Analyzing Predictors of Control Measures and Psychosocial Problems Associated with COVID-19 Pandemic: Evidence from Eight Countries
Abstract
:1. Background
2. Methods
2.1. Study Design and Respondents
- What are the differences in accessibility of COVID-19-related information among the eight countries and how do they vary across socio-demographic factors?
- What are the differences in behavior/practices related to COVID-19 information among the eight countries and how do they vary across different socio-demographic factors?
- What are the differences in COVID-19-related knowledge among the eight countries and how do they vary across socio-demographic factors?
- What are the differences in COVID-19 related opinions among the eight countries and how do they vary across socio-demographic factors?
- What are the differences in psychological profile during COVID-19 among the eight countries and across different socio-demographic factors?
- What are the differences in susceptibility to COVID-19 among the eight countries under consideration and how do they vary across socio-demographic factors?
2.2. Instruments
2.3. Data Collection and Preprocessing
2.4. Scoring Metrics
2.5. Analysis
2.6. Coding and Environment
3. Results
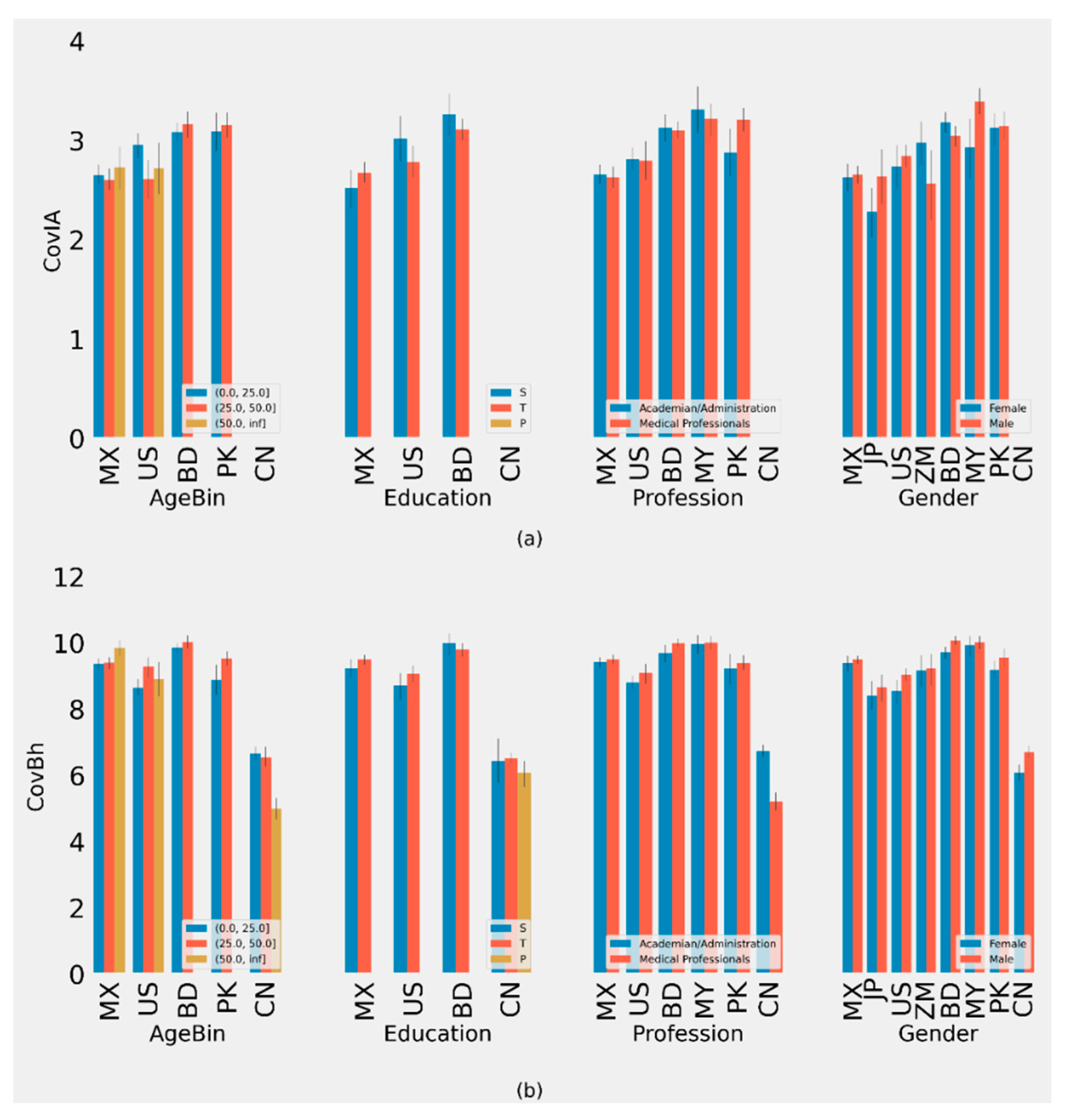
3.1. Accessibility of COVID-19 Related Information (CovIA)
3.2. Behavior/Practices Related to COVID-19 (CovBh)
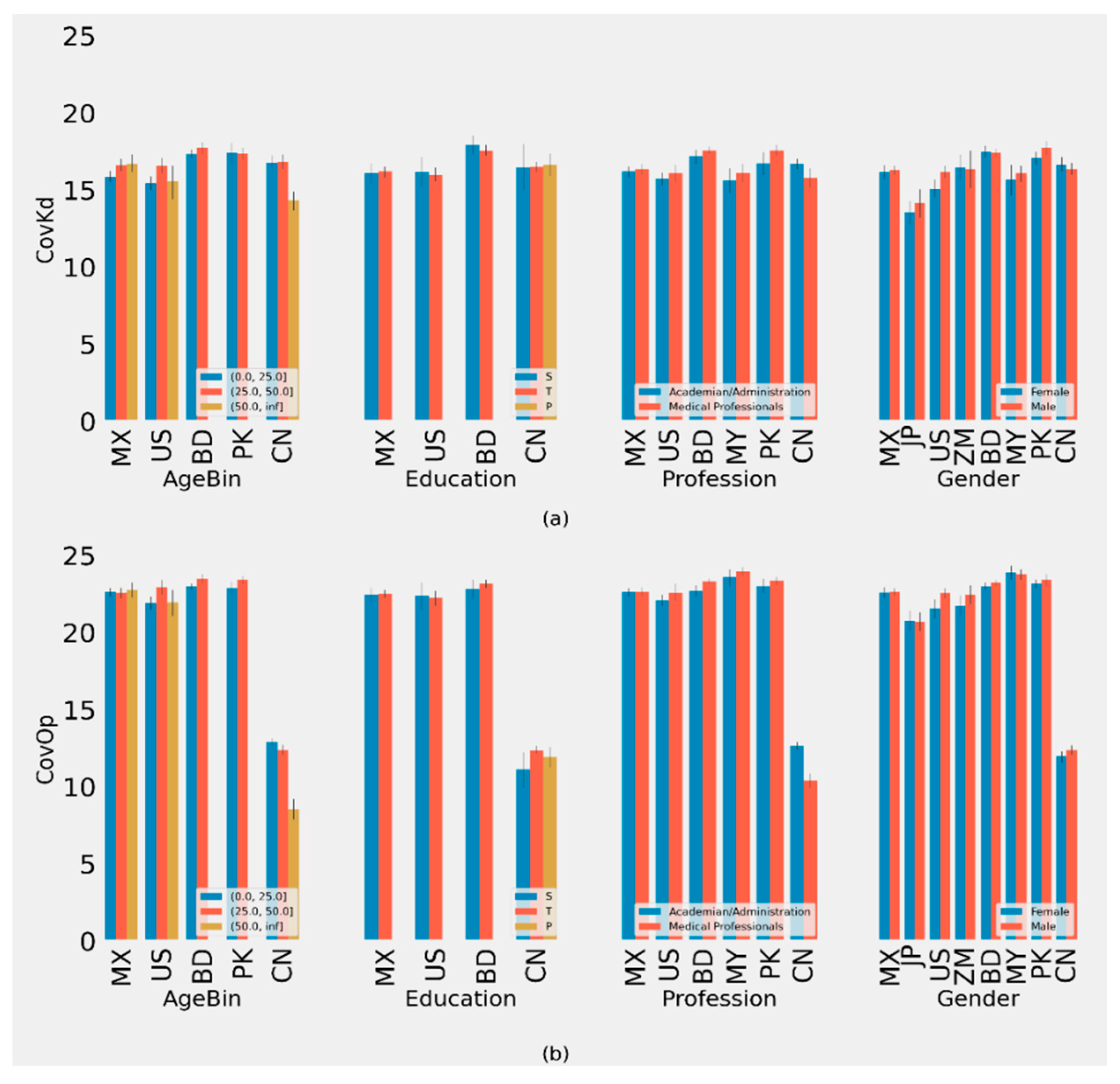
3.3. COVID-19 Related Knowledge Score (CovKd)
3.4. COVID-19 Related Opinion Score (CovOp)
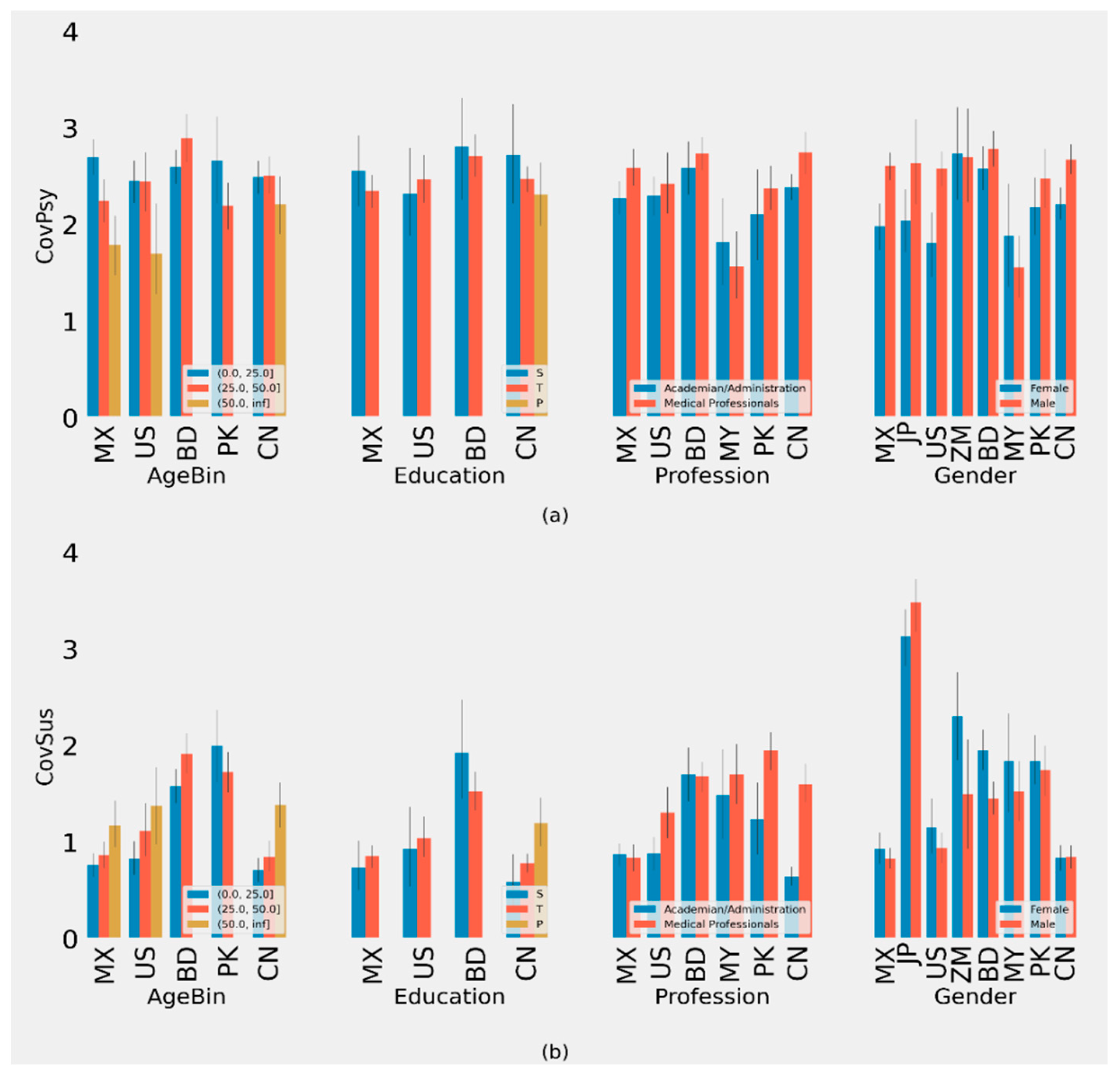
3.5. Analysis of Psychological Profile during COVID-19 (CovPsy)
3.6. Analysis of Susceptibility to COVID-19 (CovSus)
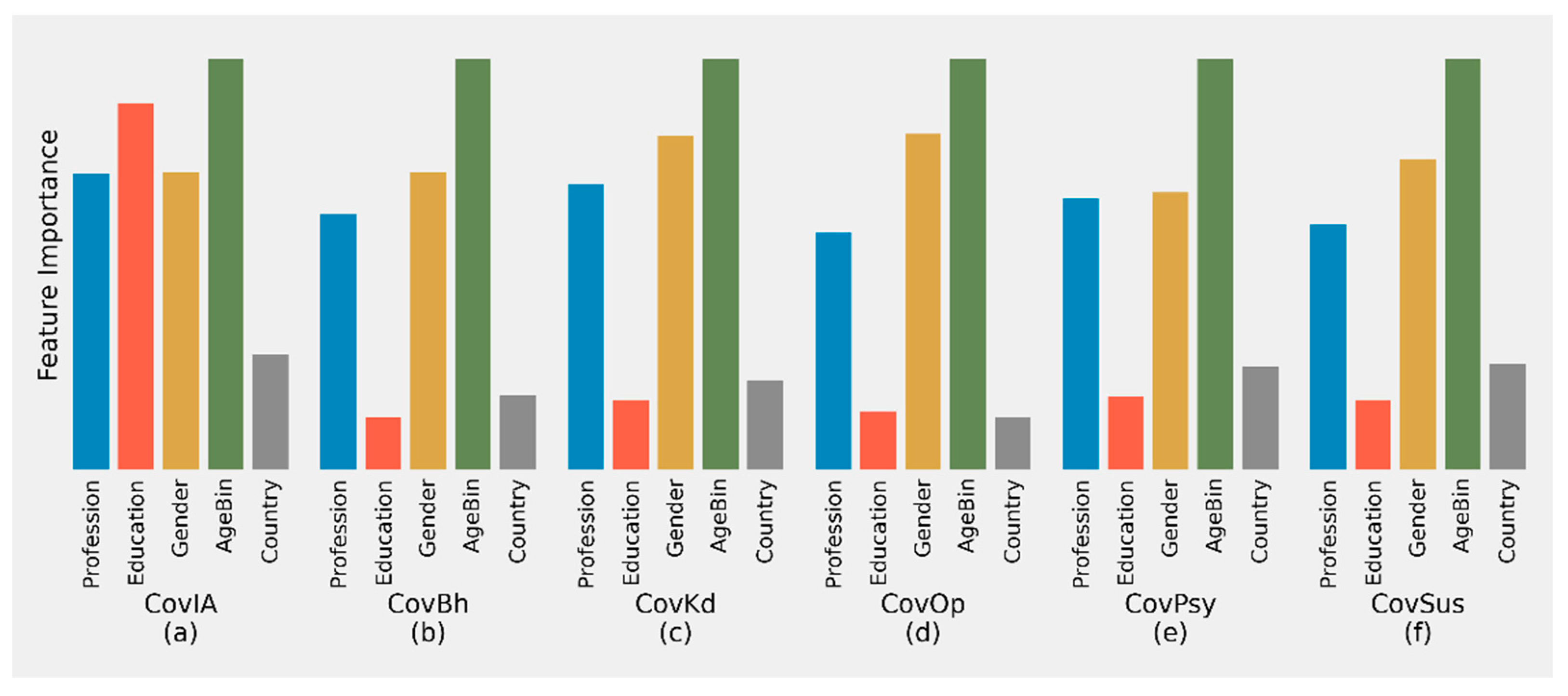
3.7. Feature Importance in Determining Different Scores
3.8. Correlation among Different Scores
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Afzal, M.S.; Khan, A.; Qureshi, U.U.R.; Saleem, S.; Saqib, M.A.N.; Shabbir, R.M.K.; Naveed, M.; Jabbar, M.; Zahoor, S.; Ahmed, H. Community-Based Assessment of Knowledge, Attitude, Practices and Risk Factors Regarding COVID-19 Among Pakistanis Residents During a Recent Outbreak: A Cross-Sectional Survey. J. Community Health 2020. [Google Scholar] [CrossRef] [PubMed]
