A Review of Accelerated Long-Term Forgetting in Epilepsy
Abstract
:1. Introduction
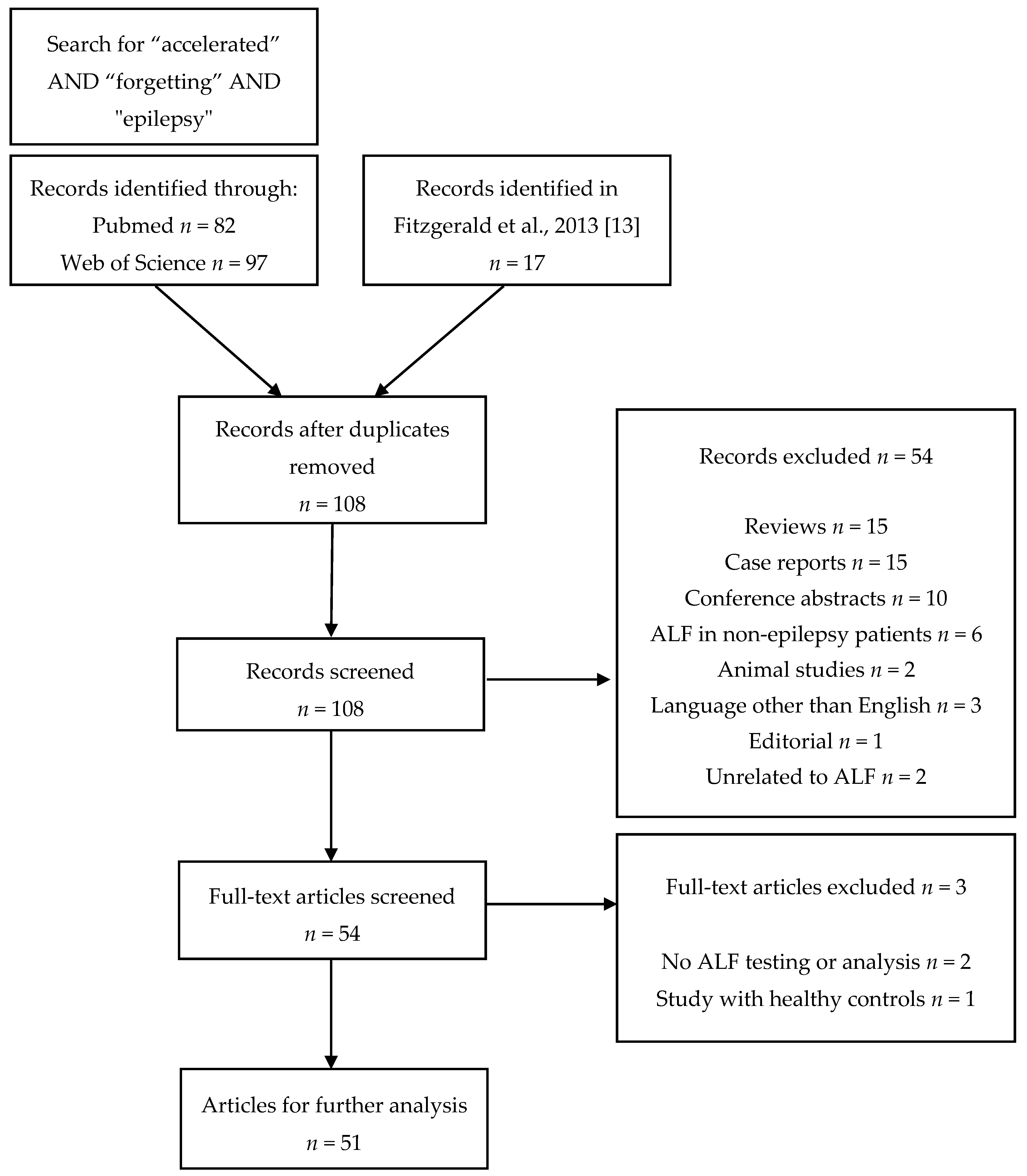
2. Search Strategy and Results
3. ALF in Different Seizure Disorders
3.1. ALF in TLE—The Relation with Structural, Clinical, and EEG Variables
3.1.1. The Hippocampus and ALF
3.1.2. Material Specificity in ALF
3.1.3. Seizures and Epileptiform Activity
3.2. ALF in TEA—The Potential Importance of Subtle Cortical Dysfunction
3.2.1. Clinical Characteristics of TEA
3.2.2. Neuropsychological Testing Results
3.2.3. Imaging Findings
3.3. Focal Extratemporal Epilepsy and ALF
3.4. ALF in GGE
4. ALF as a Late Consolidation Impairment
4.1. ALF in Non-Epileptic Disorders
4.2. Theoretical Grounds for Disrupted Long-Term Consolidation in ALF
4.3. Is Seizure Activity or Structural Damage Essential to Cause ALF?
5. Translating the Research of ALF in Epilepsy to the Clinical Setting
5.1. Detecting ALF in Clinical Practice
5.2. Treating Patients with ALF
5.3. Memory Rehabilitation
6. Conclusions
6.1. Do Memory Studies in Patients with Epilepsy Reveal a Possible Localization of ALF?
6.2. ALF as a Reflection of Impaired Late Memory Consolidation
6.3. Future Directions of ALF Research and Its Detection in Clinical Practice
6.4. Final Remarks
Author Contributions
Funding
Conflicts of Interest
References
- van Rijckevorsel, K. Cognitive Problems Related to Epilepsy Syndromes, Especially Malignant Epilepsies. Seizure 2006, 15, 227–234. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hendriks, M.P.H.; Aldenkamp, A.P.; Van Der Vlugt, H.; Alpherts, W.C.J.; Vermeulen, J. Memory Complaints in Medically Refractory Epilepsy: Relationship to Epilepsy-Related Factors. Epilepsy Behav. 2002, 3, 165–172. [Google Scholar] [CrossRef] [PubMed]
- Baker, J.; Zeman, A. Accelerated Long-Term Forgetting in Epilepsy—And Beyond. Eye Mov. Res. 2017, 401–417. [Google Scholar] [CrossRef]
- Zeman, A.; Butler, C. Transient Epileptic Amnesia. Curr. Opin. Neurol. 2010, 23, 610–616. [Google Scholar] [CrossRef] [PubMed]
- Muhlert, N.; Grünewald, R.A.; Hunkin, N.M.; Reuber, M.; Howell, S.; Reynders, H.; Isaac, C.L. Accelerated Long-Term Forgetting in Temporal Lobe but Not Idiopathic Generalised Epilepsy. Neuropsychologia 2011, 49, 2417–2426. [Google Scholar] [CrossRef] [PubMed]
- Fitzgerald, Z.; Thayer, Z.; Mohamed, A.; Miller, L.A. Examining Factors Related to Accelerated Long-Term Forgetting in Epilepsy Using Ambulatory EEG Monitoring. Epilepsia 2013, 54, 819–827. [Google Scholar] [CrossRef]
- Grayson-Collins, J.; Gascoigne, M.B.; Barton, B.; Webster, R.; Gill, D.; Lah, S. Longitudinal Study of Accelerated Long-Term Forgetting in Children with Genetic Generalized Epilepsy: Evidence of Ongoing Deficits. Cortex 2019, 110, 5–15. [Google Scholar] [CrossRef]
- Tramoni-Nègre, E.; Lambert, I.; Bartolomei, F.; Felician, O. Long-Term Memory Deficits in Temporal Lobe Epilepsy. Rev. Neurol. 2017, 173, 490–497. [Google Scholar] [CrossRef]
- Huijgen, J.; Samson, S. The Hippocampus: A Central Node in a Large-Scale Brain Network for Memory. Rev. Neurol. 2015, 171, 204–216. [Google Scholar] [CrossRef]
- Elliott, G.; Isaac, C.L.; Muhlert, N. Measuring Forgetting: A Critical Review of Accelerated Long-Term Forgetting Studies. Cortex 2014, 54, 16–32. [Google Scholar] [CrossRef]
- Cassel, A.; Kopelman, M.D. Have We Forgotten about Forgetting? A Critical Review of ‘accelerated Long-Term forgetting’ in Temporal Lobe Epilepsy. Cortex 2019, 110, 141–149. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mayes, A.R.; Hunkin, N.M.; Isaac, C.; Muhlert, N. Are There Distinct Forms of Accelerated Forgetting And, If So, Why? Cortex 2019, 110, 115–126. [Google Scholar] [CrossRef]
- Fitzgerald, Z.; Mohamed, A.; Ricci, M.; Thayer, Z.; Miller, L. Accelerated Long-Term Forgetting: A Newly Identified Memory Impairment in Epilepsy. J. Clin. Neurosci. 2013, 20, 1486–1491. [Google Scholar] [CrossRef] [PubMed]
- Butler, C.R.; Gilboa, A.; Miller, L. Accelerated Long-Term Forgetting. Cortex 2019, 110, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Djordjevic, J.; Smith, M.L.; Sziklas, V.; Piper, D.; Pénicaud, S.; Jones-Gotman, M. The Story Learning and Memory (SLAM) Test: Equivalence of Three Forms and Sensitivity to Left Temporal Lobe Dysfunction. Epilepsy Behav. 2011, 20, 518–523. [Google Scholar] [CrossRef] [PubMed]
- Mameniškienė, R.; Jatužis, D.; Kaubrys, G.; Budrys, V. The Decay of Memory between Delayed and Long-Term Recall in Patients with Temporal Lobe Epilepsy. Epilepsy Behav. 2006, 8, 278–288. [Google Scholar] [CrossRef] [PubMed]
- Helmstaedter, C.; Hauff, M.; Elger, C.E. Ecological Validity of List-Learning Tests and Self-Reported Memory in Healthy Individuals and Those with Temporal Lobe Epilepsy. J. Clin. Exp. Neuropsychol. 1998, 20, 365–375. [Google Scholar] [CrossRef]
- Polat, B.; Yılmaz, N.H.; Mantar, N.; Cadirci, F.; Sitrava, S.; Ozmansur, E.N.; Uzan, M.; Özkara, C.; Hanoglu, L. Accelerated Long-Term Forgetting After Amygdalohippocampectomy in Temporal Lobe Epilepsy. J. Clin. Neurosci. 2020, 72, 43–49. [Google Scholar] [CrossRef]
