An Examination of the Relationships between Eating-Disorder Symptoms, Difficulties with Emotion Regulation, and Mental Health in People with Binge Eating Disorder
Abstract
1. Introduction
2. Materials and Methods
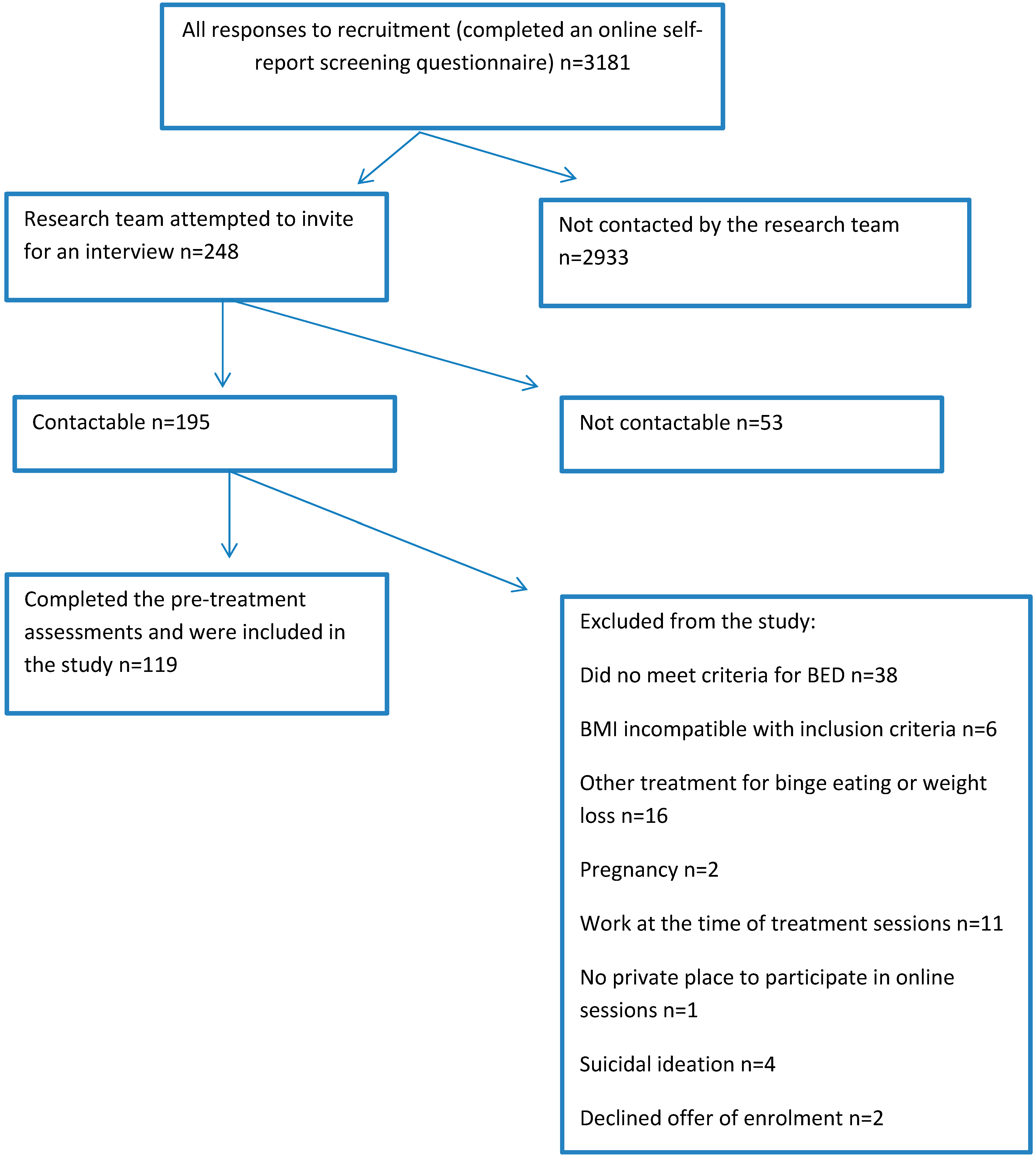
2.1. Study Design and Participants
2.2. Ethics
2.3. Measures
2.3.1. Demographic Characteristics
2.3.2. Eating Disorder Examination Questionnaire (EDE-Q)
2.3.3. Loss of Control over Eating Scale (LOCES)
2.3.4. Difficulties in Emotion Regulation Scale (DERS)
2.3.5. Depression, Anxiety and Stress Scale (DASS-21)
2.3.6. 12-Item Short Form Survey (SF-12)
2.4. Statistical Analyses
3. Results
3.1. Participants’ Demographic Characteristics
3.2. Bivariate Analyses
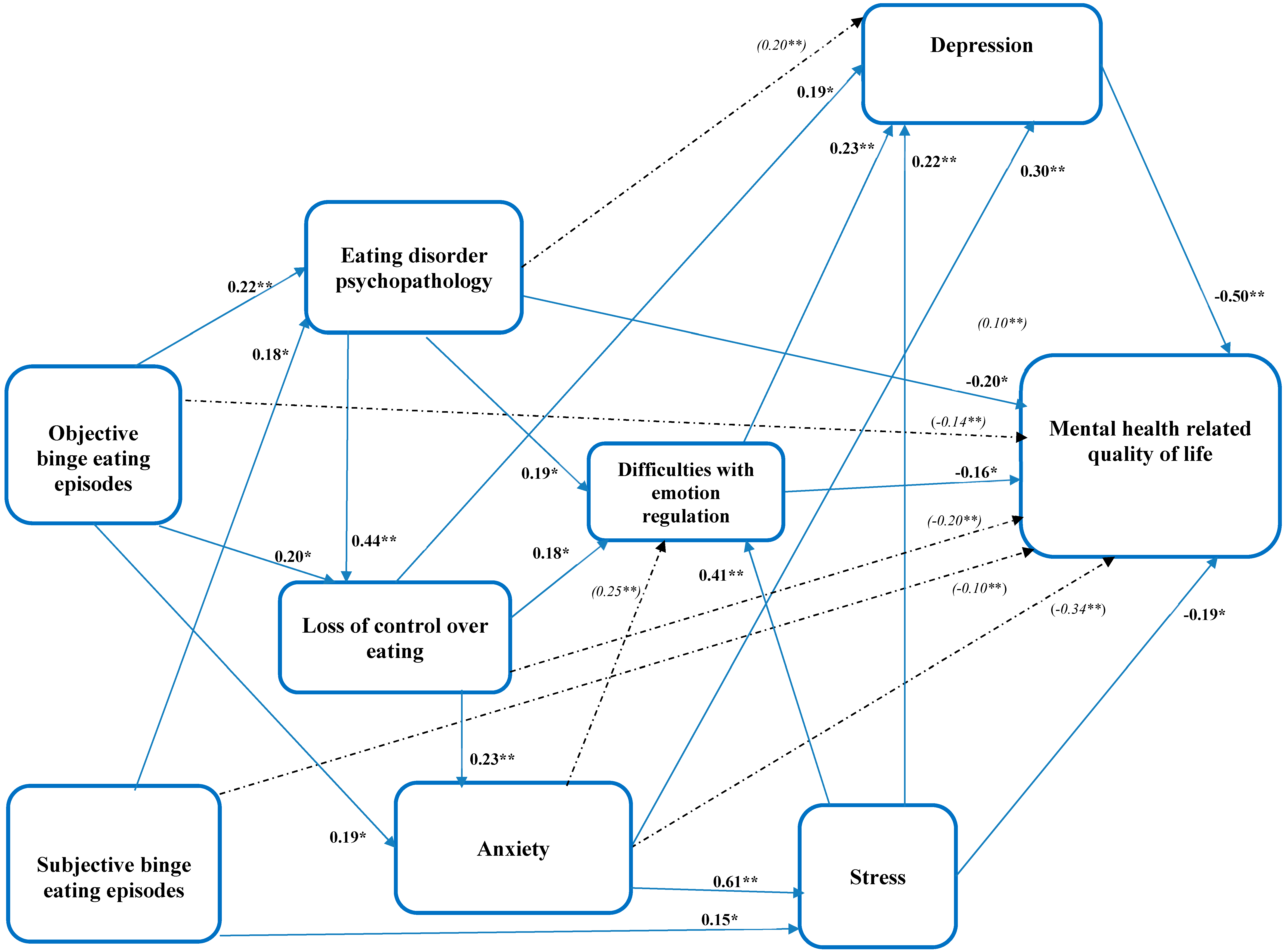
3.3. Path Analysis
3.3.1. Correlates of Mental-Health-Related Quality of Life (HRQoL)
3.3.2. Correlates of Difficulties with Emotion Regulation
3.3.3. Correlates of Depression
3.3.4. Correlates of Anxiety
3.3.5. Correlates of Psychological Stress
3.3.6. Correlates of Eating-Disorder Psychopathology
3.3.7. Correlates of Loss of Control over Eating
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
Appendix B
| 95% CI for Mean | Range | ||
|---|---|---|---|
| Clinical Features | Mean (SD) | (Lower Bound, Upper Bound) | Minimum, Maximum |
| Difficulties with emotion regulation | 100.3 (24.8) | (95.8, 100.8) | 47.0, 161.0 |
| Objective binge-eating episodes | 14.2 (15.2) | (11.5, 17.0) | 0.0, 151.0 |
| Subjective binge-eating episodes | 10.5 (8.0) | (9.1, 12.0) | 0.0, 28.0 |
| Eating-disorder psychopathology | 3.7 (0.9) | (3.5, 3.9) | 1.9, 5.5 |
| Loss of control over eating | 81.9 (14.1) | (79.4, 84.5) | 42.0, 115.0 |
| Depression | 15.6 (9.7) | (13.9, 17.4) | 0.0, 40.0 |
| Anxiety | 10.3 (7.4) | (9.0, 11.7) | 0.0, 30.0 |
| Stress | 20.8 (8.3) | (19.3, 22.3) | 2.0, 38.0 |
| Mental-health-related quality of life | 32.7 (9.7) | (31.0, 34.5) | 13.3, 55.9 |
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Publishing: Arlington VA, USA, 2013. [Google Scholar]
- Araujo, D.M.; Santos, G.F.; Nardi, A.E. Binge eating disorder and depression: A systematic review. World J. Biol. Psychiatry 2010, 11, 199–207. [Google Scholar] [CrossRef] [PubMed]
- Rosenbaum, D.L.; White, K.S. The Role of Anxiety in Binge Eating Behavior: A Critical Examination of Theory and Empirical Literature. Health Psychol. Res. 2013, 1, e19. [Google Scholar] [CrossRef] [PubMed]
