Predicting Hypnotic Use among Insomnia Patients with the Theory of Planned Behavior and Craving
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Measurements
2.2.1. Theory of Planned Behavior Questionnaire
2.2.2. Hypnotic-Use Urge Scale (HUS)
2.3. Procedure
2.4. Statistical Analysis
3. Results
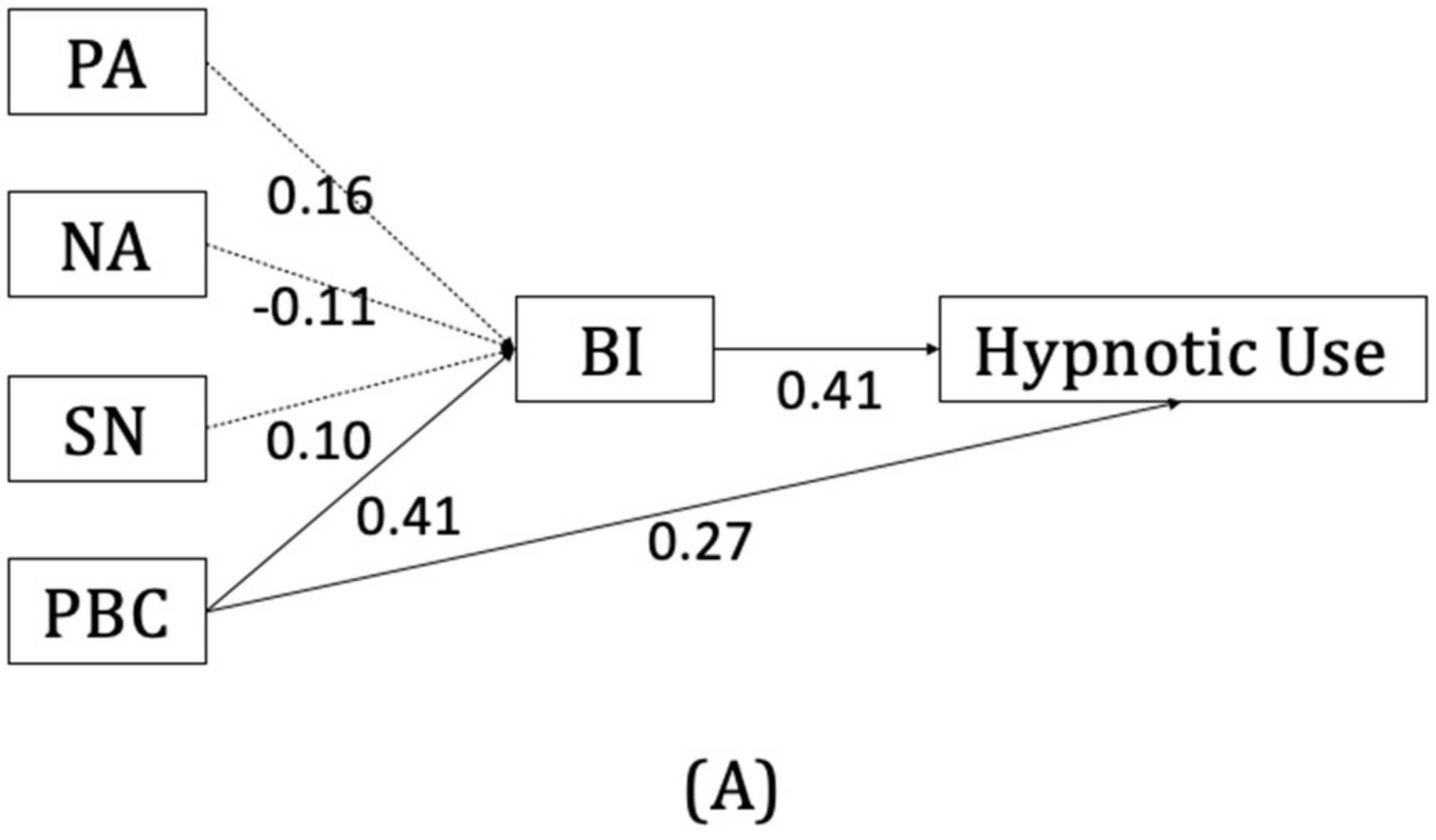
3.1. The TPB Model
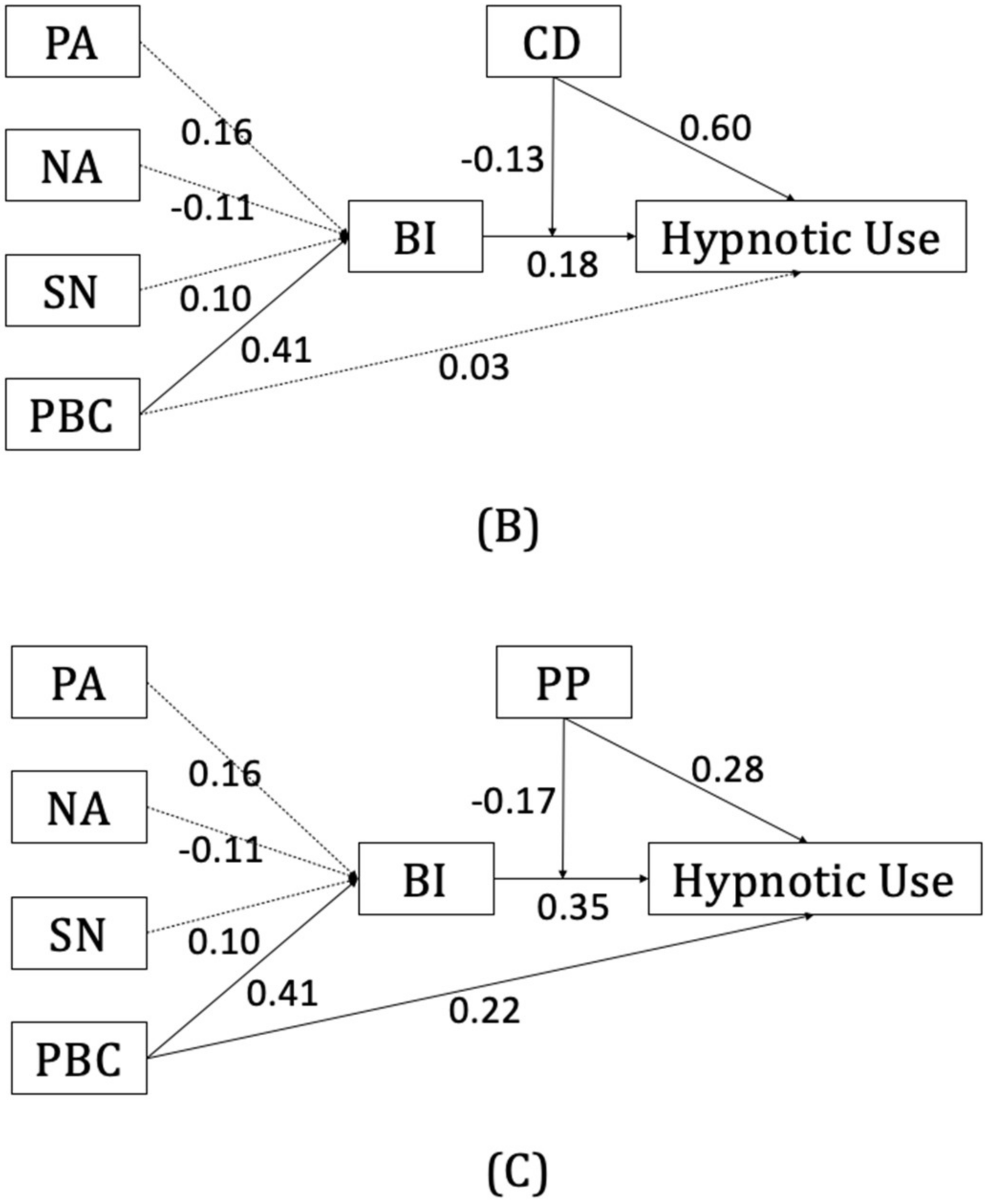
3.2. Moderation Effect of Craving
4. Discussion and Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ohayon, M. Epidemiological study on insomnia in the general population. Sleep 1996, 19, S7–S15. [Google Scholar] [CrossRef] [Green Version]
- Morin, C.M.; Jarrin, D.C.; Ivers, H.; Mérette, C.; LeBlanc, M.; Savard, J. Incidence, Persistence, and Remission Rates of Insomnia Over 5 Years. JAMA Netw. Open 2020, 3, e20180782. [Google Scholar] [CrossRef]
- Crowe, S.F.; Stranks, E.K. The residual medium and long-term cognitive effects of benzodiazepine use: An updated meta-analysis. Arch. Clin. Neuropsychol. 2018, 33, 901–911. [Google Scholar] [CrossRef]
- Holbrook, A.M.; Crowther, R.; Lotter, A.; Cheng, C.; King, D. Meta-analysis of benzodiazepine use in the treatment of insomnia. CMAJ 2000, 162, 225–233. [Google Scholar] [PubMed]
- Kripke, D.F. Chronic hypnotic use: Deadly risks, doubtful benefit: Review article. Sleep Med. Rev. 2000, 4, 5–20. [Google Scholar] [CrossRef]
- Krystal, A.D.; Durrence, H.H.; Scharf, M.; Jochelson, P.; Rogowski, R.; Ludington, E.; Roth, T. Efficacy and Safety of Doxepin 1 mg and 3 mg in a 12-week Sleep Laboratory and Outpatient Trial of Elderly Subjects with Chronic Primary Insomnia. Sleep 2010, 33, 1553–1561. [Google Scholar] [CrossRef] [Green Version]
- Nafti, M.; Sirois, C.; Kröger, E.; Carmichael, P.H.; Laurin, D. Is benzodiazepine use associated with the risk of dementia and cognitive impairment–not dementia in older persons? The Canadian study of health and aging. Ann. Pharmacother. 2020, 54, 219–225. [Google Scholar] [CrossRef]
- Picton, J.D.; Marino, A.B.; Nealy, K.L. Benzodiazepine use and cognitive decline in the elderly. Am. J. Health-Syst. Pharm. 2018, 75, e6–e12. [Google Scholar] [CrossRef]
- Roehrs, T.; Roth, T. Drug-related Sleep Stage Changes: Functional Significance and Clinical Relevance. Sleep Med. Clin. 2010, 5, 559–570. [Google Scholar] [CrossRef] [Green Version]
