A Comparison of Pre- and Post-Clinical Simulation Anxiety Levels of Undergraduate Medical Students Before and During the COVID-19 Pandemic: A Prospective Cohort Study
Abstract
1. Introduction
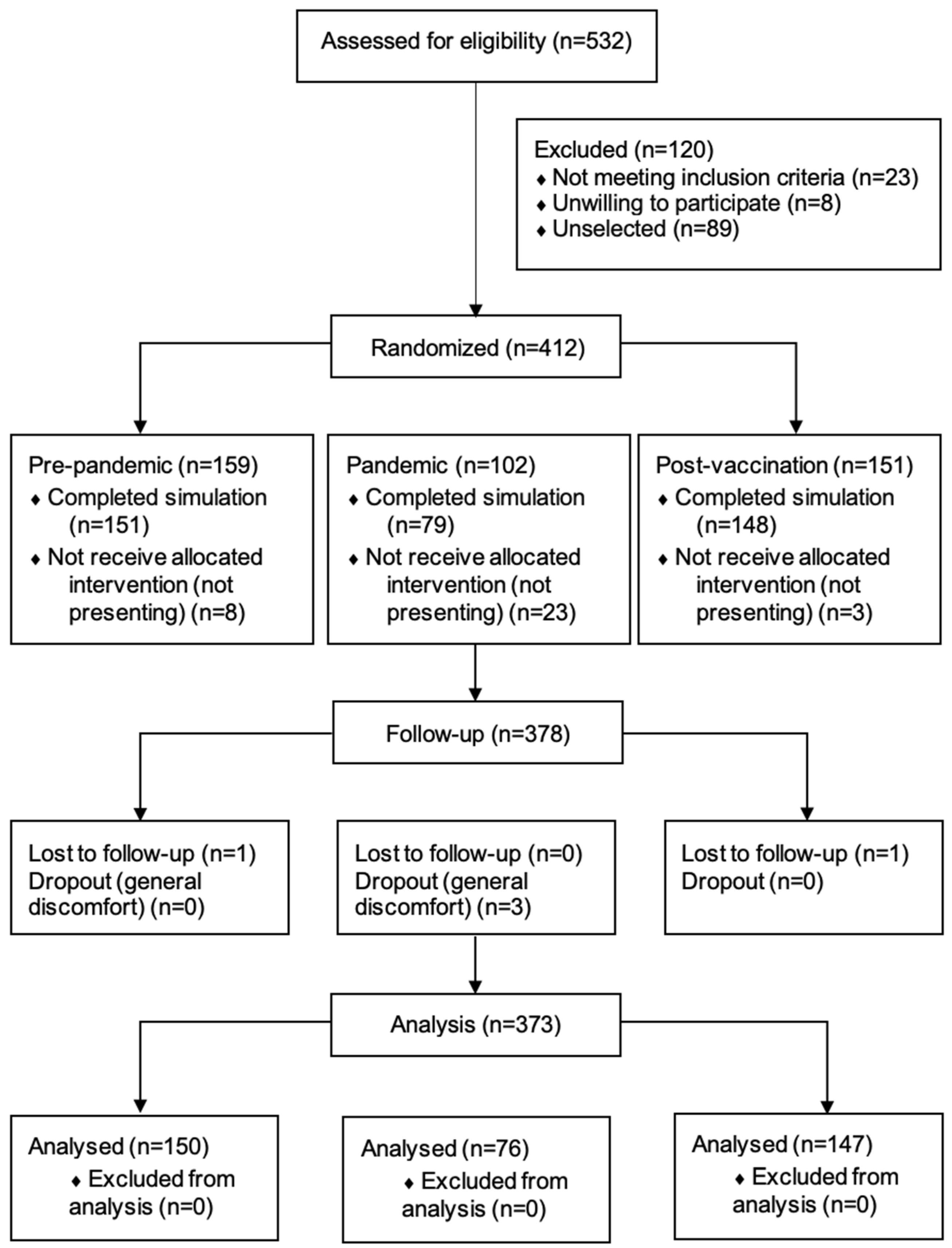
2. Materials and Methods
2.1. Study Design
2.2. Biosafety Protocol
2.3. Participants and Randomization
2.4. Outcome
2.5. Study Protocol
2.6. Statistical Analysis
3. Results
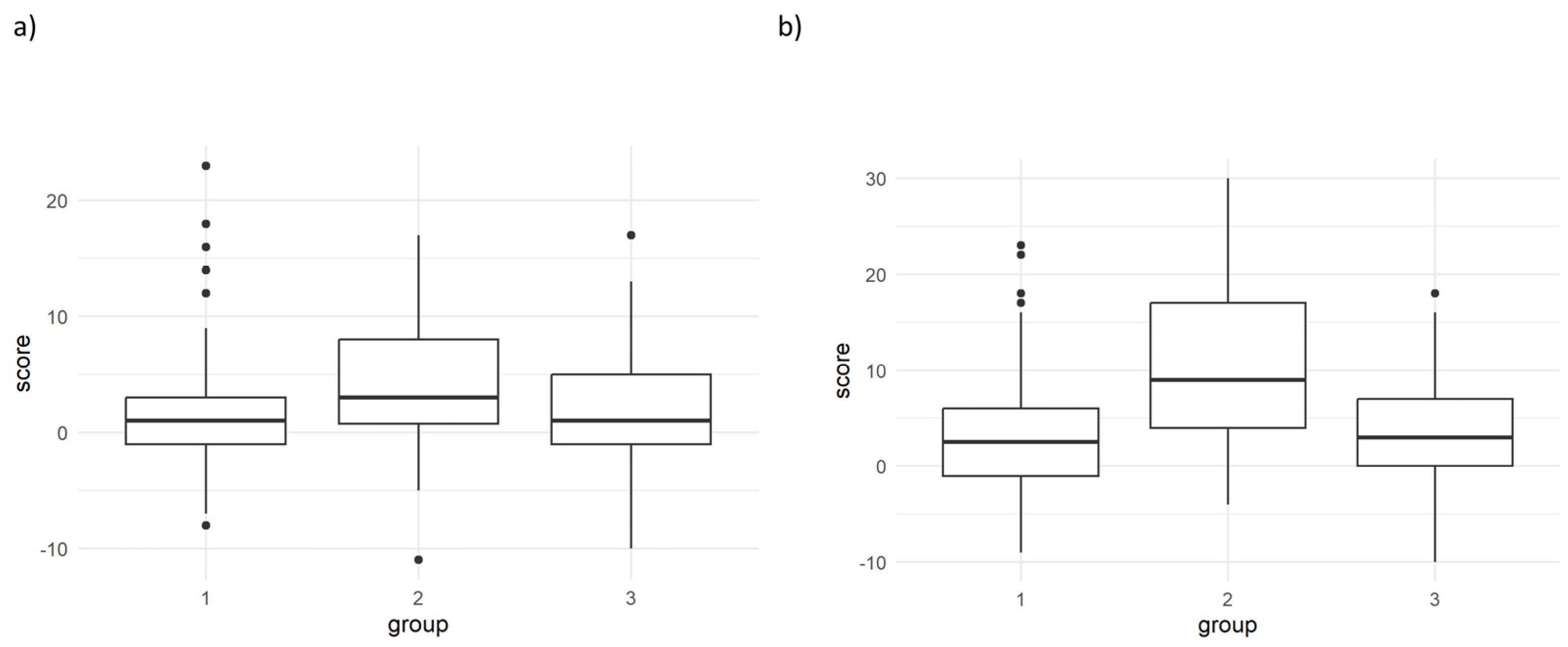
3.1. Primary Outcome
3.2. Logistic Regression
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| COVID-19 | Coronavirus Disease |
| CS | Clinical Simulation |
| GAD-7 | Generalized Anxiety Disorder Scale |
| IQRs | Interquartile Ranges |
| PHQ-9 | 9-Item Patient Health Questionnaire |
| PPE | Personal Protective Equipment |
| SARS-CoV-2 | Severe Acute Respiratory Syndrome Coronavirus |
| STAI | State-Trait Anxiety Inventory |
| STROBE | Strengthening The Reporting Of Observational Studies In Epidemiology |
References
- Al-Balas, M., Al-Balas, H. I., Jaber, H. M., Obeidat, K., Al-Balas, H., Aborajooh, E. A., Al-Taher, R., & Al-Balas, B. (2020). Distance learning in clinical medical education amid COVID-19 pandemic in Jordan: Current situation, challenges, and perspectives. BMC Medical Education, 20(1), 341. [Google Scholar]
- Alsoufi, A., Alsuyihili, A., Msherghi, A., Elhadi, A., Atiyah, H., Ashini, A., Ashwieb, A., Ghula, M., Hasan, H. B., Abudabuos, S., Alameen, H., Abokhdhir, T., Anaiba, M., Nagib, T., Shuwayyah, A., Benothman, R., Arrefae, G., Alkhwayildi, A., Alhadi, A., … Elhadi, M. (2020). Impact of the COVID-19 pandemic on medical education: Medical students’ knowledge, attitudes, and practices regarding electronic learning. PLoS ONE, 15(11), e0242905. [Google Scholar]
- Althwanay, A., Ahsan, F., Oliveri, F., Goud, H. K., Mehkari, Z., Mohammed, L., Javed, M., & Rutkofsky, I. H. (2020). Medical education, pre- and post-pandemic era: A review article. Cureus, 12(10), e10775. [Google Scholar] [CrossRef]
- Anderson, R. J., Bauer, P. R., Arghami, A., Haney, R. M., Reisdorf, E. M., & Baalson, K. (2025). Virtual Reality Simulation to Improve Postoperative Cardiothoracic Surgical Patient Outcomes. American Journal of Critical Care, 34(2), 111–118. [Google Scholar] [CrossRef]
