Molecular Characterization and Antimicrobial Susceptibilities of Corynebacterium pseudotuberculosis Isolated from Caseous Lymphadenitis of Smallholder Sheep and Goats
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. C. pseudotuberculosis Isolation and Identification
2.3. DNA Extraction and PCR Amplification
2.4. Antimicrobial Susceptibility Testing
2.5. Detection of Virulence and Resistance Genes
2.6. ERIC Genotyping
2.7. DNA Sequencing and Analysis
2.8. Data Analysis
3. Results
3.1. Study Population
3.2. C. pseudotuberculosis Isolation and Identification
3.3. Antimicrobial Resistance of C. pseudotuberculosis Isolates
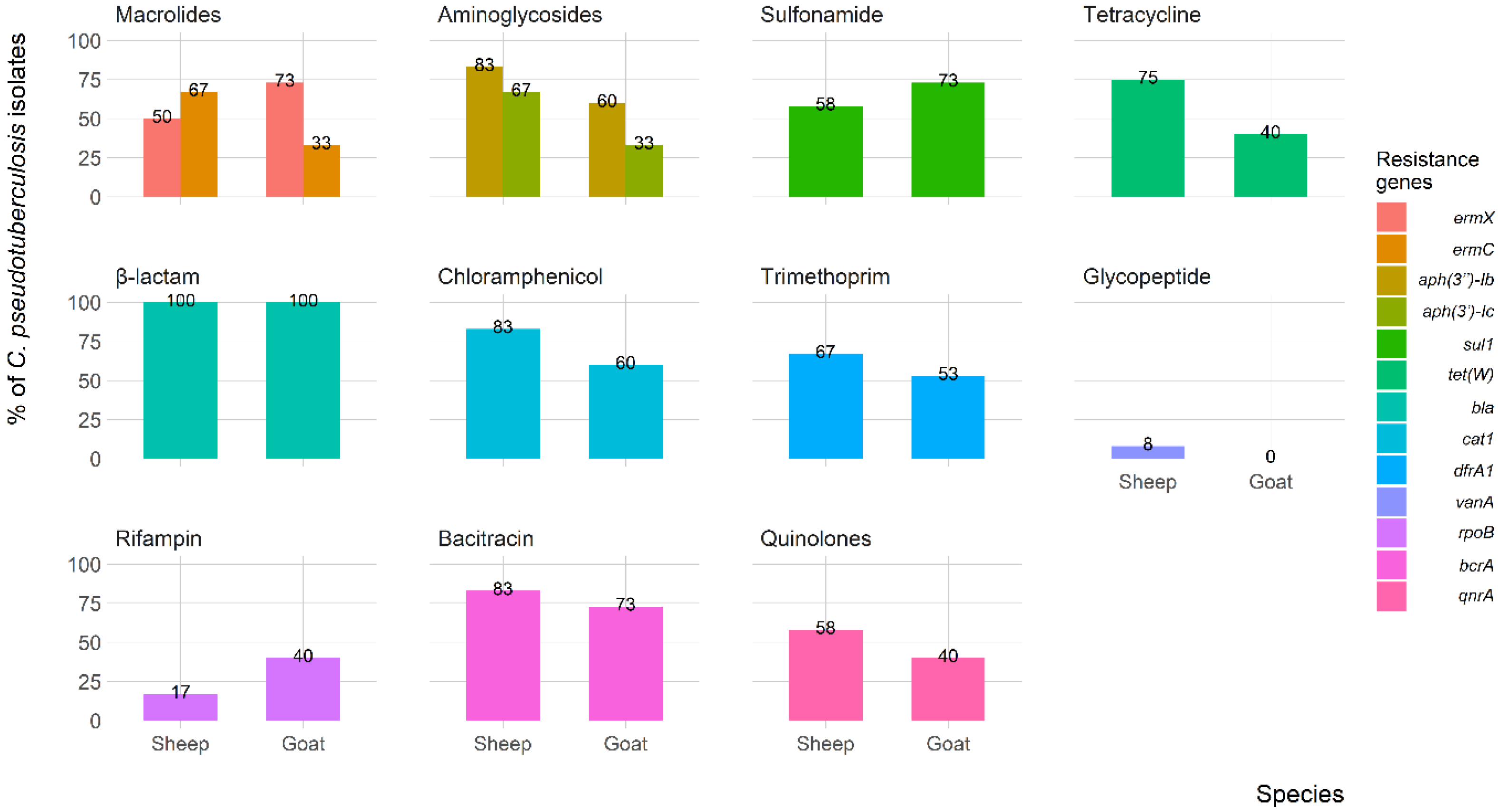
3.4. Virulence and Resistance Genes
3.5. Genotyping and Phylogenetic Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Arsenault, J.; Girard, C.; Dubreuil, P.; Daignault, D.; Galarneau, J.-R.; Boisclair, J.; Simard, C.; Bélanger, D. Prevalence of and carcass condemnation from maedi–visna, paratuberculosis and caseous lymphadenitis in culled sheep from Quebec, Canada. Prev. Vet. Med. 2003, 59, 67–81. [Google Scholar] [CrossRef]
- Oreiby, A.; Hegazy, Y.; Osman, S.; Ghanem, Y.; Al-Gaabary, M. Caseous lymphadenitis in small ruminants in Egypt. Tierärztliche Prax. Ausg. G Großtiere/Nutztiere 2014, 42, 271–277. [Google Scholar] [CrossRef]
- Collett, M.G.; Bath, G.F.; Cameron, C.M. Corynebacterium pseudotuberculosis Infections; Oxford University Press: New York, NY, USA, 1994. [Google Scholar]
- Oliveira, A.; Teixeira, P.; Azevedo, M.; Jamal, S.B.; Tiwari, S.; Almeida, S.; Silva, A.; Barh, D.; Dorneles, E.M.S.; Haas, D.J. Corynebacterium pseudotuberculosis may be under anagenesis and biovar Equi forms biovar Ovis: A phylogenic inference from sequence and structural analysis. BMC Microbiol. 2016, 16, 100. [Google Scholar] [CrossRef] [PubMed]
- Fontaine, M.; Baird, G. Caseous lymphadenitis. Small Rumin. Res. 2008, 76, 42–48. [Google Scholar] [CrossRef]
- Al-Gaabary, M.H.; Osman, S.A.; Oreiby, A.F. Caseous lymphadenitis in sheep and goats: Clinical, epidemiological and preventive studies. Small Rumin. Res. 2009, 87, 116–121. [Google Scholar] [CrossRef]
- Bastos, B.; Portela, R.D.; Dorella, F.; Ribeiro, D.; Seyffert, N.; Castro, T.; Miyoshi, A.; Oliveira, S.; Meyer, R.; Azevedo, V. Corynebacterium pseudotuberculosis: Immunological responses in animal models and zoonotic potential. J. Clin. Cell Immunol. S 2012, 4, 10.4172. [Google Scholar] [CrossRef]
- Li, H.; Yang, H.; Zhou, Z.; Li, X.; Yi, W.; Xu, Y.; Wang, Z.; Hu, S. Isolation, antibiotic resistance, virulence traits and phylogenetic analysis of Corynebacterium pseudotuberculosis from goats in southwestern China. Small Rumin. Res. 2018, 168, 69–75. [Google Scholar] [CrossRef]
- Binns, S.H.; Green, L.E.; Bailey, M. Development and validation of an ELISA to detect antibodies to Corynebacterium pseudotuberculosis in ovine sera. Vet. Microbiol. 2007, 123, 169–179. [Google Scholar] [CrossRef]
- Sutherland, S.; Hart, R.; Buller, N. Genetic differences between nitrate-negative and nitrate-positive C. pseudotuberculosis strains using restriction fragment length polymorphisms. Vet. Microbiol. 1996, 49, 1–9. [Google Scholar] [CrossRef]
- Connor, K.M.; Quirie, M.M.; Baird, G.; Donachie, W. Characterization of United Kingdom isolates of Corynebacterium pseudotuberculosis using pulsed-field gel electrophoresis. J. Clin. Microbiol. 2000, 38, 2633–2637. [Google Scholar] [CrossRef]
- Sutherland, S.; Hart, R.; Buller, N. Ribotype analysis of Corynebacterium pseudotuberculosis isolates from sheep and goats. Aust. Vet. J. 1993, 70, 454–456. [Google Scholar] [CrossRef]
- de Sa Guimaraes, A.; Dorneles, E.M.S.; Andrade, G.I.; Lage, A.P.; Miyoshi, A.; Azevedo, V.; Gouveia, A.M.G.; Heinemann, M.B. Molecular characterization of Corynebacterium pseudotuberculosis isolates using ERIC-PCR. Vet. Microbiol. 2011, 153, 299–306. [Google Scholar] [CrossRef]
- Dorneles, E.; Santana, J.; Andrade, G.; Santos, E.; Guimarães, A.; Mota, R.; Santos, A.; Miyoshi, A.; Azevedo, V.; Gouveia, A. Molecular characterization of Corynebacterium pseudotuberculosis isolated from goats using ERIC-PCR. Genet. Mol. Res. 2012, 11, 2051–2059. [Google Scholar] [CrossRef]
- Dorneles, E.M.; Santana, J.A.; Ribeiro, D.; Dorella, F.A.; Guimaraes, A.S.; Moawad, M.S.; Selim, S.A.; Garaldi, A.L.M.; Miyoshi, A.; Ribeiro, M.G. Evaluation of ERIC-PCR as genotyping method for Corynebacterium pseudotuberculosis isolates. PLoS ONE 2014, 9, e98758. [Google Scholar] [CrossRef]
