The Prognostic Role of Lactate Concentrations after Aneurysmal Subarachnoid Hemorrhage
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Participants
2.3. Data Collection
2.4. Statistical Analysis
3. Results
3.1. Study Population
3.2. Lactate and Glucose Concentrations
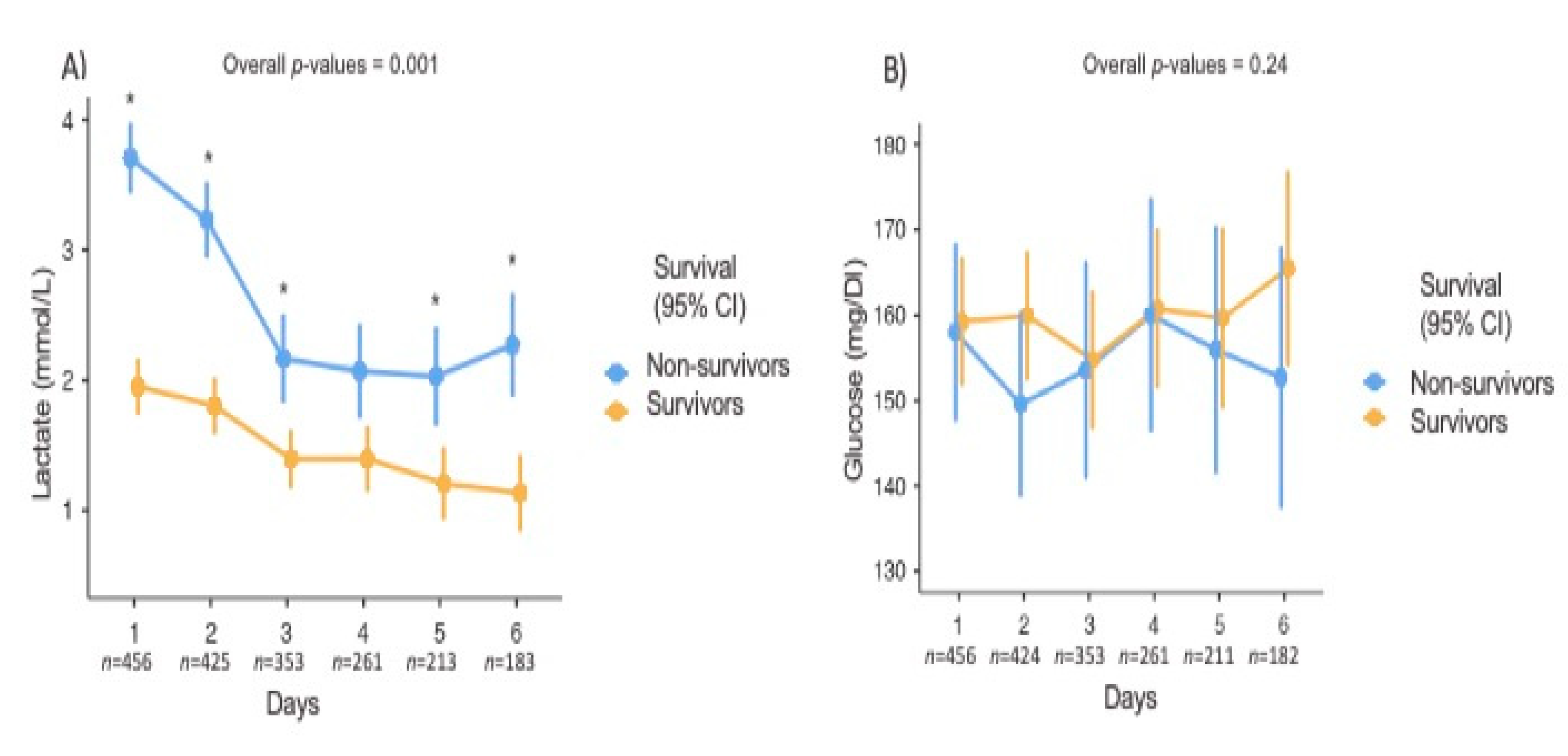
3.3. Lactate Concentrations and Hospital Mortality
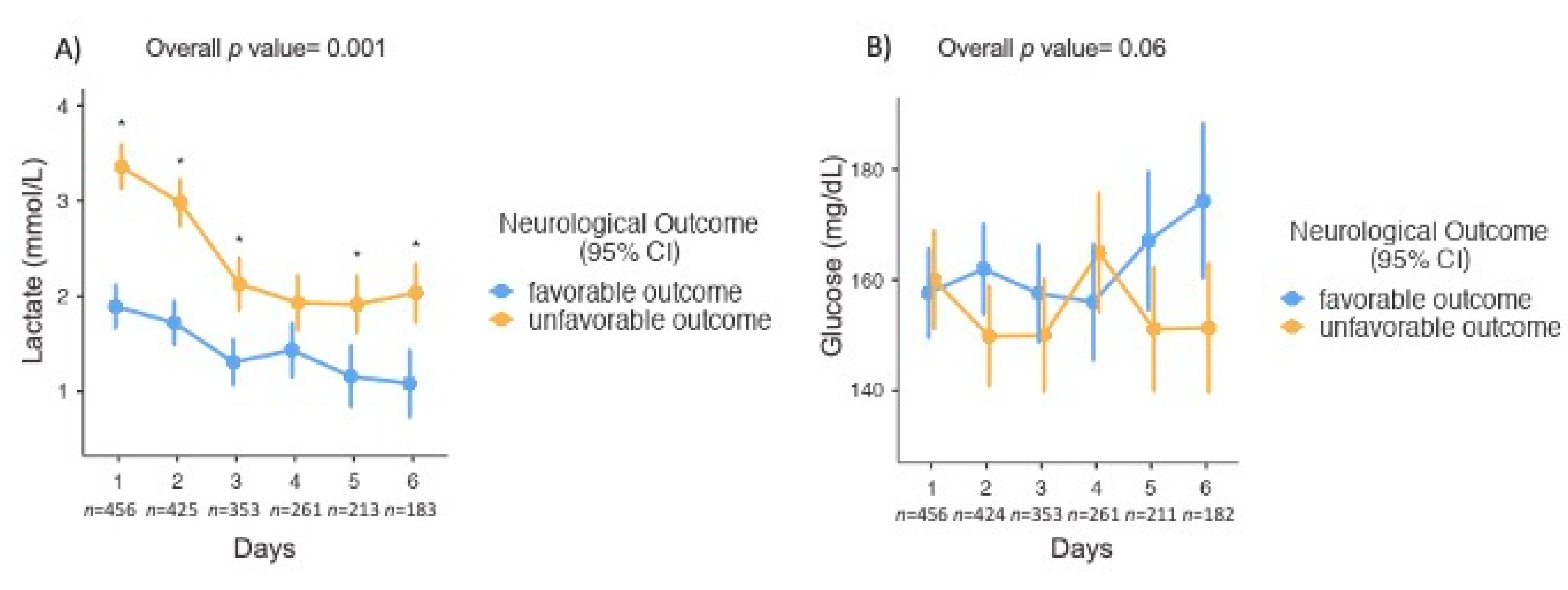
3.4. Lactate Concentrations and Neurological Outcome
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Etminan, N.; Chang, H.S.; Hackenberg, K.; de Rooij, N.K.; Vergouwen, M.D.I.; Rinkel, G.J.E.; Algra, A. worldwide incidence of aneurysmal subarachnoid hemorrhage according to region, time period, blood pressure, and smoking prevalence in the population: A systematic review and meta-analysis. JAMA Neurol. 2019, 76, 588–597. [Google Scholar] [CrossRef] [PubMed]
- Rinkel, G.J.; Algra, A. Long-term outcomes of patients with aneurysmal subarachnoid haemorrhage. Lancet Neurol. 2011, 10, 349–356. [Google Scholar] [CrossRef]
- Tam, A.K.; Ilodigwe, D.; Mocco, J.; Mayer, S.; Kassell, N.; Ruefenacht, D.; Schmiedek, P.; Weidauer, S.; Pasqualin, A.; Macdonald, R.L. Impact of systemic inflammatory response syndrome on vasospasm, cerebral infarction, and outcome after subarachnoid hemorrhage: Exploratory analysis of CONSCIOUS-1 database. Neurocrit. Care 2010, 13, 182–189. [Google Scholar] [CrossRef] [PubMed]
- De Oliveira Manoel, A.L.; Macdonald, R.L. Neuroinflammation as a Target for Intervention in Subarachnoid Hemorrhage. Front. Neurol. 2018, 9, 292. [Google Scholar] [CrossRef]
- Naredi, S.; Lambert, G.; Friberg, P.; Zall, S.; Eden, E.; Rydenhag, B.; Tylman, M.; Bengtsson, A. Sympathetic activation and inflammatory response in patients with subarachnoid haemorrhage. Intensive Care Med. 2006, 32, 1955–1961. [Google Scholar] [CrossRef]
- Macmillan, C.S.; Grant, I.S.; Andrews, P.J. Pulmonary and cardiac sequelae of subarachnoid haemorrhage: Time for active management? Intensive Care Med. 2002, 28, 1012–1023. [Google Scholar] [CrossRef]
- Capes, S.E.; Hunt, D.; Malmberg, K.; Pathak, P.; Gerstein, H.C. Stress hyperglycemia and prognosis of stroke in nondiabetic and diabetic patients: A systematic overview. Stroke 2001, 32, 2426–2432. [Google Scholar] [CrossRef]
- Bakker, J.; Nijsten, M.W.; Jansen, T.C. Clinical use of lactate monitoring in critically ill patients. Ann. Intensive Care 2013, 3, 12. [Google Scholar] [CrossRef]