- Sato, Y.; Yoshihisa, A.; Hotsuki, Y.; Watanabe, K.; Kimishima, Y.; Kiko, T.; Kanno, Y.; Yokokawa, T.; Abe, S.; Misaka, T.; et al. Associations of Benzodiazepine with Adverse Prognosis in Heart Failure Patients with Insomnia. J. Am. Heart Assoc. 2020, 9, e013982. [Google Scholar] [CrossRef]
- Uzun, S.; Kozumplik, O.; Jakovljević, M.; Sedić, B. Side effects of treatment with benzodiazepines. Psychiatr. Danub. 2010, 22, 90–93. [Google Scholar] [PubMed]
- Kales, A.; Scharf, M.B.; Kales, J.D. Rebound insomnia: A new clinical syndrome. Science 1978, 201, 1039–1041. [Google Scholar] [CrossRef] [PubMed]
- Kales, A.; Scharf, M.B.; Soldatos, C.R.; Bixler, E.O. Clinical evaluation of hypnotic drugs: Contributions from sleep laboratory studies. J. Clin. Pharmacol. 1979, 19, 329–336. [Google Scholar] [CrossRef]
- Lader, M. Benzodiazepine harm: How can it be reduced? Br. J. Clin. Pharmacol. 2014, 77, 295–301. [Google Scholar] [CrossRef] [Green Version]
- Soldatos, C.R.; Dikeos, D.G.; Whitehead, A. Tolerance and rebound insomnia with rapidly eliminated hypnotics: A meta-analysis of sleep laboratory studies. Int. Clin. Psychopharmacol. 1999, 14, 287–303. [Google Scholar] [CrossRef] [PubMed]
- Schifano, F.; Chiappini, S.; Corkery, J.M.; Guirguis, A. An Insight into Z-Drug Abuse and Dependence: An Examination of Reports to the European Medicines Agency Database of Suspected Adverse Drug Reactions. Int. J. Neuropsychopharmacol. 2019, 22, 270–277. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Harbourt, K.; Nevo, O.N.; Zhang, R.; Chan, V.; Croteau, D. Association of eszopiclone, zaleplon, or zolpidem with complex sleep behaviors resulting in serious injuries, including death. Pharmacoepidemiol. Drug Saf. 2020, 29, 684–691. [Google Scholar] [CrossRef]
- Poceta, J.S. Zolpidem ingestion, automatisms, and sleep driving: A clinical and legal case series. J. Clin. Sleep Med. 2011, 7, 632–638. [Google Scholar] [CrossRef] [Green Version]
- Victorri-Vigneau, C.; Dailly, E.; Veyrac, G.; Jolliet, P. Evidence of zolpidem abuse and dependence: Results of the French Centre for Evaluation and Information on Pharmacodependence (CEIP) network survey. Br. J. Clin. Pharmacol. 2007, 64, 198–209. [Google Scholar] [CrossRef]
