Development and Evaluation of a Screening Tool to Aid the Diagnosis of Cluster Headache
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Population
2.3. Ethics
2.4. Screening Tool Development
2.5. Statistical Methodology
Analysis
2.6. Sensitivity and Specificity and the Receiver Operating Characteristics (ROC)
3. Results
3.1. Description of the Sample
3.2. Descriptive Analysis of Test Scores
3.3. Sensitivity and Specificity of the Test Scores
3.4. ROC Analysis for Whole Data Set
3.5. ROC Analysis According to Gender
3.6. ROC Analysis with Class Balancing
4. Discussion
4.1. Clinical Indicators of CH versus Migraine
4.2. Screening Tools for CH
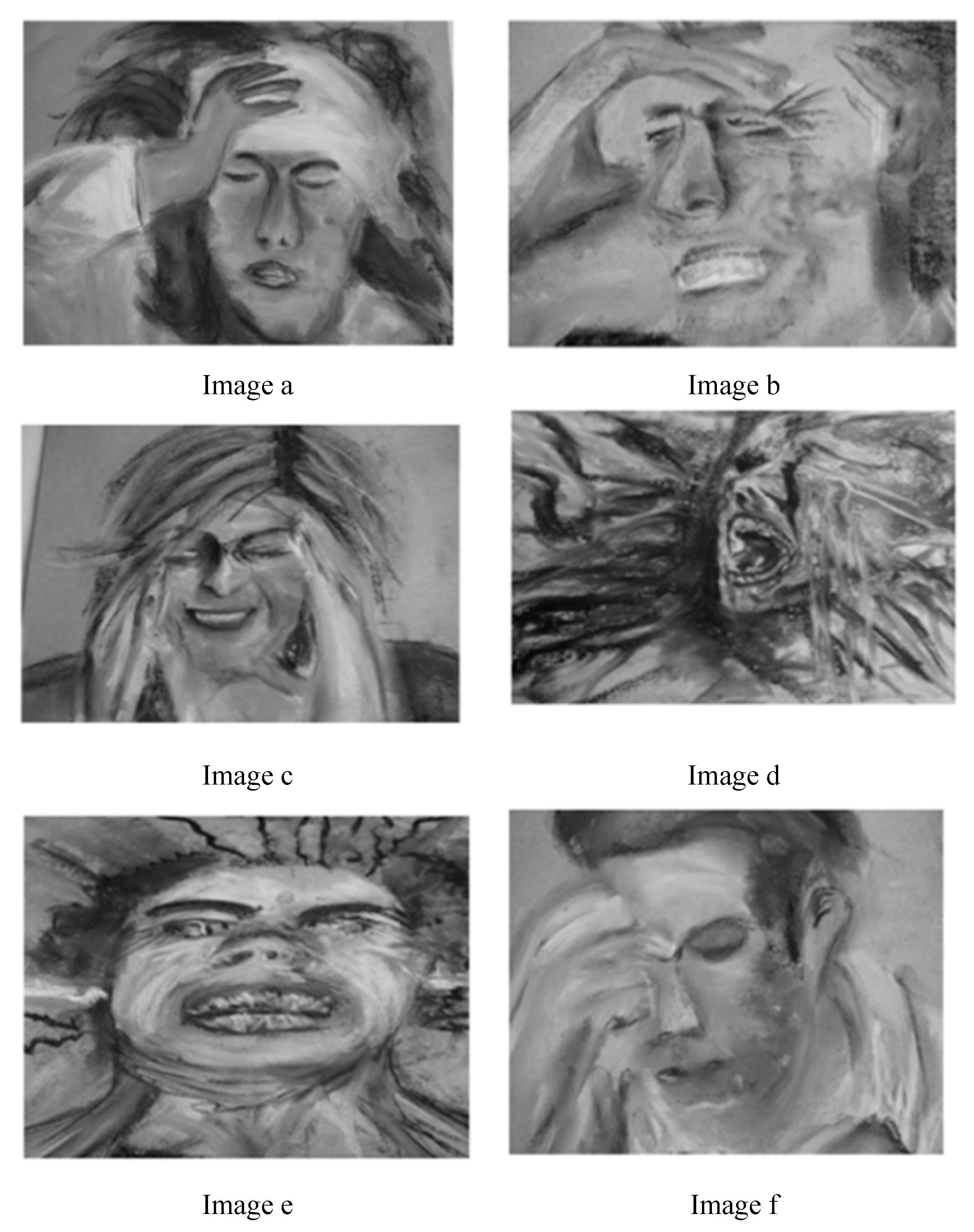
4.3. Images Depicting Headache Pain
4.4. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Availability of Data and Material
References
- Goadsby, P.J.; Wei, D.Y.-T.; Ong, J.J.Y. Cluster headache: Epidemiology, pathophysiology, clinical features, and diagnosis. Ann. Indian Acad. Neurol. 2018, 21, S3–S8. [Google Scholar] [CrossRef]
- Choong, C.K.; Ford, J.H.; Nyhuis, A.W.; Robinson, R.L.; Aurora, S.K. Health Care Utilization and Direct Costs Among Patients Diagnosed with Cluster Headache in U.S. Health Care Claims Data. J. Manag. Care Spéc. Pharm. 2018, 24, 921–928. [Google Scholar] [CrossRef] [PubMed]
- Headache Classification Committee of the International Headache Society (IHS) The International Classification of Headache Disorders, 3rd edition. Cephalalgia 2018, 38, 1–211. [CrossRef] [PubMed]
- Lund, N.; Barloese, M.; Petersen, A.; Haddock, B.; Jensen, R. Chronobiology differs between men and women with cluster headache, clinical phenotype does not. Neurology 2017, 88, 1069–1076. [Google Scholar] [CrossRef] [PubMed]
- Vikelis, M.; Rapoport, A.M. Cluster headache in Greece: an observational clinical and demographic study of 302 patients. J. Headache Pain 2016, 17, 88. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Del Rio, M.S.; Leira, R.; Pozo-Rosich, P.; Laínez, J.M.; Alvarez, R.; Pascual, J. Errors in Recognition and Management are Still Frequent in Patients with Cluster Headache. Eur. Neurol. 2014, 72, 209–212. [Google Scholar] [CrossRef] [PubMed]
