Assessing the Effectiveness of Modified Tibial Plateau Leveling Osteotomy Plates for Treating Cranial Cruciate Ligament Rupture and Medial Patellar Luxation in Small-Breed Dogs
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
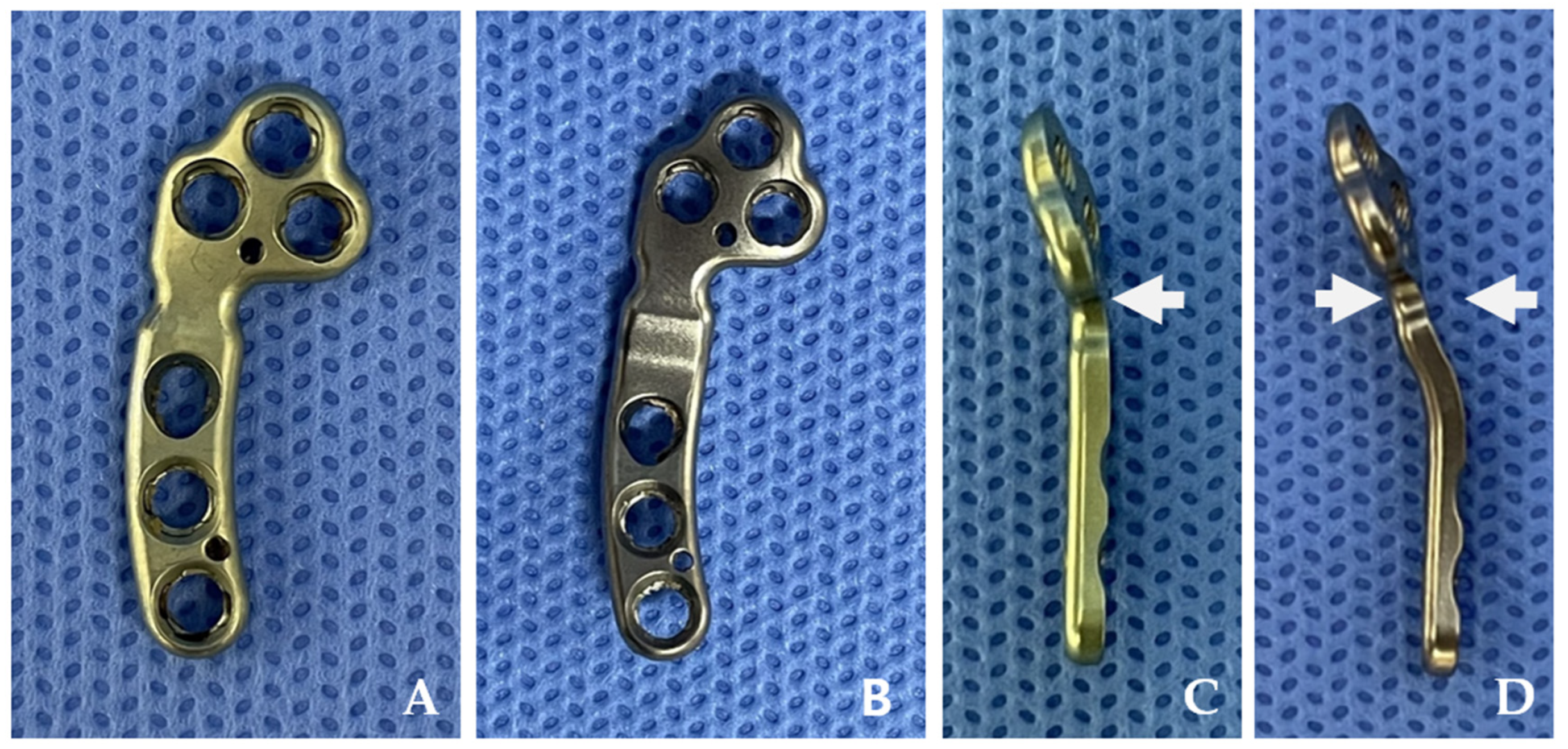
2.1. Plates
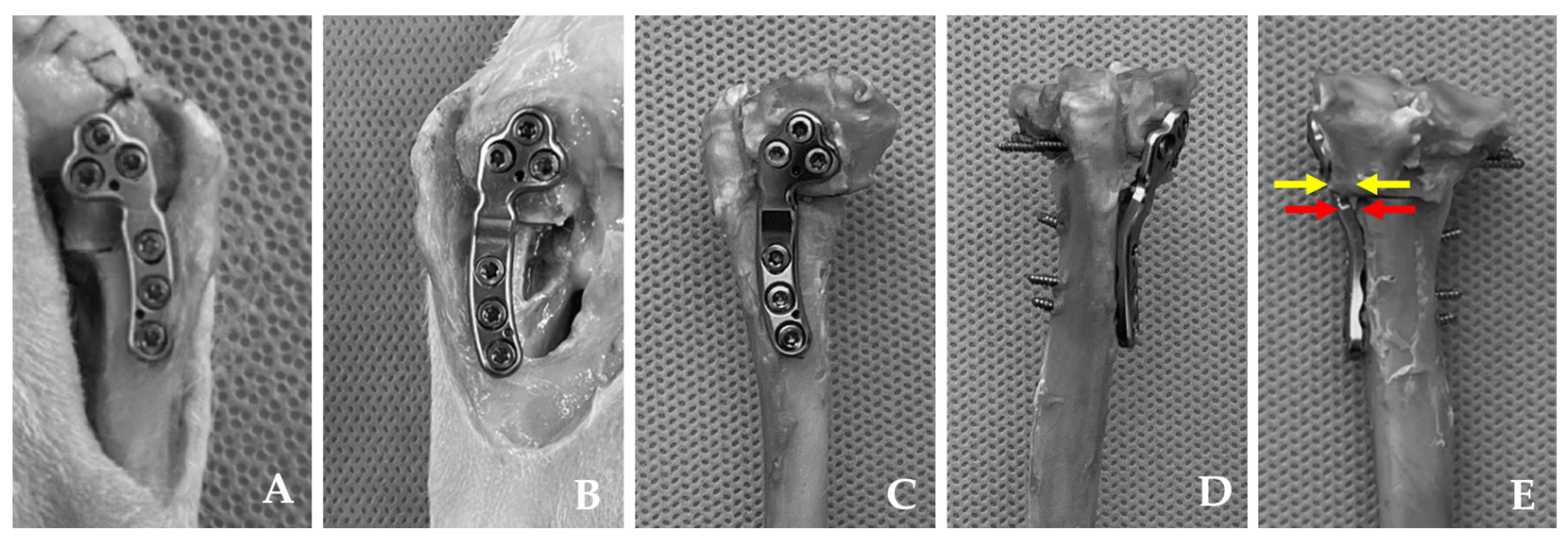
2.2. Specimens
2.3. Surgical Procedures
2.4. Postoperative Measurements
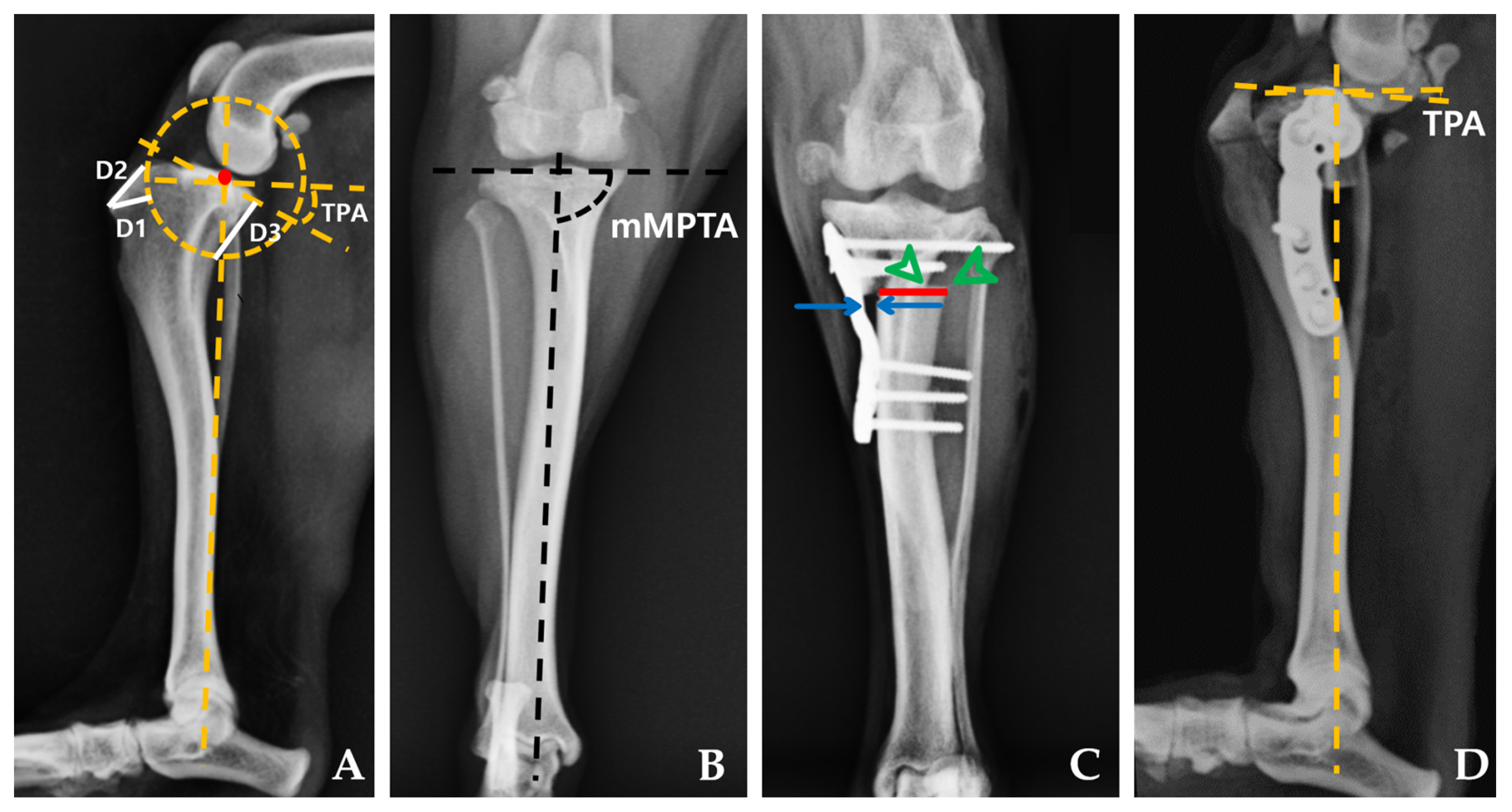
2.4.1. Radiographic Measurements
2.4.2. Compression Test
2.5. Statistical Analysis
3. Results
3.1. Specimens
3.2. Radiographic Measurements
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- LaFond, E.; Breur, G.J.; Austin, C.C. Breed susceptibility for developmental orthopedic diseases in dogs. J. Am. Anim. Hosp. Assoc. 2002, 38, 467–477. [Google Scholar] [CrossRef] [PubMed]
- Ness, M.; Abercromby, R.; May, C.; Turner, B.; Carmichael, S. A survey of orthopaedic conditions in small animal veterinary practice in Britain. Vet. Comp. Orthop. Traumatol. 1996, 9, 43–52. [Google Scholar] [CrossRef]
- Campbell, C.A.; Horstman, C.L.; Mason, D.R.; Evans, R.B. Severity of patellar luxation and frequency of concomitant cranial cruciate ligament rupture in dogs: 162 cases (2004–2007). J. Am. Vet. Med. Assoc. 2010, 236, 887–891. [Google Scholar] [CrossRef]
- Gibbons, S.; Macias, C.; Tonzing, M.; Pinchbeck, G.; McKee, W. Patellar luxation in 70 large breed dogs. J. Small Anim. Pract. 2006, 47, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Hayes, A.G.; Boudrieau, R.J.; Hungerford, L.L. Frequency and distribution of medial and lateral patellar luxation in dogs: 124 cases (1982–1992). J. Am. Vet. Med. Assoc. 1994, 205, 716–720. [Google Scholar] [CrossRef] [PubMed]
- Witsberger, T.H.; Villamil, J.A.; Schultz, L.G.; Hahn, A.W.; Cook, J.L. Prevalence of and risk factors for hip dysplasia and cranial cruciate ligament deficiency in dogs. J. Am. Vet. Med. Assoc. 2008, 232, 1818–1824. [Google Scholar] [CrossRef] [PubMed]
