Epidural Volume of Injectate Using a Dose Regimen Based on Occipito-Coccygeal Spinal Length (OCL): Randomized Clinical Study Comparing Different Ropivacaine Concentrations, with or without Morphine, in Bitches Undergoing Total Unilateral Mastectomy
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Animals
2.2. Anaesthetic Management
2.3. Epidural Administration
2.4. Postoperative Assessment
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sorenmo, K.U.; Worley, D.R.; Goldschimidt, M.H. Tumors of the Mammary Gland. In Withrow & MacEwen’s Small Animal Clinical Oncology, 5th ed.; Withrow, S.J., Vail, D.M., Page, R.L., Eds.; W.B. Saunders: Philadelphia, PA, USA, 2013; pp. 538–556. [Google Scholar]
- Johnston, S.A.; Tobias, K.M. Specific Disorders of the Skin and Subcutaneous Tissue. In Veterinary Surgery, 2nd ed.; Elsevier: Toronto, ON, Canada, 2018; Volume 2, Chapter 82; pp. 1528–1534. [Google Scholar]
- Poleshuck, E.L.; Katz, J.; Andrus, C.H.; Hogan, L.A.; Jung, B.F.; Kulick, D.I.; Dworkin, R.H. Risk factors for chronic pain following breast cancer surgery: A prospective study. J. Pain 2006, 7, 626–634. [Google Scholar] [CrossRef] [PubMed]
- Horta, R.S.; Figueiredo, M.S.; Lavalle, G.E.; Costa, M.P.; Cunha, R.M.C.; Araújo, R.B. Surgical stress and postoperative complication related to regional and radical mastectomy in dogs. Acta Vet. Scand. 2015, 57, 34. [Google Scholar] [CrossRef] [PubMed]
- Sacerdote, P.; Bianchi, M.; Gaspani, L.; Manfredi, B.; Maucione, A.; Terno, G.; Ammatuna, M.; Panerai, A.E. The effects of tramadol and morphine on immune responses and pain after surgery in cancer patients. Anesth. Analg. 2000, 90, 1411–1414. [Google Scholar] [CrossRef] [PubMed]
- Odunayo, A.; Dodam, J.R.; Kerl, M.E.; DeClue, A.E. Immunomodulatory effects of opioids. J. Vet. Emerg. Crit. Care 2010, 20, 376–385. [Google Scholar] [CrossRef]
- Bovill, J.G. Surgery for cancer: Does anesthesia matter? Anesth. Analg. 2010, 110, 1524–1526. [Google Scholar] [CrossRef]
- Perry, J.A.; Douglas, H. Immunomodulatory effects of surgery, pain, and opioids in cancer patients. Vet. Clin. N. Am. Small Anim. Pract. 2019, 49, 981–991. [Google Scholar] [CrossRef]
