Comparing Depression Prevalence and Associated Symptoms with Intolerance of Uncertainty among Chinese Urban and Rural Adolescents: A Network Analysis
Abstract
:1. Introduction
2. Methods
2.1. Participants
2.2. Measures
2.2.1. Patient Health Questionnaire-9 (PHQ-9)
2.2.2. Intolerance of Uncertainty Scale-12 (IUS-12)
2.3. Data Analysis
2.3.1. Network Estimation
2.3.2. Network Stability and Accuracy
2.3.3. Network Comparison
3. Results
3.1. Prevalence of Depression and Descriptive Statistics
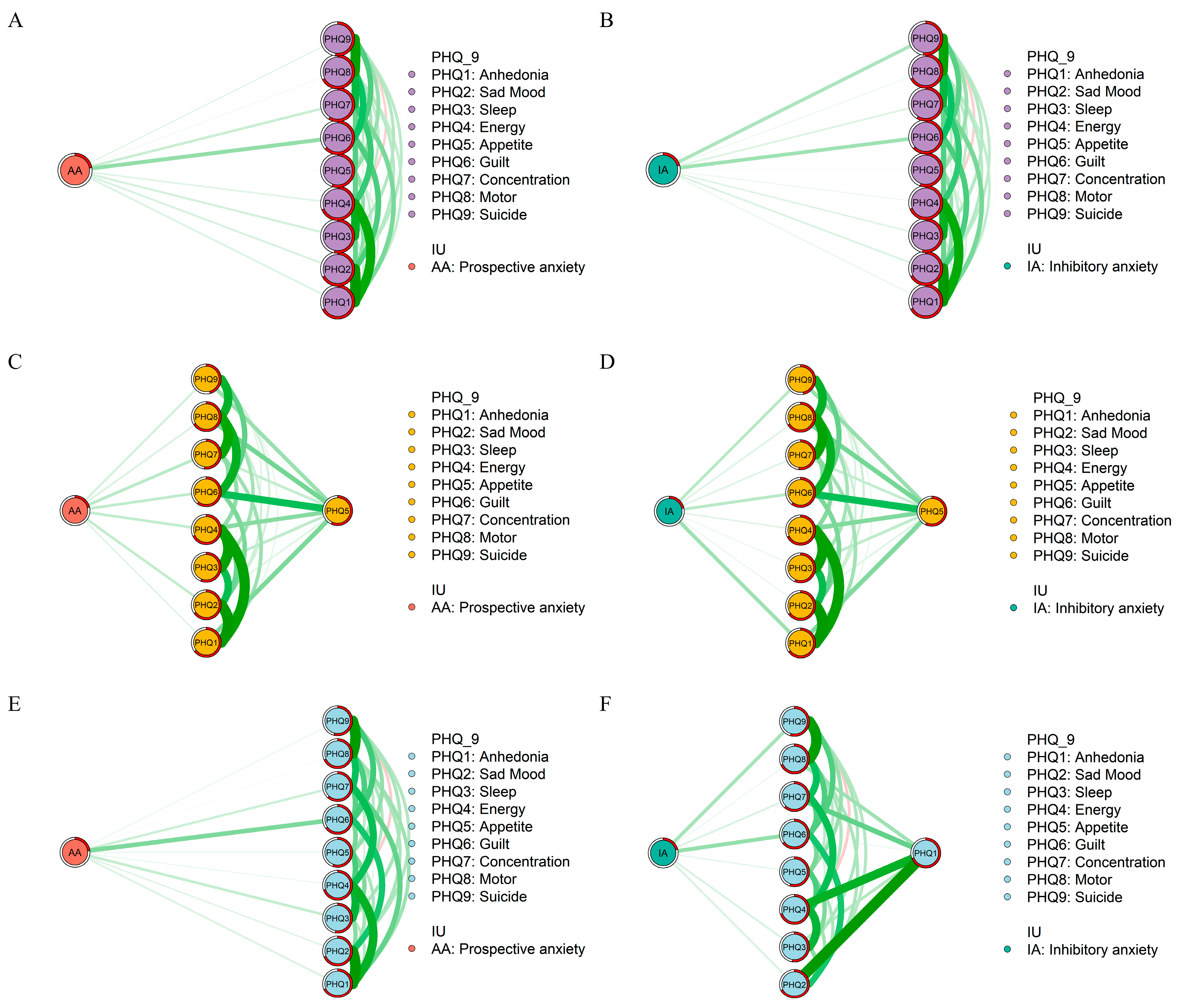
3.2. Symptom Network and Flow Network Structures
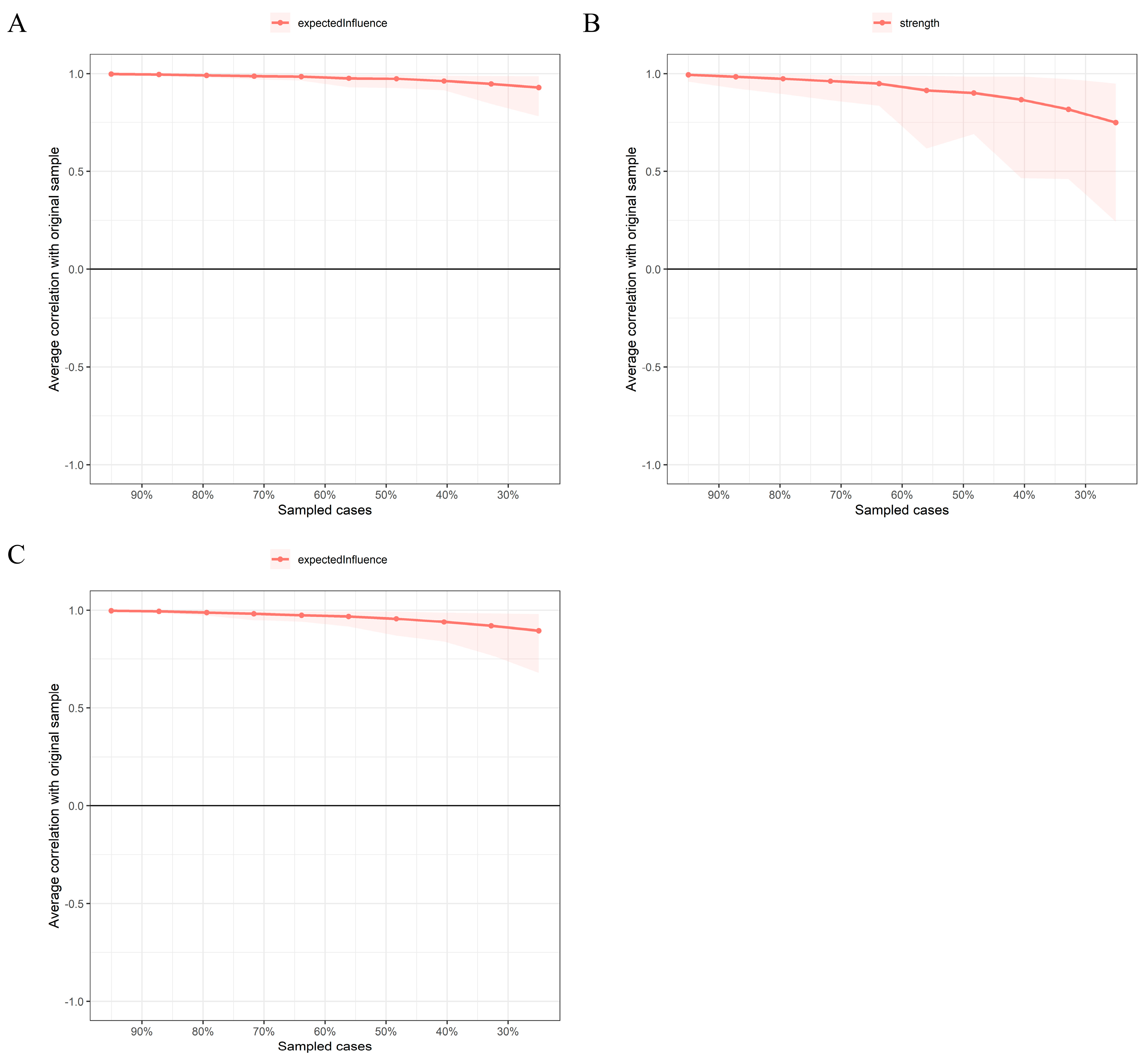
3.3. Network Stability and Accuracy
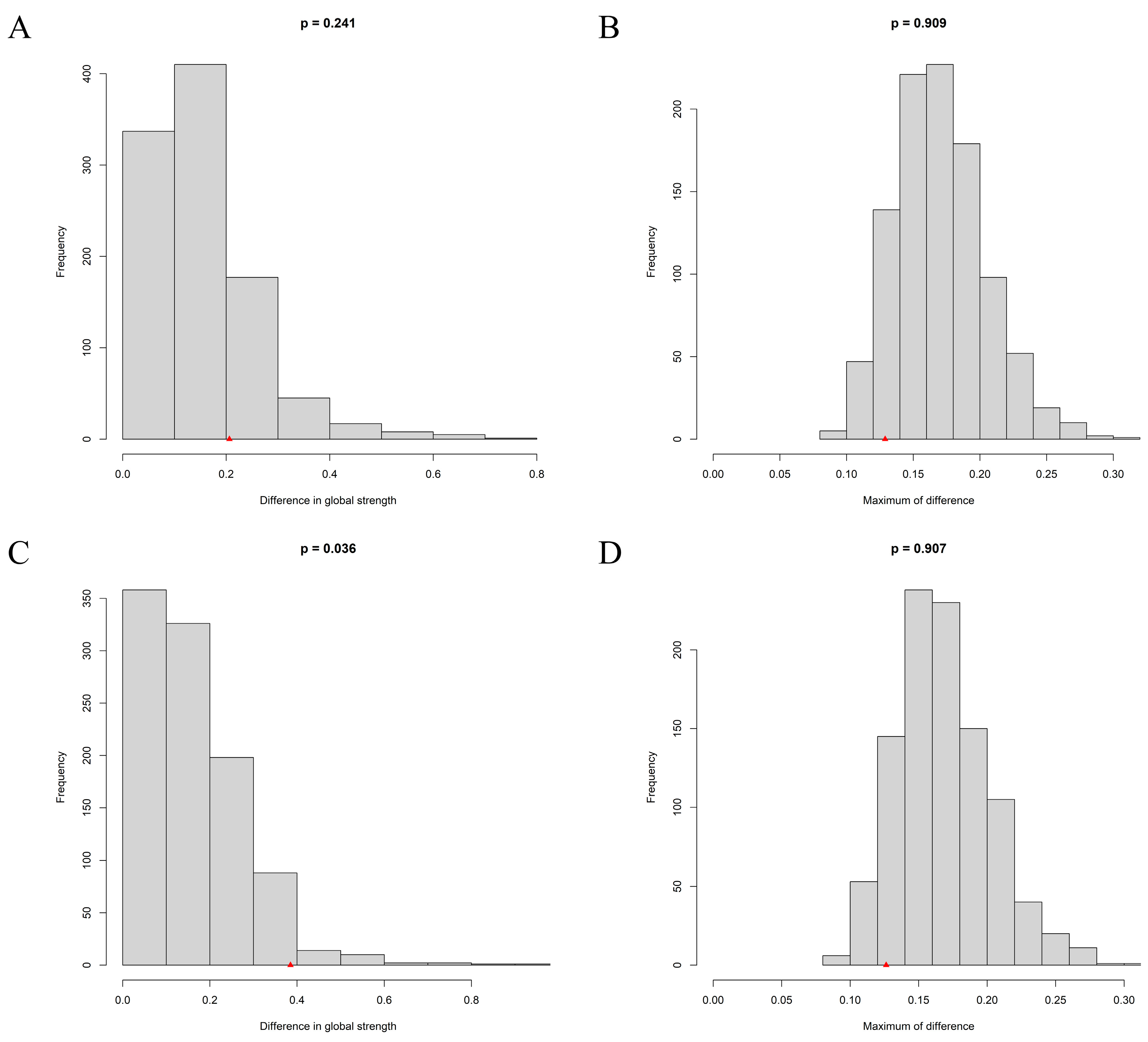
3.4. Network Comparison between Urban and Rural Adolescents
3.5. Sensitivity Analysis
4. Discussion
4.1. Differences in the Prevalence Rate of and Mean Level of Depression between Urban and Rural Adolescents
4.2. Network Comparison of Depression Symptom Network between Urban and Rural Adolescents
4.3. Network Comparison of Flow Networks between Urban and Rural Adolescents
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Malhi, G.S.; Mann, J.J. Depression. Lancet 2018, 392, 2299–2312. [Google Scholar] [CrossRef] [PubMed]
- Ma, L.; Mazidi, M.; Li, K.; Li, Y.X.; Chen, S.Q.; Kirwan, R.; Zhou, H.X.; Yan, N.; Rahman, A.; Wang, W.D.; et al. Prevalence of mental health problems among children and adolescents during the COVID-19 pandemic: A systematic review and meta-analysis. J. Affect. Disord. 2021, 293, 78–89. [Google Scholar] [CrossRef] [PubMed]
- Owens, M.; Stevenson, J.; Hadwin, J.A.; Norgate, R. Anxiety and depression in academic performance: An exploration of the mediating factors of worry and working memory. Sch. Psychol. Int. 2012, 33, 433–449. [Google Scholar] [CrossRef]
- Cermak, I.; Klimusova, H.; Vizdalova, H. Depression in childhood and its relation to problems of behaviour. Ceskoslovenska Psychol. 2005, 49, 223–236. [Google Scholar]
