Airborne Dissemination of Bacteria (Enterococci, Staphylococci and Enterobacteriaceae) in a Modern Broiler Farm and Its Environment
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Characteristics of the Broiler Farm
2.2. Sample Collection
2.3. Bacterial Identification
2.4. Characterization of Enterococcus hirae Isolates
3. Results
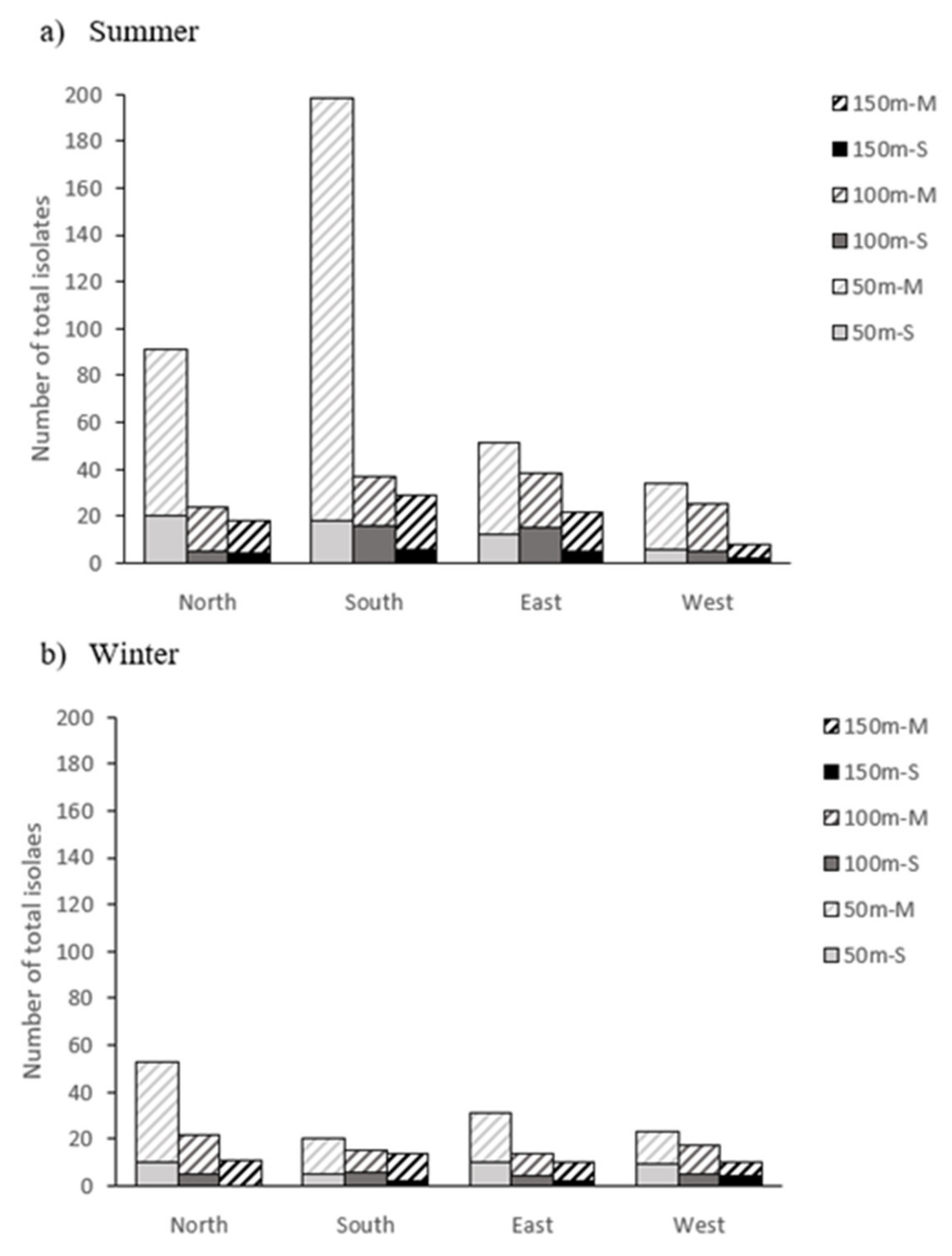
3.1. Bacterial Counts
3.2. Diversity of Bacteria Obtained
3.3. Characterization of E. hirae Isolates Recovered from Different Sampling Points Showing Similar Resistance Phenotype
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Lis, D.O.; Mainelis, G.; Górny, R.L. Microbial air contamination in farmhouses-quantitative aspects. Clean 2008, 36, 551–555. [Google Scholar] [CrossRef]
- Srikanth, P.; Sudharsanam, S.; Steinberg, R. Bio-aerosols in indoor environment: Composition, health effects and analysis. Indian J. Med. Microbiol. 2008, 26, 302–312. [Google Scholar] [CrossRef]
- Friesema, I.; Sigmundsdottir, G.; Van der Zwaluw, K.; Heuvelink, A.; Schimmer, B.; de Jager, C.; Rump, B.; Briem, H.; Hardardottir, H.; Atladottir, A.; et al. An international outbreak of Shiga toxin-producing Escherichia coli O157 infection due to lettuce, September–October 2007. Eurosurveillance 2008, 13, 19065. [Google Scholar] [CrossRef] [Green Version]
- Södeström, A.; Osterberg, P.; Lindqvist, A.; Jönsson, B.; Lindberg, A.; Blide Ulander, S.; Welinder-Olsson, C.; Löfdahl, S.; Kaijser, B.; De Jong, B.; et al. A large Escherichia coli O157 outbreak in Sweden associated with locally produced lettuce. Foodborne Pathog. Dis. 2008, 5, 339–349. [Google Scholar] [CrossRef]
- Wendel, A.M.; Jonhson, D.H.; Sharapov, U.; Grant, J.; Archer, J.R.; Monson, T.; Koschmann, C.; Dacis, J.P. Multistate of Escherichia coli O157:H7 infection associated with consumption of packaged spinach, August-September 2006: The Wisconsin investigation. Clin. Infect. Dis. 2009, 48, 1079–1086. [Google Scholar] [CrossRef] [Green Version]
- EFSA (European Food Safety Authority). Urgent advice on the public health risk of Shiga-toxin producing Escherichia coli in fresh vegetables. EFSA J. 2011, 9, 2274–2324. [Google Scholar] [CrossRef]
- Mora, A.; Herrera, A.; López, C.; Dahbi, G.; Mamani, R.; Pita, J.M.; Alonso, M.P.; Llovo, J.; Bernárdez, M.I.; Blanco, J.E.; et al. Characteristics of the Shiga-toxin-producing enteroaggregative Escherichia coli O104:H4 German outbreak strain and of STEC strains isolated in Spain. Int. Microbiol. 2011, 14, 121–141. [Google Scholar] [CrossRef]
