Examining the Role of Traditional Masculinity and Depression in Men’s Risk for Contracting COVID-19
Abstract
:1. Introduction
2. Materials and Methods
2.1. Sample and Procedure
2.2. Instruments
2.2.1. Sociodemographics and COVID-19 Related Questions
2.2.2. Male Role Norm Inventory–Short Form (MRNI–SF)
2.2.3. Gender Role Conflict Scale–Short Form (GRCS–SF)
2.2.4. Patient Health Questionnaire-9 (PHQ-9)
2.2.5. Male Depression Risk Scale-22 (MDRS-22)
2.2.6. Fear of COVID-19 Scale (FCV-19S) and COVID-19 Pandemic Stress Scale (CPSS)
2.3. Statistical Analysis
3. Results
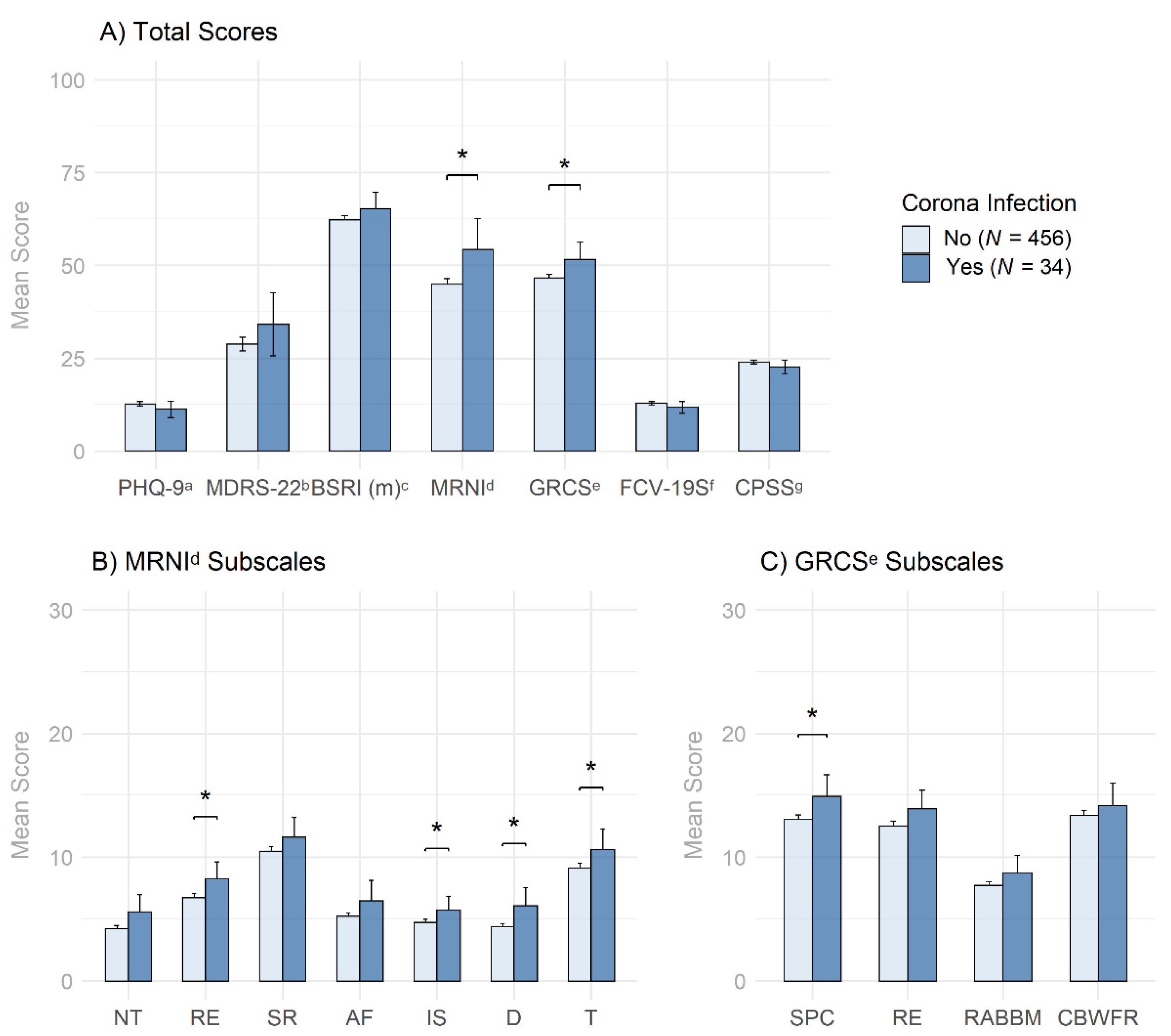
3.1. Descriptive Statistics and Group Differences in Men with and without COVID-19 Infection
3.2. Correlational Analysis
3.3. Logistic Regression Predicting COVID-19 Infection
3.4. Group Differences in Men with Low and High Traditional Masculinity
4. Discussion
4.1. Summary of Results
4.2. Integration of Findings
4.3. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Li, M.; Zhang, Z.; Cao, W.; Liu, Y.; Du, B.; Chen, C.; Liu, Q.; Uddin, M.N.; Jiang, S.; Chen, C.; et al. Identifying Novel Factors Associated with COVID-19 Transmission and Fatality Using the Machine Learning Approach. Sci. Total Environ. 2021, 764, 142810. [Google Scholar] [CrossRef] [PubMed]
- Bridges, T.; Barber, K.; Nelson, J.D.; Chatillon, A. Masculinity and COVID-19: Symposium Introduction. Men Masc. 2021, 24, 163–167. [Google Scholar] [CrossRef]