- Wall, T.; Scherwin, A.; Ma, A.; Buggy, D.J. Influence on perioperative anaesthetic and analgesic intervention on oncological outcomes: Narrative review. Br. J. Anaesth. 2019, 123, 135–150. [Google Scholar] [CrossRef]
- Troncy, E.; Junot, S.; Keroack, S.; Sammut, V.; Pibarot, P.; Genevois, J.P.; Cuvelliez, S. Results of pre-emptive epidural administration of morphine with or without bupivacaine in dogs and cats undergoing surgery: 265 cases (1997–1999). J. Am. Vet. Med. Assoc. 2002, 221, 666–672. [Google Scholar] [CrossRef]
- Kona-Boun, J.J.; Cuvelliez, S.; Troncy, E. Evaluation of epidural administration of morphine or morphine and bupivacaine for postoperative analgesia after premedication with an opioid analgesic and orthopedic surgery in dogs. J. Am. Vet. Med. Assoc. 2006, 229, 1103–1112. [Google Scholar] [CrossRef]
- Hendrix, P.K.; Raffe, M.R.; Robinson, E.P.; Felice, L.J.; Randal, D.A. Epidural administration of bupivacaine, morphine, or their combination for postoperative analgesia in dogs. J. Am. Vet. Med. Assoc. 1996, 209, 598–607. [Google Scholar]
- Valverde, A.; Mc Donell, W.N. Epidural morphine reduces halothane MAC in the dog. Can. J. Anaesth. 1989, 36, 629–632. [Google Scholar] [CrossRef] [PubMed]
- de Leon-Casasola, O.A.; Parker, B.; Lema, M.J.; Harrison, P.; Massey, J. Postoperative epidural bupivacaine-morphine therapy. Experience with 4227 surgical cancer patients. Anesthesiology 1994, 81, 368–375. [Google Scholar] [CrossRef] [PubMed]
- Brockway, M.; Bannister, J.; McClure, H.J.; McKeown, D.; Wildsmith, J.A. Comparison of extradural ropivacaine and bupivacaine. Br. J. Anaesth. 1991, 66, 31–37. [Google Scholar] [CrossRef] [PubMed]
- Valverde, A. Epidural analgesia and anesthesia in dogs and cats. Vet. Clin. N. Am. Small Anim. Pract. 2008, 38, 1205–1230. [Google Scholar] [CrossRef] [PubMed]
- Ford, D.J.; Raj, P.P.; Singh, P.; Regan, K.M.; Ohlweiler, D. Differential peripheral nerve block by local anesthetics in the cat. Anesthesiology 1984, 60, 28–33. [Google Scholar] [CrossRef] [PubMed]
- Skarda, R.T.; Tranquilli, W.J. Local and Regional Anesthetic and Analgesic Techniques: Dogs. In Lumb & Jones—Veterinary Anesthesia and Analgesia, 5th ed.; Grimm, K., Thurmon, J., Tranquilli, W.J., Eds.; Wiley-Blackwelll: Hoboken, NJ, USA, 2007; pp. 561–594. [Google Scholar]