- Udo, T.; Grilo, C.M. Psychiatric and medical correlates of DSM-5 eating disorders in a nationally representative sample of adults in the United States. Int. J. Eat. Disord. 2019, 52, 42–50. [Google Scholar] [CrossRef]
- Rosenberg, N.; Bloch, M.; Ben Avi, I.; Rouach, V.; Schreiber, S.; Stern, N.; Greenman, Y. Cortisol response and desire to binge following psychological stress: Comparison between obese subjects with and without binge eating disorder. Psychiatry Res. 2012, 208, 156–161. [Google Scholar] [CrossRef]
- Appolinario, J.C.; Sichieri, R.; Lopes, C.S.; Moraes, C.E.; da Veiga, G.V.; Freitas, S.; Nunes, M.A.A.; Wang, Y.-P.; Hay, P. Correlates and impact of DSM-5 binge eating disorder, bulimia nervosa and recurrent binge eating: A representative population survey in a middle-income country. Soc. Psychiatry Psychiatr. Epidemiol. 2022, 57, 1491–1503. [Google Scholar] [CrossRef]
- Vancampfort, D.; De Herdt, A.; Vanderlinden, J.; Lannoo, M.; Soundy, A.; Pieters, G.; Adriaens, A.; De Hert, M.; Probst, M. Health related quality of life, physical fitness and physical activity participation in treatment-seeking obese persons with and without binge eating disorder. Psychiatry Res. 2014, 216, 97–102. [Google Scholar] [CrossRef]
- Gratz, K.L.; Roemer, L. Multidimensional Assessment of Emotion Regulation and Dysregulation: Development, Factor Structure, and Initial Validation of the Difficulties in Emotion Regulation Scale. J. Psychopathol. Behav. Assess. 2004, 26, 41–54. [Google Scholar] [CrossRef]
- Trompeter, N.; Bussey, K.; Forbes, M.K.; Mitchison, D. Emotion Dysregulation within the CBT-E Model of Eating Disorders: A Narrative Review. Cogn. Ther. Res. 2021, 45, 1021–1036. [Google Scholar] [CrossRef]
- Mallorquí-Bagué, N.; Vintró-Alcaraz, C.; Sánchez, I.; Riesco, N.; Agüera, Z.; Granero, R.; Jiménez-Múrcia, S.; Menchón, J.M.; Treasure, J.; Fernández-Aranda, F. Emotion Regulation as a Transdiagnostic Feature Among Eating Disorders: Cross-sectional and Longitudinal Approach. Eur. Eat. Disord. Rev. 2018, 26, 53–61. [Google Scholar] [CrossRef]
- Monell, E.; Clinton, D.; Birgegård, A. Emotion dysregulation and eating disorders—Associations with diagnostic presentation and key symptoms. Int. J. Eat. Disord. 2018, 51, 921–930. [Google Scholar] [CrossRef] [PubMed]
- Benzerouk, F.; Djerada, Z.; Bertin, E.; Barrière, S.; Gierski, F.; Kaladjian, A. Contributions of Emotional Overload, Emotion Dysregulation, and Impulsivity to Eating Patterns in Obese Patients with Binge Eating Disorder and Seeking Bariatric Surgery. Nutrients 2020, 12, 3099. [Google Scholar] [CrossRef] [PubMed]