- Peckham, H.; de Gruijter, N.M.; Raine, C.; Radziszewska, A.; Ciurtin, C.; Wedderburn, L.R.; Rosser, E.C.; Webb, K.; Deakin, C.T. Male Sex Identified by Global COVID-19 Meta-Analysis as a Risk Factor for Death and ITU Admission. Nat. Commun. 2020, 11, 6317. [Google Scholar] [CrossRef] [PubMed]
- Hamer, M.; Kivimäki, M.; Gale, C.R.; Batty, G.D. Lifestyle Risk Factors, Inflammatory Mechanisms, and COVID-19 Hospitalization: A Community-Based Cohort Study of 387,109 Adults in UK. Brain Behav. Immun. 2020, 87, 184–187. [Google Scholar] [CrossRef] [PubMed]
- Courtenay, W.H. Engendering Health: A Social Constructionist Examination of Men’s Health Beliefs and Behaviors. Psychol. Men Masc. 2000, 1, 4–15. [Google Scholar] [CrossRef]
- Harrison, J. Warning: The Male Sex Role May Be Dangerous to Your Health. J. Soc. Issues 1978, 34, 65–86. [Google Scholar] [CrossRef]
- Umamaheswar, J.; Tan, C. “Dad, Wash Your Hands”: Gender, Care Work, and Attitudes toward Risk during the COVID-19 Pandemic. Socius 2020, 6, 2378023120964376. [Google Scholar] [CrossRef]
- Babalola, S.; Krenn, S.; Rimal, R.; Serlemitsos, E.; Shaivitz, M.; Shattuck, D.; Storey, D. KAP COVID Dashboard. In USA: Johns Hopkins Center for Communication Programs, Massachusetts Institute of Technology, Global Outbreak Alert and Response Network, Facebook Data for Good; Published September 2020. Available online: https://coronavirus.jhu.edu/map.html (accessed on 10 March 2022).