- Wolfersdorf, M. Depression and suicide. Bundesgesundheitsblatt-Gesundh.-Gesundh. 2008, 51, 443–450. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.X.; Tigelaar, D.E.H.; Admiraal, W. Connecting rural schools to quality education: Rural teachers’ use of digital educational resources. Comput. Hum. Behav. 2019, 101, 68–76. [Google Scholar] [CrossRef]
- Zhang, L. In Research on Financial Support for Rural Economic Development in China. In Proceedings of the 3rd International Conference on Advanced Engineering Materials and Architecture Science (ICAEMAS), Huhhot, China, 26–27 July 2014; pp. 1623–1626. [Google Scholar]
- Xie, J.F.; Liu, M.; Ding, S.Q.; Zhong, Z.Q.; Zeng, S.A.; Liu, A.Z.; He, S.W.; Zhou, J.D. Attitudes toward depression among rural primary healthcare providers in hunan areas, China: A cross sectional study. BMC Med. Educ. 2023, 23, 1–10. [Google Scholar] [CrossRef]
- Bronfenbrenner, U. Ecological Systems Theory; Oxford University Press: Oxford, UK, 2000. [Google Scholar]
- Halldorsdottir, T.; Piechaczek, C.; de Matos, A.P.S.; Czamara, D.; Pehl, V.; Wagenbuechler, P.; Feldmann, L.; Quickenstedt-Reinhardt, P.; Allgaier, A.K.; Freisleder, F.J.; et al. Polygenic Risk: Predicting Depression Outcomes in Clinical and Epidemiological Cohorts of Youths. Am. J. Psychiatry 2019, 176, 615–625. [Google Scholar] [CrossRef]
- Li, G.; Mei, J.; You, J.; Miao, J.; Song, X.; Sun, W.; Lan, Y.; Qiu, X.; Zhu, Z. Sociodemographic characteristics associated with adolescent depression in urban and rural areas of Hubei province: A cross-sectional analysis. BMC Psychiatry 2019, 19, 386. [Google Scholar] [CrossRef] [Green Version]
- Freeman, A.; Tyrovolas, S.; Koyanagi, A.; Chatterji, S.; Leonardi, M.; Ayuso-Mateos, J.L.; Tobiasz-Adamczyk, B.; Koskinen, S.; Rummel-Kluge, C.; Haro, J.M. The role of socio-economic status in depression: Results from the COURAGE (aging survey in Europe). BMC Public Health 2016, 16, 1098. [Google Scholar] [CrossRef] [Green Version]
- Lu, W.H. Adolescent Depression: National Trends, Risk Factors, and Healthcare Disparities. Am. J. Health Behav. 2019, 43, 181–194. [Google Scholar]