- Dorella, F.; Pacheco, L.G.C.; Oliveira, S.; Miyoshi, A.; Azevedo, V. Corynebacterium pseudotuberculosis: Microbiology, biochemical properties, pathogenesis and molecular studies of virulence. Vet. Res. 2006, 37, 201–218. [Google Scholar] [CrossRef]
- Hodgson, A.; Tachedjian, M.; Corner, L.A.; Radford, A.J. Protection of sheep against caseous lymphadenitis by use of a single oral dose of live recombinant Corynebacterium pseudotuberculosis. Infect. Immun. 1994, 62, 5275–5280. [Google Scholar] [CrossRef]
- Baird, G.; Fontaine, M. Corynebacterium pseudotuberculosis and its role in ovine caseous lymphadenitis. J. Comp. Pathol. 2007, 137, 179–210. [Google Scholar] [CrossRef]
- Billington, S.J.; Esmay, P.A.; Songer, J.G.; Jost, B.H. Identification and role in virulence of putative iron acquisition genes from Corynebacterium pseudotuberculosis. FEMS Microbiol. Lett. 2002, 208, 41–45. [Google Scholar] [CrossRef]
- Farias, A.M.; Alves, J.R.; Alves, F.S.; Pinheiro, R.R.; Faccioli-Martins, P.Y.; Lima, A.; Azevedo, S.S.; Alves, C.J. Serological study on Corynebacterium pseudotuberculosis infection in goats in the Brazilian Northeast using enzyme-linked immunosorbent assay (ELISA-indirect). Pesqui. Veterinária Bras. 2018, 38, 1344–1350. [Google Scholar] [CrossRef]
- Abebe, D.; Sisay Tessema, T. Determination of Corynebacterium pseudotuberculosis prevalence and antimicrobial susceptibility pattern of isolates from lymph nodes of sheep and goats at an organic export abattoir, Modjo, Ethiopia. Lett. Appl. Microbiol. 2015, 61, 469–476. [Google Scholar] [CrossRef]
- Algammal, A. Molecular characterization and antibiotic susceptibility of Corynebacterium pseudotuberculosis isolated from sheep and goats suffering from caseous lymphadenitis. Zagazig Vet. J. 2016, 44, 1–8. [Google Scholar] [CrossRef]
- Al-Gaabary, M.H.; Osman, S.A.; Ahmed, M.S.; Oreiby, A.F. Abattoir survey on caseous lymphadenitis in sheep and goats in Tanta, Egypt. Small Rumin. Res. 2010, 94, 117–124. [Google Scholar] [CrossRef]
- Magdy Selim, A.; Atwa, S.M.; El Gedawy, A.A.; Younis, E.E. Epidemiological, bacteriological and molecular studies on caseous lymphadenitis in sheep of Dakhlia, Egypt. Anim. Biotechnol. 2022, 33, 1655–1660. [Google Scholar] [CrossRef] [PubMed]
- Quinn, P.J.; Markey, B.K.; Leonard, F.C.; Hartigan, P.; Fanning, S.; Fitzpatrick, E. Veterinary Microbiology and Microbial Disease; John Wiley & Sons: Hoboken, NJ, USA, 2011. [Google Scholar]
- Markey, B.; Leonard, F.; Archambault, M.; Cullinane, A.; Maguire, D. Clinical Veterinary Microbiology E-Book; Elsevier Health Sciences: Amsterdam, The Netherlands, 2013. [Google Scholar]
- Cowan, S.T.; Steel, K.J. Manual for the Identification of Medical Bacteria, 3rd ed.; Cambridge University Press: Cambridge, UK, 1965; pp. 75–79. [Google Scholar]
- Cetinkaya, B.; Karahan, M.; Atil, E.; Kalin, R.; De Baere, T.; Vaneechoutte, M. Identification of Corynebacterium pseudotuberculosis isolates from sheep and goats by PCR. Vet. Microbiol. 2002, 88, 75–83. [Google Scholar] [CrossRef]
- Pacheco, L.G.; Pena, R.R.; Castro, T.L.; Dorella, F.A.; Bahia, R.C.; Carminati, R.; Frota, M.N.; Oliveira, S.C.; Meyer, R.; Alves, F.S. Multiplex PCR assay for identification of Corynebacterium pseudotuberculosis from pure cultures and for rapid detection of this pathogen in clinical samples. J. Med. Microbiol. 2007, 56, 480–486. [Google Scholar] [CrossRef]
- Ilhan, Z. Detection of Corynebacterium pseudotuberculosis from sheep lymph nodes by PCR. Rev. Med. Vet. 2013, 164, 60–66. [Google Scholar]
- D’Afonseca, V.; Prosdocimi, F.; Dorella, F.A.; Pacheco, L.G.C.; Moraes, P.M.; Pena, I.; Ortega, J.M.; Teixeira, S.; Oliveira, S.C.; Coser, E.M. Survey of genome organization and gene content of Corynebacterium pseudotuberculosis. Microbiol. Res. 2010, 165, 312–320. [Google Scholar] [CrossRef]
- de Sá, M.d.C.A.; Gouveia, G.V.; Krewer, C.d.C.; Veschi, J.L.A.; de Mattos-Guaraldi, A.L.; da Costa, M.M. Distribution of PLD and FagA, B, C and D genes in Corynebacterium pseudotuberculosis isolates from sheep and goats with caseus lymphadenitis. Genet. Mol. Biol. 2013, 36, 265–268. [Google Scholar]
- Rosato, A.E.; Lee, B.S.; Nash, K.A. Inducible macrolide resistance in Corynebacterium jeikeium. Antimicrob. Agents Chemother. 2001, 45, 1982–1989. [Google Scholar] [CrossRef]
