Is a Block of the Femoral and Sciatic Nerves an Alternative to Epidural Analgesia in Sheep Undergoing Orthopaedic Hind Limb Surgery? A Prospective, Randomized, Double Blinded Experimental Trial
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Animals
2.2. Procedure
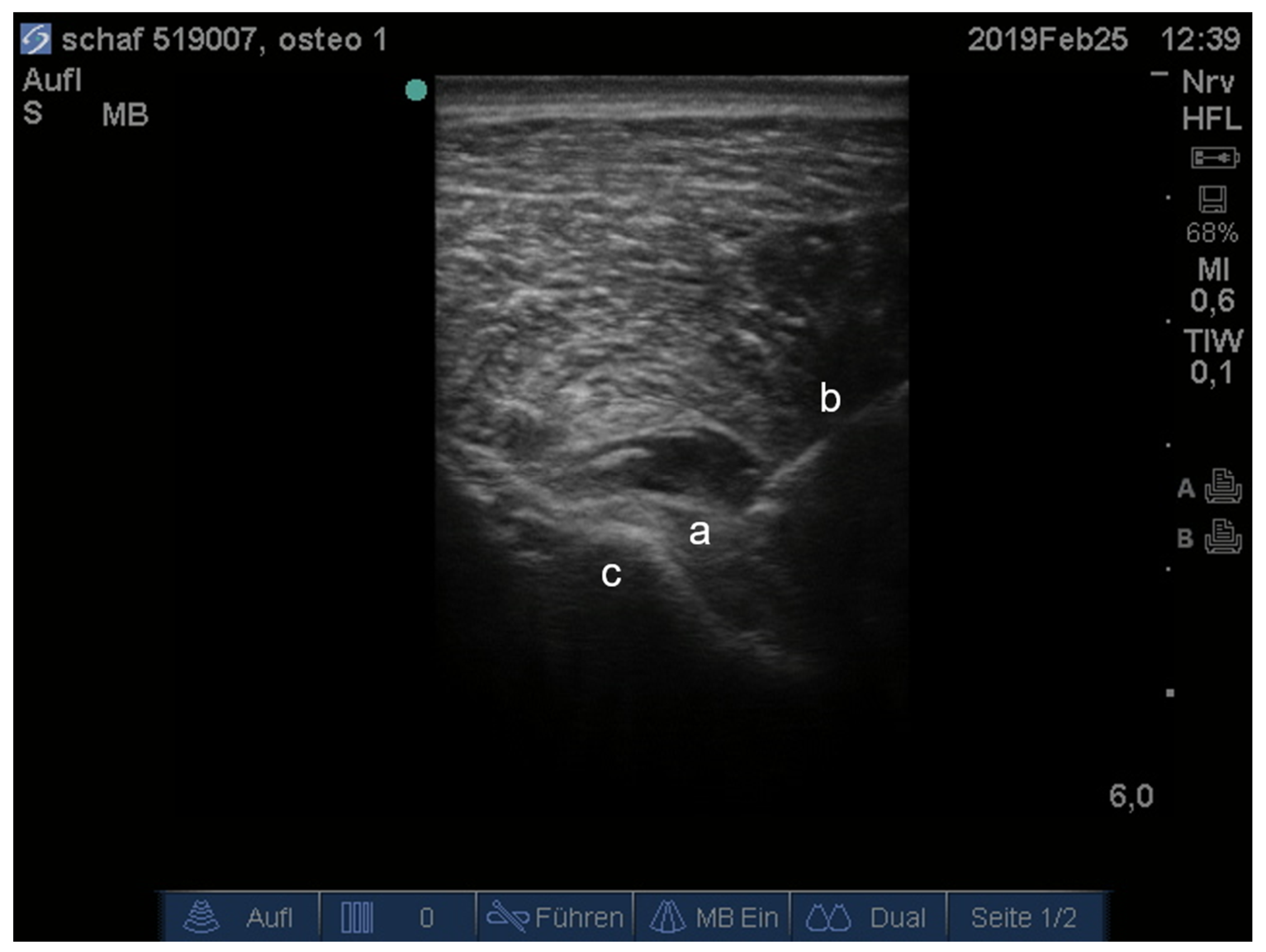
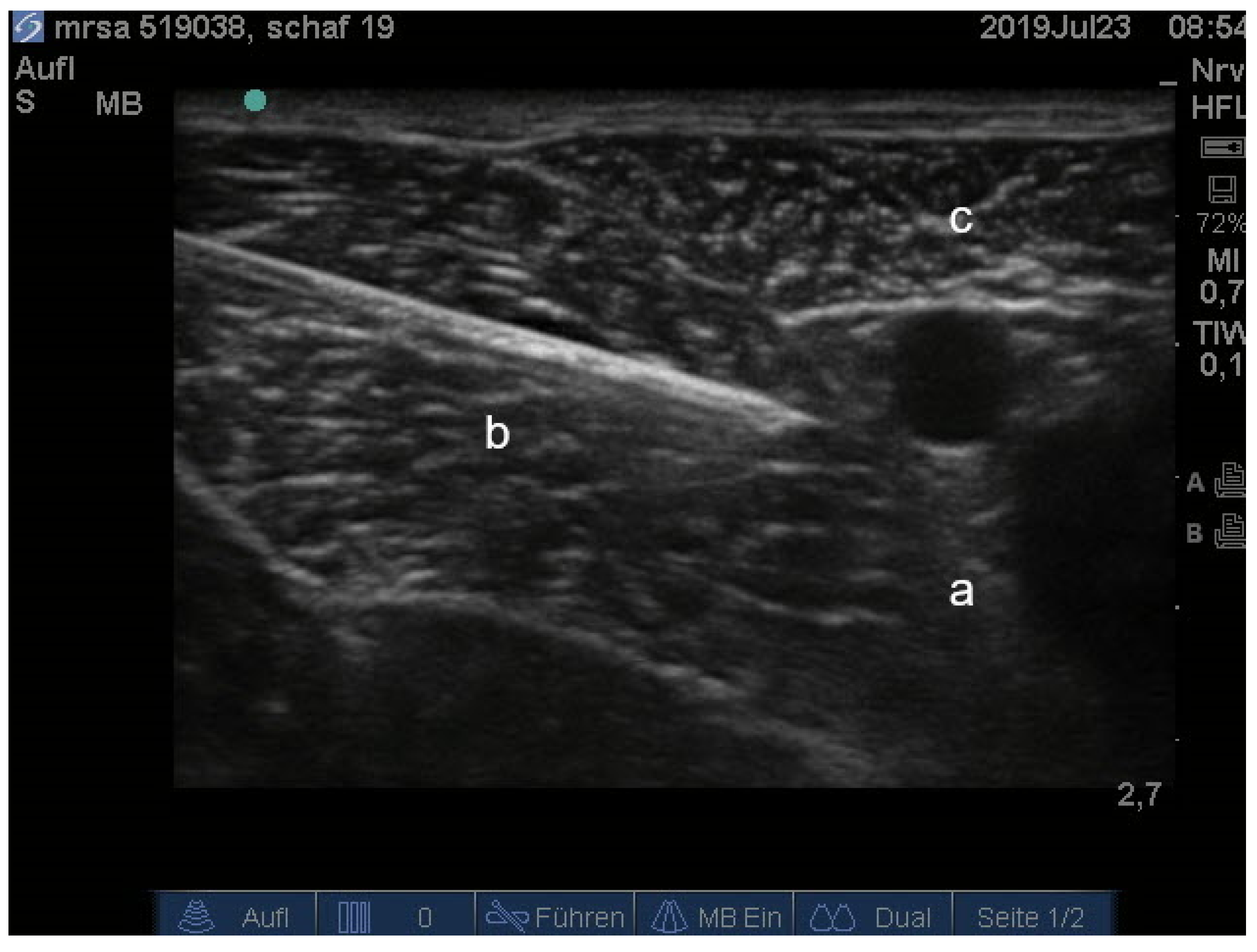
2.3. Locoregional Anaesthesia
2.4. Intra-Operative Evaluation of Nociception
2.5. Evaluation of Analgesia
2.6. Data Collection and Comparisons
2.7. Statistical Analysis
3. Results
3.1. Intra-Operative Evaluation of Nociception and Rescue Analgesia
3.2. Evaluation of Analgesia and Rescue Analgesia
3.3. Side Effects
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dias, I.R.; Camassa, J.A.; Bordelo, J.A.; Babo, P.S.; Viegas, C.; Dourado, N.; Reis, R.L.; Gomes, M.E. Preclinical and translational studies in small ruminants (sheep and goat) as models for osteoporosis research. Curr. Osteoporos. Rep. 2018, 16, 182–197. [Google Scholar] [CrossRef] [PubMed]
- Zarrinkalam, M.R.; Beard, H.; Schultz, C.G.; Moore, R.J. Validation of the sheep as a large animal model for the study of vertebral osteoporosis. Eur. Spine J. 2008, 18, 244–253. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schemitsch, E.H.; Kowalski, M.J.; Swiontkowski, M.; Senft, D. Cortical bone blood flow in reamed and unreamed locked intramedullary nailing: A fractured tibia model in sheep. J. Orthop. Trauma 1994, 8, 373–382. [Google Scholar] [CrossRef] [PubMed]
- Potes, J.C.; Reis, J.; Capela e Silva, F.; Relvas, C.; Cabrita, A.S.; Simões, J.A. The sheep as an animal model in orthopaedic research. Exp. Pathol. Health Sci. 2008, 2, 29–32. [Google Scholar]
- Martini, L.; Fini, M.; Giavaresi, G.; Giardino, R. Sheep model in orthopedic research: A literature review. Comp. Med. 2001, 51, 292–299. [Google Scholar]
- Newman, E.; Turner, A.; Wark, J. The potential of sheep for the study of osteopenia: Current status and comparison with other animal models. Bone 1995, 16, S277–S284. [Google Scholar] [CrossRef]
