Lipids in Equine Airway Inflammation: An Overview of Current Knowledge
Abstract
:Simple Summary
Abstract
1. Introduction
2. Lipids in the Equine Organ System
3. Structure and Major Cellular Functions of Main Lipid Classes
4. Lipids in Inflammation
5. Lipidome Studies in Equine Health and Disease
6. Lipids in Respiratory Diseases
6.1. Sphingolipid (SM, Cer, and HexCer) Species
6.2. Phosphatidylinositol (PI) Species
6.3. Phosphatidylcholine (PC) Species and Surfactant
7. Extracellular Vesicle Lipidome in Human and Equine Asthma
8. Modulating the Airways’ Inflammatory Reactions from a Lipidomics Perspective: Role of Diet and FA Supplements
9. Conclusions and Future Directions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Brown, H.A.; Murphy, R.C. Working towards an exegesis for lipids in biology. Nat. Chem. Biol. 2009, 5, 602–606. [Google Scholar] [CrossRef] [PubMed]
- Harayama, T.; Riezman, H. Organism lipid diversity: Understanding the diversity of membrane lipid composition. Nat. Rev. Mol. Cell Biol. 2018, 19, 281–296. [Google Scholar] [CrossRef] [PubMed]
- Hewitt, S.C.; Harrell, J.C.; Korach, K.S. Lessons in estrogen biology from knockout and transgenic animals. Annu. Rev. Physiol. 2005, 67, 285–308. [Google Scholar] [CrossRef] [PubMed]
- Swinnen, J.; Dehairs, J. A beginner’s guide to lipidomics. Biochem. Soc. Trans. 2022, 44, 20–24. [Google Scholar] [CrossRef]
- Han, X. Lipidomics for studying metabolism. Nat. Rev. Endocrinol. 2016, 12, 668–679. [Google Scholar] [CrossRef] [PubMed]
- Dennis, E.A. Lipidomics joins the omics evolution. Proc. Natl. Acad. Sci. USA 2009, 106, 2089–2090. [Google Scholar] [CrossRef]
- Anderson, J. Science-in-brief: Proteomics and metabolomics in equine veterinary science. Equine Vet. J. 2022, 54, 449–452. [Google Scholar] [CrossRef]
- Calder, P. n−3 Polyunsaturated fatty acids, inflammation, and inflammatory diseases. Am. J. Clin. Nutr. 2006, 83, 1505S–1519S. [Google Scholar] [CrossRef]
- Ghidoni, R.; Caretti, A.; Signorelli, P. Role of Sphingolipids in the Pathobiology of Lung Inflammation. Mediators Inflamm. 2015, 2015, 487508. [Google Scholar] [CrossRef]
- Hough, K.; Wilson, L.; Trevor, J.; Strenkowski, J.; Maina, N.; Kim, Y.; Spell, M.L.; Wang, Y.; Chanda, D.; Dager, J.R.; et al. Unique lipid signatures of extracellular vesicles from the airways of asthmatics. Sci. Rep. 2018, 81, 10340. [Google Scholar] [CrossRef]
- Christmann, U.; Hite, R.; Witonsky, S.; Buechner-Maxwell, V.; Wood, P. Evaluation of lipid markers in surfactant obtained from asthmatic horses exposed to hay. Am. J. Vet. Res. 2019, 803, 300–305. [Google Scholar] [CrossRef] [PubMed]
- Albornoz, A.; Alarcon, P.; Morales, N.; Uberti, B.; Henriquez, C.; Manosalva, C.; Burgos, R.A.; Moran, G. Metabolomics analysis of bronchoalveolar lavage fluid samples in horses with naturally-occurring asthma and experimentally-induced airway inflammation. Res. Vet. Sci. 2020, 133, 276–282. [Google Scholar] [CrossRef] [PubMed]
- Bazzano, M.; Laghi, L.; Zhu, C.; Magi, G.; Tesei, B.; Laus, F. Respiratory metabolites in bronchoalveolar lavage fluid (BALF) and exhaled breath condensate (EBC) can differentiate horses affected by severe equine asthma from healthy horses. BMC Vet. Res. 2020, 161, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Basil, M.; Levy, B. Specialized pro-resolving mediators: Endogenous regulators of infection and inflammation. Nat. Rev. Immunol. 2016, 16, 51–67. [Google Scholar] [CrossRef] [PubMed]
- Leuti, A.; Fazio, D.; Fava, M.; Piccoli, A.; Oddi, S.; Maccarrone, M. Bioactive lipids, inflammation and chronic diseases. Adv. Drug Deliv. Rev. 2020, 159, 133–169. [Google Scholar] [CrossRef] [PubMed]
- Zehethofer, N.; Bermbach, S.; Hagner, S.; Garn, H.; Müller, J.; Goldmann, T.; Lindner, B.; Schwudke, D.; König, P. Lipid analysis of airway epithelial cells for studying respiratory diseases. Chromatographia 2015, 78, 403–413. [Google Scholar] [CrossRef] [PubMed]
- To, K.K.; Lee, K.C.; Wong, S.S.; Sze, K.H.; Ke, Y.H.; Lui, Y.M.; Tang, B.S.; Li, I.W.; Lau, S.K.; Hung, I.F.; et al. Lipid metabolites as potential diagnostic and prognostic biomarkers for acute community acquired pneumonia. Diagn. Microbiol. Infect. Dis. 2016, 85, 249–254. [Google Scholar] [CrossRef] [PubMed]