- Arthurs, G.; Langley-Hobbs, S. Patellar luxation as a complication of surgical intervention for the management of cranial cruciate ligament rupture in dogs. Vet. Comp. Orthop. Traumatol. 2007, 20, 204–210. [Google Scholar] [CrossRef] [PubMed]
- Kowaleski, M.P.; Boudrieau, R.J.; Pozzi, A. Stifle joint. In Veterinary Surgery: Small Animal, 2nd ed.; Tobias, K.M., Johnston, S.A., Eds.; Elsevier: St. Louis, MI, USA, 2012; Volume 1, pp. 1071–1168. [Google Scholar]
- Panichi, E.; Cappellari, F.; Burkhan, E.; Principato, G.; Currenti, M.; Tabbì, M.; Macrì, F. Patient-Specific 3D-Printed Osteotomy Guides and Titanium Plates for Distal Femoral Deformities in Dogs with Lateral Patellar Luxation. Animals 2024, 14, 951. [Google Scholar] [CrossRef] [PubMed]
- L’Eplattenier, H.; Montavon, P. Patellar luxation in dogs and cats: Pathogenesis and diagnosis. Compendium 2002, 24, 234–240. [Google Scholar]
- Vasseur, P.B. Stifle Joint. In Textbook of Small Animal Surgery, 3rd ed.; Slatter, D.H., Ed.; Elsevier Health Sciences: Amsterdam, The Netherlands, 2003; Volume 1, pp. 2090–2132. [Google Scholar]
- Langenbach, A.; Marcellin-Little, D.J. Management of concurrent patellar luxation and cranial cruciate ligament rupture using modified tibial plateau levelling. J. Small Anim. Pract. 2010, 51, 97–103. [Google Scholar] [CrossRef]
- DeCamp, C.E.; Johnston, S.A.; Déjardin, L.M.; Schaefer, S.L. Brinker, Piermattei and Flo’s Handbook of Small Animal Orthopedics and Fracture Repair, 5th ed.; Elsevier: St. Louis, MI, USA, 2015. [Google Scholar]
- Flesher, K.; Beale, B.S.; Hudson, C.C. Technique and outcome of a modified tibial plateau levelling osteotomy for treatment of concurrent medial patellar luxation and cranial cruciate ligament rupture in 76 stifles. Vet. Comp. Orthop. Traumatol. 2019, 32, 026–032. [Google Scholar] [CrossRef]