- Hajak, G.; Müller, W.E.; Wittchen, H.U.; Pittrow, D.; Kirch, W. Abuse and dependence potential for the non-benzodiazepine hypnotics zolpidem and zopiclone: A review of case reports and epidemiological data. Addiction 2003, 98, 1371–1378. [Google Scholar] [CrossRef]
- Ohayon, M.M.; Caulet, M.; Arbus, L.; Billard, M.; Coquerel, A.; Guieu, J.D.; Kullmann, B.; Loffont, F.; Lemoine, P.; Paty, J.; et al. Are prescribed medications effective in the treatment of insomnia complaints? J. Psychosom. Res. 1999, 47, 359–368. [Google Scholar] [CrossRef]
- Morin, C.M.; Bastien, C.; Guay, B.; Radouco-Thomas, M.; Leblanc, J.; Vallieres, A. Randomized clinical trial of supervised tapering and cognitive behavior therapy to facilitate benzodiazepine discontinuation in older adults with chronic insomnia. Am. J. Psychiatry 2004, 161, 332–342. [Google Scholar] [CrossRef] [PubMed]
- Kaufmann, C.N.; Spira, A.P.; Depp, C.A.; Mojtabai, R. Long-Term Use of Benzodiazepines and Nonbenzodiazepine Hypnotics, 1999–2014. Psychiatr. Serv. 2018, 69, 235–238. [Google Scholar] [CrossRef] [PubMed]
- Clift, A.D. Factors leading to dependence on hypnotic drugs. Br. Med. J. 1972, 3, 614–617. [Google Scholar] [CrossRef] [Green Version]
- Enomoto, M.; Kitamura, S.; Tachimori, H.; Takeshima, M.; Mishima, K. Long-term use of hypnotics: Analysis of trends and risk factors. Gen. Hosp. Psychiatry 2020, 62, 49–55. [Google Scholar] [CrossRef]
- Morin, C.M.; Belanger, L.; Bastien, C.; Vallieres, A. Long-term outcome after discontinuation of benzodiazepines for insomnia: A survival analysis of relapse. Behav. Res. Ther. 2005, 43, 1–14. [Google Scholar] [CrossRef]
- Cheung, J.M.Y.; Bartlett, D.J.; Armour, C.L.; Laba, T.-L.; Saini, B. To Drug or Not to Drug: A Qualitative Study of Patients’ Decision-Making Processes for Managing Insomnia. Behav. Sleep Med. 2016, 16, 1–26. [Google Scholar] [CrossRef]
- Armitage, C.J.; Conner, M. Efficacy of the theory of planned behaviour: A meta-analytic review. Br. J. Soc. Psychol. 2001, 40, 471–499. [Google Scholar] [CrossRef] [Green Version]
- Conner, M.; McMillan, B. Interaction effects in the theory of planned behaviour: Studying cannabis use. Br. J. Soc. Psychol. 1999, 38, 195–222. [Google Scholar] [CrossRef]