- Campoy, L.; Martin-Flores, M.; Ludders, J.W.; Erb, H.N.; Gleed, R.D. (Comparison of bupivacaine femoral and sciatic nerve block versus bupivacaine and morphine epidural for stifle surgery in dogs. Vet Anaesth Analg 2012, 39, 91–98. [Google Scholar] [CrossRef]
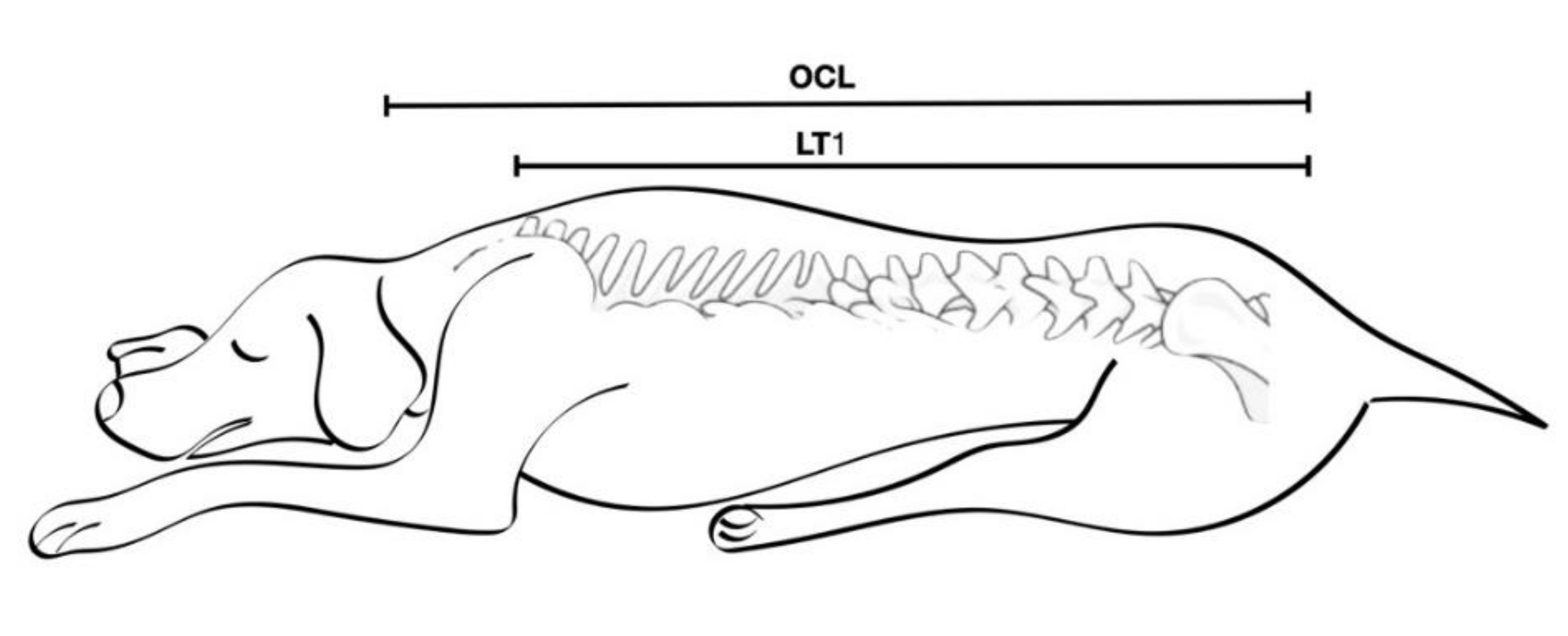
- Leite, G.M.D.P.; Augusto, L.E.F.; Pereira, V.G.; Cunha, A.F.; de Susa Pontes, K.C.; Santa, J.L.P. Comparative study of epidural anesthesia in dogs by weight or occipito-coccygeal distance. Rev. Ceres 2017, 64, 12–17. [Google Scholar] [CrossRef][Green Version]
- Valverde, A.; Skelding, A. Comparison of calculated lumbosacral epidural volumes of injectate using a dose regimen based on body weight versus length of the vertebral column in dogs. Vet. Anaesth. Analg. 2019, 46, 135–140. [Google Scholar] [CrossRef]
- Otero, P.E.; Tarragona, L.; Ceballos, M.; Portela, D. Epidural cephalic spread of a local anesthetic in dogs: A mathematical model using the column length. In Proceedings of the 10th World Congress of Veterinary Anaesthesia, Glasgow, UK, 31 August–4 September 2009; p. 35. [Google Scholar]
- Laflamme, D.P. Development and Validation of a Body Condition Score System for Dogs. Canine Pract. 1997, 1, 10–15. [Google Scholar]
- Steagall, P.V.M.; Teixeira, F.J.; Teixeira Neto, F.J.; Minto, B.W.; Campagnol, D.; Corrêa, M.A. Evaluation of the isoflurane-sparing effects of lidocaine and fentanyl during surgery in dogs. J. Am. Vet. Med. Assoc. 2006, 229, 522–527. [Google Scholar] [CrossRef]
- Mosing, M.; Reich, H.; Moens, Y. Clinical evaluation of the anaesthetic paring effect of brachial plexus block in cats. Vet. Anaesth. Analg. 2010, 37, 154–161. [Google Scholar] [CrossRef]
- Grubb, T.; Sager, J.; Gaynor, J.S.; Montgomery, E.; Parker, J.A.; Shafford, H.; Tearney, C. 2020 AAHA Anesthesia and Monitoring Guidelines for Dogs and Cats. J. Am. Anim. Hosp. Assoc. Available online: https://www.aaha.org/globalassets/02-guidelines/2020-anesthesia/anesthesia_and_monitoring-guidelines_final.pdf (accessed on 1 December 2021).