- Seidl, E.; Kiermeier, H.; Liebisch, G.; Ballmann, M.; Hesse, S.; Paul-Buck, K.; Ratjen, F.; Rietschel, E.; Griese, M. Lavage lipidomics signatures in children with cystic fibrosis and protracted bacterial bronchitis. J. Cyst. Fibros 2019, 18, 790–795. [Google Scholar] [CrossRef] [PubMed]
- Kirkwood, K.I.; Christopher, M.W.; Burgess, J.L.; Littau, S.R.; Foster, K.; Richey, K.; Pratt, B.S.; Shulman, N.; Tamura, K.; MacCoss, M.J.; et al. Development and Application of Multidimensional Lipid Libraries to Investigate Lipidomic Dysregulation Related to Smoke Inhalation Injury Severity. J. Proteome Res. 2021, 21, 232–242. [Google Scholar] [CrossRef]
- Schwarz, B.; Sharma, L.; Roberts, L.; Peng, X.; Bermejo, S.; Leighton, I.; Casanovas-Massana, A.; Minasyan, M.; Farhadian, S.; Ko, A.I.; et al. Cutting edge: Severe SARS-CoV-2 infection in humans is defined by a shift in the serum lipidome, resulting in dysregulation of eicosanoid immune mediators. J. Immunol. 2021, 206, 329–334. [Google Scholar] [CrossRef]
- Sim, S.; Choi, Y.; Park, H. Potential metabolic biomarkers in adult asthmatics. Metabolites 2021, 11, 430. [Google Scholar] [CrossRef]
- Christmann, U.; Page, A.E.; Horohov, D.W.; Adams, A.A.; Chapman, S.E.; Hancock, C.L.; Emery, A.L.; Poovey, J.R.; Hagg, C.; Morales, S.M.O.; et al. Lipidomic analysis of surfactant and plasma from horses with asthma and age-matched healthy horses. Am. J. Vet. Res. 2022, 83, 1–9. [Google Scholar] [CrossRef]
- Mönki, J.; Holopainen, M.; Ruhanen, H.; Karikoski, N.; Käkelä, R.; Mykkänen, A. Lipid species profiling of bronchoalveolar lavage fluid cells of horses housed on two different bedding materials. Sci. Rep. 2023, 13, 21778. [Google Scholar] [CrossRef] [PubMed]
- Höglund, N.; Nieminen, P.; Mustonen, A.M.; Käkelä, R.; Tollis, S.; Koho, N.; Holopainen, M.; Ruhanen, H.; Mykkänen, A. Fatty acid fingerprints in bronchoalveolar lavage fluid and its extracellular vesicles reflect equine asthma severity. Sci. Rep. 2023, 13, 9821. [Google Scholar] [CrossRef] [PubMed]
- Santos, A.S.; Rodrigues, M.A.M.; Bessa, R.J.B.; Ferreira, L.M.; Martin-Rosset, W. Understanding the equine cecum-colon ecosystem: Current knowledge and future perspectives. Animal 2011, 5, 48–56. [Google Scholar] [CrossRef] [PubMed]
- Warren, L.; Vineyard, K. Fat and fatty acids. In Equine Applied and Clinical Nutrition, 1st ed.; Geor, R.J., Harris, P.A., Coenen, M., Eds.; W.B. Saunders: Philadelphia, PA, USA, 2013; pp. 136–155. [Google Scholar]
- Harris, P.; Geor, R. Nutrition for the equine athlete: Nutrient requirements and key principles in ration design. In Equine Sports Medicine and Surgery, 2nd ed.; Hinchcliff, K.W., Kaneps, A.J., Geor, R.J., Eds.; W.B. Saunders: Philadelphia, PA, USA, 2014; pp. 797–817. [Google Scholar]
- Mueller, E. Understanding the variegation of fat: Novel regulators of adipocyte differentiation and fat tissue biology. Bioch. Biophys. Acta -Mol. Basis Dis. 2014, 1842, 352–357. [Google Scholar] [CrossRef] [PubMed]
- Radin, M.J.; Sharkey, L.C.; Holycross, B.J. Adipokines: A review of biological and analytical principles and an update in dogs, cats, and horses. Vet. Clin. Pathol. 2009, 38, 136–156. [Google Scholar] [CrossRef] [PubMed]
- Vick, M.M.; Adams, A.A.; Murphy, B.A.; Sessions, D.R.; Horohov, D.W.; Cook, R.F.; Shelton, B.J.; Fitzgerald, B.P. Relationships among inflammatory cytokines, obesity, and insulin sensitivity in the horse. J. Anim. Sci. 2007, 85, 1144–1155. [Google Scholar] [CrossRef] [PubMed]
- Giralt, M.; Cereijo, R.; Villarroya, F. Adipokines and the endocrine role of adipose tissues. In Handbook of Experimental Pharmacology: Metabolic Control, 1st ed.; Herzig, S., Ed.; Springer: Cham, Swizerland, 2015; pp. 265–282. [Google Scholar]
- Carlberg, C.; Ulven, S.M.; Molnár, F. Obesity. In Nutrigenomics; Springer: Cham, Swizerland, 2016. [Google Scholar]
- Ertelt, A.; Barton, A.K.; Schmitz, R.R.; Gehlen, H. Metabolic syndrome: Is equine disease comparable to what we know in humans? Endocr. Connect. 2014, 3, R81–R93. [Google Scholar] [CrossRef] [PubMed]
- Lipid Metabolites and Pathways Strategy (LIPID MAPS) Consortium. Available online: https://www.lipidmaps.org/ (accessed on 1 January 2024).