- Leonard, K.C.; Kowaleski, M.P.; Saunders, W.B.; McCarthy, R.J.; Boudrieau, R.J. Combined tibial plateau levelling osteotomy and tibial tuberosity transposition for treatment of cranial cruciate ligament insufficiency with concomitant medial patellar luxation. Vet. Comp. Orthop. Traumatol. 2016, 29, 536–540. [Google Scholar] [CrossRef] [PubMed]
- Lampart, M.; Knell, S.; Pozzi, A. A new approach to treatment selection in dogs with cruciate ligament rupture: Patient-specific treatment recommendations. Schweiz. Arch. Tierheilkd. 2020, 162, 345–363. [Google Scholar] [CrossRef] [PubMed]
- Slocum, B.; Slocum, T.D. Tibial plateau leveling osteotomy for repair of cranial cruciate ligament rupture in the canine. Vet. Clin. North. Am. Small Anim. Pract. 1993, 23, 777–795. [Google Scholar] [CrossRef] [PubMed]
- Arthurs, G.I.; LANGLEY-HOBBS, S.J. Complications associated with corrective surgery for patellar luxation in 109 dogs. Vet. Surg. 2006, 35, 559–566. [Google Scholar] [CrossRef] [PubMed]
- Birks, R.R.; Kowaleski, M.P. Combined tibial plateau levelling osteotomy and tibial tuberosity transposition: An ex vivo mechanical study. Vet. Comp. Orthop. Traumatol. 2018, 31, 124–130. [Google Scholar] [CrossRef] [PubMed]
- Dallago, M.; Baroncelli, A.B.; Hudson, C.; Peirone, B.; De Bakker, E.; Piras, L.A. Effect of Plate Type on Tibial Plateau Levelling and Medialization Osteotomy for Treatment of Cranial Cruciate Ligament Rupture and Concomitant Medial Patellar Luxation in Small Breed Dogs: An In Vitro Study. Vet. Comp. Orthop. Traumatol. 2023, 36, 212–217. [Google Scholar] [CrossRef] [PubMed]
- Kettleman, W.S. Ex Vivo Biomechanical Evaluation of a Novel Screw for Tibial Plateau Leveling Osteotomy. Master’s Thesis, Mississippi State University, Starkville, MS, USA, 2022. [Google Scholar]
- Curuci, E.H.; Bernardes, F.J.; Minto, B.W. Modified tibial plateau levelling osteotomy to treat lateral patellar luxation and cranial cruciate ligament deficiency in a dog. Clin. Case Rep. 2021, 9, e04365. [Google Scholar] [CrossRef] [PubMed]
