What Are the Economic Arguments for Mandating LGBT+ Health Training for Healthcare Providers? An Economic Evaluation of the Impacts of LGBT+ Health Training on Cervical Screening
Abstract
:1. Background
2. Materials and Methods
2.1. Target Population and Setting
2.2. Study Perspective
2.3. Intervention and Comparator
2.4. Model Parameters
2.5. Measure of Effectiveness
2.6. Measures of Costs
2.7. Model Design

2.8. Sensitivity Analyses
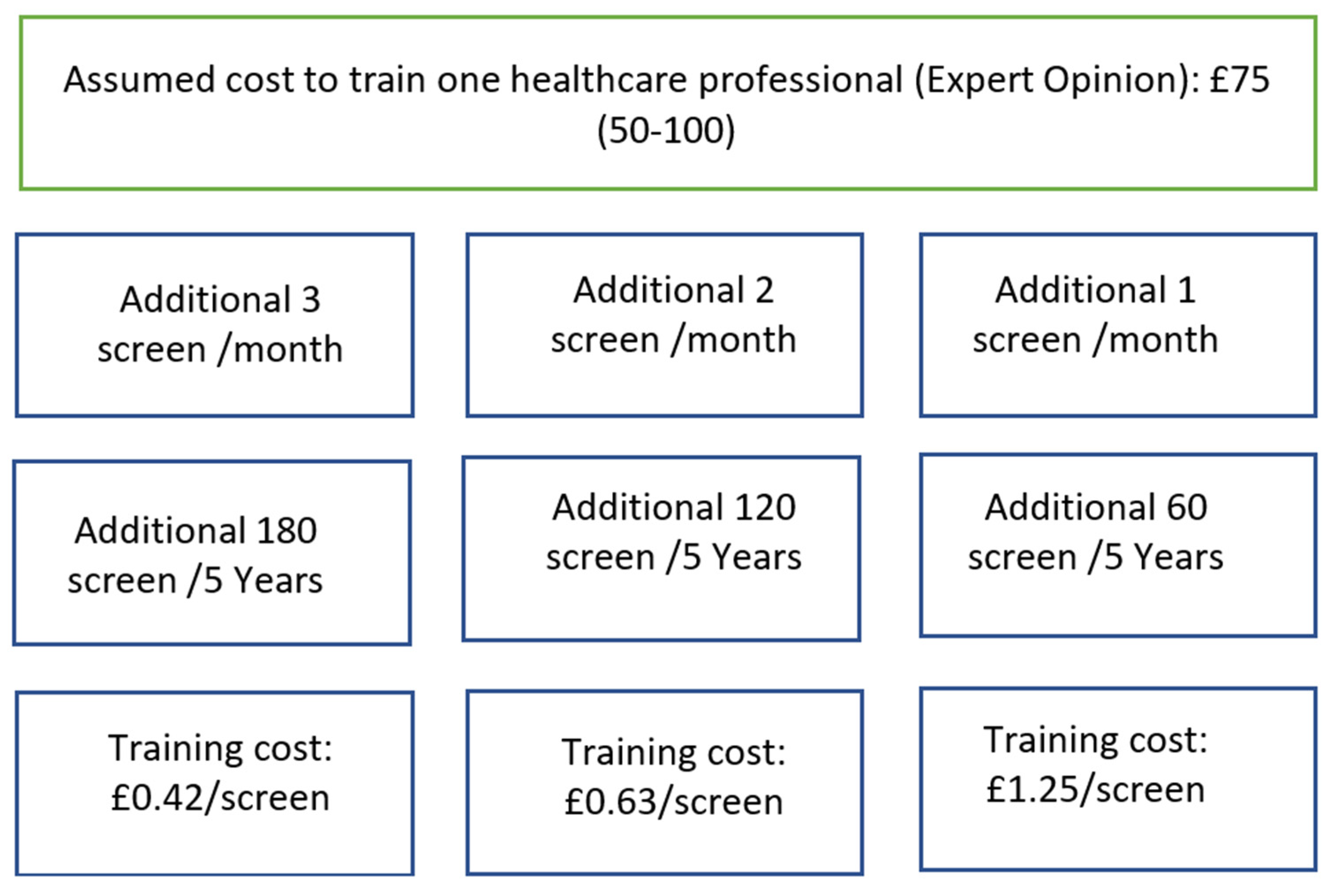
- Training costs: Where we vary the volume of the population being affected by training.