- Capraro, V.; Barcelo, H. The Effect of Messaging and Gender on Intentions to Wear a Face Covering to Slow down COVID-19 Transmission. PsyArXiv 2020. preprint. [Google Scholar] [CrossRef]
- Clark, C.; Davila, A.; Regis, M.; Kraus, S. Predictors of COVID-19 Voluntary Compliance Behaviors: An International Investigation. Glob. Transit. 2020, 2, 76–82. [Google Scholar] [CrossRef] [PubMed]
- Haischer, M.H.; Beilfuss, R.; Hart, M.R.; Opielinski, L.; Wrucke, D.; Zirgaitis, G.; Uhrich, T.D.; Hunter, S.K. Who Is Wearing a Mask? Gender-, Age-, and Location-Related Differences during the COVID-19 Pandemic. PLoS ONE 2020, 15, e0240785. [Google Scholar] [CrossRef]
- Okten, I.O.; Gollwitzer, A.; Oettingen, G. Gender Differences in Preventing the Spread of Coronavirus. Behav. Sci. Policy 2020, 6, 109–122. [Google Scholar] [CrossRef]
- Palmer, C.L.; Peterson, R.D. Toxic Mask-Ulinity: The Link between Masculine Toughness and Affective Reactions to Mask Wearing in the COVID-19 Era. Polit. Gend. 2020, 16, 1044–1051. [Google Scholar] [CrossRef]
- Cassino, D.; Besen-Cassino, Y. Of Masks and Men? Gender, Sex, and Protective Measures during COVID-19. Polit. Gend. 2020, 16, 1052–1062. [Google Scholar] [CrossRef]
- Mahalik, J.R.; Di Bianca, M.; Harris, M.P. Men’s Attitudes toward Mask-Wearing during COVID-19: Understanding the Complexities of Mask-Ulinity. J. Health Psychol. 2021. [Google Scholar] [CrossRef] [PubMed]
- Levant, R.F.; Richmond, K. The Gender Role Strain Paradigm and Masculinity Ideologies. In APA Handbook of Men and Masculinities; American Psychological Association: Washington, DC, USA, 2015; pp. 23–49. [Google Scholar] [CrossRef]
- O’Neil, J.M. Gender Role Conflict Research 30 Years Later: An Evidence-Based Diagnostic Schema to Assess Boys and Men in Counseling. J. Couns. Dev. 2013, 91, 490–498. [Google Scholar] [CrossRef]
- Cassino, D. Macho, Macho Man: Masculinity is a Major Risk Factor for COVID-19. Available online: https://www.fdu.edu/news/fdu-poll-finds-masculinity-is-a-major-risk-factor-for-covid-19/ (accessed on 10 March 2022).
- Lippa, R.A.; Martin, L.R.; Friedman, H.S. Gender-Related Individual Differences and Mortality in the Terman Longitudinal Study: Is Masculinity Hazardous to Your Health? Personal. Soc. Psychol. Bull. 2000, 26, 1560–1570. [Google Scholar] [CrossRef]
- Wong, Y.J.; Ho, M.H.R.; Wang, S.Y.; Miller, I.S.K. Meta-Analyses of the Relationship between Conformity to Masculine Norms and Mental Health-Related Outcomes. J. Couns. Psychol. 2017, 64, 80–93. [Google Scholar] [CrossRef] [PubMed]
- Eggenberger, L.; Fordschmid, C.; Ludwig, C.; Weber, S.; Grub, J.; Komlenac, N.; Walther, A. Men’s Psychotherapy Use, Male Role Norms, and Male-Typical Depression Symptoms: Examining 716 Men and Women Experiencing Psychological Distress. Behav. Sci. 2021, 11, 83. [Google Scholar] [CrossRef] [PubMed]