- Otero, P.E.; Fuensalida, S.E.; Portela, D. Section 5: Neuraxial blocks. In Otero PE, Portela DA, Manual of Small Animal Regional Anesthesia: Illustrated Anatomy for Nerve Stimulation and Ultrasound-Guided Nerve Blocks, 2nd ed.; Editorial Inter-Medica: Ciudad Autonoma de Buenos Aires, Argentina, 2019; pp. 275–311. [Google Scholar]
- Reid, J.; Nolan, A.M.; Hughes, J.M.L.; Lascelles, D.; Pawson, P.; Scott, E. Development of the short-form Glasgow Composite Measure Pain Scale (CMPS-SF) and derivation of an analgesic intervention score. Anim. Welf. 2007, 16, 97–104. [Google Scholar]
- Muguet-Chanoit, A.C.; Olby, N.J.; Babb, K.M.; Lim, J.-H.; Gallegher, R.; Niman, Z.; Dillard, S.; Campbell, J. The sensory field and repeatability of the cutaneous trunci muscle reflex of the dog. Vet. Surg. 2011, 40, 781–785. [Google Scholar] [CrossRef]
- Duke, T.; Caulkett, N.A.; Ball, S.D.; Remedios, A.M. Comparative analgesic and cardiopulmonary effects of bupivacaine and ropivacaine in the epidural space of the conscious dog. Vet. Anaesth. Analg. 2000, 27, 13–21. [Google Scholar] [CrossRef] [PubMed]
- Otero, P.E.; Campoy, L. Epidural and Spinal Anesthesia. In Small Animal Regional Anesthesia and Analgesia; Campoy, L., Read, M.R., Eds.; Wiley-Blackwell: Hoboken, NJ, USA, 2008; pp. 227–259. [Google Scholar]
- Torske, K.E.; Dyson, D.H. Epidural analgesia and anesthesia. Vet. Clin. N. Am. Small Anim. Pract. 2000, 30, 859–874. [Google Scholar] [CrossRef]
- Almeida, R.M.; Escobar, A.; Maguilnik, S. Comparison of analgesia provided by lidocaine, lidocaine-morphine or lidocaine-tramadol delivered epidurally in dogs following orchiectomy. Vet. Anaesth. Analg. 2012, 37, 542–549. [Google Scholar] [CrossRef] [PubMed]
- Freire, C.D.; Torres, M.L.A.; Fantoni, D.T.; Cavalcanti, R.L.; Noel-Morgan, J. Bupivacaine 0.25% and methylene blue spread with epidural anesthesia in dog. Vet. Anaesth. Analg. 2010, 37, 63–69. [Google Scholar] [CrossRef]
- Dias, R.S.G.; Soares, J.H.N.; Dos Santos E Castro, D.; Gress, M.A.K.A.; Lemos Machado, M.; Otero, P.E.; Ascoli, O.F. Cardiovascular and respiratory effects of lumbosacral epidural bupivacaine in isoflurane-anesthetized dogs: The effects of two volumes of 0.25% solution. PLoS ONE 2018, 13, e0195867. [Google Scholar] [CrossRef]
