 29/192) 9.9% Warmbloods (n = 19/192) 5.2% local breed (n = 10/192) 3.7% ponies (n = 7/192) | 8 ± 5.3 | mares (72.4%, n = 139/192) geldings (12.5%, n = 24/192) stallions (11.5%, n = 22/192) 4 |
| Horses on admission (n = 168) | 49.4% Arabians (n = 83/168) 19.6% Quarter horses (n = 33/168) 14.3% pacers (n = 24/168) 7.7% Friesians (n = 13/168) 4.8% Warmbloods (n = 8/168) 4.2% others (n = 7/168) | 4.5 ± 5.2 | mares (68.5%, n = 115/168) geldings (16.1%, n = 27/168) stallions (15.4%, n = 26/168) |
| Equine Cohort | Shedding (%) | Total No. of ESBL-E Isolates | MDR Isolates (%) | blaESBL Gene Group (%) |
|---|---|---|---|---|
| Farm horses | 40/192 (20.8) (95% CI: 15.3–27.3%) | 48 | 43/48 (89.6) (95% CI: 77.3–96.5) | CTX-M-1: 35/48 (72.9) CTX-M-9: 1/48 (2.1) CTX-M-25: 1/48 (2.1) SHV-12: 5/48 (10.4) |
| Horses on admission | 33/168 (19.6) (95% CI: 13.9–26.5%) | 39 | 28/39 (71.8) (95% CI: 55.1–85.0%) | CTX-M-1: 24/39 (61.5) CTX-M-9: 1/39 (2.5) SHV-12: 3/39 (7.7) SHV-2: 1/39 (2.5) SHV-28: 1/39 (2.5) |
| Hospitalized horses (72 h post admission) 1 | 67/86 (77.9) 2 (95% CI 67.7–86.1%) | 105 | 99/105 (94.3) (95% CI: 87.9–97.9%) 3 | CTX-M-1: 50/105 (47.6) CTX-M-2: 8/105 (7.6) CTX-M-9: 7/105 (6.7) CTX-M-25: 1/105 (0.95) OXA-1: 2/105 (1.9) SHV-12: 26/105 (24.7) SHV-228: 1/105 (0.95) |
| Equine Cohort | AMP | AMC 2 | LEX | CAZ | IMP | CHL 3 | ENR 4 | AMK | GEN 5 | NIT 6 | TMS 7 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Farms | 100 | 41.7 | 100 | 100 | 0 | 66.6 | 6.3 | 0 | 75 | 4.2 | 89.6 |
| On admission | 100 | 82.1 | 100 | 85.0 | 0 | 46.2 | 17.9 | 2.6 | 48.7 | 5.3 | 76.3 |
| During hospitalization | 96.0 | 32.0 | 99.0 | 90.0 | 0 | 85.3 | 51.5 | 10.8 | 84.3 | 11.0 | 95.0 |
| Variable | p-value | Odds Ratio (95% CI) |
|---|---|---|
| Breed (Arabian versus non-Arabian) | 0.006 | 3.9 (1.5–10.4) |
| Sex (reference: mare) | 0.079 | - |
| Stallion | 0.029 | 3.4 (1.1–12.2) |
| Gelding | 0.744 | 0.7 (0.07–6.4) |
| Age | 0.008 | 0.9 (0.8–0.97) |
| Hospitalization within the previous year | 0.194 | 2.9 (0.6–14.8) |
| Antibiotic treatment within the previous year | <0.0001 | 9.8 (3.6–26.8) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shnaiderman-Torban, A.; Navon-Venezia, S.; Dor, Z.; Paitan, Y.; Arielly, H.; Abu Ahmad, W.; Kelmer, G.; Fulde, M.; Steinman, A. Extended-Spectrum β-lactamase-Producing Enterobacteriaceae Shedding in Farm Horses Versus Hospitalized Horses: Prevalence and Risk Factors. Animals 2020, 10, 282. https://doi.org/10.3390/ani10020282
Shnaiderman-Torban A, Navon-Venezia S, Dor Z, Paitan Y, Arielly H, Abu Ahmad W, Kelmer G, Fulde M, Steinman A. Extended-Spectrum β-lactamase-Producing Enterobacteriaceae Shedding in Farm Horses Versus Hospitalized Horses: Prevalence and Risk Factors. Animals. 2020; 10(2):282. https://doi.org/10.3390/ani10020282
Chicago/Turabian StyleShnaiderman-Torban, Anat, Shiri Navon-Venezia, Ziv Dor, Yossi Paitan, Haia Arielly, Wiessam Abu Ahmad, Gal Kelmer, Marcus Fulde, and Amir Steinman. 2020. "Extended-Spectrum β-lactamase-Producing Enterobacteriaceae Shedding in Farm Horses Versus Hospitalized Horses: Prevalence and Risk Factors" Animals 10, no. 2: 282. https://doi.org/10.3390/ani10020282