- Bengner, T.; Malina, T.; Lindenau, M.; Voges, B.; Goebell, E.; Stodieck, S. Face Memory in MRI-Positive and MRI-Negative Temporal Lobe Epilepsy. Epilepsia 2006, 47, 1904–1914. [Google Scholar] [CrossRef]
- Bell, B.D.; Fine, J.; Dow, C.; Seidenberg, M.; Hermann, B.P. Temporal Lobe Epilepsy and the Selective Reminding Test: The Conventional 30-Minute Delay Suffices. Psychol. Assess. 2005, 17, 103–109. [Google Scholar] [CrossRef] [Green Version]
- Helmstaedter, C.; Winter, B.; Melzer, N.; Lohmann, H.; Witt, J.-A. Accelerated Long-Term Forgetting in Focal Epilepsies with Special Consideration Given to Patients with Diagnosed and Suspected Limbic Encephalitis. Cortex 2019, 110, 58–68. [Google Scholar] [CrossRef] [PubMed]
- Visser, M.; Forn, C.; Gómez-Ibáñez, A.; Rosell-Negre, P.; Villanueva, V.; Ávila, C. Accelerated Long-Term Forgetting in Resected and Seizure-Free Temporal Lobe Epilepsy Patients. Cortex 2019, 110, 80–91. [Google Scholar] [CrossRef] [PubMed]
- Miller, L.A.; Mothakunnel, A.; Flanagan, E.; Nikpour, A.; Thayer, Z. Accelerated Long Term Forgetting in Patients with Focal Seizures: Incidence Rate and Contributing Factors. Epilepsy Behav. 2017, 72, 108–113. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Giovagnoli, A.R.; Casazza, M.; Avanzini, G. Visual Learning on a Selective Reminding Procedure and Delayed Recall in Patients with Temporal Lobe Epilepsy. Epilepsia 1995, 36, 704–711. [Google Scholar] [CrossRef]
- Wilkinson, H.; Holdstock, J.S.; Baker, G.; Herbert, A.; Clague, F.; Downes, J.J. Long-Term Accelerated Forgetting of Verbal and Non-Verbal Information in Temporal Lobe Epilepsy. Cortex 2012, 48, 317–332. [Google Scholar] [CrossRef]
- Bell, B.D. WMS-III Logical Memory Performance After a Two-Week Delay in Temporal Lobe Epilepsy and Control Groups. J. Clin. Exp. Neuropsychol. 2007, 28, 1435–1443. [Google Scholar] [CrossRef] [Green Version]
- Audrain, S.P.; McAndrews, M.P. Cognitive and Functional Correlates of Accelerated Long-Term Forgetting in Temporal Lobe Epilepsy. Cortex 2019, 110, 101–114. [Google Scholar] [CrossRef]
- Gascoigne, M.; Smith, M.L.; Barton, B.; Webster, R.; Gill, D.; Lah, S. Accelerated Long-Term Forgetting and Behavioural Difficulties in Children with Epilepsy. Cortex 2019, 110, 92–100. [Google Scholar] [CrossRef]
- Lah, S.; Mohamed, A.; Thayer, Z.; Miller, L.; Diamond, K. Accelerated Long-Term Forgetting of Verbal Information in Unilateral Temporal Lobe Epilepsy: Is It Related to Structural Hippocampal Abnormalities and/Or Incomplete Learning? J. Clin. Exp. Neuropsychol. 2014, 36, 158–169. [Google Scholar] [CrossRef]
- Gascoigne, M.B.; Smith, M.; Barton, B.; Webster, R.; Gill, D.; Lah, S. Accelerated Long-Term Forgetting in Children with Temporal Lobe Epilepsy. Neuropsychologia 2014, 59, 93–102. [Google Scholar] [CrossRef]
- Ricci, M.; Mohamed, A.; Savage, G.; Miller, L.A.; Savage, G. Disruption of Learning and Long-Term Retention of Prose Passages in Patients with Focal Epilepsy. Epilepsy Behav. 2015, 51, 104–111. [Google Scholar] [CrossRef] [PubMed]
- Ricci, M.; Mohamed, A.; Savage, G.; Boserio, J.; Miller, L.A.; Savage, G. The Impact of Epileptiform Abnormalities and Hippocampal Lesions on Retention of Recent Autobiographical Experiences: Adding Insult to Injury? Neuropsychologia 2015, 66, 259–266. [Google Scholar] [CrossRef] [PubMed]
- Martin, R.C.; Loring, D.W.; Meador, K.; Lee, G.P.; Thrash, N.; Arena, J.G. Impaired Long-Term Retention Despite Normal Verbal Learning in Patients with Temporal Lobe Dysfunction. Neuropsychology 1991, 5, 3–12. [Google Scholar] [CrossRef]
- Barkas, L.; Redhead, E.; Taylor, M.; Shtaya, A.; Hamilton, D.A.; Gray, W.P. Fluoxetine Restores Spatial Learning but Not Accelerated Forgetting in Mesial Temporal Lobe Epilepsy. Brain 2012, 135, 2358–2374. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cassel, A.; Morris, R.; Koutroumanidis, M.; Kopelman, M. Forgetting in Temporal Lobe Epilepsy: When Does It Become Accelerated? Cortex 2016, 78, 70–84. [Google Scholar] [CrossRef] [Green Version]
- Narayanan, J.; Duncan, R.; Greene, J.; Leach, J.P.; Razvi, S.; McLean, J.; Evans, J.J. Accelerated Long-Term Forgetting in Temporal Lobe Epilepsy: Verbal, Nonverbal and Autobiographical Memory. Epilepsy Behav. 2012, 25, 622–630. [Google Scholar] [CrossRef]
- Blake, R.V.; Wroe, S.J.; Breen, E.K.; McCarthy, R.A. Accelerated Forgetting in Patients with Epilepsy: Evidence for an Impairment in Memory Consolidation. Brain 2000, 123, 472–483. [Google Scholar] [CrossRef]
- Miller, L.A.; Flanagan, E.; Mothakunnel, A.; Mohamed, A.; Thayer, Z. Old Dogs with New Tricks: Detecting Accelerated Long-Term Forgetting by Extending Traditional Measures. Epilepsy Behav. 2015, 45, 205–211. [Google Scholar] [CrossRef]
- Evans, S.J.; Elliott, G.; Reynders, H.; Isaac, C.L. Can Temporal Lobe Epilepsy Surgery Ameliorate Accelerated Long-Term Forgetting? Neuropsycholia 2014, 53, 64–74. [Google Scholar] [CrossRef]
- Deak, M.C.; Stickgold, R.; Pietras, A.C.; Nelson, A.P.; Bubrick, E.J. The Role of Sleep in Forgetting in Temporal Lobe Epilepsy: A Pilot Study. Epilepsy Behav. 2011, 21, 462–466. [Google Scholar] [CrossRef] [Green Version]
