How Mental Health and Suicidality Changed during the COVID-19 Pandemic: A Longitudinal Study in the General and Psychiatric Population Illustrating Risk and Protective Factors
Abstract
1. Introduction
2. Method
2.1. Participants
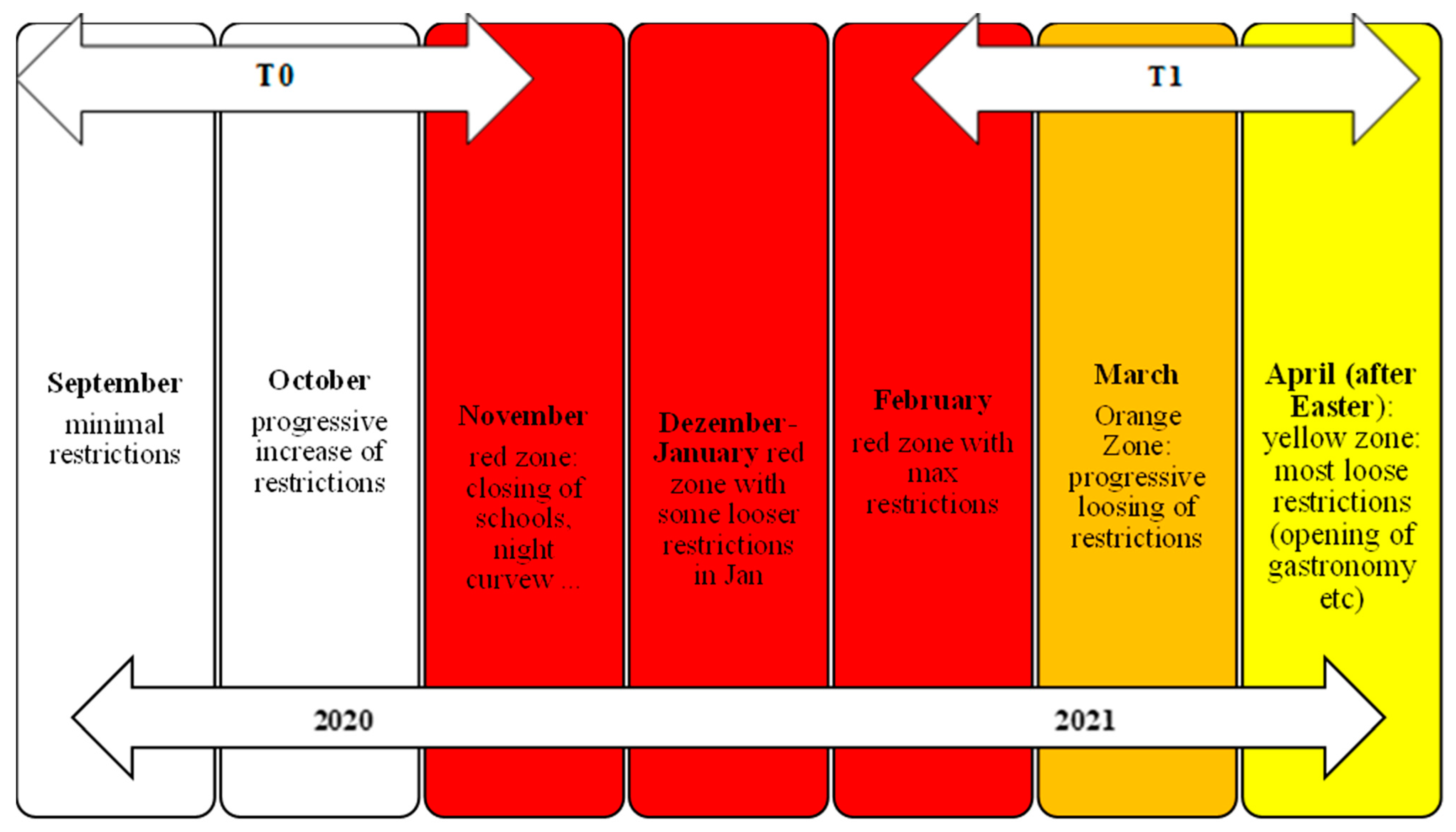
2.2. Procedure
2.3. Measures
2.4. Statistical Analysis
3. Results
3.1. Effect of Time and Group on Psychological Distress and Suicidal Ideation
3.2. Predictors of Psychological Distress and Suicidal Ideation in the Post-Test
3.3. Predictors of Active Suicidal Ideation in the Post-Test
3.4. Predictors of Passive Suicidal Ideation
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Richter, D.; Riedel-Heller, S.; Zürcher, S.J. Mental health problems in the general population during and after the first lockdown phase due to the SARS-CoV-2 pandemic: Rapid review of multi-wave studies. Epidemiol. Psychiatr. Sci. 2021, 30, e27. [Google Scholar] [CrossRef] [PubMed]
- Robinson, E.; Daly, M. Explaining the rise and fall of psychological distress during the COVID-19 crisis in the United States: Longitudinal evidence from the Understanding America Study. Br. J. Health Psychol. 2021, 26, 570–587. [Google Scholar] [CrossRef] [PubMed]
- Benatov, J.; Ochnik, D.; Rogowska, A.M.; Arzenšek, A.; Bitenc, U.M. Prevalence and Sociodemographic Predictors of Mental Health in a Representative Sample of Young Adults from Germany, Israel, Poland, and Slovenia: A Longitudinal Study during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2022, 19, 1334. [Google Scholar] [CrossRef] [PubMed]
- Gullo, S.; Misici, I.; Teti, A.; Liuzzi, M.; Chiara, E. Going through the lockdown: A longitudinal study on the psy-chological consequences of the coronavirus pandemic. Res. Psychother. Psychopathol. Process Outcome 2020, 23, 494. [Google Scholar] [CrossRef] [PubMed]
- Brosch, K.; Meller, T.; Pfarr, J.-K.; Stein, F.; Schmitt, S.; Ringwald, K.G.; Waltemate, L.; Lemke, H.; Thiel, K.; Schrammen, E.; et al. Which traits predict elevated distress during the COVID-19 pandemic? Results from a large, longitudinal cohort study with psychiatric patients and healthy controls. J. Affect. Disord. 2022, 297, 18–25. [Google Scholar] [CrossRef] [PubMed]
- Picó-Pérez, M.; Ferreira, S.; Couto, B.; Raposo-Lima, C.; Machado-Sousa, M.; Morgado, P. Sociodemographic and lifestyle predictors of mental health adaptability during COVID-19 compulsory confinement: A longitudinal study in the Portuguese population. J. Affect. Disord. 2021, 295, 797–803. [Google Scholar] [CrossRef] [PubMed]
- Hofer, A.; Kachel, T.; Plattner, B.; Chernova, A.; Conca, A.; Fronthaler, M.; Frajo-Apor, B. Mental health in individuals with severe mental disorders during the covid-19 pandemic: A longitudinal investigation. Schizophrenia 2022, 8, 17. [Google Scholar] [CrossRef] [PubMed]