- Barbadoro, P., Brunzini, A., Dolcini, J., Formenti, L., Luciani, A., Messi, D., Papetti, A., Ponzio, E., Germani, M., Starlab Working Collaborative Group, Arsego, D., Bianchi, E., De Angelis, R., Del Bene, L., Landi, R., Mandorli, F., Marcone, M. R., Micheletti, R., Paolucci, G., … Adrario, E. (2023). Stress responses in high-fidelity simulation and standard simulation training among medical students. BMC Medical Education, 23(1), 116. [Google Scholar] [CrossRef]
- Bommer, C., Sullivan, S., Campbell, K., Ahola, Z., Agarwal, S., O’Rourke, A., Jung, H. S., Gibson, A., Leverson, G., & Liepert, A. E. (2018). Pre-simulation orientation for medical trainees: An approach to decrease anxiety and improve confidence and performance. The American Journal of Surgery, 215(2), 266–271. [Google Scholar] [CrossRef]
- Buela-Casal, G., Guillén-Riquelme, A., & Seisdedos-Cubero, N. (2011). Cuestionario de ansiedad estado-rasgo: Adaptación Española (8th ed.). TEA Ediciones. [Google Scholar]
- Chow, J., Al-Duaij, L., Last, N., Sheth, U., Rehman, M., Azim, A., Khalid, F., Blissett, S., & Sibbald, M. (2024). Transformational learning and professional identity formation in postgraduate competency-based medical education. Medical Education, 59(4), 409–417. [Google Scholar] [CrossRef]
- Chu, D. K., Akl, E. A., Duda, S., Solo, K., Yaacoub, S., Schünemann, H. J., El-Harakeh, A., Bognanni, A., Lotfi, T., Loeb, M., Hajizadeh, A., Bak, A., Izcovich, A., Cuello-Garcia, C. A., Chen, C., Harris, D. J., Borowiack, E., Chamseddine, F., Schünemann, F., … Reinap, M. (2020). Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: A systematic review and meta-analysis. The Lancet, 395(10242), 1973–1987. [Google Scholar] [CrossRef]
- Dost, S., Hossain, A., Shehab, M., Abdelwahed, A., & Al-Nusair, L. (2020). Perceptions of medical students towards online teaching during the COVID-19 pandemic: A national cross-sectional survey of 2721 UK medical students. BMJ Open, 10(11), e042378. [Google Scholar] [CrossRef]
- ElBagoury, M., Tolba, M. M., Nasser, H. A., Jabbar, A., Elagouz, A. M., Aktham, Y., & Hutchinson, A. (2021). The find of COVID-19 vaccine: Challenges and opportunities. Journal of Infection and Public Health, 14(3), 389–416. [Google Scholar] [CrossRef] [PubMed]