- Kruse, O.; Grunnet, N.; Barfod, C. Blood lactate as a predictor for in-hospital mortality in patients admitted acutely to hospital: A systematic review. Scand. J. Trauma Resusc. Emerg. Med. 2011, 19, 74. [Google Scholar] [CrossRef]
- Vincent, J.-L.; Quintairos, E.S.A.; Couto, L.; Taccone, F.S. The value of blood lactate kinetics in critically ill patients: A systematic review. Crit. Care 2016, 20, 257. [Google Scholar] [CrossRef]
- Godinjak, A.; Iglica, A.; Burekovic, A.; Jusufovic, S.; Ajanovic, A.; Tancica, I.; Kukuljac, A. Hyperglycemia in Critically Ill Patients: Management and Prognosis. Med. Arch. 2015, 69, 157–160. [Google Scholar] [CrossRef] [PubMed]
- Tholance, Y.; Barcelos, G.K.; Dailler, F.; Renaud, B.; Marinesco, S.; Perret-Liaudet, A. Biochemical neuromonitoring of poor-grade aneurysmal subarachnoid hemorrhage: Comparative analysis of metabolic events detected by cerebral microdialysis and by retrograde jugular vein catheterization. Neurol. Res. 2015, 37, 578–587. [Google Scholar] [CrossRef] [PubMed]
- Oddo, M.; Levine, J.M.; Frangos, S.; Maloney-Wilensky, E.; Carrera, E.; Daniel, R.T.; Levivier, M.; Magistretti, P.J.; LeRoux, P.D. Brain lactate metabolism in humans with subarachnoid hemorrhage. Stroke 2012, 43, 1418–1421. [Google Scholar] [CrossRef] [PubMed]
- Sarrafzadeh, A.; Haux, D.; Kuchler, I.; Lanksch, W.R.; Unterberg, A.W. Poor-grade aneurysmal subarachnoid hemorrhage: Relationship of cerebral metabolism to outcome. J. Neurosurg. 2004, 100, 400–406. [Google Scholar] [CrossRef]
- Van Donkelaar, C.E.; Dijkland, S.A.; van den Bergh, W.M.; Bakker, J.; Dippel, D.W.; Nijsten, M.W.; van der Jagt, M. Early circulating lactate and glucose levels after aneurysmal subarachnoid hemorrhage correlate with poor outcome and delayed cerebral ischemia: A two-center cohort study. Crit. Care Med. 2016, 44, 966–972. [Google Scholar] [CrossRef]
- Aisiku, I.P.; Chen, P.R.; Truong, H.; Monsivais, D.R.; Edlow, J. Admission serum lactate predicts mortality in aneurysmal subarachnoid hemorrhage. Am. J. Emerg. Med. 2016, 34, 708–712. [Google Scholar] [CrossRef]
- Oh, C.H.; Kim, J.W.; Kim, G.H.; Lee, K.R.; Hong, D.Y.; Park, S.O.; Baek, K.J.; Kim, S.Y. Serum lactate could predict mortality in patients with spontaneous subarachnoid hemorrhage in the emergency department. Front. Neurol. 2020, 11, 975. [Google Scholar] [CrossRef]
