Abstract
(1) Background: The motivational determinants of health professionals to choose and remain in the public sector have been increasingly addressed, including the customized approach of Public Service Motivation (PSM). However, to date, no systematic research overview has been performed in this domain, leaving the body of literature unstructured. This article fills this gap by assessing the motivational factors of choice for the public sector in the health field, and the conceptual and methodological trends of this research stream. (2) Methods: This study follows the PRISMA protocol to ascertain patterns in past research and inform researchers, practitioners, and policymakers. Eighty-nine documents published between 1998 and 2021 were retained after selecting them according to their theme and outlined goals. (3) Results: Common motivational determinants are remuneration, available resources, work conditions, and frequency of contact and interaction with patients. The PSM construct and scale are often employed as main frameworks, but there is also a concern in assessing motivation drawing on psychological constructs that reflect the challenging line of work and environment that is health care, such as presenteeism, stress, and perception of hindrances. (4) Conclusions: By focusing on health professionals’ motivation, this study contributes to a timely systematization in challenging times for health institutions and their human resources.
1. Introduction
Public Service Motivation (PSM), as conceptualized by Perry and Wise (1990) [1], encompasses individual beliefs, motivations, values, and attitudes towards the nature and mission of public institutions. The interest in PSM as a determining factor for choosing and staying in public administration gained traction in recent years [2,3,4], shifting the way motivation was addressed in light of New Public Management (NPM). Mimicking the private sector, the NPM showed concern for efficiency, efficacy, productivity, and performance, which are of growing importance for decision makers, researchers, and professionals [5,6,7], but with counterproductive consequences in the recruitment of personnel upholding the desired public values. In fact, the use of the private sector managerial style in public administration has had a critical impact in the human resources domain, namely in the loss of specific features usually regarded as attractive in human resources, such as the guarantee of job security and more predictable promotion opportunities [8].
Although public sector workforce recruitment has been systematically addressed in the literature as a problematic issue that needs to be tackled [8], even if there is no consensus on the measures and practices to promote positive change [9], employees’ motivation to choose and remain in the public sector, however, has been overlooked for a long time, generating a gap in understanding how to recruit professionals aligned with public values.
The constructs of Public Sector Motivation and Public Service Motivation contributed prominently to this topic, by tailoring an approach to motivation adapted to features of the public sector. Public Sector Motivation emphasizes acting in one’s self-interest and maximizing individual choice, positive outcomes, and extrinsic rewards, such as job security, job progression, and salary [8,10]. Public Service Motivation (PSM) (Perry and Wise, 1990) [1] focuses on the entanglement between individual beliefs, motivations, values, and attitudes, and the nature and mission of public institutions [1,11]. PSM’s original measurement includes four conceptual dimensions: attraction to the public interest, participation in the processes of political decisions, compassion, and self-sacrifice [12], with a transcultural adaptation with 16 items [13]. This last construct has shown to influence organizational behavior [14], the choice of a sector of activity, performance [15], and workers’ satisfaction [16]. Primarily, PSM was circumscribed for public institutions and organizations, then being argued further on that its essence is also found outside these boundaries [17].
Within this context, debates have emerged around the concepts of intrinsic and extrinsic motivation [18]. This distinction proves to be useful in framing the choice determinants of the public vs. private sector. For instance, it is argued that public sector employees are more concerned with work safety and less with remuneration as opposed to employees from the private sector, who tend to aim for high paychecks [19].
Health professionals are the backbone of any health system, and their motivation and behavior significantly influence the performance of a health system [20]. Moreover, universal health coverage cannot be achieved without a workforce aligned with that purpose and practice [21,22]. Still, professionals in the health field are recognized by the World Health Organization as representing the main cost and investment in health care provision, due to job requirements, the financial and non-financial investments, and the continuous investment in education to maintain the quality of their work [23].
To this adds the current context of COVID-19, as it is particularly demanding for health professionals to stay focused, motivated, and feel safe facing such a challenge. The enlargement and allocation of the health workforce demand more strategic approaches regarding the number, availability, and distribution of health professionals; the training of specific competences and skills to deal with COVID-19; the guarantee of safe and decent work conditions; fast enactment of policies and regulations; and support mechanisms, including financial resources [24].
The growing importance of the theme of motivation in the past decade underlines the relevance of aggregating the studies conducted to draw conclusions for future research or interventions. No similar review has been conducted comparing several world regions with a special focus on the developing world [25]. In this sense, the main goals of this work are:
- (i)
- To characterize the research about health professionals’ motivational determinants, including the methodological quality, geographical distribution, choice of journals, cross-country and author collaboration, and co-citation trends;
- (ii)
- To identify the motivational factors influencing the sector’s choice by health professionals in different territories;
- (iii)
- To identify the dissemination and use of the main instruments to measure PSM; and
- (iv)
- To identify the main motivational theories supporting the studies.
The remaining sections outline the description of the methods used, including the review protocol and the search process, followed by the results and a discussion of the obtained findings, ending with some concluding remarks and suggestions/limitations for future research.
2. Materials and Methods
2.1. Research Questions
Systematic reviews of literature contribute to providing an updated state of the art of a given topic and clarify future research avenues [25]. This is achievable by highlighting important questions and gaps in the literature [26,27].
This review employed the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) protocol, developed within the context of health sciences to enhance the reliability and replication of literature reviews and meta-analyses [28,29,30]. The selection of studies to address the abovementioned goals answered three research questions:
- -
- What characterizes the research on health professionals’ motivation regarding geographical and authorship distribution, collaborations, and co-citations?
- -
- What are the factors motivating health professionals to choose the public sector for their activity?
- -
- What are the methods and instruments employed to assess health professionals’ motivation?
2.2. Search Strategy, Inclusion and Exclusion Criteria
The articles were sourced from three database—SCOPUS, Web of Science (WoS), and PubMed—including studies in the field of social and medical sciences. The expressions searched in article titles, abstracts, and keywords were: [“public service” OR “public sector” OR “public work” OR “public employ*”] AND [“motivation” OR “altruism” OR “ethic*” OR “prosocial”] AND [“health service*” OR “health provider*” OR healthcare OR “health care” OR “primary care” OR hospital* OR nurs* OR doctor* OR “health professional*” OR physician* OR medic* OR “health worker*”]. The search resulted in 2424 documents.
The search was refined by language (English) and type of document according to the database: (i) for SCOPUS, we chose “article” + “conference paper” + “book chapter” + “short survey”; (ii) for WoS, we chose “article” + “other” + “early access” + “unspecified”; (iii) and for PUBMED, all were considered. No time period was outlined in order to analyze the literature evolution according to time. After these stages, duplicated articles were eliminated.
In order to prevent the inclusion of articles not related to the theme, specifically the concept of motivation for public service and/or motivation related to the field of health and health professionals, the final selection of articles comprised the reading of titles and abstracts. The excluded articles focused on fields such as disease and comorbidity, pharmacology, microbiology, and biochemistry. This phase was conducted by one author and further verified by two authors to strengthen the assessment, substantially reducing the number of articles and avoiding the inclusion of non-related articles and the exclusion of relevant articles.
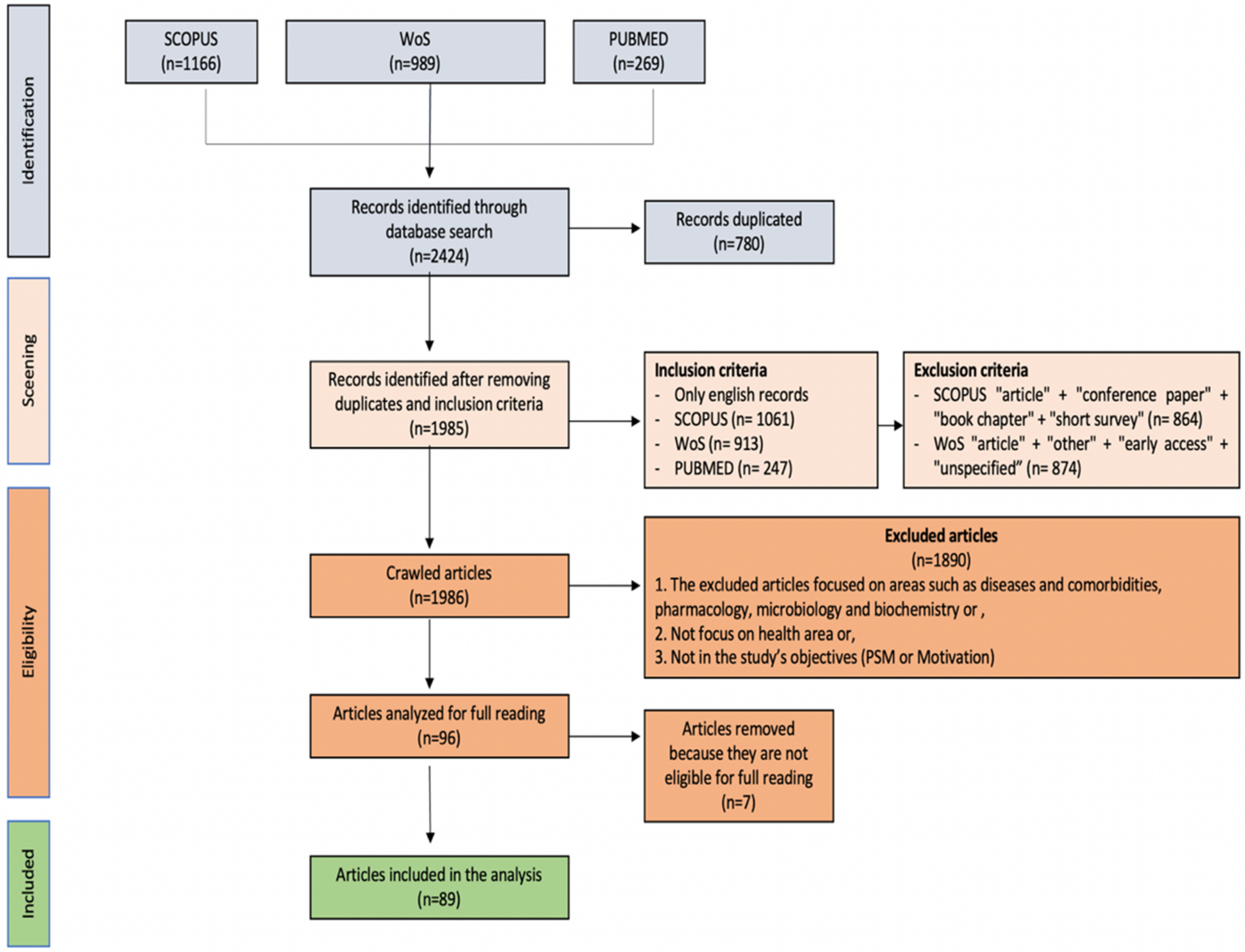
Initially, 2424 articles were retained from Scopus (n = 1166), WoS (n = 989), and PubMed (n = 269). Seventy articles were repeated and were thus excluded. Eighty-nine documents were retained after selecting them according to their theme and outlined goals, as shown in the PRISMA diagram below (Figure 1).
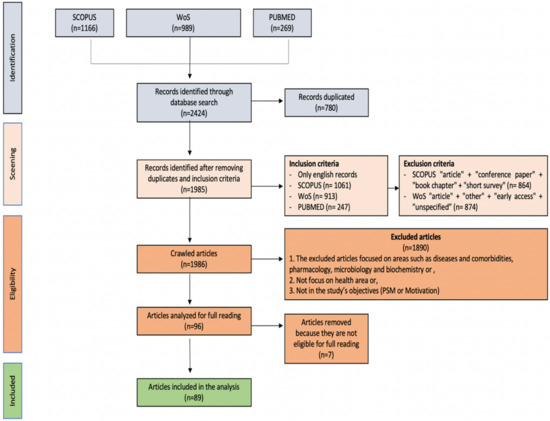
Figure 1.
PRISMA flowchart screening processes for narrative synthesis.
Bibliometrix, VOSviewer, and PlumXmetrics were used to process the bibliometric data and the Mendeley bibliographic referencing software to organize the references.
2.3. Methodological Quality Assessment
The methodological quality of each of the 89 studies was assessed using a checklist based on the works developed by Pitchforth et al. (2017) [31], Yang et al. (2020) [32], the Critical Appraisal Skills Programme (2013) [33], and Health Evidence (2018) [25]. A component approach, as advocated by the PRISMA statement, was used when applying the checklist, assessing each item individually rather than generating a summary score [34]. The checklist assesses 6 features of the study (Table 1), and responses are scored “yes” or “no”. Two authors independently conducted the quality assessment of each study. Disagreements were resolved by discussion, with the involvement of the third author, and a final decision was achieved by consensus.

Table 1.
Study quality assessment questions.
3. Results
3.1. Authors
The 89 articles were published between 1998 and 2021 and involved 297 different authors. The mean value is three authors per article and only 14 articles were written by just one author (15.7%). Author’s affiliations are distributed among several research institutions worldwide, specialized in health management, health policies, and human resources and political sciences. Table 2 presents the authors who published the greatest number of articles within the scope of this study.

Table 2.
Most relevant authors per number of documents.
The scientific collaboration between authors or institutions shows a solid internationalization of new knowledge. The collaboration index or the average number of authors on multi-authored papers is 3.79; thus, on average, a non-single author publication in this sample has almost four authors.
3.2. Publications
The analyzed sample is composed of 88 articles published in 52 scientific journals and one conference paper. Among these, seven journals published three or more articles, namely, Human Resources for Health, Health Policy and Planning, BMC Health Services Research, International Journal of Public Administration, Global Health Action, International Public Management Journal, and Social Science and Medicine. Most of these are first-quartile (Q1) journals under the scope of health policies and/or public administration (Table 3).