- Pearce, A.; Richards, R.; Milz, S.; Schneider, E.; Pearce, S. Animal models for implant biomaterial research in bone: A review. Eur. Cells Mater. 2007, 13, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Coulter, C.A.; Flecknell, P.A.; Richardson, C.A. Reported analgesic administration to rabbits, pigs, sheep, dogs and non-human primates undergoing experimental surgical procedures. Lab. Anim. 2009, 43, 232–238. [Google Scholar] [CrossRef]
- Martinez-Carranza, N.; Berg, H.; Hultenby, K.; Nurmi-Sandh, H.; Ryd, L.; Lagerstedt, A.-S. Focal knee resurfacing and effects of surgical precision on opposing cartilage. A pilot study on 12 sheep. Osteoarthr. Cartil. 2013, 21, 739–745. [Google Scholar] [CrossRef] [Green Version]
- Martinez-Carranza, N.; Hultenby, K.; Lagerstedt, A.S.; Schupbach, P.; Berg, H.E. Cartilage health in knees treated with metal resurfacing implants or untreated focal cartilage lesions: A preclinical study in sheep. Cartilage 2017, 10, 120–128. [Google Scholar] [CrossRef] [PubMed]
- Axelsen, M.G.; Overgaard, S.; Jespersen, S.M.; Ding, M. Comparison of synthetic bone graft ABM/P-15 and allograft on uninstrumented posterior lumbar spine fusion in sheep. J. Orthop. Surg. Res. 2019, 14, 2. [Google Scholar] [CrossRef] [PubMed]
- Whittle, B.J. Mechanisms underlying intestinal injury induced by anti-inflammatory COX inhibitors. Eur. J. Pharmacol. 2004, 500, 427–439. [Google Scholar] [CrossRef] [PubMed]
- Boelsterli, U.A.; Redinbo, M.R.; Saitta, K.S. Multiple NSAID-induced hits injure the small intestine: Underlying mechanisms and novel strategies. Toxicol. Sci. 2012, 131, 654–667. [Google Scholar] [CrossRef]
- MacPhail, C.M.; Lappin, M.R.; Meyer, D.J.; Smith, S.G.; Webster, C.R.; Armstrong, P.J. Hepatocellular toxicosis associated with administration of carprofen in 21 dogs. J. Am. Vet. Med. Assoc. 1998, 212, 1895–1901. [Google Scholar] [PubMed]
- Mathews, K.A.; Doherty, T.J.; Dyson, D.H.; Wilcock, B.; Valliant, A. Nephrotoxicity in dogs associated with methoxyflurane anesthesia and flunixin meglumine analgesia. Can. Vet. J. 1990, 31, 766–771. [Google Scholar] [PubMed]
- Gunson, D.E.; Soma, L.R. Renal papillary necrosis in horses after phenylbutazone and water deprivation. Vet. Pathol. 1983, 20, 603–610. [Google Scholar] [CrossRef] [Green Version]
- Mathews, K.A. Nonsteroidal anti-inflammatory analgesics in pain management in dogs and cats. Can. Vet. J. 1996, 37, 539–545. [Google Scholar] [PubMed]