- Christina, S.; Magson, N.R.; Kakar, V.; Rapee, R.M. The bidirectional relationships between peer victimization and internalizing problems in school-aged children: An updated systematic review and meta-analysis. Clin. Psychol. Rev. 2021, 85, 101979. [Google Scholar]
- Shihata, S.; McEvoy, P.M.; Mullan, B.A.; Carleton, R.N. Intolerance of uncertainty in emotional disorders: What uncertainties remain? J. Anxiety Disord. 2016, 41, 115–124. [Google Scholar] [PubMed] [Green Version]
- McEvoy, P.M.; Mahoney, A.E.J. To Be Sure, To Be Sure: Intolerance of Uncertainty Mediates Symptoms of Various Anxiety Disorders and Depression. Behav. Ther. 2012, 43, 533–545. [Google Scholar]
- Dugas, M.J.; Koerner, N. Cognitive-behavioral treatment for generalized anxiety disorder: Current status and future directions. J. Cogn. Psychother. 2005, 19, 61–81. [Google Scholar]
- Boelen, P.A.; Vrinssen, I.; van Tulder, F. Intolerance of Uncertainty in Adolescents Correlations With Worry, Social Anxiety, and Depression. J. Nerv. Ment. Dis. 2010, 198, 194–200. [Google Scholar] [PubMed]
- Lazarus, R.S. Emotion and Adaptation; Oxford University Press: Oxford, UK, 1991. [Google Scholar]
- Bakioglu, F.; Korkmaz, O.; Ercan, H. Fear of COVID-19 and Positivity: Mediating Role of Intolerance of Uncertainty, Depression, Anxiety, and Stress. Int. J. Ment. Health Addict. 2021, 19, 2369–2382. [Google Scholar] [PubMed]
- Dugas, M.J.; Savard, P.; Gaudet, A.; Turcotte, J.; Laugesen, N.; Robichaud, M.; Francis, K.; Koerner, N. Can the Components of a Cognitive Model Predict the Severity of Generalized Anxiety Disorder? Behav. Ther. 2007, 38, 169–178. [Google Scholar]
- Korkmaz, H.; Guloglu, B. The role of uncertainty tolerance and meaning in life on depression and anxiety throughout Covid-19 pandemic. Personal. Individ. Differ. 2021, 179, 110952. [Google Scholar]
- Moulds, M.L.; Kandris, E.; Starr, S.; Wong, A.C.M. The relationship between rumination, avoidance and depression in a non-clinical sample. Behav. Res. Ther. 2007, 45, 251–261. [Google Scholar]