- Livet, V.; Taroni, M.; Ferrand, F.-X.; Carozzo, C.; Viguier, E.; Cachon, T. Modified triple tibial osteotomy for combined cranial cruciate ligament rupture, tibial deformities, or patellar luxation. J. Am. Anim. Hosp. Assoc. 2019, 55, 291–300. [Google Scholar] [CrossRef]
- Windolf, M.; Leitner, M.; Schwieger, K.; Pearce, S.G.; Zeiter, S.; Schneider, E.; Johnson, K.A. Accuracy of fragment positioning after TPLO and effect on biomechanical stability. Vet. Surg. 2008, 37, 366–373. [Google Scholar] [CrossRef]
- Slocum, B.; Devine, T. Cranial tibial thrust: A primary force in the canine stifle. J. Am. Vet. Med. Assoc. 1983, 183, 456–459. [Google Scholar] [PubMed]
- Dismukes, D.I.; Tomlinson, J.L.; Fox, D.B.; Cook, J.L.; Song, K.J.E. Radiographic measurement of the proximal and distal mechanical joint angles in the canine tibia. Vet. Surg. 2007, 36, 699–704. [Google Scholar] [CrossRef] [PubMed]
- Dismukes, D.I.; Tomlinson, J.L.; Fox, D.B.; Cook, J.L.; Witsberger, T.H. Radiographic measurement of canine tibial angles in the sagittal plane. Vet. Surg. 2008, 37, 300–305. [Google Scholar] [CrossRef] [PubMed]
- Bordelon, J.; Coker, D.; Payton, M.; Rochat, M. An in vitro mechanical comparison of tibial plateau levelling osteotomy plates. Vet. Comp. Orthop. Traumatol. 2009, 22, 467–472. [Google Scholar] [CrossRef] [PubMed]
- Sembenelli, G.; Souza, G.; Wittmaack, M.; Shimano, A.; Rocha, T.; Moraes, P.; Minto, B.; Dias, L. Biomechanical comparison of a modified TPLO plate, a locking compression plate, and plate-rod constructs applied medially in a proximal gap model in canine synthetic tibias. Arq. Bras. Med. Vet. Zootec. 2022, 74, 948–953. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.-G. Statistical power analyses using G* Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef] [PubMed]