- Fredericks, S., ElSayed, M., Hammad, M., Abumiddain, O., Istwani, L., Rabeea, A., Rashid-Doubell, F., & Bella, A. M. (2021). Anxiety is associated with extraneous cognitive load during teaching using high-fidelity clinical simulation. Medical Education Online, 26(1), 1994691. [Google Scholar] [CrossRef]
- Grasselli, G., Greco, M., Zanella, A., Albano, G., Antonelli, M., Bellani, G., Bonanomi, E., Cabrini, L., Carlesso, E., Castelli, G., Cattaneo, S., Cereda, D., Colombo, S., Coluccello, A., Crescini, G., Molinari, A. F., Foti, G., Fumagalli, R., Iotti, G. A., … Cecconi, M. (2020). Risk factors associated with mortality among patients with COVID-19 in intensive care units in Lombardy, Italy. JAMA Internal Medicine, 180(10), 1345–1355. [Google Scholar] [CrossRef]
- Gustafson, L. W., Gabel, P., Hammer, A., Lauridsen, H. H., Petersen, L. K., Andersen, B., Bor, P., & Larsen, M. B. (2020). Validity and reliability of State-Trait Anxiety Inventory in Danish women aged 45 years and older with abnormal cervical screening results. BMC Medical Research Methodology, 20(1), 89. [Google Scholar] [CrossRef]
- Halperin, S. J., Henderson, M. N., Prenner, S., & Grauer, J. N. (2021). Prevalence of anxiety and depression among medical students during the COVID-19 pandemic: A cross-sectional study. Journal of Medical Education and Curricular Development, 8, 2382120521991150. [Google Scholar] [CrossRef]
- Hernández-Martínez, A., Rodríguez-Almagro, J., Martínez-Arce, A., Romero-Blanco, C., García-Iglesias, J. J., & Gómez-Salgado, J. (2021). Nursing students’ experience and training in healthcare aid during the COVID-19 pandemic in Spain. Journal of Clinical Nursing. Online ahead of print. [Google Scholar] [CrossRef]
- Ju, M., Bochatay, N., Werne, A., Essakow, J., Tsang, L., Nottingham, M., Franzon, D., Lyndon, A., & van Schaik, S. (2024). Changing the conversation: Impact of guidelines designed to optimize interprofessional facilitation of simulation-based team training. Advances in Simulation, 9(1), 43. [Google Scholar] [CrossRef]
- Koca, A., Schlatter, S., Delas, Q., Denoyel, L., Lehot, J., Lilot, M., & Rimmelé, T. (2023). Influence of the embedded participant on learners’ performance during high-fidelity simulation sessions in healthcare. BMC Medical Education, 23(1), 751. [Google Scholar] [CrossRef]