- Walenda, A.; Kostecka, B.; Santangelo, P.S.; Kucharska, K. Examining emotion regulation in binge-eating disorder. Bord. Personal. Disord. Emot. Dysregulation 2021, 8, 25. [Google Scholar] [CrossRef] [PubMed]
- Rania, M.; Monell, E.; Sjölander, A.; Bulik, C.M. Emotion dysregulation and suicidality in eating disorders. Int. J. Eat. Disord. 2021, 54, 313–325. [Google Scholar] [CrossRef] [PubMed]
- FAPESP. Available online: https://bv.fapesp.br/en/auxilios/103926/development-of-an-improved-and-accessible-treatment-program-for-people-with-binge-eating-disorder-an/ (accessed on 10 November 2022).
- Fairburn, C. Cognitive Behavior Therapy and Eating Disorders; Guilford: New York, NY, USA, 2008. [Google Scholar]
- Berg, K.C.; Peterson, C.B.; Frazier, P.; Crow, S.J. Psychometric evaluation of the eating disorder examination and eating disorder examination-questionnaire: A systematic review of the literature. Int. J. Eat. Disord. 2012, 45, 428–438. [Google Scholar] [CrossRef] [PubMed]
- Palavras, M.A.; Hay, P.; Touyz, S.; Sainsbury, A.; Luz, F.; Swinbourne, J. Comparing cognitive behavioural therapy for eating disorders integrated with behavioural weight loss therapy to cognitive behavioural therapy-enhanced alone in overweight or obese people with bulimia nervosa or binge eating disorder: Study protocol for a randomised controlled trial. Trials 2015, 16, 578. [Google Scholar] [CrossRef]
- Machado, P.P.P.; Martins, C.; Vaz, A.R.; Conceição, E.; Bastos, A.P.; Gonçalves, S. Eating Disorder Examination Questionnaire: Psychometric Properties and Norms for the Portuguese Population. Eur. Eat. Disord. Rev. 2014, 22, 448–453. [Google Scholar] [CrossRef] [PubMed]
- Latner, J.D.; Mond, J.M.; Kelly, M.C.; Haynes, S.N.; Hay, P.J. The Loss of Control over Eating Scale: Development and psychometric evaluation. Int. J. Eat. Disord. 2014, 47, 647–659. [Google Scholar] [CrossRef]
- Luz, F.Q.d.; Sainsbury, A.; Estella, N.M.; Cogo, H.; Touyz, S.W.; Palavras, M.A.; Latner, J.D.; Claudino, A.; Hay, P. An empirical evaluation of the translation to Brazilian Portuguese of the Loss of Control over Eating Scale (LOCES). Rev. De Psiquiatr. Clin. 2016, 43, 1–5. [Google Scholar] [CrossRef]
- Burton, A.L.; Brown, R.; Abbott, M.J. Overcoming difficulties in measuring emotional regulation: Assessing and comparing the psychometric properties of the DERS long and short forms. Cogent Psychol. 2022, 9, 2060629. [Google Scholar] [CrossRef]