- Stevens, K.; Rogers, T.; Campbell, M.; Bjorgvinsson, T.; Kertz, S. A transdiagnostic examination of decreased intolerance of uncertainty and treatment outcome. Cogn. Behav. Ther. 2018, 47, 19–33. [Google Scholar] [PubMed]
- Borsboom, D.; Cramer, A.O.J. Network Analysis: An Integrative Approach to the Structure of Psychopathology. Annu. Rev. Clin. Psychol. 2013, 9, 91–121. [Google Scholar] [PubMed] [Green Version]
- Borsboom, D. A network theory of mental disorders. World Psychiatry 2017, 16, 5–13. [Google Scholar]
- Andrews, J.L.; Li, M.W.; Minihan, S.; Songco, A.; Fox, E.; Ladouceur, C.D.; Mewton, L.; Moulds, M.; Pfeifer, J.H.; Van Harmelen, A.L.; et al. The effect of intolerance of uncertainty on anxiety and depression, and their symptom networks, during the COVID-19 pandemic. BMC Psychiatry 2023, 23, 261. [Google Scholar]
- Feng, T.W.; Ren, L.; Liu, C.; Li, K.L.; Wu, L.; Wei, X.Y.; Yuan, S.Q.; Cui, L.B.; Yang, X.; Li, D.Y.; et al. The relations between different components of intolerance of uncertainty and symptoms of depression during the COVID-19 pandemic: A network analysis. Front. Psychiatry 2022, 13, 993814. [Google Scholar] [PubMed]
- Sawyer, S.M.; Azzopardi, P.S.; Wickremarathne, D.; Patton, G.C. The age of adolescence... and young adulthood. Lancet Child Adolesc. Health 2018, 2, e6. [Google Scholar]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.W. The PHQ-9—Validity of a brief depression severity measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar]
- Wang, W.Z.; Bian, Q.; Zhao, Y.; Li, X.; Wang, W.W.; Du, J.; Zhang, G.F.; Zhou, Q.; Zhao, M. Reliability and validity of the Chinese version of the Patient Health Questionnaire (PHQ-9) in the general population. Gen. Hosp. Psychiatry 2014, 36, 539–544. [Google Scholar]
- Freeston, M.H.; Rheaume, J.; Letarte, H.; Dugas, M.J.; Ladouceur, R. Why Do People Worry. Personal. Individ. Differ. 1994, 17, 791–802. [Google Scholar]