- Grimm, K.A. Veterinary Anesthesia and Analgesia, 5th edition of lumb and jones; Grimm, K.A., Lamount, L.A., Tranquilli, W.J., Green, S.A., Robertson, A.R., Eds.; John Wiley & Sons: Hoboken, NJ, USA, 2015. [Google Scholar]
- Portela, D.A.; Verdier, N.; Otero, P.E. Regional anesthetic techniques for the pelvic limb and abdominal wall in small animals: A review of the literature and technique description. Vet. J. 2018, 238, 27–40. [Google Scholar] [CrossRef] [PubMed]
- Nuss, K.; Schwarz, A.; Ringer, S. Lokalanästhesien beim Wiederkäuer. Tierärztliche Prax. Ausg. G Großtiere/Nutztiere 2017, 45, 159–173. [Google Scholar]
- Segura, I.A.G.D.; Menafro, A.; Murillo, S.; Parodi, E.M.; García-Fernández, P. Analgesic and motor-blocking action of epidurally administered levobupivacaine or bupivacaine in the conscious dog. Vet. Anaesth. Analg. 2009, 36, 485–494. [Google Scholar] [CrossRef] [PubMed]
- Geist, V. Mountain Sheep. A Study in Behavior and Evolution; University of Chicago Press: Chicago, IL, USA, 1917. [Google Scholar]
- DeRossi, R.; Pagliosa, R.; Módolo, T.C.; Maciel, F.B.; Macedo, G.G. Thoracic epidural analgesia via the lumbosacral approach using multiport catheters with a low concentration of bupivacaine and morphine in sheep. Vet. Anaesth. Analg. 2012, 39, 306–314. [Google Scholar] [CrossRef] [PubMed]
- Wagner, A.E.; Dunlop, C.I.; Turner, A.S. Experiences with morphine injected into the subarachnoid space in sheep. Vet. Surg. 1996, 25, 256–260. [Google Scholar] [CrossRef] [PubMed]
- Mpanduji, D.G.; Mgasa, M.N.; Bittegeko, S.B.P.; Batamuzi, E.K. Comparison of xylazine and lidocaine effects for analgesia and cardiopulmonary functions following lumbosacral epidural injection in goats. Zentralblatt fur Vet. Reihe A 1999, 46, 605–611. [Google Scholar] [CrossRef] [PubMed]
- Richman, J.M.; Liu, S.S.; Courpas, G.; Wong, R.; Rowlingson, A.J.; Mcgready, J.; Cohen, S.R.; Wu, C.L. Does continuous peripheral nerve block provide superior pain control to opioids? A meta-analysis. Anesth. Analg. 2006, 102, 248–257. [Google Scholar] [CrossRef]
- Allen, H.W.; Liu, S.S.; Ware, P.D.; Nairn, C.S.; Owens, B.D. Peripheral nerve blocks imaprove analgesia after total knee replacement surgery. Anesth. Analg. 1998, 87, 93–97. [Google Scholar]