- Rangarajan, A.; Pritts, M.P.; Reiners, S.; Pedersen, L.H. Focusing food safety training based on current grower practices and farm scale. HortTechnology 2002, 1, 126–131. [Google Scholar] [CrossRef] [Green Version]
- Harrison, J.A.; Gaskin, J.W.; Harrison, M.A.; Cannon, J.L.; Boyer, R.R.; Zehnder, J.W. Survey of food safety practices on small to medium-sized farms and in farmer markets. J. Food Prot. 2013, 11, 1989–1993. [Google Scholar] [CrossRef] [PubMed]
- Park, S.; Navratil, S.; Gregory, A.; Bauer, A.; Srinath, I.; Jun, M.; Szonyi, B.; Nightingale, K.; Anciso, J.; Ivanek, R. Generic Escherichia coli contamination of spinach at the preharvest stage: Effects of farm management and environmental factors. Appl. Environ. Microbiol. 2013, 14, 4347–4358. [Google Scholar] [CrossRef] [Green Version]
- Strawn, L.; Grohn, Y.T.; Warchocki, S.; Worobo, R.W.; Bihn, E.A.; Wiedmann, M. Risk factors associated with Salmonella and Listeria monocytogenes contamination on produced fields. Appl. Environ. Microbiol. 2013, 24, 7618–7627. [Google Scholar] [CrossRef] [Green Version]
- Reuland, E.A.; Al Naiemi, N.; Raadsen, S.A.; Savelkoul, P.H.M.; Kluytmans, J.A.J.W.; Vandenbroucke-Grauls, C.M.J.E. Prevalence of ESBL-producing Enterobacteriaceae in raw vegetables. Eur. J. Clin. Microbiol. Infect. Dis. 2014, 33, 1843–1846. [Google Scholar] [CrossRef] [Green Version]
- Matković, K.; Vučemilo, M.; Vinković, B.; Šeol, B.; Pavičić, Ž.; Tofant, A.; Matković, S. Effect of microclimate on bacterial count and airborne emission from dairy barns on the environment. Ann. Agric. Environ. Med. 2006, 13, 349–354. [Google Scholar]
- Sanz, S.; Olarte, C.; Martínez-Olarte, R.; Navajas-Benito, E.V.; Alonso, C.A.; Hidalgo-Sanz, S.; Somalo, S.; Torres, C. Airborne dissemination of Escherichia coli in a dairy cattle farm and its environment. Int. J. Food Microbiol. 2015, 197, 40–44. [Google Scholar] [CrossRef]
- Seedorf, J.; Schulz, J.; Hartung, J. Outdoor measurements of airborne emission of staphylococci from a broiler barn and its predictability by dispersion models. WIT Trans. Ecol. Environ. 2005, 85, 33–42. [Google Scholar]
- Chinivasagam, H.N.; Tran, T.; Maddock, L.; Gale, A.; Blackall, P.J. The aerobiology of the environment around mechanically ventilated broiler shed. J. Appl. Microbiol. 2010, 108, 1657–1667. [Google Scholar] [CrossRef] [PubMed]
- Friese, A.; Schulz, J.; Zimmermann, K.; Tenhagen, B.A.; Fetsch, A.; Hartung, J.; Rösler, U. Occurrence of livestock-associated Methicillin resistant Staphylococcus aureus in turkey and broiler barns and contamination of air and soil surfaces in their vicinity. Appl. Environ. Microbiol. 2013, 79, 2759–2766. [Google Scholar] [CrossRef] [Green Version]