- Erfani, A.; Shahriarirad, R.; Ranjbar, K.; Mirahmadizadeh, A.; Moghadami, M. Knowledge, Attitude and Practice toward the Novel Coronavirus (COVID-19) Outbreak: A Population-Based Survey in Iran. Bull World Health Organ 2020. [Google Scholar] [CrossRef]
- Isah, M.B.; Abdulsalam, M.; Bello, A.; Ibrahim, M.I.; Usman, A.; Nasir, A.; Abdulkadir, B.; Usman, A.R.; Matazu, K.I.; Sani, A.; et al. Coronavirus Disease 2019 (COVID-19): Knowledge, attitudes, practices (KAP) and misconceptions in the general population of Katsina State, Nigeria. MedRxiv 2020. [Google Scholar] [CrossRef]
- Alahdal, H.; Basingab, F.; Alotaibi, R. An analytical study on the awareness, attitude and practice during the COVID-19 pandemic in Riyadh, Saudi Arabia. J. Infect. Public Health 2020, 13, 1446–1452. [Google Scholar] [CrossRef]
- Spagnuolo, R.; Larussa, T.; Iannelli, C.; Cosco, C.; Nistico, E.; Manduci, E.; Bruno, A.; Boccuto, L.; Abenavoli, L.; Luzza, F.; et al. COVID-19 and Inflammatory Bowel Disease: Patient Knowledge and Perceptions in a Single Center Survey. Medicina 2020, 56, 407. [Google Scholar] [CrossRef]
- Czeisler, M.É.; Tynan, M.A.; Howard, M.E.; Honeycutt, S.; Fulmer, E.B.; Kidder, D.P.; Robbins, R.; Barger, L.K.; Facer-Childs, E.R.; Baldwin, G.; et al. Public Attitudes, Behaviors, and Beliefs Related to COVID-19, Stay-at-Home Orders, Nonessential Business Closures, and Public Health Guidance—United States, New York City, and Los Angeles, 5–12 May 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 751–758. [Google Scholar] [CrossRef]
- Fisher, K.A.; Barile, J.P.; Guerin, R.J.; Esschert, K.L.V.; Jeffers, A.; Tian, L.H.; Garcia-Williams, A.; Gurbaxani, B.; Thompson, W.W.; Prue, C.E. Factors Associated with Cloth Face Covering Use Among Adults During the COVID-19 Pandemic- United States, April and May 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 933–937. [Google Scholar] [CrossRef]
