Abstract
Type 2 diabetes mellitus is one of the main chronic diseases worldwide, with a significant impact on public health. Behavioral changes are an important step in disease prevention and management, so the way in which individuals adapt their lifestyle to new circumstances will undoubtedly be a predictor of the success of the treatments instituted, contributing to a reduction in the morbidity and mortality that may be associated with them. It is essential to prepare and educate all diabetic patients on the importance of changing behavioral patterns in relation to the disease, with health professionals assuming an extremely important role in this area, both from a pharmacological and non-pharmacological point of view, and also ensuring the monitoring of the progress of these measures. Diabetes is a chronic disease that requires a high self-management capacity on the part of patients in order to achieve success in treating the disease, and non-adherence to therapy or non-compliance with the previously defined plan, together with an erratic lifestyle, will contribute to failure in controlling the disease. The lower adherence to pharmacological and non-pharmacological treatment in diabetes is mainly correlated to socio-economic aspects, lower health literacy, the side effects associated with the use of antidiabetic therapy or even the concomitant use of several drugs. This article consists of a narrative review that aims to synthesize the findings published in the literature, retrieved by searching databases, manuals, previously published scientific articles and official texts, following the methodology of the Scale for Assessment of Narrative Review Articles (SANRA). We aim to address the importance of behavioral sciences in the treatment of diabetes, in order to assess behavior factors and barriers for behavior changes that have an impact on the therapeutic and non-therapeutic optimization in patients with type 2 diabetes mellitus control.
1. Introduction
The high incidence of chronic diseases and non-adherence (or inadequate adherence) to pharmacological and non-pharmacological treatments by patients represent a serious problem in terms of public health, constituting a growing challenge for the different institutions and health professionals involved.
Failure to comply with the defined therapeutic plans can result in clinical complications, physical and emotional stress caused by the need for successive hospitalizations, consequently leading to economic and financial implications at the level of health systems [1,2].
Diabetes is one of the chronic diseases with the greatest impact worldwide in terms of morbidity and mortality, being closely associated with poor eating habits, sedentary lifestyle, smoking, alcoholism, increased life expectancy and the genetic component of each individual [3,4,5]. It has a multifactorial nature, is complex and heterogeneous, whose pathophysiology is closely associated with the development of insulin resistance and hyperglycemia, contributing to the impairment of the normal functioning of different organs and physiological systems, with type 2 diabetes mellitus (DM2) being the most prevalent form (about 90% versus 10% of type 1) [6,7].
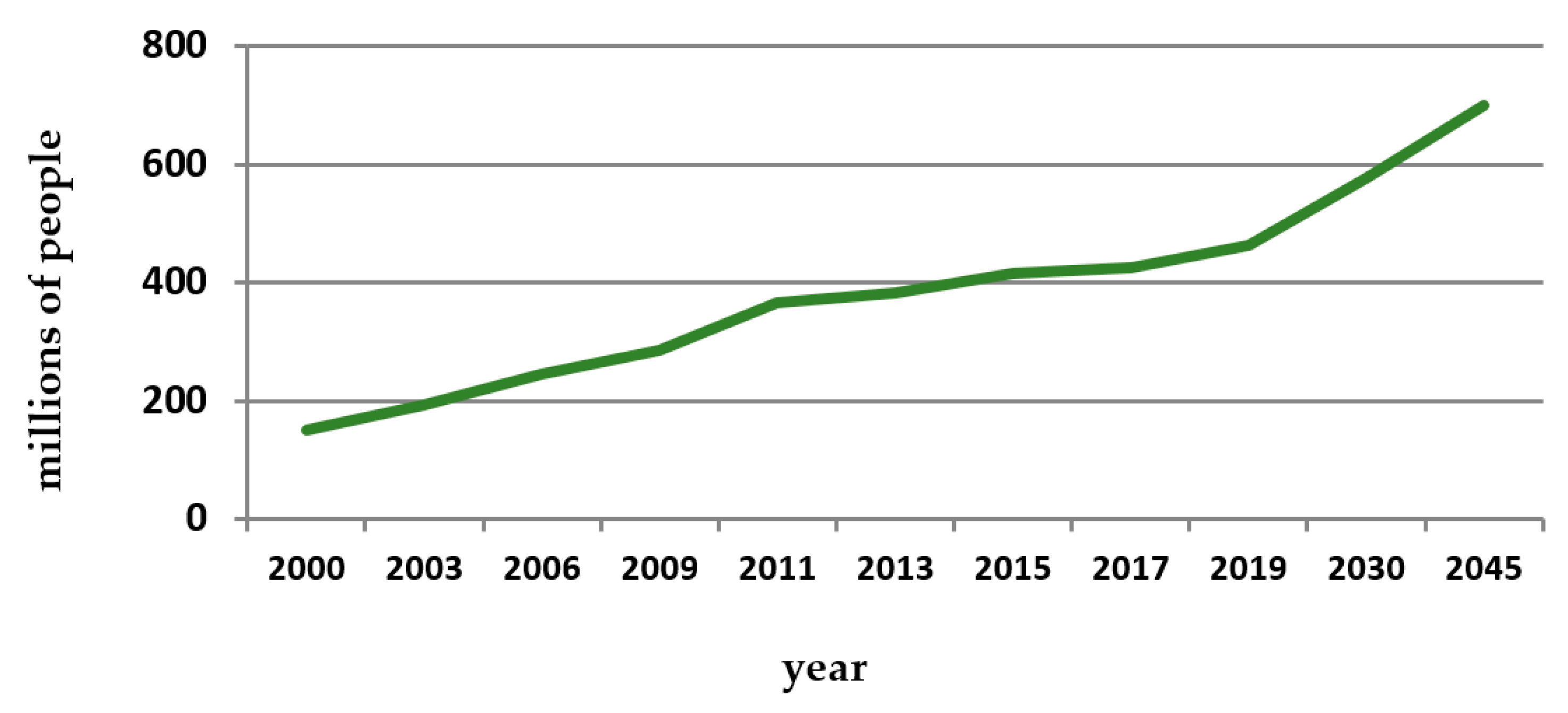
According to the International Diabetes Federation (IDF), for 2019, both forms of diabetes caused 4.2 million deaths, and there are around 463 million adults aged between 20 and 79 years diagnosed with the disease, a number that will likely increase to 700 million by 2045 (Figure 1) [8,9]. Furthermore, the disease is likely to be under-represented, as there are suggestive data indicating that 1 in 3 patients are under-diagnosed [8].
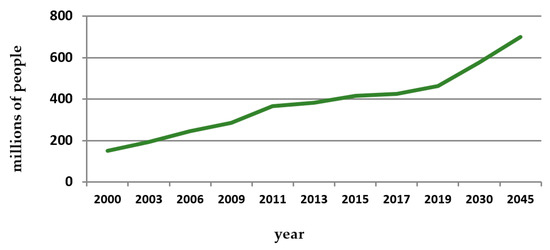
Figure 1.
Estimated number of adults with diabetes (in millions) since 2000 to 2045. Source: IDF Diabetes Atlas editions [8].
Sarwar N. et al. (2010) demonstrated through a meta-analysis that there is a strong association between DM2 and an increased risk of coronary heart disease, ischemic stroke, retinopathy, nephropathy, foot ulcers (diabetic foot) and lower limb amputations [10,11].
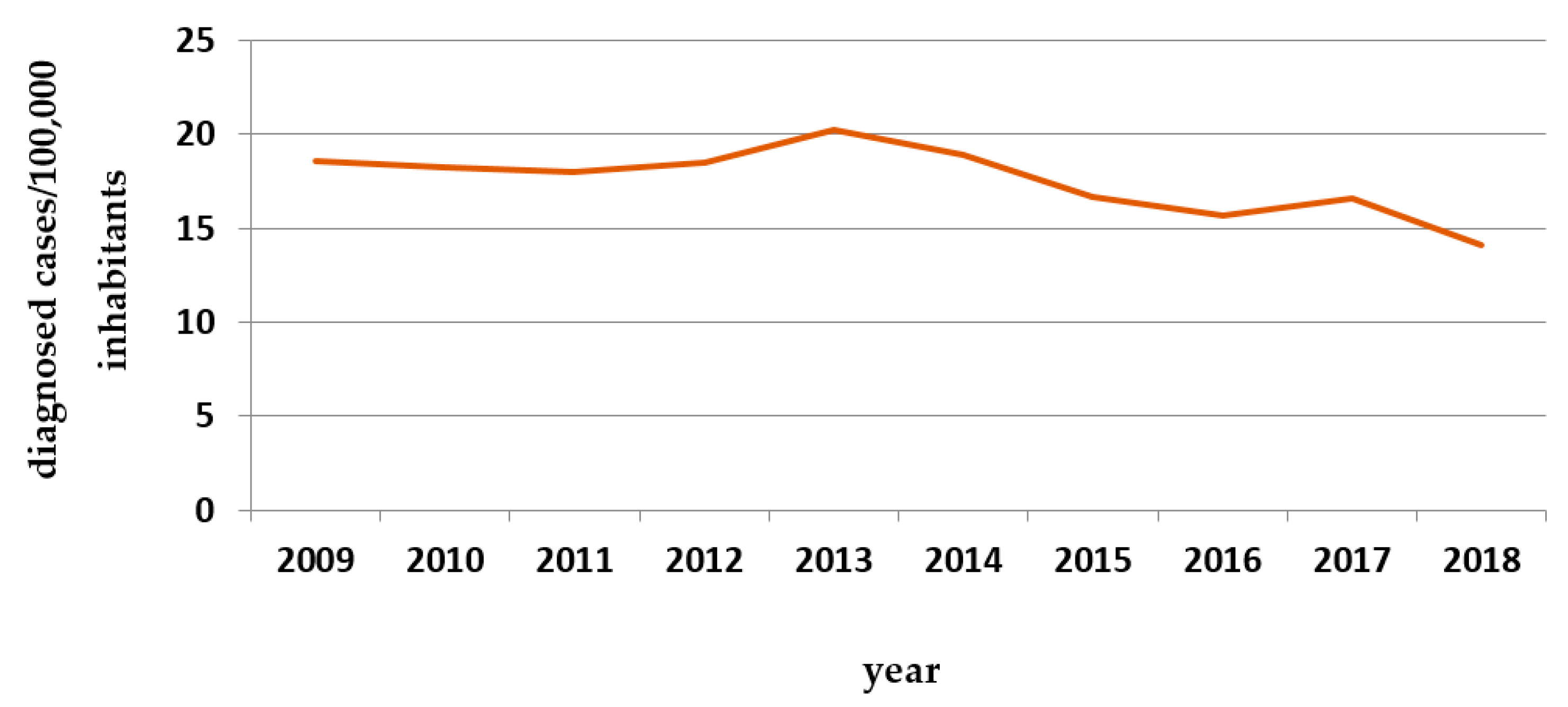
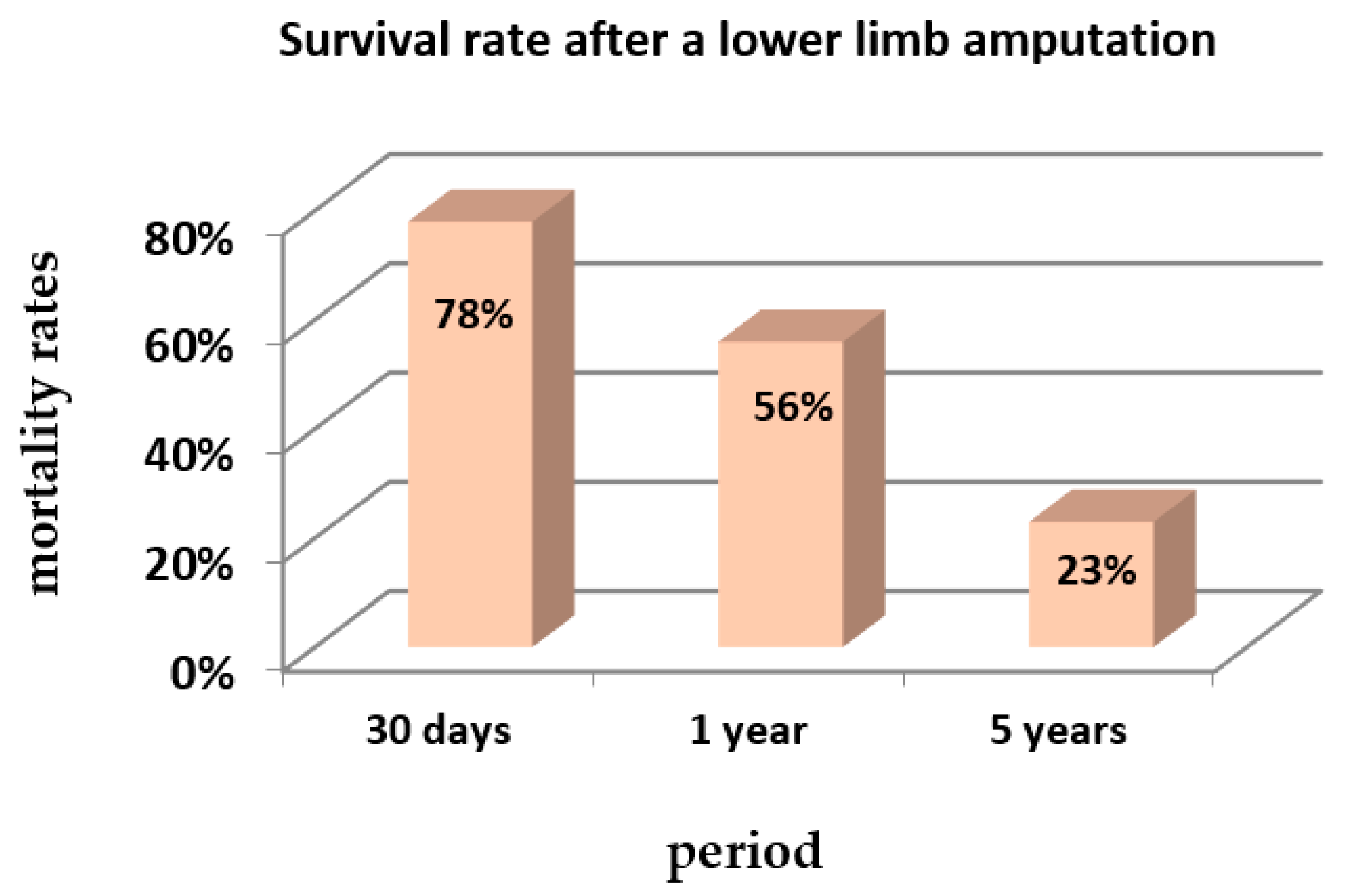
The following figures contain data on the incidence of diabetic foot (Table 1 and Figure 2) and mean survival after lower limb amputation (Figure 3), two of the most common complications in diabetic patients.