- Okazaki, T.; Hifumi, T.; Kawakita, K.; Shishido, H.; Ogawa, D.; Okauchi, M.; Shindo, A.; Kawanishi, M.; Inoue, S.; Tamiya, T.; et al. Serial blood lactate measurements and its prognostic significance in intensive care unit management of aneurysmal subarachnoid hemorrhage patients. J. Crit. Care 2017, 41, 229–233. [Google Scholar] [CrossRef]
- Poblete, R.A.; Cen, S.Y.; Zheng, L.; Emanuel, B.A. Serum lactic acid following aneurysmal subarachnoid hemorrhage is a marker of disease severity but is not associated with hospital outcomes. Front. Neurol. 2018, 9, 593. [Google Scholar] [CrossRef]
- Bogossian, E.G.; Attanasio, L.; Creteur, J.; Grimaldi, D.; Schuind, S.; Taccone, F.S. The impact of extra-cerebral infection after subarachnoid hemorrhage: A single center cohort study. World Neurosurg. 2020, 144, e883–e897. [Google Scholar] [CrossRef]
- Knaus, W.A.; Draper, E.A.; Wagner, D.P.; Zimmerman, J.E. APACHE II: A severity of disease classification system. Crit. Care Med. 1985, 13, 818–829. [Google Scholar] [CrossRef] [PubMed]
- Teasdale, G.; Maas, A.; Lecky, F.; Manley, G.; Stocchetti, N.; Murray, G. The Glasgow coma scale at 40 years: Standing the test of time. Lancet Neurol. 2014, 13, 844–854. [Google Scholar] [CrossRef]
- Drake, C.G. Report of world federation of neurological surgeons committee on a universal subarachnoid hemorrhage grading scale. J. Neurosurg. 1988, 68, 985–986. [Google Scholar]
- Fisher, C.M.; Roberson, G.H.; Ojemann, R.G. Cerebral vasospasm with ruptured saccular aneurysm—The clinical manifestations. Neurosurgery 1977, 1, 245–248. [Google Scholar] [CrossRef] [PubMed]
- Vincent, J.L.; Moreno, R.; Takala, J.; Willatts, S.; De Mendonca, A.; Bruining, H.; Reinhart, C.K.; Suter, P.M.; Thijs, L.G. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the working group on sepsis-related problems of the European society of intensive care medicine. Intensive Care Med. 1996, 22, 707–710. [Google Scholar] [CrossRef] [PubMed]
- Kliegel, A.; Losert, H.; Sterz, F.; Holzer, M.; Zeiner, A.; Havel, C.; Laggner, A.N. Serial lactate determinations for prediction of outcome after cardiac arrest. Medicine (Baltimore) 2004, 83, 274–279. [Google Scholar] [CrossRef]
- Bilotta, F.; Rosa, G. Glucose management in the neurosurgical patient: Are we yet any closer? Curr. Opin. Anaesthesiol. 2010, 23, 539–543. [Google Scholar] [CrossRef]
- McMillan, T.; Wilson, L.; Ponsford, J.; Levin, H.; Teasdale, G.; Bond, M. The Glasgow outcome scale—40 years of application and refinement. Nat. Rev. Neurol. 2016, 12, 477–485. [Google Scholar] [CrossRef]