- Liaw, S. Y., Chan, S. W., Chen, F., Hooi, S. C., & Siau, C. (2014). Comparison of Virtual Patient Simulation With Mannequin-Based Simulation for Improving Clinical Performances in Assessing and Managing Clinical Deterioration: Randomized Controlled Trial. Journal of Medical Internet Research, 16(9), e214. [Google Scholar] [CrossRef]
- Liaw, S. Y., Rethans, J., Scherpbier, A., & Piyanee, K. (2011). Rescuing A Patient In Deteriorating Situations (RAPIDS): A simulation-based educational program on recognizing, responding and reporting of physiological signs of deterioration. Resuscitation, 82(9), 1224–1230. [Google Scholar] [CrossRef]
- Lim, W. Y., Ong, J., Vimal, V., Lim, H., Tan, H. C., Wong, P., Ho, V. K., & Ong, S. G. K. (2020). High-fidelity simulation training with PPE may optimise resuscitation outcomes in the COVID-19 era. Resuscitation, 159, 42–44. [Google Scholar] [CrossRef]
- Martín Rodríguez, F., Fernández Pérez, C., Castro Villamor, M., Martín Conty, J. L., Arnillas Gómez, P., & Casado Vicente, V. (2018). Does level D personal protective equipment guard against hazardous biologic agents during cardiopulmonary resuscitation? Emergencias, 30(2), 119–122. [Google Scholar] [PubMed]
- Martín-Rodríguez, F., Sanz-García, A., López-Izquierdo, R., Benito, J. F. D., Martín-Conty, J. L., Villamor, M. A. C., & Ortega, G. J. (2020). Predicting health care workers’ tolerance of personal protective equipment: An observational simulation study. Clinical Simulation in Nursing, 47, 65–72. [Google Scholar] [CrossRef] [PubMed]
- Martín-Rodríguez, F., Villamor, M. A. C., López-Izquierdo, R., Rubiales, R. M. P., Ortega, G. J., & Sanz-García, A. (2021). Can anxiety in undergraduate students in a high-fidelity clinical simulation be predicted? A randomized, sham-controlled, blinded trial. Nurse Education Today, 98, 104774. [Google Scholar] [CrossRef]
- McCoy, C. E., Rahman, A., Rendon, J. C., Anderson, C. L., Langdorf, M. I., Lotfipour, S., & Chakravarthy, B. (2018). Randomized controlled trial of simulation vs. standard training for teaching medical students high-quality cardiopulmonary resuscitation. Western Journal of Emergency Medicine, 20(1), 15–22. [Google Scholar] [CrossRef] [PubMed]
- Métais, A., Omarjee, M., Valero, B., Gleich, A., Mekki, A., Henry, A., Duclos, A., Lilot, M., Rode, G., & Schlatter, S. (2025). Determining the influence of an intervention of stress management on medical students’ levels of psychophysiological stress: The protocol of the PROMESS-Stress clinical trial. BMC Medical Education, 25(1), 225. [Google Scholar] [CrossRef]