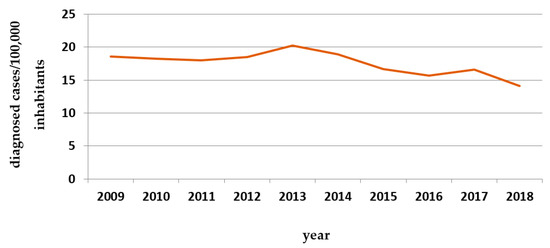
Figure 2.
Number of cases diagnosed in Portugal with “diabetic foot” per 100,000 inhabitants (hospital admissions) since 2009 to 2018. Source: INFARMED [13].
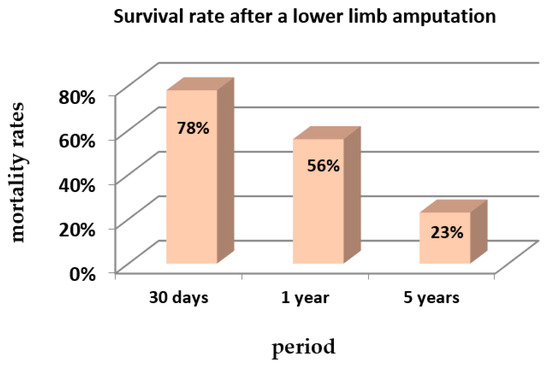
Figure 3.
Mortality rates after a first lower limb amputation (%) in a period of 5 years—retrospective cohort study. Source: Fortington et al., 2013 [14].

Table 1.
Prevalence of diabetic foot ulcers in different countries in the population of patients with DM2 followed at the hospital level and in public health study centers. Source: Pengzi Zhang et al., 2017 [12].
Table 1.
Prevalence of diabetic foot ulcers in different countries in the population of patients with DM2 followed at the hospital level and in public health study centers. Source: Pengzi Zhang et al., 2017 [12].
| Country | No. of Studies | Prevalence | Country | No. of Studies | Prevalence |
|---|---|---|---|---|---|
| Belgium | 1 | 16.6% | South Africa | 2 | 5.8% |
| Canada | 1 | 14.8% | France | 1 | 5.6% |
| USA | 3 | 13.0% | Greece | 1 | 4.8% |
| Trinidad | 1 | 12.2% | Jordan | 2 | 4.2% |
| India | 2 | 11.6% | China | 10 | 4.1% |
| Norway | 1 | 10.4% | Uganda | 1 | 4.0% |
| Cameroon | 3 | 9.9% | Ireland | 1 | 3.9% |
| Italy | 1 | 9.7% | Turkey | 1 | 3.1% |
| Thailand | 2 | 8.8% | Spain | 5 | 3.0% |
| Denmark | 1 | 7.8% | Germany | 2 | 2.8% |
| Pakistan | 4 | 7.4% | Saudi Arabia | 1 | 2.3% |
| Tanzania | 2 | 7.3% | Japan | 1 | 2.0% |
| Pacific island countries | 1 | 6.8% | Netherlands | 2 | 1.8% |
| United Kingdom | 4 | 6.3% | Korea | 2 | 1.7% |
| Egypt | 2 | 6% | Poland | 1 | 1.7% |
| Bahrain | 1 | 5.9% | Australia | 2 | 1.5% |
The burden of suffering due to diabetes is increasing despite significant investment in clinical care and pharmaceutical research. Notably, Western Europe has a rate of increase greater than that of global and Asian averages. Even with the high levels of clinical and public health expenditure, this region is losing the battle against diabetes. One explanation might be non-modifiable risk factors, such as age and family history [15]. In fact, global aging, economic growth, rapid and trending urbanization, as well as nutritional transitions (to a highly processed, high-calorie diet) associated with a sedentary lifestyle, exacerbate this trend [16].
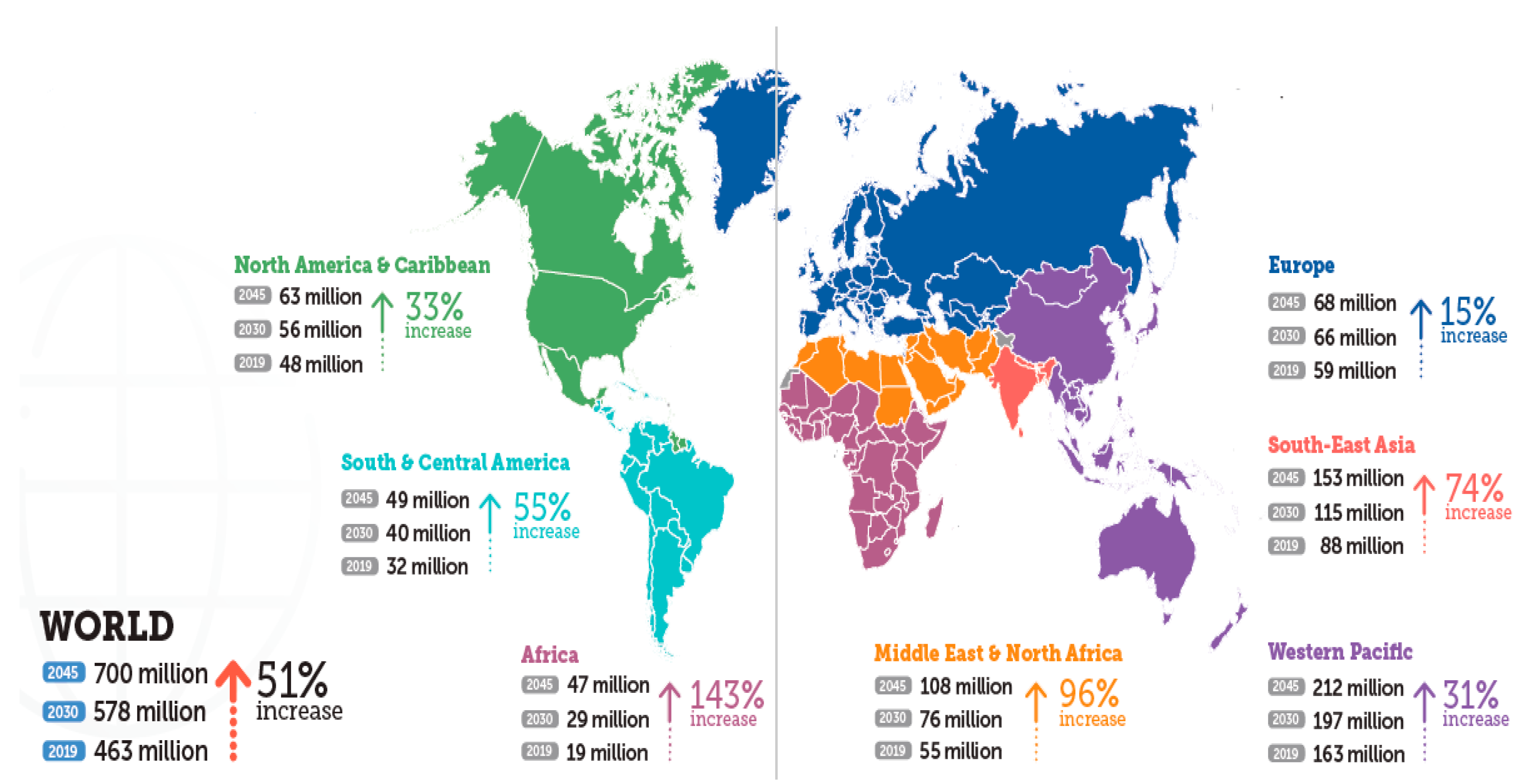
According IDF, and Figure 4 illustrates this reality, developed countries endure the highest burdens of human suffering due to diabetes and some findings support the correlation between diabetes and economic development [17].
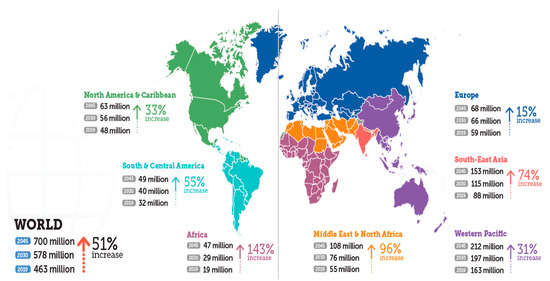
Figure 4.
Number of people with diabetes worldwide and per IDF region in 2019, 2030 and 2045 (age 20–79 years). Source: IDF Diabetes Atlas editions [8].
These findings have direct implications for health systems planning and resource allocation. Clearly, hospital-based management and subspecialist care are not sustainable strategies. Resource allocation in healthcare budgets for the prevention of diabetes, promoting health behaviors that are consistent with more effective disease prevention, needs to be comparable to expenditures on treatment [18].
The consequences associated with erratic behavior, both in terms of adherence to therapy and in terms of lifestyle, preventing adequate glycemic control can trigger potential complications, including cardiovascular disease, peripheral neuropathy, kidney disease, retinopathy, skin disorders, hearing changes, sleep apnea or neurological disorders associated with dementia, which can be extremely disabling and compromise the life expectancy of patients [19,20].
In order to ensure an acceptable level of quality of life in the face of the clinical condition of diabetes, it is essential that patients adopt appropriate behaviors in terms of adherence to therapy and that they are complemented with a healthy lifestyle, with health professionals taking on a fundamental role in terms of education and guidance in this regard. In this context, the behavioral sciences meet this premise, aiming to assess how human actions can contribute to a greater or lesser effectiveness of the pharmacological and non-pharmacological measures instituted and, therefore, how they influence the quality of the disease’s prognosis [20].