- Peng, Y.; Pei, C.; Zheng, Y.; Wang, J.; Zhang, K.; Zheng, Z.; Zhu, P. A cross-sectional survey of knowledge, attitude and practice associated with COVID-19 among undergraduate students in China. BMC Public Health 2020, 20, 1292. [Google Scholar] [CrossRef]
- Hager, E.; Odetokun, I.A.; Bolarinwa, O.; Zainab, A.; Okechukwu, O.; Al-Mustapha, A.I. Knowledge, attitude, and perceptions towards the 2019 Coronavirus Pandemic: A bi-national survey in Africa. PLoS ONE 2020, 15, e0236918. [Google Scholar] [CrossRef]
- Olum, R.; Kajjimu, J.; Kanyike, A.M.; Chekwech, G.; Wekha, G.; Nassozi, D.R.; Kemigisa, J.; Mulyamboga, P.; Muhoozi, O.K.; Nsenga, L.; et al. Perspective of Medical Students on the COVID-19 Pandemic: Survey of Nine Medical Schools in Uganda. JMIR Public Health Surveill. 2020, 6, e19847. [Google Scholar] [CrossRef]
- Saqlain, M.; Munir, M.M.; Rehman, S.U.; Gulzar, A.; Naz, S.; Ahmed, Z.; Tahir, A.H.; Mashhood, M. Knowledge, attitude, practice and perceived barriers among healthcare workers regarding COVID-19: A cross-sectional survey from Pakistan. J. Hosp. Infect. 2020, 105, 419–423. [Google Scholar] [CrossRef] [PubMed]
- Bhagavathula, A.S.; Aldhaleei, W.A.; Rahmani, J.; Mahabadi, M.A.; Bandari, D.K. Knowledge and Perceptions of COVID-19 Among Health Care Workers: Cross-Sectional Study. JMIR Public Health Surveill. 2020, 6, e19160. [Google Scholar] [CrossRef]
- Ahmed, N.; Shakoor, M.; Vohra, F.; Abduljabbar, T.; Mariam, Q.; Rehman, M.A. Knowledge, Awareness and Practice of Health care Professionals amid SARS-CoV-2, Corona Virus Disease Outbreak. Pak. J. Med. Sci. 2020, 36, S49–S56. [Google Scholar] [CrossRef] [PubMed]
- Roy, D.; Tripathy, S.; Kar, S.K.; Sharma, N.; Verma, S.K.; Kaushal, V. Study of knowledge, attitude, anxiety & perceived mental healthcare need in Indian population during COVID-19 pandemic. Asian J. Psychiatr. 2020, 51, 102083. [Google Scholar] [CrossRef]