- Lederer, D.J.B.S.; Branson, R.D.; Chalmers, J.D.; Marshall, R.; Maslove, D.M.; Ost, D.E.; Punjabi, N.M.; Schatz, M.; Smyth, A.R.; Stewart, P.W.; et al. Control of confounding and reporting of results in causal inference studies. Guidance for authors from editors of respiratory, sleep, and critical care journals. Ann. Am. Thorac. Soc. 2019, 16, 22–28. [Google Scholar] [CrossRef]
- Mutoh, T.; Kazumata, K.; Ajiki, M.; Ushikoshi, S.; Terasaka, S. Goal-directed fluid management by bedside transpulmonary hemodynamic monitoring after subarachnoid hemorrhage. Stroke 2007, 38, 3218–3224. [Google Scholar] [CrossRef]
- Tung, P.; Kopelnik, A.; Banki, N.; Ong, K.; Ko, N.; Lawton, M.T.; Gress, D.; Drew, B.; Foster, E.; Parmley, W.; et al. Predictors of neurocardiogenic injury after subarachnoid hemorrhage. Stroke 2004, 35, 548–551. [Google Scholar] [CrossRef] [PubMed]
- Lee, V.H.; Connolly, H.M.; Fulgham, J.R.; Manno, E.M.; Brown, R.D.; Wijdicks, E.F., Jr. Tako-tsubo cardiomyopathy in aneurysmal subarachnoid hemorrhage: An underappreciated ventricular dysfunction. J. Neurosurg. 2006, 105, 264–270. [Google Scholar] [CrossRef] [PubMed]
- Dorhout Mees, S.M.; Hoff, R.G.; Rinkel, G.J.; Algra, A.; van den Bergh, W.M. Brain natriuretic peptide concentrations after aneurysmal subarachnoid hemorrhage: Relationship with hypovolemia and hyponatremia. Neurocrit. Care 2011, 14, 176–181. [Google Scholar] [CrossRef] [PubMed]
- Wartenberg, K.E.; Schmidt, J.M.; Claassen, J.; Temes, R.E.; Frontera, J.A.; Ostapkovich, N.; Parra, A.; Connolly, E.S.; Mayer, S.A. Impact of medical complications on outcome after subarachnoid hemorrhage. Crit. Care Med. 2006, 34, 617–623. [Google Scholar] [CrossRef]
- Gattinoni, L.; Vasques, F.; Camporota, L.; Meessen, J.; Romitti, F.; Pasticci, I.; Duscio, E.; Vassalli, F.; Forni, L.G.; Payen, D.; et al. Understanding Lactatemia in Human Sepsis. Potential Impact for Early Management. Am. J. Respir. Crit. Care Med. 2019, 200, 582–589. [Google Scholar] [CrossRef]
- Meyerhof, O. Recent investigations on the aerobic and an—Aerobic metabolism of carbohydrates. J. Gen. Physiol. 1927, 8, 531–542. [Google Scholar] [CrossRef]
- Cori, C.F.; Cori, G.T. Carbohydrate metabolism. Annu. Rev. Biochem. 1946, 15, 193–218. [Google Scholar] [CrossRef]
- Marik, P.E.; Bellomo, R. Stress hyperglycemia: An essential survival response! Crit. Care 2013, 17, 305. [Google Scholar] [CrossRef]