- Laube, H.; Friese, A.; von Salviati, C.; Guerra, B.; Rösler, U. Transmission of ESBL/AmpC-produicing Escherichia coli from broiler chicken farms to surrounding areas. Vet. Microbiol. 2014, 172, 519–527. [Google Scholar] [CrossRef] [PubMed]
- Ferguson, D.D.; Smith, T.C.; Hanson, B.M.; Wardyn, S.E.; Kelley, J.; Donham, K.J. Detection of airborne Methicillin-Resistant Staphylococcus aureus inside and downwind of a swine building, and in animal feed: Potential occupational, animal health, and environmental implications. J. Agromed. 2016, 21, 149–153. [Google Scholar] [CrossRef] [Green Version]
- Sanz, S.; Olarte, C.; Martínez-Olarte, R.; Alonso, C.A.; Hidalgo-Sanz, R.; Gómez, P.; Ruiz-Ripa, L.; Torres, C. Identification of Enterococci, Staphylococci, and Enteriobacteriaceae from slurries and air in and around two pork farms. J. Food Protect. 2018, 81, 1776–1782. [Google Scholar] [CrossRef]
- Bakutis, B.; Monstviliene, E.; Januskeviciene, G. Analyses of airborne contamination with bacteria, endotoxins and dust in livestock barns and poultry houses. Acta Vet. Brno 2004, 73, 283–289. [Google Scholar] [CrossRef] [Green Version]
- Lonc, E.; Plewa, K. Microbial air contamination in poultry houses. Pol. J. Environ. Stud. 2010, 19, 15–19. [Google Scholar]
- Lonc, E.; Plewa, K. Comparison of indoor and outdoor bioaerosols in poultry farming. In Advanced Topics in Environmental Health and Air Pollution Case Studies; Moldoveanu, A.M., Ed.; IntechOpen: Rijeka, Croatia, 2011; pp. 339–352. [Google Scholar] [CrossRef] [Green Version]
- Jorgensen, J.H.; Ferraro, M.J. Antimicrobial Susceptibility Testing: General Principles and Contemporary Practices. Clin. Infect. Dis. 1998, 26, 973–980. [Google Scholar] [CrossRef] [Green Version]
- Torres, C.; Cercenado, E. Interpretive reading of the antibiogram in gram positive cocci. Enferm. Infecc. Microbiol. Clin. 2010, 28, 541–553. [Google Scholar] [CrossRef]
- Clinical and Laboratory Standards Institute (CLSI). Performance Standards for Antimicrobial Susceptibility Testing, 28th ed.; CLSI Supplement M100; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2018. [Google Scholar]