Table 3.
Journals with three or more articles published.
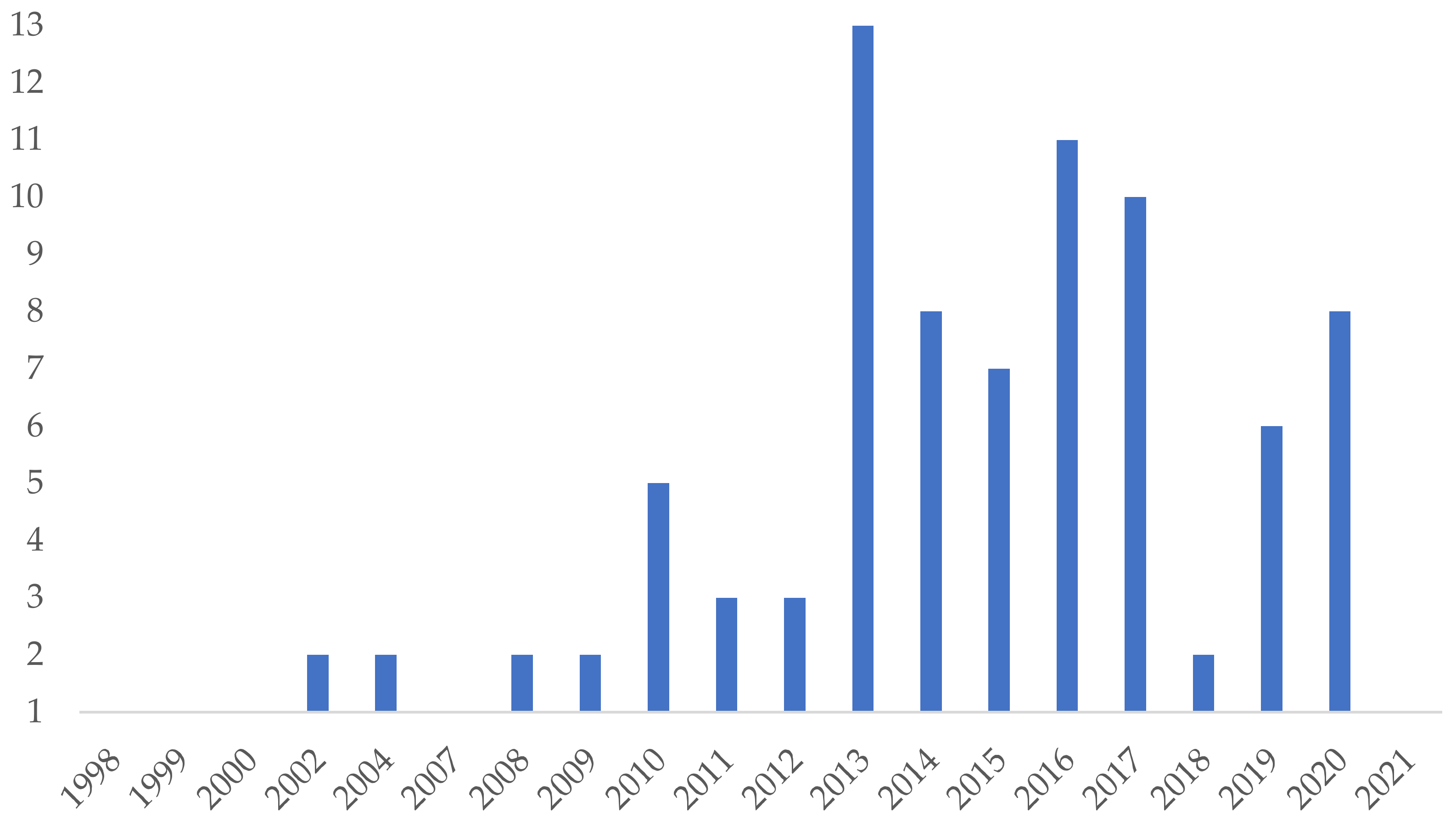
The topic under analysis is quite recent, particularly in the health field, but steadily growing, with an increase of 12.25% of articles per year. As shown in Figure 2, the majority of the publications are from 2013 (n = 13), increasing afterwards with two-thirds of the total of publications (n = 66).
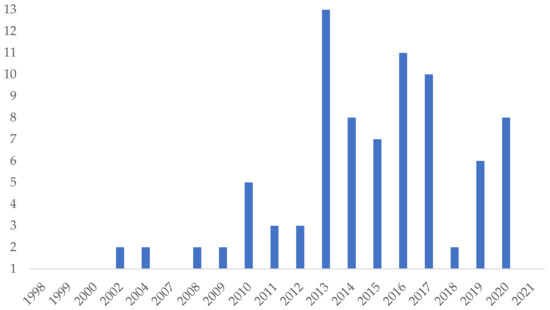
Figure 2.
Number of publications per year.
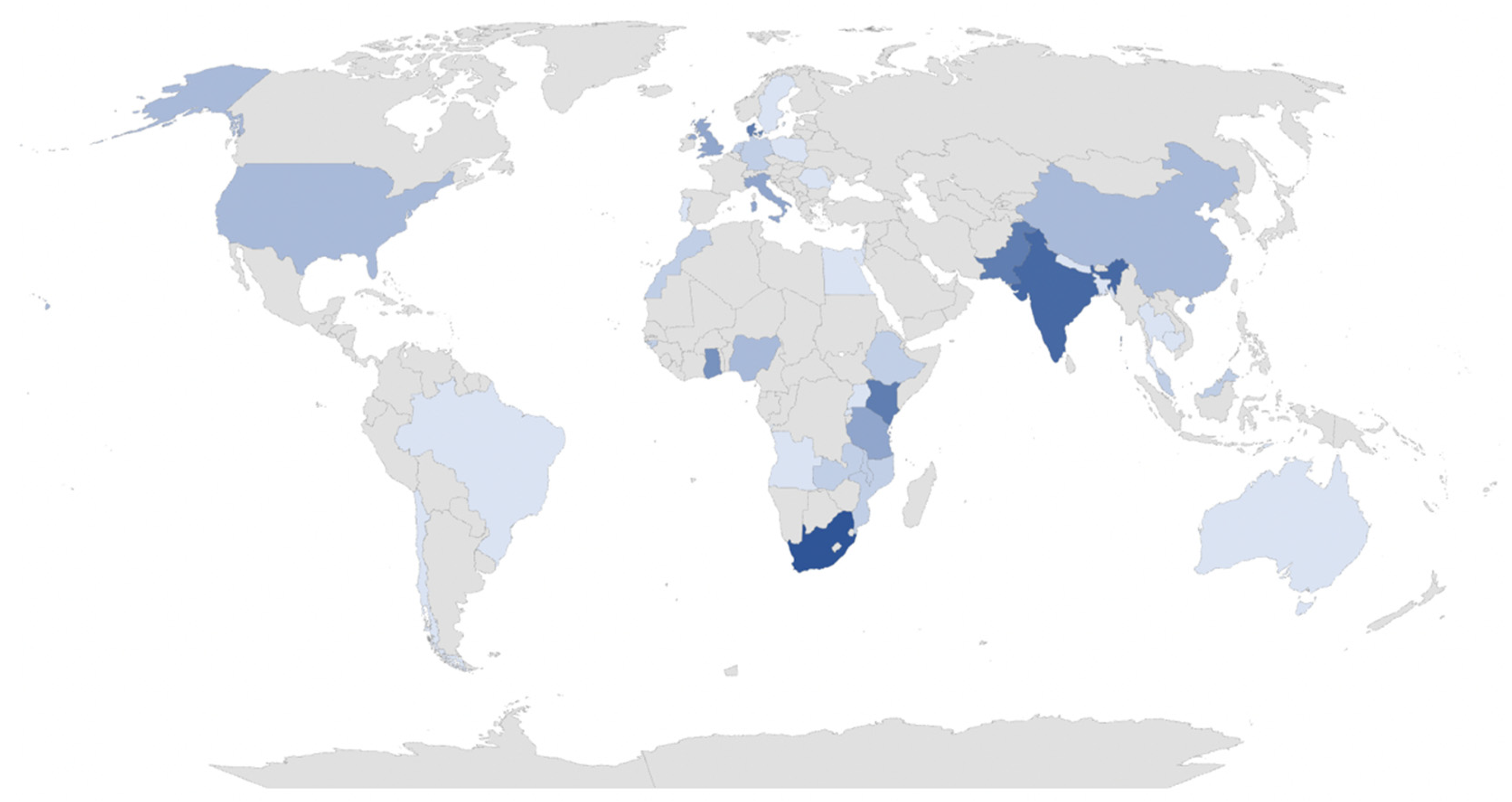
3.3. Countries
In our sample, the geographical distribution of the articles—based on the contexts of the study—suggest that the interest of PSM when applied to the health field shows a wide geographical dispersion (Table 4 and Figure 3). Interestingly, most of the studies are from non-WEIRD (White, Educated, Industrialized, Rich, and Democratic) samples, particularly African (40%, n = 36) and Asian (26.7%, n = 24) countries. European contexts are the least addressed (24.4%, n = 22). India (7.8%, n = 7), Pakistan (6.74%, n = 6), and Denmark (6.74%, n = 6) are the countries with the most publications on the topic.

Table 4.
Geographical distribution.
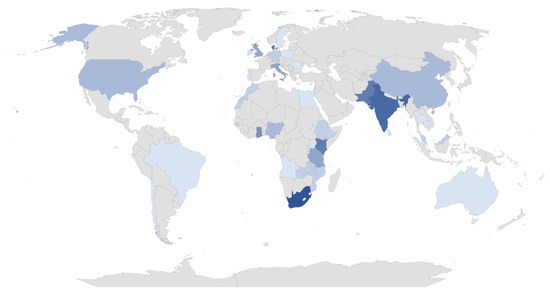
Figure 3.
Map with scientific dissemination per country (“Bibliometrix”).
The geographical analysis also shows a prevalence of Commonwealth countries. The interest shown may be due to human capital, i.e., the chronic lack of human resources in the health sector in some lesser-developed countries, particularly in Western Africa [13]. In addition, historically, many health professionals of the U.K. emigrated to English-speaking countries, such as South Africa, Pakistan, India, and Nigeria [35]. In Sub-Saharan African countries, and particularly in rural and remote areas, there are few human resources, driven by the often poor working conditions in those contexts [36]. On the other hand, Danish workers were considered the most satisfied in their workplace and can serve as an example for the health system/context and conditions in which they operate [37]. This being said, the distribution of countries involved in the research prevents us from generalizing and providing exact reasons.
3.4. Analysis of Scientific Collaboration
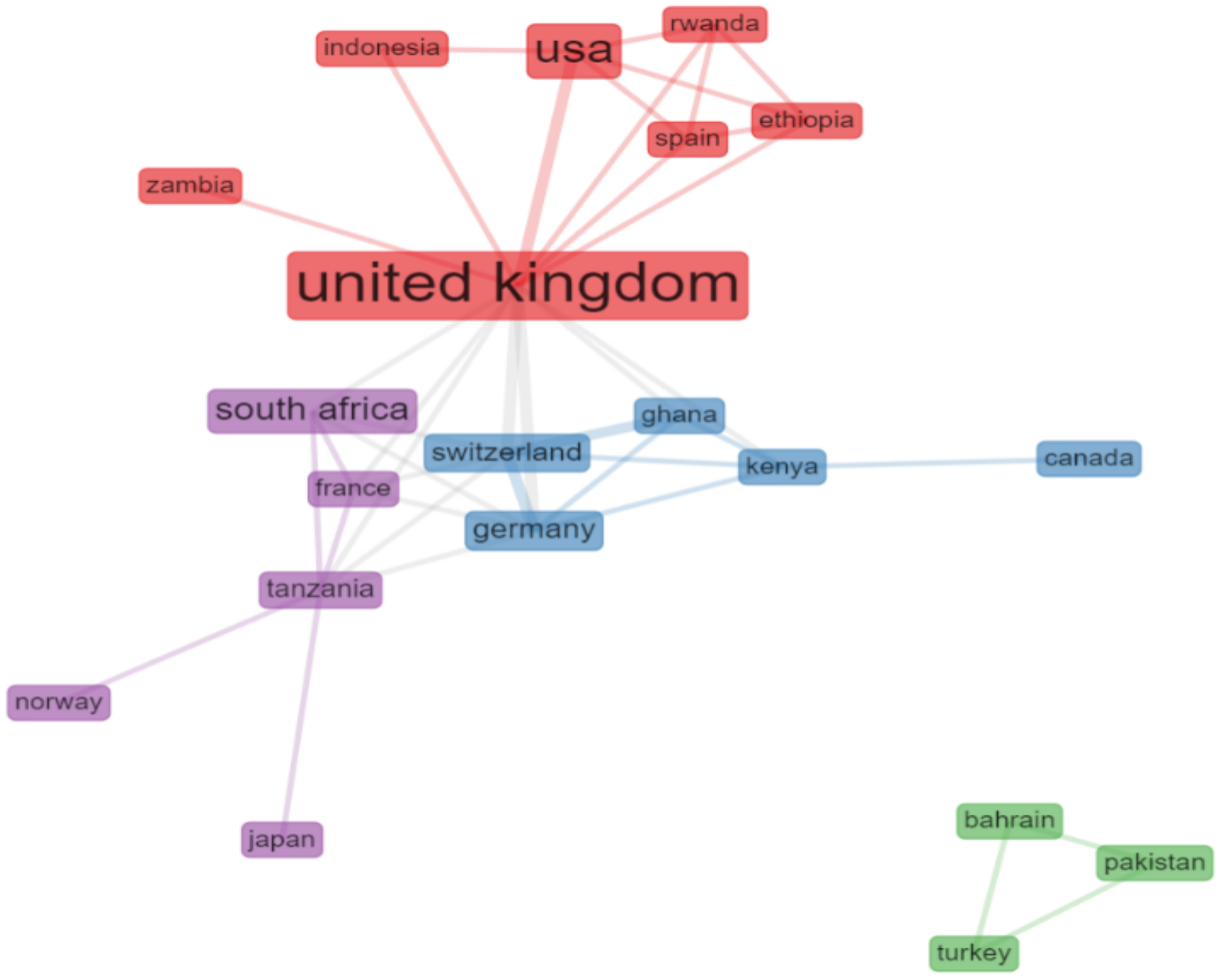
The more significant interactions between countries (Figure 4 and Table 5) and authors (Figure 4) are presented below, emphasizing links that represent co-authorships [38].