- Jalilian, F.; Mirzaei-Alavijeh, M.; Ahmadpanah, M.; Mostafaei, S.; Kargar, M.; Pirouzeh, R.; Bahmani, D.S.; Brand, S. Extension of the Theory of Planned Behavior (TPB) to Predict Patterns of Marijuana Use among Young Iranian Adults. Int. J. Environ. Res. Public Health 2020, 17, 1981. [Google Scholar] [CrossRef] [Green Version]
- Tapera, R.; Mbongwe, B.; Mhaka-Mutepfa, M.; Lord, A.; Phaladze, N.A.; Zetola, N.M. The theory of planned behavior as a behavior change model for tobacco control strategies among adolescents in Botswana. PLoS ONE 2020, 15, e0233462. [Google Scholar] [CrossRef] [PubMed]
- Ajzen, I. The theory of planned behavior. Organ. Behav. Hum. Decis. Process 1991, 50, 179–211. [Google Scholar] [CrossRef]
- Ajzen, I. Constructing a Theory of Planned Behavior Questionnaire: Conceptual and Methodological Considerations. 2006. Available online: http://www.people.umass.edu/aizen/pdf/tpb.measurement.pdf (accessed on 18 June 2022).
- McMillan, B.; Conner, M. Using the theory of planned behaviour to understand alcohol and tobacco use in students. Psychol. Health Med. 2003, 8, 317–328. [Google Scholar] [CrossRef]
- De Wilde, K.; Maes, L.; Boudrez, H.; Tency, I.; Temmerman, M.; Clays, E. Analysis of smoking cessation beliefs in pregnant smokers and ex-smokers using the theory of planned behavior. J. Public Health 2017, 25, 267–274. [Google Scholar] [CrossRef]
- Record, R.A.; Harrington, N.G.; Helme, D.W.; Savage, M.W. Using the theory of planned behavior to guide focus group development of messages aimed at increasing compliance with a tobacco-free policy. Am. J. Health Promot. 2018, 32, 143–152. [Google Scholar] [CrossRef]
- Van Hulten, R.; Lodder, A.C.; Teeuw, K.B.; Bakker, A.; Leufkens, H.G.; Bakker, A.B. Determinants of change in the intention to use benzodiazepines. Pharm. World Sci. 2001, 23, 70–75. [Google Scholar] [CrossRef]
- Van Hulten, R.; Bakker, A.B.; Lodder, A.C.; Teeuw, K.B.; Bakker, A.; Leufkens, H.G. The impact of attitudes and beliefs on length of benzodiazepine use: A study among inexperienced and experienced benzodiazepine users. Soc. Sci. Med. 2003, 56, 1345–1354. [Google Scholar] [CrossRef]
- Rosenberg, H. Clinical and laboratory assessment of the subjective experience of drug craving. Clin. Psychol. Rev. 2009, 29, 519–534. [Google Scholar] [CrossRef]