- Hamza, C.A.; Ewing, L.; Heath, N.L.; Goldstein, A.L. When social isolation is nothing new: A longitudinal study on psychological distress during COVID-19 among university students with and without preexisting mental health concerns. Can. Psychol./Psychol. Can. 2021, 62, 20. [Google Scholar] [CrossRef]
- Elbogen, E.B.; Lanier, M.; Blakey, S.M.; Wagner, H.R.; Tsai, J. Suicidal ideation and thoughts of self-harm during the COVID-19 pandemic: The role of COVID-19-related stress, social isolation, and financial strain. Depress. Anxiety 2021, 38, 739–748. [Google Scholar] [CrossRef]
- Knipe, D.; John, A.; Padmanathan, P.; Eyles, E.; Dekel, D.; Higgins, J.P.T.; Bantjes, J.; Dandona, R.; Macleod-Hall, C.; McGuinness, L.A.; et al. Suicide and self-harm in low- and middle-income countries during the COVID-19 pandemic: A systematic review. PLOS Glob. Public Health 2022, 2, e0000282. [Google Scholar] [CrossRef]
- Liem, A.; Prawira, B.; Magdalena, S.; Siandita, M.J.; Hudiyana, J. Predicting self-harm and suicide ideation during the COVID-19 pandemic in Indonesia: A nationwide survey report. BMC Psychiatry 2022, 22, 304. [Google Scholar] [CrossRef] [PubMed]
- Pirkis, J.; John, A.; Shin, S.; DelPozo-Banos, M.; Arya, V.; Analuisa-Aguilar, P.; Appleby, L.; Arensman, E.; Bantjes, J.; Baran, A.; et al. Suicide trends in the early months of the COVID-19 pandemic: An interrupted time-series analysis of preliminary data from 21 countries. Lancet Psychiatry 2021, 8, 579–588. [Google Scholar] [CrossRef] [PubMed]
- Iob, E.; Steptoe, A.; Fancourt, D. Abuse, self-harm and suicidal ideation in the UK during the COVID-19 pandemic. Br. J. Psychiatry 2020, 217, 543–546. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, R.C.; Wetherall, K.; Cleare, S.; McClelland, H.; Melson, A.J.; Niedzwiedz, C.L.; O’Carroll, R.E.; O’Connor, D.B.; Platt, S.; Scowcroft, E.; et al. Mental health and well-being during the COVID-19 pandemic: Longitudinal analyses of adults in the UK COVID-19 Mental Health & Wellbeing study. Br. J. Psychiatry 2021, 218, 326–333. [Google Scholar] [PubMed]
- Batterham, P.J.; Calear, A.L.; Shou, Y.; Farrer, L.M.; Gulliver, A.; McCallum, S.M.; Dawel, A. Effects of the COVID-19 pandemic on suicidal ideation in a representative Australian population sample–Longitudinal cohort study. J. Affect. Disord. 2022, 300, 385–391. [Google Scholar] [CrossRef] [PubMed]
- Hyland, P.; Rochford, S.; Munnelly, A.; Dodd, P.; Fox, R.; Vallières, F.; Murphy, J. Predicting risk along the sui-cidality continuum: A longitudinal, nationally representative study of the Irish population during the COVID-19 pandemic. Suicide Life-Threat. Behav. 2022, 52, 83–98. [Google Scholar] [CrossRef] [PubMed]