There is some scarcity of studies addressing the topic of diabetes mellitus in an interdisciplinary way, with most published studies addressing disease behaviors as being essentially clinical and pharmacological in nature, without reflection on the role that behavioral sciences can play in disease management. To address this gap, our aim with this narrative review is to address the potentially modifiable factors that can influence the adoption of appropriate behaviors by patients with DM2, in order to enable an adequate treatment and control of the disease, emphasizing the role of behavioral sciences. It is a global approach that, in addition to aspects directly related to lifestyle and adherence to pharmacological therapy, intends to provide a historical and statistical context of the disease, complemented with a brief summary of its pathophysiology, of the pharmacological therapies currently available as well as of elementary concepts for the understanding and applicability of behavioral sciences. Since health professionals need to carry out a constant review and update of knowledge in order to optimize their professional practice, the growing knowledge about diseases, the continuous emergence of new therapeutic formulations, as well as the definition of strategies each time more rigorous in terms of influencing behaviors, highlight the importance of carrying out review studies in these areas that are capable of offering a holistic view of all the factors, bringing together those which may impact on the control and treatment of chronic diseases.
2. Materials and Methods
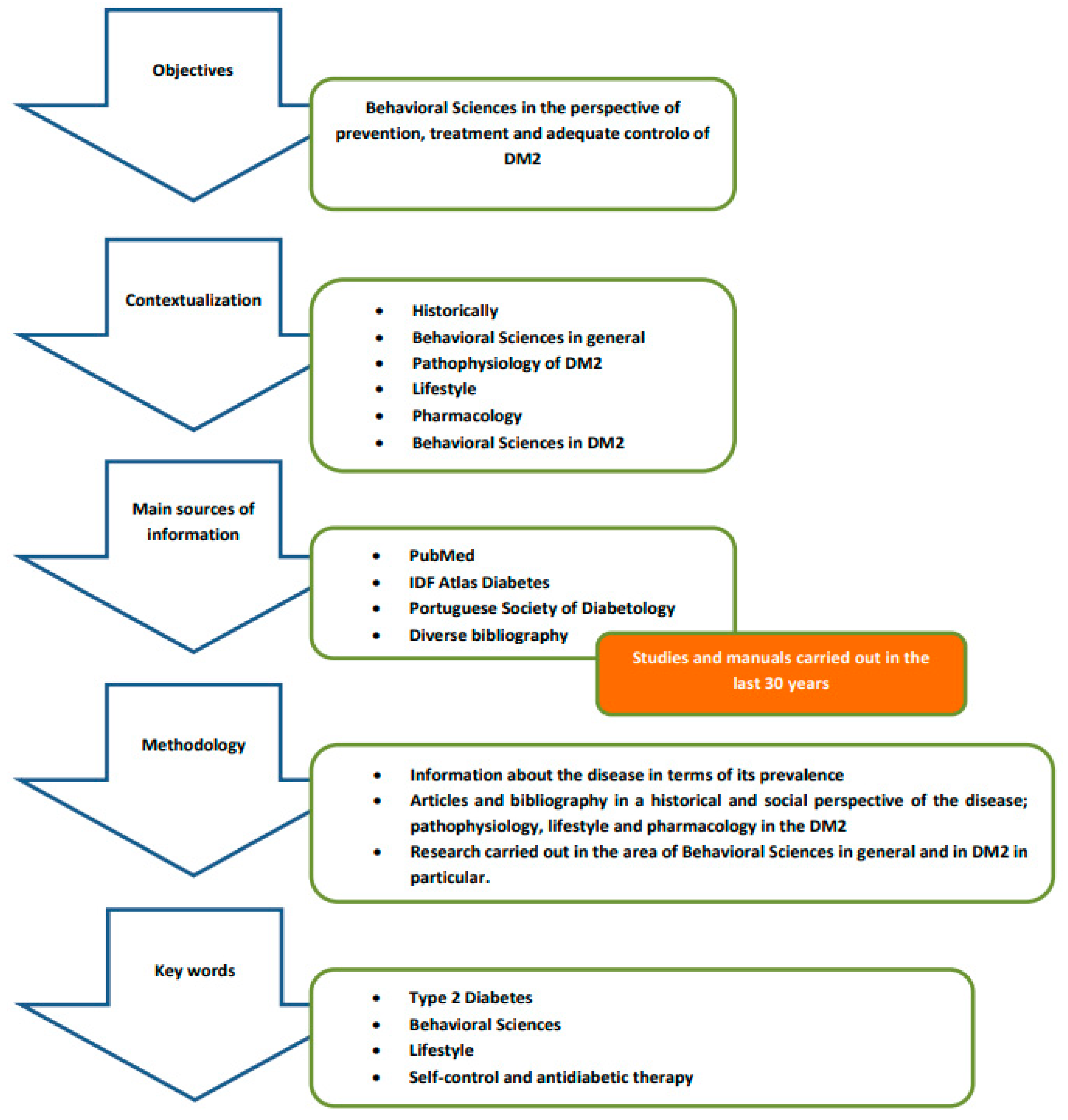
A narrative review was developed to synthesize the findings published in the literature, retrieved through a search of databases, manuals, previously published scientific articles and official texts, following the Scale for the Assessment of Narrative Review Articles (SANRA) methodology as schematized in Figure 5 [21].
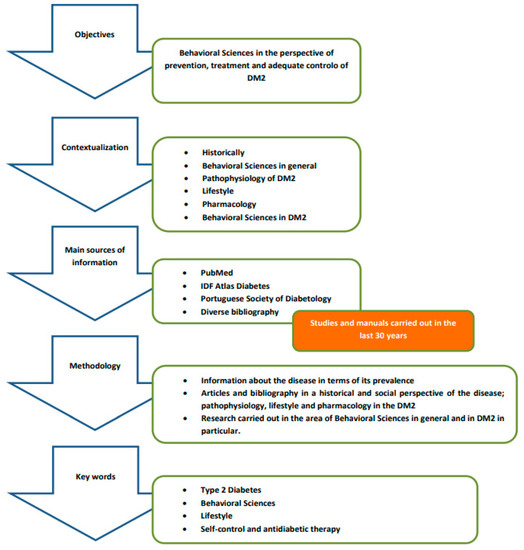
Figure 5.
Research methodology and information synthesis.
- -
- The guiding principle used in this review, which, in the end, defines the central issue of this work, is the importance of behavioral sciences in the perspective of prevention, treatment and adequate control of DM2, so the adoption of assertive behaviors assumes an extreme preponderance in achieving positive results, with health professionals having a decisive role in defining effective strategies to ensure that patients can assume a commitment, at a behavioral level, leading to the success of pharmacological and non-pharmacological treatments instituted.
- -
- This narrative review intends to contextualize the disease from a historical point of view; summarize the essence of behavioral sciences and what is its framework; discuss what kind of approach should be taken both in terms of lifestyle and pharmacologically, given the pathophysiology of DM2, reviewing the therapeutic options currently available and its main characteristics that can influence the behavior of patients; and address the potentially modifiable aspects that are decisive in influencing the behavior of patients with DM2.
- -
- The main sources of information were databases such as PubMed, IDF Diabetes Atlas, the Portuguese Society of Diabetology, as well as manuals in the field of Pharmacology/Pharmacotherapy, focusing generically on search terms such as behavioral sciences, history, pathophysiology, lifestyle and complications/comorbidities in diabetes, and specifically guidelines for the treatment of DM2 and behavioral sciences in diabetes.
- -
- The key statements are supported by references to studies carried out in the past 30 years in the field of behavioral sciences as well as on the history, incidence, pathophysiology and drug therapy of DM2. We used a three-stage approach to review the literature:
- The first stage consisted of researching statistical information about the disease in terms of its prevalence.
- The second stage refers to the research of articles and bibliography in a historical and social perspective of the disease; pathophysiology, lifestyle and pharmacology in the DM2.
- The third stage reports on research carried out in the area of behavioral sciences in general and in DM2 in particular.
- -
- The initial keywords were organized into the following conceptual categories: type 2 diabetes, behavioral sciences, lifestyle, self-control and antidiabetic therapy. Search terms were developed and customized for each database.
- -
- The data and information gathered are presented establishing a logical sequence that aims to demonstrate how it is possible to identify and act to ensure adequate control of DM2 from the behavioral perspective of patients with the disease.
3. Main Findings
3.1. Historical and Social Context of the Disease and Behaviors
The first known mention of diabetes symptoms was in 1552 BC, when Hesy-Ra, an Egyptian physician, documented frequent urination as a symptom of a mysterious illness that also caused weight loss. Also at this time, ancient healers recorded that ants seemed to be attracted to the urine of people who had this disease [22].
In AD 150, the Greek physician Arateus described what we now call diabetes as “the melting of flesh and limbs in urine” [23].
Centuries later, people known as “water testers” diagnosed diabetes by sampling the urine of people suspected of suffering from the disease. If the urine tasted sweet, diabetes would be diagnosed [24].
During the Franco-Prussian War in the early 1870s, the French physician Apollinaire Bouchardat observed that the symptoms of his diabetic patients improved due to food rationing caused by the war, and from then on, he developed individualized diets for the treatment of diabetes. This logic led to very common diets in the early 1900s, which included the “oat cure”, the “potato therapy” and the “hunger diet” [25].
In 1916, scientist Elliott Joslin established himself as one of the world’s leading diabetes experts by creating the book The Treatment of Diabetes Mellitus, which reported that a fasting diet combined with regular exercise could significantly reduce the risk of death in patients with diabetes [26].
The association of insulin shortage with the disease in the first half of the 20th century radically changed the approach to the disease, marking the beginning of a therapeutic revolution in this area.
Today, healthcare professionals still use some of these principles when modulating their patients’ behavior towards lifestyle changes that allow for adequate disease control [24,27,28].
In the first half of the 20th century, public health was mainly dominated by a biomedical perspective, and only after the Second World War was it also framed within a social science perspective. From that period on, there was a theoretical development in economics, political science, sociology and anthropology, re-dimensioning the concept of public health, which previously focused mainly on the individual, now coming to understand the entire social structure [2,6]. It is also from this moment that many individual behaviors were not only recognized as risk factors for health problems, but also began to be inserted in a broader social context. Public health policy, based on social sciences, was the key to the development of strategies capable of promoting appropriate practices in the promotion of healthy lifestyles, with a clear impact on the prevention and control of several chronic diseases such as DM2 [6,29].
3.2. The Essence of Behavioral Sciences
Behavioral sciences generally correspond to a branch of science (such as psychology, sociology or anthropology) directly applicable to human action, with the aim of generalizing about human behavior in society.
A patient’s psychological aspects such as personal values, beliefs, cognitive function and emotion form the basis of behaviors in human health, which, in turn, influence self-management, self-efficacy, quality of life, control and clinical outcomes in patients with chronic diseases [30].
Whitley and Kite (2013) argue that the behavioral sciences are based on three fundamental and closely related principles: research that generates knowledge, theory that organizes knowledge and application that puts knowledge to use [2].
The main objective of science in behavior change is to improve our understanding of the mechanisms of action of the interventions that are intended to be implemented [31].
Behavior theories identify potential “determinants” of behavior, that is, factors that can influence the behavior under analysis. These determinants are the pathways through which behavior change techniques are applied in order to achieve the intended results [32,33].
Currently, behavior change intervention mechanisms are typically studied using mediation analyses, where the impact of X (an intervention) on Y (a behavioral outcome) is adapted to be subject to a third variable M (for example, a theoretical determinant of the behavioral outcome targeted by the intervention). In the presence of classical mediation, the X-Y path would be reduced to almost zero when variable M is added to the model. In the case of behavior change interventions, one could conclude that intervention (X) changed behavior (Y) because it changed important theoretical determinants of behavior (M) [34].
In an analysis of behavioral mechanisms, its accuracy tends to be simpler if certain requirements are met, such as [34]:
- -
- The number of variables involved is small and the dynamics can be significantly evaluated in just a few points of time;
- -
- The change process is the same for all individuals, e.g., following the same sequence;
- -
- The dynamics between variables is linear, additive and does not change over time; and
- -
- Included variables are not diluted in context or omitted.
However, human behavior is complex, and although theories have been formulated as close as possible to linear methods of analysis, this approach can mask important characteristics of behavior change. Linear models are inadequate in most studies related to behavioral sciences, because on the one hand, there are many non-linear interactions in the time scale [35,36,37,38], and on the other hand, traditional statistical analyses start from the simplification that everything is regardless of what surrounds it [39,40].
To face this limitation, complex adaptive systems (CAS) have emerged, which represent a more useful analytical lever for behaviors [41]. A CAS involves several levels of interaction between heterogeneous agents; not all intervention components are created equally, thus giving it a non-linear nature. It is a system that is composed of heterogeneous actors and the behavior of each responds to the actions of other people within the system (it is adaptive) [42]. The agents within a CAS are interconnected in such a way that each action of an individual affects the context of the other agents—with indirect implications for all subsequent behavior [43]. In this case, the control of behavior is distributed rather than hierarchical. It is the ability to respond to change between agents, acting locally within the CAS, that gives such systems their dynamic, responsive and productive nature [44]. Due to the dynamic and changing nature of social contexts, actors within a complex system are constantly adapting to changes at the local level. If social behavior evolves in this way, a CAS does not reach stagnation—instead, it expresses a double movement between stability and instability; regularity and irregularity [45].