- Contador, I.; Sánchez, A.; Kopelman, M.D.; De La Aleja, J.G. Long-Term Forgetting in Temporal Lobe Epilepsy: Is This Phenomenon a Norm? Epilepsy Behav. 2017, 77, 30–32. [Google Scholar] [CrossRef] [PubMed]
- Tramoni-Nègre, E.; Felician, O.; Barbeau, E.; Guedj, E.; Guye, M.; Bartolomei, F.; Ceccaldi, M. Long-Term Consolidation of Declarative Memory: Insight from Temporal Lobe Epilepsy. Brain 2011, 134, 816–831. [Google Scholar] [CrossRef] [PubMed]
- Savage, S.A.; Butler, C.R.; Milton, F.; Han, Y.; Zeman, A. On the Nose: Olfactory Disturbances in Patients with Transient Epileptic Amnesia. Epilepsy Behav. 2017, 66, 113–119. [Google Scholar] [CrossRef] [PubMed]
- Mosbah, A.; Tramoni-Nègre, E.; Guedj, E.; Aubert, S.; Daquin, G.; Ceccaldi, M.; Felician, O.; Bartolomei, F. Clinical, Neuropsychological, and Metabolic Characteristics of Transient Epileptic Amnesia Syndrome. Epilepsia 2014, 55, 699–706. [Google Scholar] [CrossRef] [PubMed]
- Hoefeijzers, S.; Zeman, A.; Della Sala, S.; Dewar, M. Capturing Real-Life Forgetting in Transient Epileptic Amnesia via an Incidental Memory Test. Cortex 2019, 110, 47–57. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Butler, C.R.; Graham, K.S.; Hodges, J.; Kapur, N.; Wardlaw, J.M.; Zeman, A. The Syndrome of Transient Epileptic Amnesia. Ann. Neurol. 2007, 61, 587–598. [Google Scholar] [CrossRef]
- Butler, C.R.; Van Erp, W.; Bhaduri, A.; Hammers, A.; Heckemann, R.; Zeman, A. Magnetic Resonance Volumetry Reveals Focal Brain Atrophy in Transient Epileptic Amnesia. Epilepsy Behav. 2013, 28, 363–369. [Google Scholar] [CrossRef]
- Butler, C.R.; Bhaduri, A.; Acosta-Cabronero, J.; Nestor, P.J.; Kapur, N.; Graham, K.S.; John, R.H.; Zeman, A.Z. Transient Epileptic Amnesia: Regional Brain Atrophy and Its Relationship to Memory Deficits. Brain 2009, 132, 357–368. [Google Scholar] [CrossRef] [Green Version]
- Dewar, M.; Hoefeijzers, S.; Zeman, A.Z.J.; Butler, C.; Della Sala, S. Impaired Picture Recognition in Transient Epileptic Amnesia. Epilepsy Behav. 2015, 42, 107–116. [Google Scholar] [CrossRef]
- Butler, C.; Kapur, N.; Zeman, A.; Weller, R.; Connelly, A. Epilepsy-Related Long-Term Amnesia: Anatomical Perspectives. Neuropsychologia 2012, 50, 2973–2980. [Google Scholar] [CrossRef]
- Hoefeijzers, S.; Dewar, M.; Della Sala, S.; Zeman, A.; Butler, C. Accelerated Long-Term Forgetting in Transient Epileptic Amnesia: An Acquisition or Consolidation Deficit? Neuropsychologia 2013, 51, 1549–1555. [Google Scholar] [CrossRef] [PubMed]
- Atherton, K.E.; Filippini, N.; Zeman, A.Z.; Nobre, A.C.; Butler, C.R. Encoding-Related Brain Activity and Accelerated Forgetting in Transient Epileptic Amnesia. Cortex 2019, 110, 127–140. [Google Scholar] [CrossRef] [PubMed]
- Savage, S.A.; Hoefeijzers, S.; Milton, F.; Streatfield, C.; Dewar, M.; Zeman, A. The Evolution of Accelerated Long-Term Forgetting: Evidence from the TIME Study. Cortex 2017, 110, 16–36. [Google Scholar] [CrossRef] [PubMed]
- Hoefeijzers, S.; Dewar, M.; Della Sala, S.; Butler, C.; Zeman, A.Z.J. Accelerated Long-Term Forgetting Can Become Apparent Within 3–8 Hours of Wakefulness in Patients with Transient Epileptic Amnesia. Neuropsychology 2015, 29, 117–125. [Google Scholar] [CrossRef]
- Atherton, K.E.; Nobre, A.C.; Zeman, A.; Butler, C.R. Sleep-Dependent Memory Consolidation and Accelerated Forgetting. Cortex 2014, 54, 92–105. [Google Scholar] [CrossRef] [Green Version]
- Atherton, K.E.; Nobre, A.C.; Lazar, A.S.; Wulff, K.; Whittaker, R.G.; Dhawan, V.; Lazar, Z.I.; Zeman, A.; Butler, C.R. Slow Wave Sleep and Accelerated Forgetting. Cortex 2016, 84, 80–89. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Muhlert, N.; Milton, F.; Butler, C.; Kapur, N.; Zeman, A. Accelerated Forgetting of Real-Life Events in Transient Epileptic Amnesia. Neuropsycholia 2010, 48, 3235–3244. [Google Scholar] [CrossRef]
- Manes, F.; Graham, K.S.; Zeman, A.; Calcagno, M.D.L.; Hodges, J. Autobiographical Amnesia and Accelerated Forgetting in Transient Epileptic Amnesia. J. Neurol. Neurosurg. Psychiatry 2005, 76, 1387–1391. [Google Scholar] [CrossRef]
- Davidson, M.; Dorris, L.; O’Regan, M.; Zuberi, S.M. Memory Consolidation and Accelerated Forgetting in Children with Idiopathic Generalized Epilepsy. Epilepsy Behav. 2007, 11, 394–400. [Google Scholar] [CrossRef] [PubMed]
- Gascoigne, M.B.; Barton, B.; Webster, R.; Gill, D.; Antony, J.; Lah, S.S. Accelerated Long-Term Forgetting in Children with Idiopathic Generalized Epilepsy. Epilepsia 2012, 53, 2135–2140. [Google Scholar] [CrossRef]
- Beilharz, J.E.; Thayer, Z.; Nikpour, A.; Lah, S. Accelerated Long-Term Forgetting Is Not Evident in Adults With Genetic Generalized Epilepsy Irrespective of the Paradigm Used. Epilepsy Behav. 2020, 104, 106920. [Google Scholar] [CrossRef] [PubMed]
- Ricci, M.; Wong, T.; Nikpour, A.; Miller, L.A. Testing the Effectiveness of Cognitive Interventions in Alleviating Accelerated Long Term Forgetting (ALF). Cortex 2019, 110, 37–46. [Google Scholar] [CrossRef] [PubMed]
- Skidmore, C.T. Adult Focal Epilepsies. Contin. Lifelong Learn. Neurol. 2016, 22, 94–115. [Google Scholar] [CrossRef] [PubMed]