- Castro, D.S.; Soares, J.H.N.; Gress, M.A.K.A.; Otero, P.E.; Marostica, E.; Ascoli, F.O. Hypoventilation exacerbates the cardiovascular depression caused by a high volume of lumbosacral epidural bupivacaine in two isoflurane-anesthetized dogs. Vet. Anaesth. Analg. 2016, 37, 63–69. [Google Scholar] [CrossRef]
- Son, W.G.; Jang, M.; Yoon, J.; Lee, L.Y.; Lee, I. The effect of epidural injection speed on epidural pressure and distribution of solution in anesthetized dogs. Vet. Anaesth. 2014, 41, 526–533. [Google Scholar] [CrossRef]
- Iff, I.; Moens, Y.; Schatzmann, U. Use of pressure waves to confirm the correct placement of epidural needles in dogs. Vet. Rec. 2007, 161, 22–25. [Google Scholar] [CrossRef] [PubMed]
- Reina, M.A.; Franco, C.D.; López, A.; Dé Andrés, J.A.; van Zundert, A. Clinical implications of epidural fat in the spinal canal. A scanning electron microscopic study. Acta Anaesthesiol. Belg. 2009, 60, 7–17. [Google Scholar] [PubMed]
- Williamson, A.J.; Soares, J.H.; Henao-Guerrero, N.; McAlister Council-Troche, R.; Pavlisko, N.D. Cardiovascular and respiratory effects of two doses of fentanyl in the presence or absence of bradycardia in isoflurane-anesthetized dogs. Vet. Anaesth. Analg. 2018, 45, 423–431. [Google Scholar] [CrossRef] [PubMed]
- Griffioen, K.J.; Venkatesan, P.; Huang, Z.G.; Wang, X.; Bouairi, E.; Evans, C.; Gold, A.; Mendelowitz, D. Fentanyl inhibits GABAergic neurotransmission to cardiac vagal neurons in the nucleus ambiguus. Brain Res. 2004, 1007, 109–115. [Google Scholar] [CrossRef]
- Galloway, D.S.; Ko, J.C.; Reaugh, H.F.; Mandsager, R.E.; Payton, M.E.; Inoue, T.; Portillo, E. Anesthetic indices of sevoflurane and isoflurane in unpremedicated dogs. J. Am. Vet. Med. Assoc. 2004, 225, 700–704. [Google Scholar] [CrossRef]
- Sousa, M.G.; Carareto, R.; De-Nardi, A.B.; Brito, F.L.C.; Nunes, N.; Camaho, A.A. Effects of isoflurane on echocardiographic parameters in healthy dogs. Vet. Anaesth. Analg. 2008, 35, 185–190. [Google Scholar] [CrossRef]
- Gutierrez-Blanco, E.; Victoria-Mora, J.M.; Ibancovichi-Camarillo, J.A.; Sauri-Arceo, C.; Bolio-Gonzáles, M.E.; Acevedo-Arcique, C.M.; Marin-Cano, G.; Steagall, P.V.M. Evaluation of the isoflurane-sparing effects of fentanyl, lidocaine, ketamine, dexmedetomidine, or the combination lidocaine-ketamine-dexmedetomidine during ovariohysterectomy in dogs. Vet. Anaesth. Analg. 2013, 40, 599–609. [Google Scholar] [CrossRef]