Understanding the mechanisms that can influence the behavior of patients in order to promote optimal adherence to therapeutic plans in the treatment of chronic diseases requires a comprehensive vision that understands the dynamism of the environment in which they live, as well as their individual characteristics that may affect whole the process.
3.3. Pathophysiology of Type 2 Diabetes
Obesity and sedentary lifestyle are states of insulin resistance that, when associated with genetic factors, adversely affect the functioning of pancreatic β cells, which, in a compensatory way, increase insulin secretion. An excessive intake of carbohydrates, associated with a malfunction in the feedback circuits between the action of insulin and its secretion, results in abnormally high levels of glucose in the blood [3,19,46,47]. The maintenance of this compensatory state in insulin secretion leads, over time, to the appearance in an initial phase of high levels of postprandial glucose, in a second phase of fasting glucose, ultimately culminating in the onset of diabetes mellitus of the type 2 [4,19]. If the dysfunction is present in the β-cells, insulin secretion is reduced, limiting the body’s ability to maintain physiological glucose levels. On the other hand, insulin resistance contributes to an increase in the hepatic production of glucose and a decrease in its uptake by muscle, liver and adipose tissue [4,19,48]. β-cell dysfunction is generally more severe than insulin resistance, but when both are present, hyperglycemia is amplified, leading to DM2 progression [49,50,51]. This dysfunction has traditionally been associated with β-cell death; however, recent evidence suggests that it may be associated with a more complex network of interactions between the environment and the different molecular pathways involved in cell biology [52]. Hyperglycemia results from the combination of different pathophysiological anomalies ranging from resistance to insulin action (both liver and muscle), by its inadequate secretion, by excessive or inappropriate glucagon secretion, by reduced incretin effect, by increased lipolysis, due to increased renal glucose reabsorption and dysfunction of brain neurotransmitters [5,51,53,54]. In the face of an excessive nutritional status, similar to that found in obesity, hyperglycemia and hyperlipidemia are often present, promoting insulin resistance and chronic inflammation. Under these circumstances, β cells, due to differences in terms of genetic susceptibility, are subject to toxic pressures, inflammation and metabolic/oxidative and amyloid stress, with the potential to ultimately lead to a loss of their integrity [47,50,52,53].
DM2 patients often present, in terms of symptoms, lethargy, polyuria, nocturia and polydipsia [5,51].
3.4. Healthy Lifestyle
Therapeutic success in DM2 depends on the effectiveness of the pharmacological treatments instituted, which must be complemented with a healthy lifestyle, so it is essential that adequate behavioral practices are ensured both in terms of a balanced/adequate diet as well as by the need for regular physical exercise, especially in obese patients who are at an increased risk of developing the disease [55,56,57,58].
From a dietary point of view, compliance with certain recommendations allows not only preventing the onset of the disease, but also delaying/preventing its progression. A decrease in the intake of added sugars and processed foods; an increase in the intake of fiber, fruits and vegetables; a reduction in the intake of processed meat and red meat; and the intake of healthier fats are key aspects for a more balanced diet, capable of contributing to a significant improvement in the clinical prognosis of the disease [59,60].
Physical exercise is also extremely important in the prevention and control of DM2, and the incidence of the disease is inversely proportional to the participation in physical activities, and this relationship was demonstrated by the systematic review by Warburton et al. (2010) when they analyzed several cohort studies in this area [58,59,60,61,62].
Weight loss is important for the prevention of DM2, and studies of intensive lifestyle intervention have shown that there was a 16% reduction in the risk of diabetes per kilogram of weight lost [60,62].
The patient must be made aware of the importance of strict adherence to therapy as well as the adoption of a healthy lifestyle so that the benefit of pharmacological therapy is maximized, being essential the differentiating intervention of health professionals in this regard, both by the need to promote good practices as well as to ensure ever more rigorous information channels are ensured, especially in an era where very unreliable sources of information proliferate [63,64].
According to the World Health Organization, “without a system that addresses the determinants of adherence, advances in biomedical technology will fail to realize their potential to reduce the burden of chronic disease” [65].
According to the clinical guidelines for the treatment of diabetes, there are three fundamental principles that must be adhered to in order to ensure adequate control of the disease [66]:
- Lifestyle changes with the adoption of adequate eating habits and physical exercise throughout the course of the disease;
- Individualization of therapy and patient-centeredness; and
- Therapeutic Education (TE) or DSMES (Diabetes Self-Management Education and Support), which is essential in the care provided to people with type 2 diabetes.
Since patient-centeredness is one of the fundamental points in the treatment and control of DM2, behavioral sciences play a fundamental role at this level, especially in terms of their inclusion in informed and shared decision-making. Some studies estimate that one in three patients do not comply with the established therapeutic regimen, with higher non-compliance rates among racial/ethnic minorities and in people with low socioeconomic status [67,68]. The impact of non-adherence to the instituted therapy leads to an increase in morbidity and mortality rates, in addition to having an impact on costs at the level of healthcare systems [69,70,71].
There are several factors that contribute to non-adherence to therapy, such as side effects of medication, disbelief in the treatment, lack of motivation, deterioration of the relationship between the health professional and the patient, difficulties in accessing treatment, impaired cognitive function and inability to adopt healthy lifestyle habits [67,68].
It is essential that communicational strategies are adopted that influence behaviors, especially by selecting theories of behavioral influence, which provide patients with DM2 with assertive behavior and that allow for the proper treatment and control of the disease [70,71,72]. An adequate theory should demonstrate effectiveness in predicting behavior, focused on modifiable targets, able to provide a sufficient description of how targets explain or mediate effects on behavior (specific pathways), and include measures that properly operationalize the intended targets to drive behavior change, following the information-motivation and behavioral skills (MBS) model to these premises [71,72,73,74,75,76].
Briefly, the MBS model defends that an informed patient, motivated and available to act, has the skills and confidence to make more assertive decisions that will allow greater success in the desired results. Patient/disease characteristics can be classified as being generally non-modifiable or potentially modifiable [77,78]. Poor adherence to therapy is associated with factors that may not be directly related to the patient (such as lack of integrated care at the level of health systems and clinical inertia among health professionals), demographic factors (young age, low level of poor education and financial situation), the patient’s beliefs about the therapy (perceived treatment ineffectiveness) and the implications for the patient that are directly related to the therapeutic regimen (treatment complexity, direct costs and hypoglycemia) [77,78,79]. Aspects such as the risks potentially associated with hypoglycemia and other adverse drug effects, the duration of diabetes (whether the diagnosis is recent or long-term), the life expectancy, concomitant pathologies and established vascular complications are generally not modifiable [78]. The patient’s attitude and motivation, as well as their capacity for self-care, together with the resources and support systems at their disposal, are potentially modifiable aspects that can decisively influence the disease’s evolutionary state [77,78,79,80].
Strategies aimed at low adherence should focus not only on reducing the impact of therapy in terms of adverse events, but also on addressing and correcting patients’ negative beliefs regarding medication. In order to overcome these obstacles, it is essential to use methodologies based on behavioral innovations, as well as new methods and modes of drug administration [77,78]. The specific barriers to adherence to therapy in type 2 diabetes, especially those that are potentially modifiable, should be identified more rigorously and should be seen as a priority target for action in terms of behavioral influence.
It is important, first of all, to know some concepts that are often used interchangeably in the description of behavior in patients’ compliance with a therapeutic regimen, namely adherence (to what extent a patient’s behavior—taking medication, following a diet and/or making lifestyle changes—corresponds to the recommendations agreed with a health professional), agreement (joint agreement between the prescriber and the patient regarding therapeutic decisions, including the use of prescribed drugs in a certain way), compliance (to what extent the patient’s behavior corresponds to the prescriber’s recommendations) and persistence (the length of the process use of a drug) [81]. However, the use of the term “compliance” has fallen into disuse, as it suggests a lack of patient involvement [81].
3.5. Pharmacological Treatment
Treatment includes the definition of a glycemic target with a view to its normalization (with most patients having an HbA1c < 6.5%, which should be evaluated every 3 months), educational measures, evaluation of micro and macrovascular complications, monitoring and control of cardiovascular risk factors and, in the long term, avoiding drugs that may exacerbate inappropriate insulin levels or influence lipid metabolism [54,66,82].
The selection of an appropriate “p-treatment” should follow defined guidelines (consensus report by the American Diabetes Association—ADA—and the European Association for the Study of Diabetes—EASD), considering the intended therapeutic objectives and inter-individual and intra-individual variability (age, life expectancy and concomitant comorbidities) [66,82]. It is essential that certain risk groups be considered and classified, in which the treatment of hyperglycemia requires the use of specific references, such as in cases of cardiovascular patients or patients with chronic kidney disease, in the most debilitated elderly, in patients in whom hypoglycemia occurrence is potentially more serious and even in the obese. Given the specificities inherent to the treatment of hyperglycemia in these populations, these recommendations include specific references for these situations [66,83].
Over the past few decades, we have witnessed the market introduction of different therapeutic formulations, varying in terms of mechanisms of action, routes of administration and even the emergence of fixed-dose combinations, which have, on the one hand, allowed the therapeutic objectives to be achieved and pre-defined clinical stability and, on the other hand, facilitate/optimize adherence to therapy, bypassing behavioral barriers that may compromise the success of established therapeutic regimens [48,84].
The available pharmacological treatments focus on increasing the availability of insulin (either through the direct administration of insulin or the administration of drugs that promote its secretion), increasing insulin sensitivity and reducing or preventing the absorption of glucose at the level of the gastrointestinal tract, by increasing urinary glucose excretion or by a combination of several approaches (Table 2).

Table 2.
General characteristics of anti-diabetic therapy [4,5,51,54,83,84,85,86].
The association of drugs with different mechanisms of action to benefit from the synergistic effect should be privileged. The combination of three oral antidiabetics may possibly be considered; however, if necessary, the early initiation of insulin should be considered in patients who have difficulty in achieving the defined goal in therapeutic terms [51,54].
3.6. Potentially Modifiable Factors in Which Efforts Should Be Made to Influence the Behavior of Patients with DM2
3.6.1. The Effectiveness of the Treatment According to the Patient’s Perception
Patients are more likely to adhere to treatment regimens when they have some tangible sense that the prescribed medication contributes to relatively immediate positive outcomes.
In DM2, most patients are asymptomatic, and the pathology can only be diagnosed after blood analysis. However, in more advanced/severe stages of the disease, symptoms such as lethargy, polyuria, nocturia and polydipsia are frequent, mainly in overweight patients [51].
The benefits resulting from the fulfillment of a certain therapeutic plan that makes it possible to correct/attenuate the symptoms undoubtedly contribute to a more effective adherence by the patients and better self-control [87,88,89].
3.6.2. The Incidence of Hypoglycemia
The fear of a hypoglycemic crisis is generally considered one of the main barriers to achieving adequate DM2 control [89,90,91,92,93].
A cross-sectional study of DM2 patients treated with metformin and a sulfonylurea demonstrated that patients who reported moderate or severe symptoms of hypoglycemia had conditioned medication adherence compared to those without mild hypoglycemia or without hypoglycemia [92,93].
According to Polonsky and Henry study [76], 56% of patients with type 2 diabetes had experienced hypoglycemia and had higher HbA1c levels compared to the rest.
Strategies must be adopted by health professionals who work at the level of prevention of the risk of hypoglycemia, focused on patient education and also favoring the use of new therapeutic agents that are associated with a lower incidence of hypoglycemic events [94].
3.6.3. Complexity and Convenience of Treatment
Adherence to therapy becomes more challenging when the treatment itself is seen as more complex, costly or painful [95,96]. Treatment persistence is a key element associated with the effectiveness of pharmacological therapies in DM2 patients.
Antidiabetic drugs act through different mechanisms of action; therefore, the definition of the therapeutic regimen must consider the characteristics of the patients, the mode of administration (oral or injectable), the intended glycemic effect and the potential risks (hypoglycemia, weight gain, cardiovascular safety profile and side effects) [96,97].
In a comprehensive review including 76 studies, Claxton et al. (2010) concluded that, for polymedicated patients (with several prescribed drugs and with multiple daily doses), there is a decreasing adherence to the treatment plan [98].