- Bottlender, M.; Soyka, M. Impact of craving on alcohol relapse during, and 12 months following, outpatient treatment. Alcohol 2004, 39, 357–361. [Google Scholar] [CrossRef] [Green Version]
- Germovsek, E.; Hansson, A.; Karlsson, M.O.; Westin, Å.; Soons, P.A.; Vermeulen, A.; Kjellsson, M.C. A time-to-event model relating integrated craving to risk of smoking relapse across different nicotine replacement therapy formulations. Clin. Pharmacol. Ther. 2020, 109, 416–423. [Google Scholar] [CrossRef]
- Killen, J.D.; Fortmann, S.P. Craving is associated with smoking relapse: Findings from three prospective studies. Exp. Clin. Psychopharmacol. 1997, 5, 137–142. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.-M.; Lin, Y.-S.; Tu, A.Y.; Huang, Y.-C.; Sung, J.-Y. Attentional bias assessed with event related potentials in long-term hypnotic users. J. Clin. Psychopharmacol. 2020, 40, 391–395. [Google Scholar] [CrossRef]
- American Psychiatric Association [APA]. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Arlington, VA, USA, 2013; ISBN 978-0-89042-554-1. [Google Scholar]
- Ajzen, I. Perceived Behavioral Control, Self-Efficacy, Locus of Control, and the Theory of Planned Behavior. J. Appl. Soc. Psychol. 2006, 32, 665–683. [Google Scholar] [CrossRef]
- Francis, J.; Eccles, M.P.; Johnston, M.; Walker, A.E.; Grimshaw, J.M.; Foy, R.; Kaner, E.F.S.; Smith, L.; Bonetti, D. Constructing Questionnaires Based on the Theory of Planned Behaviour: A Manual for Health Services Researchers, 5th ed.; Centre for Health Services Research, University of Newcastle: Newcastle, UK, 2004; ISBN 0-9540161-5-7. [Google Scholar]
- Jen, C.-H.; Yang, C.-M.; Chen, C.-W.; Yu, H.-T.; Lai, Y.-S.; Lee, H.-C.; Sung, J.-Y. Development and psychometric evaluation of the Hypnotic-Use Urge Scale. Sleep Biol. Rhythms 2019, 17, 63–72. [Google Scholar] [CrossRef]
- Sheehan, D.V.; Lecrubier, Y.; Sheehan, K.H.; Amorim, P.; Janavs, J.; Weiller, E.; Hergueta, T.; Baker, R.; Dunbar, G.C. The Mini-International Neuropsychiatric Interview (MINI): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J. Clin. Psychiatry 1998, 59, 22–33. [Google Scholar] [PubMed]
- Spoormaker, V.I.; Verbeek, I.; van den Bout, J.; Klip, E.C. Initial validation of the SLEEP-50 questionnaire. Behav. Sleep Med. 2005, 3, 227–246. [Google Scholar] [CrossRef] [Green Version]