- Antonelli-Salgado, T.; Monteiro, G.M.C.; Marcon, G.; Roza, T.H.; Zimerman, A.; Hoffmann, M.S.; Cao, B.; Hauck, S.; Brunoni, A.R.; Passos, I.C. Loneliness, but not social distancing, is associated with the incidence of suicidal ideation during the COVID-19 outbreak: A longitudinal study. J. Affect. Disord. 2021, 290, 52–60. [Google Scholar] [CrossRef] [PubMed]
- Latikka, R.; Koivula, A.; Oksa, R.; Savela, N.; Oksanen, A. Loneliness and psychological distress before and during the COVID-19 pandemic: Relationships with social media identity bubbles. Soc. Sci. Med. 2022, 293, 114674. [Google Scholar] [CrossRef]
- Lommer, K.; Schurr, T.; Frajo-Apor, B.; Plattner, B.; Chernova, A.; Conca, A.; Fronthaler, M.; Haring, C.; Holzner, B.; Macina, C.; et al. Addiction in the time of COVID-19: Longitudinal course of substance use, psychological distress, and loneliness among a transnational Tyrolean sample with substance use disorders. Front. Psychiatry 2022, 13, 918465. [Google Scholar] [CrossRef]
- Groarke, J.M.; McGlinchey, E.; McKenna-Plumley, P.E.; Berry, E.; Graham-Wisener, L.; Armour, C. Examining temporal interactions between loneliness and depressive symptoms and the mediating role of emotion regulation difficulties among UK residents during the COVID-19 lockdown: Longitudinal results from the COVID-19 psychological wellbeing study. J. Affect. Disord. 2021, 285, 1–9. [Google Scholar] [CrossRef]
- Song, S.; Yang, X.; Yang, H.; Zhou, P.; Ma, H.; Teng, C.; Chen, H.; Ou, H.; Li, J.; Mathews, C.A.; et al. Psychological Resilience as a Protective Factor for Depression and Anxiety Among the Public during the Outbreak of COVID-19. Front. Psychol. 2021, 11, 618509. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Bi, K.; Sun, P.; Bonanno, G.A. Psychopathology and resilience following strict COVID-19 lockdowns in Hubei, China: Examining person-and context-level predictors for longitudinal trajectories. Am. Psychol. 2022, 77, 262. [Google Scholar] [CrossRef] [PubMed]
- Chernova, A.; Frajo-Apor, B.; Pardeller, S.; Tutzer, F.; Plattner, B.; Haring, C.; Holzner, B.; Kemmler, G.; Marksteiner, J.; Miller, C.; et al. The Mediating Role of Resilience and Extraversion on Psychological Distress and Loneliness Among the General Population of Tyrol, Austria Between the First and the Second Wave of the COVID-19 Pandemic. Front. Psychiatry 2021, 12, 766261. [Google Scholar] [CrossRef] [PubMed]
- Schmit, A.; Schurr, T.; Frajo-Apor, B.; Pardeller, S.; Plattner, B.; Tutzer, F.; Conca, A.; Fronthaler, M.; Haring, C.; Holzner, B.; et al. Long-term impact of resilience and extraversion on psychological distress during the COVID-19 pandemic: A longitudinal investigation among individuals with and without mental health disorders. Front. Psychiatry 2024, 15, 1304491. [Google Scholar] [CrossRef] [PubMed]