Studies carried out on the relationship between the onset of depressive symptoms and glycemic control in DM2 have shown that patients undergoing insulin therapy are more prone to depression than those undergoing treatment only with oral formulations, this pattern being related to the greater complexity of the regimen and the need for multiple daily injections [99,100,101].
The convenience or complexity of drug delivery devices can also influence adherence. Some studies have shown that with the use of an insulin pen instead of the use of a bottle and syringe in patients with DM2, adherence, glycemic control and lower incidence rates of hypoglycemia were obtained in the groups of patients treated with insulin pens instead of syringes [77,90]. In the case of oral formulations, patients who were previously treated with only one drug and who need additional therapy show significantly greater adherence when the regimen comprises fixed-dose combined therapy compared to combined therapy using each of the agents separately; similarly, patients who receive combination therapy and who switch to fixed-dose combination regimens also adhere to the treatment plan more strictly after the switch [102]. The most recent oral formulations (i-DPP4, i-SGLT−2), with greater therapeutic efficacy, greater dosage convenience (possibility of a single daily dose) and better tolerability by patients, are associated with higher rates of persistence in the treatment of DM2 than with metformin and sulfonylureas, and the route of administration also influences this parameter (GLP−1 agonists, although being of the new generation, are administered subcutaneously and, given the i-DPP4 and SGLT−2, they have less persistence in the treatment) [93,103].
One of the aspects that is closely associated with the lesser efficacy of oral antidiabetic therapy is related to forgetting to take the medications, leading to fluctuations in glycemic levels, being important at this level the reinforcement of the educational component by health professionals [104].
3.6.4. Costs of Treatment
Health costs must be analyzed in two ways: direct costs, which refer to the amount paid by patients when purchasing therapy, and which have been consistently associated with non-adherence in all conditions of treatment of chronic diseases, especially at higher purchase values; and indirect costs, when a disease that is poorly controlled, resulting from inadequate patient adherence to treatment, is closely associated with an increased probability of needing hospital admission and more costly therapeutic approaches [105,106,107].
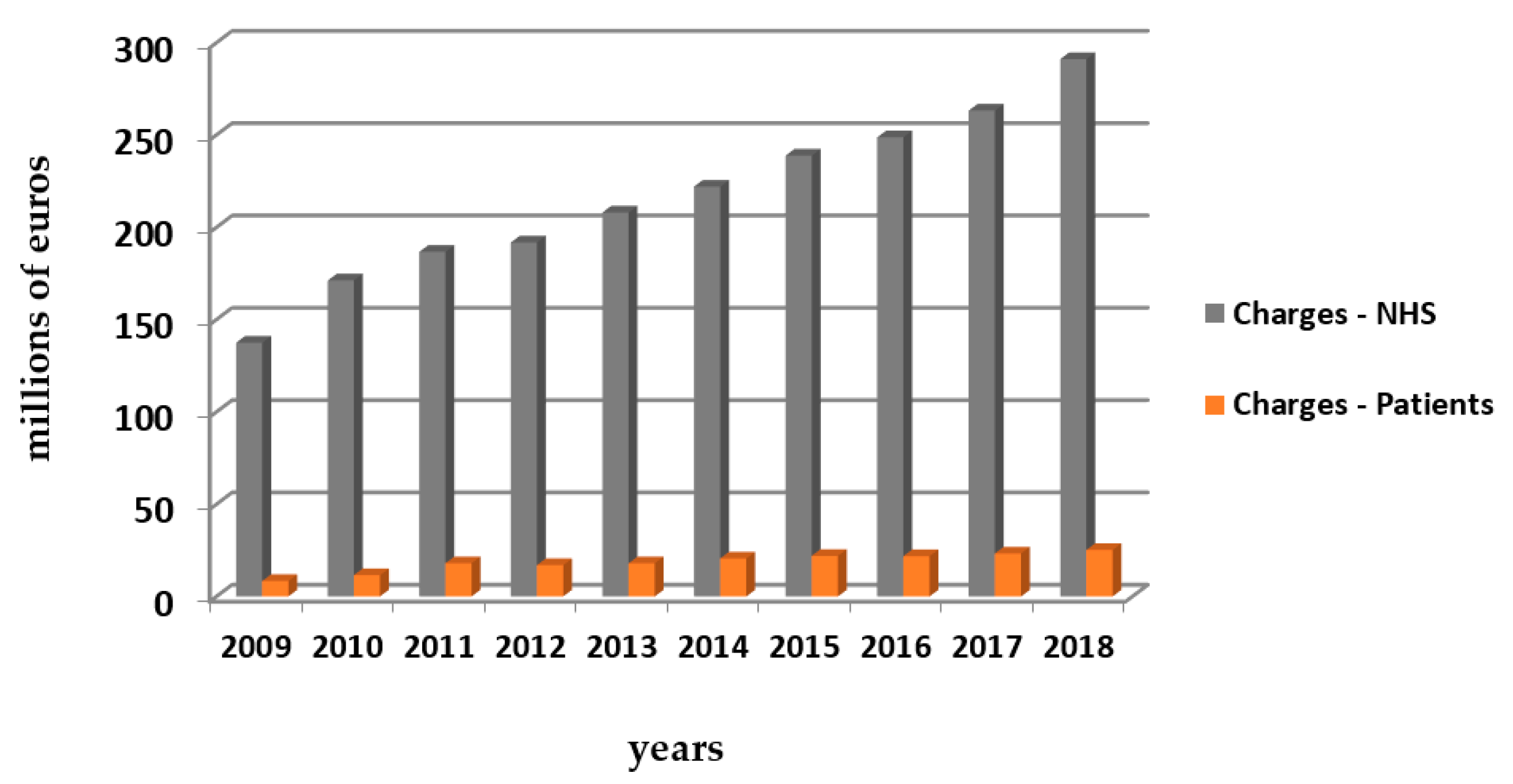
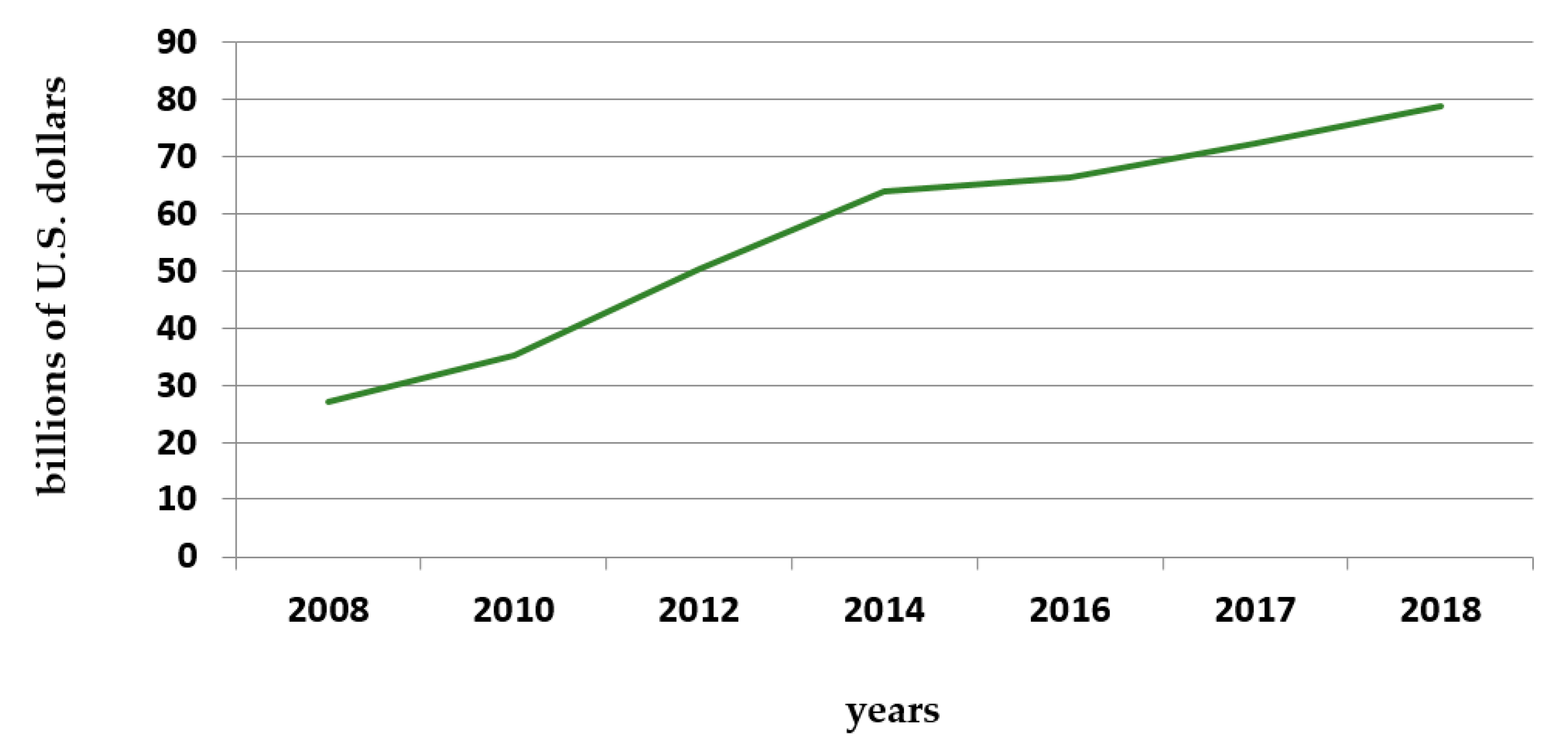
Diabetes caused at least USD 760 billion in health expenditures in 2019, comprising 10% of total spending on adults [8]. The following graphs (Figure 6 and Figure 7) provide an idea about the costs of antidiabetic medication in Portugal and worldwide.
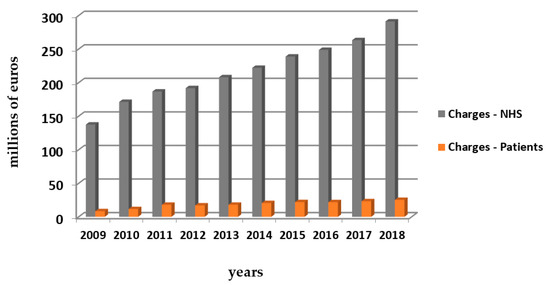
Figure 6.
Outpatient sales of insulin and non-insulin drugs within the NHS in Continental Portugal—in value (millions of euros) since 2009 to 2018. Source: Raposo J., 2020 [13].
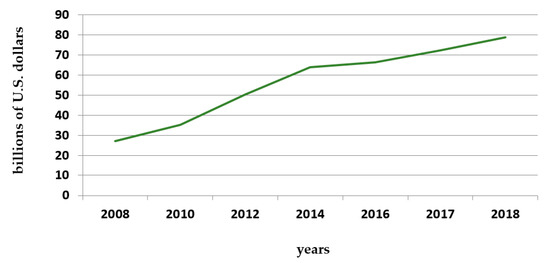
Figure 7.
Global pharmaceutical revenue of anti-diabetic products in billions of U.S. dollars from 2008 to 2018. Source: Mikulic 2020—Statistics & Facts [105].
When defining government strategies in the health area, the correlation between the increase in non-adherence and the higher prevalence of the disease must be considered, so that the available resources are managed more efficiently, assuming patient education, with strategies of behavioral intervention, a fundamental role in this issue [107,108].
3.6.5. Beliefs Regarding Medication
Health behaviors can be affected both by patients’ literacy and their self-management capacity. Cognitive and social skills are directly related to the motivation of patients, influencing it, which is decisive in the ability to assimilate knowledge, which, in turn, contributes to a better understanding of the intended therapeutic goals [109]. Many patients have markedly negative or highly skeptical beliefs about therapy, often fearing that the long-term risks will outweigh any likely benefits [110,111].
In patients with DM2, concerns about poor adherence to the defined therapeutic regimen demand from health professionals an objective approach in relation to the clear demonstration of benefits for the patient through correct adherence, as well as the identification of barriers/socio-psychological factors that may negatively influence strict compliance with the established regime, allowing assertive action in this regard [109,110,111].
3.6.6. Trust in Health Professionals
Optimum adherence to treatment with hypoglycemic drugs is closely related to a trusting relationship between health professionals and patients [112,113]. The consonance/complicity between patient and physician (a patient’s feeling that their needs and concerns, during medical consultations, were heard and attended to) predicts the quality of adherence to pharmacological treatment in the long term, contributing to the prevention of complications and, when established, to a greater effectiveness in their control [114,115].