- Carleton, R.N.; Norton, P.J.; Asmundson, G.J.G. Fearing the unknown: A short version of the Intolerance of Uncertainty Scale. J. Anxiety Disord. 2007, 21, 105–117. [Google Scholar]
- Zhang, Y.; Song, J.; Gao, Y.; Wu, S.; Song, L.; Miao, D. Reliability and Validity of the Intolerance of Uncertainty Scale-Short form in University Students. Chin. J. Clin. Psychol. 2017, 25, 285–288. [Google Scholar]
- Chen, J.H.; Chen, Z.H. Extended Bayesian information criteria for model selection with large model spaces. Biometrika 2008, 95, 759–771. [Google Scholar]
- Epskamp, S.; Borsboom, D.; Fried, E.I. Estimating psychological networks and their accuracy: A tutorial paper. Behav. Res. Methods 2018, 50, 195–212. [Google Scholar] [PubMed] [Green Version]
- Epskamp, S.; Cramer, A.O.J.; Waldorp, L.J.; Schmittmann, V.D.; Borsboom, D. qgraph: Network Visualizations of Relationships in Psychometric Data. J. Stat. Softw. 2012, 48, 1–18. [Google Scholar]
- Opsahl, T.; Agneessens, F.; Skvoretz, J. Node centrality in weighted networks: Generalizing degree and shortest paths. Soc. Netw. 2010, 32, 245–251. [Google Scholar]
- Robinaugh, D.J.; Millner, A.J.; McNally, R.J. Identifying Highly Influential Nodes in the Complicated Grief Network. J. Abnorm. Psychol. 2016, 125, 747–757. [Google Scholar] [PubMed] [Green Version]
- Haslbeck, J.M.B.; Waldorp, L.J. mgm: Estimating Time-Varying Mixed Graphical Models in High-Dimensional Data. J. Stat. Softw. 2020, 93, 1–46. [Google Scholar]
- Epskamp, S.; Waldorp, L.J.; Mõttus, R.; Borsboom, D. The Gaussian graphical model in cross-sectional and time-series data. Multivar. Behav. Res. 2018, 53, 453–480. [Google Scholar]
- Van Borkulo, C.D.; Van Bork, R.; Boschloo, L.; Kossakowski, J.J.; Tio, P.; Schoevers, R.A.; Borsboom, D.; Waldorp, L.J. Comparing Network Structures on Three Aspects: A Permutation Test. Psychol. Methods 2022. [Google Scholar]
- Manea, L.; Gilbody, S.; McMillan, D. Optimal cut-off score for diagnosing depression with the Patient Health Questionnaire (PHQ-9): A meta-analysis. Can. Med. Assoc. J. 2012, 184, E191–E196. [Google Scholar]