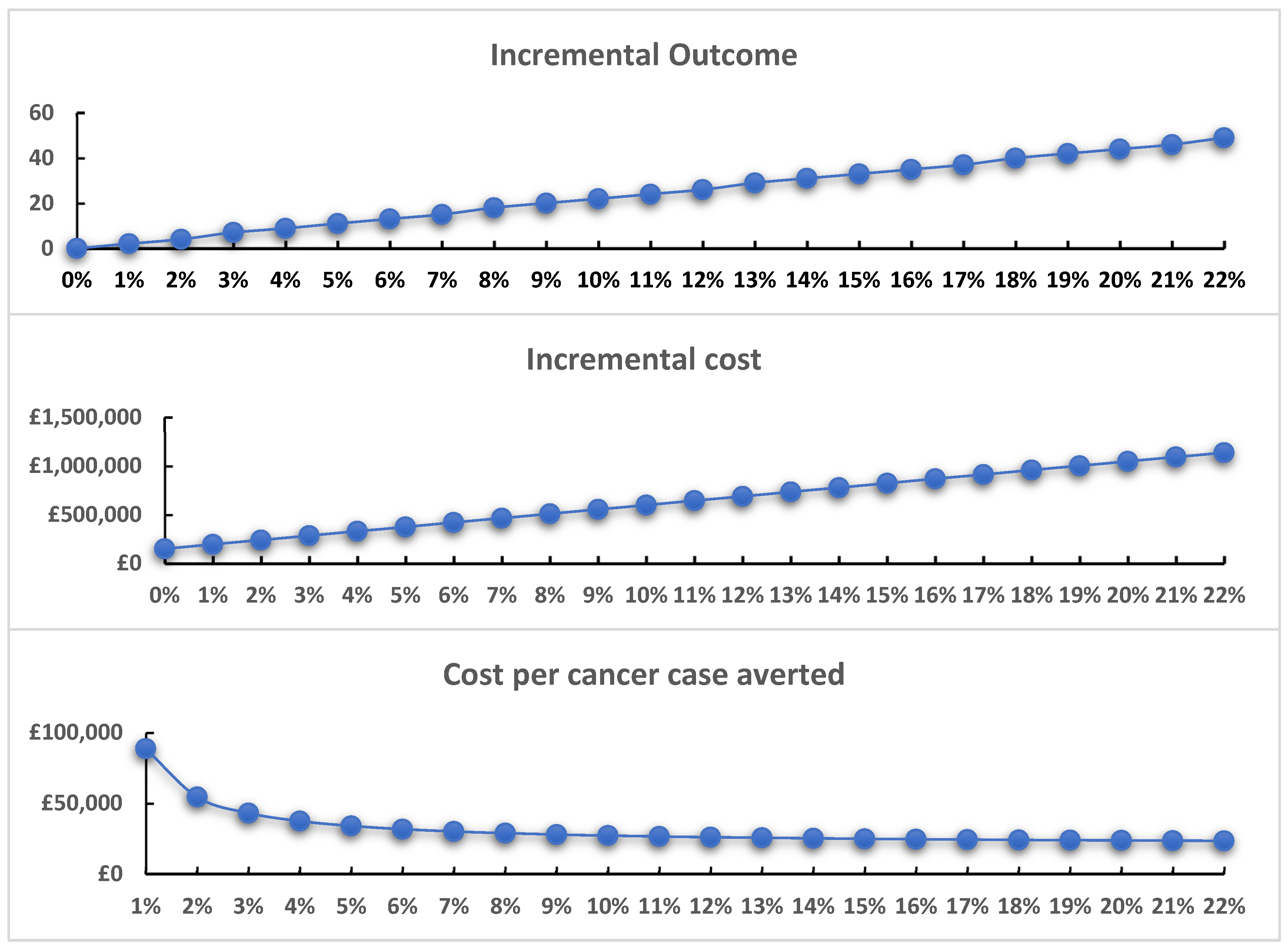
- Training effectiveness: Where we vary the effectiveness of the training.