- Walther, A.; Grub, J.; Tsar, S.; Ehlert, U.; Heald, A.; Perrin, R.; Ogrodniczuk, J.S.; Seidler, Z.E.; Rice, S.M.; Kealy, D.; et al. Status Loss Due to COVID-19, Traditional Masculinity, and the Prediction of Suicidal Ideation and Recent Suicide Attempts. PsyArXiv 2021. preprint. [Google Scholar] [CrossRef]
- Coleman, D.; Feigelman, W.; Rosen, Z. Association of High Traditional Masculinity and Risk of Suicide Death: Secondary Analysis of the Add Health Study. JAMA Psychiatry 2020, 77, 435–437. [Google Scholar] [CrossRef] [PubMed]
- Gerdes, Z.T.; Levant, R.F. Complex Relationships among Masculine Norms and Health/Well-Being Outcomes: Correlation Patterns of the Conformity to Masculine Norms Inventory Subscales. Am. J. Mens. Health 2018, 12, 229–240. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bem, S.L. The Measurement of Psychological Androgyny. J. Consult. Clin. Psychol. 1974, 42, 155–162. [Google Scholar] [CrossRef] [PubMed]
- Pleck, J.H. The Myth of Masculinity; MIT Press (MA): Combridge, MA, USA, 1981. [Google Scholar]
- Levant, R.F.; Hirsch, L.S.; Celentano, E.; Cozza, T.M. The Male Role: An Investigation of Contemporary Norms. J. Ment. Health Couns. 1992, 14, 325–337. [Google Scholar]
- Mahalik, J.R.; Locke, B.D.; Ludlow, L.H.; Diemer, M.A.; Scott, R.P.J.; Gottfried, M.; Freitas, G. Development of the Conformity to Masculine Norms Inventory. Psychol. Men Masc. 2003, 4, 3–25. [Google Scholar] [CrossRef]
- O’Neil, J.M.; Helms, B.J.; Gable, R.K.; David, L.; Wrightsman, L.S. Gender-Role Conflict Scale: College Men’s Fear of Femininity. Sex Roles 1986, 14, 335–350. [Google Scholar] [CrossRef]
- Levant, R.F.; Wimer, D.J. Masculinity Constructs as Protective Buffers and Risk Factors for Men’s Health. Am. J. Mens. Health 2014, 8, 110–120. [Google Scholar] [CrossRef] [PubMed]
- Shinn, A.K.; Viron, M. Perspectives on the COVID-19 Pandemic and Individuals with Serious Mental Illness. J. Clin. Psychiatry 2020, 81, 14205. [Google Scholar] [CrossRef] [PubMed]
- Yao, H.; Chen, J.H.; Xu, Y.F. Patients with Mental Health Disorders in the COVID-19 Epidemic. Lancet Psychiatry 2020, 7, e21. [Google Scholar] [CrossRef]
- Chang, T.S.; Ding, Y.; Freund, M.K.; Johnson, R.; Schwarz, T.; Yabu, J.M.; Hazlett, C.; Chiang, J.N.; Wulf, A.; Geschwind, D.H. Prior Diagnoses and Medications as Risk Factors for COVID-19 in a Los Angeles Health System. medRxiv 2020. preprint. [Google Scholar] [CrossRef]
- Tang, O.; Bigelow, B.F.; Sheikh, F.; Peters, M.; Zenilman, J.M.; Bennett, R.; Katz, M.J. Outcomes of Nursing Home COVID-19 Patients by Initial Symptoms and Comorbidity: Results of Universal Testing of 1970 Residents. J. Am. Med. Dir. Assoc. 2020, 21, 1767–1773. [Google Scholar] [CrossRef]
- Taquet, M.; Luciano, S.; Geddes, J.R.; Harrison, P.J. Bidirectional Associations between COVID-19 and Psychiatric Disorder: Retrospective Cohort Studies of 62 354 COVID-19 Cases in the USA. Lancet Psychiatry 2021, 8, 130–140. [Google Scholar] [CrossRef]