- Albuquerque, V.B.; Souza, T.F.B.S.; Vivan, M.C.R.; Ferreira, J.Z.; Frade, M.C.; Perri, S.H.V.; de Souza Oliva, V.N.L. Ropivacaína isolada ou associada à morfina, butorfanol ou tramadol pela via peridural em cadelas para realização de ovariosalpingohisterectomia. Vet. Zootec. 2013, 20, 111–123. [Google Scholar]
- Pascoe, P.J.; Dyson, D.H. Analgesia after lateral thoracotomy in dogs. Epidural morphine vs. intercostal bupivacaine. Vet. Surg. 1993, 22, 141–147. [Google Scholar] [CrossRef]
- De Negri, P.; Ivani, G.; Tirri, T.; Modano, P.; Reato, C.; Eksborg, S.; Lonnqvist, P.-A. A comparison of epidural bupivacaine, levobupivacaine, and ropivacaine on postoperative analgesia and motor blockade. Anesth. Analg. 2004, 99, 45–48. [Google Scholar] [CrossRef]
- Taylor, A.; McLeod, G. Basic pharmacology of local anaesthetics. BJA Educ. 2020, 20, 34–41. [Google Scholar] [CrossRef] [PubMed]
| Time | Procedure |
|---|---|
| Sbase | 5 min before skin incision |
| SX1 | Skin incision |
| SX2 | Subcutaneous dissection |
| SX3 | Large veins and artery ligatures |
| SX4 | Mammary chain removal |
| SX5 | Skin closure |
| Number | Breed |
|---|---|
| 7 | Cross breed > 10 kg |
| 6 | Cross breed < 10 kg |
| 5 | Beagle |
| 2 | Boxer |
| 5 | Dachshund |
| 3 | German Shepherd |
| 6 | Labrador |
| 2 | Lagotto |
| 3 | Maltese |
| 2 | Pointer |
| 1 | Miniature Poodle |
| 4 | Retriever |
| 2 | Rottweiler |
| 1 | Standard Poodle |
| 1 | Yorkshire terrier |
| Group | Ages (month) | Weight (kg) | OCL (cm) | OCL Range (cm) | LT1 (cm) | LT1 Range (cm) | OCL% (%) | Injected (mL/cm OCL%) | Injected (mL/kg range) | Injected (Total mL) | Injected (mL kg−1) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| C | 124 ± 15 | 20.2 ± 11.5 | 69.4 ± 5 | (43–72) | 48.8 ± 16 | (30–67) | 69.3 ± 5 | - | - | - | - |
| R0.5% | 117 ± 26 | 21.5 ± 10 | 65.1 ± 12 | (41–78) | 46.5 ± 8.9 | (29–57) | 71.1 ± 1.5 | 0.16 ± 0.05 | (0.2–1) | 7.8 ± 2.7 | 0.48 ± 0.2 |
| MR0.5% | 123 ± 17 | 20.5 ± 12.3 | 63 ± 12.4 | (41–83) | 45 ± 10 | (28–64) | 69.5 ± 4.5 | 0.14 ± 0.1 | (0.3–0.9) | 8.8 ± 3.4 | 0.51 ± 0.2 |
| MR0.35% | 129 ± 16 | 28 ± 5.8 | 68.7 ± 7 | (49–87) | 48.7 ± 23 | (25–61) | 69.8 ± 1 | 0.15 ± 0.07 | (0.2–1.1) | 9.5 ± 2.6 | 0.5 ± 0.3 |
| MR0.25% | 113 ± 24 | 25 ± 7.5 | 70.9 ± 12 | (39–75) | 48.8 ± 10 | (28–58) | 70.1 ± 2 | 0.15 ± 0.04 | (0.25–1) | 8.7 ± 1.5 | 0.49 ± 0.3 |
| Variables | Group | Sbase | SX1 | SX2 | SX3 | SX4 | SX5 |
|---|---|---|---|---|---|---|---|
| HR (bpm) | C | 80 ± 19 | 92 ± 15 | 65 ± 17 | 67 ± 19 | 64 ± 13 | 68 ± 18 |