- Cockcroft, S. Mammalian lipids: Structure, synthesis and function. Essays Biochem. 2021, 65, 813–845. [Google Scholar] [CrossRef]
- Clayden, J.; Warren, S.; Greeves, N. Organic structures. In Organic Chemistry, 2nd ed.; OUP: Oxford, UK, 2012; pp. 16–33. [Google Scholar]
- Baccouch, R.; Shi, Y.; Vernay, E.; Mathelié-Guinlet, M.; Taib-Maamar, N.; Villette, S.; Feuillie, C.; Rascol, E.; Nuss, P.; Lecomte, S.; et al. The impact of lipid polyunsaturation on the physical and mechanical properties of lipid membranes. Biochim. Biophys. Acta Biomembr. 2022, 1865, 184084. [Google Scholar] [CrossRef] [PubMed]
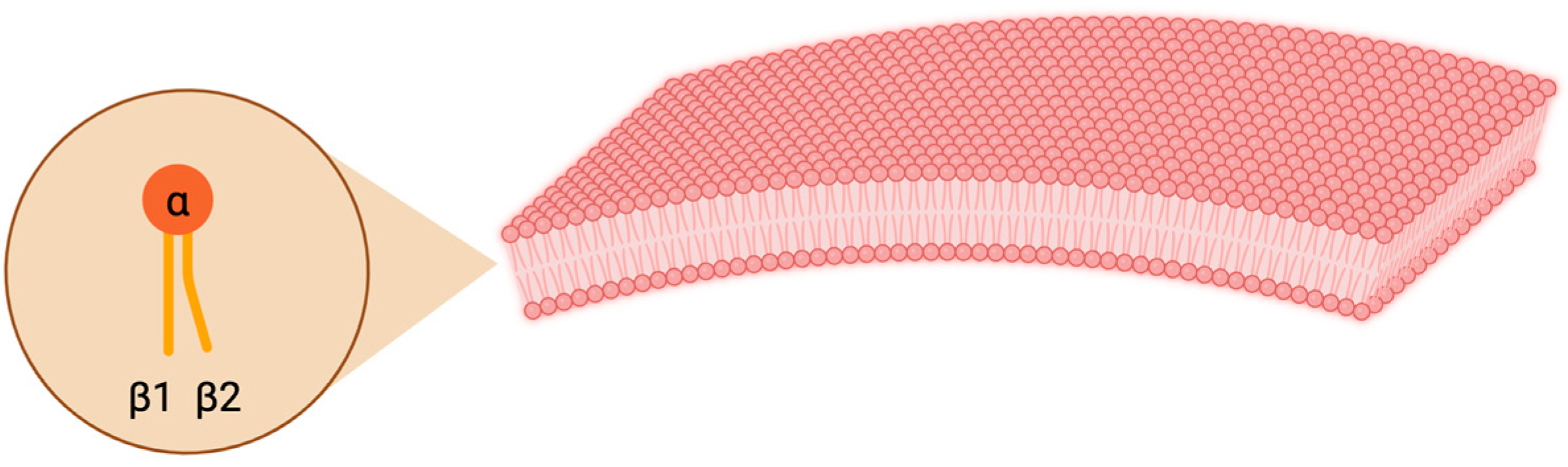
- Pollard, T.; Earnshaw, W.; Lippincott-Schwartz, J. Membrane structure and dynamics. In Cell Biology, 4th ed.; Elsevier: Amsterdam, The Netherlands, 2023; pp. 237–250. [Google Scholar]
- Vance, J.E. Phospholipid synthesis and transport in mammalian cells. Traffic 2015, 16, 1–18. [Google Scholar] [CrossRef]
- Gil-de-Gómez, L.; Monge, P.; Rodríguez, J.P.; Astudillo, A.M.; Balboa, M.A.; Balsinde, J. Phospholipid arachidonic acid remodeling during phagocytosis in mouse peritoneal macrophages. Biomedicines 2020, 8, 274. [Google Scholar] [CrossRef] [PubMed]
- Agassandian, M.; Mallampalli, R.K. Surfactant phospholipid metabolism. Biochim. Biophys. Acta Mol. Cell Biol. Lipids 2013, 1831, 612–625. [Google Scholar] [CrossRef] [PubMed]
- Mishra, S.; Chakraborty, H. Phosphatidylethanolamine and cholesterol promote hemifusion formation: A tug of war between membrane interfacial order and intrinsic negative curvature of lipids. J. Phys. Chem. B 2023, 127, 7721–7729. [Google Scholar] [CrossRef] [PubMed]
- van Meer, G.; Voelker, D.R.; Feigenson, G.W. Membrane lipids: Where they are and how they behave. Nat. Rev. Mol. Cell Biol. 2008, 9, 112–124. [Google Scholar] [CrossRef] [PubMed]
- Vance, J.E.; Tasseva, G. Formation and function of phosphatidylserine and phosphatidylethanolamine in mammalian cells. Biochim. Biophys. Acta 2013, 1831, 543–554. [Google Scholar] [CrossRef] [PubMed]
- Numata, M.; Kandasamy, P.; Nagashima, Y.; Fickes, R.; Murphy, R.C.; Voelker, D.R. Phosphatidylinositol inhibits respiratory syncytial virus infection. J. Lipid Res. 2015, 56, 578–587. [Google Scholar] [CrossRef] [PubMed]
- Balla, T. Phosphoinositides: Tiny lipids with giant impact on cell regulation. Physiol. Rev. 2013, 93, 1019–1137. [Google Scholar] [CrossRef]
- Slotte, J.P. Biological functions of sphingomyelins. Prog. Lipid Res. 2013, 52, 424–437. [Google Scholar] [CrossRef]
- Ogiso, H.; Taniguchi, M.; Okazaki, T. Analysis of lipid-composition changes in plasma membrane microdomains. J. Lipid Res. 2015, 56, 1594–1605. [Google Scholar] [CrossRef] [PubMed]
- Hammerschmidt, P.; Brüning, J.C. Contribution of specific ceramides to obesity-associated metabolic diseases. Cell. Mol. Life Sci. 2022, 79, 395. [Google Scholar] [CrossRef]
- Kim, S.H.; Jung, H.W.; Kim, M.; Moon, J.Y.; Ban, G.Y.; Kim, S.J.; Yoo, H.J.; Park, H.S. Ceramide/sphingosine-1-phosphate imbalance is associated with distinct inflammatory phenotypes of uncontrolled asthma. Allergy 2020, 75, 1991–2004. [Google Scholar] [CrossRef]
- Quinville, B.M.; Deschenes, N.M.; Ryckman, A.E.; Walia, J.S. A comprehensive review: Sphingolipid metabolism and implications of disruption in sphingolipid homeostasis. Int. J. Mol. Sci. 2021, 22, 5793. [Google Scholar] [CrossRef] [PubMed]
- Duan, Y.; Gong, K.; Xu, S.; Zhang, F.; Meng, X.; Han, J. Regulation of cholesterol homeostasis in health and diseases: From mechanisms to targeted therapeutics. Signal Transduct. Target Ther. 2022, 7, 265. [Google Scholar] [CrossRef] [PubMed]
- Deng, L.; Kersten, S.; Stienstra, R. Triacylglycerol uptake and handling by macrophages: From fatty acids to lipoproteins. Prog. Lipid Res. 2023, 92, 101250. [Google Scholar] [CrossRef]
- Masoodi, M.; Kuda, O.; Rossmeisl, M.; Flachs, P.; Kopecky, J. Lipid signaling in adipose tissue: Connecting inflammation & metabolism. Biochim. Biophys. Acta Mol. Cell Biol. Lipids 2015, 1851, 503–518. [Google Scholar]
- Warren, L.; Kivipelto, J.; Gettinger, E. Evaluation of the capacity for maternal transfer and foal synthesis of long-chain polyunsaturated fatty acids. J. Anim. Sci. 2010, 88, 203. [Google Scholar]