- Nembhard, M. D., Burton, D. J., & Cohen, J. M. (2020). Ventilation use in nonmedical settings during COVID-19: Cleaning protocol, maintenance, and recommendations. Toxicology and Industrial Health, 36(9), 644–653. [Google Scholar] [CrossRef]
- Pandemic Fatigue. (2020). Pandemic fatigue—Reinvigorating the public to prevent COVID-19. Policy framework for supporting pandemic prevention and management (Licence: CC BY-NC-SA 3.0 IGO). WHO Regional Office for Europe. [Google Scholar]
- Rajab, M. H., Gazal, A. M., & Alkattan, K. (2020). Challenges to online medical education during the COVID-19 pandemic. Cureus, 12(7), e8966. [Google Scholar] [CrossRef]
- Rose, S. (2020). Medical student education in the time of COVID-19. JAMA, 323(21), 2131–2132. [Google Scholar] [CrossRef]
- Saddik, B., Hussein, A., Sharif-Askari, F. S., Kheder, W., Temsah, M., Koutaich, R. A., Haddad, E. S., Al-Roub, N. M., Marhoon, F. A., Hamid, Q., & Halwani, R. (2020). Increased levels of anxiety among medical and non-medical university students during the COVID-19 pandemic in the united Arab emirates. Risk Management and Healthcare Policy, 13, 2395–2406. [Google Scholar] [CrossRef]
- Segura Azuara, N. d. l. Á., Eraña Rojas, I. E., Valeria Luna-de-la-Garza, M., Castorena-Ibarr, J., & López Cabrera, M. V. (2020). Analysis of anxiety on early clinical encounters: Experiences using clinical simulation in undergraduate students. Educación Médica, 21(6), 377–382. [Google Scholar] [CrossRef]
- Shin, S., Park, J., & Kim, J. (2015). Effectiveness of patient simulation in nursing education: Meta-analysis. Nurse Education Today, 35(1), 176–182. [Google Scholar] [CrossRef] [PubMed]
- Sindiani, A. M., Obeidat, N., Alshdaifat, E., Elsalem, L., Alwani, M. M., Rawashdeh, H., Fares, A. S., Alalawne, T., & Tawalbeh, L. I. (2020). Distance education during the COVID-19 outbreak: A cross-sectional study among medical students in North of Jordan. Annals of Medicine & Surgery, 59, 186–194. [Google Scholar] [CrossRef]
- Son, C., Hegde, S., Smith, A., Wang, X., & Sasangohar, F. (2020). Effects of COVID-19 on college students’ mental health in the United States: Interview survey study. Journal of Medical Internet Research, 22(9), e21279. [Google Scholar] [CrossRef] [PubMed]