- Tutzer, F.; Frajo-Apor, B.; Pardeller, S.; Plattner, B.; Chernova, A.; Haring, C.; Holzner, B.; Kemmler, G.; Marksteiner, J.; Miller, C.; et al. The Impact of Resilience and Extraversion on Psychological Distress, Loneliness, and Boredom During the COVID-19 Pandemic: A Follow-Up Study Among the General Population of Tyrol, Austria. Front. Psychiatry 2021, 12, 777527. [Google Scholar] [CrossRef] [PubMed]
- Vannini, P.; Gagliardi, G.P.; Kuppe, M.; Dossett, M.L.; Donovan, N.J.; Gatchel, J.R.; Quiroz, Y.T.; Premnath, P.Y.; Amariglio, R.; Sperling, R.A.; et al. Stress, resilience, and coping strategies in a sample of community-dwelling older adults during COVID-19. J. Psychiatr. Res. 2021, 138, 176–185. [Google Scholar] [CrossRef]
- Zhang, J.; Yang, Z.; Wang, X.; Li, J.; Dong, L.; Wang, F.; Zhang, J. The relationship between resilience, anxiety and depression among patients with mild symptoms of COVID-19 in China: A cross-sectional study. J. Clin. Nurs. 2020, 29, 4020–4029. [Google Scholar] [CrossRef] [PubMed]
- Davis, E.B.; McElroy-Heltzel, S.E.; Lemke, A.W.; Cowden, R.G.; VanderWeele, T.J.; Worthington, E.L., Jr.; Glowiak, K.J.; Shannonhouse, L.R.; Davis, D.E.; Hook, J.N.; et al. Psychological and spiritual outcomes during the COVID-19 pandemic: A prospective longitudinal study of adults with chronic disease. Health Psychol. 2021, 40, 347. [Google Scholar] [CrossRef] [PubMed]
- Havnen, A.; Anyan, F.; Hjemdal, O.; Solem, S.; Gurigard Riksfjord, M.; Hagen, K. Resilience Moderates Negative Outcome from Stress During the COVID-19 Pandemic: A Moderated-Mediation Approach. Int. J. Environ. Res. Public Health 2020, 17, 6461. [Google Scholar] [CrossRef]
- Aten, J.D.; Smith, W.R.; Davis, E.B.; Van Tongeren, D.R.; Hook, J.N.; Davis, D.E.; Shannonhouse, L.; DeBlaere, C.; Ranter, J.; O'Grady, K.; et al. The psychological study of religion and spirituality in a disaster context: A systematic review. Psychol. Trauma Theory Res. Pract. Policy 2019, 11, 597–613. [Google Scholar] [CrossRef]
- Mizuno, Y.; Hofer, A.; Frajo-Apor, B.; Wartelsteiner, F.; Kemmler, G.; Pardeller, S.; Suzuki, T.; Mimura, M.; Fleischhacker, W.W.; Uchida, H. Religiosity and psychological resilience in patients with schizophrenia and bipolar disorder: An international cross-sectional study. Acta Psychiatr. Scand. 2018, 137, 316–327. [Google Scholar] [CrossRef]
- Roberto, A.; Sellon, A.; Cherry, S.T.; Hunter-Jones, J.; Winslow, H. Impact of spirituality on resilience and coping during the COVID-19 crisis: A mixed-method approach investigating the impact on women. Health Care Women Int. 2020, 41, 1313–1334. [Google Scholar] [CrossRef]