Pharmacists also assume a differentiating role in this domain, both in a hospital context and in a community environment, interpreting the medical prescription by the identification of any non-compliance with the prescribed medication (if it appears to be unsafe to use with a patient’s other medications, if the dose or duration is inappropriate or if the cost is overly burdensome). They have the ability to recommend appropriate alternatives by reaching out to the prescriber, as well as when performing therapeutic reconciliation, ensuring the efficacy and safety of the defined therapeutic regimens. They can play an integral role in diabetes control, either by educating patients about lifestyle changes and medications, or even managing the general state of the disease [116,117].
Nurses are also extremely important in this dynamic. Its intervention includes not only instruction in the administration of medications and treatments (for example, in the “diabetic foot”), but also psychological support so that patients can be better able to face the daily challenges of a chronic condition [118].
Education is the cornerstone of health. The International Diabetes Federation (IDF) advocates the sharing of information and continuously improved practices in the field of diabetes in order to equip healthcare professionals with the best understanding and skills to be able to provide optimal care and support to their patients.
4. Discussion
Focusing on potentially modifiable aspects in the approach to the treatment and control of diabetes, it is possible to see that the behavioral, motivational and self-care components of the patient, combined with their cognitive capacity and the wealth of information they have at their disposal, undoubtedly contribute to their success of the pharmacological and non-pharmacological therapeutics instituted [119,120,121]. In addition to aspects directly related to drug therapy (the right drug, in the right dose, at the right time), it is essential to ensure a healthy lifestyle (balanced diet with sugar restriction, adequate exercise, sleep hygiene, avoid the consumption of alcohol, smoking or consumption of illegal substances), so that the intended therapeutic effect is maximized, that acute exacerbations of the disease are prevented and, consequently, the incidence of morbidity and mortality is reduced. Although several studies have shown that adherence to treatment is associated with better control [122,123,124], almost 60% of patients with diabetes are unable to reach their glycemic goals, so it is essential to understand the factors associated with non-adherence, so that patient-focused strategies can be developed, enabling effective intervention by health professionals and thus reducing complications associated with uncontrolled diabetes and, on the other hand, the potential impact in terms of health expenditure.
Scientific advances in the development of new treatments and improvements in drug delivery systems, together with innovative technologies, can and should be used to help patients overcome some of the challenges associated with controlling the disease.
5. Conclusions
Diabetes is a pathology that has a strong psychological burden for its patients, both because of the need for thorough control of glycemic levels, implying strict adherence to the instituted therapeutic regimen, and because of the indispensability of adopting healthy lifestyle habits, due the side effects of disease and the therapy itself, as well as fears arising from acute clinical conditions (hypoglycemia).
More research is needed to promote a more effective discussion on the importance of investing in the social and behavioral component of the chronically ill, as also concluded in several recent studies. It is important to understand how patients live with chronic diseases such as DM2, the impact it has on their lives and how it can be minimized through the influence of behaviors, especially by the intervention of health professionals, combining this aspect with knowledge about the pathophysiology of DM2 and about the pharmacological characteristics of available therapies.
Health systems must evolve towards increasing efficiency of the services provided, guaranteeing all patients with the appropriate clinical, pharmaceutical and social follow-up to each need, as well as minimizing potential complications that could compromise the quality and life expectancy of patients, with natural implications in terms of economic expenditure.
Author Contributions
Conceptualization, A.L., F.R. and M.M.; methodology, A.L., C.D., F.R.; M.M., M.T.H. and S.M.; investigation, A.L., C.D., F.R.; M.M., M.T.H. and S.M.; resources, A.L., F.R.; M.M.; data curation, A.L.; writing—original draft preparation, A.L.; writing—review and editing, C.D., F.R.; M.M., M.T.H. and S.M.; supervision, F.R.; M.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Sokol, M.C.; McGuigan, K.A.; Verbrugge, R.R.; Epstein, R.S. Impact of Medication Adherence on Hospitalization Risk and Healthcare Cost. Med. Care 2005, 43, 521–530. [Google Scholar] [CrossRef]
- Whitley, B.E.; Kite, M.E. Principles of Research in Behavioral Science, 3rd ed.; Routledge: Oxfordshire, UK, 2013. [Google Scholar] [CrossRef]
- Grarup, N.; Sandholt, C.H.; Hansen, T.; Pedersen, O. Genetic susceptibility to type 2 diabetes and obesity: From genome-wide association studies to rare variants and beyond. Diabetologia 2014, 57, 1528–1541. [Google Scholar] [CrossRef]
- Katzung, B.G.; Masters, S.B.; Trevor, A.J. Basic and Clinical Pharmacology, 12th ed.; Mcgraw-Hill: New York, NY, USA, 2012. [Google Scholar]
- Bacha, F.; Lee, S.; Gungor, N.; Arslanian, S.A. From Pre-Diabetes to Type 2 Diabetes in Obese Youth: Pathophysiological characteristics along the spectrum of glucose dysregulation. Diabetes Care 2010, 33, 2225–2231. [Google Scholar] [CrossRef] [PubMed]
- Morello, C.M.; Chynoweth, M.; Kim, H.; Singh, R.F.; Hirsch, J.D. Strategies to Improve Medication Adherence Reported by Diabetes Patients and Caregivers: Results of a Taking Control of Your Diabetes Survey. Ann. Pharmacother. 2011, 45, 145–153. [Google Scholar] [CrossRef] [PubMed]
- Abate, N.; Chandalia, M. The impact of ethnicity on type 2 diabetes. J. Diabetes Its Complicat. 2003, 17, 39–58. [Google Scholar] [CrossRef]
- International Diabetes Federation. IDF Diabetes Atlas, 9th ed.; International Diabetes Federation: Brussels, Belgium, 2019. [Google Scholar]
- Kaiser, A.B.; Zhang, N.; van der Pluijm, W. Global Prevalence of Type 2 Diabetes over the Next Ten Years (2018–2028). Diabetes 2018, 67, 202. [Google Scholar] [CrossRef]
- The Emerging Risk Factors Collaboration. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: A collaborative meta-analysis of 102 prospective studies. Lancet 2010, 375, 2215–2222. [Google Scholar] [CrossRef]
- Gæde, P.; Vedel, P.; Larsen, N.; Jensen, G.V.H.; Parving, H.-H.; Pedersen, O. Multifactorial Intervention and Cardiovascular Disease in Patients with Type 2 Diabetes. N. Engl. J. Med. 2003, 348, 383–393. [Google Scholar] [CrossRef]
- Zhang, P.; Lu, J.; Jing, Y.; Tang, S.; Zhu, D.; Bi, Y. Global epidemiology of diabetic foot ulceration: A systematic review and meta-analysis. Ann. Med. 2016, 49, 106–116. [Google Scholar] [CrossRef] [PubMed]
- Raposo, J. Diabetes: Factos e Números 2016, 2017 e 2018. Rev. Port. Diabetes 2020, 15, 19–27. [Google Scholar]
- Fortington, L.; Geertzen, J.; van Netten, J.J.; Postema, K.; Rommers, G.; Dijkstra, P. Short and Long Term Mortality Rates after a Lower Limb Amputation. Eur. J. Vasc. Endovasc. Surg. 2013, 46, 124–131. [Google Scholar] [CrossRef] [PubMed]
- AB Khan, M.; Hashim, M.J.; King, J.K.; Govender, R.D.; Mustafa, H.; Al Kaabi, J. Epidemiology of Type 2 Diabetes—Global Burden of Disease and Forecasted Trends. J. Epidemiol. Glob. Health 2019, 10, 107–111. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.A.B.; Hashim, M.J.; King, J.K.; Govender, R.D.; Mustafa, H.; Al Kaabi, J. Trends in the incidence of diabetes mellitus: Results from the Global Burden of Disease Study 2017 and implications for diabetes mellitus prevention. BMC Public Health 2020, 20, 1415. [Google Scholar] [CrossRef]
- Meo, S.A.; Sheikh, S.A.; Sattar, K.; Akram, A.; Hassan, A.; Meo, A.S.; Usmani, A.M.; Qalbani, E.; Ullah, A. Prevalence of Type 2 Diabetes Mellitus Among Men in the Middle East: A Retrospective Study. Am. J. Mens Health 2019, 13, 1557988319848577. [Google Scholar] [CrossRef] [PubMed]
- Noshad, S.; Afarideh, M.; Heidari, B.; Mechanick, J.I.; Esteghamati, A. Diabetes Care in Iran: Where We Stand and Where We Are Headed. Ann. Glob. Health 2015, 81, 839–850. [Google Scholar] [CrossRef] [PubMed]
- Moini, J. (Ed.) Epidemiology of Diabetes; Chapter 3: Pathophysiology of Diabetes; Elsevier: Amsterdam, The Netherlands, 2019. [Google Scholar]
- Wing, R.R.; Goldstein, M.G.; Acton, K.J.; Birch, L.L.; Jakicic, J.M.; Sallis, J.F.; Smith-West, D.; Jeffery, R.W.; Surwit, R.S. Behavioral Science Research in Diabetes: Lifestyle changes related to obesity, eating behavior, and physical activity. Diabetes Care 2001, 24, 117–123. [Google Scholar] [CrossRef] [PubMed]
- Baethge, C.; Goldbeck-Wood, S.; Mertens, S. SANRA—A scale for the quality assessment of narrative review articles. Res. Integr. Peer Rev. 2019, 4, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Cragg, R. A Brief History of Diabetes. Available online: https://www.eyescreening.org.uk/userFiles/File/Conference%202017/2017%20BARS%20presentations/07%20Brief%20History%20of%20Diabetes.pdf; (accessed on 21 October 2021).
- Laios, K.; Karamanou, M.; Saridaki, Z.; Androutsos, G. Aretaeus of Cappadocia and the first description of diabetes. Hormones 2012, 11, 109–113. [Google Scholar] [CrossRef]
- Mandal, A. História do diabetes. News-Medical. 2019. Available online: https://www.news-medical.net/health/History-of-Diabetes.aspx (accessed on 27 June 2021).
- Chast, F.; Slama, G. Apollinaire Bouchardat et le diabète. Hist. Sci. Med. 2007, 41, 287–301. (In French) [Google Scholar] [PubMed]
- Mazur, A. Why were “starvation diets” promoted for diabetes in the pre-insulin period? Nutr. J. 2011, 10, 23. [Google Scholar] [CrossRef]
- Lakhtakia, R. The History of Diabetes Mellitus. Sultan Qaboos Univ. Med. J. 2013, 13, 368–370. [Google Scholar] [CrossRef] [PubMed]
- Higuera, V. Medical News Today. Diabetes: Past Treatments, New Discoveries. 2020. Available online: https://www.medicalnewstoday.com/articles/317484 (accessed on 1 September 2019).