| R0.5% | 109 ± 8 | 77 ± 8 | 70 ± 9 | 74 ± 5 | 73 ± 15 | 72 ± 16 | |
| MR0.5% | 91 ± 9 | 88 ± 7 | 69 ± 5 | 71 ± 9 | 75 ± 4 | 71 ± 9 | |
| MR0.35% | 88 ± 10 | 79 ± 7 | 74 ± 9 | 80 ± 3 | 74 ± 8 | 73 ± 8 | |
| MR0.25% | 84 ± 13 | 82 ± 12 | 77 ± 9 | 86 ± 12 | 83 ± 8 | 86 ± 10 | |
| MAP (mmHg) | C | 104 ± 18 | 71 ± 14 | 66 ± 11 | 63 ± 8 | 60 ± 12 | 60 ± 8 |
| R0.5% | 71 ± 16 | 76 ± 9 | 74 ± 8 | 72 ± 12 | 72 ± 8 | 78 ± 9 | |
| MR0.5% | 73 ± 10 | 65 ± 12 | 70 ± 8 | 74 ± 9 | 69 ± 7 | 67 ± 8 | |
| MR0.35% | 81 ± 15 | 74 ± 7 | 74 ± 10 | 79 ± 11 | 75 ± 9 | 82 ± 10 | |
| MR0.25% | 86 ± 10 | 87 ± 15 | 86 ± 8 | 85 ± 7 | 87 ± 12 | 86 ± 9 | |
| fR (brpm) | C | 18 ± 5 | 15 ± 3 | 15 ± 4 | 13 ± 2 | 15 ± 3 | 10 ± 2 |
| R0.5% | 15 ± 5 | 15 ± 4 | 17 ± 3 | 18 ± 6 | 16 ± 5 | 18 ± 2 | |
| MR0.5% | 12 ± 7 | 14 ± 8 | 11 ± 6 | 15 ± 5 | 12 ± 8 | 11 ± 6 | |
| MR0.35% | 17 ± 4 | 15 ± 6 | 15 ± 3 | 13 ± 6 | 12 ± 3 | 13 ± 3 | |
| MR0.25% | 18 ± 5 | 15 ± 6 | 17 ± 9 | 14 ± 5 | 12 ± 6 | 14 ± 3 | |
| Pe’CO2 (mmHg) | C | 49 ± 10 | 39 ± 10 | 44 ± 3 | 44 ± 5 | 45 ± 5 | 46 ± 6 |
| R0.5% | 46 ± 7 | 41 ± 7 | 45 ± 8 | 42 ± 8 | 39 ± 6 | 41 ± 7 | |
| MR0.5% | 45 ± 5 | 43 ± 7 | 43 ± 7 | 44 ± 6 | 43 ± 8 | 40 ± 8 | |
| MR0.35% | 42 ± 8 | 41 ± 5 | 42 ± 7 | 40 ± 6 | 41 ± 4 | 43 ± 7 | |
| MR0.25% | 44 ± 3 | 43 ± 6 | 42 ± 9 | 41 ± 7 | 40 ± 7 | 40 ± 7 | |
| Fe’Iso (%) | C | 1.3 ± 0.05 | 1.3 ± 0.2 † | 1.3 ± 0.15 † | 1.3 ± 0.15 † | 1.3 ± 0.05 † | 1.3 ± 0.15 † |
| R0.5% | 1.3 ± 0.04 | 1.2 ± 0.04 | 1.2 ± 0.03 | 1.1 ± 0.05 | 1.1 ± 0.05 | 1.2 ± 0.05 | |
| MR0.5% | 1.3 ± 0.05 | 1.1 ± 0.05 | 1.0 ± 0.05 | 0.9 ± 0.04 | 0.9 ± 0.05 | 0.9 ± 0.05 | |
| MR0.35% | 1.3 ± 0.03 | 1.2 ± 0.05 | 1.1 ± 0.02 | 1.0 ± 0.03 | 1.0 ± 0.05 | 1.0 ± 0.05 | |
| MR0.25% | 1.3 ± 0.05 | 1.2 ± 0.05 | 1.1 ± 0.1 | 1.1 ± 0.1 | 1.1 ± 0.05 | 1.1 ± 0.1 | |
| Temp (C°) | C | 36.2 ± 0.5 | 36.2 ± 0.5 | 36.7 ± 0.3 | 36.6 ± 0.2 | 36.8 ± 0.4 | 36.5 ± 0.9 |
| R0.5% | 35.7 ± 0.7 | 35.4 ± 0.5 | 35.2 ± 0.5 | 35.3 ± 0.7 | 36.2 ± 0.8 | 36.5 ± 0.5 | |
| MR0.5% | 35.5 ± 0.8 | 35.2 ± 0.8 | 34.8 ± 0.8 | 34.9 ± 0.8 | 35.4 ± 0.8 | 36.6 ± 0.5 | |
| MR0.35% | 35.9 ± 0.9 | 35.2 ± 0.7 | 35 ± 0.9 | 35.5 ± 0.3 | 35.8 ± 0.5 | 36.2 ± 0.4 | |
| MR0.25% | 35.2 ± 0.7 | 35.1 ± 0.9 | 35 ± 0.5 | 35.5 ± 0.5 | 35.8 ± 0.5 | 36.0 ± 0.7 | |
| Mean Fentanyl | C | 9.8 ± 5.5 µg kg−1 h−1 † | |||||
| R0.5% | 1.1 ± 0.5 µg kg−1 h−1 | ||||||
| MR0.5% | 0.2 ± 0.14 µg kg−1 h−1 | ||||||