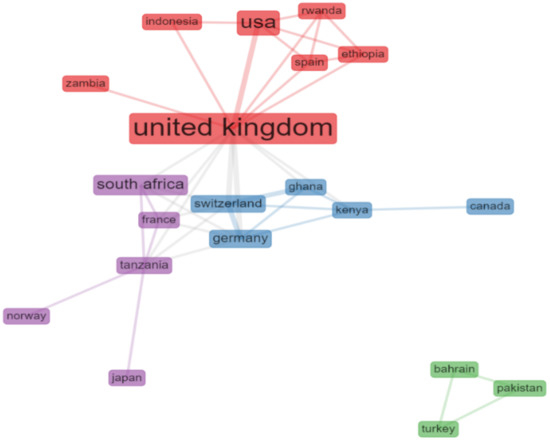
Figure 4.
Collaboration between countries (“Bibliometrix”).

Table 5.
Scientific production and collaboration between countries.
3.4.1. Cross-Country Collaboration
Collaboration between countries in these studies has its main central node in the U.K. (betweenness centrality = 71.083), followed by the USA, Germany, and Switzerland. These results corroborate the salience of the scientific field in Anglo-Saxon countries. Table 4 depicts the publications based on the main ten countries. Most are published within one country; among these, the U.K. and the USA present more publications and collaborations, with an MCP publication rate of 25%.
3.4.2. Collaboration among Authors
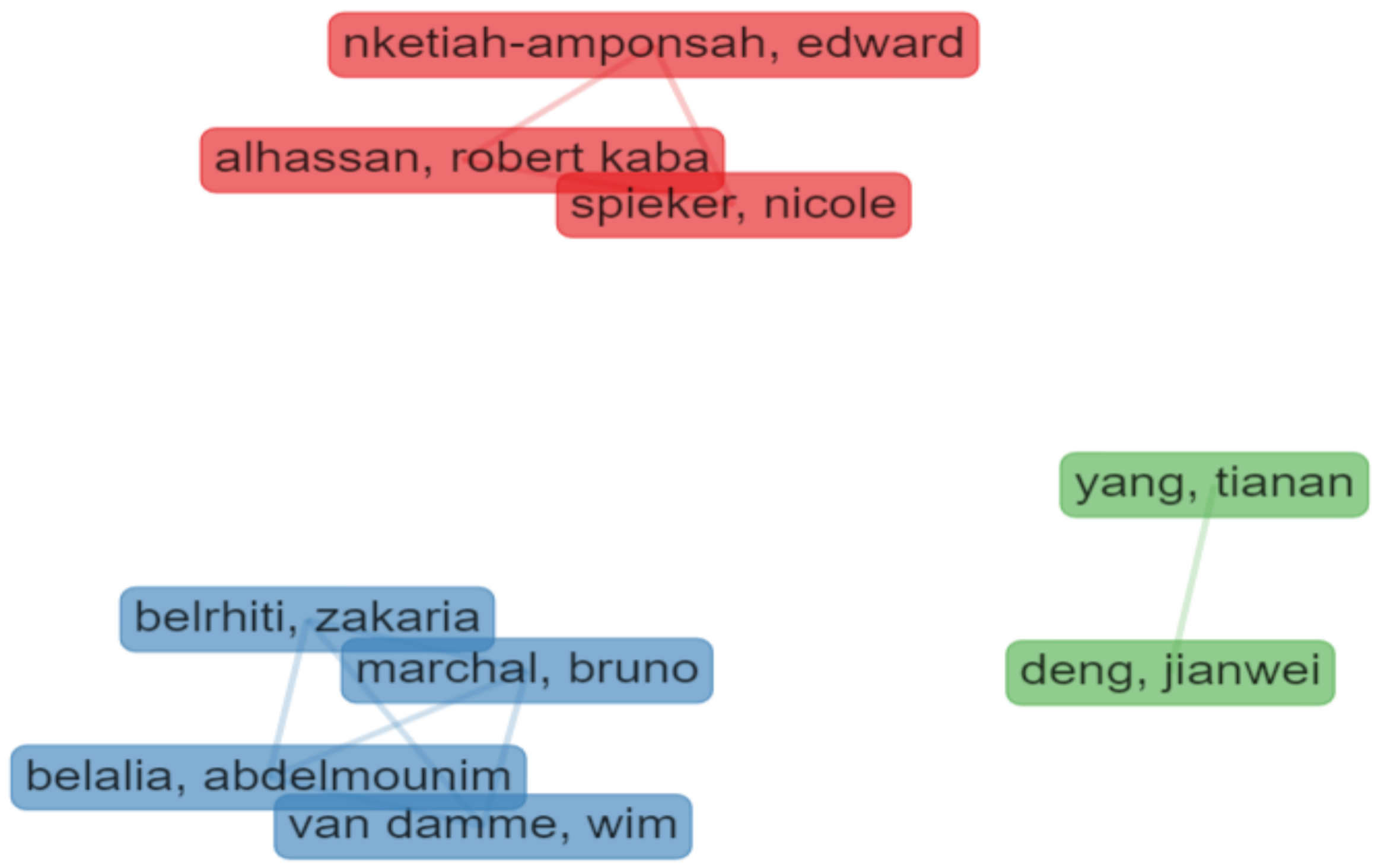
In the analysis of the authors’ collaborations, only one-shot collaborations were excluded (min. edge = 2), resulting in nine authors identified in three clusters (Figure 5):
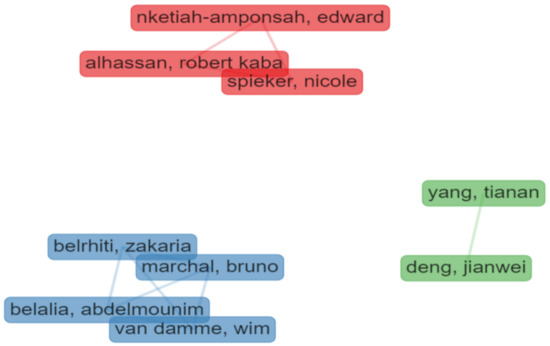
Figure 5.
Collaboration among authors (“Bibliometrix”).
- Cluster 1 (in blue) includes four authors from Morocco and Belgium and focuses on motivation and public sector choice;
- Cluster 2 (in red) includes three authors from The Netherlands and Ghana and mostly pays attention to the quality of health services and human resources; and
- Cluster 3 (in green) is based on two Chinese authors from the Institute of Technology in Beijing, focused on health policies management.
3.4.3. Co-Citation Analysis
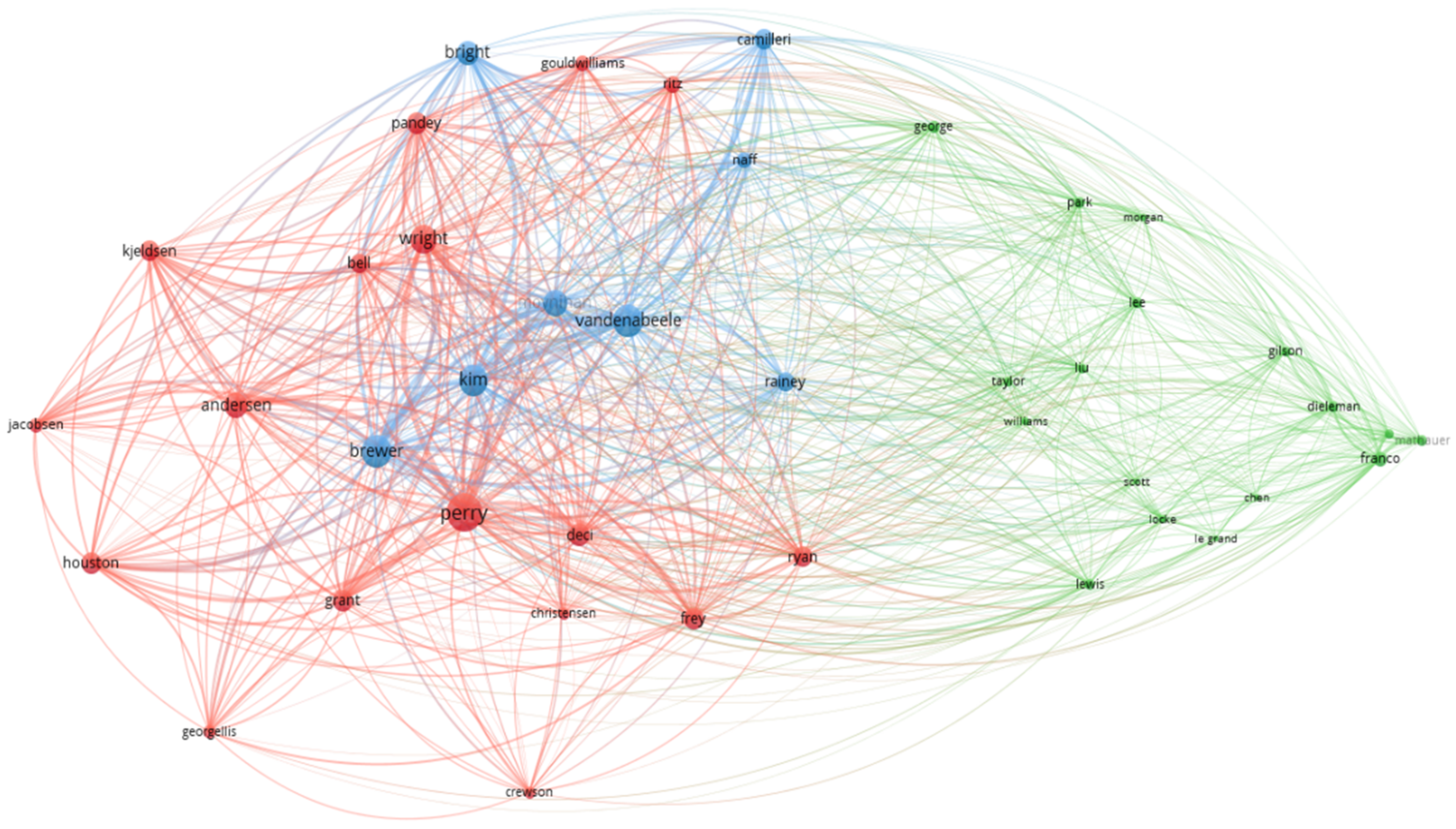
The co-citation analysis, representing the frequency of which two documents are cited together in the literature, thus being conceptually close to each other [39], is depicted in Figure 5. The items are represented by a label, pattern, and circle, the size of which is determined by the weight it has in the network, connected by the links (lines). Usually, the closer the authors, the stronger their co-citation link, which is also represented by the lines.
Their graphic representation is similar to the net visualization with three clusters, also represented by blue, green, and red (Figure 6). In Figure 6 and Table 6, the larger number of items corresponds to the more yellow and dense nodes. Three clusters (blue, red, and green) represent the data using the authors’ surnames. The interpretation of these data is described in Table 6.
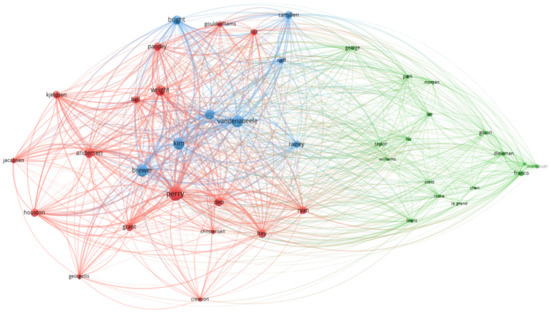
Figure 6.
Analysis of co-citations—authors.

Table 6.
Analysis of co-citations—authors by clusters (“Bibliometrix”).