- Nogradi, N. Omega-3 fatty acid supplementation in the management of chronic lower airway inflammatory conditions in horses. Open Access Theses 2013, 140. [Google Scholar]
- Bannenberg, G.; Serhan, C.N. Specialized pro-resolving lipid mediators in the inflammatory response: An update. Biochim. Biophys. Acta Mol. Cell Biol. Lipids 2010, 1801, 1260–1273. [Google Scholar] [CrossRef]
- Olave, C.; Ivester, K.; Couëtil, L.; Burgess, J.; Park, J.; Mukhopadhyay, A. Effects of low-dust forages on dust exposure, airway cytology, and plasma omega-3 concentrations in Thoroughbred racehorses: A randomized clinical trial. J. Vet. Inter. Med. 2022, 37, 338–348. [Google Scholar] [CrossRef] [PubMed]
- Serhan, C. Resolution phase of inflammation: Novel endogenous anti-inflammatory and proresolving lipid mediators and pathways. Annu. Rev. Immunol. 2007, 25, 101–137. [Google Scholar] [CrossRef] [PubMed]
- Chiurchiù, V.; Leuti, A.; Dalli, J.; Jacobsson, A.; Battistini, L.; Maccarrone, M.; Serhan, C.N. Proresolving lipid mediators resolvin D1, resolvin D2, and maresin 1 are critical in modulating T cell responses. Sci. Transl. Med. 2016, 8, 353ra111. [Google Scholar] [CrossRef] [PubMed]
- Kasuga, K.; Yang, R.; Porter, T.F.; Agrawal, N.; Petasis, N.A.; Irimia, D.; Toner, M.; Serhan, C.N. Rapid appearance of resolvin precursors in inflammatory exudates: Novel mechanisms in resolution. J. Immunol. 2008, 181, 8677–8687. [Google Scholar] [CrossRef] [PubMed]
- Miyata, J.; Arita, M. Role of omega-3 fatty acids and their metabolites in asthma and allergic diseases. Allergol. Int. 2015, 64, 27–34. [Google Scholar] [CrossRef] [PubMed]
- Barnig, C.; Frossard, N.; Levy, B. Towards targeting resolution pathways of airway inflammation in asthma. Pharmacol. Ther. 2018, 186, 98–113. [Google Scholar] [CrossRef] [PubMed]
- Folch, J.; Lees, M.; Stanley, G. A simple method for the isolation and purification of total lipides from animal tissues. J. Biol. Chem. 1957, 226, 497–509. [Google Scholar] [CrossRef] [PubMed]
- Wood, P.; Scoggin, K.; Ball, B.; Troedsson, M.; Squires, E. Lipidomics of equine sperm and seminal plasma: Identification of amphiphilic (O-acyl)-ω-hydroxy-fatty acids. Theriogenology 2016, 86, 1212–1221. [Google Scholar] [CrossRef] [PubMed]
- Wood, P.; Ball, B.; Scoggin, K.; Troedsson, M.; Squires, E. Lipidomics of equine amniotic fluid: Identification of amphiphilic (O-acyl)-ω-hydroxy-fatty acids. Theriogenology 2018, 105, 120–125. [Google Scholar] [CrossRef]
- Barreto, Í.M.; Urbano, S.A.; Oliveira, C.A.; Macêdo, C.S.; Borba, L.H.; Chags, B.M.; Rangel, A.H. Chemical composition and lipid profile of mare colostrum and milk of the quarter horse breed. PLoS ONE 2020, 15, e0238921. [Google Scholar] [CrossRef]
- Yuan, M.; Breitkopf, S.; Asara, J. Serial-omics characterization of equine urine. PLoS ONE 2017, 12, e0186258. [Google Scholar] [CrossRef] [PubMed]
- Kosinska, M.; Eichner, G.; Schmitz, G.; Liebisch, G.; Steinmeyer, J. Comparative study on the lipidome of normal knee synovial fluid from humans and horses. PLoS ONE 2021, 16, e0250146. [Google Scholar] [CrossRef]
- Elzinga, S.; Wood, P.; Adams, A. Plasma lipidomic and inflammatory cytokine profiles of horses with equine metabolic syndrome. J. Equine Vet. Sci. 2016, 40, 49–55. [Google Scholar] [CrossRef]
- Coleman, M.; Whitfield-Cargile, C.; Madrigal, R.; Cohen, N. Comparison of the microbiome, metabolome, and lipidome of obese and non-obese horses. PLoS ONE 2019, 14, e0215918. [Google Scholar] [CrossRef] [PubMed]
- Wood, P.; Steinman, M.; Erol, E.; Carter, G.; Christmann, U.; Verma, A. Lipidomic analysis of immune activation in equine leptospirosis and Leptospira-vaccinated horses. PLoS ONE 2018, 13, e0193424. [Google Scholar] [CrossRef] [PubMed]
- Sanclemente, J.; Rivera-Velez, S.; Dasgupta, N.; Horohov, D.; Wood, P.; Sanz, M. Plasma lipidome of healthy and Rhodococcus equi-infected foals over time. Equine Vet. J. 2022, 54, 121–131. [Google Scholar] [CrossRef] [PubMed]
- Hallamaa, R.; Batchu, K. Phospholipid analysis in sera of horses with allergic dermatitis and in matched healthy controls. Lipids Health Dis. 2016, 15, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Schauberger, E.; Peinhaupt, M.; Cazares, T.; Lindsley, A. Lipid Mediators of Allergic Disease: Pathways, Treatments, and Emerging Therapeutic Targets. Curr. Allergy Asthma Rep. 2016, 16, 48. [Google Scholar] [CrossRef] [PubMed]