- Tabah, A., Ramanan, M., Laupland, K. B., Buetti, N., Cortegiani, A., Mellinghoff, J., Morris, A. C., Camporota, L., Zappella, N., Elhadi, M., Povoa, P., Amrein, K., Vidal, G., Derde, L., Bassetti, M., Francois, G., Kai, N. S. Y., & De Waele, J. J. (2020). Personal protective equipment and intensive care unit healthcare worker safety in the COVID-19 era (PPE-SAFE): An international survey. Journal of Critical Care, 59, 70–75. [Google Scholar] [CrossRef]
- Wang, H., Zhou, Y., Dai, P., Guan, Y., Zhong, J., Li, N., & Yu, M. (2023). Anxiety symptoms and associated factors among school students after 2 years of the COVID-19 pandemic: A cross-sectional study in Zhejiang Province, China. BMJ Open, 13(12), e079084. [Google Scholar] [CrossRef]
- Weimer, J. M., Sprengart, F. M., Vieth, T., Göbel, S., Dionysopoulou, A., Krüger, R., Beer, J., Weimer, A. M., Buggenhagen, H., Kloeckner, R., Pillong, L., Helfrich, J., Waezsada, E., Wand, P., & Weinmann-Menke, J. (2025). Simulator training in focus assessed transthoracic echocardiography (FATE) for undergraduate medical students: Results from the FateSim randomized controlled trial. BMC Medical Education, 25(1), 21. [Google Scholar] [CrossRef]
| Study Period | ||||
|---|---|---|---|---|
| Variable a | Prepandemic | Pandemic | Postvaccination | p Value b |
| No. (%) with data | 150 (40.2) | 76 (20.4) | 147 (39.4) | N.A. |
| Sex at birth, female | 99 (66) | 54 (71.1) | 103 (70.1) | 0.660 |
| Age, year | 23 (23–24) | 24 (23–24) | 23 (23–24) | 0.338 |
| Body mass index, kg/m2 | 21.6 (19.8–23.3) | 22.2 (20.1–24.7) | 21.1 (19.5–23.2) | 0.078 |
| Lifestyle habits | ||||
| Smoking | 20 (13.3) | 15 (19.7) | 7 (4.76) | 0.002 |
| Coffee/tea | 130 (86.7) | 64 (84.2) | 110 (74.8) | 0.025 |
| Energy drinks | 9 (6) | 12 (15.8) | 8 (5.44) | 0.014 |
| Prior simulation experience, yes | 0 (0) | 51 (67.1) | 102 (69.4) | <0.001 |
| Leader, yes | 78 (52) | 41 (53.9) | 78 (53.1) | 0.960 |
| Randomization | 0.998 | |||
| Hip fracture | 20 (13.3) | 11 (14.5) | 20 (13.6) | |
| Asthmatic exacerbation | 20 (13.3) | 10 (13.2) | 20 (13.6) | |
| Sepsis | 20 (13.3) | 9 (11.8) | 20 (13.6) | |
| Acute heart failure | 18 (12.0) | 7 (9.21) | 17 (11.6) | |
| Polytraumatized | 20 (13.3) | 11 (14.5) | 18 (12.2) | |