- Tao, Y.; Niu, H.; Hou, W.; Zhang, L.; Ying, R. Hopelessness during and after the COVID-19 pandemic lockdown among Chinese college students: A longitudinal network analysis. J. Clin. Psychol. 2023, 79, 748–761. [Google Scholar]
- Tao, Y.; Wang, S.; Tang, Q.; Ma, Z.; Zhang, L.; Liu, X. Centrality depression–anxiety symptoms linked to suicidal ideation among depressed college students—A network approach. PsyCh J. 2023, 1–11. [Google Scholar]
- Han, J.; Hao, Y.J.; Cui, N.X.; Wang, Z.H.; Lyu, P.; Yue, L. Parenting and parenting resources among Chinese parents with children under three years of age: Rural and urban differences. BMC Prim. Care 2023, 24, 38. [Google Scholar] [PubMed]
- Florean, I.S.; Dobrean, A.; Roman, G.D. Early Adolescents’ Perceptions of Parenting Practices and Mental Health Problems: A Network Approach. J. Fam. Psychol. 2022, 36, 438–448. [Google Scholar]
- Kapphahn, C.; Morreale, M.; Rickert, V.I.; Walker, L. Financing mental health services for adolescents: A background paper. J. Adolesc. Health 2006, 39, 318–327. [Google Scholar] [PubMed]
- Christie, D.; Viner, R. Adolescent development. BMJ 2005, 330, 301–304. [Google Scholar]
- Tao, Y.Q.; Hou, W.X.; Niu, H.Q.; Ma, Z.J.; Zheng, Z.Q.; Wang, S.J.; Liu, X.P.; Zhang, L. Comparing the centrality symptoms of major depressive disorder samples across junior high school students, senior high school students, college students and elderly adults during city lockdown of COVID-19 pandemic-A network analysis. J. Affect. Disord. 2023, 324, 190–198. [Google Scholar]
- Finazzi, M.E.; Mesquita, M.E.; Lopes, J.R.; Fu, L.; Oliveira, M.G.; Del Porto, J.A. Motor Activity and Depression Severity in Adolescent Outpatients. Neuropsychobiology 2010, 61, 33–40. [Google Scholar]
- Perzow, S.E.D.; Bray, B.C.; Wadsworth, M.E.; Young, J.F.; Hankin, B.L. Individual Differences in Adolescent Coping: Comparing a Community Sample and a Low-SES Sample to Understand Coping in Context. J. Youth Adolesc. 2021, 50, 693–710. [Google Scholar]