- Arnholz, M.K. Vergleich Einer Ultraschallgesteuerten Nervenblockade des Nervus Femoralis und des Nervus Ischiadicus mit Einer Epiduralanästhesie Bei Orthopädischen Eingriffen an der Hintergliedmaße von Katzen und Hunden. Ph.D. Thesis, Tierärztliche Hochschule Hannover, Hannover, Germany, 2017. [Google Scholar]
- Davies, A.F.; Segar, E.P.; Murdoch, J.; Wright, D.E.; Wilson, I.H. Epidural infusion or combined femoral and sciatic nerve blocks as perioperative analgesia for knee arthroplasty. Br. J. Anaesth. 2004, 93, 368–374. [Google Scholar] [CrossRef] [Green Version]
- Waag, S.; Stoffel, M.H.; Spadavecchia, C.; Eichenberger, U.; Rohrbach, H. Ultrasound-guided block of sciatic and femoral nerves: An anatomical study. Lab. Anim. 2014, 48, 97–104. [Google Scholar] [CrossRef]
- Farag, E.; Atim, A.; Ghoghs, R.; Bauer, M.; Sreenivasalu, T.; Kot, M.; Kurz, A.; Dalton, J.E.; Mascha, E.J.; Mounir-Soliman, L.; et al. Comparison of three techniques for ultrasound-guided femoral nerve catheter insertion a randomized, blinded trial. Anesthesiology. J. Am. Soc. Anesthesiol. 2014, 121, 239–248. [Google Scholar] [CrossRef] [Green Version]
- Campoy, L.; Bezuidenhout, A.J.; Gleed, R.D.; Martin-Flores, M.; Raw, R.M.; Santare, C.L.; Jay, R.A.; Wang, L.A. Ultrasound-guided approach for axillary brachial plexus, femoral nerve, and sciatic nerve blocks in dogs. Vet. Anaesth. Analg. 2010, 37, 144–153. [Google Scholar] [CrossRef] [PubMed]
- Echeverry, D.F.; Gil, F.; Laredo, F.; Ayala, M.D.; Belda, E.; Soler, M.; Agut, A. Ultrasound-guided block of the sciatic and femoral nerves in dogs: A descriptive study. Vet. J. 2010, 186, 210–215. [Google Scholar] [CrossRef] [PubMed]
- Echeverry, D.F.; Laredo, F.G.; Gil, F.; Belda, E.; Soler, M.; Agut, A. Ventral ultrasound-guided suprainguinal approach to block the femoral nerve in the dog. Vet. J. 2012, 192, 333–337. [Google Scholar] [CrossRef]
- Pypendop, B.H.; Pascoe, P.J.; Newbold, G.; Shilo-Benjamini, Y. Abstracts presented at the Association of Veterinary Anaesthetists Meeting, 24–26th September, 2014, Vienna, Austria: Quantitative evaluation of the antinociceptive effects of an ultrasound-guided injection of ropivacaine 0.5% to the sciatic nerve in experimental sheep preliminary data. J. Vet. Anaesth. Analg. 2015, 42, A1–A40. [Google Scholar]