- Cancian, A.C.M.; Souza, L.A.S.d.; Silva, V.H.P.E.; Machado, W.d.L.; Oliveira, M.d.S. Psychometric properties of the Brazilian version of the Difficulties in Emotion Regulation Scale (DERS). Trends Psychiatry Psychother. 2019, 41, 18–26. [Google Scholar] [CrossRef]
- Lovibond, S.H.; Lovibond, P.F. Manual for the Depression Anxiety Stress Scales, 2nd ed.; Psychology Foundation of Australia: Sydney, NSW, Australia, 1995. [Google Scholar]
- Henry, J.D.; Crawford, J.R. The short-form version of the Depression Anxiety Stress Scales (DASS-21): Construct validity and normative data in a large non-clinical sample. Br. J. Clin. Psychol. 2005, 44, 227–239. [Google Scholar] [CrossRef] [PubMed]
- Vignola, R.C.B.; Tucci, A.M. Adaptation and validation of the depression, anxiety and stress scale (DASS) to Brazilian Portuguese. J. Affect. Disord. 2014, 155, 104–109. [Google Scholar] [CrossRef] [PubMed]
- Huo, T.; Guo, Y.; Shenkman, E.; Muller, K. Assessing the reliability of the short form 12 (SF-12) health survey in adults with mental health conditions: A report from the wellness incentive and navigation (WIN) study. Health Qual. Life Outcomes 2018, 16, 34. [Google Scholar] [CrossRef]
- Mitchison, D.; Hay, P.; Engel, S.; Crosby, R.; Le Grange, D.; Lacey, H.; Mond, J.; Slewa-Younan, S.; Touyz, S. Assessment of quality of life in people with severe and enduring anorexia nervosa: A comparison of generic and specific instruments. BMC Psychiatry 2013, 13, 284. [Google Scholar] [CrossRef] [PubMed]
- Fagundes Silveira, M.; Almeida, J.C.; Silveira Freire, R.; Sant’Ana Haikal, D.; de Barros Lima Martins, A.E. Propriedades psicométricas do instrumento de avaliação da qualidade de vida: 12-Item health survey (SF-12). Ciência Saúde Coletiva 2013, 18, 1923–1931. [Google Scholar] [CrossRef]
- National Statistics Directorate (NSD); Ministry of Finance; ICF Macro. Timor-Leste Demographic and Health Survey 2009–10; NSD and ICF Macro: Dili, Timor-Leste, 2010.
- Marcoulides, G.A.; Schumacker, R.E. Advanced Structural Equation Modeling: Issues and Techniques; Psychology Press: New York, NY, USA, 1996. [Google Scholar]
- Hu, L.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct Equ. Model 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Muthén, L.K.; Muthén, B.O. Mplus User’s Guide, 7th ed.; Muthén & Muthén: Los Angeles, CA, USA, 1998–2012. [Google Scholar]
- Kline, R.B. Principles and Practice of Structural Equation Modeling, 3rd ed.; The Guilford Press: New York, NY, USA, 2011. [Google Scholar]