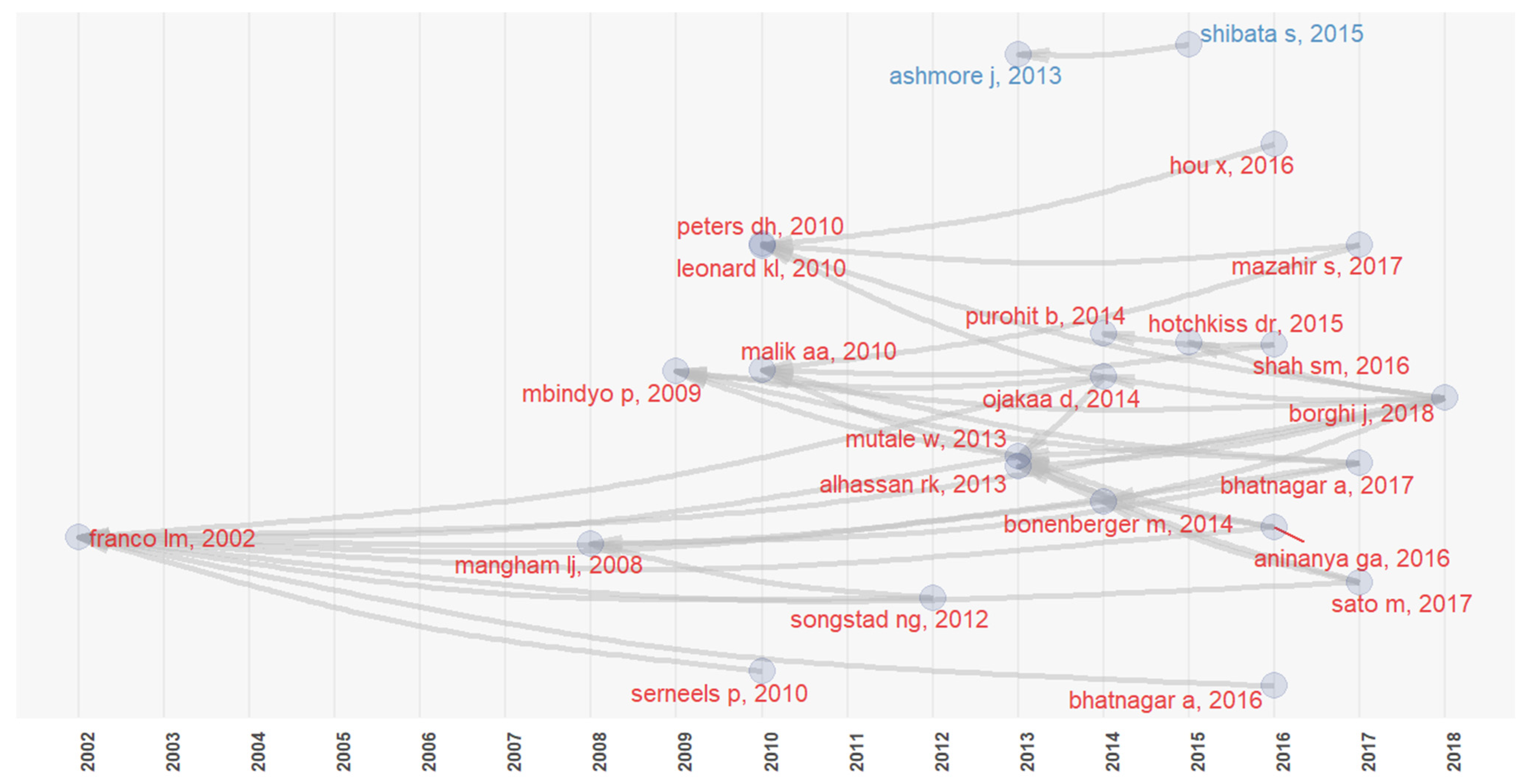
The historiographic analysis allows us to identify the research on a given topic while providing a graphic and genealogic presentation of the citation connections [40]. For each article, there is a Global Citation Score (GCS) as well as a Local Citation Score (LCS), which identifies the number of times the article is cited [39]. As shown in Figure 7, Franco et al. (2002) is the most referenced work (LCS = 10/GCS = 363), addressing the determinants of work motivation and the ways in which health sector reform may positively affect workers’ motivation. It is followed by Mutale et al. (2013) [41] (LCS = 5/GCS = 42), who evaluate the motivation shown by rural health workers, and Mbindyo et al. (2009) (LCS = 4/GCS = 81), who explore contextual influences on workers’ motivation and recommend a change in clinical practices in Kenyan hospitals.
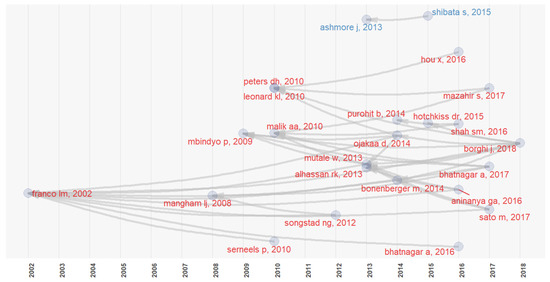
Figure 7.
Historiographic analysis (“Bibliometrix”).
3.5. Methodological Quality Assessment
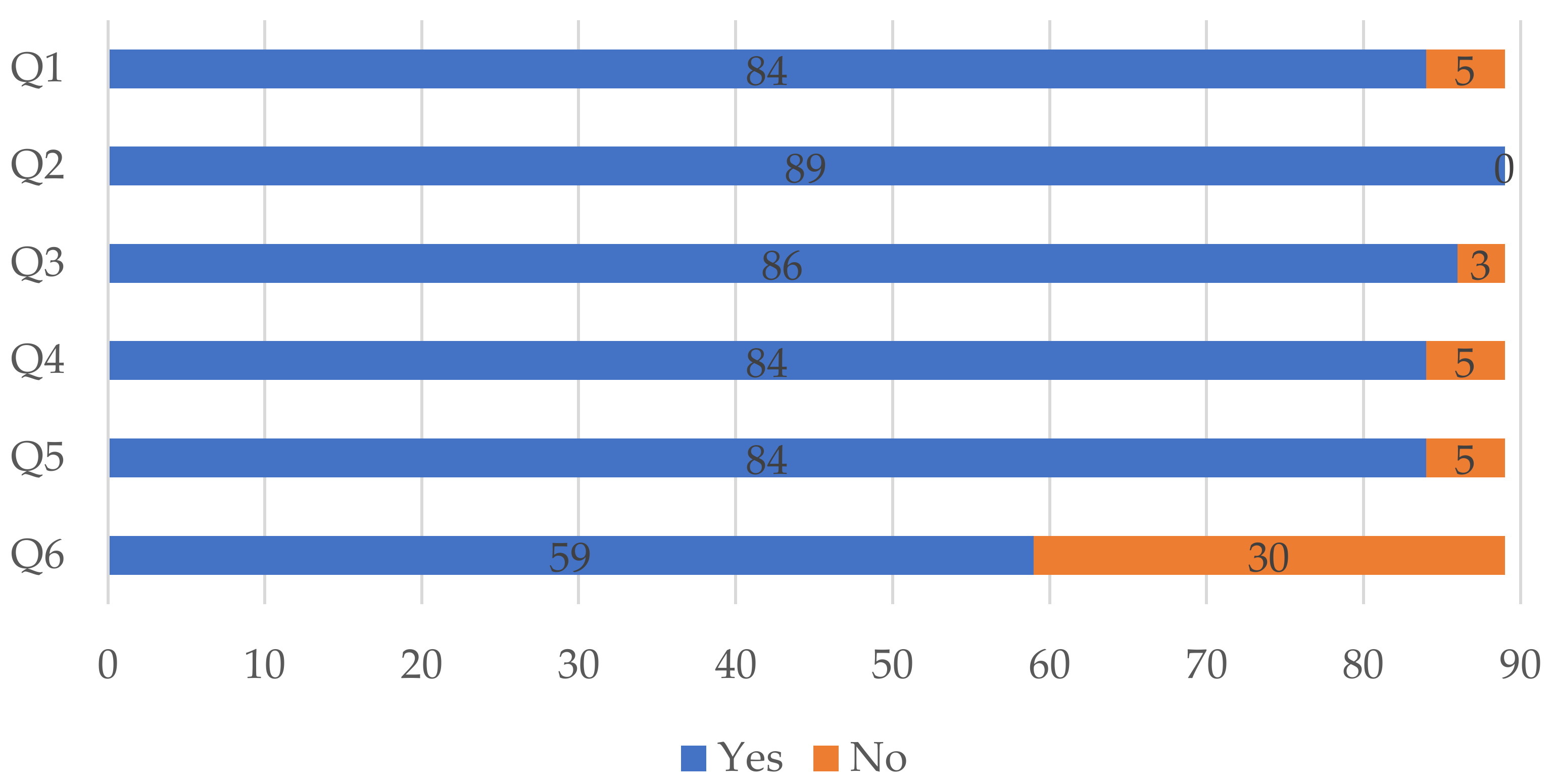
Overall, studies performed well according to the quality assessment checklist, as depicted graphically in Figure 8. Eighty-four studies clearly stated the aims of the conducted research (Q1), provided a clear and comprehensive description of the instruments and/or scales used (Q4), and presented a clear statement of the findings (Q5). All eighty-nine studies stated plainly the context of the study (Q2) and only three studies did not explicitly explain and use methods that supported the research in a clear manner (Q3). In turn, thirty studies did not discuss openly and extensively the limitations of their research (Q6).
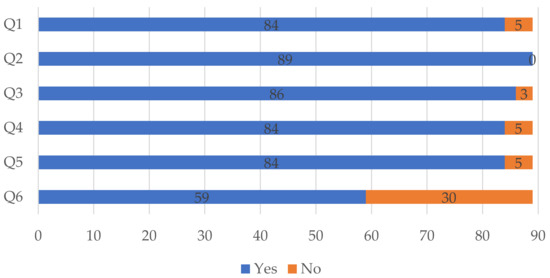
Figure 8.
Results of the quality assessment.
3.6. Object of Analysis
The majority of the studies (n = 56, 62.9%) analyze the public sector exclusively (62.9%, n = 56), while 34.8% (n = 31) compare public professionals with the private sector and only two focus on the private sector.
As for the nature of care, 34.8% (n = 31) are based on an analysis of professionals working at different care facilities, followed by an exclusive focus on hospital workforces (32.6%, n = 29). Some 13.48% (n = 12) studied primary care facilities and 12.4% (n = 11) address college students of health-related degrees (Table 7). The type of professionals in the institutions and in the articles of the study are presented in the Table 8.

Table 7.
Number of publications by main types of health care provision.

Table 8.
Type of professionals present in the articles.
3.7. Main Motivation Theories
The main motivation theories are addressed in 16 articles (Table 9). Four articles focus on Maslow’s Hierarchy of Needs (Maslow, 1943) [42] (n = 4) and the other theories—Self-Determination Theory (Deci and Ryan, 1985) [43], McClelland Theory (McClelland, 1960) [44], Herzberg Theory (Herzberg, 1959) [45], and the Job Characteristics Model (Hackman and Oldham, 1975) [46]—are addressed by three articles each. Table 10 briefly describes each one of these motivations’ theories.

Table 9.
Main theories addressed in the analyzed studies.

Table 10.
Brief description of the main motivation theories.
As shown in Table 9, most of these theories are needs-based theories of motivation, attempting to identify the drives and needs that motivate workers. These theories consider that motivated behavior is driven by individuals’ efforts to satisfy specific intrinsic needs. In turn, the Job Characteristics Model is the only one focusing more on the nature of the task.
It is curious, though, that in our sample, only a few studies are anchored in major theories of motivation. The lack of more theoretically cohesive research may result from the topic being addressed by several research areas, some of them intending to approach the topic more superficially or only in a descriptive fashion. It is also suggestive of a gap in health professionals’ motivation research regarding an integrated conceptual and methodological model tailored to this specific population group.
The main theories of motivation used attempt to identify content and processes that determine motivated behavior. Despite sometimes being referred to as theory (as in five of the articles analyzed), PSM is rather a construct that describes prosocial motivation to serve the public interest and help others. PSM antecedents are seen as focusing on five main factors that may also be shared by the other theories, namely, care, fairness, loyalty, authority, and sanctity [47].
3.8. Methods
Almost half of the studies (47.2%, n = 42) are exclusively quantitative, based on surveys, but a significant number are of a qualitative nature, namely interviews (24.7%, n = 22). These preferred instruments are combined solely with focus groups in 6.7% (n = 6) and altogether in three studies (Table 11).

Table 11.
Instruments of data collection.
3.9. Instruments Used to Measure Motivation and Related Constructs
The first assessment of the public service motivation scale was developed by Perry (1996) [12]. In our sample, only seven of the studies used this four-dimension scale, which was the first to measure this construct through four distinct dimensions: compassion, self-sacrifice, commitment to public interest, and attraction to public policy. It was later subjected to a transcultural adaptation (Kim et al., 2013) [13], involving 12 countries—Australia, Belgium, China, Denmark, France, Italy, South Korea, Lithuania, The Netherlands, Switzerland, the United Kingdom, and the United States—and the four dimensions were updated to attraction to public service, commitment to public values, compassion, and self-sacrifice.
Particularly, in the quantitative studies, there is a wide dispersion of the type of instruments used, addressing related constructs that impact the motivation of health professionals, including inflexible work schedules, long hours, and heavy workloads, which are known to cause high levels of stress and impair their motivation and efficiency. Thus, many of the scales employed do not measure motivation per se (as the PSM scale) but other factors that impact motivation at work. An example is the Challenge and Hindrance-Related Self-Reported Stress (C-HSS), with 11 items, six measuring stress-related challenges and five using stress-related obstacles. Developed by Cavanaugh (2000) [48] (n = 4), C-HSS addresses stress in relation to organizational responsibilities, position, insecurity, and resources. The Presenteeism Scale [49] also employed, in turn, addresses important processual and behavioral aspects of how health professionals feel at work, namely, the level of stress awareness, the pleasure in performing tasks, and the energy and concentration to conclude tasks, all important intrinsic motivators. On the other hand, the Job Satisfaction Scale [50] and Job Performance Scale [51] are also focused on important constructs that determine motivation, namely, satisfaction and performance evaluation, more in line with the process theories of motivation regarding behavior that attempt to identify the variables that may go into motivation. The assessment of related variables, and not the determinants of motivation themselves, may also explain the lack of more studies with a strong theoretical basis.