- Jeong, D.-W.; Lee, B.; Heo, S.; Oh, Y.; Heo, G.; Lee, J.-H. Two genes involved in clindamycin resistance of Bacillus licheniformis and Bacillus paralicheniformis identified by comparative genomic analysis. PLoS ONE 2020, 15, e0231274. [Google Scholar] [CrossRef]
- Dutka-Malen, S.; Evers, S.; Courvalin, P. Detection of glycopeptide resistance genotypes and identification to the species level of clinically relevant Enterococci by PCR. J. Clin. Microbiol. 1995, 33, 24–27. [Google Scholar] [CrossRef]
- Williams, D.; Spring, L.; Collins, L.; Miller, L.; Heifets, L.; Gangadharam, P.; Gillis, T. Contribution of rpoB mutations to development of rifamycin cross-resistance in Mycobacterium tuberculosis. Antimicrob. Agents Chemother. 1998, 42, 1853–1857. [Google Scholar] [CrossRef]
- Charlebois, A.; Jalbert, L.-A.; Harel, J.; Masson, L.; Archambault, M. Characterization of genes encoding for acquired bacitracin resistance in Clostridium perfringens. PLoS ONE 2012, 7, e44449. [Google Scholar] [CrossRef]
- Jacoby, G.A.; Chow, N.; Waites, K.B. Prevalence of plasmid-mediated quinolone resistance. Antimicrob. Agents Chemother. 2003, 47, 559–562. [Google Scholar] [CrossRef]
- Gebreyes, W.A.; Altier, C. Molecular characterization of multidrug-resistant Salmonella enterica subsp. enterica serovar Typhimurium isolates from swine. J. Clin. Microbiol. 2002, 40, 2813–2822. [Google Scholar] [CrossRef]
- Miró, E.; Grünbaum, F.; Gómez, L.; Rivera, A.; Mirelis, B.; Coll, P.; Navarro, F. Characterization of aminoglycoside-modifying enzymes in Enterobacteriaceae clinical strains and characterization of the plasmids implicated in their diffusion. Microb. Drug Resist. 2013, 19, 94–99. [Google Scholar] [CrossRef]
- Heuer, H.; Smalla, K. Manure and sulfadiazine synergistically increased bacterial antibiotic resistance in soil over at least two months. Environ. Microbiol. 2007, 9, 657–666. [Google Scholar] [CrossRef]
- Schröder, J.; Maus, I.; Meyer, K.; Wördemann, S.; Blom, J.; Jaenicke, S.; Schneider, J.; Trost, E.; Tauch, A. Complete genome sequence, lifestyle, and multi-drug resistance of the human pathogen Corynebacterium resistens DSM 45100 isolated from blood samples of a leukemia patient. BMC Genom. 2012, 13, 141. [Google Scholar] [CrossRef]
- Alibi, S.; Ferjani, A.; Boukadida, J.; Cano, M.E.; Fernández-Martínez, M.; Martínez-Martínez, L.; Navas, J. Occurrence of Corynebacterium striatum as an emerging antibiotic-resistant nosocomial pathogen in a Tunisian hospital. Sci. Rep. 2017, 7, 9704. [Google Scholar] [CrossRef]
- Abdolmaleki, Z.; Mashak, Z.; Safarpoor Dehkordi, F. Phenotypic and genotypic characterization of antibiotic resistance in the methicillin-resistant Staphylococcus aureus strains isolated from hospital cockroaches. Antimicrob. Resist. Infect. Control 2019, 8, 54. [Google Scholar] [CrossRef]
- Versalovic, J.; Koeuth, T.; Lupski, R. Distribution of repetitive DNA sequences in eubacteria and application to finerpriting of bacterial enomes. Nucleic Acids Res. 1991, 19, 6823–6831. [Google Scholar] [CrossRef] [PubMed]
- CLSI. Clinical and Laboratory Standards Institute: Performance Standards for Antimicrobial Susceptibility Testing, 30th ed.; CLSI Doc. M100; CLSI: Wayne, PA, USA, 2020. [Google Scholar]
- Tambekar, D.; Dhanorkar, D.; Gulhane, S.; Khandelwal, V.; Dudhane, M. Antibacterial susceptibility of some urinary tract pathogens to commonly used antibiotics. Afr. J. Biotechnol. 2006, 5, 1562–1565. [Google Scholar]
- Kumar, S.; Stecher, G.; Tamura, K. MEGA7: Molecular evolutionary genetics analysis version 7.0 for bigger datasets. Mol. Biol. Evol. 2016, 33, 1870–1874. [Google Scholar] [CrossRef] [PubMed]
- Saitou, N.; Nei, M. The neighbor-joining method: A new method for reconstructing phylogenetic trees. Mol. Biol. Evol. 1987, 4, 406–425. [Google Scholar]
- Kimura, M. A simple method for estimating evolutionary rates of base substitutions through comparative studies of nucleotide sequences. J. Mol. Evol. 1980, 16, 111–120. [Google Scholar] [CrossRef]
- Collignon, P.J.; Conly, J.M.; Andremont, A.; McEwen, S.A.; Aidara-Kane, A.; WHO-AGISAR; Agerso, Y.; Andremont, A.; Collignon, P.; Conly, J.; et al. World Health Organization ranking of antimicrobials according to their importance in human medicine: A critical step for developing risk management strategies to control antimicrobial resistance from food animal production. Clin. Infect. Dis. 2016, 63, 1087–1093. [Google Scholar] [CrossRef]