- Alonso, C.A.; Rezusta, A.; Seral, C.; Ferrer, I.; Castillo, F.J.; Torres, C. Persistence of a ST6 clone of Enterococcus faecalis genotype vanB2 in two Hospitals in Aragón (Spain). Enferm. Infecc. Microbiol. Clin. 2017, 35, 578–581. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Heras, J.; Domínguez, C.; Mata, E.; Pascual, V.; Lozano, C.; Torres, C.; Zarazaga, M. GelJ-a tool for analyzing DNA fingerprint gel images. BMC Bioinform. 2015, 16, 270. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tenover, F.C.; Arbeit, R.D.; Goering, R.V.; Mikelsen, P.A.; Murray, B.E.; Persing, D.H.; Swaminathan, B. Interpreting chromosomal DNA restriction patterns produced by pulsed-filed gel electrophoresis criteria for bacterial strain typing. J. Clin. Microbiol. 1995, 33, 2233–2239. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Omeira, N.; Barbou, E.K.; Nehme, P.A.; Hamadeh, S.K.; Zurayk, R.; Bashour, I. Microbiological and chemical properties of litter from different chicken types and production systems. Sci. Total Environ. 2006, 367, 156–162. [Google Scholar] [CrossRef]
- Barker, K.J.; Purswell, J.L.; Davis, J.D.; Parker, H.M.; Kidd, M.T.; McDaniel, C.D.; Kiess, A.S. Distribution of bacteria at different poultry litter depths. Int. J. Poul. Sci. 2010, 9, 10–13. [Google Scholar] [CrossRef]
- Kostadinova, G.; Petrov, G.; Denev, S.; Miteva, C.; Stefanova, R.; Penev, T. Microbial pollution of manure, litter, air and soil in poultry farm. Bulg. J. Agric. Sci. 2014, 20, 56–65. [Google Scholar]
- Shale, K.; Lues, J.F.R. The etiology of bioaerosols in food environments. Food Rev. Int. 2007, 23, 73–90. [Google Scholar] [CrossRef]
- Schulz, J.; Hartung, J.; Seedorf, J.; Formosa, L.C. Staphylococci as an indicator for bacterial emission from a broiler house. In Proceedings of the International Congress of International Society for Animal Hygiene, St. Malo, France, 11–13 October 2004; pp. 6565–6581. [Google Scholar]
- Friese, A.; Schulz, J.; Hoehle, L.; Tenhagen, B.A.; Fetsch, A.; Hartung, J.; Roesler, U. Occurrence of MRSA in air and housing environments of pig barns. Vet. Microbiol. 2012, 158, 129–135. [Google Scholar] [CrossRef]
- Crozier-Dodson, B.A.; Fung, D.Y.C. Comparison of recovery of airborne microorganisms in a dairy cattle facility using selective agar and thin agar layer resuscitation media. J. Food Prot. 2002, 65, 1488–1492. [Google Scholar] [CrossRef]
- Schulz, J.; Friese, A.; Klee, S.; Tenhagen, B.A.; Fetsch, A.; Rösler, U.; Hartung, J. Longitudinal study of the contamination of air and soil surfaces in the vicinity of pigs barns by livestock-associated methilcillin-resistant Staphylococcus aureus. Appl. Environ. Microbiol. 2012, 78, 5666–5671. [Google Scholar] [CrossRef] [Green Version]