- Warzee, C.C.; Dejardin, L.M.; Arnoczky, S.P.; Perry, R.L. Effect of tibial plateau leveling on cranial and caudal tibial thrusts in canine cranial cruciate–deficient stifles: An in vitro experimental study. Vet. Surg. 2001, 30, 278–286. [Google Scholar] [CrossRef] [PubMed]
- Robinson, D.A.; Mason, D.R.; Evans, R.; Conzemius, M.G. The effect of tibial plateau angle on ground reaction forces 4–17 months after tibial plateau leveling osteotomy in Labrador Retrievers. Vet. Surg. 2006, 35, 294–299. [Google Scholar] [CrossRef] [PubMed]
- Olimpo, M.; Piras, L.A.; Peirone, B. Pelvic limb alignment in small breed dogs: A comparison between affected and free subjects from medial patellar luxation. Vet. Ital. 2016, 52, 45–50. [Google Scholar] [CrossRef]
- Reif, U.; Dejardin, L.M.; Probst, C.W.; DeCamp, C.E.; Flo, G.L.; Johnson, A.L. Influence of limb positioning and measurement method on the magnitude of the tibial plateau angle. Vet. Surg. 2004, 33, 368–375. [Google Scholar] [CrossRef]
- Wheeler, J.L.; Cross, A.R.; Gingrich, W. In vitro effects of osteotomy angle and osteotomy reduction on tibial angulation and rotation during the tibial plateau-leveling osteotomy procedure. Vet. Surg. 2003, 32, 371–377. [Google Scholar] [CrossRef] [PubMed]
- Aghapour, M.; Bockstahler, B.; Vidoni, B. Evaluation of the femoral and tibial alignments in dogs: A systematic review. Animals 2021, 11, 1804. [Google Scholar] [CrossRef]
- Kloc, P.A.; Kowaleski, M.P.; Litsky, A.S.; Brown, N.O.; Johnson, K.A. Biomechanical comparison of two alternative tibial plateau leveling osteotomy plates with the original standard in an axially loaded gap model: An in vitro study. Vet. Surg. 2009, 38, 40–48. [Google Scholar] [CrossRef]
- Duerr, F.M. Canine Lameness; John Wiley & Sons: Hoboken, NJ, USA, 2020. [Google Scholar]
- Caporn, T.; Roe, S. Biomechanical evaluation of the suitability of monofilament nylon fishing and leader line for extra-articular stabilisation of the canine cruciate-deficient stifle. Vet. Comp. Orthop. Traumatol. 1996, 9, 126–133. [Google Scholar] [CrossRef]