- Wang, Q.; Xu, R.; Volkow, N.D. Increased Risk of COVID-19 Infection and Mortality in People with Mental Disorders: Analysis from Electronic Health Records in the United States. World Psychiatry 2021, 20, 124–130. [Google Scholar] [CrossRef]
- Izurieta, H.S.; Graham, D.J.; Jiao, Y.; Hu, M.; Lu, Y.; Wu, Y.; Chillarige, Y.; Wernecke, M.; Menis, M.; Pratt, D.; et al. Natural History of Coronavirus Disease 2019: Risk Factors for Hospitalizations and Deaths among >26 Million US Medicare Beneficiaries. J. Infect. Dis. 2021, 223, 945–956. [Google Scholar] [CrossRef] [PubMed]
- Ammerman, B.A.; Burke, T.A.; Jacobucci, R.; McClure, K. Preliminary Investigation of the Association between COVID-19 and Suicidal Thoughts and Behaviors in the U.S. J. Psychiatr. Res. 2021, 134, 32–38. [Google Scholar] [CrossRef] [PubMed]
- Ceban, F.; Nogo, D.; Carvalho, I.P.; Lee, Y.; Nasri, F.; Xiong, J.; Lui, L.M.W.; Subramaniapillai, M.; Gill, H.; Liu, R.N. Association Between Mood Disorders and Risk of COVID-19 Infection, Hospitalization, and Death: A Systematic Review and Meta-Analysis. JAMA Psychiatry 2021, 78, 1079–1091. [Google Scholar] [CrossRef] [PubMed]
- Rice, S.M.; Fallon, B.J.; Aucote, H.M.; Möller-Leimkühler, A.M. Development and Preliminary Validation of the Male Depression Risk Scale: Furthering the Assessment of Depression in Men. J. Affect. Disord. 2013, 151, 950–958. [Google Scholar] [CrossRef] [PubMed]
- Cavanagh, A.; Wilson, C.J.; Kavanagh, D.J.; Caputi, P. Differences in the Expression of Symptoms in Men Versus Women with Depression: A Systematic Review and Meta-Analysis. Harv. Rev. Psychiatry 2017, 25, 29–38. [Google Scholar] [CrossRef] [PubMed]
- Martin, L.A.; Neighbors, H.W.; Griffith, D.M. The Experience of Symptoms of Depression in Men vs Women: Analysis of the National Comorbidity Survey Replication. JAMA Psychiatry 2013, 70, 1100–1106. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Walther, A.; Grub, J.; Ehlert, U.; Wehrli, S.; Rice, S.M.; Seidler, Z.E.; Debelak, R. Male Depression Risk, Psychological Distress, and Psychotherapy Uptake: Validation of the German Version of the Male Depression Risk Scale. J. Affect. Disord. Rep. 2021, 4, 100107. [Google Scholar] [CrossRef]
- Winkler, D.; Pjrek, E.; Kasper, S. Anger Attacks in Depression–Evidence for a Male Depressive Syndrome. Psychother. Psychosom. 2005, 74, 303–307. [Google Scholar] [CrossRef]
- Walther, A.; Seidler, Z.E. Männliche Formen der Depression und deren Behandlung. PiD-Psychother. Im Dialog 2020, 21, 40–45. [Google Scholar] [CrossRef]
- Sudre, C.H.; Murray, B.; Varsavsky, T.; Graham, M.S.; Penfold, R.S.; Bowyer, R.C.; Pujol, J.C.; Klaser, K.; Antonelli, M.; Canas, L.S.; et al. Attributes and Predictors of Long COVID. Nat. Med. 2021, 27, 626–631. [Google Scholar] [CrossRef] [PubMed]
- Levant, R.F.; Hall, R.J.; Rankin, T.J. Male Role Norms Inventory-Short Form (Mrni-Sf): Development, Confirmatory Factor Analytic Investigation of Structure, and Measurement Invariance across Gender. J. Couns. Psychol. 2013, 60, 228–238. [Google Scholar] [CrossRef] [PubMed]