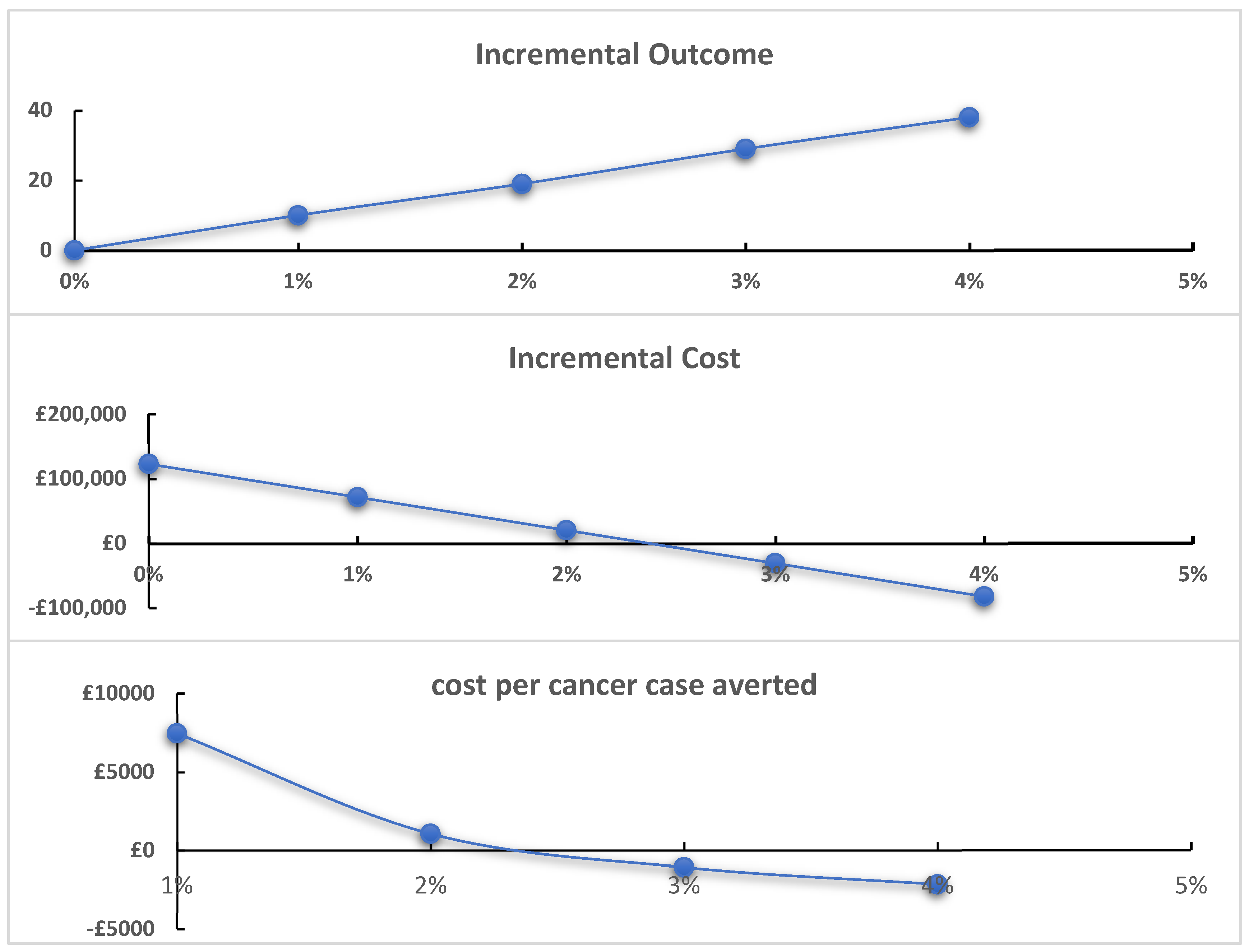
- Population covered: Where we vary the population age groups affected by training.
3. Results
3.1. Study Parameters
3.2. Sensitivity Analyses
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO. It’s Time to Build a Fairer, Healthier World for Everyone, Everywhere. Health Equity and Its Determinants. World Health Day. 2021. Available online: https://cdn.who.int/media/docs/default-source/world-health-day-2021/health-equity-and-its-determinants.pdf?sfvrsn=6c36f0a5_1&download=true (accessed on 1 May 2023).