- Rozen, T.D.; Fishman, R.S. Cluster headache in the United States of America: demographics, clinical characteristics, triggers, suicidality, and personal burden. Headache 2012, 52, 99–113. [Google Scholar] [CrossRef]
- Van Alboom, E.; Louis, P.; Van Zandijcke, M.; Crevits, L.; Vakaet, A.; Paemeleire, K. Diagnostic and therapeutic trajectory of cluster headache patients in Flanders. Acta Neurol. Belg. 2009, 109, 10–17. [Google Scholar]
- Voiticovschi-Iosob, C.; Allena, M.; De Cillis, I.; Nappi, G.; Sjaastad, O.; Antonaci, F. Diagnostic and therapeutic errors in cluster headache: A hospital-based study. J. Headache Pain 2014, 15, 56. [Google Scholar] [CrossRef] [Green Version]
- Schürks, M.; Kurth, T.; De Jesus, J.; Jonjic, M.; Rosskopf, D.; Diener, H.-C. Cluster Headache: Clinical Presentation, Lifestyle Features, and Medical Treatment. Headache: J. Head Face Pain 2006, 46, 1246–1254. [Google Scholar] [CrossRef]
- Joshi, S.; Rizzoli, P.; Loder, E. The comorbidity burden of patients with cluster headache: A population-based study. J. Headache Pain 2017, 18, 76. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gooriah, R.; Buture, A.; Ahmed, F. Evidence-based treatments for cluster headache. Ther. Clin. Risk Manag. 2015, 11, 1687–1696. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Buture, A.; Ahmed, F.; Dikomitis, L.; Boland, J.W. Systematic literature review on the delays in the diagnosis and misdiagnosis of cluster headache. Neurol. Sci. 2018, 40, 25–39. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jensen, R.; Lyngberg, A.; Jensen, R. Burden of Cluster Headache. Cephalalgia 2007, 27, 535–541. [Google Scholar] [CrossRef]
- Choi, Y.-J.; Kim, B.-K.; Chung, P.-W.; Lee, M.J.; Park, J.-W.; Chu, M.K.; Ahn, J.-Y.; Kim, B.-S.; Song, T.-J.; Sohn, J.-H.; et al. Impact of cluster headache on employment status and job burden: A prospective cross-sectional multicenter study. J. Headache Pain 2018, 19, 78. [Google Scholar] [CrossRef]
- Bahra, A.; Goadsby, P.J. Diagnostic delays and mis-management in cluster headache. Acta Neurol. Scand. 2004, 109, 175–179. [Google Scholar] [CrossRef]