- IBMCorp. IBM SPSS Statistics for Windows; Version 27.0; IBM Corp.: Armonk, NY, USA, 2020. [Google Scholar]
- Hay, P.; Palavras, M.A.; da Luz, F.Q.; Dos Anjos Garnes, S.; Sainsbury, A.; Touyz, S.; Appolinario, J.C.; Claudino, A.M. Physical and mental health outcomes of an integrated cognitive behavioural and weight management therapy for people with an eating disorder characterized by binge eating and a high body mass index: A randomized controlled trial. BMC Psychiatry 2022, 22, 355. [Google Scholar] [CrossRef]
- Fairburn, C.G.; Cooper, Z.; Shafran, R. Cognitive behaviour therapy for eating disorders: A “transdiagnostic” theory and treatment. Behav. Res. Ther. 2003, 41, 509–528. [Google Scholar] [CrossRef]
- Q da Luz, F.; Hay, P.; Wisniewski, L.; Cordás, T.; Sainsbury, A. The treatment of binge eating disorder with cognitive behavior therapy and other therapies: An overview and clinical considerations. Obes. Rev. 2021, 22, e13180. [Google Scholar] [CrossRef]
- Baer, R.A.; Carmody, J.; Hunsinger, M. Weekly Change in Mindfulness and Perceived Stress in a Mindfulness-Based Stress Reduction Program. J. Clin. Psychol. 2012, 68, 755–765. [Google Scholar] [CrossRef]
- Rozakou-Soumalia, N.; Dârvariu, Ş.; Sjögren, J.M. Dialectical Behaviour Therapy Improves Emotion Dysregulation Mainly in Binge Eating Disorder and Bulimia Nervosa: A Systematic Review and Meta-Analysis. J. Pers. Med. 2021, 11, 931. [Google Scholar] [CrossRef] [PubMed]
- Linardon, J.; Fairburn, C.G.; Fitzsimmons-Craft, E.E.; Wilfley, D.E.; Brennan, L. The empirical status of the third-wave behaviour therapies for the treatment of eating disorders: A systematic review. Clin. Psychol. Rev. 2017, 58, 125–140. [Google Scholar] [CrossRef] [PubMed]
- Monteleone, A.M.; Pellegrino, F.; Croatto, G.; Carfagno, M.; Hilbert, A.; Treasure, J.; Wade, T.; Bulik, C.M.; Zipfel, S.; Hay, P.; et al. Treatment of eating disorders: A systematic meta-review of meta-analyses and network meta-analyses. Neurosci. Biobehav. Rev. 2022, 142, 104857. [Google Scholar] [CrossRef]
- Giel, K.E.; Bulik, C.M.; Fernandez-Aranda, F.; Hay, P.; Keski-Rahkonen, A.; Schag, K.; Schmidt, U.; Zipfel, S. Binge eating disorder. Nat. Rev. Dis. Prim. 2022, 8, 16. [Google Scholar] [CrossRef] [PubMed]
| Characteristics of a binge-eating episode: |
|
| Binge-eating episodes were associated with three or more of the following five criteria: |
|
| Additional criteria: |
|