- UK Government. Equality Act 2010. Available online: https://www.legislation.gov.uk/ukpga/2010/15/contents (accessed on 15 June 2023).
- Department of Health and Social Care. Introduction to the NHS Constitution. 2021. Available online: https://www.gov.uk/government/publications/the-nhs-constitution-for-england/the-nhs-constitution-for-england (accessed on 15 June 2023).
- Light, B.; Ormandy, P. Lesbian, Gay and Bisexual Women in the North West: A Multi-Method Study of Cervical Screening Attitudes, Experiences and Uptake; University of Salford: Salford, UK, 2011. [Google Scholar]
- Saunders, C.L.; Massou, E.; Waller, J.; Meads, C.; Marlow, L.A.V.; Usher-Smith, J.A. Cervical screening attendance and cervical cancer risk among women who have sex with women. J. Med. Screen. 2021, 28, 349–356. [Google Scholar] [CrossRef] [PubMed]
- Mercer, C.H.; Bailey, J.V.; Johnson, A.M.; Erens, B.; Wellings, K.; Fenton, K.A.; Copas, A.J. Women who report having sex with women: British national probability data on prevalence, sexual behaviors, and health outcomes. Am. J. Public Health 2007, 97, 1126–1133. [Google Scholar] [CrossRef] [PubMed]
- Hodson, K.; Meads, C.; Bewley, S. Lesbian and bisexual women’s likelihood of becoming pregnant: A systematic review and meta-analysis. BJOG Int. J. Obstet. Gynaecol. 2017, 124, 393–402. [Google Scholar] [CrossRef] [PubMed]
- Robinson, K.; Galloway, K.Y.; Bewley, S.; Meads, C. Lesbian and bisexual women’s gynaecological conditions: A systematic review and exploratory meta-analysis. BJOG Int. J. Obstet. Gynaecol. 2017, 124, 381–392. [Google Scholar] [CrossRef] [PubMed]
- Gulliford, M.; Figueroa-Munoz, J.; Morgan, M.; Hughes, D.; Gibson, B.; Beech, R.; Hudson, M. What does ‘access to health care’ mean? J. Health Serv. Res. Policy 2002, 7, 186–188. [Google Scholar] [CrossRef] [PubMed]
- McIntyre, D.; Thiede, M.; Birch, S. Access as a policy-relevant concept in low-and middle-income countries. Health Econ. Policy Law 2009, 4, 179–193. [Google Scholar] [CrossRef] [PubMed]
- Macredie, S. The Challenge for Change. Health Needs of lesbian, Gay and Bisexual People in Bradford and District; Equity Partnership: Bradford, UK, 2010. [Google Scholar]
- Meads, C.; Hunt, R.; Martin, A.; Varney, J. A systematic review of sexual minority women’s experiences of health care in the UK. Int. J. Environ. Res. Public Health 2019, 16, 3032. [Google Scholar] [CrossRef] [PubMed]
- Morrison, C.M.C. LGBTQ+ Health Training and Education Research: Unpublished Report to Dr Michael Brady; NHS England, Anglia Ruskin University: Cambridge, UK, 2023. [Google Scholar]
- Brown, M.; Mccann, E.; McCormick, F. Making the Invisible Visible: The Inclusion of LGBTQ+ Health Needs and Concerns within Nursing and Midwifery Pre-Registration Programmes: Making the Invisible Visible; Queen’s University Belfast: Belfast, Ireland; Trinity College Dublin: Dublin, Ireland, 2021. [Google Scholar]
- Sekoni, A.O.; Gale, N.K.; Manga-Atangana, B.; Bhadhuri, A.; Jolly, K. The effects of educational curricula and training on LGBT-specific health issues for healthcare students and professionals: A mixed-method systematic review. J. Int. AIDS Soc. 2017, 20, 21624. [Google Scholar] [CrossRef] [PubMed]
- Hunt, R.; Bates, C.; Walker, S.; Grierson, J.; Redsell, S.; Meads, C. A systematic review of UK educational and training materials aimed at health and social care staff about providing appropriate services for LGBT+ people. Int. J. Environ. Res. Public Health 2019, 16, 4976. [Google Scholar] [CrossRef] [PubMed]
- Women and Equalities Select Committee. Health and Social Care in the LGBT Communities; UK Government: London, UK, 2019.