- Büssing, A.; Baumann, K.; Surzykiewicz, J. Loss of Faith and Decrease in Trust in a Higher Source during COVID-19 in Germany. J. Relig. Health 2022, 61, 741–766. [Google Scholar] [CrossRef]
- Papadopoulos, I.; Lazzarino, R.; Wright, S.; Ellis Logan, P.; Koulouglioti, C. Spiritual support during COVID-19 in England: A scoping study of online sources. J. Relig. Health 2021, 60, 2209–2230. [Google Scholar] [CrossRef]
- González-Sanguino, C.; Ausín, B.; Castellanos, M.Á.; Saiz, J.; López-Gómez, A.; Ugidos, C.; Muñoz, M. Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID-19) in Spain. Brain Behav. Immun. 2020, 87, 172–176. [Google Scholar] [CrossRef] [PubMed]
- Tutzer, F.; Schurr, T.; Frajo-Apor, B.; Pardeller, S.; Plattner, B.; Schmit, A.; Conca, A.; Fronthaler, M.; Haring, C.; Holzner, B.; et al. Relevance of spirituality and perceived social support to mental health of people with pre-existing mental health disorders during the COVID-19 pandemic: A longitudinal investigation. Chest 2023, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Holzner, B.; Giesinger, J.M.; Pinggera, J.; Zugal, S.; Schöpf, F.; Oberguggenberger, A.S.; Gamper, E.M.; Zabernigg, A.; Weber, B.; Rumpold, G. The Computer-based Health Evaluation Software (CHES): A software for electronic patient-reported outcome monitoring. BMC Med. Inform. Decis. Mak. 2012, 12, 1–11. [Google Scholar] [CrossRef]
- Autonome Provinz Bozen. Sicherheit und Zivilschutz. 2024. Available online: https://www.provinz.bz.it/sicherheit-zivilschutz/zivilschutz/downloads-dokumente-zum-herunterladen.asp (accessed on 19 April 2024).
- Franke, G.H. BSCL: Brief-Symptom-Checklist: Manual; Hogrefe: Göttingen, Germany, 2017. [Google Scholar]
- Hughes, M.E.; Waite, L.J.; Hawkley, L.C.; Cacioppo, J.T. A short scale for measuring loneliness in large surveys: Results from two population-based studies. Res. Aging 2004, 26, 655–672. [Google Scholar] [CrossRef] [PubMed]
- Leppert, K.; Koch, B.; Brähler, E.; Strauß, B. Die resilienzskala (RS)–Überprüfung der langform RS-25 und einer kurzform RS-13. Klin. Diagn. Eval. 2008, 1, 226–243. [Google Scholar]
- Bredle, J.M.; Salsman, J.M.; Debb, S.M.; Arnold, B.J.; Cella, D. Spiritual Well-Being as a Component of Health-Related Quality of Life: The Functional Assessment of Chronic Illness Therapy—Spiritual Well-Being Scale (FACIT-Sp). Religions 2011, 2, 77–94. [Google Scholar] [CrossRef]
- Geisheim, C.; Hahlweg, K.; Fiegenbaum, W.; Frank, M.; Schröder, B.; von Witzleben, I. Das Brief Symptom Inventory (BSI) als Instrument zur Qualitätssicherung in der Psychotherapie. Diagnostica 2002, 48, 28–36. [Google Scholar] [CrossRef]
- ANQ. 2012. Available online: https://www.anq.ch/fileadmin/redaktion/italiano/120611_Info-Instrument_BSCL_IT_v2.pdf (accessed on 15 December 2023).