- Cesarini, K.G.; Enblad, P.; Ronne-Engstrom, E.; Marklund, N.; Salci, K.; Nilsson, P.; Hardemark, H.G.; Hillered, L.; Persson, L. Early cerebral hyperglycolysis after subarachnoid haemorrhage correlates with favourable outcome. Acta Neurochir. (Wien.) 2002, 144, 1121–1131. [Google Scholar] [CrossRef]
- Zahra, K.; Gopal, N.; Freeman, W.D.; Turnbull, M.T. Using cerebral metabolites to guide precision medicine for subarachnoid hemorrhage: Lactate and pyruvate. Metabolites 2019, 9, 245. [Google Scholar] [CrossRef]
- Rhodes, A.; Evans, L.E.; Alhazzani, W.; Levy, M.M.; Antonelli, M.; Ferrer, R.; Kumar, A.; Sevransky, J.E.; Sprung, C.L.; Nunnally, M.E.; et al. Surviving sepsis campaign: International guidelines for management of sepsis and septic shock 2016. Crit. Care Med. 2017, 45, 486–552. [Google Scholar] [CrossRef] [PubMed]
- Williams, T.A.; Martin, R.; Celenza, A.; Bremner, A.; Fatovich, D.; Krause, J.; Arena, S.; Finn, J. Use of serum lactate levels to predict survival for patients with out-of-hospital cardiac arrest: A cohort study. Emerg. Med. Australas. 2016, 28, 171–178. [Google Scholar] [CrossRef]
- Hermanides, J.; Plummer, M.P.; Finnis, M.; Deane, A.M.; Coles, J.P.; Menon, D.K. Glycaemic control targets after traumatic brain injury: A systematic review and meta-analysis. Crit. Care 2018, 22, 11. [Google Scholar] [CrossRef] [PubMed]
- Jansen, T.C.; van Bommel, J.; Schoonderbeek, F.J.; Sleeswijk Visser, S.J.; van der Klooster, J.M.; Lima, A.P.; Willemsen, S.P.; Bakker, J.; LACTATE Study Group. Early lactate-guided therapy in intensive care unit patients: A multicenter, open-label, randomized controlled trial. Am. J. Respir. Crit. Care Med. 2010, 182, 752–761. [Google Scholar] [CrossRef]
- Hernandez, G.; Ospina-Tascon, G.A.; Damiani, L.P.; Estenssoro, E.; Dubin, A.; Hurtado, J.; Friedman, G.; Castro, R.; Alegria, L.; Teboul, J.L.; et al. Effect of a resuscitation strategy targeting peripheral perfusion status vs. serum lactate levels on 28-day mortality among patients with septic shock: The ANDROMEDA-SHOCK randomized clinical trial. JAMA 2019, 321, 654–664. [Google Scholar] [CrossRef] [PubMed]
- Cecconi, M.; De Backer, D.; Antonelli, M.; Beale, R.; Bakker, J.; Hofer, C.; Jaeschke, R.; Mebazaa, A.; Pinsky, M.R.; Teboul, J.L.; et al. Consensus on circulatory shock and hemodynamic monitoring. Task force of the European society of intensive care medicine. Intensive Care Med. 2014, 40, 1795–1815. [Google Scholar] [CrossRef] [PubMed]