- Husereau, D.; Drummond, M.; Petrou, S.; Carswell, C.; Moher, D.; Greenberg, D.; Augustovski, F.; Briggs, A.H.; Mauskopf, J.; Loder, E. Consolidated health economic evaluation reporting standards (CHEERS)—Explanation and elaboration: A report of the ISPOR health economic evaluation publication guidelines good reporting practices task force. Value Health 2013, 16, 231–250. [Google Scholar] [CrossRef] [PubMed]
- NHSCSP. Cervical Screening: Programme Overview. Available online: https://www.gov.uk/guidance/cervical-screening-programme-overview (accessed on 6 March 2023).
- NICE. NICE Health Technology Evaluations: The Manual, Process and Methods. 31 January 2022. Available online: www.nice.org.uk/process/pmg36 (accessed on 1 May 2023).
- Roberts, M.; Russell, L.B.; Paltiel, A.D.; Chambers, M.; McEwan, P.; Krahn, M. Conceptualizing a Model: A Report of the ISPOR-SMDM Modeling Good Research Practices Task Force–2. Med. Decis. Mak. 2012, 32, 678–689. [Google Scholar] [CrossRef] [PubMed]
- Bains, I.; Choi, Y.H.; Soldan, K.; Jit, M. Clinical impact and cost-effectiveness of primary cytology versus human papillomavirus testing for cervical cancer screening in England. Int. J. Gynecol. Cancer 2019, 29, 669–675. [Google Scholar] [CrossRef] [PubMed]
- Landy, R.; Pesola, F.; Castañón, A.; Sasieni, P. Impact of cervical screening on cervical cancer mortality: Estimation using stage-specific results from a nested case–control study. Br. J. Cancer 2016, 115, 1140–1146. [Google Scholar] [CrossRef] [PubMed]
- Sun, L.; Patel, S.; Fiorina, C.; Glass, A.; Rochaix, L.; The CBIG-SCREEN Consortium; Foss, A.M.; Legood, R. A systematic review of the cost-effectiveness of interventions to increase cervical cancer screening among underserved women in Europe. Eur. J. Health Econ. 2023, 1–16. [Google Scholar] [CrossRef] [PubMed]