- Kusiluka, L.; Kambarage, D. Diseases of small ruminants: A handbook. Common Dis. Sheep Goats Sub-Sahar. Afr. 1996, 35–37. [Google Scholar]
- Kumar, J.; Singh, F.; Tripathi, B.N.; Kumar, R.; Dixit, S.K.; Sonawane, G.G. Epidemiological, bacteriological and molecular studies on caseous lymphadenitis in Sirohi goats of Rajasthan, India. Trop. Anim. Health Prod. 2012, 44, 1319–1322. [Google Scholar] [CrossRef]
- Yitagesu, E.; Alemnew, E.; Olani, A.; Asfaw, T.; Demis, C. Survival analysis of clinical cases of caseous lymphadenitis of goats in North Shoa, Ethiopia. Vet. Med. Int. 2020, 2020, 8822997. [Google Scholar] [CrossRef]
- Sayed, S.M.; El Berbawy, S.M.; Al Habaty, S.H. Sheep caseous lymphadenitis: Causative bacterial agents and their in vitro some antimicrobial susceptibility. Assiut Univ. Bull. Environ. Res. 2012, 15, 65–76. [Google Scholar]
- Rizk, A.M.; El-Tawab, A.; Awad, A.; AFIFI, S.E.; Mohamed, S.R. Corynebacterium pseudotuberculosis infection in small ruminant and molecular study of virulence and resistance genes in Beni-Suef Governorate. Benha Vet. Med. J. 2019, 37, 122–127. [Google Scholar] [CrossRef]
- Selim, A.M.; Atwa, S.M.; El Gedawy, A.A.; Hegazy, Y.M.; Rizk, M.A.; Younis, E.E. Risk factors associated with the seroprevalence of caseous lymphadenitis in sheep. Comp. Clin. Pathol. 2021, 30, 285–291. [Google Scholar] [CrossRef]
- Al-Harbi, K.B. Prevalence and etiology of abscess disease of sheep and goats at Qassim region, Saudi Arabia. Vet. World 2011, 4, 495. [Google Scholar] [CrossRef]
- Tripathi, B.; Kumar, J.; Sonawane, G.; Kumar, R.; Dixit, S. Microbiological and molecular investigation of clinically suspected caseous lymphadenitis cases in goats. Agric. Res. 2016, 5, 413–419. [Google Scholar] [CrossRef]
- Pathirana, H.N.K.S.; Cho, H.S.; Cho, Y.I.; Kim, C.L.; Wimalasena, S.H.M.P.; Rajapaksha, L.G.T.G.; Gunasekara, C.W.R.; Kim, C.H.; Seo, B.J.; Moon, S.H. Molecular characterization and antimicrobial susceptibility of Corynebacterium pseudotuberculosis isolated from skin abscesses of native Korean goats (Capra hircus coreanae). J. Appl. Microbiol. 2022, 133, 2074–2082. [Google Scholar] [CrossRef]
- Hassan, N.; Al-Humiany, A.; Bahobail, A.; Mansour, A. Bacteriological and pathological studies on Caseous lymphadenitis in sheep in Saudi Arabia. Int. J. Microbiol. Res. 2011, 2, 28–37. [Google Scholar]
- Robaj, A.; Hamidi, A.; Bytyqi, H.; Sylejmani, D. Frequency and antimicrobial susceptibility of bacterial isolates from caseous lymphadenitis in sheep in Kosovo. Bulg. J. Agri. Sci. 2017, 23, 1033–1036. [Google Scholar]
- Guerrero, J.A.V.; de Oca Jiménez, R.M.; Dibarrat, J.A.; León, F.H.; Morales-Erasto, V.; Salazar, H.G.M. Isolation and molecular characterization of Corynebacterium pseudotuberculosis from sheep and goats in Mexico. Microb. Pathog. 2018, 117, 304–309. [Google Scholar] [CrossRef]
- Gallardo, A.A.; Toledo, R.A.; González Pasayo, R.A.; Azevedo, V.; Robles, C.; Paolicchi, F.A.; Estevao Belchior, S.G. Corynebacterium pseudotuberculosis biovar Ovis: Evaluación de la sensibilidad antibiótica in vitro. Rev. Argent. Microbiol. 2019, 51, 334–338. [Google Scholar] [CrossRef] [PubMed]
- Dorado-García, A.; Bos, M.E.; Graveland, H.; Van Cleef, B.A.; Verstappen, K.M.; Kluytmans, J.A.; Wagenaar, J.A.; Heederik, D.J. Risk factors for persistence of livestock-associated MRSA and environmental exposure in veal calf farmers and their family members: An observational longitudinal study. BMJ Open 2013, 3, e003272. [Google Scholar] [CrossRef] [PubMed]
- Ruiz, J.C.; D’Afonseca, V.; Silva, A.; Ali, A.; Pinto, A.C.; Santos, A.R.; Rocha, A.A.; Lopes, D.O.; Dorella, F.A.; Pacheco, L.G. Evidence for reductive genome evolution and lateral acquisition of virulence functions in two Corynebacterium pseudotuberculosis strains. PLoS ONE 2011, 6, e18551. [Google Scholar] [CrossRef]
- Soares, S.C.; Silva, A.; Trost, E.; Blom, J.; Ramos, R.; Carneiro, A.; Ali, A.; Santos, A.R.; Pinto, A.C.; Diniz, C. The pan-genome of the animal pathogen Corynebacterium pseudotuberculosis reveals differences in genome plasticity between the biovar Ovis and equi strains. PLoS ONE 2013, 8, e53818. [Google Scholar] [CrossRef] [PubMed]