- Cherkaoui, A.; Hibbs, J.; Emonet, S.; Tangomo, M.; Girard, M.; Francois, P.; Schrenzel, P.J. Comparison of two matrix-assisted laser desorption ionization-time of flight mass spectrometry methods with conventional phenotypic identification for routine identification of bacteria to the species level. J. Clin. Microbiol. 2010, 48, 1169–1175. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Devriese, L.A.; Hommez, J.; Wijfels, R.; Haesebrouck, F. Composition of the enterococcal and streptococcal intestinal flora of poultry. J. Appl. Bacteriol. 1991, 71, 46–50. [Google Scholar] [CrossRef]
- Xiao, Y.; Xiang, Y.; Zhou, W.; Chen, J.; Li, K.; Yang, H. Microbial community mapping in intestinal tract of broiler chicken. Poult. Sci. 2017, 96, 1387–1393. [Google Scholar] [CrossRef]
- Klein, G. Taxonomy, ecology and antibiotic resistance of enterococci from food and the gastro-intestinal tract. Int. J. Food Microbiol. 2003, 88, 123–131. [Google Scholar] [CrossRef]
- Kühn, I.; Iversen, A.; Burnman, L.G.; Olsson-Liljequist, B.; Franklin, A.; Finn, M.; Aarestrup, F.; Seyfarth, A.M.; Blanch, A.R.; Vilanova, X.; et al. Comparison of enterococcal population in animals, humans and environment-a European study. Int. J. Food Microbiol. 2003, 88, 133–145. [Google Scholar] [CrossRef]
- Fisher, K.; Phillips, C. The ecology, epidemiology and virulence of Enterococcus. Microbiology 2009, 155, 1749–1757. [Google Scholar] [CrossRef] [Green Version]
- Jones, A.M.; Harrison, R.M. The effects of meteorological factors on atmospheric bioaerosol concentrations-A review. Sci. Total Environ. 2004, 326, 151–180. [Google Scholar] [CrossRef] [PubMed]
- Navajas-Benito, E.V.; Alonso, C.A.; Sanz, S.; Olarte, C.; Martínez-Olarte, R.; Hidalgo-Sanz, S.; Somalo, S.; Torres, C. Molecular characterization of antibiotic resistance in Escherichia coli strains from a dairy cattle farm and its surroundings. J. Sci. Food Agric. 2017, 97, 362–365. [Google Scholar] [CrossRef] [PubMed]
| Sample | Season | Sampling Conditions | Bacterial Counts in the Culture Media | |||
|---|---|---|---|---|---|---|
| T (°C) | RH (%) | MSA | SB | CCA | ||
| Litter a | Winter | 26–28 | 70–72 | 4.9 × 107 cfu/g | 2.6 × 106 cfu/g | 2.9 × 105 cfu/g |
| Summer | 26–28 | 70–72 | 5.8 × 107 cfu/g | 4.7 × 106 cfu/g | 3.1 × 105 cfu/g | |
| Inside air b | Winter | 26–28 | 70–72 | >105 cfu/m3 | >105 cfu/m3 | >105 cfu/m3 |
| Summer | 26–28 | 70–72 | >105 cfu/m3 | >105 cfu/m3 | >105 cfu/m3 | |
| Outside air c | Winter | 2.4–14.7 | 53–77 | n.d.−4 cfu/m3 | n.d.−3 cfu/m3 | n.d.−2 cfu/m3 |
| Summer | 17.1–29.0 | 42–68 | n.d.−6 cfu/m3 | n.d.−4 cfu/m3 | n.d.−5 cfu/m3 | |
| Microorganisms: | Air | ||