- Gallassi, R.; Sambati, L.; Poda, R.; Stanzani-Maserati, M.; Oppi, F.; Giulioni, M.; Tinuper, P. Accelerated Long-Term Forgetting in Temporal Lobe Epilepsy: Evidence of Improvement After Left Temporal Pole Lobectomy. Epilepsy Behav. 2011, 22, 793–795. [Google Scholar] [CrossRef]
- Bonelli, S.; Thompson, P.J.; Yogarajah, M.; Powell, H.W.R.; Samson, R.S.; McEvoy, A.W.; Symms, M.R.; Koepp, M.J.; Duncan, J.S. Memory Reorganization Following Anterior Temporal Lobe Resection: A Longitudinal Functional MRI Study. Brain 2013, 136, 1889–1900. [Google Scholar] [CrossRef]
- Hirokawa, Y.; Fujimoto, A.; Ichikawa, N.; Sato, K.; Tanaka, T.; Enoki, H.; Otsuki, Y.; Okanishi, T. Temporal Lobe Cavernous Malformation Caused Epileptic Amnesic Episodes and Mild Cognitive Impairment. Front. Neurol. 2019, 10, 1–6. [Google Scholar] [CrossRef]
- Lam, A.D.; Deck, G.; Goldman, A.; Eskandar, E.N.; Noebels, J.; Cole, A.J. Silent Hippocampal Seizures and Spikes Identified by Foramen Ovale Electrodes in Alzheimer’s Disease. Nat. Med. 2017, 23, 678–680. [Google Scholar] [CrossRef]
- Holmes, M.J.; Folley, B.S.; Sonmezturk, H.H.; Gore, J.C.; Kang, H.; Abou-Khalil, B.; Morgan, V.L. Resting State Functional Connectivity of the Hippocampus Associated with Neurocognitive Function in Left Temporal Lobe Epilepsy. Hum. Brain Mapp. 2012, 35, 735–744. [Google Scholar] [CrossRef] [Green Version]
- Cabeza, R.; Nyberg, L. Imaging Cognition II: An Empirical Review of 275 PET and FMRI Studies. J. Cogn. Neurosci. 2000, 12, 1–47. [Google Scholar] [CrossRef]
- Saddiki, N.; Hennion, S.; Viard, R.; Ramdane, N.; Lopes, R.; Baroncini, M.; Szurhaj, W.; Reyns, N.; Pruvo, J.P.; Delmaire, C. Encoding and Immediate Retrieval Tasks in Patients With Epilepsy: A Functional MRI Study of Verbal and Visual Memory. J. Neuroradiol. 2018, 45, 157–163. [Google Scholar] [CrossRef]
- Golby, A.J.; Poldrack, R.A.; Illes, J.; Chen, D.; Desmond, J.E.; Gabrieli, J.D.E. Memory Lateralization in Medial Temporal Lobe Epilepsy Assessed by Functional MRI. Epilepsia 2002, 43, 855–863. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Helmstaedter, C. Cognitive Outcomes of Different Surgical Approaches in Temporal Lobe Epilepsy. Epileptic Disord. 2013, 15, 221–239. [Google Scholar] [CrossRef] [PubMed]
- Sherman, E.M.S.; Wiebe, S.; Fay-McClymont, T.B.; Tellez-Zenteno, J.; Metcalfe, A.; Hernandez-Ronquillo, L.; Hader, W.J.; Jetté, N. Neuropsychological Outcomes After Epilepsy Surgery: Systematic Review and Pooled Estimates. Epilepsia 2011, 52, 857–869. [Google Scholar] [CrossRef] [PubMed]
- McConley, R.; Martin, R.; Palmer, C.A.; Kuzniecky, R.; Knowlton, R.; Faught, E. Rey Osterrieth Complex Figure Test Spatial and Figural Scoring: Relations to Seizure Focus and Hippocampal Pathology in Patients with Temporal Lobe Epilepsy. Epilepsy Behav. 2008, 13, 174–177. [Google Scholar] [CrossRef]
- Helmstaedter, C.; Kurthen, M.; Linke, D.B.; Elger, C.E. Right Hemisphere Restitution of Language and Memory Functions in Right Hemisphere Language-Dominant Patients with Left Temporal Lobe Epilepsy. Brain 1994, 117, 729–737. [Google Scholar] [CrossRef]
- Helmstaedter, C.; Fritz, N.; Pérez, P.G.; Elger, C.; Weber, B. Shift-Back of Right into Left Hemisphere Language Dominance After Control of Epileptic Seizures: Evidence for Epilepsy Driven Functional Cerebral Organization. Epilepsy Res. 2006, 70, 257–262. [Google Scholar] [CrossRef]
- Barr, W.B.; Chelune, G.J.; Hermann, B.P.; Loring, D.W.; Perrine, K.; Strauss, E.; Trenerry, M.R.; Westerveld, M. The Use of Figural Reproduction Tests as Measures of Nonverbal Memory in Epilepsy Surgery Candidates. J. Int. Neuropsychol. Soc. 1997, 3, 435–443. [Google Scholar] [CrossRef]
- Saling, M.M. Verbal Memory in Mesial Temporal Lobe Epilepsy: Beyond Material Specificity. Brain 2009, 132, 570–582. [Google Scholar] [CrossRef]
- Loring, D.W.; Strauss, E.; Hermann, B.P.; Barr, W.B.; Perrine, K.; Trenerry, M.R.; Chelune, G.; Westerveld, M.; Lee, G.P.; Meador, K.J.; et al. Differential Neuropsychological Test Sensitivity to Left Temporal Lobe Epilepsy. J. Int. Neuropsychol. Soc. 2008, 14, 394–400. [Google Scholar] [CrossRef]
- Zeman, A.Z.J.; Boniface, S.J.; Hodges, J.R. Transient Epileptic Amnesia: A Description of the Clinical and Neuropsychological Features in 10 Cases and a Review of the Literature. J. Neurol. Neurosurg. Psychiatry 1998, 64, 435–443. [Google Scholar] [CrossRef] [Green Version]
- Felician, O.; Tramoni, E.; Bartolomei, F. Transient Epileptic Amnesia: Update on a Slowly Emerging Epileptic Syndrome. Rev. Neurol. 2015, 171, 289–297. [Google Scholar] [CrossRef] [PubMed]
- Lemesle, B.; Planton, M.; Pagès, B.; Pariente, J. Accelerated Long-Term Forgetting and Autobiographical Memory Disorders in Temporal Lobe Epilepsy: One Entity or Two? Rev. Neurol. 2017, 173, 498–505. [Google Scholar] [CrossRef] [PubMed]
- Ukai, K.; Watanabe, M. Transient Epileptic Amnesia without Epileptic Seizures: Proposal of a New Entity. Psychogeriatrics 2017, 17, 491–492. [Google Scholar] [CrossRef]
- Asadi-Pooya, A.A. Transient Epileptic Amnesia: A Concise Review. Epilepsy Behav. 2014, 31, 243–245. [Google Scholar] [CrossRef] [PubMed]