- Wester, S.R.; Vogel, D.L.; O’Neil, J.M.; Danforth, L. Development and Evaluation of the Gender Role Conflict Scale Short Form (GRCS-SF). Psychol. Men Masc. 2012, 13, 199–210. [Google Scholar] [CrossRef]
- Komlenac, N.; Siller, H.; Bliem, H.R.; Hochleitner, M. Validation of the Internal Structure of a German-Language Version of the Gender Role Conflict Scale—Short Form. Front. Psychol. 2018, 9, 1161. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.W. The Phq-9. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®), 5th ed.; American Psychiatric Pub: Arlington, VA, USA, 2013. [Google Scholar]
- Levis, B.; Sun, Y.; He, C.; Wu, Y.; Krishnan, A.; Bhandari, P.M.; Neupane, D.; Imran, M.; Brehaut, E.; Negeri, Z.; et al. Accuracy of the PHQ-2 Alone and in Combination with the PHQ-9 for Screening to Detect Major Depression: Systematic Review and Meta-Analysis. JAMA J. Am. Med. Assoc. 2020, 323, 2290–2300. [Google Scholar] [CrossRef]
- Martin, A.; Rief, W.; Klaiberg, A.; Braehler, E. Validity of the Brief Patient Health Questionnaire Mood Scale (PHQ-9) in the General Population. Gen. Hosp. Psychiatry 2006, 28, 71–77. [Google Scholar] [CrossRef]
- Ahorsu, D.K.; Lin, C.-Y.; Imani, V.; Saffari, M.; Griffiths, M.D.; Pakpour, A.H. The Fear of COVID-19 Scale: Development and Initial Validation. Int. J. Ment. Health Addict. 2020. [Google Scholar] [CrossRef] [Green Version]
- Werner, A.; Kater, M.-J.; Schlarb, A.; Lohaus, A. COVID-19-Pandemie-Stress-Skala (CPSS). PsyArXiv 2021. preprints. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2020. [Google Scholar]
- Revelle, W. Psych: Procedures for Personality and Psychological Research; Northwestern University: Evanston, IL, USA, 2020. [Google Scholar]
- Fox, J.; Sanford, W. An {R} Companion to Applied Regression, 3rd ed.; Sage: Thousand Oaks, CA, USA, 2019. [Google Scholar]
- Mangiafico, S. Rcompanion: Functions to Support Extension Education Program Evaluation [R Package Rcompanion Version 2.4. 0]; 2021. Available online: https://cran.r-project.org/web/packages/rcompanion/index.html (accessed on 10 March 2022).
- Wickham, H. Ggplot2: Elegant Graphics for Data Analysis; Springer: New York, NY, USA, 2016. [Google Scholar]
- Holm, S. A Simple Sequentially Rejective Multiple Test Procedure. Scand. J. Stat. 1979, 6, 65–70. [Google Scholar]
- Levene, H. Robust Tests for Equality of Variances. In Contributions to Probability and Statistics; Essays in Honor of Harold Hotelling; Stanford University Press: Palo Alto, CA, USA, 1961; pp. 279–292. [Google Scholar]
- Fox, J.; Monette, G. Generalized Collinearity Diagnostics. J. Am. Stat. Assoc. 1992, 87, 178–183. [Google Scholar] [CrossRef]
- Cook, R.D. Detection of Influential Observation in Linear Regression. Technometrics 1977, 19, 15–18. [Google Scholar] [CrossRef]