|---|---|---|---|
| Litter | Inside | Outside | |
| Staphylococci: | 15 (10%) | 20 (14%) | 127 (50%) |
| Staphylococcus aureus | 4 | - | - |
| S. arlettae | - | 1 | 19 |
| S. capitis | - | - | 1 |
| S. cohnii | - | 1 | 5 |
| S. epidermidis | 1 | - | 6 |
| S. equorum | - | - | 6 |
| S. haemolyticus | - | - | 1 |
| S. hominis | - | - | 6 |
| S. lentus | 1 | 3 | 2 |
| S. nepalensis | - | 1 | 4 |
| S. pasteuri | 1 | - | - |
| S. saprophyticus | 6 | 10 | 50 |
| S. sciuri | - | - | 1 |
| S. xylosus | 2 | 4 | 26 |
| Enterobacteriaceae: | 57 (39%) | 68 (48%) | 51 (20%) |
| Escherichia coli | 57 | 54 | - |
| Escherichia hermani | - | - | 1 |
| Klebsiella pneumoniae | - | 11 | - |
| Pantoea agglomerans | - | 3 | 50 |
| Enterococci: | 74 (51%) | 52 (38%) | 64 (25%) |
| Enterococcus faecalis | 8 | 2 | 3 |
| E. faecium | 3 | 4 | 10 |
| E. hirae | 63 | 46 | 49 |
| E. casseliflavus | - | - | 2 |
| Others: | - | 2 | 14 (5%) |
| Achromobacter spanius | - | - | 1 |
| Acinetobacter radioresistens | - | 1 | 3 |
| Acinetobacter baumanii | - | 1 | - |
| Aerococcus viridans | - | - | 6 |
| Corynebacterium proping. | - | - | 1 |
| Micrococcus luteus | - | - | 1 |
| Pseudomonas corrugata | - | - | 1 |
| Pseudomonas koreensis | - | - | 1 |
| TOTAL | 146 | 142 | 256 |
| Microorganisms (Number in Summer/Winter) | North | South | East | West | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 50 m | 100 m | 150 m | 50 m | 100 m | 150 m | 50 m | 100 m | 150 m | 50 m | 100 m | 150 m | |
| Staphylococci: 24/103 | 5/28 | 1/8 | -/5 | 6/5 | 4/2 | 2/3 | -/14 | -/3 | 1/7 | 4/20 | 1/7 | -/1 |
| S. arlettae | -/2 | -/1 | -/1 | 3/- | - | - | -/2 | - | -/1 | -/8 | -/1 | - |
| S. capitis | - | - | - | - | 1/- | - | - | - | - | - | - | - |
| S. cohnii | -/1 | - | - | - | - | - | -/2 | - | - | -/1 | - | -/1 |
| S. equorum | -/1 | - | - | -/4 | -/1 | - | - | - | - | - | - | - |
| S. epidermidis | 4/1 | - | - | - | 1/- | - | - | - | - | - | - | - |
| S. haemolyticus | - | - | - | - | - | -/1 | - | - | - | - | - | - |
| S. hominis | - | -/1 | - | - | 1/1 | -/2 | - | - | - | 1/- | - | - |
| S. lentus | - | - | - | - | - | - | -/1 | - | -/1 | - | - | - |
| S. nepalensis | - | - | - | - | - | - | - | - | - | -/4 | - | - |
| S. saprophyticus | -/19 | 1/6 | - | 2/- | 1/- | - | -/9 | -/3 | 1/- | -/7 | -/1 | - |
| S. sciuri | - | - | - | - | - | 1/- | - | - | - | - | - | - |
| S. xylosus | 1/4 | - | -/4 | 1/1 | - | 1/- | - | - | -/5 | 3/- | 1/5 | - |
| Enterobacteriaceae: 46/5 | 4/2 | 6/- | 4/- | 1/- | 4/1 | - | - | 11/1 | 4/- | 9/1 | 3/- | - |