- Van der Jagt, M. Fluid management of the neurological patient: A concise review. Crit. Care 2016, 20, 126. [Google Scholar] [CrossRef]
- Francoeur, C.L.; Mayer, S.A. Management of delayed cerebral ischemia after subarachnoid hemorrhage. Crit. Care 2016, 20, 277. [Google Scholar] [CrossRef]
- Alali, A.S.; McCredie, V.A.; Golan, E.; Shah, P.S.; Nathens, A.B. Beta blockers for acute traumatic brain injury: A systematic review and meta-analysis. Neurocritical Care 2014, 20, 514–523. [Google Scholar] [CrossRef]
| All Patients | FO | UO | p-Value | Survivors | Non-Survivors | p-Value | |
|---|---|---|---|---|---|---|---|
| (n = 456) | (n = 247) | (n = 209) | (n = 298) | (n = 158) | |||
| Age (years), median (IQR) | 54 (46–63) | 51 (43–59) | 56 (48–67) | <0.01 | 52 (44–60) | 56 (47–67) | <0.01 |
| Female, n (%) | 290 (64) | 153 (62) | 137 (66) | 0.44 | 187 (63) | 103 (64) | 0.84 |
| GCS, median (IQR) | 13 (3–15) | 15 (13–15) | 4 (3–12) | <0.01 | 15 (10–15) | 3 (3–9) | <0.01 |
| Fisher 3–4, n (%) | 419 (94) | 145 (60) | 184 (89) | <0.01 | 145 (60) | 184 (89) | <0.01 |
| WFNS 4–5, n (%) | 216 (47) | 57 (23) | 159 (76) | <0.01 | 57 (23) | 159 (76) | <0.01 |
| SOFA, median (IQR) | 5 (2–8) | 2 (1–4) | 8 (5–10) | <0.01 | 2 (1–5) | 8 (6–10) | <0.01 |
| APACHE II, median (IQR) | 13 (8–19) | 8 (6–12) | 19 (14–22) | <0.01 | 9 (7–15) | 19 (16–22) | <0.01 |
| Comorbidities | |||||||
| Hypertension, n (%) | 191 (42) | 111 (45) | 80 (38) | 0.15 | 134 (45) | 57 (36) | 0.05 |
| Diabetes, n (%) | 38 (8) | 13 (5) | 25 (12) | 0.01 | 22 (7) | 16 (10) | 0.38 |
| Heart disease, n (%) | 54 (12) | 20 (8) | 34 (16) | 0.01 | 27 (9) | 27 (17) | 0.02 |
| Neurologic disease, n (%) | 34 (8) | 7 (17) | 8 (17) | 0.72 | 19 (6) | 15 (9) | 0.27 |
| Kidney disease, n (%) | 8 (2) | 5 (2) | 3 (1) | 0.73 | 6 (2) | 2 (1) | 0.72 |
| Asthma/COPD, n (%) | 37 (8) | 16 (7) | 21 (10) | 0.17 | 18 (6) | 19 (12) | 0.03 |
| Cancer, n (%) | 22 (5) | 11 (5) | 11 (5) | 0.83 | 11 (4) | 11 (7) | 0.17 |
| Cirrhosis, n (%) | 5 (1) | 1 (0.4) | 4 (2) | 0.18 | 1 (0.3) | 4 (3) | 0.05 |
| Treatments | |||||||
| Vasopressors, n (%) | 249 (55) | 71 (29) | 178 (85) | <0.01 | 25 (8) | 43 (27) | <0.01 |
| Inotropes, n (%) | 68 (15) | 14 (6) | 54 (26) | <0.01 | 113 (38) | 136 (85) | <0.01 |
| MV, n (%) | 268 (59) | 77 (31) | 192 (92) | <0.01 | 115 (39) | 154 (96) | <0.01 |