- Franklin, S.P.; Gilley, R.S.; Palmer, R.H. Meniscal injury in dogs with cranial cruciate ligament rupture. Compend. Contin. Educ. Vet. 2010, 32, E1–E10. [Google Scholar] [PubMed]
- Polisetty, T.; DeVito, P.; Judd, H.; Malarkey, A.; Levy, J.C. Reverse shoulder arthroplasty for failed proximal humerus osteosynthesis with intramedullary allograft: A case series. J. Shoulder Elb. Arthroplast. 2020, 4, 2471549220925464. [Google Scholar] [CrossRef]

| Parameters | TPLO Plate Group | PCM–TPLO Plate Group | p Value | ||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| Preoperative TPA (°) | 25.00 | 2.00 | 25.25 | 2.86 | 0.798 |
| Postoperative TPA (°) | 5.48 | 1.66 | 5.38 | 2.15 | 0.878 |
| Preoperative mMPTA (°) | 96.96 | 4.33 | 96.13 | 6.17 | 0.721 |
| Postoperative mMPTA (°) | 97.04 | 1.84 | 94.34 | 4.38 | 0.131 |
| Bone–plate gap (mm) | 0.59 | 0.54 | 1.90 | 0.44 | 0.001 |
| Load to failure (N) | 798.80 | 375.02 | 721.50 | 292.02 | 0.818 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jeong, E.; Jeon, Y.; Kim, T.; Lee, D.; Roh, Y. Assessing the Effectiveness of Modified Tibial Plateau Leveling Osteotomy Plates for Treating Cranial Cruciate Ligament Rupture and Medial Patellar Luxation in Small-Breed Dogs. Animals 2024, 14, 1937. https://doi.org/10.3390/ani14131937
Jeong E, Jeon Y, Kim T, Lee D, Roh Y. Assessing the Effectiveness of Modified Tibial Plateau Leveling Osteotomy Plates for Treating Cranial Cruciate Ligament Rupture and Medial Patellar Luxation in Small-Breed Dogs. Animals. 2024; 14(13):1937. https://doi.org/10.3390/ani14131937
Chicago/Turabian StyleJeong, Eunbin, Youngjin Jeon, Taewan Kim, Dongbin Lee, and Yoonho Roh. 2024. "Assessing the Effectiveness of Modified Tibial Plateau Leveling Osteotomy Plates for Treating Cranial Cruciate Ligament Rupture and Medial Patellar Luxation in Small-Breed Dogs" Animals 14, no. 13: 1937. https://doi.org/10.3390/ani14131937