- Torky, H.A.; Saad, H.M.; Khaliel, S.A.; Kassih, A.T.; Sabatier, J.-M.; Batiha, G.E.-S.; Hetta, H.F.; Elghazaly, E.M.; De Waard, M. Isolation and Molecular Characterization of Corynebacterium pseudotuberculosis: Association with Proinflammatory Cytokines in Caseous Lymphadenitis Pyogranulomas. Animals 2023, 13, 296. [Google Scholar] [CrossRef]
- O’reilly, K.; Green, L.; Malone, F.; Medley, G. Parameter estimation and simulations of a mathematical model of Corynebacterium pseudotuberculosis transmission in sheep. Prev. Vet. Med. 2008, 83, 242–259. [Google Scholar] [CrossRef]
- Retamal, P.; Ríos, M.; Cheuquepán, F.; Abalos, P.; Pizarro-Lucero, J.; Borie, C.; Gutierrez, J. Host associated polymorphisms in the Corynebacterium pseudotuberculosis rpoB gene sequence. Vet. Microbiol. 2011, 151, 400–403. [Google Scholar] [CrossRef]
- Sellyei, B.; Bányai, K.; Bartha, D.; Hajtós, I.; Fodor, L.; Makrai, L. Multilocus sequencing of Corynebacterium pseudotuberculosis biotype ovis strains. BioMed. Res. Int. 2017, 2017, 1762162. [Google Scholar] [CrossRef]





| Target Genes | Nucleotide Sequence (5′→3′) | Amplicon Size (bp) | Annealing Temperature (°C) | Reference |
|---|---|---|---|---|
| Bacterial identification: | ||||
| 16S rRNA | F: ACCGCACTTTAGTGTGTGTG | 815 | 56 | [28] |
| R: TCTCTACGCCGATCTTGTAT | ||||
| rpoB | F: CGTATGAACATCGGCCAGGT | 446 | 55 | [29] |
| R: TCCATTTCGCCGAAGCGCTG | ||||
| Virulence genes: | ||||
| PLD | F: ATAAGCGTAAGCAGGGAGCA | 203 | 56 | [30] |
| R: ATCAGCGGTGATTGTCTTCCAGG | ||||
| PIP | F: AACTGCGGCTTTCTTTATTC | 551 | 54 | [31] |
| R: GACAAGTGGGAACGGTATCT | ||||
| FagA | F:AGCAAGACCAAGAGACATGC | 245 | 58 | [32] |
| R:AGTCTCAGCCCAACGTACAG | ||||
| FagB | F:GTGAGAAGAACCCCGGTATAAG | 291 | 55 | [32] |
| R: TACCGCACTTATTCTGACACTG | ||||
| FagC | F:GTTTGGCTATCTCCTTGGTATG | 173 | 60 | [32] |
| R: CGACCTTAGTGTTGACATACCC | ||||
| FagD | F:GAGACTATCGACCAGGCAG | 226 | 61 | [32] |
| R: ACTTCTTGGGGAGCAGTTCT | ||||
| Resistance genes: | ||||
| ermX | F:TCCTTACCAGTGCCCTTATCC | 390 | 65 | [33] |
| R: GAGTTCCAGCGCATCACC | ||||
| ermC | ermC-106: ATTGTGGATCGGGCAAATATT | 447 | 53 | [34] |
| ermC-535: TGGAGGGGGAGAAAAATG | ||||
| vanA | F:GGGAAAACGACAATTGC | 732 | 60 | [35] |
| R: GTACAATGCGGCCGTTA | ||||
| rpoB | TbRif1: AG ACG TTG ATC AAC ATC CG | 304 | 55 | [36] |
| TbRif2: TAC GGC GTT TCG ATG AAC | ||||
| bcrA | CP-F: GGCAATACCAAGCCGTTGCTTCAT | 408 | 55 | [37] |
| CP-R: TTACGAAGCGATACGGAACAGCCA | ||||
| qnrA | QP1: GATAAAGTTTTTCAGCAAGAGG | 657 | 57 | [38] |
| QP2: ATCCAGATCGGCAAAGGTTA | ||||
| ermA | F: TCCTTACCAGTGCCCTTATCC | 390 | 65 | [33] |
| R: GAGTTCCAGCGCATCACC | ||||
| aph(3″)-Ib | F: CTTGGTGATAACGGCAATTC | 548 | 52 | [39] |
| R: CCAATCGCAGATAGAAGGC | ||||
| aph(3′)-Ic | F: CGAGCATCAAATGAAACTGC | 624 | 54 | [40] |
| R: GCGTTGCCAATGATGTTACAG | ||||
| sul1 | F: CGG CGT GGG CTA CCT GAA CG | 433 | 50 | [41] |
| R: GCC GAT CGC GTG AAG TTC CG | ||||
| tet (W) | F: TTCGATGGTGGCACAGTA | 234 | 60 | [42] |
| R: TTGTTCGGCTGGAACGTA | ||||
| bla | F: CAGTCTAGCCACTTCGCCAAT | 808 | 55 | [43] |
| R: TGACTGCACGGATGGAGATGG | ||||
| cat1 | F: AGTTGCTCAATGTACCTATAACC | 547 | 55 | [44] |
| R: TTGTAATTCATTAAGCATTCTGCC | ||||
| dfrA1 | F: CTCACGATAAACAAAGAGTCA | 201 | 50 | [44] |
| R: CAATCATTGCTTCGTATAACG | ||||
| ERIC-PCR: | ||||
| ERIC-1 ERIC-2 | F: ATGTAAGCTCCTGGGGATTCAC | Variable | 52 | [45] |
| R: AAGTAAGTGACTGGGGTGAGCG | ||||
| Variable | Categories | N (%) | Number of Examined (%) | |
|---|---|---|---|---|
| Sheep | Goats | |||
| Gender | ||||
| Female | 91 (41.4) | 57 (43.8) | 34 (37.8) | |
| Male | 129 (58.6) | 73 (56.2) | 56 (62.2) | |
| Age | ||||
| <1 year | 40 (18.2) | 25 (19.2) | 15 (16.7) | |
| 1–2 years | 83 (37.7) | 39 (30.0) | 44 (48.9) | |
| >2 years | 97 (44.1) | 66 (50.8) | 31 (34.4) | |
| Locality | ||||
| Zagazig | 90 (40.9) | 54 (41.5) | 36 (40.0) | |
| Belbis | 55 (25.0) | 34 (26.1) | 21 (23.3) | |
| Abo-Hammad | 40 (18.2) | 18 (13.9) | 22 (24.4) | |
| Menia ElKamh | 35 (15.9) | 24 (18.5) | 11 (12.3) | |
| Feeding | ||||
| Concentrates | 143 (65.0) | 83 (63.9) | 60 (66.7) | |
| Grazing | 77 (35.0) | 47 (36.2) | 30 (33.3) | |
| Season | ||||
| Autumn | 40 (18.2) | 22 (16.9) | 18 (20.0) | |
| Spring | 91 (41.4) | 55 (42.3) | 36 (40.0) | |
| Summer | 33 (15.0) | 18 (13.9) | 15 (16.7) | |
| Winter | 56 (25.4) | 35 (26.9) | 21 (23.3) | |
| Skin lesions | ||||
| Yes | 36 (16.4) | 19 (14.6) | 17 (18.9) | |
| No | 184 (83.6) | 111 (85.4) | 73 (81.1) | |
| Enlarged lymph nodes | ||||
| Yes | 54 (24.6) | 24 (18.5) | 30 (33.3) | |