| Demographic Characteristics | Mean Scores of Clinical Features | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Difficulties with Emotion Regulation | Objective Binge Eating | Subjective Binge Eating | Eating-Disorder Psychopathology | Loss of Control over Eating | Depression | Anxiety | Stress | Mental-Health-Related Quality of Life | ||
| Number (%) | Mean | Mean | Mean | Mean | Mean | Mean | Mean | Mean | Mean | |
| All participants | 119 (100.0) | 100.3 | 14.2 | 10.5 | 3.7 | 81.9 | 15.6 | 10.3 | 20.8 | 32.7 |
| Gender | ||||||||||
| Male | 11 (9.2) | 100.4 | 19.8 | 10.3 | 3.6 | 82.8 | 16.2 | 10.9 | 24.4 | 29.0 |
| Female | 108 (90.8) | 100.2 | 13.7 | 10.6 | 3.7 | 81.8 | 15.6 | 10.3 | 20.5 | 33.1 |
| p-values from t-test | 0.99 | 0.20 | 0.91 | 0.64 | 0.82 | 0.85 | 0.78 | 0.14 | 0.18 | |
| Age group | ||||||||||
| <30 | 26 (21.8) | 106.1 | 13.4 | 11.3 | 3.8 | 84.3 | 14.8 | 10.8 | 22.5 | 32.3 |
| 30–39 | 54 (45.4) | 96.8 | 15.7 | 10.4 | 3.7 | 82.5 | 16.2 | 9.5 | 20.5 | 32.0 |
| 40 and above | 39 (32.8) | 101.1 | 12.8 | 10.2 | 3.7 | 79.5 | 15.5 | 11.1 | 20.3 | 34.0 |
| p-values from F-test | 0.28 | 0.63 | 084 | 0.81 | 0.37 | 0.83 | 0.53 | 0.52 | 0.60 | |
| Race | ||||||||||
| White | 89 (75.0) | 99.3 | 13.1 | 10.6 | 3.7 | 82.1 | 15.7 | 10.6 | 21.0 | 33.3 |
| Black and others | 30 (25.0) | 103.2 | 17.6 | 10.4 | 3.7 | 81.3 | 15.5 | 9.4 | 20.3 | 31.0 |
| p-values from t-test | 0.45 | 0.16 | 0.93 | 0.739 | 0.80 | 0.94 | 0.43 | 0.663 | 0.27 | |
| Occupation | ||||||||||
| Employed full/part time | 78 (66) | 98.7 | 15.5 | 10.9 | 3.7 | 83.2 | 15.5 | 10.6 | 21.3 | 32.9 |
| Unemployed/Others | 41 (34) | 103.1 | 11.8 | 9.8 | 3.7 | 79.4 | 16.0 | 9.8 | 20.0 | 32.5 |
| p-values from t-test | 0.36 | 0.20 | 0.44 | 0.90 | 0.16 | 0.81 | 0.55 | 0.40 | 0.82 | |
| Marital status | ||||||||||
| Married/Living with partner | 77 (65) | 100.8 | 15.7 | 10.7 | 3.8 | 83.3 | 15.4 | 10.1 | 21.0 | 33.1 |
| Single/Never married/Others | 42 (35) | 99.3 | 11.5 | 10.2 | 3.6 | 79.4 | 16.1 | 10.8 | 20.5 | 32.0 |
| p-values from t-test | 0.75 | 0.15 | 0.71 | 0.34 | 0.15 | 0.68 | 0.63 | 0.76 | 0.53 | |
| Income | ||||||||||
| None to BRL 3.135 | 69 (58) | 99.6 | 14.3 | 10.4 | 3.7 | 81.9 | 15.4 | 10.5 | 20.2 | 33.3 |
| Above BRL 3.135 | 50 (42) | 101.1 | 14.1 | 10.7 | 3.6 | 82.0 | 15.9 | 10.1 | 21.8 | 31.9 |
| p-values from t-test | 0.74 | 0.95 | 0.83 | 0.47 | 0.96 | 0.80 | 0.76 | 0.30 | 0.42 | |
| Measures and Correlation Co-Efficient (r) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Measures | Difficulties with Emotion Regulation | Objective Binge Eating | Subjective Binge Eating | Eating-Disorder Psycho-Pathology | Loss of Control over Eating | Depression | Anxiety | Stress | Mental-Health-Related Quality of Life |