Forty-four studies employ instruments validated by other authors and 45 use instruments created by their own authors based on (i) the motivational constructs for public service and (ii) the intrinsic and extrinsic factors that health professionals value in the public or private sector. This profusion of adaptations, especially considering the wide geographical dispersion of the studies, impairs the further fine-tuning of major measurement tools as well as sound systematic comparisons between the same constructs.
3.10. Main Extrinsic and Intrinsic Factors
The main motivational factors mentioned by health professionals in the analyzed studies (see Table 12) are those associated with a concern at a pre-entry level in the public sector and present, overall, a clear negative valence, namely, low salaries (n = 47), few material resources and work conditions (n = 23), and frozen careers (n = 11). Only three cases are related to satisfaction with salary, career progression, and favorable work conditions, and only in seven cases is a suitable work environment reported, comprising general factors such as appropriate work conditions, financial incentives and bonuses, and professional recognition and respect from supervisors and patients.

Table 12.
Extrinsic motivation factors.
As for the main intrinsic motivational factors, reports on absenteeism are very common (n = 22) (see Table 13). Absenteeism is the recurrent absence of the worker during the normal schedule of daily work, a common reality in countries in Sub-Saharan Africa [52], which may be related to the location of health units in rural contexts with longer commuting, unpleasant and poor work environments, among other factors.

Table 13.
Intrinsic motivation factors.
However, overall, studies refer to other elements with a positive valence, namely, contact with patients (n = 21), work safety (n = 16), and the recognition of their work (n = 11).
4. Discussion of Intrinsic and Extrinsic Factors
4.1. Work Environment
The studies analyzed reveal that the lack of communication between coworkers in the workplace, the nature of the supervision, the personal values of the professionals, the low salaries, and the work conditions affect motivation and may promote an undesirable work environment (e.g., [46,47,48,49,50,51,52,53,54,55,56,57,58,59] (see Appendix A)).
A weak politics of recruitment may cause uneasiness [60]. As shown in article [50], there is a political interference in public sector hospitals’ management and, as such, a perceived better work environment in the private health sector. On the other hand, notwithstanding the better extrinsic work conditions in the private sector, article [61] postulates that health professionals of the NHS (British health system) do not necessarily exclude the public sector in their pursuit of a suitable work environment. Article [59] identifies inland areas as more prone to stressful work environments, particularly when basic conditions such as housing and comfortable commuting are lacking.
4.2. Career Progression
Eight studies [60,62,63,64,65,66,67,68,69] highlight that delays in career progressions are substantial demotivators, corroborating the motivational power of this particular reward. Regardless of external determinants (e.g., financial crisis or hospital management), to perceive chances of being promoted is an important motivator. The contrary affects career prospects and often influences the intention to migrate to more resourceful countries, especially among nurses and doctors [70,71]. On a lesser scale, this lack of progression is due to the lack of required professional qualifications and investment in updated professional training [63].
Another factor of tension between colleagues is the unfair promotion of a professional instead of another equally deserving. A promotion is a nuclear motivation factor, perceived as a way of growth, recognition, and advancement, and is hence interconnected with the self-esteem and personal and professional self-realization of workers [72].
4.3. Work Conditions
Work conditions are nuclear motivational factors, encompassing the physical space and physical resources that are fundamental to the activities conducted [5,42,45,57,59,60,64,73,74,75,76,77,78,79]. These are particularly impactful in rural areas.
A lack of electricity, necessary medicine and medical equipment, hospital materials (e.g., protection gloves, masks), and resources and degraded physical conditions of health units are the most commonly reported factors related to poor work conditions. The lack of essential goods, such as water, soap, and gloves, is described as a common reality in African countries [80]. In rural areas with few resources, the lack of supplies is often accompanied by poor equipment and infrastructure, which affects the work conditions and the workforce well-being (for example, the storage and preservation of food and water in extreme climacteric conditions) [81].
4.4. Remuneration
The most important motivational factor is undoubtedly the remuneration of health professionals. All studies mention this motivational factor as being detrimental to motivation as remuneration is perceived as lower than necessary or what would be fair. Thus, it is common for these professionals to work in both public and private sectors as a way to earn higher incomes. Article [34] states that the salary should be proportional to the work hours. Articles [60,62,72,73,82,83] emphasize the higher remuneration in the private sector and its impact on health professionals’ preference to work there, except for article [26], referring to the geographical context of India. At last, article [64] concluded that higher salaries are not associated with an increase in motivation, and that relationships among peers and with patients constitute the main motivational factor. Bratton et al., (2010) [84] also state that financial incentives should entail a particular group of rewards and not an isolated predictive factor. Furthermore, higher salaries should be accompanied by other rewards, such as more personal and professional stability, stronger peer relations, better work conditions, and work recognition.
4.5. Recognition, Self-Realization, and Responsibility
The articles [54,55,75,77,78,85,86,87,88,89] identify some intrinsic factors connected with higher levels of motivation. To be recognized and appreciated by supervisors, colleagues, and patients is a major reward attuned to a sense of value and contribution. The lack thereof is associated with less satisfaction and a worse work environment. Research on self-realization, work values, workplace commitment, work satisfaction, and performance have attracted ample research in recent decades [88], especially due to the relation between these key variables and engagement and work motivation [89,90,91].
4.6. Life-Long Learning and Professional Development
According to some studies (e.g., [55,59,60,66,78,92,93,94]), training programs and life-long learning are especially valued because they are perceived as important for the career progression of health professionals. The progress in their capacity and knowledgeability that may allow them to provide higher quality treatment enhances the motivational indexes, self-esteem, and strengthens the feeling of expected recognition by supervisors and patients. Health professionals describe the importance of ongoing training and updates with other professionals and physicians. In rural areas in developing countries, the lack of education training and qualification available to health professionals is highlighted.
5. Summary of Main Findings
This sample, retrieved from three databases, reflects the vitality of this field of inquiry, including a considerable number of articles with an increase of more than 12% per year. This is suggestive of a timely focus on health professionals’ motivation from the perspective of public administration and health management. Among the analyzed articles, four are conceptual and draw on document analysis and secondary data analysis. However, only a small portion draws on theories of motivation or more solid conceptual bases. Eighty-five articles (95.5%) analyze empirical data collected, quantitative methodology being the most frequent approach.
The collaboration among authors, besides highlighting the salience of the Anglo-Saxon-based scientific production, speaks favorably about the internationalization of this research, mostly on the following topics: motivation and public sector choice, the quality of health services and human resources, and health policy management. The analysis of co-citations shows stronger cross-country and continental links in three main research areas: PSM and organization management, motivation and organizational behavior, and policies for health motivation.
The focus on the field of health and its professionals derives from job requirements, financial and non-financial incentives, career opportunities, and continuous investment in education to maintain the quality and equity of their work [22].
Overall, Perry is the most relevant author, being connected to most of the publications given his role in developing and disseminating the concept of PSM, of which the scale of 24 items is one of the outputs [1]. Still, the majority of the researchers developed their own instrument combining items of several scales, of which the most common is Perry’s (1996). For instance, a transcultural adaptation of this scale was developed and applied by Kim et al. (2013), with an update of the four dimensions to attraction to public service, commitment to public values, compassion, and self-sacrifice. However, many of the scales employed do not measure motivation per se (as the PSM scale) but other factors that impact motivation at work. Examples include Challenge and Hindrance-related Self-Reported Stress—C-HSS [36], the Presenteeism Scale [37], and the Job Performance Scale [51]. There is, however, a wide dispersion of measurements and adaptations that impair a more systematic and robust comparison of factors and contexts.
In the analyzed studies, interestingly, the African continent is the most represented one, which can result from the scarcity of health professionals and material resources [25]. It is followed by Asia and Europe, with emphasis on the United Kingdom and the lack of human capital in the British health system [95].
More than half the studies draw on the public sector of health (n = 56), with 31 comparing both and two circumscribed to the private health sector. Although such results may be expected, the fact that the clear sectoral divide (public vs. private) has been undermined in recent decades (mainly due to the implementation of the NPM principles in the public sector, resulting in a broader definition of public service to include all forms of occupation that serve the community and not just those employed by the government directly, could reveal a different pattern of research, i.e., with more focus on the private sector instead. As far as PSM is concerned, although originally associated with public institutions and organizations, it has been argued that it applies to the private sector, as well, when it targets public interest.
Despite the variations according to geographical contexts and specific organizational cultures, there are common denominators affecting health employees’ motivation and work engagement that intertwine other-oriented and self-oriented motives. The more common elements refer to remuneration, available resources and working conditions, absenteeism, and frequency of contact and interaction with patients. All of the above adopt a more individualistic perspective of the health worker in relation to his/her professional work/context specificities and less of an organization-based viewpoint related to career development in the institution or management/leadership approaches.
Partially explained by the sample composition, these main motivational elements are reported in a more negative light (e.g., low salaries, lack of resources, and absenteeism). On the other hand, the recognition and valorization of their work by supervisors and patients is consensually seen as relevant, even more by health workers from less resourceful settings, as is the case in rural areas and developing countries.
The structural and chronic limitations that characterize those contexts may explain that, instead of physical and material incentives and conditions beyond personal control, stronger individual-based determinants are privileged, as symbolic and identity-based notions of contribution, respect, and recognition, altogether reflecting the inherent sense of value of health care provision.
Being consensually regarded as important factors in the motivation of health workers, health and public administration institutions should prioritize these criteria through direct and indirect mechanisms, assuring health workers that their efforts and contributions to society are clearly valued and recognized.
6. Final Remarks
Research on Public Service Motivation (PSM) started with an exploratory conceptual approach three decades ago [1,45,96]. With the evolution of the research stream, PSM gradually anchored in organizational management and policies. However, overall, it seems that the research on PSM in the field of health and human resources is gauging more attention in recent years, as shown by the increasing number of publications in diverse geographical realities. Focused on health professionals’ motivation, this study contributes a timely and useful systematization during the current challenging times for health institutions and their human resources. Its contribution is threefold: (i) the analysis of the scientific production meta data informs an integrated “shadow history” of this topic; (ii) the identification of the most productive authors and countries/regions provides well-founded insights into their cooperation networks and dynamics; and (iii) the characterization of the most relevant themes, topics, determining factors of motivation, and cultural patterns indicates future research avenues.
As with other methods, this systematic literature review presents limitations that should be considered in further studies. First, the selected documents only include those written in English, leaving aside (few) documents referring to more specific or endogenous contexts that can enrich further analyses. Second, only articles were considered, overlooking potential interesting contributions from other types of sources. Third, the geo-cultural heterogeneity of the sample impairs a more robust comparison between the interaction of motivational factors with specific cultural contexts and respective health policies and work conditions.
The lack of more cohesive theoretical and methodological approaches to address health professionals’ motivation, as shown in this study, reflects a somewhat loose and fragmented approach to this issue. The development of an overarching conceptual approach of motivation of health professionals, including a specific measure validated and adapted to specific geo-cultural contexts, would significantly benefit this line of research. A systematic comparison within countries with similar geo-cultural contexts (for example, samples from WEIRD and developing contexts) could contribute to identify the moderation role of specific healthcare contexts and policies in health workers’ motivation. It may also provide useful insight on how motivation is modeled by specific cultural context expectations and socio-economic conditions, strengthening the need to approach it from a socio-psychological perspective. Future research would also benefit from a transcultural framework since, as evident in the current pandemic, there are many common denominators motivating and shaping health care workers’ commitment to their professions.
Author Contributions
Conceptualization, A.F., G.S., and T.F.; methodology, A.F., G.S., and T.F.; writing—original draft preparation, A.F., G.S., and T.F.; results, A.F., G.S., and T.F.; writing—review and editing, A.F., G.S., and T.F. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Fundação para a Ciência e Tecnologia, grant number 020.05144.BD, and partially funded by Programa Operacional Centro 2020, through Fundo Social Europeu.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The review used existing research data.
Acknowledgments
Gonçalo Santinha and Alexandre Fernandes would like to acknowledge the contribution of the research unit on Governance, Competitiveness, and Public Policy (UIDB/04058/2020), funded by national funds through FCT—Portuguese Foundation for Science and Technology.
Conflicts of Interest
The authors declare no conflict of interest.