- Buture, A.; Boland, J.W.; Dikomitis, L.; Ahmed, F. Update on the pathophysiology of cluster headache: Imaging and neuropeptide studies. J. Pain Res. 2019, 12, 269–281. [Google Scholar] [CrossRef] [Green Version]
- Ferraro, S.; Nigri, A.; Bruzzone, M.G.; Demichelis, G.; Pinardi, C.; Brivio, L.; Giani, L.; Proietti, A.; Leone, M.; Chiapparini, L. Cluster headache: Insights from resting-state functional magnetic resonance imaging. Neurol. Sci. 2019, 40, 45–47. [Google Scholar] [CrossRef]
- Gibson, K.F.; Santos, A.D.; Lund, N.; Jensen, R.; Stylianou, I.M. Genetics of cluster headache. Cephalalgia 2019, 39, 1298–1312. [Google Scholar] [CrossRef]
- Morris, J.; Straube, A.; Diener, H.-C.; Ahmed, F.; Silver, N.; Walker, S.; Liebler, E.; Gaul, C. Cost-effectiveness analysis of non-invasive vagus nerve stimulation for the treatment of chronic cluster headache. J. Headache Pain 2016, 17, 43. [Google Scholar] [CrossRef] [Green Version]
- Martelletti, P.; Jensen, R.H.; Antal, A.; Arcioni, R.; Brighina, F.; De Tommaso, M.; Franzini, A.; Fontaine, D.; Heiland, M.; Jürgens, T.P.; et al. Neuromodulation of chronic headaches: position statement from the European Headache Federation. J. Headache Pain 2013, 14, 86. [Google Scholar] [CrossRef] [PubMed]
- Buture, A.; Boland, J.W.; Ahmed, F.; Dikomitis, L. Images depicting headache pain—A tool to aid the diagnosis of cluster headache: A pilot study. J. Multidiscip. Heal. 2019, 12, 691–698. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- ICHD3beta. The international classification of headache disorders: 3rd edition (beta version). Cephalalgia 2013, 33, 629–808. [Google Scholar] [CrossRef] [Green Version]
- Alcecluster. Available online: http://alcecluster.cefalea.it/ (accessed on 27 February 2019).
- Rossi, P.; Geraci, C.; Navarro, F.M. EHMTI-0041. ARTe Cluster project. Cluster headache—From pain to inspiration. J. Headache Pain 2014, 15, C55. [Google Scholar] [CrossRef] [Green Version]
- Migraine Art Collection. Available online: http://www.migraineart.org.uk (accessed on 16 June 2019).
- Art by Faderhead. Available online: https://www.deviantart.com/faderhead/art/Migraine-Headache-286959 (accessed on 16 June 2019).