- Coleman, J.S. Foundations of Social Theory; Belknap Press of Harvard University: Cambridge, MA, USA, 1994. [Google Scholar]
- Michie, S.; West, R.; Campbell, R.; Brown, J.; Gainforth, H. ABC of Behaviour Change Theories; Silverback: Sutton, UK, 2014. [Google Scholar]
- Carey, R.N.; Connell, L.E.; Johnston, M.; Rothman, A.J.; de Bruin, M.; Kelly, M.P.; Michie, S. Behavior Change Techniques and Their Mechanisms of Action: A Synthesis of Links Described in Published Intervention Literature. Ann. Behav. Med. 2018, 53, 693–707. [Google Scholar] [CrossRef]
- Short, S.E.; Mollborn, S. Social determinants and health behaviors: Conceptual frames and empirical advances. Curr. Opin. Psychol. 2015, 5, 78–84. [Google Scholar] [CrossRef]
- Matthews, L.; Simpson, S.A. Evaluation of Behavior Change Interventions. In The Handbook of Behavior Change; Hamilton, K., Cameron, L.D., Hagger, M.S., Hankonen, N., Lintunen, T., Eds.; Cambridge University Press: Cambridge, UK, 2020. [Google Scholar]
- Green, D.; Ha, S.E.; Bullock, J.G. Enough Already about “Black Box” Experiments: Studying Mediation Is More Difficult than Most Scholars Suppose. Ann. Am. Acad. Political Soc. Sci. 2010, 628, 200–208. [Google Scholar] [CrossRef]
- Eiler, B.A.; Kallen, R.W.; Richardson, M.J. Interaction-dominant dynamics, timescale enslavement, and the emergence of social behavior. In Computational Social Psychology; Vallacher, R.R., Read, S.J., Nowak, A., Eds.; Taylor & Francis: Oxfordshire, UK, 2017; pp. 105–126. [Google Scholar] [CrossRef]
- Roe, R. What is wrong with mediators and moderators. Eur. Health Psychol. 2012, 14, 4–10. [Google Scholar]
- Hofmann, S.G.; Curtiss, J.E.; Hayes, S. Beyond linear mediation: Toward a dynamic network approach to study treatment processes. Clin. Psychol. Rev. 2020, 76, 101824. [Google Scholar] [CrossRef] [PubMed]
- Rickles, D. Causality in complex interventions. Med. Health Care Philos. 2008, 12, 77–90. [Google Scholar] [CrossRef]
- Meehl, P.E. Why summaries of research on psychological theories are often uninterpretable. Psychol. Rep. 1990, 66, 195–244. [Google Scholar] [CrossRef]
- Heino, M.; Knittle, K.; Noone, C.; Hasselman, F.; Hankonen, N. Studying Behaviour Change Mechanisms under Complexity. Behav. Sci. 2021, 11, 77. [Google Scholar] [CrossRef]
- Gomersall, T. Complex adaptive systems: A new approach for understanding health practices. Health Psychol. Rev. 2018, 12, 405–418. [Google Scholar] [CrossRef] [PubMed]
- Plsek, P.E.; Greenhalgh, T. Complexity science: The challenge of complexity in health care. BMJ 2001, 323, 625–628. [Google Scholar] [CrossRef] [PubMed]
- Axelrod, R.; Cohen, M. Harnessing Complexity: Organizational Implications of a Scientific Frontier; Free Press: New York, NY, USA, 2001. [Google Scholar]
- Stacey, R. Strategic Management and Organisational Dynamics: The Challenge of Complexity to Ways of Thinking about Organisations; Financial Times/Prentice Hall: Hoboken, NJ, USA, 2011. [Google Scholar]
- Pype, P.; Mertens, F.; Helewaut, F.; Krystallidou, D. Healthcare teams as complex adaptive systems: Understanding team behaviour through team members’ perception of interpersonal interaction. BMC Health Serv. Res. 2018, 18, 570. [Google Scholar] [CrossRef]
- Stumvoll, M.; Goldstein, B.J.; van Haeften, T.W. Type 2 diabetes: Principles of pathogenesis and therapy. Lancet 2005, 365, 1333–1346. [Google Scholar] [CrossRef]
- Cerf, M.E. Beta Cell Dysfunction and Insulin Resistance. Front. Endocrinol. 2013, 4, 37. [Google Scholar] [CrossRef]
- Freeman, A.M.; Pennings, N. Insulin Resistance; StatPearls Publishing: Treasure Island, FL, USA, 2021. [Google Scholar]
- Saisho, Y. β-cell dysfunction: Its critical role in prevention and management of type 2 diabetes. World J. Diabetes 2015, 6, 109–124. [Google Scholar] [CrossRef]
- Christensen, A.; Gannon, M. The Beta Cell in Type 2 Diabetes. Curr. Diabetes Rep. 2019, 19, 81. [Google Scholar] [CrossRef] [PubMed]
- Wells, B.; DiPiro, J.; Schwinghammer, T.; Dipiro, C. Manual de Farmacoterapia; McGraw Hill Eduaction: New York, NY, USA, 2016. [Google Scholar]
- Leiter, L.A.; Lundman, P.; da Silva, P.M.; Drexel, H.; Jünger, C.; Gitt, A.K. on behalf of the DYSIS investigators Persistent lipid abnormalities in statin-treated patients with diabetes mellitus in Europe and Canada: Results of the Dyslipidaemia International Study. Diabet. Med. 2011, 28, 1343–1351. [Google Scholar] [CrossRef]
- Zheng, Y.; Ley, S.; Hu, F.B. Global aetiology and epidemiology of type 2 diabetes mellitus and its complications. Nat. Rev. Endocrinol. 2017, 14, 88–98. [Google Scholar] [CrossRef]
- Caramona, M.; Vitória, I.; Teixeira, M.; Alcobia, A.; Almeida, P.; Horta, R.; Reis, L.; Grupo de Farmacoterapia da Ordem dos Farmacêuticos. Normas de Orientação Terapêutica; Cadaval Gráfica: Terrugem, Portugal, 2012. [Google Scholar]
- Eckstein, M.L.; Williams, D.M.; O’Neil, L.; Hayes, J.; Stephens, J.W.; Bracken, R. Physical exercise and non-insulin glucose-lowering therapies in the management of Type 2 diabetes mellitus: A clinical review. Diabet. Med. 2018, 36, 349–358. [Google Scholar] [CrossRef]
- Aune, D.; Giovannucci, E.; Boffetta, P.; Fadnes, L.T.; Keum, N.; Norat, T.; Greenwood, D.C.; Riboli, E.; Vatten, L.J.; Tonstad, S. Fruit and vegetable intake and the risk of cardiovascular disease, total cancer and all-cause mortality—A systematic review and dose-response meta-analysis of prospective studies. Int. J. Epidemiol. 2017, 46, 1029–1056. [Google Scholar] [CrossRef] [PubMed]
- Knowler, W.C.; Barrett-Connor, E.; Fowler, S.E.; Hamman, R.F.; Lachin, J.; Walker, E.A.; Nathan, D.M. Reduction in the Incidence of Type 2 Diabetes with Lifestyle Intervention or Metformin. N. Engl. J. Med. 2002, 346, 393–403. [Google Scholar] [CrossRef] [PubMed]
- Warburton, D.E.; Charlesworth, S.; Ivey, A.; Nettlefold, L.; Bredin, S.S. A systematic review of the evidence for Canada’s Physical Activity Guidelines for Adults. Int. J. Behav. Nutr. Phys. Act. 2010, 7, 39. [Google Scholar] [CrossRef]
- Knowler, W.C.; Fowler, S.E.; Hamman, R.F.; Christophi, C.A.; Hoffman, H.J.; Brenneman, A.T.; Brown-Friday, J.O.; Goldberg, R.; Venditti, E.; Nathan, D.M.; et al. 10-year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study. Lancet 2009, 374, 1677–1686. [Google Scholar] [CrossRef] [PubMed]
- Balk, E.M.; Earley, A.; Raman, G.; Avendano, E.A.; Pittas, A.G.; Remington, P.L. Combined Diet and Physical Activity Promotion Programs to Prevent Type 2 Diabetes Among Persons at Increased Risk: A Systematic Review for the Community Preventive Services Task Force. Ann. Intern. Med. 2015, 163, 437–451. [Google Scholar] [CrossRef]
- Hamman, R.F.; Wing, R.R.; Edelstein, S.L.; Lachin, J.M.; Bray, G.A.; Delahanty, L.; Hoskin, M.; Kriska, A.M.; Mayer-Davis, E.J.; Pi-Sunyer, X.; et al. Effect of Weight Loss with Lifestyle Intervention on Risk of Diabetes. Diabetes Care 2006, 29, 2102–2107. [Google Scholar] [CrossRef] [PubMed]
- Mirahmadizadeh, A.; Khorshidsavar, H.; Seif, M.; Sharifi, M.H. Adherence to Medication, Diet and Physical Activity and the Associated Factors Amongst Patients with Type 2 Diabetes. Diabetes Ther. 2020, 11, 479–494. [Google Scholar] [CrossRef]
- Kirkman, M.S.; Rowan-Martin, M.T.; Levin, R.; Fonseca, V.A.; Schmittdiel, J.A.; Herman, W.H.; Aubert, R.E. Determinants of Adherence to Diabetes Medications: Findings from a Large Pharmacy Claims Database. Diabetes Care 2015, 38, 604–609. [Google Scholar] [CrossRef]
- Capoccia, K.L.; Odegard, P.S.; Letassy, N. Medication Adherence with Diabetes Medication. Diabetes Educ. 2015, 42, 34–71. [Google Scholar] [CrossRef]
- Kisa, A.; Sabaté, E.; Nuño-Solinís, R. Adherence to Long-Term Therapies: Evidence for Action; World Health Organization: Geneva, Switzerland, 2003. [Google Scholar]
- SPD National Recommendations for the Treatment of Hyperglycemia in Type 2 Diabetes—Update Based in the ADA/EASD JointPositionStatement. Available online: http://www.revportdiabetes.com/wp-content/uploads/2019/01/RPD-DEzembro-2018-Recomenda%C3%A7%C3%B5es-p%C3%A1gs-154-180.pdf (accessed on 21 October 2021).
- Mayberry, L.S.; Bergner, E.M.; Chakkalakal, R.J.; Elasy, T.A.; Osborn, C.Y. Self-Care Disparities Among Adults with Type 2 Diabetes in the USA. Curr. Diabetes Rep. 2016, 16, 1–13. [Google Scholar] [CrossRef]
- Rolnick, S.J.; Pawloski, P.; Hedblom, B.D.; Asche, S.E.; Bruzek, R.J. Patient Characteristics Associated with Medication Adherence. Clin. Med. Res. 2013, 11, 54–65. [Google Scholar] [CrossRef]
- Berkowitz, S.A.; Seligman, H.K.; Choudhry, N.K. Treat or Eat: Food Insecurity, Cost-related Medication Underuse, and Unmet Needs. Am. J. Med. 2014, 127, 303–310.e3. [Google Scholar] [CrossRef] [PubMed]
- Demoz, G.T.; Wahdey, S.; Bahrey, D.; Kahsay, H.; Woldu, G.; Niriayo, Y.L.; Collier, A. Predictors of poor adherence to antidiabetic therapy in patients with type 2 diabetes: A cross-sectional study insight from Ethiopia. Diabetol. Metab. Syndr. 2020, 12, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Guerci, B.; Chanan, N.; Kaur, S.; Jasso-Mosqueda, J.G.; Lew, E. Lack of Treatment Persistence and Treatment Nonadherence as Barriers to Glycaemic Control in Patients with Type 2 Diabetes. Diabetes Ther. 2019, 10, 437–449. [Google Scholar] [CrossRef] [PubMed]
- McSharry, J.; Byrne, M.; Casey, B.; Dinneen, S.F.; Fredrix, M.; Hynes, L.; Lake, A.J.; Morrissey, E. Behaviour change in diabetes: Behavioural science advancements to support the use of theory. Diabet. Med. 2019, 37, 455–463. [Google Scholar] [CrossRef]
- Evangelista, L.S.; Shinnick, M.A. What do we know about adherence and self-care? J. Cardiovasc. Nurs. 2008, 23, 250–257. [Google Scholar] [CrossRef] [PubMed]
- Fisher, J.D.; Fisher, W.A.; Amico, K.R.; Harman, J.J. An information-motivation-behavioral skills model of adherence to antiretroviral therapy. Health Psychol. 2006, 25, 462–473. [Google Scholar] [CrossRef]
- Klonoff, D.C. Behavioral Theory: The Missing Ingredient for Digital Health Tools to Change Behavior and Increase Adherence. J. Diabetes Sci. Technol. 2018, 13, 276–281. [Google Scholar] [CrossRef] [PubMed]
- Polonsky, W.H.; Henry, R.R. Poor medication adherence in type 2 diabetes: Recognizing the scope of the problem and its key contributors. Patient Prefer. Adherence 2016, 10, 1299–1307. [Google Scholar] [CrossRef] [PubMed]
- Lauffenburger, J.C.; Lewey, J.; Jan, S.; Lee, J.; Ghazinouri, R.; Choudhry, N.K. Association of Potentially Modifiable Diabetes Care Factors with Glycemic Control in Patients with Insulin-Treated Type 2 Diabetes. JAMA Netw. Open 2020, 3, e1919645. [Google Scholar] [CrossRef] [PubMed]
- Gbadamosi, M.A.; Tlou, B. Modifiable risk factors associated with non-communicable diseases among adult outpatients in Manzini, Swaziland: A cross-sectional study. BMC Public Health 2020, 20, 665. [Google Scholar] [CrossRef] [PubMed]
- Horne, R.; Weinman, J.; Barber, N.; Elliott, R.; Morgan, M. Concordance, Adherence and Compliance in Medicine Taking; A Report for the National Coordinating Centre for NHS Service Delivery and Organisation R&D; National Coordinating Centre for NHS Service Delivery and Organisation R&D: London, UK, 2005. [Google Scholar]
- Gadkari, A.S.; McHorney, C.A. Medication nonfulfillment rates and reasons: Narrative systematic review. Curr. Med. Res. Opin. 2010, 26, 683–705. [Google Scholar] [CrossRef] [PubMed]
- Burrell, A.; Wong, P.; Ollendorf, D.; Fuldeore, M.; Roy, A.; Fairchild, C.; Cramer, J. PHP46 defining compliance/adherence and persistence: ISPOR special interest working group. Value Health 2005, 8, A194–A195. [Google Scholar] [CrossRef]
- Brawley, L.R.; Culos-Reed, S. Studying Adherence to Therapeutic Regimens: Overview, Theories, Recommendations. Control. Clin. Trials 2000, 21, S156–S163. [Google Scholar] [CrossRef]
- Holt, R.I.G.; Cockram, C.S.; Flyvbjerg, A.; Goldstein, B.J. (Eds.) Textbook of Diabetes, 4th ed.; Wiley-Blackwell: Hoboken, NJ, USA, 2010. [Google Scholar]
- Duarte, R. Inibidores da DPP-4 (Gliptinas)—10 anos depois (2007–2017). Rev. Port. Diabetes 2017, 12, 62–67. [Google Scholar]
- Pape, E.; Nascimento, E.; Jordão, A. Fármacos na Diabetes; LIDEL: Lisboa, Portugal, 2019. [Google Scholar]
- Committee Physical Activity Guidelines Advisory. 2018 Physical Activity Guidelines Advisory Committee Scientific Report; Department of Health and Human Services: Washington, DC, USA, 2018.