- Alhaj, A.K.; Al-Saadi, T.; Mohammad, F.; Alabri, S. Neurosurgery Residents’ Perspective on COVID-19: Knowledge, Readiness, and Impact of this Pandemic. World Neurosurg. 2020, 139, e848–e858. [Google Scholar] [CrossRef]
- Newby, J.M.; O’Moore, K.; Tang, S.; Christensen, H.; Faasse, K. Acute mental health responses during the COVID-19 pandemic in Australia. PLoS ONE 2020, 15, e0236562. [Google Scholar] [CrossRef]
- Sallam, M.; Dababseh, D.; Yaseen, A.; Al-Haidar, A.; Ababneh, N.A.; Bakri, F.G.; Mahafzah, A. Conspiracy Beliefs Are Associated with Lower Knowledge and Higher Anxiety Levels Regarding COVID-19 among Students at the University of Jordan. Int. J. Environ. Res. Public Health 2020, 17, 4915. [Google Scholar] [CrossRef]
- Ricco, M.; Ferraro, P.; Gualerzi, G.; Ranzieri, S.; Bragazzi, N.L.; Balzarini, F.; Signorelli, C. Point-of-Care diagnostic of SARS-CoV-2: Knowledge, attitudes, and perceptions (KAP) of medical workforce in Italy. Acta Biomed. 2020, 91, 57–67. [Google Scholar] [CrossRef]
- Collantoni, E.; Saieva, A.M.; Meregalli, V.; Girotto, C.; Carretta, G.; Boemo, D.G.; Bordignon, G.; Capizzi, A.; Contessa, C.; Nesoti, M.V.; et al. Psychological Distress, Fear of COVID-19, and Resilient Coping Abilities among Healthcare Workers in a Tertiary First-Line Hospital during the Coronavirus Pandemic. J. Clin. Med. 2021, 10, 1465. [Google Scholar] [CrossRef] [PubMed]
- Gambhir, R.S.; Dhaliwal, J.S.; Aggarwal, A.; Anand, S.; Anand, V.; Kaur Bhangu, A. Covid-19: A survey on knowledge, awareness and hygiene practices among dental health professionals in an Indian scenario. Rocz. Panstw. Zakl. Hig. 2020, 71, 223–229. [Google Scholar] [CrossRef]
- Geana, M.V. Kansans in the Middle of the Pandemic: Risk Perception, Knowledge, Compliance with Preventive Measures, and Primary Sources of Information about COVID-19. Kans. J. Med. 2020, 13, 160–164. [Google Scholar] [CrossRef]
- Moro, M.; Vigezzi, G.P.; Capraro, M.; Biancardi, A.; Nizzero, P.; Signorelli, C.; Odone, A. 2019-novel coronavirus survey: Knowledge and attitudes of hospital staff of a large Italian teaching hospital. Acta Biomed. 2020, 91, 29–34. [Google Scholar] [CrossRef]