- Ahmed, F.; Dikomitis, L.; Zafar, H.; Goadsby, P.; Paemeliere, K. EHMTI-0357. Perceptions and experiences of cluster headache among patients, general practitioners and neurologists in the north of england: A qualitative study. J. Headache Pain 2014, 15, J1. [Google Scholar] [CrossRef] [Green Version]
- Khoo, S.B. Masqurades of Cluster headache. Malays Fam Physician. 2009, 4, 51–56. [Google Scholar] [PubMed]
- Tsang, S.; Royse, C.F.; Terkawi, A.S. Guidelines for developing, translating, and validating a questionnaire in perioperative and pain medicine. Saudi J. Anaesth. 2017, 11, 80–S89. [Google Scholar] [CrossRef]
- Van Der Meer, H.A.; Visscher, C.M.; Engelbert, R.H.; Mulleners, W.M.; Van Der Sanden, M.W.N.; Speksnijder, C.M. Development and psychometric validation of the headache screening questionnaire—Dutch Version. Musculoskelet. Sci. Pr. 2017, 31, 52–61. [Google Scholar] [CrossRef]
- Trochim, W.M.K. “Descriptive statistics” Research Methods Knowledge Base. Retrieved October 2006, 10, 2011. [Google Scholar]
- Mehta, N.; Maloney, G.E.; Bana, D.S.; Scrivani, S.J. Head, Face, and Neck Pain Science, Evaluation, and Management: An Interdisciplinary Approach; John Wiley & Sons: Hoboken, NJ, USA, 2011. [Google Scholar]
- Chung, P.W.; Cho, S.J.; Kim, B.K.; Kim, S.K.; Lee, M.J.; Choi, Y.J.; Park, J.W.; Kim, B.S.; Oh, K.; Moon, H.S.; et al. Development and Validation of the Cluster Headache Screening Questionnaire. J. Clin. Neurol. 2019, 15, 90–96. [Google Scholar] [CrossRef]
- Trevethan, R. Sensitivity, Specificity, and Predictive Values: Foundations, Pliabilities, and Pitfalls in Research and Practice. Front. Public Health 2017, 5, 307. [Google Scholar] [CrossRef] [PubMed]
- Tape, G.T. Interpreting Diagnostic Tests. Introduction to ROC curves. Available online: http://gim.unmc.edu/dxtests/ROC1.htm (accessed on 10 May 2019).
- Unal, I. Defining an Optimal Cut-Point Value in ROC Analysis: An Alternative Approach. Comput. Math. Methods Med. 2017, 2017, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Bujang, M.A.; Adnan, T.H. Requirements for Minimum Sample Size for Sensitivity and Specificity Analysis. J. Clin. Diagn. Res. 2016, 10, YE01–YE06. [Google Scholar] [CrossRef] [PubMed]
- Lai, T.H.; Fuh, J.L.; Wang, S.J. Cranial autonomic symptoms in migraine: Characteristics and comparison with cluster headache. J. Neurol. Neurosurg. Psychiatry 2009, 80, 1116–1119. [Google Scholar] [CrossRef] [PubMed]
- May, A.; Schwedt, T.J.; Magis, D.; Pozo-Rosich, P.; Evers, S.; Wang, S.J. Cluster headache. Nat. Rev. Dis. Primers. 2018, 4, 18006. [Google Scholar] [CrossRef] [PubMed]
- Ekbom, K.; Hardebo, J.E. Cluster headache: aetiology, diagnosis and management. Drugs 2002, 62, 61–69. [Google Scholar] [CrossRef]
- Magis, D. Emerging treatments for cluster headache: hopes and disappointments. Curr. Opin. Neurol. 2019, 32, 432–437. [Google Scholar] [CrossRef]