- Abarrategui, B.; Parejo-Carbonell, B.; García, M.E.G.; Di Capua, D.; García, M.E.G. The Cognitive Phenotype of Idiopathic Generalized Epilepsy. Epilepsy Behav. 2018, 89, 99–104. [Google Scholar] [CrossRef] [PubMed]
- Loughman, A.; Bowden, S.; D’Souza, W. Cognitive Functioning in Idiopathic Generalised Epilepsies: A Systematic Review and Meta-Analysis. Neurosci. Biobehav. Rev. 2014, 43, 20–34. [Google Scholar] [CrossRef] [PubMed]
- Zimmermann, J.F.; Butler, C.R. Accelerated long-term forgetting in asymptomatic APOE ε4 carriers. Lancet Neurol. 2018, 17, 394–395. [Google Scholar] [CrossRef] [Green Version]
- Geurts, S.; Van Der Werf, S.P.; Kessels, R.P.C. Accelerated Forgetting? An Evaluation on the Use of Long-Term Forgetting Rates in Patients with Memory Problems. Front. Psychol. 2015, 6. [Google Scholar] [CrossRef] [Green Version]
- Weston, P.S.J.; Nicholas, J.M.; Henley, S.M.D.; Liang, Y.; MacPherson, K.; Donnachie, E.; Schott, J.M.; Rossor, M.N.; Crutch, S.J.; Butler, C.R.; et al. Accelerated Long-Term Forgetting in Presymptomatic Autosomal Dominant Alzheimer’s Disease: A Cross-Sectional Study. Lancet Neurol. 2018, 17, 123–132. [Google Scholar] [CrossRef]
- Lah, S.; Black, C.; Gascoigne, M.B.; Gott, C.; Epps, A.; Parry, L. Accelerated Long-Term Forgetting Is Not Epilepsy Specific: Evidence from Childhood Traumatic Brain Injury. J. Neurotrauma 2017, 34, 2536–2544. [Google Scholar] [CrossRef]
- Ward, H.; Shum, D.H.K.; Dick, B.; McKinlay, L.; Baker-Tweney, S. Interview Study of the Effects of Paediatric Traumatic Brain Injury on Memory. Brain Inj. 2004, 18, 471–495. [Google Scholar] [CrossRef] [PubMed]
- Geurts, S.; Van Der Werf, S.P.; Kwa, V.I.; Kessels, R.P. Accelerated Long-Term Forgetting After TIA or Minor Stroke: A More Sensitive Measure for Detecting Subtle Memory Dysfunction? Cortex 2019, 110, 150–156. [Google Scholar] [CrossRef] [PubMed]
- McGaugh, J.L. Memory—A Century of Consolidation. Science 2000, 287, 248–251. [Google Scholar] [CrossRef] [Green Version]
- Dudai, Y.; Karni, A.; Born, J. The Consolidation and Transformation of Memory. Neuron 2015, 88, 20–32. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nadel, L.; Moscovitch, M. Memory Consolidation, Retrograde Amnesia and the Hippocampal Complex. Curr. Opin. Neurobiol. 1997, 7, 217–227. [Google Scholar] [CrossRef]
- Dash, P.K.; Hebert, A.E.; Runyan, J.D. A Unified Theory for Systems and Cellular Memory Consolidation. Brain Res. Rev. 2004, 45, 30–37. [Google Scholar] [CrossRef]
- Morris, R.G.M. Elements of a Neurobiological Theory of Hippocampal Function: The Role of Synaptic Plasticity, Synaptic Tagging and Schemas. Eur. J. Neurosci. 2006, 23, 2829–2846. [Google Scholar] [CrossRef]
- Runyan, J.D.; Moore, A.N.; Dash, P.K. Coordinating What We’ve Learned about Memory Consolidation: Revisiting a Unified Theory. Neurosci. Biobehav. Rev. 2019, 100, 77–84. [Google Scholar] [CrossRef]
- Kandel, E.R.; Dudai, Y.; Mayford, M.R. The Molecular and Systems Biology of Memory. Cell 2014, 157, 163–186. [Google Scholar] [CrossRef] [Green Version]
- McGibbon, T.; Jansari, A.S. Detecting the Onset of Accelerated Long-Term Forgetting: Evidence from Temporal Lobe Epilepsy. Neuropsychologia 2013, 51, 114–122. [Google Scholar] [CrossRef]
- Holmes, G.L. Cognitive Impairment in Epilepsy: The Role of Network Abnormalities. Epileptic Disord. 2015, 17, 101–116. [Google Scholar] [CrossRef] [PubMed]
- Zeman, A.; Butler, C.; Muhlert, N.; Milton, F. Novel Forms of Forgetting in Temporal Lobe Epilepsy. Epilepsy Behav. 2013, 26, 335–342. [Google Scholar] [CrossRef] [PubMed]
- Baddeley, A.; Atkinson, A.; Kemp, S.; Allen, R. The Problem of Detecting Long-Term Forgetting: Evidence from the Crimes Test and the Four Doors Test. Cortex 2019, 110, 69–79. [Google Scholar] [CrossRef] [PubMed]
- Razavi, M.; Barrash, J.; Paradiso, S. A Longitudinal Study of Transient Epileptic Amnesia. Cogn. Behav. Neurol. 2010, 23, 142–145. [Google Scholar] [CrossRef]
- Midorikawa, A.; Kawamura, M. Recovery of Long-Term Anterograde Amnesia, But Not Retrograde Amnesia, After Initiation of an Anti-Epileptic Drug in a Case of Transient Epileptic Amnesia. Neurocase 2008, 13, 385–389. [Google Scholar] [CrossRef]
- Jokeit, H.; Krämer, G.; Ebner, A. Do Antiepileptic Drugs Accelerate Forgetting? Epilepsy Behav. 2005, 6, 430–432. [Google Scholar] [CrossRef]
- Dewar, M.; Alber, J.; Butler, C.; Cowan, N.; Della Sala, S. Brief Wakeful Resting Boosts New Memories Over the Long Term. Psychol. Sci. 2012, 23, 955–960. [Google Scholar] [CrossRef]
- Dewar, M.; Alber, J.; Cowan, N.; Della Sala, S. Boosting Long-Term Memory via Wakeful Rest: Intentional Rehearsal Is Not Necessary, Consolidation Is Sufficient. PLoS ONE 2014, 9, e109542. [Google Scholar] [CrossRef]
- Del Felice, A.; Alderighi, M.; Martinato, M.; Grisafi, D.; Bosco, A.; Thompson, P.J.; Sander, J.W.; Masiero, S. Memory Rehabilitation Strategies in Nonsurgical Temporal Lobe Epilepsy. Am. J. Phys. Med. Rehabil. 2017, 96, 506–514. [Google Scholar] [CrossRef]
- Dubourg, L.; Silva, A.R.; Fitamen, C.; Moulin, C.; Souchay, C. SenseCam: A New Tool for Memory Rehabilitation? Rev. Neurol. 2016, 172, 735–747. [Google Scholar] [CrossRef] [Green Version]