- Dai, W.; Meng, G.; Zheng, Y.; Li, Q.; Dai, B.; Liu, X. The Impact of Intolerance of Uncertainty on Negative Emotions in COVID-19: Mediation by Pandemic-Focused Time and Moderation by Perceived Efficacy. Int. J. Environ. Res. Public Health 2021, 18, 4189. [Google Scholar]
- Chang, H.; Dong, X.-Y.; MacPhail, F. Labor migration and time use patterns of the left-behind children and elderly in rural China. World Dev. 2011, 39, 2199–2210. [Google Scholar]
- Wang, J.Y.; Zou, J.J.; Luo, J.; Liu, H.M.; Yang, Q.P.; Ouyang, Y.F.; Hu, M.; Lin, Q. Mental health symptoms among rural adolescents with different parental migration experiences: A cross-sectional study in China. Psychiatry Res. 2019, 279, 222–230. [Google Scholar] [PubMed]
- Wang, L.; Zheng, L. Family Care and Early Childhood Development: Evidence from China’s Four Rural Subpopulations; REAP Working Paper: Stanford, CA, USA, 2019. [Google Scholar]
- Wang, H.X.; Chen, J.Q.; Zhao, X.X.; Feng, Y.A.; Song, Y. Physical Violence against Children by Parents among Primary School Students from a Rural Area in Shandong Province, China. Soc. Work. Public Health 2021, 36, 392–404. [Google Scholar]
- Balan, R.; Dobrean, A.; Roman, G.D.; Balazsi, R. Indirect Effects of Parenting Practices on Internalizing Problems among Adolescents: The Role of Expressive Suppression. J. Child Fam. Stud. 2017, 26, 40–47. [Google Scholar]
- Rote, W.M.; Flak, S.R.; Ellison, C. “That’s Not What I Heard!”: Adolescent Internalizing, Negative Perceptions of Maternal Communication, and Felt Shame and Guilt. J. Youth Adolesc. 2021, 50, 1693–1708. [Google Scholar] [PubMed]
- Baumeister, R.F. Suicide as Escape from Self. Psychol. Rev. 1990, 97, 90–113. [Google Scholar]
- Yip, P.S.F.; Liu, K.Y.; Hu, J.P.; Song, X.M. Suicide rates in China during a decade of rapid social changes. Soc. Psychiatry Psychiatr. Epidemiol. 2005, 40, 792–798. [Google Scholar]
- Holder, M.K.; Blaustein, J.D. Puberty and adolescence as a time of vulnerability to stressors that alter neurobehavioral processes. Front. Neuroendocrinol. 2014, 35, 89–110. [Google Scholar]