- Martinez-Taboada, F.; Redondo, J.I. Comparison of the hanging-drop technique and running-drip method for identifying the epidural space in dogs. Vet. Anaesth. Analg. 2017, 44, 329–336. [Google Scholar] [CrossRef]
- Todorov, L.; VadeBoncouer, T. Etiology and use of the “hanging drop” technique: A review. Pain Res. Treat. 2014, 2014, 146750. [Google Scholar] [CrossRef] [PubMed]
- Häger, C.; Biernot, S.; Buettner, M.; Glage, S.; Keubler, L.M.; Held, N.; Bleich, E.M.; Otto, K.; Müller, C.W.; Decker, S.; et al. The sheep grimace scale as an indicator of post-operative distress and pain in laboratory sheep. PLoS ONE 2017, 12, e0175839. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bromage, P.R. A comparison of the hydrochloride and carbon dioxide salts of lidocaine and prilocaine in epidural analgesia. Acta Anaesthesiol. Scand. 1965, 9, 55–69. [Google Scholar] [CrossRef]
- Campoy, L.; Martin-Flores, M.; Ludders, J.W.; Erb, H.N.; Gleed, R.D. Comparison of bupivacaine femoral and sciatic nerve block versus bupivacaine and morphine epidural for stifle surgery in dogs. Vet. Anaesth. Analg. 2012, 39, 91–98. [Google Scholar] [CrossRef] [PubMed]
- Bradbrook, C.; Gurney, M.; Aprea, F.; Clark, L.; Corletto, F.; Vettorato, E. Peripheral nerve blocks of the pelvic limb in dogs: A retrospective clinical study. Vet. Comp. Orthop. Traumatol. 2012, 25, 314–320. [Google Scholar] [CrossRef] [PubMed]
- Laur, J.J.; Weinberg, G.L. Comparing safety in surface landmarks versus ultrasound-guided peripheral nerve blocks: An observational study of a practice in transition. Reg. Anesth. Pain Med. 2012, 37, 569–570. [Google Scholar] [CrossRef] [PubMed]
- Peduto, V.A.; Baroncini, S.; Montanini, S.; Proietti, R.; Rosignoli, L.; Tufano, R.; Casati, A. A prospective, randomized, double-blind comparison of epidural levobupivacaine 0.5% with epidural ropivacaine 0.75% for lower limb procedures. Eur. J. Anaesthesiol. 2003, 20, 979–983. [Google Scholar] [CrossRef]