| Reference | Epilepsy Types | Controls (M/F) | Patients (M/F) | Lateralization (M/F) | Patient Age (Mean, SD or Range) | GASE Rating (SD) | AEDs (Mean, SD if Indicated) | Experiences Seizures? Frequency, SD (if Indicated) | Material | ALF Detected? | Delay Points | Comment |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Djordjevic et al., 2011 [15] | TLE | 11/8 | 44/46 | R-TLE: 14/30 L-TLE: 30/16 | R-TLE: 36.8 L-TLE: 33.5 | Story recall | No | 30 min, 24 h | ||||
| Mameniskiene, Jatuzis, Kaubrys, & Budrys, 2006 [16] | TLE | 19/40 | 29/41 | 33.3 (9.5) | 36 on monotherapy 34 on polytherapy | Yes, 6.6 (5.6) sz/month | RAVLT ROCFT Story recall | Yes (all tests) | 30 min, 4 weeks | ALF worse with frequent seizures | ||
| Helmstaedter, Hauff, & Elger, 1998 [17] | TLE | 11/10 | 27/28 | R-TLE: 27 L-TLE: 28 | 26.9 | Yes | Yes (but not during the past 8 h) | VLMT DCS-R | Yes (both tests) | 30 min, 1 week | ||
| Polat et al., 2020 [18] | TLE | 10/14 | 23/28 | R-TLE: 10/15 L-TLE: 13/13 | R-TLE 36.44 (8.30) L-TLE 37.15 (9.47) | No (Engel class I) | VLMT WMS-R-LM | Yes (seizure free L-TLE) | 30 min, 1 week, 6 weeks | Follow-up years after epilepsy surgery | ||
| Bengner et al., 2006 [19] | TLE and GGE | 6/6 | 20/36 | R-TLE: 11/13 L-TLE: 7/13 IGE: 2/10 | 39.2 (11.8) | Yes | Yes (9 during delay) | Face recognition | Yes | 2 min, 24 h | Face recognition is worse in R-TLE | |
| Bell, Fine, Dow, Seidenberg, & Hermann, 2005 [20] | TLE | 22/27 | 14/28 | R-TLE: 9/11 L-TLE: 5/17 | R-TLE: 40.0 (9.8) L-TLE: 34.0 (13.0) | Yes, 1.9 (0.75) (R-TLE), 1.7 (0.70) (L-TLE) on average | Yes, monthly | Word list SRT recall Design SRT recall | No | 30 min, 24 h | ||
| Helmstaedter, Winter, Melzer, Lohmann, & Witt, 2019 [21] | TLE and ETE | 65/89 | 16/20 | Temporal: 32 (72% LE+) Extratemporal: 4 (0% LE+) Left:15 Right:14 Bilateral: 7 | 43 (17) | Yes | Yes, LE+ 2.6 (1.7) sz/month, LE- 5.9 (6.4) sz/month | VLMT | Yes | 30 min, 1 week | ALF in 31–67% patients | |
| Visser et al., 2019 [22] | TLE | 14/16 | 15/15 | R-TLE: 17 L-TLE: 13 | 41.3 (19–62) | 4 on monotherapy 26 on polytherapy | Yes: 14 No: 16 | RAVLT | Yes (both R/L-TLE) | 30 min, 1 week | Post antero-temporal lobectomy with amygdalo-hippocampectomy (16 Engel class I, 4 Engel class II, 10 Engel class III). ALF in the seizure-free group. | |
| Miller, Mothakunnel, Flanagan, Nikpour, & Thayer, 2017 [23] | TLE and ETE | 29/31 | 22/22 | Temporal: 27 Extratemporal: 14 Temporal and extratemporal: 3 Left:22 Right:21 Bilateral: 1 | 40.7 (13.4) | Yes | No: 20 Yes: 24 (>1 sz/y) | RAVLT Aggie | Yes (especially RAVLT) | 30 min, 1 week | 23% of patients with ALF. Both temporal and extratemporal. ALF frequent with hippocampal lesions. | |
| Giovagnoli, Casazza, & Avanzini, 1995 [24] | TLE | 13/12 | 14/14 | R-TLE: 5/7 L-TLE: 9/7 | 38 (11.6) | Yes | No (past 6 months): 7 Yes: 21 | Design recall | No | 1 h, 1 day, 3 days, 6 days, 13 days | ||
| Wilkinson et al., 2012 [25] | TLE | 22 | 27 | R-TLE: 12 L-TLE: 15 (based on hippocampal sclerosis) | R-TLE: 38.67 (8.07) L-TLE: 34.80 (10.13) | Yes, 25 on polytherapy | Yes, uncontrolled | Story recall ROCFT | Yes (both tests) | 1 h, 6 weeks | Different ALF patterns, depending on lateralization | |
| Bell, 2006 [26] | TLE | 8/17 | 10/15 | R-TLE: 6 L-TLE: 11 Bilateral: 2 Uncertain: 6 | 39 (10) | Yes: 23 (1.5 (1.0)) No: 2 | Yes: 11 Yearly seizures/seizure-free: 14 | WMS-III-LM | No | 30 min, 2 weeks | ||
| Audrain & McAndrews, 2019 [27] | TLE | 12/12 | 14/9 | R-TLE: 9 L-TLE: 12 Bilateral: 2 | 37.17 (12.35) | Over 72 h delay: Yes: 8 No: 8 N/a: 7 | Digital object-scene pair recognition | Yes | 15 min, 90 min, 6 h, 16 h, 72 h | Indications of greater forgetting after 90 min | ||
| Gascoigne et al., 2019 [28] | IGE and TLE | 27/31 | IGE 10/10 TLE 10/13 | R-TLE: 6 L-TLE: 15 n/a: 2 | 11.3 (3.3) | IGE 2.1 (1.7) TLE 2.6 (1.2) | IGE: 17 on monotherapy, 3 on polytherapy TLE: 2 no AEDs, 14 on monotherapy, 7 on polytherapy | Yes (at least one 2 years prior) | CVLT-C | Yes | 2 min, 30 min, 1 week | ALF associated with behavioral problems |
| Lah, Mohamed, Thayer, Miller, & Diamond, 2014 [29] | TLE | 13/14 | 9/14 | R-TLE: 13 (7 with hippocampal lesions) L-TLE: 10 (5 with hippocampal lesions) | 44.8 (13.4) | 3 no AEDs 11 on monotherapy 9 on polytherapy | No: 5 < 1 sz/month: 8 >1 sz/month: 10 | HVLT-R | Yes | 30 min, 1 day, 1 week | ALF worse with hippocampal abnormalities | |
| Gascoigne et al., 2014 [30] | TLE | 27/31 | 10/13 | R-TLE: 2/4 L-TLE: 6/9 Unconfirmed: 2 | 12.5 (2.8) | 2.6 (1.2) | 2 no AEDs 14 on monotherapy 7 on polytherapy | Yes | CVLT-C Visual memory (Design location) | Yes (CVLT-C) | 2 min, 30 min, 1 week | ALF unrelated to epilepsy variables |
| Ricci, Mohamed, Savage, & Miller, 2015 [31] | TLE and ETE | 29 | 32 | TLE: R-TLE: 12 L-TLE: 5 Bilateral: 1 Unconfirmed: 3 ETE: Right: 3 Left: 3 Bilateral: 1 Unconfirmed: 4 | 39.0 (11.8) | Yes, 1.7 (1.1) on average | Yes, 18.6 (22.7) sz/year | Prose passage recall and recognition | Yes | 30 min, 24 h, 4 days | TLE, hippocampal lesions—worse recall between 30 min and 24 h ETE—greater decay between 24 h and 4 days | |