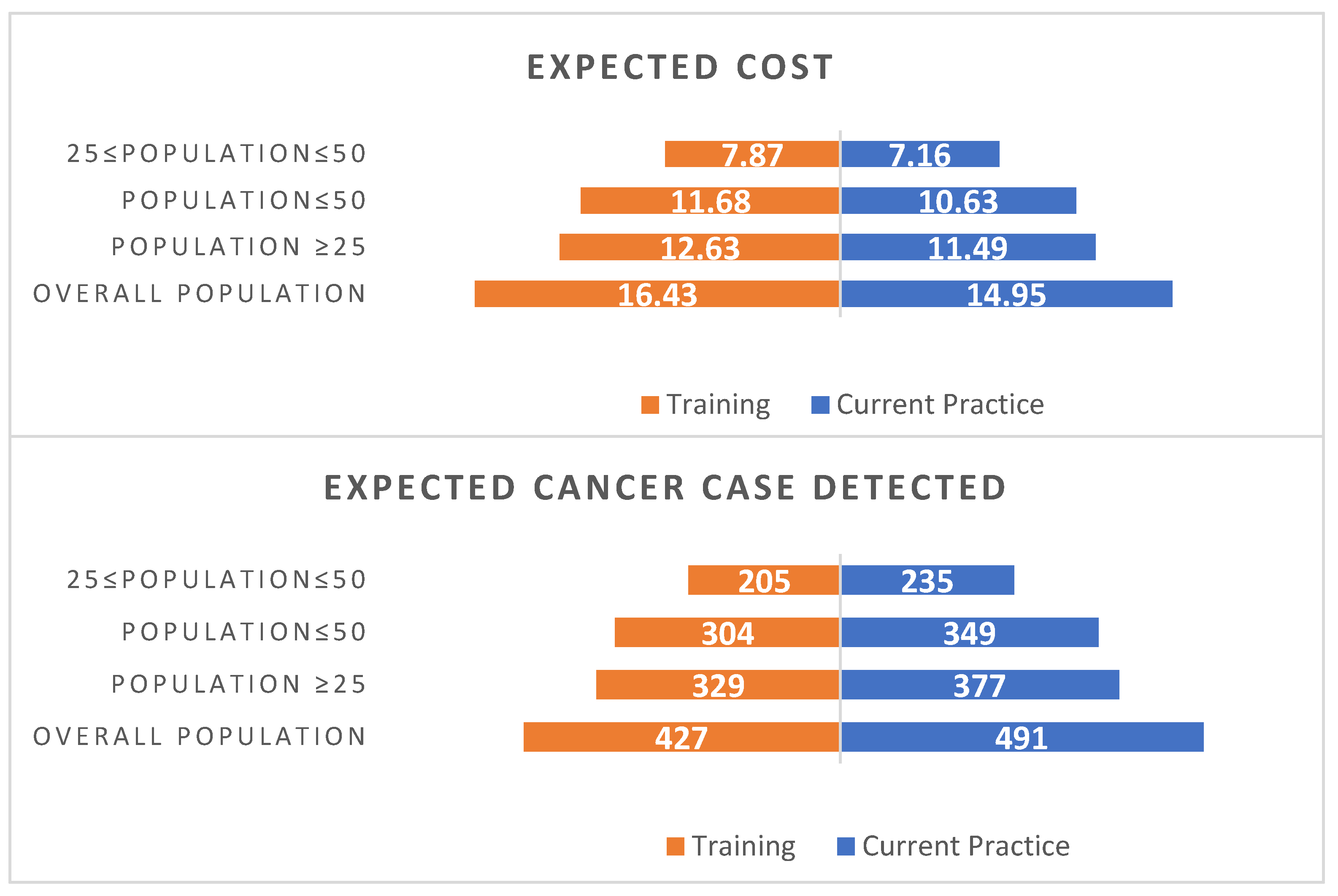
| Sexual Identity | Overall Population | 25 ≤ Population ≤ 50 | Population ≤ 50 | Population ≥ 25 |
|---|---|---|---|---|
| Lesbian | 311 | 149 | 221 | 239 |
| Bisexual | 450 | 144 | 399 | 195 |
| Heterosexual or straight | 25,680 | 10,170 | 13,059 | 22,791 |
| Decision problem | What are the benefits and costs of introducing formal education training in LGB health issues for healthcare providers? Cervical smears are used as an exemplar case for measuring impacts |
| Intervention | Mandated training to healthcare professional about LGB issues |
| Comparator | The comparator is the current standard of care in the United Kingdom |
| Population | Population groups of persons identifying as lesbian and bisexual in UK |
| Model type | Decision Tree |
| Software | TreeAge and Excel |
| Time horizon | 5 years’ time frame (this time frame comprises the maximum amount of time that each person is eligible for screening) |
| Study perspective | National Health Service (NHS) (health system perspective) |
| Cost | National currency (£) at 2022 prices * |
| Consequences | Cancer case averted |
| Uncertainty | Deterministic: one-way sensitivity analysis/scenario analysis |
| Parameters | Current Practice | Training | Source |
|---|---|---|---|
| Probability of smear uptake in lesbians | 61.50% | 75.03% * | [5] |
| Probability of CC in lesbians who do smear screening | 0.10% | 0.10% | [5] |
| Probability of CC in lesbians who do not do smear screening | 0.25% | 0.25% | [23] |
| Probability of smear uptake in bisexuals | 81.90% | 84.6% ** | [5] |
| Probability of CC in bisexuals who do smear screening | 0.40% | 0.40% | [5] |
| Probability of CC in bisexuals who do not do smear screening | 1.01% | 1.01% | [23] |
| Probability of CC at early stage in population who do smear screening | 83.5% | 83.5% | [23] |