- Vollesen, A.L.; Benemei, S.; Cortese, F.; Labastida-Ramírez, A.; Marchese, F.; Pellesi, L.; Romoli, M.; Ashina, M.; Lampl, C.; School of Advanced Studies of the European Headache Federation (EHF-SAS); et al. Migraine and cluster headache—The common link. J. Headache Pain 2018, 19, 89. [Google Scholar] [CrossRef] [Green Version]
- McDonald, D.D.; Shea, M.; Rose, L.; Fedo, J. The Effect of Pain Question Phrasing on Older Adult Pain Information. J. Pain Symptom Manag. 2010, 37, 1050–1060. [Google Scholar] [CrossRef]
- Daoust, R.; Sirois, M.-J.; Lee, J.S.; Perry, J.J.; Griffith, L.E.; Worster, A.; Lang, E.; Paquet, J.; Chauny, J.-M.; Émond, M. Painful Memories: Reliability of Pain Intensity Recall at 3 Months in Senior Patients. Pain Res. Manag. 2017, 2017, 1–7. [Google Scholar] [CrossRef] [Green Version]
- Garbi, M.D.O.S.S.; Hortense, P.; Gomez, R.R.F.; Silva, T.D.C.R.D.; Castanho, A.C.F.; Sousa, F.A.E.F. Pain intensity, disability and depression in individuals with chronic back pain1. Rev. Latino-Americana de Enferm. 2014, 22, 569–575. [Google Scholar] [CrossRef] [PubMed]
- Karimi, Z.; Pilenko, A.; Held, S.M.; Hasenbring, M.I. Recall Bias in Patients with Chronic Low Back Pain: Individual Pain Response Patterns Are More Important Than Pain Itself! Int. J. Behav. Med. 2016, 23, 12–20. [Google Scholar] [CrossRef] [PubMed]
- Snoer, A.H.; Lund, N.; Jensen, R.H.; Kristoffersen, E.S.; Barloese, M.; Hansen, J.M. More precise phenotyping of cluster headache using prospective attack reports. Eur. J. Neurol. 2019, 26, 1303-e85. [Google Scholar] [CrossRef]
- Bhargava, A.; Pujar, G.S.; Banakar, B.F.; Kasundra, G.; Bhushan, B.; Shubhakaran, K. Study of cluster headache: A hospital-based study. J. Neurosci. Rural. Pr. 2014, 5, 369–373. [Google Scholar] [CrossRef] [PubMed]
- Lin, K.-H.; Wang, P.-J.; Fuh, J.-L.; Lu, S.-R.; Chung, C.-T.; Tsou, H.-K.; Wang, S.-J. Cluster Headache in the Taiwanese—A Clinic-Based Study. Cephalalgia 2004, 24, 631–638. [Google Scholar] [CrossRef] [PubMed]
- Torelli, P.; Beghi, E.; Manzoni, G.C. Validation of a Questionnaire for the Detection of Cluster Headache. Headache: J. Head Face Pain 2005, 45, 644–652. [Google Scholar] [CrossRef]
- A Wilbrink, L.; Weller, C.M.; Cheung, C.; Stijnen, T.; Haan, J.; Ferrari, M.D.; Terwindt, G.M. Stepwise web-based questionnaires for diagnosing cluster headache: LUCA and QATCH. Cephalalgia 2013, 33, 924–931. [Google Scholar] [CrossRef]
- Dousset, V.; Laporte, A.; LeGoff, M.; Brochet, B.; Traineau, M.-H.; Dartigues, J.-F. Validation of a Brief Self-Administered Questionnaire for Cluster Headache Screening in a Tertiary Center. Headache: J. Head Face Pain 2009, 49, 64–70. [Google Scholar] [CrossRef]
- Fritsche, G.; Hueppe, M.; Kukava, M.; Dzagnidze, A.; Schuerks, M.; Yoon, M.-S.; Diener, H.-C.; Katsarava, Z. Validation of a German Language Questionnaire for Screening for Migraine, Tension-Type Headache, and Trigeminal Autonomic Cephalgias. Headache: J. Head Face Pain 2007, 47, 546–551. [Google Scholar] [CrossRef]