| No | 166 (75.4) | 106 (81.5) | 60 (66.7) | |
| Total | 220 | 130 | 90 | |
| Isolate | Source | Antimicrobial Resistance Profiles 1 | MAR Index 2 | Virulence Genes | Resistance Genes |
|---|---|---|---|---|---|
| S1 | Sheep | PEN, NB, AMC, AM, OXA, VAN, CRO, CXM, CEP, BAC, AMP, DOX, CLI, NAL, STR, KAN, AMK, NEO, FFC, ERY, SXT | 0.88 | PLD, PIP, FagA, FagB, FagC, FagD | aph(3″)-Ib, aph(3′)-Ic, sul1, tet(W), bla, cat1, dfrA1, ermC, vanA, bcrA, qnrA |
| S2 | Sheep | PEN, NB, AMC, AM, OXA, VAN, CRO, CXM, BAC, AMP, DOX, CLI, NAL, STR, KAN, AMK, NEO, FFC, ERY, SXT | 0.83 | PLD, PIP, FagA, FagB, FagC, FagD | aph(3″)-Ib, aph(3′)-Ic, tet(W), bla, cat1, dfrA1, ermC, vanA, bcrA, qnrA |
| S3 | Sheep | PEN, NB, AMC, AM, OXA, BAC, DOX, NAL, STR, NEO, FFC, ERY, SXT | 0.5 | PLD, PIP, FagA, FagB, FagC, FagD | aph(3″)-Ib, tet(W), bla, cat1, dfrA1 |
| S4 | Sheep | PEN, NB, AMC, OXA, BAC, DOX, CLI, NAL, STR, KAN, NEO, FFC, ERY, SXT | 0.58 | PLD, PIP, FagA, FagB, FagC, FagD | aph(3″)-Ib, aph(3′)-Ic, tet(W), bla, cat1, dfrA1, ermC, bcrA, qnrA |
| S5 | Goat | PEN, NB, AMC, OXA, CEP, BAC, DOX, CLI, NAL, STR, KAN, NEO, FFC, ERY, SXT | 0.54 | PLD, PIP, FagA, FagB, FagC, FagD | aph(3″)-Ib, aph(3′)-Ic, tet(W), bla, cat1, dfrA1, ermC, bcrA, qnrA |
| S6 | Goat | PEN, NB, AMC, OXA, CEP, BAC, DOX, CLI, NAL, STR, KAN, NEO, FFC, ERY, SXT | 0.58 | PLD, PIP, FagA, FagB, FagC, FagD | ermX, aph(3″)-Ib, aph(3′)-Ic, sul1, tet(W), bla, cat1, ermC, bcrA, qnrA |
| S7 | Goat | PEN, NB, AMC, OXA, PIP, CEP, BAC, DOX, CLI, NAL, STR, KAN, FFC, ERY, SXT | 0.54 | PLD, PIP, FagA, FagB, FagC, FagD | sul1, tet(W), bla, cat1, qnrA |
| S8 | Sheep | PEN, NB, AMC, OXA, PIP, CRO, CXM, CEP, BAC, AMP, DOX, CLI, NAL, STR, KAN, FFC, ERY, SXT | 0.63 | PLD, PIP, FagA, FagB, FagC | aph(3″)-Ib, aph(3′)-Ic, sul1, tet(W), bla, cat1, ermC, bcrA, qnrA |
| S9 | Sheep | PEN, NB, AMC, OXA, PIP, CEP, BAC, AMP, DOX, CLI, NAL, STR, KAN, FFC, ERY, SXT | 0.63 | PLD, PIP, FagA, FagB, FagC, FagD | aph(3″)-Ib, aph(3′)-Ic, sul1, tet(W), bla, ermC, bcrA |
| S10 | Goat | PEN, AMC, OXA, PIP, CXM, CEP, BAC, AMP, DOX, CLI, FFC, ERY, SXT | 0.75 | PLD, PIP, FagA, FagB, FagC, FagD | ermX, aph(3′)-Ic, sul1, tet(W), bla, ermC, bcrA, qnrA |
| S11 | Sheep | PEN, NB, AMC, OXA, PIP, CXM, CEP, BAC, AMP, DOX, CLI, NAL, STR, KAN, NEO, FFC, ERY, SXT | 0.63 | PLD, PIP, FagA, FagB, FagC, FagD | ermX, sul1, bla, dfrA1, ermC, bcrA, qnrA |
| S12 | Goat | PEN, AMC, OXA, PIP, CEP, BAC, AMP, DOX, STR, KAN, NEO, FFC | 0.5 | PLD, PIP, FagA, FagB, FagC, FagD | sul1, bla, dfrA1 |
| S13 | Goat | PEN, NB, AMC, OXA, PIP, CRO, CXM, CEP, BAC, AMP, CLI, STR, KAN, AMK, NEO, FFC, RIF, ERY, SXT | 0.79 | PLD, PIP, FagA, FagB, FagC, FagD | ermX, aph(3″)-Ib, aph(3′)-Ic, bla, rpoB |
| S14 | Goat | PEN, NB, AMC, OXA, PIP, CRO, CXM, CEP, BAC, AMP, DOX, CLI, STR, KAN, AMK, NEO, FFC, RIF, ERY, SXT | 0.83 | PLD, PIP, FagA, FagB, FagC, FagD | ermX, aph(3″)-Ib, sul1, tet(W), bla, cat1, dfrA1, ermC, rpoB, bcrA |
| S15 | Sheep | PEN, NB, OXA, PIP, CRO, CXM, CEP, BAC, AMP, DOX, CLI, NAL, STR, KAN, AMK, FFC, RIF, ERY, SXT | 0.71 | PLD, PIP, FagA, FagB, FagC, FagD | ermX, aph(3″)-Ib, aph(3′)-Ic, tet(W), bla, cat1, dfrA1, ermC, rpoB, bcrA, qnrA |
| S16 | Sheep | PEN, NB, AMC, OXA, PIP, CRO, CXM, CEP, BAC, AMP, DOX, CLI, NAL, STR, KAN, AMK, FFC, ERY, SXT | 0.67 | PLD, PIP, FagA, FagB, FagC, FagD | ermX, aph(3″)-Ib, aph(3′)-Ic, tet(W), bla, cat1, dfrA1, ermC, bcrA, qnrA |
| S17 | Goat | PEN, NB, OXA, PIP, CRO, CXM, CEP, BAC, CLI, NAL, STR, KAN, AMK, NEO, FFC, ERY, SXT | 0.79 | PLD, PIP, FagA, FagB, FagC, FagD | ermX, sul1, bla, cat1, dfrA1, bcrA |
| S18 | Sheep | PEN, AM, OXA, PIP, CRO, CXM, CEP, BAC, STR, KAN, AMK, NEO, FFC, RIF, ERY, SXT | 0.54 | PLD, PIP, FagA, FagB, FagC, FagD | ermX, sul1, bla, cat1, dfrA1, bcrA |
| S19 | Goat | PEN, PIP, CXM, CEP, BAC, DOX, AMK, FFC, SXT | 0.79 | PLD, PIP, FagA, FagB, FagC, FagD | sul1, bla, cat1, dfrA1, rpoB |
| S20 | Sheep | PIP, CXM, CEP, BAC, DOX, STR, KAN, FFC, RIF, ERY, SXT | 0.75 | PLD, PIP, FagA, FagB | ermX, aph(3″)-Ib, aph(3′)-Ic, sul1, tet(W), bla, cat1, rpoB, bcrA |
| S21 | Sheep | PEN, AMC, CXM, CEP, BAC, AMP, DOX, STR, KAN, FFC, ERY, SXT | 0.5 | PLD, PIP, FagA, FagB | ermX, aph(3″)-Ib, sul1, bla, cat1 |
| S22 | Goat | PEN, PIP, CXM, CEP, BAC, DOX, STR, KAN, NEO, FFC, RIF, ERY, SXT | 0.71 | PLD, PIP, FagA, FagB | ermX, aph(3″)-Ib, aph(3′)-Ic, sul1, bla, cat1, rpoB, bcrA |