| City (N = 439) | Rural (N = 1049) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Items | Node | M | SD | Skewness | Kurtosis | M | SD | Skewness | Kurtosis | t |
| PHQ1 | Anhedonia | 0.77 | 0.83 | 0.89 | 0.19 | 0.84 | 0.83 | 0.78 | 0.04 | −1.41 |
| PHQ2 | Sad Mood | 0.70 | 0.79 | 1.00 | 0.47 | 0.73 | 0.80 | 0.90 | 0.18 | −0.65 |
| PHQ3 | Sleep | 0.64 | 0.87 | 1.23 | 0.59 | 0.75 | 0.88 | 0.95 | −0.03 | −2.20 * |
| PHQ4 | Energy | 0.81 | 0.87 | 0.86 | −0.04 | 0.88 | 0.87 | 0.75 | −0.18 | −1.46 |
| PHQ5 | Appetite | 0.62 | 0.83 | 1.20 | 0.60 | 0.69 | 0.85 | 1.07 | 0.32 | −1.47 |
| PHQ6 | Guilt | 0.57 | 0.82 | 1.34 | 0.99 | 0.68 | 0.84 | 1.04 | 0.22 | −2.39 * |
| PHQ7 | Concentration | 0.71 | 0.87 | 1.00 | 0.03 | 0.82 | 0.90 | 0.87 | −0.14 | −2.30 * |
| PHQ8 | Motor | 0.49 | 0.76 | 1.48 | 1.48 | 0.61 | 0.82 | 1.22 | 0.69 | −2.61 ** |
| PHQ9 | Suicide | 0.27 | 0.61 | 2.51 | 6.24 | 0.40 | 0.73 | 1.81 | 2.46 | −3.30 ** |
| AA | Prospective anxiety | 2.54 | 0.79 | 0.36 | 0.10 | 2.54 | 0.83 | 0.56 | 0.28 | 0.05 |
| IA | Inhibitory anxiety | 2.41 | 0.82 | 0.50 | 0.07 | 2.40 | 0.86 | 0.70 | 0.35 | 0.03 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jing, Z.; Ding, F.; Sun, Y.; Zhang, S.; Li, N. Comparing Depression Prevalence and Associated Symptoms with Intolerance of Uncertainty among Chinese Urban and Rural Adolescents: A Network Analysis. Behav. Sci. 2023, 13, 662. https://doi.org/10.3390/bs13080662
Jing Z, Ding F, Sun Y, Zhang S, Li N. Comparing Depression Prevalence and Associated Symptoms with Intolerance of Uncertainty among Chinese Urban and Rural Adolescents: A Network Analysis. Behavioral Sciences. 2023; 13(8):662. https://doi.org/10.3390/bs13080662
Chicago/Turabian StyleJing, Zhi, Fengqin Ding, Yishu Sun, Sensen Zhang, and Ning Li. 2023. "Comparing Depression Prevalence and Associated Symptoms with Intolerance of Uncertainty among Chinese Urban and Rural Adolescents: A Network Analysis" Behavioral Sciences 13, no. 8: 662. https://doi.org/10.3390/bs13080662