| Endovascular coiling, n (%) | 336 (74) | 215 (87) | 121 (58) | <0.01 | 256 (87) | 80 (50) | <0.01 |
| Surgical clipping, n (%) | 72 (16) | 29 (12) | 43 (21) | 0.01 | 39 (13) | 33 (21) | 0.04 |
| Complications | |||||||
| Hypotension *, n (%) | 356 (78) | 199 (81) | 157 (75) | 0.17 | 227 (76) | 129 (82) | 0.19 |
| Rebleeding, n (%) | 33 (7) | 4 (2) | 29 (14) | <0.01 | 8 (3) | 25 (16) | <0.01 |
| DCI, n (%) | 94 (21) | 25 (10) | 69 (33) | <0.01 | 45 (15) | 49 (31) | <0.01 |
| ICHT, n (%) | 192 (42) | 34 (14) | 158 (76) | <0.01 | 59 (20) | 133 (83) | <0.01 |
| Seizures, n (%) | 110 (24) | 46 (19) | 64 (31) | <0.01 | 69 (23) | 41 (26) | 0.65 |
| Hydrocephalus, n (%) | 148 (33) | 58 (24) | 90 (43) | <0.01 | 81 (27) | 42 (67) | <0.01 |
| All Patients | FO | UO | p-Value | Survivors | Non-Survivors | p-Value | |
|---|---|---|---|---|---|---|---|
| (n = 456) | (n = 247) | (n = 209) | (n = 298) | (n = 158) | |||
| Peak lactate concentration, median (IQR) | 2.7 (1.8–3.9) | 2.1 (1.5–2.9) | 3.5 (2.5–4.9) | <0.01 | 2.3 (1.6–3.0) | 3.7 (2.7–5.2) | <0.01 |
| Hyperlactatemia in the first 24h of ICU admission, n (%) | 234 (51) | 85 (34) | 149 (71) | <0.01 | 59 (20) | 90 (157) | <0.01 |
| Hyperlactatemia in the first 6 days of ICU stay, n (%) | 310 (68) | 129 (52) | 181 (87) | <0.01 | 171 (57) | 139 (88) | <0.01 |
| Highest serum lactate day 1-mmol/L, median (IQR) | 2.1 (1.2–3.2) | 129 (52) | 181 (87) | <0.01 | 1.7 (1–2.7) | 3.1 (2.1–4.4) | <0.01 |
| Highest serum lactate day 2-mmol/L, median (IQR) | 1.9 (1.4–2.6) | 1.5 (0.9–2.6) | 2.9 (1.9–4.1) | <0.01 | 1.6 (1–2.3) | 2.4 (1.8–3.8) | <0.01 |
| Highest serum lactate day 3-mmol/L, median (IQR) | 1.4 (1.1–1.8) | 1.5 (1–2.1) | 2.3 (1.7–3.2) | <0.01 | 1.2 (0.9–1.6) | 1.7 (1.3–2.1) | <0.01 |
| Highest serum lactate day 4-mmol/L, median (IQR) | 1.3 (1.0–1.8) | 1.1 (0.9–1.6) | 1.6 (1.2–2) | <0.01 | 1.2 (0.9–1.5) | 1.5 (1.1–2.1) | <0.01 |
| Highest serum lactate day 5-mmol/L, median (IQR) | 1.2 (0.9–1.6) | 1.2 (0.9–1.5) | 1.4 (1.1–2) | <0.01 | 1.1 (0.9–1.5) | 1.3 (1.1–1.8) | <0.01 |
| Highest serum lactate day 6-mmol/L, median (IQR) | 1.2 (0.9–1.5) | 1.1 (0.8–1.3) | 1.4 (1.1–1.8) | <0.01 | 1.1 (0.9–1.4) | 1.3 (1–1.7) | <0.01 |
| Peak glucose-mg/dL, median (IQR) | 188 (157–231) | 171(146-204) | 214 (180-265) | <0.01 | 176 (149–210) | 218 (180–267) | <0.01 |
| Hyperglycemia in the first 24 h of ICU admission, n (%) | 121 (27) | 33 (13) | 88 (42) | <0.01 | 46 (15) | 75 (48) | <0.01 |