| Escherichia hermani | - | - | - | - | 1/- | - | - | - | - | - | - | - |
| Pantoea agglomerans | 4/2 | 6/- | 4/- | 1/- | 3/1 | - | - | 11/1 | 4/- | 9/1 | 3/- | - |
| Enterococci: 58/6 | 6/- | 2/- | 2/- | 13/- | 7/- | - | 10/- | 1/5 | 4/- | 13/1 | - | - |
| E. faecalis | - | - | - | - | 3/- | - | - | - | - | - | - | - |
| E. faecium | 2/- | 1/- | - | 1/- | 1/- | - | 1/- | -/2 | - | 1/1 | - | - |
| E. hirae | 4/- | - | 2/- | 12/- | 3/- | - | 9/- | 1/3 | 3/- | 12/- | - | - |
| E. casseliflavus | - | 1/- | - | - | - | - | - | - | 1/- | - | - | - |
| Others: 9/5 | -/1 | 2/- | 1/- | - | 1/- | 2/- | 1/1 | -/2 | 2/1 | - | - | - |
| Achromobacter spanius | -/1 | - | - | - | - | - | - | - | - | - | - | - |
| Acinetobacter radioresistens | - | 1/- | - | - | - | - | - | - | 2/- | - | - | - |
| Aerococcus viridans | - | - | - | - | 1/- | 2/- | - | -/2 | -/1 | - | - | - |
| Corynebacterium propinq. | - | - | - | - | - | - | -/1 | - | - | - | - | - |
| Micrococcus luteus | - | 1/- | - | - | - | - | - | - | - | - | - | - |
| Pseudomonas corrugata | - | - | 1/- | - | - | - | - | - | - | - | - | - |
| Pseudomonas koreensis | - | - | - | - | - | - | 1/- | - | - | - | - | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sanz, S.; Olarte, C.; Hidalgo-Sanz, R.; Ruiz-Ripa, L.; Fernández-Fernández, R.; García-Vela, S.; Martínez-Álvarez, S.; Torres, C. Airborne Dissemination of Bacteria (Enterococci, Staphylococci and Enterobacteriaceae) in a Modern Broiler Farm and Its Environment. Animals 2021, 11, 1783. https://doi.org/10.3390/ani11061783
Sanz S, Olarte C, Hidalgo-Sanz R, Ruiz-Ripa L, Fernández-Fernández R, García-Vela S, Martínez-Álvarez S, Torres C. Airborne Dissemination of Bacteria (Enterococci, Staphylococci and Enterobacteriaceae) in a Modern Broiler Farm and Its Environment. Animals. 2021; 11(6):1783. https://doi.org/10.3390/ani11061783
Chicago/Turabian StyleSanz, Susana, Carmen Olarte, Raquel Hidalgo-Sanz, Laura Ruiz-Ripa, Rosa Fernández-Fernández, Sara García-Vela, Sandra Martínez-Álvarez, and Carmen Torres. 2021. "Airborne Dissemination of Bacteria (Enterococci, Staphylococci and Enterobacteriaceae) in a Modern Broiler Farm and Its Environment" Animals 11, no. 6: 1783. https://doi.org/10.3390/ani11061783
APA StyleSanz, S., Olarte, C., Hidalgo-Sanz, R., Ruiz-Ripa, L., Fernández-Fernández, R., García-Vela, S., Martínez-Álvarez, S., & Torres, C. (2021). Airborne Dissemination of Bacteria (Enterococci, Staphylococci and Enterobacteriaceae) in a Modern Broiler Farm and Its Environment. Animals, 11(6), 1783. https://doi.org/10.3390/ani11061783