- Yan, F.; Wen, Z.; Wang, R.; Luo, W.; Du, Y.; Wang, W.; Chen, X. Identification of the lipid biomarkers from plasma in idiopathic pulmonary fibrosis by Lipidomics. BMC Pulm. Med. 2017, 17, 1–12. [Google Scholar] [CrossRef]
- Snider, J.M.; You, J.K.; Wang, X.; Snider, A.J.; Hallmark, B.; Zec, M.M.; Seeds, M.C.; Sergeant, S.; Johnstone, L.; Wang, Q.; et al. Group IIA secreted phospholipase A 2 is associated with the pathobiology leading to COVID-19 mortality. J. Clin. Investig. 2021, 131, e149236. [Google Scholar] [CrossRef]
- Bullone, M.; Lavoie, J.-P. Asthma “of horses and men”—How can equine heaves help us better understand human asthma immunopathology and its functional consequences? Mol. Immunol. 2015, 66, 97–105. [Google Scholar] [CrossRef] [PubMed]
- Uhlig, S.; Gulbins, E. Sphingolipids in the lungs. Am. J. Respir. Crit. Care Med. 2008, 178, 1100–1114. [Google Scholar] [CrossRef] [PubMed]
- Kowal, K.; Zebrowska, E.; Chabowski, A. Altered sphingolipid metabolism is associated with asthma phenotype in house dust mite-allergic patients. Allergy Asthma Immunol. Res. 2019, 11, 330–342. [Google Scholar] [CrossRef] [PubMed]
- Pond, C.M. An evolutionary and functional view of mammalian adipose tissue. Proc. Nutr. Soc. 1992, 51, 367–377. [Google Scholar] [CrossRef] [PubMed]
- Jiang, T.; Dai, L.; Li, P.; Zhao, J.; Wang, X.; An, L.; Liu, M.; Wu, S.; Wang, Y.; Peng, Y.; et al. Lipid metabolism and identification of biomarkers in asthma by lipidomic analysis. Biochim. Biophys. Acta Mol. Cell Biol. Lipids 2021, 1866, 158853. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Tang, K.; Lu, Y.; Tian, Z.; Huang, Z.; Wang, M.; Zhao, J.; Xie, J. Revealing the role of glycerophospholipid metabolism in asthma through plasma lipidomics. Clin. Chim. Acta 2021, 513, 34–42. [Google Scholar] [CrossRef] [PubMed]
- Kang, Y.P.; Lee, W.J.; Hong, J.Y.; Lee, S.B.; Park, J.H.; Kim, D.; Park, S.; Park, C.S.; Park, S.W.; Kwon, S.W. Novel approach for analysis of bronchoalveolar lavage fluid (BALF) using HPLC-QTOF-MS-based lipidomics: Lipid levels in asthmatics and corticosteroid-treated asthmatic patients. J. Proteome Res. 2014, 13, 3919–3929. [Google Scholar] [CrossRef] [PubMed]
- Berry, K.; Murphy, R.; Kosmide, B.; Mason, R. Lipidomic characterization and localization of phospholipids in the human lung [S]. J. Lipid Res. 2017, 58, 926–933. [Google Scholar] [CrossRef] [PubMed]
- Brandsma, J.; Goss, V.M.; Yang, X.; Bakke, P.S.; Caruso, M.; Chanez, P.; Dahlén, S.E.; Fowler, S.J.; Horvath, I.; Krug, N.; et al. Lipid phenotyping of lung epithelial lining fluid in healthy human volunteers. Metabolomics 2018, 14, 1–12. [Google Scholar] [CrossRef]
- Sanak, M.; Mastalerz, L.; Gielicz, A.; Sokolowska, B.; Celejewska-Wόjcik, N.; Szczeklik, A. Targeted eicosanoid lipidomics of induced sputum as compared to exhaled breath condensate in asthmatics. Eur. Respir. J. 2011, 38, 4789. [Google Scholar]
- Christmann, U.; Hancock, C.L.; Poole, C.M.; Emery, A.L.; Poovey, J.R.; Hagg, C.; Mattson, E.A.; Scarborough, J.J.; Christopher, J.S.; Dixon, A.T.; et al. Dynamics of DHA and EPA supplementation: Incorporation into equine plasma, synovial fluid, and surfactant glycerophosphocholines. Metabolomics 2021, 17, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Lam, M.; Bourke, J. Solving the riddle: Targeting the imbalance of sphingolipids in asthma to oppose airway hyper-responsiveness. Am. J. Respir. Cell Mol. Biol. 2020, 63, 555–557. [Google Scholar] [CrossRef] [PubMed]
- Horbay, R.; Hamraghani, A.; Ermini, L.; Holcik, S.; Beug, S.T.; Yeganeh, B. Role of ceramides and lysosomes in extracellular vesicle biogenesis, cargo sorting and release. Int. J. Mol. Sci. 2022, 23, 15317. [Google Scholar] [CrossRef] [PubMed]
- Masini, E.; Giannini, L.; Nistri, S.; Cinci, L.; Mastroianni, R.; Xu, W.; Comhair, S.A.; Li, D.; Cuzzocrea, S.; Matuschak, G.M.; et al. Ceramide: A key signaling molecule in a Guinea pig model of allergic asthmatic response and airway inflammation. J. Pharmacol. Exp. Ther. 2008, 324, 548–557. [Google Scholar] [CrossRef] [PubMed]