| Hyperglycemia in the first 6 days of ICU admission, n (%) | 256 (56) | 101 (41) | 155 (74) | <0.01 | 248 (83) | 155 (98) | <0.01 |
| Highest blood glucose day 1-mg/dL, median (IQR) | 157 (131–188) | 149 (123–176) | 167 (142–203) | <0.01 | 150 (125–181) | 171 (148–206) | <0.01 |
| Highest blood glucose day 2-mg/dL, median (IQR) | 154 (133–183) | 149 (127–166) | 163 (138–193) | <0.01 | 151 (131–177) | 163 (139–198) | <0.01 |
| Highest blood glucose day 3-mg/dL, median (IQR) | 148 (126–167) | 148 (127–163) | 149 (126–172) | <0.01 | 149 (127–167) | 143 (123–165) | <0.01 |
| Highest blood glucose day 4-mg/dL, median (IQR) | 149 (130–188) | 147 (126–189) | 156 (134–187) | 0.03 | 148 (127–189) | 155 (137–187) | <0.12 |
| Highest blood glucose day 5-mg/dL, median (IQR) | 152 (129–186) | 151(123–174) | 156 (137–192) | <0.01 | 151 (127–181) | 160 (138–192) | 0.02 |
| Highest blood glucose day 6-mg/dL, median (IQR) | 149 (128–176) | 143 (126–170) | 156 (129–179) | 0.27 | 148 (127–176) | 150 (129–178) | 0.93 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ndieugnou Djangang, N.; Ramunno, P.; Izzi, A.; Garufi, A.; Menozzi, M.; Diaferia, D.; Peluso, L.; Prezioso, C.; Talamonti, M.; Njimi, H.; et al. The Prognostic Role of Lactate Concentrations after Aneurysmal Subarachnoid Hemorrhage. Brain Sci. 2020, 10, 1004. https://doi.org/10.3390/brainsci10121004
Ndieugnou Djangang N, Ramunno P, Izzi A, Garufi A, Menozzi M, Diaferia D, Peluso L, Prezioso C, Talamonti M, Njimi H, et al. The Prognostic Role of Lactate Concentrations after Aneurysmal Subarachnoid Hemorrhage. Brain Sciences. 2020; 10(12):1004. https://doi.org/10.3390/brainsci10121004
Chicago/Turabian StyleNdieugnou Djangang, Narcisse, Pamela Ramunno, Antonio Izzi, Alessandra Garufi, Marco Menozzi, Daniela Diaferia, Lorenzo Peluso, Chiara Prezioso, Marta Talamonti, Hassane Njimi, and et al. 2020. "The Prognostic Role of Lactate Concentrations after Aneurysmal Subarachnoid Hemorrhage" Brain Sciences 10, no. 12: 1004. https://doi.org/10.3390/brainsci10121004
APA StyleNdieugnou Djangang, N., Ramunno, P., Izzi, A., Garufi, A., Menozzi, M., Diaferia, D., Peluso, L., Prezioso, C., Talamonti, M., Njimi, H., Schuind, S., Vincent, J.-L., Creteur, J., Taccone, F. S., & Gouvea Bogossian, E. (2020). The Prognostic Role of Lactate Concentrations after Aneurysmal Subarachnoid Hemorrhage. Brain Sciences, 10(12), 1004. https://doi.org/10.3390/brainsci10121004