- Yoon, M.-S.; Obermann, M.; Fritsche, G.; Slomke, M.; Dommes, P.; Schilf, C.; Diener, H.-C.; Katsarava, Z. Population-Based Validation of a German-Language Self-Administered Headache Questionnaire. Cephalalgia 2008, 28, 605–608. [Google Scholar] [CrossRef]
- Kukava, M.; Dzagnidze, A.; Mirvelashvili, E.; Djibuti, M.; Fritsche, G.; Jensen, R.; Stovner, L.J.; Steiner, T.J.; Katsarava, Z. Validation of a Georgian language headache questionnaire in a population-based sample. J. Headache Pain 2007, 8, 321–324. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peláez, I.; Ferrera, D.; Barjola, P.; Fernandes, R.; Mercado, F. Subliminal emotional pictures are capable of modulating early cerebral responses to pain in fibromyalgia. PLoS ONE 2019, 14, e0217909. [Google Scholar] [CrossRef] [PubMed]
- Linton, S.J.; Shaw, W.S. Impact of Psychological Factors in the Experience of Pain. Phys. Ther. 2011, 91, 700–711. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schott, G.D. Pictures of pain: their contribution to the neuroscience of empathy. Brain 2015, 138, 812–820. [Google Scholar] [CrossRef] [PubMed]
- De Coo, I.F.; Wilbrink, L.A.; Haan, J.; Ferrari, M.D.; Terwindt, G.M. Evaluation of the new ICHD-III beta cluster headache criteria. Cephalalgia 2016, 36, 547–551. [Google Scholar] [CrossRef]



| Question | Variable | Coded Test Scores |
|---|---|---|
| 1. Please choose one image that best illustrates the most severe headache you have experienced | Image preference | f = 1 (least severe); a = 2; c = 3; b = 4; e = 5; d = 6 (most severe) |
| 2. Please mark with an X the intensity of your pain on the scale below | Pain scale | Scores from zero to ten (0 = No pain; 5 = Moderate pain; 10 = Worst possible pain) |
| 3. Please choose only one option from the following list that describes your headaches | Intensity | Mild = 1; Moderate = 2; Severe = 3; Very Severe = 4; Excruciating = 5 |
| 4. Please choose only one option from the following list that describes your headaches | Nature of pain | Throbbing/Other = 1; Pressure = 2; Stabbing/Burning = 3 |
| 5. Please choose only one option from the following list that describes your headaches | Description of pain | Red hot poker in the eye = 1; Pounding heart in the head/Other = 0 |
| 6. Do you feel restless during the headache attack? | Restlessness | No = 0; Yes = 1 |
| 7. Is the pain ‘excruciating agony’? | Excruciating agony | No = 0; Yes = 1 |
| 8. Does the pain wake you up from sleep the same time each night/ or attack comes at a specific time of the day? | Headache at specific times | No = 0; Yes = 1 |
| 9. Is the pain strictly on one side? | Strictly unilateral pain | No = 0; Yes = 1 |
| 10. Ipsilateral cranial autonomic symptoms (e.g., red watery eyes and/or runny nose?) | Ipsilateral cranial autonomic symptoms | No = 0; Yes = 1 |