| r | r | r | r | r | r | r | r | r | |
| Difficulties with emotion regulation | 1.00 | ||||||||
| Objective binge-eating episodes | 0.09 | 1.00 | |||||||
| Subjective binge-eating episodes | 0.09 | 0.07 | 1.00 | ||||||
| Eating-disorder psychopathology | 0.34 ** | 0.21 * | 0.19 * | 1.00 | |||||
| Loss of control over eating | 0.31 ** | 0.29 ** | 0.13 | 0.48 ** | 1.00 | ||||
| Depression | 0.49 ** | 0.07 | 0.06 | 0.27 ** | 0.32 ** | 1.00 | |||
| Anxiety | 0.34 ** | 0.23 * | −0.01 | 0.17 | 0.28 ** | 0.52 ** | 1.00 | ||
| Stress | 0.47 ** | 0.07 | 0.16 | 0.21 * | 0.16 | 0.57 ** | 0.63 ** | 1.00 | |
| Mental-health-related quality of life | −0.47 ** | 0.00 | −0.13 | −0.33 ** | −0.25 ** | −0.67 ** | −0.35 ** | −0.49 ** | 1.00 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
da Luz, F.Q.; Mohsin, M.; Jana, T.A.; Marinho, L.S.; Santos, E.d.; Lobo, I.; Pascoareli, L.; Gaeta, T.; Ferrari, S.; Teixeira, P.C.; et al. An Examination of the Relationships between Eating-Disorder Symptoms, Difficulties with Emotion Regulation, and Mental Health in People with Binge Eating Disorder. Behav. Sci. 2023, 13, 234. https://doi.org/10.3390/bs13030234
da Luz FQ, Mohsin M, Jana TA, Marinho LS, Santos Ed, Lobo I, Pascoareli L, Gaeta T, Ferrari S, Teixeira PC, et al. An Examination of the Relationships between Eating-Disorder Symptoms, Difficulties with Emotion Regulation, and Mental Health in People with Binge Eating Disorder. Behavioral Sciences. 2023; 13(3):234. https://doi.org/10.3390/bs13030234
Chicago/Turabian Styleda Luz, Felipe Q., Mohammed Mohsin, Tatiana A. Jana, Leticia S. Marinho, Edilaine dos Santos, Isabella Lobo, Luisa Pascoareli, Tamiris Gaeta, Silvia Ferrari, Paula C. Teixeira, and et al. 2023. "An Examination of the Relationships between Eating-Disorder Symptoms, Difficulties with Emotion Regulation, and Mental Health in People with Binge Eating Disorder" Behavioral Sciences 13, no. 3: 234. https://doi.org/10.3390/bs13030234
APA Styleda Luz, F. Q., Mohsin, M., Jana, T. A., Marinho, L. S., Santos, E. d., Lobo, I., Pascoareli, L., Gaeta, T., Ferrari, S., Teixeira, P. C., Cordás, T., & Hay, P. (2023). An Examination of the Relationships between Eating-Disorder Symptoms, Difficulties with Emotion Regulation, and Mental Health in People with Binge Eating Disorder. Behavioral Sciences, 13(3), 234. https://doi.org/10.3390/bs13030234