Appendix A
| Authors | Year | Remuneration | Work Environment/ Work Conditions | Life-Long Learning/ Professional Development | High Workload | Absenteeism | Altruism | Job Security | Recognition of Work | Responsibility/ Autonomy |
| Jiang et al. [97] | 2021 | x | ||||||||
| Stefurak et al. [98] | 2020 | x | ||||||||
| Cantarelli et al. [85] | 2020 | x | x | x | x | |||||
| Ebenso et al. [99] | 2020 | x | x | |||||||
| Jensen et al. [100] | 2020 | x | x | x | x | x | ||||
| Belrhiti et al. [86] | 2020 | x | x | |||||||
| Androniceanu et al. [73] | 2020 | x | x | x | ||||||
| Abdelmotaleb et al. [101] | 2020 | x | x | |||||||
| van Loon et al. [102] | 2020 | x | x | |||||||
| Belrhiti et al. [86] | 2019 | x | x | x | x | |||||
| Deng et al. [103] | 2019 | x | ||||||||
| Deng et al. [104] | 2019 | x | x | |||||||
| Adams et al. [105] | 2019 | x | x | |||||||
| Prust et al. [75] | 2019 | x | x | x | ||||||
| Chang et al. [63] | 2019 | x | x | x | ||||||
| Borghi, et al. [106] | 2018 | x | x | |||||||
| Zweigenthal et al. [107] | 2018 | x | x | |||||||
| Aguilera et al. [108] | 2017 | x | ||||||||
| Abera et al. [109] | 2017 | x | x | x | ||||||
| Masood et al. [110] | 2017 | x | ||||||||
| Levitats et al. [111] | 2017 | x | ||||||||
| Millar et al. [112] | 2017 | x | x | x | x | |||||
| Sato et al. [75] | 2017 | x | x | x | ||||||
| Korlén et al. [76] | 2017 | x | x | x | ||||||
| Bhatnagar et al. [42] | 2017 | x | x | x | ||||||
| Seth [113] | 2017 | x | x | |||||||
| Mazahir et al. [77] | 2017 | x | x | |||||||
| Hou et al. [114] | 2016 | x | x | x | ||||||
| Russo et al. [82] | 2016 | x | ||||||||
| Bhatnagar and George [115] | 2016 | x | x | x | ||||||
| Shah et al. [116] | 2016 | x | x | x | x | x | ||||
| Alhassan et al. [64] | 2016 | x | x | x | x | |||||
| Namakula et al. [117] | 2016 | x | x | |||||||
| Bansal and Malhotra [71] | 2016 | x | x | x | ||||||
| Van Loon [118] | 2016 | x | x | x | ||||||
| Kadam et al. [119] | 2016 | x | x | |||||||
| Aninanya et al. [87] | 2016 | x | x | x | ||||||
| Khim [55] | 2016 | x | x | x | x | |||||
| Mir et al. [61] | 2015 | x | x | |||||||
| Hotchkiss et al. [53] | 2015 | x | x | x | x | |||||
| Gasiorowski et al. [56] | 2015 | x | x | x | x | |||||
| Ashmore and Gilson [120] | 2015 | x | ||||||||
| Shibata et al. [92] | 2015 | x | x | |||||||
| Bellé [121] | 2015 | x | ||||||||
| Schmiedeknecht et al. [122] | 2015 | x | x | x | x | x | ||||
| Russo et al. [123] | 2014 | x | x | x | ||||||
| Bonenberger et al. [65] | 2014 | x | x | x | ||||||
| Ojakaa et al. [57] | 2014 | x | x | x | x | |||||
| Hennig-Schmidt and Wiesen [124] | 2014 | x | x | |||||||
| Purohit et al. [66] | 2014 | x | x | x | x | x | x | |||
| Lagarde and Blaauw [125] | 2014 | x | ||||||||
| Krogsgaard et al. [126] | 2014 | x | ||||||||
| Schott and Pronk [127] | 2014 | x | x | x | ||||||
| Diwan et al. [128] | 2013 | x | x | x | ||||||
| Alhassan et al. [129] | 2013 | x | x | x | ||||||
| Kolstad et al. [130] | 2013 | x | ||||||||
| Ghimire et al. [57] | 2013 | x | x | x | x | x | ||||
| George et al. [131] | 2013 | x | x | x | ||||||
| Mutale et al. [93] | 2013 | x | x | x | x | |||||
| Dos Santos et al. [132] | 2013 | x | ||||||||
| Bellé [133] | 2013 | x | ||||||||
| van Loon et al. [134] | 2013 | x | ||||||||
| Chew et al. [67] | 2013 | x | x | |||||||
| Mariappan [135] | 2013 | x | x | x | x | |||||
| Ashmore [68] | 2013 | x | x | |||||||
| Andersen et al. [136] | 2013 | x | x | x | x | x | ||||
| Songstad et al. [137] | 2012 | x | x | x | x | |||||
| Waitzkin H. et al. [69] | 2012 | x | x | x | ||||||
| Kjeldsen [138] | 2012 | x | ||||||||
| Georgellis et al. [139] | 2011 | x | ||||||||
| Aysen and Parumasur [140] | 2011 | x | x | x | ||||||
| Halepota and Shah [95] | 2011 | x | x | x | ||||||
| Leonard and Masatu [141] | 2010 | x | x | x | x | |||||
| Peters et al. [59] | 2010 | x | x | x | ||||||
| Malik et al. [142] | 2010 | x | x | x | x | x | x | |||
| Serneels et al. [143] | 2010 | x | ||||||||
| Le Julian [144] | 2010 | x | ||||||||
| Mbindyo et al. [67] | 2009 | x | x | x | x | x | x | x | ||
| Andersen [145] | 2009 | x | ||||||||
| Mangham and Hanson [146] | 2008 | x | x | |||||||
| Modipa and Dambisya [147] | 2008 | x | ||||||||
| Dambisya et al. [79] | 2007 | x | x | x | x | |||||
| Agyepong et al. [148] | 2004 | x | x | x | x | |||||
| Humphrey and Russell [62] | 2004 | x | x | x | ||||||
| Franco et al. [89] | 2002 | x | x | x | x | |||||
| Lee-Ross [149] | 2002 | x | x | |||||||
| Pipan [150] | 2000 | x | ||||||||
| Smith [94] | 1999 | x | x | x | ||||||
| Ferrinho et al. [83] | 1998 | x | x |
References
- Perry, J.L.; Wise, L. The motivational bases of public service. Public Adm. Rev. 1990, 50, 367–373. [Google Scholar]
- Ritz, A.; Brewer, G.A.; Neumann, O. Public Service Motivation: A Systematic Literature Review and Outlook. Public Adm. Rev. 2016, 76, 414–426. [Google Scholar]
- Waterhouse, J. Motivation in Public Management: The Call of Public Service. Aust. J. Public Adm. 2008, 67, 505–507. [Google Scholar]
- O’Riordan, J. Public Service Motivation: State of Public Service Series. Inst. Public Adm. 2013, 1–36. [Google Scholar]
- George, A.; Scott, K.; Govender, V. A Health Policy and Systems Research Reader on Human Resources for Health; World Health Organization: Geneva, Switzerland, 2017; pp. 1–528. [Google Scholar]
- Dieleman, M.; Gerretsen, B.; van der Wilt, G. Human resource management interventions to improve health workers’ performance in low and middle income countries: A realist review. Health Res. Policy Syst. 2009, 7, 7. [Google Scholar]
- Lee, M.T.; Raschke, R.L. Understanding employee motivation and organizational performance: Arguments for a set-theoretic approach. J. Innov. Knowl. 2016, 1, 162–169. [Google Scholar]
- Santinha, G.; Carvalho, T.; Forte, T.; Fernandes, A.; Tavares, J. Profiling Public Sector Choice: Perceptions and Motivational Determinants at the Pre-Entry Level. Sustainability 2021, 13, 1272. [Google Scholar]
- Collins, B. What’s the problem in Public Sector workforce recruitment? A comparative analysis of the public, non-profit, and private sectors. Int. J. Public Adm. 2008, 31, 1592–1608. [Google Scholar]
- French, P.; Emerson, M. Assessing the Variations in Reward Preference for Local Government Employees in Terms of Position, Public Service Motivation, and Public Sector Motivation. Public Perform. Manag. Rev. 2014, 37, 552–576. [Google Scholar]
- Rainey, H.G. Reward preferences among public and private managers: In search of the service ethic. Am. Rev. Public Adm. 1982, 16, 288–302. [Google Scholar]
- Perry, J.L. Measuring Public Service Motivation: An Assessment of Construct Reliability and Validity. J. Public Adm. Res. Theory 1996, 6, 5–22. [Google Scholar]
- Kim, S.; Vandenabeele, W.; Wright, B.E.; Andersen, L.B.; Cerase, F.P.; Christensen, R.K.; Desmarais, C.; Koumenta, M.; Leisink, P.; Liu, B.; et al. Investigating the Structure and Meaning of Public Service Motivation across Populations: Developing an International Instrument and Addressing Issues of Measurement Invariance. J. Public Adm. Res. Theory 2013, 23, 79–102. [Google Scholar]
- Paarlberg, L.E.; Perry, J.L. Values Management: Aligning Employee Values and Organization Goals. Am. Rev. Public Adm. 2007, 37, 387–408. [Google Scholar]
- Miao, Q.; Eva, N.; Newman, A.; Schwarz, G. Public service motivation and performance: The role of organizational identification. Public Money Manag. 2019, 39, 77–85. [Google Scholar]
- Breaugh, J.; Ritz, A.; Alfes, K. Work motivation and public service motivation: Disentangling varieties of motivation and job satisfaction. Public Manag. Rev. 2018, 20, 1423–1443. [Google Scholar]
- O’Leary, C. Public Service Motivation: A Rationalist Critique. Public Pers. Manag. 2019, 48, 82–96. [Google Scholar]
- Legault, L. Intrinsic and Extrinsic Motivation. In Encyclopedia of Personality and Individual Differences; Zeigler-Hill, V., Shackelford, T., Eds.; Springer: Cham, Switzerland, 2016. [Google Scholar]
- Lewis, B.G.; Frank, S.A. Who Wants to Work for the Government? Public Adm. Rev. 2002, 62, 395–404. [Google Scholar]
- Okello, D.R.; Gilson, L. Exploring the influence of trust relationships on motivation in the health sector: A systematic review. Hum. Resour. Health 2015, 13, 16. [Google Scholar]
- Fritzen, S. Strategic management of the health workforce in developing countries: What have we learned? Hum. Res. Health 2007, 5, 4. [Google Scholar]
- Campbell, J.; Dussault, G.; Buchan, J.; Pozo-Martin, F.; Guerra, M.G.; Leone, C.; Siyam, A.; Cometto, G. A Universal Truth: No Health without a Workforce. Forum Report, Third Global Forum on Human Resources for Health; Global Health Workforce Alliance and World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- Muthuri, R.; Senkubuge, F.; Hongoro, C. Determinants of Motivation among Healthcare Workers in the East African Community between 2009–2019: A Systematic Review. Healthcare 2020, 8, 164. [Google Scholar]
- World Health Organization. Health Workforce Policy and Management in the Context of the COVID-19 Pandemic Response: Interim Guidance; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Kunisch, S.; Menz, M.; Bartunek, J.M.; Cardinal, L.B.; Denyer, D. Feature topic at organizational research methods: How to conduct rigorous and impactful literature reviews? Organ. Res. Methods 2018, 21, 519–523. [Google Scholar]
- Dixon-Woods, M.; Bonas, S.; Booth, A.; Jones, D.R.; Miller, T.; Sutton, A.J.; Shaw, R.; Smith, J.; Young, B. How can systematic reviews incorporate qualitative research? A critical perspective. Qual. Res. 2006, 6, 27–44. [Google Scholar]
- Cooper, H. Research Synthesis and Meta-Analysis, 4th ed.; Sage Publications: Thousand Oaks, CA, USA, 2010. [Google Scholar]
- Migchelbrink, K.; Van de Walle, S. A systematic review of the literature on determinants of public managers’ attitudes toward public participation. Local Gov. Stud. 2021, 48, 1–22. [Google Scholar]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.P.; Devereaux, J.; Kleijnen, J.; Moher, D. The PRISMA Statement for Reporting Systematic Reviews and Meta-analyses of Studies that Evaluate Health Care Interventions: Explanation and Elaboration. J. Clin. Epidemiol. 2009, 62, e1–e34. [Google Scholar]
- Shamseer, L.; Moher, D.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: Elaboration and explanation. BMJ 2015, 4, 1. [Google Scholar]
- Pitchforth, E.; Nolte, E.; Corbett, J.; Miani, C.; Winpenny, E.; van Teijlingen, E.; Elmore, N.; King, S.; Ball, S.; Miler, J.; et al. Community hospitals and their services in the NHS: Identifying transferable learning from international developments—Scoping review, systematic review, country reports and case studies. NIHR J. Libr. 2017, 5, 1–220. [Google Scholar]
- Yang, L.; Zhang, H.; Shen, H.; Huang, X.; Zhou, X.; Rong, G.; Shao, D. Quality Assessment in Systematic Literature Reviews: A Software Engineering Perspective. Inf. Softw. Technol. 2020, 130, 106397. [Google Scholar]
- Critical Appraisal Skills Programme (2013) CASP Checklist. Available online: https://casp-uk.net/casp-tools-checklists/ (accessed on 2 January 2022).
- Health Evidence. Quality Assessment Tool—Review Articles. Available online: https://healthevidence.org/practice-tools.aspx#PT1 (accessed on 2 January 2022).