| S23 | Goat | NB, OXA, PIP, CXM, CEP, BAC, STR, KAN, NEO, FFC, RIF, ERY, SXT | 0.67 | PLD, PIP, FagA, FagB, FagC | ermX, aph(3″)-Ib, sul1, bla, cat1, dfrA1, bcrA |
| S24 | Goat | PEN, NB, PIP, CXM, CEP, BAC, AMP, DOX, CLI, NAL, STR, NEO, FFC, RIF, ERY, SXT | 0.38 | PLD, PIP, FagA, FagC | ermX, aph(3″)-Ib, sul1, tet(W), bla, dfrA1, ermC, rpoB, bcrA, qnrA |
| S25 | Goat | PEN, PIP, CXM, CEP, BAC, AMP, DOX, STR, KAN, NEO, FFC, ERY, SXT | 0.46 | PLD, PIP, FagA, FagB | ermX, aph(3″)-Ib, sul1, bla, dfrA1, bcrA |
| S26 | Goat | PEN, NB, OXA, PIP, CXM, CEP, BAC, AMP, DOX, STR, NEO, FFC, RIF, ERY | 0.5 | PLD, PIP, FagA, FagB, FagC | ermX, aph(3″)-Ib, bla, cat1, rpoB, bcrA |
| S27 | Goat | PEN, NB, OXA, PIP, CXM, CEP, BAC, AMP, DOX, NAL, NEO, FFC, ERY | 0.54 | PLD, PIP, FagA, FagC | ermX, bla, bcrA, qnrA |
| S28 | Sheep | PEN, NB, AMC, OXA, PIP, CXM, CEP, BAC, AMP, DOX, CLI, NAL, STR, KAN, NEO, FFC, ERY, SXT | 0.79 | PLD, PIP, FagA, FagB, FagC, FagD | ermX, sul1, bla, dfrA1, ermC, bcrA, qnrA |
| S29 | Goat | PEN, AMC, OXA, PIP, CEP, BAC, AMP, DOX, STR, KAN, NEO, FFC | 0.54 | PLD, PIP, FagA, FagB, FagC, FagD | sul1, bla, dfrA1 |
| S30 | Goat | PEN, NB, AMC, OXA, PIP, CRO, CXM, CEP, BAC, AMP, CLI, STR, KAN, AMK, NEO, FFC, RIF, ERY, SXT | 0.67 | PLD, PIP, FagA, FagB, FagC, FagD | ermX, aph(3″)-Ib, aph(3′)-Ic, bla, rpoB |
| S31 | Goat | PEN, NB, AMC, OXA, PIP, CRO, CXM, CEP, BAC, AMP, DOX, CLI, STR, KAN, AMK, NEO, FFC, RIF, ERY, SXT | 0.54 | PLD, PIP, FagA, FagB, FagC, FagD | ermX, aph(3″)-Ib, sul1, tet(W), bla, cat1, dfrA1, ermC, rpoB, bcrA |
| S32 | Sheep | PEN, NB, OXA, PIP, CRO, CXM, CEP, BAC, AMP, DOX, CLI, NAL, STR, KAN, AMK, FFC, RIF, ERY, SXT | 0.83 | PLD, PIP, FagA, FagB, FagC, FagD | ermX, aph(3″)-Ib, aph(3′)-Ic, tet(W), bla, cat1, dfrA1, ermC, rpoB, bcrA, qnrA |
| S33 | Sheep | PEN, NB, AMC, OXA, PIP, CRO, CXM, CEP, BAC, AMP, DOX, CLI, NAL, STR, KAN, AMK, FFC, ERY, SXT | 0.79 | PLD, PIP, FagA, FagB, FagC, FagD | ermX, aph(3″)-Ib, aph(3′)-Ic, tet(W), bla, cat1, dfrA1, ermC, bcrA, qnrA |
| S34 | Goat | PEN, NB, OXA, PIP, CRO, CXM, CEP, BAC, CLI, NAL, STR, KAN, AMK, NEO, FFC, ERY, SXT | 0.58 | PLD, PIP, FagA, FagB, FagC, FagD | ermX, sul1, bla, cat1, dfrA1, bcrA |
| S35 | Sheep | PEN, AM, OXA, PIP, CRO, CXM, CEP, BAC, STR, KAN, AMK, NEO, FFC, RIF, ERY, SXT | 0.79 | PLD, PIP, FagA, FagB, FagC, FagD | ermX, sul1, bla, cat1, dfrA1, bcrA |
| S36 | Goat | PEN, PIP, CXM, CEP, BAC, DOX, AMK, FFC, SXT | 0.54 | PLD, PIP, FagA, FagB, FagC, FagD | sul1, bla, cat1, dfrA1, rpoB |
| S37 | Sheep | PIP, CXM, CEP, BAC, DOX, STR, KAN, FFC, RIF, ERY, SXT | 0.71 | PLD, PIP, FagA, FagB | ermX, aph(3″)-Ib, aph(3′)-Ic, sul1, tet(W), bla, cat1, rpoB, bcrA |
| S38 | Sheep | PEN, AMC, CXM, CEP, BAC, AMP, DOX, STR, KAN, FFC, ERY, SXT | 0.67 | PLD, PIP, FagA, FagB | ermX, aph(3″)-Ib, sul1, bla, cat1 |
| S39 | Goat | PEN, PIP, CXM, CEP, BAC, DOX, STR, KAN, NEO, FFC, RIF, ERY, SXT | 0.88 | PLD, PIP, FagA, FagB | ermX, aph(3″)-Ib, aph(3′)-Ic, sul1, bla, cat1, rpoB, bcrA |
| S40 | Goat | NB, OXA, PIP, CXM, CEP, BAC, STR, KAN, NEO, FFC, RIF, ERY, SXT | 0.83 | PLD, PIP, FagA, FagB, FagC | ermX, aph(3″)-Ib, sul1, bla, cat1, dfrA1, bcrA |
| S41 | Goat | PEN, NB, PIP, CXM, CEP, BAC, AMP, DOX, CLI, NAL, STR, NEO, FFC, RIF, ERY, SXT | 0.5 | PLD, PIP, FagA, FagC | ermX, aph(3″)-Ib, sul1, tet(W), bla, dfrA1, ermC, rpoB, bcrA, qnrA |
| S42 | Goat | PEN, PIP, CXM, CEP, BAC, AMP, DOX, STR, KAN, NEO, FFC, ERY, SXT | 0.58 | PLD, PIP, FagA, FagB | ermX, aph(3″)-Ib, sul1, bla, dfrA1, bcrA |
| S43 | Goat | PEN, NB, OXA, PIP, CXM, CEP, BAC, AMP, DOX, STR, NEO, FFC, RIF, ERY | 0.63 | PLD, PIP, FagA, FagB, FagC | ermX, aph(3″)-Ib, bla, cat1, rpoB, bcrA |
| S44 | Goat | PEN, NB, OXA, PIP, CXM, CEP, BAC, AMP, DOX, NAL, NEO, FFC, ERY | 0.63 | PLD, PIP, FagA, FagC | ermX, bla, bcrA, qnrA |
| S45 | Sheep | PEN, NB, AMC, AM, OXA, VAN, CRO, CXM, CEP, BAC, AMP, DOX, CLI, NAL, STR, KAN, AMK, NEO, FFC, ERY, SXT | 0.38 | PLD, PIP, FagA, FagB, FagC, FagD | aph(3″)-Ib, aph(3′)-Ic, sul1, tet(W), bla, cat1, dfrA1, ermC, bcrA, qnrA |
| S46 | Sheep | PEN, NB, AMC, AM, OXA, VAN, CRO, CXM, BAC, AMP, DOX, CLI, NAL, STR, KAN, AMK, NEO, FFC, ERY, SXT | 0.46 | PLD, PIP, FagA, FagB, FagC, FagD | aph(3″)-Ib, aph(3′)-Ic, tet(W), bla, cat1, dfrA1, ermC, bcrA, qnrA |
| S47 | Sheep | PEN, NB, AMC, AM, OXA, BAC, DOX, NAL, STR, NEO, FFC, ERY, SXT | 0.5 | PLD, PIP, FagA, FagB, FagC, FagD | aph(3″)-Ib, tet(W), bla, cat1, dfrA1 |