- Baron, R.M.; Kenny, D.A. The moderator-mediator variable distinction in social Psychological research: Conceptual, strategic, and statistical considerations. J. Pers. Soc. Psychol. 1986, 51, 1173–1182. [Google Scholar] [CrossRef]
- Sobel, M.E. Asymptotic confidence intervals for indirect effects in structural equations models. Sociol. Methodol. 1982, 13, 290–312. [Google Scholar] [CrossRef]
- Rich, A.; Brandes, K.; Mullan, B.; Hagger, M.S. Theory of planned behavior and adherence in chronic illness: A meta-analysis. J. Behav. Med. 2015, 38, 673–688. [Google Scholar] [CrossRef] [Green Version]
- Belleville, G.; Morin, C.M. Hypnotic discontinuation in chronic insomnia: Impact of psychological distress, readiness to change, and self-efficacy. Health Psychol. 2008, 27, 239–248. [Google Scholar] [CrossRef]
- Yang, C.-M.; Tseng, C.-H.; Lai, Y.-S.; Hsu, S.-C. Self-efficacy enhancement can facilitate hypnotic tapering in patients with primary insomnia. Sleep Bio. Rhythms. 2015, 13, 242–251. [Google Scholar] [CrossRef]
- Chen, C.-W.; Yang, C.-M.; Lin, Y.-S.; Tsai, Y.-L. Qualitative Study of Long-Term Sedative-Hypnotic Use Patterns. J. Sleep Disord. Treat. Care 2016, 5, 4. [Google Scholar] [CrossRef]
- Gass, J.C.; Motschman, C.A.; Tiffany, S.T. The relationship between craving and tobacco use behavior in laboratory studies: A meta-analysis. Psychol. Addict. Behav. 2014, 28, 1162–1176. [Google Scholar] [CrossRef]
- Green, R.; Grodin, E.; Lim, A.C.; Venegas, A.; Bujarski, S.; Krull, J.; Ray, L.A. The interplay between subjective response to alcohol, craving, and alcohol self-administration in the human laboratory. Alcohol. Clin. Exp. Res. 2019, 43, 907–915. [Google Scholar] [CrossRef]
- Law, B.; Gullo, M.J.; Daglish, M.; Kavanagh, D.J.; Feeney, G.F.X.; Young, R.M.; Connor, J.P. Craving mediates stress in predicting lapse during alcohol dependence treatment. Alcohol. Clin. Exp. Res. 2016, 40, 1058–1064. [Google Scholar] [CrossRef] [PubMed]
- Serre, F.; Fatseas, M.; Swendsen, J.; Auriacombe, M. Ecological momentary assessment in the investigation of craving and substance use in daily life: A systematic review. Drug Alcohol Depend. 2015, 148, 1–20. [Google Scholar] [CrossRef] [PubMed]