| Probability of CC at early stage in population who do not do smear screening | 64.8% | 64.8% | [23] |
| Cost of screening *** | [22] | ||
| Sample collection | £18.22 (14.88, 22.17) | ||
| HPV test per sample * | £11.60 (8.61, 15.51) | ||
| Cytology test per slide * | £21.60 (17.79, 26.21) | ||
| Total | £51.43 | ||
| Cost of training | £ (50–100) **** | Assumption | |
| Cost of treatment | [22] | ||
| Stage I | £5498 (4886, 6137) | ||
| Stage II | £24,642 (21,337, 27,981) | ||
| Stage III | £24,265 (20,993, 27,981) | ||
| Stage IV | £20,614 (17,798, 23,814) | ||
| Average cost of stage II, III, and IV | £23,174 (16,253, 21,478) |
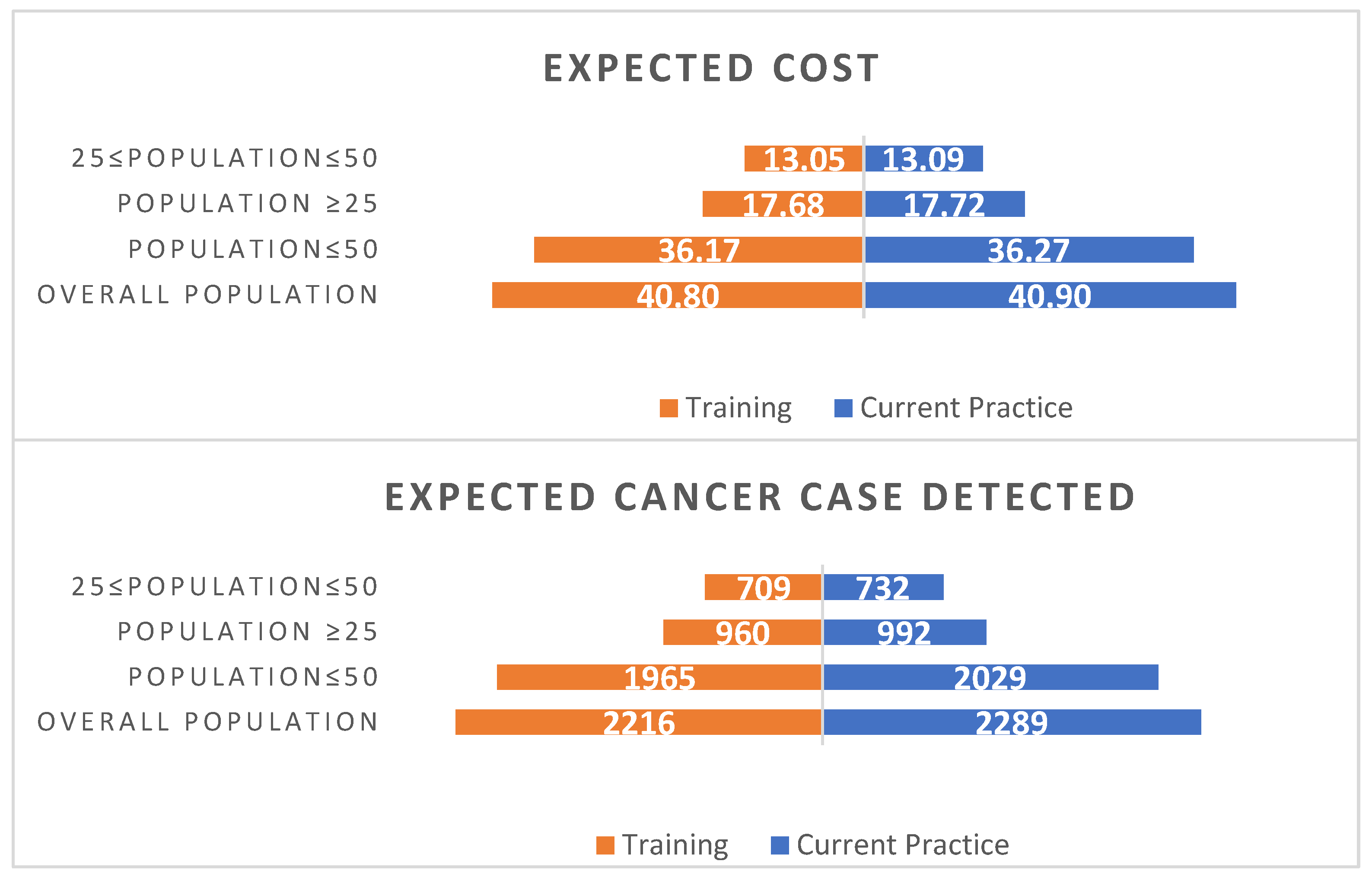
| Current Practice | Training | |||
|---|---|---|---|---|
| Lesbian Population | ||||
| Expected Cost (£m) | Expected Outcome (Cancer Detected) | Expected Cost (£m) | Expected Outcome (Cancer Detected) | |
| Screened | 8.80 | 147 | 10.84 | 179 |
| Not screened | 2.70 | 230 | 1.79 | 149 |
| Total | 11.49 | 377 | 12.63 | 329 |
| Incremental cost | 1.14 | |||
| Incremental outcome (cancers detected) | −49 | |||
| Incremental outcome (cancers averted) * | 49 | |||
| Cost per case averted | 23,467 | |||
| Bisexual Female Population | ||||
| Screened | 13.59 | 639 | 14.14 | 660 |
| Not screened | 4.14 | 353 | 3.54 | 300 |
| Total | 17.72 | 992 | 17.68 | 960 |
| Incremental cost | −0.05 | |||
| Incremental outcome (cancers detected) | −32 | |||
| Incremental outcome (cancers averted) * | 32 | |||
| Cost per case averted | −1463 | |||
| Training Cost | Current Practice | Training | Incremental Cost | Incremental Outcome (Case Detected) | Incremental Outcome (Case Averted) | ICER | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Screened | Not Screened | Total | Screened | Not Screened | Total | |||||
| Lesbian Population | ||||||||||