- Boffo, M.; Mannarini, S.; Munari, C. Exploratory structure equation modeling of the UCLA loneliness scale: A con-tribution to the Italian adaptation. TPM Test. Psychom. Methodol. Appl. Psychol. 2012, 19, 345–363. [Google Scholar]
- Lamm, H.; Stephan, E. Loneliness among German university students: Some correlates. Soc. Behav. Pers. Int. J. 1987, 15, 161–164. [Google Scholar] [CrossRef]
- Bottaro, R.; Valenti, G.D.; Faraci, P. Assessment of an Epidemic Urgency: Psychometric Evidence for the UCLA Loneliness Scale. Psychol. Res. Behav. Manag. 2023, 16, 2843–2855. [Google Scholar] [CrossRef]
- Wagnild, G.M.; Young, H.M. Development and psychometric. J. Nurs. Meas. 1993, 1, 165–17847. [Google Scholar] [PubMed]
- Girtler, N.; Casari, E.-F.; Brugnolo, A.; Cutolo, M.; Dessi, B.; Guasco, S.; Olmi, C.; De Carli, F. Italian validation of the Wagnild and Young Resilience Scale: A perspective to rheumatic diseases. Clin. Exp. Rheumatol. 2010, 28, 669. [Google Scholar] [PubMed]
- Joaquim, R.M.; Pinto, A.L.; Guatimosim, R.F.; de Paula, J.J.; Costa, D.S.; Diaz, A.P.; da Silva, A.G.; Pinheiro, M.I.; Serpa, A.L.; Miranda, D.M.; et al. Bereavement and psychological distress during COVID-19 pandemics: The impact of death experience on mental health. Curr. Res. Behav. Sci. 2021, 2, 100019. [Google Scholar] [CrossRef]
- Kølbæk, P.; Jefsen, O.H.; Speed, M.; Østergaard, S.D. Mental health of patients with mental illness during the COVID-19 pandemic lockdown: A questionnaire-based survey weighted for attrition. Nord. J. Psychiatry 2022, 76, 338–347. [Google Scholar] [CrossRef]
- Rek, S.V.; Freeman, D.; Reinhard, M.A.; Bühner, M.; Grosen, S.; Falkai, P.; Adorjan, K.; Padberg, F. Differential psychological response to the COVID-19 pandemic in psychiatric inpatients compared to a non-clinical population from Germany. Eur. Arch. Psychiatry Clin. Neurosci. 2022, 272, 67–79. [Google Scholar] [CrossRef]
- Batterham, P.J.; Walker, J.; Leach, L.S.; Ma, J.; Calear, A.L.; Christensen, H. A longitudinal test of the predictions of the intepersonal-psychological theory of suicidal behaviour for passive and active suicidal ideation in a large community-based cohort. J. Affect. Disord. 2018, 227, 97–102. [Google Scholar] [CrossRef]
- Liu, R.T.; Bettis, A.H.; Burke, T.A. Characterizing the phenomenology of passive suicidal ideation: A systematic review and meta-analysis of its prevalence, psychiatric comorbidity, correlates, and comparisons with active suicidal ideation. Psychol. Med. 2020, 50, 367–383. [Google Scholar] [CrossRef] [PubMed]
- Sapara, A.; Shalaby, R.; Osiogo, F.; Hrabok, M.; Gusnowski, A.; Vuong, W.; Surood, S.; Urichuk, L.; Greenshaw, A.J.; Agyapong, V.I.O. COVID-19 pandemic: Demographic and clinical correlates of passive death wish and thoughts of self-harm among Canadians. J. Ment. Health 2021, 30, 170–178. [Google Scholar] [CrossRef] [PubMed]