- Cahn, A.; Miccoli, R.; Dardano, A.; del Prato, S. New forms of insulin and insulin therapies for the treatment of type 2 diabetes. Lancet Diabetes Endocrinol. 2015, 3, 638–652. [Google Scholar] [CrossRef]
- Mahmoodi, H.; Nahand, F.J.; Shaghaghi, A.; Shooshtari, S.; Jafarabadi, M.A.; Allahverdipour, H. Gender Based Cognitive Determinants of Medication Adherence in Older Adults with Chronic Conditions. Patient Prefer. Adherence 2019, 13, 1733–1744. [Google Scholar] [CrossRef]
- Brown, M.T.; Bussell, J.; Dutta, S.; Davis, K.; Strong, S.; Mathew, S. Medication Adherence: Truth and Consequences. Am. J. Med. Sci. 2016, 351, 387–399. [Google Scholar] [CrossRef] [PubMed]
- Davis, S.N.; Wei, W.; Garg, S. Clinical Impact of Initiating Insulin Glargine Therapy with Disposable Pen Ve;rsus Vial in Patients with Type 2 Diabetes Mellitus in a Managed Care Setting. Endocr. Pract. 2011, 17, 845–852. [Google Scholar] [CrossRef] [PubMed]
- Anderbro, T.; Amsberg, S.; Adamson, U.; Bolinder, J.; Lins, P.-E.; Wredling, R.; Moberg, E.; Lisspers, J.; Johansson, U.-B. Fear of hypoglycaemia in adults with Type 1 diabetes. Diabet. Med. 2010, 27, 1151–1158. [Google Scholar] [CrossRef] [PubMed]
- Walz, L.; Pettersson, B.; Rosenqvist, U.; Deleskog, A.; Journath, G.; Wändell, P. Impact of symptomatic hypoglycemia on medication adherence, patient satisfaction with treatment, and glycemic control in patients with type 2 diabetes. Patient Prefer. Adherence 2014, 8, 593–601. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Jermendy, G.; Kiss, Z.; Rokszin, G.; Abonyi-Tóth, Z.; Wittmann, I.; Kempler, P. Persistence to Treatment with Novel Antidiabetic Drugs (Dipeptidyl Peptidase-4 Inhibitors, Sodium-Glucose Co-Transporter-2 Inhibitors, and Glucagon-Like Peptide-1 Receptor Agonists) in People with Type 2 Diabetes: A Nationwide Cohort Study. Diabetes Ther. 2018, 9, 2133–2141. [Google Scholar] [CrossRef] [PubMed]
- Lopez, J.; Annunziata, K.; Bailey, R.; E Morisky, D.; Rupnow, M. Impact of hypoglycemia on patients with type 2 diabetes mellitus and their quality of life, work productivity, and medication adherence. Patient Prefer. Adherence 2014, 8, 683–692. [Google Scholar] [CrossRef] [PubMed]
- García-Pérez, L.-E.; Álvarez, M.; Dilla, T.; Gil-Guillén, V.F.; Orozco-Beltran, D. Adherence to Therapies in Patients with Type 2 Diabetes. Diabetes Ther. 2013, 4, 175–194. [Google Scholar] [CrossRef] [PubMed]
- Moghissi, E. Management of Type 2 Diabetes Mellitus in Older Patients: Current and Emerging Treatment Options. Diabetes Ther. 2013, 4, 239–256. [Google Scholar] [CrossRef] [PubMed]
- Melikian, C.; White, T.; Vanderplas, A.; Dezii, C.M.; Chang, E. Adherence to oral antidiabetic therapy in a managed care organization: A comparison of monotherapy, combination therapy, and fixed-dose combination therapy. Clin. Ther. 2002, 24, 460–467. [Google Scholar] [CrossRef]
- Claxton, A.J.; Cramer, J.; Pierce, C. A systematic review of the associations between dose regimens and medication compliance. Clin. Ther. 2001, 23, 1296–1310. [Google Scholar] [CrossRef]
- Bădescu, S.V.; Tătaru, C.; Kobylinska, L.; Georgescu, E.L.; Zahiu, D.M.; Zagrean, A.-M.; Zăgrean, L. The association between Diabetes mellitus and Depression. J. Med. Life 2016, 9, 120–125. [Google Scholar]
- Holt, R.I.G.; de Groot, M.; Golden, S.H. Diabetes and Depression. Curr. Diabetes Rep. 2014, 14, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Hasanovic, E.; Trifunovic, N.; Dzambo, I.; Erkocevic, H.; Cemerlic, A.; Jatic, Z.; Kulenovic, A.D. The Association among Glycemic Control and Depression Symptoms in Patients with Type 2 Diabetes. Mater. Soc. Med. 2020, 32, 177–182. [Google Scholar] [CrossRef] [PubMed]
- Han, S.; Iglay, K.; Davies, M.J.; Zhang, Q.; Radican, L. Glycemic effectiveness and medication adherence with fixed-dose combination or coadministered dual therapy of antihyperglycemic regimens: A meta-analysis. Curr. Med. Res. Opin. 2012, 28, 969–977. [Google Scholar] [CrossRef]
- Khunti, N.; Khunti, N.; Khunti, K. Adherence to type 2 diabetes management. Br. J. Diabetes Vasc. Dis. 2019, 19, 99–104. [Google Scholar] [CrossRef]
- Sefah, I.A.; Okotah, A.; Afriyie, D.K.; Amponsah, S.K. Adherence to Oral Hypoglycemic Drugs among Type 2 Diabetic Patients in a Resource-Poor Setting. Int. J. Appl. Basic Med. Res. 2020, 10, 102–109. [Google Scholar]
- Mikulic, M. Statistics & Facts, Global Pharmaceutical, Industry; Statista: Hamburg, Germany, 2020. [Google Scholar]
- Osterberg, L.; Blaschke, T. Adherence to Medication. N. Engl. J. Med. 2005, 353, 487–497. [Google Scholar] [CrossRef] [PubMed]
- Cutler, R.L.; Fernandez-Llimos, F.; Frommer, M.; Benrimoj, C.; Garcia-Cardenas, V. Economic impact of medication non-adherence by disease groups: A systematic review. BMJ Open 2018, 8, e016982. [Google Scholar] [CrossRef] [PubMed]
- Turcu-Stiolica, A.; Subtirelu, M.-S.; Taerel, A.-E.; Boboia, A.; Berbecaru-Iovan, A. Analysis of Financial Losses due to Poor Adherence of Patients with Chronic Diseases and Their Impact on Health Economics. In Financial Management from an Emerging Market Perspective; IntechOpen: London, UK, 2018. [Google Scholar] [CrossRef]
- Aikens, J.E.; Piette, J.D. Diabetic Patients’ Medication Underuse, Illness Outcomes, and Beliefs About Antihyperglycemic and Antihypertensive Treatments. Diabetes Care 2008, 32, 19–24. [Google Scholar] [CrossRef]
- Shahin, W.; A Kennedy, G.; Stupans, I. The impact of personal and cultural beliefs on medication adherence of patients with chronic illnesses: A systematic review. Patient Prefer. Adherence 2019, 13, 1019–1035. [Google Scholar] [CrossRef] [PubMed]
- Straßner, C.; Mahler, C.; Strauss, B.; Wehrmann, U.; Krug, K.; Szecsenyi, J.; Haefeli, W.E.; Seidling, H.M. Medication beliefs and use of medication lists—Is there a connection? Results from a before-and-after study in Germany. BMC Geriatr. 2020, 20, 116. [Google Scholar] [CrossRef]
- Nasir, N.M.; Ariffin, F.; Yasin, S.M. Physician-patient interaction satisfaction and its influence on medication adherence and type-2 diabetic control in a primary care setting. Med. J. Malays. 2018, 73, 163–169. [Google Scholar]
- Kerse, N.; Buetow, S.; Iii, A.G.M.; Young, G.; Coster, G.; Arroll, B. Physician-Patient Relationship and Medication Compliance: A Primary Care Investigation. Ann. Fam. Med. 2004, 2, 455–461. [Google Scholar] [CrossRef] [PubMed]
- Viswanathan, M.; Golin, C.E.; Jones, C.D.; Ashok, M.; Blalock, S.J.; Wines, R.C.; Coker-Schwimmer, E.J.; Rosen, D.L.; Sista, P.; Lohr, K.N. Interventions to Improve Adherence to Self-administered Medications for Chronic Diseases in the United States. Ann. Intern. Med. 2012, 157, 785–795. [Google Scholar] [CrossRef]
- Soto, C.; Strain, W.D. Tackling clinical inertia: Use of coproduction to improve patient engagement. J. Diabetes 2018, 10, 942–947. [Google Scholar] [CrossRef]
- Werble, C. Health Policy Brief: Pharmacy Benefit Managers. Health Aff. J. 2017. [Google Scholar] [CrossRef]
- Carroll, A.E. The Unsung Role of the Pharmacist in Patient Health. The New York Times, 2019. Available online: https://www.nytimes.com/2019/01/28/upshot/pharmacists-drugs-health-unsung-role.html (accessed on 21 September 2021).
- Shin, L.; Bowling, F.L.; Armstrong, D.G.; Boulton, A.J. Saving the Diabetic Foot During the COVID-19 Pandemic: A Tale of Two Cities. Diabetes Care 2020, 43, 1704–1709. [Google Scholar] [CrossRef] [PubMed]
- Benkel, I.; Arnby, M.; Molander, U. Living with a chronic disease: A quantitative study of the views of patients with a chronic disease on the change in their life situation. SAGE Open Med. 2020, 8. [Google Scholar] [CrossRef]
- Reynolds, R.; Dennis, S.; Hasan, I.; Slewa, J.; Chen, W.; Tian, D.; Bobba, S.; Zwar, N. A systematic review of chronic disease management interventions in primary care. BMC Fam. Pract. 2018, 19, 11. [Google Scholar] [CrossRef] [PubMed]
- Trikkalinou, A.; Papazafiropoulou, A.K.; Melidonis, A. Type 2 diabetes and quality of life. World J. Diabetes 2017, 8, 120–129. [Google Scholar] [CrossRef] [PubMed]
- Gerland, H.-M.E.; Prell, T. Association Between the Health Locus of Control and Medication Adherence: An Observational, Cross-Sectional Study in Primary Care. Front. Med. 2021, 8. [Google Scholar] [CrossRef]
- Fernandez-Lazaro, C.I.; García-González, J.M.; Adams, D.P.; Fernandez-Lazaro, D.; Mielgo-Ayuso, J.; Caballero-Garcia, A.; Racionero, F.M.; Córdova, A.; Miron-Canelo, J.A. Adherence to treatment and related factors among patients with chronic conditions in primary care: A cross-sectional study. BMC Fam. Pract. 2019, 20, 132. [Google Scholar] [CrossRef] [PubMed]
- Scialli, A.R.; Saavedra, K.; Fugh-Berman, A. The Benefits and Risks of Adherence to Medical Therapy. J. Sci. Pract. Integr. 2021, 21386. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).