- Wismar, M.; Maier, C.B.; Glinos, I.A.; Dussault, G.; Figueras, J. Health Professional Mobility and Health Systems: Evidence from 17 European Countries; European Observatory on Health Systems and Policies, WHO: Geneva, Switzerland, 2011. [Google Scholar]
- Mathauer, I.; Imhoff, I. Health Worker Motivation in Africa: The Role of Non-Financial Incentives and Human Resource Management Tools. Hum. Resour. Health 2006, 4, 24. [Google Scholar]
- Eskildsen, J.K.; Kristensen, K.; Westlund, A.H. Work motivation and job satisfaction in the Nordic countries. Empl. Relat. 2004, 26, 122–136. [Google Scholar]
- Abbasi, A.; Hossain, L.; Uddin, S.; Rasmussen, K.J. Evolutionary dynamics of scientific collaboration networks: Multi-levels and cross-time analysis. Scientometrics 2011, 89, 687–710. [Google Scholar]
- Trujillo, C.M.; Long, T.M. Document co-citation analysis to enhance transdisciplinary research. Sci. Adv. 2018, 4, e1701130. [Google Scholar]
- Garfield, E.; Pudovkin, A.I.; Istomin, V.S. Why do we need algorithmic historiography? J. Am. Soc. Inf. Sci. Technol. 2003, 54, 400–412. [Google Scholar]
- Mutale, W.; Ayles, H.; Bond, V.; Mwanamwenge, M.T.; Balabanova, D. Measuring Health Workers’ Motivation in Rural Health Facilities: Baseline Results from Three Study Districts in Zambia. Hum. Resour. Health 2013, 11, 8. [Google Scholar]
- Maslow, A.H. A theory of human motivation. Psychol. Rev. 1943, 50, 370–396. [Google Scholar]
- Deci, E.L.; Ryan, R.M. Self-Determination Theory: When Mind Mediates Behavior. J. Mind Behav. 1980, 1, 33–43. [Google Scholar]
- McClelland, C.A. The function of theory in international relations. J. Confl. Resolut. 1960, 4, 303–336. [Google Scholar]
- Herzberg, F.; Mausner, B.; Snyderman, B. The Motivation to Work, 2nd ed.; Wiley: Hoboken, NJ, USA, 1959. [Google Scholar]
- Hackman, J.R.; Oldham, G.R. Development of the job diagnostic survey. J. Appl. Psychol. 1975, 60, 159–170. [Google Scholar]
- Wang, T.M.; Witteloostuijn, A.; Heine, F. A Moral Theory of Public Service Motivation. Front. Psychol. 2020, 11, 517763. [Google Scholar]
- Cavanaugh, M.A.; Boswell, W.R.; Roehling, M.V.; Boudreau, J.W. An empirical examination of self-reported work stress among U.S. managers. J. Appl. Psychol. 2000, 85, 65–74. [Google Scholar]
- Koopman, C.; Pelletier, K.R.; Murray, J.F.; Sharda, C.E.; Berger, M.L.; Turpin, R.S.; Hackleman, P.; Gibson, P.; Holmes, D.M.; Bendel, T. Stanford presenteeism scale: Health status and employee productivity. J. Occup. Environ. Med. 2002, 44, 14–20. [Google Scholar]
- Vandenabeele, W. The mediating effect of job satisfaction and organizational commitment on self-reported performance: More robust evidence of the PSM-performance relationship. Int. Rev. Adm. Sci. 2009, 75, 11–34. [Google Scholar]
- Naff, K.C.; Crum, J. Working for America: Does Public Service Motivation Make a Difference? Rev. Public Pers. Adm. 1999, 19, 5–16. [Google Scholar]
- Belita, A.; Mbindyo, P.; English, M. Absenteeism amongst Health Workers—Developing a Typology to Support Empiric Work in Low-Income Countries and Characterising Reported Associations. Hum. Resour. Health 2013, 11, 34. [Google Scholar]
- Hotchkiss, D.R.; Banteyerga, H.; Tharaney, M. Job Satisfaction and Motivation among Public Sector Health Workers: Evidence from Ethiopia. Hum. Resour. Health 2015, 13, 83. [Google Scholar]
- Bhatnagar, A.; Gupta, S.; Alonge, O.; George, A.S. Primary Health Care Workers’ Views of Motivating Factors at Individual, Community and Organizational Levels: A Qualitative Study from Nasarawa and Ondo States, Nigeria. Int. J. Health Plan. Manag. 2017, 32, 217–233. [Google Scholar]
- Khim, K. Are Health Workers Motivated by Income? Job Motivation of Cambodian Primary Health Workers Implementing Performance-Based Financing. Glob. Health Action 2016, 9, 31068. [Google Scholar]
- Gąsiorowski, J.; Rudowicz, E.; Safranow, K. Motivation towards medical career choice and future career plans of Polish medical students. Adv. Health Sci. Educ. Theory Pract. 2015, 20, 709–725. [Google Scholar]
- Ojakaa, D.; Olango, S.; Jarvis, J. Factors Affecting Motivation and Retention of Primary Health Care Workers in Three Disparate Regions in Kenya. Hum. Resour. Health 2014, 12, 33. [Google Scholar]
- Ghimire, J.; Gupta, R.P.; Kumal, A.B.; Mahato, R.K.; Bhandari, R.M.; Thapa, N. Factors associated with the motivation and de-motivation of health workforce in Nepal. J. Nepal Health Res. Counc. 2013, 11, 112–118. [Google Scholar]
- Peters, D.H.; Chakraborty, S.; Mahapatra, P.; Steinhardt, L. Job Satisfaction and Motivation of Health Workers in Public and Private Sectors: Cross-Sectional Analysis from Two Indian States. Hum. Resour. Health 2010, 8, 27. [Google Scholar]
- Bansal, R.N.; Malhotra, M. A Case Study of Motivational Levels among Personnel Working in a Government Teaching Hospital of Punjab. Biomed. Pharmacol. J. 2016, 9, 585–591. [Google Scholar]
- Mir, A.M.; Shaikh, M.S.; Rashida, G.; Mankani, N. To Serve or to Leave: A Question Faced by Public Sector Healthcare Providers in Pakistan. Health Res. Policy Syst. 2015, 13, S58. [Google Scholar]
- Humphrey, C.; Russell, J. Motivation and Values of Hospital Consultants in South-East England Who Work in the National Health Service and Do Private Practice. Soc. Sci. Med. 2004, 59, 1241–1250. [Google Scholar]
- Chang, C.T.; Hassali, M.A.; Hss, A.S.; Lee, J.C.Y.; Chan, H.K. Perceived motivators, training supports and challenges to career advancement among pharmacists in the Malaysian public healthcare system. Int. J. Pharm. Pract. 2019, 27, 555–564. [Google Scholar]
- Alhassan, R.K.A.; Nketiah-Amponsah, E.; Spieker, N.; Arhinful, D.K.; de Rinke Wit, T.F. Assessing the Impact of Community Engagement Interventions on Health Worker Motivation and Experiences with Clients in Primary Health Facilities in Ghana: A Randomized Cluster Trial. PLoS ONE 2016, 11, e0158541. [Google Scholar]
- Bonenberger, M.; Aikins, M.; Akweongo, P.; Wyss, K. The Effects of Health Worker Motivation and Job Satisfaction on Turnover Intention in Ghana: A Cross-Sectional Study. Hum. Resour. Health 2014, 12, 43. [Google Scholar]
- Purohit, B.; Bandyopadhyay, T. Beyond Job Security and Money: Driving Factors of Motivation for Government Doctors in India. Hum. Resour. Health 2014, 12, 12. [Google Scholar]
- Chew, B.; Ramli, A.; Omar, M.; Ismail, I. A preliminary study of job satisfaction and motivation among the Malaysian primary healthcare professionals. Malays. Fam. Physician 2013, 8, 15–25. [Google Scholar]
- Ashmore, J. “Going Private”: A Qualitative Comparison of Medical Specialists Job Satisfaction in the Public and Private Sectors of South Africa. Hum. Resour. Health 2013, 11, 6. [Google Scholar]
- Waitzkin, H.; Yager, J.; Santos, R. Advancing the Business Creed? The Framing of Decisions about Public Sector Managed Care. Sociol. Health Illn. 2012, 34, 31–48. [Google Scholar]
- Frehywot, S.; Mullan, F.; Payne, P.W.; Ross, H. Compulsory service programmes for recruiting health workers in remote and rural areas: Do they work? Bull. World Health Organ. 2010, 88, 364–370. [Google Scholar]
- Rahman, S.M.; Ali, N.A.; Jennings, L.; Seraji, M.H.R.; Mannan, I.; Shah, R.; Al-Ahmud, A.B.; Bari, S.; Hossain, D.; Das, M.K.; et al. Factors affecting recruitment and retention of community health workers in a newborn care intervention in Bangladesh. Hum. Resour. Health 2010, 8, 10–12. [Google Scholar]
- Armstrong, M. Human Resource Management Practice, 12th ed.; KoganPage: London, UK, 2012. [Google Scholar]
- Androniceanu, A.; Sabie, O.M.; Pegulescu, A. An integrated approach of the human resources motivation and the quality of health services. Theor. Empir. Res. Urban Manag. 2020, 15, 42–53. [Google Scholar]
- Prust, M.L.; Kamanga, A.; Ngosa, L.; McKay, C.; Muzongwe, C.M.; Mukubani, M.T.; Chihinga, R.; Misapa, R.; van den Broek, J.W.; Wilmink, N. Assessment of Interventions to Attract and Retain Health Workers in Rural Zambia: A Discrete Choice Experiment. Hum. Resour. Health 2019, 17, 26. [Google Scholar]
- Sato, M.; Maufi, D.; Mwingira, U.J.; Leshabari, M.T.; Ohnishi, M.; Honda, S. Measuring Three Aspects of Motivation among Health Workers at Primary Level Health Facilities in Rural Tanzania. PLoS ONE 2017, 12, e0184599. [Google Scholar]
- Korlén, S.; Essén, A.; Lindgren, P.; Amer-Wahlin, I.; von Thiele Schwarz, U. Managerial Strategies to Make Incentives Meaningful and Motivating. J. Health Organ. Manag. 2017, 31, 126–141. [Google Scholar]
- Mazahir, S.; Khalid, S. Work Environment and Situational Motivation of Doctors in Public Sector Hospitals. Ann. King Edw. Med. Univ. 2017, 23, 1509. [Google Scholar]
- Mbindyo, P.; Gilson, L.; Blaauw, D.; English, M. Contextual Influences on Health Worker Motivation in District Hospitals in Kenya. Implement. Sci. 2009, 4, 43. [Google Scholar]
- Dambisya, Y.M.; Modipa, I.S.; Legodi, M.G. Factors Influencing the Distribution of Pharmacy Graduates of the University of the North, South Africa. East Afr. Med. J. 2007, 84, 481–488. [Google Scholar]
- Jaeger, F.N.; Bechir, M.; Harouna, M.; Moto, D.D.; Utzinger, J. Challenges and opportunities for healthcare workers in a rural district of Chad. BMC Health Serv. Res. 2018, 18, 7. [Google Scholar]
- Topp, S.M.; Chipukuma, J.M.; Hanefeld, J. Understanding the dynamic interactions driving Zambian health centre performance: A case-based health systems analysis. Health Policy Plan. 2015, 30, 485–499. [Google Scholar]
- Russo, G.; Rego, I.; Perelman, J.; Barros, P.P. A Tale of Loss of Privilege, Resilience and Change: The Impact of the Economic Crisis on Physicians and Medical Services in Portugal. Health Policy 2016, 120, 1079–1086. [Google Scholar]
- Ferrinho, P.; Van Lerberghe, W.; Julien, M.R.; Fresta, E.; Gomes, A.; Dias, F.; Gonçalves, A.; Bäckström, B. How and why public sector doctors engage in private practice in Portuguese-speaking African countries. Health Policy Plan. 1998, 13, 332–338. [Google Scholar]
- Bratton, J.; Sawchuk, P.; Forshaw, C.; Callinan, M.; Corbet, M. Work and Organizational Behaviour, 2nd ed.; Palgrave Macmillan: Basingstoke, UK, 2010. [Google Scholar]
- Cantarelli, P.; Belle, N.; Longo, F. Exploring the Motivational Bases of Public Mission-Driven Professions Using a Sequential-Explanatory Design. Public Manag. Rev. 2020, 22, 1535–1559. [Google Scholar]
- Belrhiti, Z.; van Damme, W.; Belalia, A.; Marchal, B. The Effect of Leadership on Public Service Motivation: A Multiple Embedded Case Study in Morocco. BMJ Open 2020, 10, e033010. [Google Scholar]
- Aninanya, G.A.; Howard, N.; Williams, J.E.; Apam, B.; Prytherch, H.; Loukanova, S.; Kamara, E.K.; Otupiri, E. Can Performance-Based Incentives Improve Motivation of Nurses and Midwives in Primary Facilities in Northern Ghana? A Quasi-Experimental Study. Glob. Health Action 2016, 9, 32404. [Google Scholar]
- Kitsios, F.; Kamariotou, M. Job satisfaction behind motivation: An empirical study in public health workers. Heliyon 2021, 7, e06857. [Google Scholar]
- Franco, L.M.; Bennett, S.; Kanfer, R. Health sector reform and public sector health worker motivation: A conceptual framework. Soc. Sci. Med. 2002, 54, 1255–1266. [Google Scholar]
- Ralston, D.A.; Egri, C.P.; Stewart, S.; Terpstra, R.H.; Yu, K. Doing business in 21st century with the new generation of Chinese manager: A study of generational shifts in work values in China. J. Int. Bus. Stud. 1999, 30, 415–428. [Google Scholar]
- Jing, L.; Ma, Z.; Ma, Z.; Chen, B.; Cheng, S. Nurse Practitioners’ Work Values and Their Conflict Management Approaches in a Stressful Workplace: A Taiwan Study. Sustainability 2020, 12, 1040. [Google Scholar]
- Shibata, S.; Thepthien, B.T.; Sermsri, S. Intention toward Working in the Private Sector among Fourth-Year Nursing Students in Thailand. J. Health Res. 2015, 29, 23–29. [Google Scholar]
- Halepota, J.A.; Shah, N. An Empirical Investigation of Organisational Antecedents on Employee Job Satisfaction in a Developing Country. Transform. Gov. People Process Policy 2011, 5, 280–294. [Google Scholar]