| Ricci, Mohamed, Savage, Boserio, & Miller, 2015 [32] | TLE and ETE | 29 | 32 | TLE: 21 (12 with hippocampal lesions) ETE: 11 | 39.0 (11.8) | Yes | Yes | Autobiographical experience recall and recognition | Yes | 30 min, 24 h, 4 days | Hippocampal lesions—worse recall between 30 min and 24 h Seizures, discharges-greater decay between 24 h and 4 days | |
| Martin et al., 1991 [33] | TLE | 6/15 | 10/11 | R-TLE: 4/4 L-TLE: 6/7 | 31 (7.5) | Yes | Word list SRT recall | Yes | 30 min, 24 h | |||
| Barkas et al., 2012 [34] | TLE | 6/6 | 10/13 | R-TLE: 7/6 L-TLE: 3/7 | 48 | Virtual water maze | Yes | 3–6 weeks | Both hippocampal sclerosis and surgery groups demonstrate ALF | |||
| Cassel, Morris, Koutroumanidis, & Kopelman, 2016 [35] | TLE | 9/9 | 9/9 | R-TLE: 6 L-TLE: 6 Bilateral:4 n/a: 2 | 39.3 (9.8) | 1 no AEDs 9 on monotherapy 8 on polytherapy | Yes, 5 during participation | Story task Route video recall | Yes (story task) | 30 s, 10 min, 1 day, 1 week | Faster route forgetting in R-TLE | |
| Narayanan et al., 2012 [36] | TLE | 3/14 | 6/9 | R-TLE: 2/4 L-TLE: 4/4 | R-TLE: 34.5 (12.21) L-TLE: 32.88 (9.09) | Yes | RAVLT ROCFT Labyrinth maze Autobiographic events | Yes (RAVLT) | 30 min, 4 weeks | |||
| Blake, Wroe, Breen, & Mccarthy, 2000 [37] | TLE and others | 6/10 | 7/14 (14 TLE) | R-TLE: 5 L-TLE: 9 | R-TLE: 36.67 (9.41) L-TLE: 33.20 (10.94) | Yes, 2.05 (0.86) on average | Yes | Story recall and recognition | Yes | 30 min, 8 weeks | ||
| Muhlert et al., 2011 [5] | TLE and GGE | TLE: 3/7 GGE: 7/8 | TLE: 4/10 GGE: 6/8 | EEG: Left: 2 Right: 2 Bilateral: 2 n/a: 8 | TLE: 46.4 (11) GGE: 31.6 (14.6) | TLE: 2 no AEDs 6 on monotherapy 6 on polytherapy GGE: 1 no AEDs 8 on monotherapy 5 on polytherapy | Yes, 3.8 sz/month (TLE), 5.4 sz/month (GGE) | Visual scene recall and recognition Story recall and recognition Spatial discrimination Descriptive recall | Yes (TLE, visual scene recall, descriptive recall, story recognition) | 40 s, 30 min, 3 weeks | ALF not related to seizure variables. ALF in TLE, not GGE. | |
| Miller, Flanagan, Mothakunnel, Mohamed, & Thayer, 2015 [38] | TLE and ETE | 28/32 | 7/8 | TLE: R-TLE: 3 L-TLE: 6 ETE: Left: 2 Right: 2 Bilateral: 1 Unconfirmed: 1 | 37 | Yes | RAVLT WMS-IV-LM Aggie figures | Yes (all tests, RAVLT more sensitive) | 30 min, 1 week | ALF predominance in TLE. ALF irrespective of laterality. | ||
| Evans, Elliott, Reynders, & Isaac, 2014 [39] | TLE | 12/13 | 3/4 | R-TLE: 2/2 L-TLE: 1/2 | 39.71 (15.77) | 2 on monotherapy 5 on polytherapy | Yes | Visual scene recall and recognition Story recall and recognition | Yes (both tests) | 30 min, 1 week | ALF tested pre- and post-operatively: ALF improvement after resection | |
| Deak, Stickgold, Pietras, Nelson, & Bubrick, 2011 [40] | TLE | 9 | 7 | R-TLE: 1 L-TLE: 5 Bilateral: 1 | 44.0 | 2 on monotherapy 5 on polytherapy | Yes, 1 (during testing) | Word list SRT recall Finger tapping motor sequence | Yes (word test) | 30 min, 12 h, 24 h | Indication of sleep being protective in ALF | |
| Contador, Sánchez, Kopelman, & González de la Aleja, 2017 [41] | TLE (one patient with TLE+TEA) | 4/6 | 2/3 | 24.40 (4.09) | 2 on monotherapy 3 on polytherapy | Yes (4.2 sz/year) | Cued story recall Cued visuospatial route recall | No | 30 s, 10 min, 1 day, 1 week | |||
| Tramoni et al., 2011 [42] | TLE and TEA | 15 | 4/1 | Left: 1 Right: 2 Bilateral: 2 | 42.6 (9.3) | Yes, on monotherapy | No (past 1 year) | Story recall and recognition Virtual route recall and recognition Real route recall and recognition Ecological episode recall and recognition Single item recognition Recall and recognition of new facts | Yes (story, route, episode tasks) | 1 h, 6 weeks | ||
| Reference | Epilepsy Type | Controls (M/F) | Patients (M/F) | Patient Age (SD) | AEDs | Experiences Seizures? Mean, SD if Indicated | Material | ALF Detected? | Delay Points | Comment |
|---|---|---|---|---|---|---|---|---|---|---|
| Savage, Butler, Milton, Han, & Zeman, 2017 [43] | TEA | 38/12 | 42/13 | 70.59 (8.14) | Yes, mean number of attacks 17.85 (18.05) | RAVLT | Yes | 30 min, 1 week | Olfactory hallucination and reduction in olfactory function more frequent in TEA. | |
| Mosbah et al., 2014 [44] | TEA | 15 | 18/12 | 1 no AEDs 24 on monotherapy 5 on polytherapy | Yes | WMS-III-LM ROCF Single items recognition | Yes (WMS-III-LM, ROCF) | 1 h, 6 weeks | Neurometabolic correlates for ALF in the medial temporal lobe. | |
| Hoefeijzers, Zeman, Della Sala, & Dewar, 2019 [45] | TEA | 14/18 | 20/7 | 66.44 (9.48) | 27 on monotherapy | No (past 6 months) | Incidental story recall and recognition | Yes | 30 min, 1 week | |
| Butler et al., 2007 [46] | TEA | 24 | 34/16 (24 tested for ALF) | 68 (8.7) | Yes, 48 on monotherapy | No (between sessions) | RAVLT GKMDT | Yes (both tests) | 30 min, 1 week, 3 weeks | |
| Butler et al., 2013 [47] | TEA | 20 | 28/13 (22 tested for ALF) | 67.7 (8.9) | Yes, on monotherapy | No (past 6 months) | Word, prose, and design recall | Yes | 30 min, 1 week, 3 weeks | No significant structural MRI correlates with ALF |