- Iwamoto, D.K.; Cheng, A.; Lee, C.S.; Takamatsu, S.; Gordon, D. “Man-Ing” up and Getting Drunk: The Role of Masculine Norms, Alcohol Intoxication and Alcohol-Related Problems among College Men. Addict. Behav. 2011, 36, 906–911. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rice, S.M.; Ogrodniczuk, J.S.; Kealy, D.; Seidler, Z.E.; Dhillon, H.M.; Oliffe, J.L. Validity of the Male Depression Risk Scale in a Representative Canadian Sample: Sensitivity and Specificity in Identifying Men with Recent Suicide Attempt. J. Ment. Health 2019, 28, 132–140. [Google Scholar] [CrossRef] [PubMed]
- Ettman, C.K.; Abdalla, S.M.; Cohen, G.H.; Sampson, L.; Vivier, P.M.; Galea, S. Prevalence of Depression Symptoms in US Adults Before and During the COVID-19 Pandemic. JAMA Netw. Open 2020, 3, e2019686. [Google Scholar] [CrossRef] [PubMed]



| Total (N = 490) | No CV19 (N = 456) | CV19 (N = 34) | ||||||
|---|---|---|---|---|---|---|---|---|
| N (%) | M (SD) | N (%) | M (SD) | N (%) | M (SD) | Test-Statistic (df) | p | |
| Age | 25.7 (9.8) | 25.7 (9.8) | 25.9 (9.5) | −0.10 (448) | 0.924 | |||
| Nationality | 26.63 (6) | <0.001 *** | ||||||
| Swiss | 71 (14.5) | 62 (13.6) | 9 (26.5) | |||||
| German | 358 (73.1) | 342 (75.0) | 16 (47.1) | |||||
| Austrian | 43 (8.8) | 36 (7.9) | 7 (20.6) | |||||
| Luxembourger | 4 (0.8) | 4 (0.9) | 0 (0) | |||||
| Liechtensteiner | 1 (0.2) | 1 (0.2) | 0 (0) | |||||
| Belgian | 1 (0.2) | 0 (0) | 1 (2.9) | |||||
| Other | 12 (2.4) | 11 (2.4) | 1 (2.9) | |||||
| Sexual orientation | 0.88 (4) | 0.927 | ||||||
| Heterosexual-identified | 361 (73.7) | 334 (73.2) | 27 (79.4) | |||||
| Gay/Lesbian-identified | 39 (8.0) | 37 (8.1) | 2 (5.9) | |||||
| Bisexual-identified | 67 (13.7) | 63 (13.8) | 4 (11.8) | |||||
| Asexual-identified | 5 (1.0) | 5 (1.1) | 0 (0) | |||||
| Other | 18 (3.7) | 17 (3.7) | 1 (2.9) | |||||
| Marital status | 1.45 (2) | 0.484 | ||||||
| Single | 311 (63.5) | 291 (63.8) | 20 (58.8) | |||||
| In a relationship | 168 (34.3) | 154 (33.8) | 14 (41.2) | |||||
| Separated after permanent relationship | 11 (2.2) | 11 (2.4) | 0 (0) | |||||
| Education | 3.69 (3) | 0.296 | ||||||
| None completed | 10 (2.0) | 10 (2.2) | 0 (0) | |||||
| Secondary education | 348 (71.0) | 325 (71.3) | 23 (67.6) | |||||
| Tertiary education | 106 (21.6) | 99 (21.7) | 7 (20.6) | |||||
| Other | 26 (5.3) | 22 (4.8) | 4 (11.8) | |||||
| Yearly household income (in CHF) | 1.88 (2) | 0.392 | ||||||
| <25,000 | 233 (47.6) | 220 (48.2) | 13 (38.2) | |||||
| 25,000–50,000 | 92 (18.8) | 86 (18.9) | 6 (17.6) | |||||
| >50,000 | 165 (33.7) | 150 (32.9) | 15 (44.1) | |||||
| Due to CV19 Pandemic † | ||||||||
| Status Loss | 72 (14.7) | 67 (14.7) | 5 (14.7) | 0 (1) | 1 | |||
| Financial problems | 100 (20.4) | 92 (20.2) | 8 (23.5) | 0.06 (1) | 0.804 | |||
| Job insecurity | 112 (22.9) | 102 (22.4) | 10 (29.4) | 0.54 (1) | 0.464 | |||
| Job loss | 41 (8.4) | 37 (8.1) | 4 (11.8) | 0.18 (1) | 0.674 | |||
| Registration with the employment center (RAV) | 34 (6.9) | 30 (6.6) | 4 (11.8) | 0.64 (1) | 0.425 | |||