- Temsah, M.H.; Alhuzaimi, A.N.; Alamro, N.; Alrabiaah, A.; Al-Sohime, F.; Alhasan, K.; Kari, J.A.; Almaghlouth, I.; Aljamaan, F.; Al-Eyadhy, A.; et al. Knowledge, attitudes and practices of healthcare workers during the early COVID-19 pandemic in a main, academic tertiary care centre in Saudi Arabia. Epidemiol. Infect. 2020, 148, e203. [Google Scholar] [CrossRef]
- Jones, J.; Sullivan, P.S.; Sanchez, T.H.; Guest, J.L.; Hall, E.W.; Luisi, N.; Zlotorzynska, M.; Wilde, G.; Bradley, H.; Siegler, A.J. Similarities and Differences in COVID-19 Awareness, Concern, and Symptoms by Race and Ethnicity in the United States: Cross-Sectional Survey. J. Med. Internet Res. 2020, 22, e20001. [Google Scholar] [CrossRef]
- Raamkumar, A.S.; Tan, S.G.; Wee, H.L. Use of Health Belief Model-Based Deep Learning Classifiers for COVID-19 Social Media Content to Examine Public Perceptions of Physical Distancing: Model Development and Case Study. JMIR Public Health Surveill. 2020, 6, e20493. [Google Scholar] [CrossRef]
- Shrestha, N.; Shad, M.Y.; Ulvi, O.; Khan, M.H.; Karamehic-Muratovic, A.; Nguyen, U.D.T.; Baghbanzadeh, M.; Wardrup, R.; Aghamohammadi, N.; Cervantes, D.; et al. The impact of COVID-19 on globalization. One Health 2020. [Google Scholar] [CrossRef] [PubMed]
- Ke, G.; Meng, Q.; Finley, T.; Wang, T.; Chen, W.; Ma, W.; Ye, Q.; Liu, T.Y. LightGBM: A Highly Efficient Gradient Boosting Decision Tree. In Proceedings of the 31st Conference on Neural Information Processing Systems (NIPS 2017), Long Beach, CA, USA, 20 December 2017. [Google Scholar]
- Hossain, M.A.; Jahid, M.I.K.; Hossain, K.M.A.; Walton, L.M.; Uddin, Z.; Haque, M.O.; Kabir, M.F.; Arafat, S.M.Y.; Sakel, M.; Faruqui, R.; et al. Knowledge, attitudes, and fear of COVID-19 during the Rapid Rise Period in Bangladesh. PLoS ONE 2020, 15, e0239646. [Google Scholar] [CrossRef]
- Zhong, B.L.; Luo, W.; Li, H.M.; Zhang, Q.Q.; Liu, X.G.; Li, W.T.; Li, Y. Knowledge, attitudes, and practices towards COVID-19 among Chinese residents during the rapid rise period of the COVID-19 outbreak: A quick online cross-sectional survey. Int. J. Biol. Sci. 2020, 16, 1745–1752. [Google Scholar] [CrossRef]