| Butler et al., 2009 [48] | TEA | 20 | 28/13 (22 tested for ALF) | 67.7 (8.9) | Yes, on monotherapy | No (past 6 months) | Word, prose, and design recall | Yes | 30 min, 1 week, 3 weeks | Bilateral hippocampal volumes smaller in patients |
| Dewar, Hoefeijzers, Zeman, Butler, & Della Sala, 2015 [49] | TEA | 8/8 | 12/4 | 69.63 (6.33) | Yes, on monotherapy | No (past 6 months) | Picture recognition test | No | 5 min, 2.5 h, 7.5 h, 24 h, 1 week | In TEA patients, picture recognition impaired after 5 min with no acceleration in rate afterwards |
| Butler, Kapur, Zeman, Weller, & Connelly, 2012 [50] | TEA | 8/12 | 12/10 | 66.4 (8.8) | Yes | No (during study) | RAVLT | Yes | 30 min, 1 week | Hippocampal volumetry not related to ALF |
| Hoefeijzers, Dewar, Della Sala, Zeman, & Butler, 2013 [51] | TEA | 7/11 | 9/8 | 65.47 (8.79) | Yes, on monotherapy | No (past 6 months) | Word recall (reanalysis of Butler et al., 2007 [46]) | Yes | 30 min, 1 week, 3 weeks | Support for ALF as a consolidation issue |
| Atherton, Filippini, Zeman, Nobre, & Butler, 2019 [52] | TEA | 10/5 | 12/3 | 67.73 (1.63) | Yes, on monotherapy | No (past 6 months) | Digital image recognition RAVLT | Yes (RAVLT) | 30 min, 1 week | Significant fMRI results (hypoactive left hippocampus prior forgetting) |
| Savage et al., 2019 [53] | TEA | 7/5 | 9/5 | 78.3 (7.0) | 1 no AEDs 13 on monotherapy | At T2: No (stable): 9 Yes: 5 | RAVLT Story recall GKMDT | Yes (story recall, GKMDT) | 30 min, 1 week | 10-year follow-up (4 converters ALF to no ALF, but 0 converters from no ALF to ALF) |
| Hoefeijzers, Dewar, Sala, Butler, & Zeman, 2015 [54] | TEA | 8/8 | 10/1 | 69.82 (5.60) | Yes, on monotherapy | No (past 6 months) | 4 Word Lists, recall and recognition | Yes | 30 min, 3 h, 8 h, 24 h, 1 week | Evidence of ALF from 3 to 8 h post-learning |
| Atherton, Nobre, Zeman, & Butler, 2014 [55] and Atherton et al., 2016 [56] | TEA | 7/5 | 10/1 | 67.73 (1.63) | Yes, on monotherapy | No (past 6 months) | Word pairs association | Yes | 30 min, 12 h | Sleep promotes memory retention in ALF |
| Muhlert, Milton, Butler, Kapur, & Zeman, 2010 [57] | TEA | 1/10 | 10/1 | 68.6 (9.9) | Yes, on monotherapy | No (past 4 months) | Word recall Real-life event SenseCam test | Yes (both tests) | 30 min, 1 day, 1 week, 3 weeks | |
| Manes, Graham, Zeman, De Luján Calcagno, & Hodges, 2005 [58] | TEA | 7 | 6/1 | 57 (8.1) | Yes, on monotherapy | No | Story recall and recognition Drawing recall and recognition | Yes (story tests) | 30 min, 6 weeks |
| Reference | Epilepsy Type | Controls (M/F) | Patients (M/F) | Patient age (Mean, SD, or Range) | GASE Rating (SD) | AEDs | Experiences Seizures? Frequency, SD (if Indicated) | Material | ALF Detected? | Delay Points Tested | Comment |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Fitzgerald, Thayer, Mohamed, & Miller, 2013 [6] | Various Normal EEG: 18 Focal: 10 Generalized: 5 | 15 | 34 | Normal EEG: 36.89 (10.47) Focal: 41.8 (14.60) Generalized: 32.60 (14.54) | 4 no AEDs 17 on monotherapy 12 on polytherapy | Yes | Word Memory Test Design Memory Test | Yes (both tests) | 30 min, 24 h, 4 days | No relation with seizure variables. Information better retained with naps. | |
| Davidson, Dorris, O’Regan, & Zuberi, 2007 [59] | GGE | 21 | 7/14 | 11.5 (8–16) | 4 no AEDs 15 on monotherapy 2 on polytherapy | Yes: 16 No: 5 | Children’s memory scale: Stories and Dot location subtests | Yes (stories task) | 30 min, 1 week | Poor initial learning | |
| Gascoigne et al., 2012 [60] | GGE | 20/21 | 10/10 | 10.76 (2.47) | 2.17 (1.69) | 18 on monotherapy 2 on polytherapy | Yes (at least one 2 years prior) | CVLT-C | Yes | 2 min, 30 min, 1 week | Epilepsy severity related to ALF |
| Grayson-Collins et al., 2019 [7] | GGE | 11/18 | 11/7 | 10.90 (2.53) | 1.68 (1.08) | 7 no AEDs 7 on monotherapy 4 on polytherapy | At T2: No: 7 Yes: 11 | CVLT-C | Yes | 2 min, 30 min, 1 week | No improvement in ALF after seizure reduction (7.53 (2.43) years of follow-up) |
| Beilharz, Thayer, Nikpour, & Lah, 2020 [61] | GGE | 2/12 | 4/12 | 42.93 (13.09) | 3.31 (1.18) | 5 on monotherapy 9 on polytherapy | n/a, last seizure at 4.51 (8.60) years | CVLT-III WMS-IV-LM | No | 2 min, 30 min, 1 week | |
| Ricci, Wong, Nikpour, & Miller, 2019 [62] | Symptoms of epilepsy | 10/0 | 3/0 | 66.7 (5.7) | 2 no AEDs 1 on monotherapy | No | Story recall | Yes | 30 min, 24 h, 1 week, 2 weeks, 4 weeks | Testing ALF patients after a 2 weeks delay and early rehearsal improved recall up to 1 week |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mameniškienė, R.; Puteikis, K.; Jasionis, A.; Jatužis, D. A Review of Accelerated Long-Term Forgetting in Epilepsy. Brain Sci. 2020, 10, 945. https://doi.org/10.3390/brainsci10120945
Mameniškienė R, Puteikis K, Jasionis A, Jatužis D. A Review of Accelerated Long-Term Forgetting in Epilepsy. Brain Sciences. 2020; 10(12):945. https://doi.org/10.3390/brainsci10120945
Chicago/Turabian StyleMameniškienė, Rūta, Kristijonas Puteikis, Arminas Jasionis, and Dalius Jatužis. 2020. "A Review of Accelerated Long-Term Forgetting in Epilepsy" Brain Sciences 10, no. 12: 945. https://doi.org/10.3390/brainsci10120945