| S48 | Sheep | PEN, NB, AMC, OXA, BAC, DOX, CLI, NAL, STR, KAN, NEO, FFC, ERY, SXT | 0.54 | PLD, PIP, FagA, FagB, FagC, FagD | aph(3″)-Ib, aph(3′)-Ic, tet(W), bla, cat1, dfrA1, ermC, bcrA, qnrA |
| S49 | Goat | PEN, NB, AMC, OXA, CEP, BAC, DOX, CLI, NAL, STR, KAN, NEO, FFC, ERY, SXT | 0.63 | PLD, PIP, FagA, FagB, FagC, FagD | aph(3″)-Ib, aph(3′)-Ic, tet(W), bla, cat1, dfrA1, ermC, bcrA, qnrA |
| S50 | Goat | PEN, NB, AMC, OXA, CEP, BAC, DOX, CLI, NAL, STR, KAN, NEO, FFC, ERY, SXT | 0.71 | PLD, PIP, FagA, FagB, FagC, FagD | ermX, aph(3″)-Ib, aph(3′)-Ic, sul1, tet(W), bla, cat1, ermC, bcrA, qnrA |
| S51 | Goat | PEN, NB, AMC, OXA, PIP, CEP, BAC, DOX, CLI, NAL, STR, KAN, FFC, ERY, SXT | 0.05 | PLD, PIP, FagA, FagB, FagC, FagD | sul1, tet(W), bla, cat1, qnrA |
| S52 | Sheep | PEN, NB, AMC, OXA, PIP, CRO, CXM, CEP, BAC, AMP, DOX, CLI, NAL, STR, KAN, FFC, ERY, SXT | 0.54 | PLD, PIP, FagA, FagB, FagC | aph(3″)-Ib, aph(3′)-Ic, sul1, tet(W), bla, cat1, ermC, bcrA, qnrA |
| S53 | Sheep | PEN, NB, AMC, OXA, PIP, CEP, BAC, AMP, DOX, CLI, NAL, STR, KAN, FFC, ERY, SXT | 0.67 | PLD, PIP, FagA, FagB, FagC, FagD | aph(3″)-Ib, aph(3′)-Ic, sul1, tet(W), bla, ermC, bcrA |
| S54 | Goat | PEN, AMC, OXA, PIP, CXM, CEP, BAC, AMP, DOX, CLI, FFC, ERY, SXT | 0.54 | PLD, PIP, FagA, FagB, FagC, FagD | ermX, aph(3′)-Ic, sul1, tet(W), bla, ermC, bcrA, qnrA |
| Rank 1 | Class | Agent 2 | No. of Resistant C. pseudotuberculosis Isolates (%) | ||
|---|---|---|---|---|---|
| n = 54 | Sheep (n = 24) | Goats (n = 30) | |||
| I | Aminoglycosides | AMK | 18 (33.3) | 10 (41.7) | 8 (26.7) |
| KAN | 42 (77.8) | 22 (91.7) | 20 (66.7) | ||
| NEO | 36 (66.7) | 12 (50.0) | 24 (80.0) | ||
| STR | 48 (88.9) | 24 (100) | 24 (80.0) | ||
| I | Cephalosporins | CRO | 18 (33.3) | 12 (50.0) | 6 (20.0) |
| CXM | 40 (74.1) | 18 (75.0) | 22 (73.3) | ||
| CEP | 48 (88.9) | 18 (75.0) | 30 (100) | ||
| I | Macrolides | ERY | 50 (92.6) | 24 (100) | 26 (86.7) |
| I | Quinolones | NAL | 30 (55.6) | 18 (75.0) | 12 (40.0) |
| NOR | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||
| II | Aminocoumarins | NB | 38 (70.4) | 18 (75.0) | 20 (66.7) |
| II | Glycopeptides | VAN | 4 (7.4) | 4 (16.7) | 0 (0.0) |
| Lincosamides | CLI | 32 (59.3) | 16 (66.7) | 16 (53.3) | |
| II | Penicillins | PEN | 50 (92.6) | 22 (91.7) | 28 (93.3) |
| AMC | 32 (59.3) | 18 (75.0) | 14 (46.7) | ||
| OXA | 42 (77.8) | 20 (83.3) | 22 (73.3) | ||
| SAM | 8 (14.8) | 8 (33.3) | 0 (0.0) | ||
| AMP | 32 (59.3) | 16 (66.7) | 16 (53.3) | ||
| PIP | 40 (74.1) | 14 (58.3) | 26 (86.7) | ||
| II | Sulfonamides | SXT | 48 (88.9) | 24 (100) | 24 (80.0) |
| II | Tetracyclines | DOX | 46 (85.2) | 22 (91.7) | 24 (80.0) |
| Amphenicols | FFC | 54 (100) | 24 (100) | 30 (100) | |
| Bacitracin | BAC | 54 (100) | 24 (100) | 30 (100) | |
| Rifampin | RIF | 18 (33.3) | 6 (25.0) | 12 (40.0) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
El Damaty, H.M.; El-Demerdash, A.S.; Abd El-Aziz, N.K.; Yousef, S.G.; Hefny, A.A.; Abo Remela, E.M.; Shaker, A.; Elsohaby, I. Molecular Characterization and Antimicrobial Susceptibilities of Corynebacterium pseudotuberculosis Isolated from Caseous Lymphadenitis of Smallholder Sheep and Goats. Animals 2023, 13, 2337. https://doi.org/10.3390/ani13142337
El Damaty HM, El-Demerdash AS, Abd El-Aziz NK, Yousef SG, Hefny AA, Abo Remela EM, Shaker A, Elsohaby I. Molecular Characterization and Antimicrobial Susceptibilities of Corynebacterium pseudotuberculosis Isolated from Caseous Lymphadenitis of Smallholder Sheep and Goats. Animals. 2023; 13(14):2337. https://doi.org/10.3390/ani13142337
Chicago/Turabian StyleEl Damaty, Hend M., Azza S. El-Demerdash, Norhan K. Abd El-Aziz, Sarah G. Yousef, Ahmed A. Hefny, Etab M. Abo Remela, Asmaa Shaker, and Ibrahim Elsohaby. 2023. "Molecular Characterization and Antimicrobial Susceptibilities of Corynebacterium pseudotuberculosis Isolated from Caseous Lymphadenitis of Smallholder Sheep and Goats" Animals 13, no. 14: 2337. https://doi.org/10.3390/ani13142337
APA StyleEl Damaty, H. M., El-Demerdash, A. S., Abd El-Aziz, N. K., Yousef, S. G., Hefny, A. A., Abo Remela, E. M., Shaker, A., & Elsohaby, I. (2023). Molecular Characterization and Antimicrobial Susceptibilities of Corynebacterium pseudotuberculosis Isolated from Caseous Lymphadenitis of Smallholder Sheep and Goats. Animals, 13(14), 2337. https://doi.org/10.3390/ani13142337