- McGlade, D.P.; Kalpokas, M.V.; Mooney, P.H.; Buckland, M.R.; Vallipuram, S.K.; Hendrata, M.V.; Torda, T.A. Comparison of 0.5% ropivacaine and 0.5% bupivacaine in lumbar epidural anaesthesia for lower limb orthopaedic surgery. Anaesth. Intensiv. Care 1997, 25, 262–266. [Google Scholar] [CrossRef]
- Fanelli, G.; Casati, A.; Beccaria, P.; Aldegheri, G.; Berti, M.; Tarantino, F.; Torri, G. A double-blind comparison of ropivacaine, bupivacaine, and mepivacaine during sciatic and femoral nerve blockade. Anesth. Analg. 1998, 87, 597–600. [Google Scholar]
- Kuthiala, G.; Chaudhary, G. Ropivacaine: A review of its pharmacology and clinical use. Indian J. Anaesth. 2011, 55, 104–110. [Google Scholar] [CrossRef] [PubMed]
- Veering, B.T.; Cousins, M.J. Cardiovascular and pulmonary effects of epidural anaesthesia. Anaesth. Intensiv. Care 2000, 28, 620–635. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jones, R.S.; Tranquilli, W.J.; Thurmon, J.C.; Grimm, K.A. Lumb and Jones Veterinary Anesthesia and Analgesia; Saunders, W.B., Ed.; Blackwell Publishing: Hoboken, NJ, USA, 2007; p. 1112. ISBN 9780781754712. [Google Scholar]
- Felten, D.L.; O’Banion, M.K.; Maida, S.M. Netter’s Atlas of Neuroscience, 3rd ed.; Elsevier: Amsterdam, The Netherlands, 2016. [Google Scholar]
- Stoffel, M.H. Funktionelle Neuroanatomie für die Tiermedizin; Georg Thieme Verlag: New York, NY, USA, 2010. [Google Scholar]
- Johnson, R.A.; Lopez, M.; Hendrickson, D.A.; Kruse-Elliott, K.T. Cephalad distribution of three differing volumes of new methylene blue injected into the epidural space in adult goats. Vet. Surg. 1996, 25, 448–451. [Google Scholar] [CrossRef]



| Peripheral Block | Epidural | p-Value | |
|---|---|---|---|
| Age (years) | 2.75 (IQR 2–3.75) | 3 (IQR 2–5.25) | 0.597 |
| Weight (kg) | 70 (IQR 64–77.75) | 68 (IQR 60.9–72) | 0.414 |
| Duration (min) | Peripheral Block | Epidural | p-Value |
|---|---|---|---|
| Anaesthesia both types of surgery | 153 (130–176) | 155 (133–181) | 0.9 |
| Surgery both types of surgery | 58 (50–84.5) | 50 (45–68) | 0.3 |
| Anaesthesia tibia osteotomy group | 210 (185–225) | 232 (212–234) | 0.4 |
| Anaesthesia intramedullary nail | 148 (125–158) | 135 (123–156) | 0.8 |
| Surgery tibia osteotomy group | 110 (102–113) | 100 (93–111) | 0.7 |
| Surgery intramedullary nail group | 52 (49–61) | 48 (45–54) | 0.2 |