| Anaphylactic shock | 20 (13.3) | 11 (14.5) | 18 (12.2) | |
| Acute myocardial infarction | 19 (12.7) | 10 (13.2) | 19 (12.9) | |
| Thromboembolism in PW | 13 (8.67) | 7 (9.21) | 15 (10.2) | |
| Baseline evaluation | ||||
| Vital signs | ||||
| Oxygen saturation, % | 98 (97–98) | 98 (97–98) | 98 (97–98) | 0.743 |
| Perfusion index, % | 2.1 (1.1–4.4) | 2.1 (1–4.3) | 1.9 (0.9–4.4) | 0.989 |
| SBP, mmHg | 130 (122–146) | 125 (115–136) | 134 (124–154) | <0.001 |
| DBP, mmHg | 84 (75–91) | 76 (71–86) | 84 (77–90) | 0.006 |
| MBP, mmHg | 100 (92–110) | 92 (87–102) | 102 (93–112) | <0.001 |
| Heart rate, beats/min | 84 (74–96) | 91 (74–104) | 93 (80–111) | 0.002 |
| Temperature, °C | 37 (36.8–37.3) | 37.1 (36.6–37.3) | 36.9 (36.6–37.2) | 0.076 |
| Postsimulation evaluation | ||||
| Vital signs | ||||
| Oxygen saturation, % | 98 (97–99) | 98 (97–99) | 98 (97–99) | 0.905 |
| Perfusion index, % | 1.4 (0.9–2.4) | 1.3 (0.7–2.3) | 1.4 (0.8–2.4) | 0.787 |
| SBP, mmHg | 130 (121–149) | 132 (122–137) | 133 (123–160) | 0.005 |
| DBP, mmHg | 83 (76–91) | 84 (79–91) | 83 (77–92) | 0.932 |
| MBP, mmHg | 101 (91–113) | 101 (95–105) | 104 (90–114) | 0.206 |
| Heart rate, beats/min | 85 (74–98) | 88 (75–100) | 91 (80–114) | 0.001 |
| Temperature, °C | 36.9 (36.7–37.2) | 36.9 (36.6–37.2) | 36.8 (36.6–37.1) | 0.044 |
| Study Period | ||||
|---|---|---|---|---|
| Variable a | Prepandemic | Pandemic | Postvaccination | p Value b |
| No. (%) with data | 150 (40.2) | 76 (20.4) | 147 (39.4) | N.A. |
| Baseline evaluation | ||||
| State-Trait Anxiety Inventory | ||||
| State, points | 41 (37–47) | 57 (50–63) | 41 (37–45) | <0.001 |
| Trait, points | 31 (27–37) | 41 (33–48) | 32 (29–37) | <0.001 |
| Postsimulation evaluation | ||||
| State-Trait Anxiety Inventory | ||||
| State, points | 45 (40–50) | 66 (62–71) | 46 (41–50) | <0.001 |
| Trait, points | 32 (27–39) | 47 (40–51) | 34 (29–39) | <0.001 |
| State-Trait Anxiety Inventory difference | ||||
| State, points | 2.5 (−1 to 6) | 9 (4–17) | 3 (0–7) | <0.001 |
| Trait, points | 1 (−1 to 3) | 3 (0.2–8) | 1 (−1 to 5) | <0.001 |
| Variable a | Estimate | Standard Error | Z Value | p Value |
|---|---|---|---|---|
| Previous experience: prepandemic | 20.5 | 831.8 | NA | NA |
| Previous experience: postvaccination | −0.23 | 0.36 | −0.66 | 0.508 |
| SBP: prepandemic | 0.04 | 0.02 | 2.04 | 0.040 |