| MR0.35% | 0.7 ± 0.6 µg kg−1 h−1 | ||||||
| MR0.25% | 1.2 ± 0.9 µg kg−1 h−1 | ||||||
| Groups | CMT Reflex | Patellar Reflex | Withdrawal Response | Ability to Stand | Ability to Walk | Spontaneous Urination | Methadone over 24 h |
|---|---|---|---|---|---|---|---|
| C | 0.25 ± 0 * | 0.25 ± 0 * | 0.25 ± 0 * | 0.5 ± 0.2 * | 0.5 ± 0.7 * | 6.9 ± 3.2 | 1.8 ± 0.5 * |
| R0.5% | 6.1 ± 1.2 | 6.6 ± 1.5 | 7.1 ± 1.1 | 7.4 ± 1.3 | 7.8 ± 1.1 | 6.1 ± 1.2 | 0.8 ± 0.1 |
| MR0.5% | 5.6 ± 1.0 | 5.3 ± 1.4 | 5.3 ± 1.2 | 7.4 ± 1.2 | 7 ± 1.5 | 7.6 ± 1 | 0.0 ± 0.0 *,** |
| MR0.35% | 3.2 ± 0.5 ** | 3.7 ± 1.5 ** | 3.5 ± 0.2 ** | 3.6 ± 0.7 ** | 3.8 ± 0.5 ** | 5.0 ± 1.6 | 0.3 ± 0.05 |
| MR0.25% | 3.3 ± 0.6 ** | 3.5 ± 0.8 ** | 3.2 ± 1 ** | 3.5 ± 0.1 ** | 3.6 ± 0.1 ** | 5.5 ± 2.8 | 0.4 ± 0.03 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tayari, H.; Otero, P.E.; D’Agostino, M.; Bartolini, F.; Briganti, A. Epidural Volume of Injectate Using a Dose Regimen Based on Occipito-Coccygeal Spinal Length (OCL): Randomized Clinical Study Comparing Different Ropivacaine Concentrations, with or without Morphine, in Bitches Undergoing Total Unilateral Mastectomy. Animals 2022, 12, 587. https://doi.org/10.3390/ani12050587
Tayari H, Otero PE, D’Agostino M, Bartolini F, Briganti A. Epidural Volume of Injectate Using a Dose Regimen Based on Occipito-Coccygeal Spinal Length (OCL): Randomized Clinical Study Comparing Different Ropivacaine Concentrations, with or without Morphine, in Bitches Undergoing Total Unilateral Mastectomy. Animals. 2022; 12(5):587. https://doi.org/10.3390/ani12050587
Chicago/Turabian StyleTayari, Hamaseh, Pablo E. Otero, Marco D’Agostino, Flavia Bartolini, and Angela Briganti. 2022. "Epidural Volume of Injectate Using a Dose Regimen Based on Occipito-Coccygeal Spinal Length (OCL): Randomized Clinical Study Comparing Different Ropivacaine Concentrations, with or without Morphine, in Bitches Undergoing Total Unilateral Mastectomy" Animals 12, no. 5: 587. https://doi.org/10.3390/ani12050587
APA StyleTayari, H., Otero, P. E., D’Agostino, M., Bartolini, F., & Briganti, A. (2022). Epidural Volume of Injectate Using a Dose Regimen Based on Occipito-Coccygeal Spinal Length (OCL): Randomized Clinical Study Comparing Different Ropivacaine Concentrations, with or without Morphine, in Bitches Undergoing Total Unilateral Mastectomy. Animals, 12(5), 587. https://doi.org/10.3390/ani12050587