- Moghanibashi-Mansourieh, A. Assessing the anxiety level of Iranian general population during COVID-19 outbreak. Asian J. Psychiatr. 2020, 51, 102076. [Google Scholar] [CrossRef]
- Pieh, C.; Budimir, S.; Probst, T. The effect of age, gender, income, work, and physical activity on mental health during coronavirus disease (COVID-19) lockdown in Austria. J. Psychosom. Res. 2020, 136, 110186. [Google Scholar] [CrossRef]
- Rossi, R.; Socci, V.; Talevi, D.; Mensi, S.; Niolu, C.; Pacitti, F.; Di Marco, A.; Rossi, A.; Siracusano, A.; Di Lorenzo, G. COVID-19 Pandemic and Lockdown Measures Impact on Mental Health Among the General Population in Italy. Front. Psychiatry 2020, 11, 790. [Google Scholar] [CrossRef]
- Alon, T.M.; Doepke, M.; Olmstead-Rumsey, J.; Tertilt, M. The Impact of COVID-19 on Gender Equality (No. w26947); National Bureau of Economic Research: Cambridge, MA, USA, 2020. [Google Scholar]
- Flesia, L.; Monaro, M.; Mazza, C.; Fietta, V.; Colicino, E.; Segatto, B.; Roma, P. Predicting Perceived Stress Related to the Covid-19 Outbreak through Stable Psychological Traits and Machine Learning Models. J. Clin. Med. 2020, 9, 3350. [Google Scholar] [CrossRef]
- Klaiber, P.; Wen, J.H.; DeLongis, A.; Sin, N.L. The ups and downs of daily life during COVID-19: Age differences in affect, stress, and positive events. J. Gerontol. Ser. B 2021, 76, e30–e37. [Google Scholar] [CrossRef]
- Ferguson, P.E.; Jordens, C.F.; Gilroy, N.M. Patient and family education in HSCT: Improving awareness of respiratory virus infection and influenza vaccination. A descriptive study and brief intervention. Bone Marrow Transpl. 2010, 45, 656–661. [Google Scholar] [CrossRef] [PubMed]
- Total Analysis. China Ranked 96th out of 100 Countries in Covid Data Transparency Index. 2021. Available online: https://www.prnewswire.com/news-releases/china-ranked-96th-out-of-100-countries-in-covid-data-transparency-index-301206339.html (accessed on 8 April 2021).