- Robinson, T.E.; Berridge, K.C. The neural basis of drug craving: An incentive-sensitization theory of addiction. Brain Res. Rev. 1993, 18, 247–291. [Google Scholar] [CrossRef]
| Medication | N (%) | Medication | N (%) |
|---|---|---|---|
| BZD | BzRAs | ||
| Estazolam | 36 (21.3%) | Zolpidem | 45 (26.6%) |
| Clonazepam | 23 (13.6%) | Zopiclone | 6 (3.6%) |
| Lorazepam | 15 (8.9%) | ||
| Alprazolam | 12 (7.1%) | Antidepressants/Antipsychotics | |
| Bromazepam | 7 (4.1%) | Trazodone | 7 (4.1%) |
| Flunitrazepam | 5 (3.0%) | Mirtazapine | 2 (1.2%) |
| Diazepam | 3 (1.8%) | Sulpiride | 3 (1.8%) |
| Brotizolam | 2 (1.2%) | ||
| Triazolam | 2 (1.2%) | ||
| Fludiazepam | 1 (0.6%) |
| Predictor | B | β | t |
|---|---|---|---|
| Step 1 | DV: Behavioral Intention | ||
| Attitude (positive) | 0.01 | 0.16 | 1.93 |
| Attitude (negative) | −0.01 | −0.11 | −1.42 |
| Subjective Norm | 0.02 | 0.10 | 1.23 |
| Perceived Behavioral Control | 0.02 | 0.41 | 5.02 *** |
| R2 = 0.26; Adj. R2 = 0.24 F(4, 134) = 11.64; p < 0.001 | |||
| Step 2 | DV: Hypnotic Use | ||
| Behavioral Intention | 1.23 | 0.54 | 7.49 *** |
| Step 3 | DV: Hypnotic Use | ||
| Model 1 | |||
| Attitude (positive) | 0.01 | 0.07 | 0.89 |
| Attitude (negative) | 0.01 | 0.04 | 0.48 |
| Subjective Norm | 0.03 | 0.07 | 0.93 |
| Perceived Behavioral Control | 0.05 | 0.43 | 5.32 *** |
| Model 2 | |||
| Attitude (positive) | 0.00 | 0.01 | 0.12 |
| Attitude (negative) | 0.03 | 0.08 | 1.14 |
| Subjective Norm | 0.01 | 0.04 | 0.48 |
| Perceived Behavioral Control | 0.03 | 0.27 | 3.30 ** |
| Behavioral Intention | 0.95 | 0.41 | 5.07 *** |
| R2 = 0.37; Adj. R2 = 0.34 F(5, 132) = 15.36; p < 0.001 | |||
| Subscale 1: Anticipated Effects | Subscale 2: Compelling Desire | Subscale 3: Preoccupation and Pleasurable Feelings | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Predictor | B | β | t | Predictor | B | β | t | Predictor | B | β | t | |||
| Model 1 | Model 1 | Model 1 | ||||||||||||
| PA | −0.03 | −0.18 | −1.75 | PA | −0.02 | −0.12 | −1.79 | PA | −0.02 | −0.12 | −1.38 | |||
| NA | 0.03 | 0.08 | 1.20 | NA | 0.01 | 0.04 | 0.73 | NA | 0.03 | 0.10 | 1.42 | |||
| SN | 0.01 | 0.03 | 0.37 | SN | 0.02 | 0.06 | 0.94 | SN | 0.01 | 0.02 | 0.25 | |||
| PBC | 0.02 | 0.18 | 2.15 * | PBC | 0.00 | 0.04 | 0.52 | PBC | 0.02 | 0.22 | 2.76 ** | |||