- Christmann, U.; Livesey, L.; Taintor, J.; Waldridge, B.; Schumacher, J.; Grier, B.; Hite, R.D. Lung surfactant function and composition in neonatal foals and adult horses. J. Vet. Intern. Med. 2006, 20, 1402–1407. [Google Scholar] [CrossRef] [PubMed]
- Howlett, A.; Ohlsson, A.; Plakkal, N. Inositol in preterm infants at risk for or having respiratory distress syndrome. Cochrane Database Syst. Rev. 2019, 2019, CD000366. [Google Scholar] [CrossRef] [PubMed]
- Murphy, R.C.; Folco, G. Lysophospholipid acyltransferases and leukotriene biosynthesis: Intersection of the Lands cycle and the arachidonate PI cycle. J. Lipid Res. 2019, 60, 219–226. [Google Scholar] [CrossRef]
- Astudillo, A.; Pérez-Chacón, G.; Meana, C.; Balgoma, D.; Pol, A.; Del Pozo, M.; Balboa, M.A.; Balsinde, J. Altered arachidonate distribution in macrophages from caveolin-1 null mice leading to reduced eicosanoid synthesis. J. Biol. Chem. 2011, 286, 5299–5307. [Google Scholar] [CrossRef]
- Wenzel, S. The role of leukotrienes in asthma. Prostaglandins Leukot. Essent. Fatty Acids 2003, 69, 145–155. [Google Scholar] [CrossRef]
- Hallstrand, T.; Henderson, W., Jr. An update on the role of leukotrienes in asthma. Curr. Opin. Allergy Clin. Immunol. 2010, 10, 60–66. [Google Scholar] [CrossRef]
- Bernhard, W.; Hoffmann, S.; Dombrowsky, H.; Rau, G.; Kamlage, A.; Kappler, M.; Haitsma, J.J.; Freihorst, J.; von der Hardt, H.; Poets, C.F. Phosphatidylcholine molecular species in lung surfactant: Composition in relation to respiratory rate and lung development. Am. J. Respir. Cell Mol. Biol. 2001, 25, 725–731. [Google Scholar] [CrossRef] [PubMed]
- Hohlfeld, J. The role of surfactant in asthma. Respir. Res. 2001, 3, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Christmann, U.; Buechner-Maxwell, V.; Witonsky, S.; Hite, R. Role of lung surfactant in respiratory disease: Current knowledge in large animal medicine. J. Vet. Intern. Med. 2009, 23, 227–242. [Google Scholar] [CrossRef]
- Forbes, A.; Pickell, M.; Foroughian, M.; Yao, L.J.; Lewis, J.; Veldhuizen, R. Alveolar macrophage depletion is associated with increased surfactant pool sizes in adult rats. J. Appl. Physiol. 2007, 103, 637–645. [Google Scholar] [CrossRef] [PubMed]
- Brandsma, J.; Postle, A.D. Analysis of the regulation of surfactant phosphatidylcholine metabolism using stable isotopes. Ann. Anat. 2017, 211, 176–183. [Google Scholar] [CrossRef] [PubMed]
- de Aguiar Vallim, T.; Lee, E.; Merriott, D.; Goulbourne, C.; Cheng, J.; Cheng, A.; Gonen, A.; Allen, R.M.; Palladino, E.N.; Ford, D.A.; et al. ACG1 regulates pulmonary surfactant metabolism in mice and men. J. Lipid Res. 2017, 58, 941–954. [Google Scholar] [CrossRef] [PubMed]
- Bartussio, A. Lung surfactant, asthma, and allergens: A story in evolution. Am. J. Respir. Crit. 2004, 169, 550–551. [Google Scholar] [CrossRef]
- Christmann, U. Relationship between surfactant alterations and severity of disease in horses with recurrent airway obstruction (RAO). Ph.D. Thesis, Virginia Tech, Blacksburg, VA, USA, 2008. [Google Scholar]
- Treede, I.; Braun, A.; Sparla, R.; Kühnel, M.; Giese, T.; Turner, J.; Anes, E.; Kulaksiz, H.; Fullekrug, J.; Stremmel, W.; et al. Anti-inflammatory effects of phosphatidylcholine. J. Biol. Chem. 2007, 282, 27155–27164. [Google Scholar] [CrossRef]
- Dewhurst, R.; Scollan, N.; Youell, S.; Tweed, J.; Humphreys, M. Influence of species, cutting date and cutting interval on the fatty acid composition of grasses. Grass Forage Sci. 2001, 56, 68–74. [Google Scholar] [CrossRef]
- Lorenzo, J.; Fuciños, C.; Purriños, L.; Franco, D. Intramuscular fatty acid composition of “Galician Mountain” foals breed: Effect of sex, slaughtered age and livestock production system. Meat. Sci. 2010, 86, 825–831. [Google Scholar] [CrossRef]
- Hansen, R.; Savage, C.; Reidlinger, K.; Traub-Dargatz, J.; Ogilvie, G.; Mitchell, D. Effects of dietary flaxseed oil supplementation on equine plasma fatty acid concentrations and whole blood platelet aggregation. J. Vet. Intern. Med. 2002, 16, 457–463. [Google Scholar] [CrossRef] [PubMed]
- Vineyard, K.; Warren, L.; Kivipelto, J. Effect of dietary omega-3 fatty acid source on plasma and red blood cell membrane composition and immune function in yearling horses. J. Anim. Sci. 2010, 88, 248–257. [Google Scholar] [CrossRef]