- Alonso, P.; Bertolín, S.; Segalàs, J.; Tubío-Fungueiriño, M.; Real, E.; Mar-Barrutia, L.; Fernández-Prieto, M.; Carvalho, S.R.; Carracedo, A.; Menchón, J. How is COVID-19 affecting patients with obsessive–compulsive disorder? A longitudinal study on the initial phase of the pandemic in a Spanish cohort. Eur. Psychiatry 2021, 64, e45. [Google Scholar] [CrossRef] [PubMed]
- Knowles, J.R.P.; Gray, N.S.; O’connor, C.; Pink, J.; Simkiss, N.J.; Snowden, R.J. The role of hope and resilience in protecting against suicidal thoughts and behaviors during the COVID-19 Pandemic. Arch. Suicide Res. 2022, 26, 1487–1504. [Google Scholar] [CrossRef] [PubMed]
- Verdolini, N.; Amoretti, S.; Montejo, L.; García-Rizo, C.; Hogg, B.; Mezquida, G.; Rabelo-Da-Ponte, F.D.; Vallespir, C.; Radua, J.; Martinez-Aran, A.; et al. Resilience and mental health during the COVID-19 pandemic. J. Affect. Disord. 2021, 283, 156–164. [Google Scholar] [CrossRef] [PubMed]
- Ausín, B.; González-Sanguino, C.; Castellanos, M.; Muñoz, M. Gender-related differences in the psychological impact of confinement as a consequence of COVID-19 in Spain. J. Gend. Stud. 2021, 30, 29–38. [Google Scholar] [CrossRef]
- Agha, S. Mental well-being and association of the four factors coping structure model: A perspective of people living in lockdown during COVID-19. Ethic Med. Public Health 2021, 16, 100605. [Google Scholar] [CrossRef] [PubMed]
- Budimir, S.; Probst, T.; Pieh, C. Coping strategies and mental health during COVID-19 lockdown. J. Ment. Health 2021, 30, 156–163. [Google Scholar] [CrossRef]
- Losada-Baltar, A.; Martínez-Huertas, J.; Jiménez-Gonzalo, L.; Pedroso-Chaparro, M.D.S.; Gallego-Alberto, L.; Fernandes-Pires, J.; Márquez-González, M. Longitudinal Correlates of Loneliness and Psychological Distress During the Lockdown Situation due to COVID-19. Effects of Age and Self-Perceptions of Aging. J. Gerontol. Ser. B 2022, 77, 652–660. [Google Scholar] [CrossRef]
- Westrin, Å.; Lam, R.W. Seasonal Affective Disorder: A Clinical Update. Ann. Clin. Psychiatry 2007, 19, 239–246. [Google Scholar] [CrossRef]
- Wastler, H.M.; Khazem, L.R.; Ammendola, E.; Baker, J.C.; Bauder, C.R.; Tabares, J.; Bryan, C.J. An empirical in-vestigation of the distinction between passive and active ideation: Understanding the latent structure of suicidal thought content. Suicide Life-Threat. Behav. 2022, 53, 219–226. [Google Scholar] [CrossRef] [PubMed]
- Peterman, A.H.; Fitchett, G.; Brady, M.J.; Hernandez, L.; Cella, D. Measuring spiritual well-being in people with cancer: The functional assessment of chronic illness therapy—Spiritual well-being scale (FACIT-Sp). Ann. Behav. Med. 2002, 24, 49–58. [Google Scholar] [CrossRef] [PubMed]

| Variables | Controls N = 234 | Patients N = 80 | Test | p | |
|---|---|---|---|---|---|
| N (%) | N (%) | ||||
| Sex | <0.001 | ||||
| Males | 54 (23.1) | 36 (45) | |||
| Females | 180 (76.9) | 44 (55) | |||
| Age—M (SD) | 45.62 (12.24) | 45.39 (14.23) | t (312) = −0.140 | 0.88 | |
| Ethnic group | |||||
| German | 214 (91.5) | 58 (72.5) | <0.001 | ||
| Italian | 17 (7.3) | 22 (27.5) | |||
| Ladin | 1 (4) | 0 (0) | |||
| Other | 2 (9) | 0 (0) | χ2 (3) = 23.15 | ||