| BI | 0.81 | 0.35 | 4.31 *** | BI | 0.35 | 0.15 | 1.97 | BI | 0.81 | 0.35 | 4.33 *** | |||
| AE | 0.27 | 0.32 | 2.73 ** | CD | 0.60 | 0.64 | 7.19 *** | PP | 0.48 | 0.28 | 3.17 ** | |||
| Model 2 | Model 2 | Model 2 | ||||||||||||
| PA | −0.02 | −0.13 | −1.30 | PA | −0.02 | −0.09 | 1.38 | PA | −0.02 | −0.09 | −1.10 | |||
| NA | 0.03 | 0.08 | 1.22 | NA | 0.02 | 0.05 | 0.84 | NA | 0.02 | 0.08 | 1.15 | |||
| SN | 0.01 | 0.03 | 0.47 | SN | 0.02 | 0.05 | 0.81 | SN | 0.01 | 0.02 | 0.26 | |||
| PBC | 0.02 | 0.18 | 2.08 * | PBC | 0.00 | 0.03 | 0.38 | PBC | 0.02 | 0.22 | 2.74 ** | |||
| BI | 0.86 | 0.37 | 4.52 *** | BI | 0.41 | 0.18 | 2.30 * | BI | 0.82 | 0.35 | 4.49 *** | |||
| AE | 0.21 | 0.25 | 2.05 * | CD | 0.57 | 0.60 | 6.68 *** | PP | 0.48 | 0.28 | 3.22 ** | |||
| BIxAE | −0.02 | −0.12 | −1.60 | BIxCD | −0.02 | −0.13 | −2.05 * | BIxPP | −0.05 | −0.17 | −2.54 * | |||
| Model Comparison | ||||||||||||||
| R2 | Adj. R2 | ΔR2 | ΔF | R2 | Adj. R2 | ΔR2 | ΔF | R2 | Adj. R2 | ΔR2 | ΔF | |||
| Model 1 | 0.40 | 0.37 | 0.40 | 14.66 *** | 0.55 | 0.52 | 0.55 | 26.31 *** | 0.41 | 0.38 | 0.41 | 15.35 *** | ||
| Model 2 | 0.41 | 0.38 | 0.01 | 2.55 | 0.56 | 0.54 | 0.01 | 4.21 * | 0.44 | 0.41 | 0.03 | 6.46 * | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, C.-M.; Lai, Y.-S.; Huang, Y.-H.; Huang, Y.-C.; Lee, H.-C. Predicting Hypnotic Use among Insomnia Patients with the Theory of Planned Behavior and Craving. Behav. Sci. 2022, 12, 209. https://doi.org/10.3390/bs12070209
Yang C-M, Lai Y-S, Huang Y-H, Huang Y-C, Lee H-C. Predicting Hypnotic Use among Insomnia Patients with the Theory of Planned Behavior and Craving. Behavioral Sciences. 2022; 12(7):209. https://doi.org/10.3390/bs12070209
Chicago/Turabian StyleYang, Chien-Ming, Yu-Shuan Lai, Yun-Hsin Huang, Ya-Chuan Huang, and Hsin-Chien Lee. 2022. "Predicting Hypnotic Use among Insomnia Patients with the Theory of Planned Behavior and Craving" Behavioral Sciences 12, no. 7: 209. https://doi.org/10.3390/bs12070209
APA StyleYang, C.-M., Lai, Y.-S., Huang, Y.-H., Huang, Y.-C., & Lee, H.-C. (2022). Predicting Hypnotic Use among Insomnia Patients with the Theory of Planned Behavior and Craving. Behavioral Sciences, 12(7), 209. https://doi.org/10.3390/bs12070209