- Al-Omiri, M.K.; Alzoubi, I.A.; Al Nazeh, A.A.; Alomiri, A.K.; Maswady, M.N.; Lynch, E. COVID-19 and Personality: A—Cross-Sectional Multicenter Study of the Relationship Between Personality Factors and COVID-19-Related Impacts, Concerns, and Behaviors. Front. Psychiatry 2021, 12, 608730. [Google Scholar] [CrossRef]
- Collaborative, T.M.-G.C. Perceived Stress of Quarantine and Isolation During COVID-19 Pandemic: A Global Survey. Front. Psychiatry 2021, 12, 656664. [Google Scholar] [CrossRef]
- Ribeiro, F.S.; Santos, F.H.; Anunciacao, L.; Barrozo, L.; Landeira-Fernandez, J.; Leist, A.K. Exploring the Frequency of Anxiety and Depression Symptoms in a Brazilian Sample during the COVID-19 Outbreak. Int. J. Environ. Res. Public Health 2021, 18, 4847. [Google Scholar] [CrossRef]
- Guimaraes, V.H.A.; de Oliveira-Leandro, M.; Cassiano, C.; Marques, A.L.P.; Motta, C.; Freitas-Silva, A.L.; de Sousa, M.A.D.; Silveira, L.A.M.; Pardi, T.C.; Gazotto, F.C.; et al. Knowledge About COVID-19 in Brazil: Cross-Sectional Web-Based Study. JMIR Public Health Surveill. 2021, 7, e24756. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Song, B.; Di, J.; Yang, X.; Wu, A.; Lau, J.; Xin, M.; Wang, L.; Mo, P.K. Intentions to Seek Mental Health Services During the COVID-19 Pandemic Among Chinese Pregnant Women With Probable Depression or Anxiety: Cross-sectional, Web-Based Survey Study. JMIR Ment. Health 2021, 8, e24162. [Google Scholar] [CrossRef] [PubMed]
- Zidkova, R.; Malinakova, K.; van Dijk, J.P.; Tavel, P. The Coronavirus Pandemic and the Occurrence of Psychosomatic Symptoms: Are They Related? Int. J. Environ. Res. Public Health 2021, 18, 3570. [Google Scholar] [CrossRef]
- Ruiz-Frutos, C.; Palomino-Baldeón, J.C.; Ortega-Moreno, M.; Villavicencio-Guardia, M.d.C.; Dias, A.; Bernardes, J.M.; Gómez-Salgado, J. Effects of the COVID-19 Pandemic on Mental Health in Peru: Psychological Distress. Healthcare 2021, 9, 691. [Google Scholar] [CrossRef] [PubMed]
- Rossell, S.L.; Neill, E.; Phillipou, A.; Tan, E.J.; Toh, W.L.; Van Rheenen, T.E.; Meyer, D. An overview of current mental health in the general population of Australia during the COVID-19 pandemic: Results from the COLLATE project. Psychiatry Res. 2021, 296, 113660. [Google Scholar] [CrossRef] [PubMed]
- Zhou, R.; Chen, H.; Zhu, L.; Chen, Y.; Chen, B.; Li, Y.; Chen, Z.; Zhu, H.; Wang, H. Mental Health Status of the Elderly Chinese Population During COVID-19: An Online Cross-Sectional Study. Front. Psychiatry 2021, 12, 645938. [Google Scholar] [CrossRef] [PubMed]
- Iwendi, C.; Bashir, A.K.; Peshkar, A.; Sujatha, R.; Chatterjee, J.M.; Pasupuleti, S.; Mishra, R.; Pillai, S.; Jo, O. COVID-19 Patient Health Prediction Using Boosted Random Forest Algorithm. Front. Public Health 2020, 8, 357. [Google Scholar] [CrossRef]
- Mackey, T.; Purushothaman, V.; Li, J.; Shah, N.; Nali, M.; Bardier, C.; Liang, B.; Cai, M.; Cuomo, R. Machine Learning to Detect Self-Reporting of Symptoms, Testing Access, and Recovery Associated With COVID-19 on Twitter: Retrospective Big Data Infoveillance Study. JMIR Public Health Surveill 2020, 6, e19509. [Google Scholar] [CrossRef]
- Teng, Y.M.; Wu, K.S.; Wang, W.C.; Xu, D. Assessing the Knowledge, Attitudes and Practices of COVID-19 among Quarantine Hotel Workers in China. Healthcare 2020, 9, 772. [Google Scholar] [CrossRef]
- Li, Y.; Liu, G.; Egolet, R.O.; Yang, R.; Huang, Y.; Zheng, Z. Knowledge, Attitudes, and Practices Related to COVID-19 Among Malawi Adults: A Community-Based Survey. Int. J. Environ. Res. Public Health 2021, 18, 4090. [Google Scholar] [CrossRef] [PubMed]
- Shorten, C.; Khoshgoftaar, T.M.; Furht, B. Deep Learning applications for COVID-19. J. Big Data 2021, 8, 18. [Google Scholar] [CrossRef]
- Eder, S.J.; Steyrl, D.; Stefanczyk, M.M.; Pieniak, M.; Molina, J.M.; Pešout, O.; Binter, J.; Smela, P.; Scharnowski, F.; Nicholson, A.A. Predicting fear and perceived health during the COVID-19 pandemic using machine learning: A cross-national longitudinal study. PLoS ONE 2021, 16, e0247997. [Google Scholar] [CrossRef]
- Sazali, M.F.; Rahim, S.; Mohamed, M.H.; Omar, A.; Pang, N.T.P.; Jeffree, M.S.; Tat, Y.B.; Giloi, N.; Mohd Bahar, F.H.; Afridah, W.; et al. Knowledge, attitude and practice on COVID-19 among students during the early phase of pandemic in a university in Borneo, Malaysia. J. Public. Health. Res. 2021. [Google Scholar] [CrossRef]