- Ross-Jones, T.; Hess, T.; Rexford, J.; Ahrens, N.; Engle, T.; Hansen, D. Effects of omega-3 long chain polyunsaturated fatty acid supplementation on equine synovial fluid fatty acid composition and prostaglandin E2. J. Equine Vet. Sci. 2014, 34, 779–783. [Google Scholar] [CrossRef]
- Pagan, J.; Hauss, A.; Pagan, E.; Simons, J.; Waldridge, B. Long-chain polyunsaturated fatty acid supplementation increases levels in red blood cells and reduces the prevalence and severity of squamous gastric ulcers in exercised Thoroughbreds. J. Am. Vet. Med. Assoc. 2022, 260, S121–S128. [Google Scholar] [CrossRef] [PubMed]
- Sembratowicz, I.; Zięba, G.; Cholewinska, E.; Czech, A. Effect of dietary flaxseed oil supplementation on the redox status, haematological and biochemical parameters of horses’ blood. Animals 2020, 10, 2244. [Google Scholar] [CrossRef]
- Gordon, M.; Jacobs, R. Feeding stalled horses a diet high omega-3 fatty acids results in a plasma fatty acid profile similar to horses on pasture. J. Equine Vet. Sci. 2021, 100, 103505. [Google Scholar] [CrossRef]
- Olave, C.; Ivester, K.; Couëtil, L.; Franco-Marmolejo, J.; Mukhopadhyay, A.; Robinson, J.; Park, J.H. Effects of forages, dust exposure and proresolving lipids on airway inflammation in horses. Am. J. Vet. Res. 2021, 83, 153–161. [Google Scholar] [CrossRef]
- Khol-Parisini, A.; van den Hoven, R.; Leinker, S.; Hulan, H.; Zentek, J. Effects of feeding sunflower oil or seal blubber oil to horses with recurrent airway obstruction. Can. J. Vet. Res. 2007, 71, 59. [Google Scholar]
- Nogradi, N.; Couëtil, L.; Messick, J.; Stochelski, M.; Burgess, J. Omega-3 fatty acid supplementation provides an additional benefit to a low-dust diet in the management of horses with chronic lower airway inflammatory disease. J. Vet. Intern. Med. 2015, 29, 299–306. [Google Scholar] [CrossRef]

| Lipid Class | Location and Main Functions |
|---|---|
| Phosphatidylcholine (PC) and phosphatidylethanolamine (PE) | Most abundant structural phospholipids of the membranes in mammalian cells [39]. Major storage for arachidonic acid (AA), among other signalling lipid mediators [40]. AA can be released from these lipids by the action of phospholipase A2 (PLA2) enzymes [40]. PC is also the main component of lung surfactant [41]. PC:PE ratio in the endoplasmic reticulum (ER) membranes is important; a reduction in PC:PE leads to loss of membrane integrity due to bilayer stress caused by the differences in the biophysical properties of PC and PE [42]. PE is most concentrated in the membranes of ER and mitochondria. PE is involved in membrane structure, curvature, and dynamics. It promotes membrane budding and vesicle fission and fusion [40]. |
| Phosphatidylserine (PS) | Membrane phospholipids in mammalian cells with multiple roles in cell signalling, endocytosis, platelet activation, blood coagulation, and apoptosis [43]. In healthy cells, PSs are confined to the inner bilayer of the plasma membrane, whereas apoptotic cells translocate PSs to the outer leaflet of the plasma membrane [35]. Exposure of PSs to the outer leaflet is a critical signal to macrophages to remove the damaged cells [44]. PSs activate kinases and many other membrane proteins and promote cell fusions of immunologically active cells [43]. |
| Phosphatidylinositol (PI) | Membrane phospholipids in mammalian cells with numerous roles in cell signalling [45]. PI’s major function is to act as a substrate for making phosphorylated derivatives and PLA2 [35]. PI’s headgroup is remarkably versatile: three of the five hydroxyls can be phosphorylated, resulting in seven different phosphoinositides [43], which, in turn, can recruit and activate cytosolic proteins. Many proteins contain lipid-binding domains that can recognize a specific phosphoinositide. PIs also form protein anchors in membranes [46]. |
| Sphingomyelin (SM) | Membrane phospholipids of mammalian cells; consist of a ceramide backbone bound to a phosphorylcholine molecule [35]. SMs are vital in viscous microdomain formation (so-called lipid rafts) in the cell membrane [47,48] and serve as precursors for sphingolipids in the sphingomyelin cycle [48]. |