| SBP: postvaccination | 0.05 | 0.01 | NA | NA |
| MBP: prepandemic | −0.02 | 0.02 | −0.81 | 0.415 |
| MBP: postvaccination | −0.01 | 0.02 | −0.72 | 0.466 |
| STAI-State: prepandemic | −0.17 | 0.03 | −5.43 | <0.001 |
| STAI-State: postvaccination | −0.12 | 0.02 | −4.63 | <0.001 |
| STAI-Trait: prepandemic | −0.001 | 0.04 | −0.03 | 0.974 |
| STAI-Trait: postvaccination | −0.03 | 0.03 | −1.03 | 0.302 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martín-Sánchez, R.; Sanz-García, A.; Diaz-Gonzalez, S.; Castro Villamor, M.Á.; Sáez-Belloso, S.; Rabanales Sotos, J.; Pinilla-Arribas, L.T.; González-Izquierdo, P.; de Santos Sánchez, S.; Martín-Rodríguez, F. A Comparison of Pre- and Post-Clinical Simulation Anxiety Levels of Undergraduate Medical Students Before and During the COVID-19 Pandemic: A Prospective Cohort Study. Behav. Sci. 2025, 15, 447. https://doi.org/10.3390/bs15040447
Martín-Sánchez R, Sanz-García A, Diaz-Gonzalez S, Castro Villamor MÁ, Sáez-Belloso S, Rabanales Sotos J, Pinilla-Arribas LT, González-Izquierdo P, de Santos Sánchez S, Martín-Rodríguez F. A Comparison of Pre- and Post-Clinical Simulation Anxiety Levels of Undergraduate Medical Students Before and During the COVID-19 Pandemic: A Prospective Cohort Study. Behavioral Sciences. 2025; 15(4):447. https://doi.org/10.3390/bs15040447
Chicago/Turabian StyleMartín-Sánchez, Rafael, Ancor Sanz-García, Samantha Diaz-Gonzalez, Miguel Ángel Castro Villamor, Silvia Sáez-Belloso, Joseba Rabanales Sotos, Leyre T. Pinilla-Arribas, Pablo González-Izquierdo, Sara de Santos Sánchez, and Francisco Martín-Rodríguez. 2025. "A Comparison of Pre- and Post-Clinical Simulation Anxiety Levels of Undergraduate Medical Students Before and During the COVID-19 Pandemic: A Prospective Cohort Study" Behavioral Sciences 15, no. 4: 447. https://doi.org/10.3390/bs15040447
APA StyleMartín-Sánchez, R., Sanz-García, A., Diaz-Gonzalez, S., Castro Villamor, M. Á., Sáez-Belloso, S., Rabanales Sotos, J., Pinilla-Arribas, L. T., González-Izquierdo, P., de Santos Sánchez, S., & Martín-Rodríguez, F. (2025). A Comparison of Pre- and Post-Clinical Simulation Anxiety Levels of Undergraduate Medical Students Before and During the COVID-19 Pandemic: A Prospective Cohort Study. Behavioral Sciences, 15(4), 447. https://doi.org/10.3390/bs15040447