- Roberts, M.; Driggs, D.; Thorpe, M.; Gilbey, J.; Yeung, M.; Ursprung, S.; Aviles-Rivero, A.I.; Etmann, C.; McCague, C.; Beer, C.; et al. Common pitfalls and recommendations for using machine learning to detect and prognosticate for COVID-19 using chest radiographs and CT scans. Nat. Mach. Intell. 2021, 3, 199–217. [Google Scholar] [CrossRef]
- Chinazzi, M.; Davis, J.T.; Ajelli, M.; Chinazzi, M.; Davis, J.T.; Ajelli, M.; Gioannini, C.; Litvinova, M.; Merler, S.; Pastore, Y.P.A.; et al. The effect of travel restrictions on the spread of the 2019 novel coronavirus (COVID-19) outbreak. Science 2020, 368, 395–400. [Google Scholar] [CrossRef] [Green Version]
- Budd, J.; Miller, B.S.; Manning, E.M.; Lampos, V.; Zhuang, M.; Edelstein, M.; Rees, G.; Emery, V.C.; Stevens, M.M.; Keegan, N.; et al. Digital technologies in the public-health response to COVID-19. Nat. Med. 2020, 26, 1183–1192. [Google Scholar] [CrossRef]
- Saha, K.; Torous, J.; Caine, E.D.; De Choudhury, M. Psychosocial Effects of the COVID-19 Pandemic: Large-scale Quasi-Experimental Study on Social Media. J. Med. Internet Res. 2020, 22, e22600. [Google Scholar] [CrossRef]
- Ge, F.; Zhang, D.; Wu, L.; Mu, H. Predicting Psychological State Among Chinese Undergraduate Students in the COVID-19 Epidemic: A Longitudinal Study Using a Machine Learning. Neuropsychiatr. Dis. Treat. 2020, 16, 2111–2118. [Google Scholar] [CrossRef]
- Prout, T.A.; Zilcha-Mano, S.; Aafjes-van Doorn, K.; Békés, V.; Christman-Cohen, I.; Whistler, K.; Kui, T.; Di Giuseppe, M. Identifying Predictors of Psychological Distress During COVID-19: A Machine Learning Approach. Front. Psychol. 2020, 11, 586202. [Google Scholar] [CrossRef]
- Srivatsan, R.; Indi, P.N.; Agrahari, S.; Menon, S.; Ashok, S.D. Machine learning based prognostic model and mobile application software platform for predicting infection susceptibility of COVID-19 using healthcare data. Res. Biomed. Eng. 2020. [Google Scholar] [CrossRef]

| AgeBin | Education | Profession | Gender | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Country | (0.0, 25.0] | (25.0, 50.0] | (50.0, inf] | P * | S * | T * | Academician/Administration | Medical Professionals | Female | Male |
| Bangladesh | 332 | 150 | 0 | 0 | 42 | 204 | 145 | 337 | 227 | 255 |
| China | 381 | 245 | 86 | 106 | 32 | 565 | 564 | 148 | 324 | 388 |
| Japan | 14 | 55 | 10 | 0 | 12 | 52 | 59 | 20 | 46 | 33 |
| Malaysia | 12 | 117 | 15 | 0 | 2 | 81 | 51 | 93 | 45 | 99 |
| Mexico | 282 | 198 | 86 | 0 | 77 | 307 | 339 | 227 | 185 | 381 |
| Pakistan | 68 | 193 | 0 | 0 | 7 | 122 | 58 | 203 | 140 | 121 |
| United States | 174 | 103 | 50 | 0 | 44 | 146 | 233 | 94 | 104 | 223 |
| Zambia | 11 | 63 | 2 | 0 | 0 | 42 | 57 | 19 | 46 | 30 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jony, S.S.R.; Haque, U.; Webb, N.J.; Spence, E.; Rahman, M.S.; Aghamohammadi, N.; Lie, Y.; Angulo-Molina, A.; Ananth, S.; Ren, X.; et al. Analyzing Predictors of Control Measures and Psychosocial Problems Associated with COVID-19 Pandemic: Evidence from Eight Countries. Behav. Sci. 2021, 11, 106. https://doi.org/10.3390/bs11080106
Jony SSR, Haque U, Webb NJ, Spence E, Rahman MS, Aghamohammadi N, Lie Y, Angulo-Molina A, Ananth S, Ren X, et al. Analyzing Predictors of Control Measures and Psychosocial Problems Associated with COVID-19 Pandemic: Evidence from Eight Countries. Behavioral Sciences. 2021; 11(8):106. https://doi.org/10.3390/bs11080106
Chicago/Turabian StyleJony, Sheikh Saifur Rahman, Ubydul Haque, Nathaniel J. Webb, Emily Spence, Md. Siddikur Rahman, Nasrin Aghamohammadi, Yongchan Lie, Aracely Angulo-Molina, Sushmitha Ananth, Xuelian Ren, and et al. 2021. "Analyzing Predictors of Control Measures and Psychosocial Problems Associated with COVID-19 Pandemic: Evidence from Eight Countries" Behavioral Sciences 11, no. 8: 106. https://doi.org/10.3390/bs11080106
APA StyleJony, S. S. R., Haque, U., Webb, N. J., Spence, E., Rahman, M. S., Aghamohammadi, N., Lie, Y., Angulo-Molina, A., Ananth, S., Ren, X., Kawachi, N., Ito, H., Ulvi, O., Lubinda, J., Karamehic-Muratovic, A., Maher, W., Ali, P., & Rahman, M. S. (2021). Analyzing Predictors of Control Measures and Psychosocial Problems Associated with COVID-19 Pandemic: Evidence from Eight Countries. Behavioral Sciences, 11(8), 106. https://doi.org/10.3390/bs11080106