| Existential threat | 95 (19.4) | 86 (18.9) | 9 (26.5) | 0.74 (1) | 0.391 | |||
| Psychological Disorder † | 117 (23.9) | 112 (24.6) | 5 (14.7) | 1.19 (1) | 0.275 | |||
| Psychotherapy † | 95 (19.4) | 92 (20.2) | 3 (8.8) | 1.93 (1) | 0.164 | |||
| Psychiatric Medication † | 64 (13.1) | 62 (13.6) | 2 (5.9) | 1.05 (1) | 0.306 | |||
| Depression Cutoff | ||||||||
| PHQ-9 (≥10) | 322 (65.7) | 305 (66.9) | 17 (50.0) | 3.29 (1) | 0.070 | |||
| MDRS-22 (≥51) | 67 (13.7) | 58 (12.7) | 9 (26.5) | 3.07 (1) | 0.046 * | |||
| PHQ-9 a | 12.6 (6.6) | 12.7 (6.6) | 11.3 (6.3) | 1.21 (488) | 0.225 | |||
| MDRS-22 b | 29.2 (20.6) | 28.8 (20.3) | 34.1 (24.4) | −1.45 (488) | 0.169 | |||
| BSRI (m) c | 62.5 (14.6) | 62.2 (14.6) | 65.4 (15.2) | −1.20 (488) | 0.116 | |||
| MRNI-SF d | 45.6 (21.4) | 44.9 (20.7) | 54.4 (28.9) | −1.87 (35.6) | 0.025 * | |||
| GRCS-SF e | 47.0 (12.6) | 46.7 (12.2) | 51.7 (16.0) | −1.78 (35.9) | 0.042 * | |||
| FCV-19S f | 12.8 (4.9) | 12.9 (4.90) | 11.8 (4.60) | 1.28 (488) | 0.200 | |||
| CPSS g | 23.9 (5.2) | 24.0 (5.15) | 22.6 (5.38) | 1.52 (488) | 0.130 | |||
| M | SD | 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|---|---|
| 1. PHQ-9 a | 12.6 | 6.6 | ̶ | |||||
| 2. MDRS-22 b | 29.2 | 20.6 | 0.64 *** | ̶ | ||||
| 3. BSRI (m) c | 62.5 | 14.6 | −0.36 *** | −0.10 | ̶ | |||
| 4. MRNI-SF d | 45.6 | 21.4 | −0.06 | 0.17 ** | 0.33 *** | ̶ | ||
| 5. GRCS-SF e | 47.0 | 12.6 | 0.41 *** | 0.48 *** | 0.01 | 0.39 *** | ̶ | |
| 6. FCV-19S f | 12.8 | 4.9 | 0.29 *** | 0.28 *** | −0.16 ** | −0.15 ** | 0.18 *** | ̶ |
| 7. CPSS g | 23.9 | 5.2 | 0.31 *** | 0.28 *** | 0.03 | −0.04 | 0.24 *** | 0.58 *** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Walther, A.; Eggenberger, L.; Grub, J.; Ogrodniczuk, J.S.; Seidler, Z.E.; Rice, S.M.; Kealy, D.; Oliffe, J.L.; Ehlert, U. Examining the Role of Traditional Masculinity and Depression in Men’s Risk for Contracting COVID-19. Behav. Sci. 2022, 12, 80. https://doi.org/10.3390/bs12030080
Walther A, Eggenberger L, Grub J, Ogrodniczuk JS, Seidler ZE, Rice SM, Kealy D, Oliffe JL, Ehlert U. Examining the Role of Traditional Masculinity and Depression in Men’s Risk for Contracting COVID-19. Behavioral Sciences. 2022; 12(3):80. https://doi.org/10.3390/bs12030080
Chicago/Turabian StyleWalther, Andreas, Lukas Eggenberger, Jessica Grub, John S. Ogrodniczuk, Zac E. Seidler, Simon M. Rice, David Kealy, John L. Oliffe, and Ulrike Ehlert. 2022. "Examining the Role of Traditional Masculinity and Depression in Men’s Risk for Contracting COVID-19" Behavioral Sciences 12, no. 3: 80. https://doi.org/10.3390/bs12030080
APA StyleWalther, A., Eggenberger, L., Grub, J., Ogrodniczuk, J. S., Seidler, Z. E., Rice, S. M., Kealy, D., Oliffe, J. L., & Ehlert, U. (2022). Examining the Role of Traditional Masculinity and Depression in Men’s Risk for Contracting COVID-19. Behavioral Sciences, 12(3), 80. https://doi.org/10.3390/bs12030080