| Ceramide (Cer) | Sphingolipids found in mammalian cell membranes in small but varying amounts. Cers are the precursors for SMs [35]. Despite their minimal presence, they are key mediators of apoptosis, autophagy, selective degradation of mitochondria, cell-cycle arrest, and natural aging [49]. Cers are involved in numerous pathological states of the body, such as inflammation [9,50]. Cell stressors, such as ionizing radiation and chemotherapeutic drugs, can trigger Cer accumulation [35]. |
| Hexosylceramide (HexCer) | Minor components of mammalian cell membranes; belong to the group of cerebrosides within the sphingolipids [35]. HexCers participate in forming microdomains (rafts) and influence membrane stability and function, especially in the nervous system [51]. Regulators of endothelial permeability, functioning, for example, in preventing trans-epidermal water loss [48]. |
| Cholesterol esters (CE) | Belong to the group of cholesterol lipids within the sterol lipids [35]. Storage lipids in cytosolic lipid droplets and circulating lipoprotein particles. CE content varies depending on nutritional and metabolic conditions [52]. CEs transport cholesterol in plasma and in cells in lipid droplets and buffer excess cholesterol [52]. |
| Triacylglyserol/triglyceride (TG) | Storage lipids in cytosolic lipid droplets found especially in adipocytes and in circulating lipoprotein particles [53]. TG acyl chains can produce membrane and signalling lipids [54]. TG content varies depending on the animal’s nutritional and metabolic status [53]. |
| Reference | Sample Type | Horses | The Main Findings Summarized |
|---|---|---|---|
| Wood et al. (2016) [65] | sperm, seminal plasma | 6 healthy stallions | Individual ether glycerophospholipids and seminolipids essential for membrane lipid raft function in equine sperm. Equine sperm contain OAHFAs. Potential roles of diacylglycerols as both important structural and signalling molecules in sperm are presented. |
| Wood et al. (2018) [66] | amniotic fluid | 6 pregnant mares | Detection of very-long-chain dicarboxylic acids, cholesterol sulphate, and OAHFAs in amniotic fluid of normal pregnancies in mares. |
| Barreto et al. (2020) [67] | colostrum | 34 lactating mares | Variation in the milk’s lipid composition according to the lactation stage. |
| Yuan et al. (2017) [68] | urine | 1 healthy mare | Five TGs, two phosphatidic acids, two PEs, are two phosphatidylethanols identified in mare’s urine. |
| Kosinska et al. (2021) [69] | synovial fluid | 15 humans, 13 horses | Horse synovial fluid contained about half of the PL content of human synovial fluid; changes in PL composition are characteristic for each species. |
| Elzinga et al. (2016) [70] | plasma | 14 cases, 9 controls | EMS horses had increased plasma TG, diacylglycerides, monoacylglycerides, and Cer. Plasma SM, sulfatide, and choline ether lipids were lower in EMS horses. |
| Coleman et al. (2019) [71] | serum | 20 cases, 20 controls | Lipid profile in obese horses closely resembled that of obese humans, humans with metabolic syndrome, or both. For example, CE, diacylglycerol (DAG), and PC classes were increased in obese horses. |
| Wood et al. (2018) [72] | serum | 15 unvaccinated, naturally infected; 15 vaccinated; 15 unvaccinated and unexposed | CPAs, diacylglycerols, and hydroperoxide oxidation products of choline plasmalogens are increased in the serum of naturally Leptospira-infected and Leptospira-vaccinated horses. TGs were only elevated in the serum of infected horses. SMs were increased only in the serum of vaccinated horses. |
| Sanclemente et al. (2022) [73] | plasma | 9 cases, 4 controls | Ageing and Rhodococcus equi-infection-induced changes in the plasma lipidome of foals. |
| Hallamaa and Batchu (2016) [74] | serum | 10 cases, 10 controls | IBH horses had lower total concentrations of PC and SM. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mönki, J.; Mykkänen, A. Lipids in Equine Airway Inflammation: An Overview of Current Knowledge. Animals 2024, 14, 1812. https://doi.org/10.3390/ani14121812
Mönki J, Mykkänen A. Lipids in Equine Airway Inflammation: An Overview of Current Knowledge. Animals. 2024; 14(12):1812. https://doi.org/10.3390/ani14121812
Chicago/Turabian StyleMönki, Jenni, and Anna Mykkänen. 2024. "Lipids in Equine Airway Inflammation: An Overview of Current Knowledge" Animals 14, no. 12: 1812. https://doi.org/10.3390/ani14121812