| 0.42 | 8.796 | 2.696 | 11.492 | 10.806 | 1.774 | 12.580 | 1.088 | −49 | 49 | £22,432 |
| 0.63 | 8.796 | 2.696 | 11.492 | 10.844 | 1.786 | 12.630 | 1.138 | −49 | 49 | £23,467 |
| 1.25 | 8.796 | 2.696 | 11.492 | 10.955 | 1.823 | 12.778 | 1.286 | −49 | 49 | £26,522 |
| Bisexual Population | ||||||||||
| 0.42 | 13.588 | 4.136 | 17.725 | 14.106 | 3.532 | 17.638 | −0.087 | −32 | 32 | −£2759 |
| 0.63 | 13.588 | 4.136 | 17.725 | 14.140 | 3.538 | 17.679 | −0.046 | −32 | 32 | −£1463 |
| 1.25 | 13.588 | 4.136 | 17.725 | 14.243 | 3.557 | 17.800 | 0.075 | −32 | 32 | £2364 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bashir, S.; Whittaker, W.; Meads, C. What Are the Economic Arguments for Mandating LGBT+ Health Training for Healthcare Providers? An Economic Evaluation of the Impacts of LGBT+ Health Training on Cervical Screening. Behav. Sci. 2024, 14, 260. https://doi.org/10.3390/bs14030260
Bashir S, Whittaker W, Meads C. What Are the Economic Arguments for Mandating LGBT+ Health Training for Healthcare Providers? An Economic Evaluation of the Impacts of LGBT+ Health Training on Cervical Screening. Behavioral Sciences. 2024; 14(3):260. https://doi.org/10.3390/bs14030260
Chicago/Turabian StyleBashir, Saima, William Whittaker, and Catherine Meads. 2024. "What Are the Economic Arguments for Mandating LGBT+ Health Training for Healthcare Providers? An Economic Evaluation of the Impacts of LGBT+ Health Training on Cervical Screening" Behavioral Sciences 14, no. 3: 260. https://doi.org/10.3390/bs14030260
APA StyleBashir, S., Whittaker, W., & Meads, C. (2024). What Are the Economic Arguments for Mandating LGBT+ Health Training for Healthcare Providers? An Economic Evaluation of the Impacts of LGBT+ Health Training on Cervical Screening. Behavioral Sciences, 14(3), 260. https://doi.org/10.3390/bs14030260