| Mental disorder | yes | 27 (11.5) | - (-) | - | |
| Diagnosis | |||||
| Substance disorders | - (-) | 6 (7.5) | |||
| Psychotic disorders | - (-) | 6 (7.5) | |||
| Affective disorders | - (-) | 47 (58.8) | |||
| Anxiety disorders | - (-) | 3 (3.8) | |||
| Obsessive-compulsive disorder | - (-) | 2 (2.5) | |||
| Stress disorders | - (-) | 6 (7.5) | |||
| Somatic disorders | - (-) | 1 (1.3) | |||
| Neurotic disorders | - (-) | 1 (1.3) | |||
| Sleep disorders | - (-) | 4 (5) | |||
| Personality disorders | - (-) | 1 (1.3) | |||
| Impulse control disorders | - (-) | 2 (2.5) | |||
| Behavioral disorders (childhood) | - (-) | 1 (1.3) |
| Variable | T0: M (SD) | T1: M (SD) | |
|---|---|---|---|
| GSI | Control | 0.57 (0.53) | 0.54 (0.55) |
| Patients | 0.85 (0.70) | 0.81 (0.67) | |
| BSCL-9 | Controls | 0.18 (0.55) | 0.13 (0.43) |
| Patients | 0.51 (0.87) | 0.39 (0.72) | |
| BSCL-39 | Control | 0.19 (0.49) | 0.22 (0.59) |
| Patients | 0.24 (0.60) | 0.48 (0.94) | |
| RES-13 | Control | 71.62 (11.48) | 70.57 (14.17) |
| Patients | 59.31 (15.11) | 62.06 (13.47) | |
| TILS | Control | 5.28 (1.88) | 5.51 (1.86) |
| Patients | 5.95 (1.95) | 5.72 (1.94) | |
| FACIT Peace | Control | 2.98 (0.76) | 3.03 (0.73) |
| Patients | 2.32 (0.93) | 2.42 (0.89) | |
| FACIT Faith | Control | 1.65 (1.06) | 1.76 (1.08) |
| Patients | 1.48 (1.15) | 1.48 (1.08) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stockner, M.; Plattner, B.; Innamorati, M.; Hofer, A.; Burian, I.; Fronthaler, M.; Giupponi, G.; Huber, M.; Macina, C.; Perwanger, V.; et al. How Mental Health and Suicidality Changed during the COVID-19 Pandemic: A Longitudinal Study in the General and Psychiatric Population Illustrating Risk and Protective Factors. Behav. Sci. 2024, 14, 386. https://doi.org/10.3390/bs14050386
Stockner M, Plattner B, Innamorati M, Hofer A, Burian I, Fronthaler M, Giupponi G, Huber M, Macina C, Perwanger V, et al. How Mental Health and Suicidality Changed during the COVID-19 Pandemic: A Longitudinal Study in the General and Psychiatric Population Illustrating Risk and Protective Factors. Behavioral Sciences. 2024; 14(5):386. https://doi.org/10.3390/bs14050386
Chicago/Turabian StyleStockner, Mara, Barbara Plattner, Marco Innamorati, Alex Hofer, Iuliia Burian, Martin Fronthaler, Giancarlo Giupponi, Markus Huber, Christian Macina, Verena Perwanger, and et al. 2024. "How Mental Health and Suicidality Changed during the COVID-19 Pandemic: A Longitudinal Study in the General and Psychiatric Population Illustrating Risk and Protective Factors" Behavioral Sciences 14, no. 5: 386. https://doi.org/10.3390/bs14050386
APA StyleStockner, M., Plattner, B., Innamorati, M., Hofer, A., Burian, I., Fronthaler, M., Giupponi, G., Huber, M., Macina, C., Perwanger, V., Pycha, R., Schaller, G., & Conca, A. (2024). How Mental Health and Suicidality Changed during the COVID-19 Pandemic: A Longitudinal Study in the General and Psychiatric Population Illustrating Risk and Protective Factors. Behavioral Sciences, 14(5), 386. https://doi.org/10.3390/bs14050386