- Smith, L. An Evaluation of Programmes for Staff Motivation in NHS and Hotel Ancillary Staff. Facilities 1999, 17, 264–271. [Google Scholar]
- Bimpong, K.A.A.; Khan, A.; Slight, R.; Tolley, C.L.; Slight, S.P. Relationship between labour force satisfaction, wages and retention within the UK National Health Service: A systematic review of the literature. BMJ Open 2020, 10, e034919. [Google Scholar]
- McCarthy, D.; Wei, P.; Homberg, F.; Tabvuma, V. Public service motivation in the Chinese public and private sectors. Evid. -Based HRM 2021, 9, 1–17. [Google Scholar]
- Jiang, H.; Jia, H.; Zhang, J.; Li, Y.; Song, F.; Yu, X. Nurses’ Occupational Stress and Presenteeism: The Mediating Role of Public Service Motivation and the Moderating Role of Health. Int. J. Environ. Res. Public Health 2021, 18, 3523. [Google Scholar]
- Stefurak, T.; Morgan, R.; Johnson, R.B. The Relationship of Public Service Motivation to Job Satisfaction and Job Performance of Emergency Medical Services Professionals. Public Pers. Manag. 2020, 49, 590–616. [Google Scholar]
- Ebenso, B.; Mbachu, C.; Etiaba, E.; Huss, R.; Manzano, A.; Onwujekwe, O.; Uzochukwu, B.; Ezumah, N.; Ensor, T.; Hicks, J.P.; et al. Which Mechanisms Explain Motivation the of Primary Health Workers? Insights from the Realist Evaluation of a Maternal and Child Health Programme in Nigeria. BMJ Glob. Health 2020, 5, e002408. [Google Scholar]
- Jensen, U.T.; Kjeldsen, A.M.; Vestergaard, C.F. How is public service motivation affected by regulatory policy changes? Int. Public Manag. J. 2020, 23, 465–495. [Google Scholar]
- Abdelmotaleb, M. The Moderating and Mediating Role of Public Service Motivation between Organization’s Social Responsibility and Employee Engagement: Evidence from Egyptian Public Hospitals. Int. Rev. Public Adm. 2020, 25, 207–223. [Google Scholar]
- Van Loon, N.M.; Baekgaard, M.; Moynihan, D.P. Stability Not Change: Improving Frontline Employee Motivation through Organizational Reform Is Harder than It Looks. Public Adm. 2020, 98, 591–608. [Google Scholar]
- Deng, J.; Li, Y.; Sun, Y.; Lei, R.; Yang, T. Public Service Motivation as a Mediator of the Relationship between Job Stress and Presenteeism: A Cross-Sectional Study from Chinese Public Hospitals. BMC Health Serv. Res. 2019, 19, 625. [Google Scholar]
- Deng, J.; Guo, Y.; Ma, T.; Yang, T.; Tian, X. How Job Stress Influences Job Performance among Chinese Healthcare Workers: A Cross-Sectional Study. Environ. Health Prev. Med. 2019, 24, 2. [Google Scholar]
- Adams, A.M.; Ahmed, R.; Shuvo, T.A.; Yusuf, S.S.; Akhter, S.; Anwar, I. Exploratory Qualitative Study to Understand the Underlying Motivations and Strategies of the Private For-Profit Healthcare Sector in Urban Bangladesh. BMJ Open 2019, 9, e026586. [Google Scholar]
- Borghi, J.; Lohmann, J.; Dale, E.; Meheus, F.; Goudge, J.; Oboirien, K.; Kuwawenaruwa, A. How to Do (or Not to Do)—Measuring Health Worker Motivation in Surveys in Low- and Middle-Income Countries. Health Policy Plan. 2018, 33, 192–203. [Google Scholar]
- Zweigenthal, V.E.M.; Pick, W.M.; London, L. Motivations of South African Physicians Specialising in Public Health. Glob. Health Action 2018, 11, 1475039. [Google Scholar]
- Aguilera Dreyse, B.; López Gaete, G. ¿Tiene El Médico El Deber Moral de Trabajar En El Sector Público de Salud? Consideraciones Éticas Sobre Las Obligaciones Sociales Del Médico. Medwave 2017, 17, 7105. [Google Scholar]
- Abera, G.G.; Alemayehu, Y.K.; Henry, J. Public-on-Private Dual Practice among Physicians in Public Hospitals of Tigray National Regional State, North Ethiopia: Perspectives of Physicians, Patients and Managers. BMC Health Serv. Res. 2017, 17, 713. [Google Scholar]
- Masood, M.; Afsar, B. Transformational Leadership and Innovative Work Behavior among Nursing Staff. Nurs. Inq. 2017, 24, e12188. [Google Scholar]
- Levitats, Z.; Vigoda-Gadot, E. Yours Emotionally: How Emotional Intelligence Infuses Public Service Motivation and Affects the Job Outcomes of Public Personnel. Public Adm. 2017, 95, 759–775. [Google Scholar]
- Millar, R.; Chen, Y.; Wang, M.; Fang, L.; Liu, J.; Xuan, Z.; Li, G. It’s All about the Money? A Qualitative Study of Healthcare Worker Motivation in Urban China. Int. J. Equity Health 2017, 16, 120. [Google Scholar]
- Seth, K. Heterogeneity in the Background and Earnings of Nurses in India: Evidence from a Cross-Sectional Study in Gujarat. Health Policy Plan. 2017, 32, 1285–1293. [Google Scholar]
- Hou, X.; Witter, S.; Zaman, R.U.; Engelhardt, K.; Hafidz, F.; Julia, F.; Lemiere, C.; Sullivan, E.B.; Saldanha, E.; Palu, T.; et al. What Do Health Workers in Timor-Leste Want, Know and Do Findings from a National Health Labour Market Survey. Hum. Resour. Health 2016, 14, 69. [Google Scholar]
- Bhatnagar, A.; George, A.S. Motivating Health Workers up to a Limit: Partial Effects of Performance-Based Financing on Working Environments in Nigeria. Health Policy Plan. 2016, 31, 868–877. [Google Scholar]
- Shah, S.M.; Zaidi, S.; Ahmed, J.; Ur Rehman, S. Motivation and Retention of Physicians in Primary Healthcare Facilities: A Qualitative Study from Abbottabad, Pakistan. Int. J. Health Policy Manag. 2016, 5, 467–475. [Google Scholar]
- Namakula, J.; Witter, S.; Ssengooba, F. Health Worker Experiences of and Movement between Public and Private Not-for-Profit Sectors-Findings from Post-Conflict Northern Uganda. Hum. Resour. Health 2016, 14, 18. [Google Scholar]
- Van Loon, N.M. Is Public Service Motivation Related to Overall and Dimensional Work-Unit Performance as Indicated by Supervisors? Int. Public Manag. J. 2016, 19, 78–110. [Google Scholar]
- Kadam, S.; Nallala, S.; Zodpey, S.; Pati, S.; Hussain, M.A.; Chauhan, A.S.; Das, S.; Martineau, T. A Study of Organizational versus Individual Needs Related to Recruitment, Deployment and Promotion of Doctors Working in the Government Health System in Odisha State, India. Hum. Resour. Health 2016, 14, 7. [Google Scholar]
- Ashmore, J.; Gilson, L. Conceptualizing the Impacts of Dual Practice on the Retention of Public Sector Specialists—Evidence from South Africa. Hum. Resour. Health 2015, 13, 3. [Google Scholar]
- Bellé, N. Performance-Related Pay and the Crowding out of Motivation in the Public Sector: A Randomized Field Experiment. Public Adm. Rev. 2015, 75, 230–241. [Google Scholar]
- Schmiedeknecht, K.; Perera, M.; Schell, E.; Jere, J.; Geoffroy, E.; Rankin, S. Predictors of Workforce Retention Among Malawian Nurse Graduates of a Scholarship Program: A Mixed-Methods Study. Glob. Health Sci. Pract. 2015, 3, 85–96. [Google Scholar]
- Russo, G.; de Sousa, B.; Sidat, M.; Ferrinho, P.; Dussault, G. Why Do Some Physicians in Portuguese-Speaking African Countries Work Exclusively for the Private Sector? Findings from a Mixed-Methods Study. Hum. Resour. Health 2014, 12, 51. [Google Scholar]
- Hennig-Schmidt, H.; Wiesen, D. Other-Regarding Behavior and Motivation in Health Care Provision: An Experiment with Medical and Non-Medical Students. Soc. Sci. Med. 2014, 108, 156–165. [Google Scholar]
- Lagarde, M.; Blaauw, D. Pro-Social Preferences and Self-Selection into Jobs: Evidence from South African Nurses. J. Econ. Behav. Organ. 2014, 107, 136–152. [Google Scholar]
- Krogsgaard, J.A.; Thomsen, P.; Andersen, L.B. Only If We Agree? How Value Conflicts Moderate the Relationship Between Transformational Leadership and Public Service Motivation. Int. J. Public Adm. 2014, 37, 895–907. [Google Scholar]
- Schott, C.; Pronk, J.L.J. Investigating and Explaining Organizational Antecedents of PSM. Evid. Based HRM 2014, 2, 28–56. [Google Scholar]
- Diwan, V.; Minj, C.; Chhari, N.; de Costa, A. Indian Medical Students in Public and Private Sector Medical Schools: Are Motivations and Career Aspirations Different?—Studies from Madhya Pradesh, India. BMC Med. Educ. 2013, 13, 127. [Google Scholar]
- Alhassan, R.K.; Spieker, N.; van Ostenberg, P.; Ognik, A.; Nketiah-Amponsah, E.; De Wit, T.F.R. Association between health worker motivation and healthcare quality efforts in Ghana. Hum. Resour. Health 2013, 11, 37. [Google Scholar]
- Kolstad, J.R.; Lindkvist, I. Pro-Social Preferences and Self-Selection into the Public Health Sector: Evidence from an Economic Experiment. Health Policy Plan. 2013, 28, 320–327. [Google Scholar]
- George, G.; Gow, J.; Bachoo, S. Understanding the Factors Influencing Health-Worker Employment Decisions in South Africa. Hum. Resour. Health 2013, 11, 15. [Google Scholar]
- Dos Santos, B.F.; Nicolau, B.; Muller, K.; Bedos, C.; Zuanon, A.C. Brazilian dental students’ intentions and motivations towards their professional career. J. Dent. Educ. 2013, 77, 337–344. [Google Scholar]
- Bellé, N. Experimental Evidence on the Relationship between Public Service Motivation and Job Performance. Public Adm. Rev. 2012, 73, 143–153. [Google Scholar]
- Van Loon, N.M.; Leisink, P.; Vandenabeele, W. Talking the Talk of Public Service Motivation: How Public Organization Logics Matter for Employees’ Expressions of PSM. Int. J. Public Adm. 2013, 36, 1007–1019. [Google Scholar]
- Mariappan, M. Analysis of Nursing Job Characteristics in Public Sector Hospitals. J. Health Manag. 2013, 15, 253–262. [Google Scholar]
- Andersen, L.B.; Kristensen, N.; Pedersen, L.H. Models of Public Service Provision-When Will Knights and Knaves Be Responsive to Pawns and Queens? Int. J. Public Adm. 2013, 36, 126–136. [Google Scholar]
- Songstad, N.G.; Moland, K.M.; Massay, D.A.; Blystad, A. Why Do Health Workers in Rural Tanzania Prefer Public Sector Employment? BMC Health Serv. Res. 2012, 12, 92. [Google Scholar]
- Kjeldsen, A.M. Sector and Occupational Differences in Public Service Motivation: A Qualitative Study. Int. J. Public Adm. 2012, 35, 58–69. [Google Scholar]
- Georgellis, Y.; Iossa, E.; Tabvuma, V.; Smith, S.; Estache, A.; Pommet, S.; Hunter, J.; Roy, J.; Pouliakas, K.; Clark, A. Crowding Out Intrinsic Motivation in the Public Sector. J. Public Adm. Res. Theory 2011, 21, 473–493. [Google Scholar]
- Aysen, G.; Parumasur, S.B. Managerial role in enhancing employee motivation in public health care. Corp. Ownersh. Control. 2011, 8, 401–410. [Google Scholar]
- Leonard, K.L.; Masatu, M.C. Professionalism and the Know-Do Gap: Exploring Intrinsic Motivation among Health Workers in Tanzania. Health Econ. 2010, 19, 1461–1477. [Google Scholar]
- Malik, A.A.; Yamamoto, S.S.; Souares, A.; Malik, Z.; Sauerborn, R. Motivational Determinants among Physicians in Lahore, Pakistan. BMC Health Serv. Res. 2010, 10, 201. [Google Scholar]
- Serneels, P.; Montalvo, J.G.; Pettersson, G.; Lievens, T.; Buterae, J.D.; Kidanu, A. Qui Est Disposé à Travailler Dans Un Poste de Santé En Milieu Rural? Le Rôle de La Motivation Propre, Des Origines Rurales et Des Institutions Confessionnelles En Éthiopie et Au Rwanda. Bull. World Health Organ. 2010, 88, 342–349. [Google Scholar]
- Le Julian, G. Knights and Knaves Return: Public Service Motivation and the Delivery of Public Services. Int. Public Manag. J. 2010, 13, 56–71. [Google Scholar]
- Andersen, B.L. What Determines the Behaviour and Performance of Health Professionals? Public Service Motivation, Professional Norms and/or Economic Incentives. Int. Rev. Adm. Sci. 2009, 75, 79–97. [Google Scholar]
- Mangham, L.J.; Hanson, K. Employment Preferences of Public Sector Nurses in Malawi: Results from a Discrete Choice Experiment. Trop. Med. Int. Health 2008, 13, 1433–1441. [Google Scholar]
- Modipa, S.I.; Dambisya, Y.M. Profile and career preferences of pharmacy students at the University of Limpopo, Turfloop Campus, South Africa. Educ. Health 2008, 21, 164. [Google Scholar]
- Agyepong, I.A.; Anafi, P.; Asiamah, E.; Ansah, E.K.; Ashon, D.A.; Narh-Dometey, C. Health Worker (Internal Customer) Satisfaction and Motivation in the Public Sector in Ghana. Int. J. Health Plan. Manag. 2004, 19, 319–336. [Google Scholar]
- Lee-Ross, D. An Exploratory Study of Work Motivation among Private and Public Sector Hospital Chefs in Australia. J. Manag. Dev. 2002, 21, 576–588. [Google Scholar]
- Pipan, T. Metaphors and Organizational Identity in the Italian Public Services. Scand. J. Manag. 2000, 16, 391–409. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).