| Peripheral Block | Epidural | p-Value | |
|---|---|---|---|
| Duration of loss of sensation at coronary band (h) | 10 (9.5–11.75) * | 6 (5–8) | <0.001 * |
| Duration of analgesia at surgical wound (h) | 6 (5–8.5) | 8 (6.5–9) | 0.17 |
| Duration of loss of sensation in sacral area (h) | 0 | 8 (6.3–8.8) | <0.001 |
| Time to standing (h) | 4 (3–4.5) | 7 (6–7.5) | <0.001 |
| Estimate | Standard Error | p-Value | |
|---|---|---|---|
| VAS | |||
| Group (P vs. E) | 0.40 | 0.42 | 0.34 |
| Time | −0.10 | 0.04 | 0.04 |
| Group*Time interaction | −0.11 | 0.07 | 0.11 |
| SGS | |||
| Group (P vs. E) | 3.89 | 1.47 | 0.008 |
| Time | −0.31 | 0.16 | 0.052 |
| Group*Time interaction | −0.68 | 0.24 | 0.004 |
| Duration of loss of sensation at coronary band | |||
| Group (P vs. E) | −4.99 | 1.60 | 0.002 |
| Time | −0.87 | 0.21 | <0.001 |
| Group*Time interaction | 1.17 | 0.23 | <0.001 |
| Duration of analgesia at surgical wound | |||
| Group (P vs. E) | −5.48 | 1.71 | 0.001 |
| Time | −0.75 | 0.21 | <0.001 |
| Group*Time interaction | 0.68 | 0.25 | 0.007 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stenger, V.; Zeiter, S.; Buchholz, T.; Arens, D.; Spadavecchia, C.; Schüpbach-Regula, G.; Rohrbach, H. Is a Block of the Femoral and Sciatic Nerves an Alternative to Epidural Analgesia in Sheep Undergoing Orthopaedic Hind Limb Surgery? A Prospective, Randomized, Double Blinded Experimental Trial. Animals 2021, 11, 2567. https://doi.org/10.3390/ani11092567
Stenger V, Zeiter S, Buchholz T, Arens D, Spadavecchia C, Schüpbach-Regula G, Rohrbach H. Is a Block of the Femoral and Sciatic Nerves an Alternative to Epidural Analgesia in Sheep Undergoing Orthopaedic Hind Limb Surgery? A Prospective, Randomized, Double Blinded Experimental Trial. Animals. 2021; 11(9):2567. https://doi.org/10.3390/ani11092567
Chicago/Turabian StyleStenger, Valentina, Stephan Zeiter, Tim Buchholz, Daniel Arens, Claudia Spadavecchia, Gertraud Schüpbach-Regula, and Helene Rohrbach. 2021. "Is a Block of the Femoral and Sciatic Nerves an Alternative to Epidural Analgesia in Sheep Undergoing Orthopaedic Hind Limb Surgery? A Prospective, Randomized, Double Blinded Experimental Trial" Animals 11, no. 9: 2567. https://doi.org/10.3390/ani11092567