| 11. How long does the most severe pain last for with medication? | Treated attack duration | > 3 h = 0; ≤ 3 h = 1; |
| 12. How long does the most severe pain last for without medication? | Untreated attack duration | > 3 h = 0; ≤ 3 h = 1; |
| Variable | Minimum | Maximum | |
|---|---|---|---|
| 1 | Image preference | 1 | 6 |
| 2 | Pain scale | 0 | 10 |
| 3 | Intensity | 1 | 5 |
| 4 | Nature of pain | 1 | 3 |
| 5 | Description of pain | 0 | 1 |
| 6 | Restlessness | 0 | 1 |
| 7 | Excruciating agony | 0 | 1 |
| 8 | Headache at specific times | 0 | 1 |
| 9 | Strictly unilateral pain | 0 | 1 |
| 10 | Ipsilateral cranial autonomic symptoms | 0 | 1 |
| 11 | Treated attack duration ≤ 3 h | 0 | 1 |
| 12 | Untreated attack duration ≤ 3 h | 0 | 1 |
| Total Score | 3 | 32 | |
| Test Item | Category | % within Diagnosis | |
|---|---|---|---|
| Case Group | Control Group | ||
| CH (n = 81) | Migraine (n = 215) | ||
| Image preference | a | 4.7 | 18.9 |
| b | 10.8 | 21.5 | |
| c | 3.9 | 23.3 | |
| d | 61.9 | 18.0 | |
| e | 8.3 | 7.4 | |
| f | 10.3 | 14.3 | |
| Pain scale | 1 | 0.0 | 0.0 |
| 2 | 0.0 | 0.0 | |
| 3 | 0.0 | 1.6 | |
| 4 | 0.0 | 2.0 | |
| 5 | 1.1 | 3.1 | |
| 6 | 0.0 | 5.4 | |
| 7 | 3.3 | 15.8 | |
| 8 | 3.6 | 33.8 | |
| 9 | 28.0 | 20.2 | |
| 10 | 63.9 | 19.9 | |
| Intensity of pain | Mild | 0.0 | 1.1 |
| Moderate | 0.0 | 13.8 | |
| Severe | 7.8 | 35.0 | |
| Very severe | 8.6 | 33.6 | |
| Excruciating | 83.6 | 16.4 | |
| Nature of pain | Throbbing/ Other | 18.0 | 40.0 |
| Pressure | 14.1 | 33.2 | |
| Stabbing/ Burning | 67.8 | 26.7 | |
| Treated attack duration | ≤ 3 h | 100.0 | 24.3 |
| > 3 h | 0.0 | 75.7 | |
| Untreated attack duration | ≤ 3 h | 100.0 | 0.0 |
| > 3 h | 0.0 | 100.0 | |
| Description of pain | Pounding heart/other | 30.8 | 84.4 |
| Red hot poker in the eye | 69.2 | 15.6 | |
| Restlessness | No | 10 | 56.7 |
| Yes | 90.0 | 43.2 | |
| Excruciating agony | No | 10 | 56.7 |
| Yes | 90.0 | 43.2 | |
| Attacks at specific times | No | 39.1 | 80.6 |
| Yes | 60.8 | 19.4 | |
| Strictly unilateral pain | No | 13.3 | 55.5 |
| Yes | 86.6 | 44.5 | |
| Ipsilateral cranial autonomic symptoms | No | 3.6 | 57.8 |
| Yes | 96.4 | 42.2 | |
| Test item | Sensitivity% (CI) | Specificity% (CI) | PPV% (CI) | NPV% (CI) | FPR% (CI) | FNR% (CI) |
|---|---|---|---|---|---|---|
| Description of pain | 68 (58;78) | 84 (79;89) | 62 (52;72) | 87 (83;92) | 16 (11;21) | 32 (22;38) |
| Presence of restlessness | 90 (84;97) | 56 (50;63) | 44 (36;51) | 94 (90;98) | 44 (37;50) | 10 (3;15) |
| Excruciating agony | 93 (87;98) | 33 (27;40) | 34 (28;41) | 92 (86;98) | 67 (60;73) | 7 (2;13) |
| Attacks at specific times | 60 (50;71) | 81 (76;86) | 54 (44;65) | 84 (80;89) | 19 (14;24) | 40 (29;46) |
| Strictly unilateral pain | 86 (79;94) | 56 (49;62) | 42 (35;50) | 92 (87;96) | 44 (38;51) | 14 (6;19) |
| Ipsilateral cranial autonomic symptoms | 96 (92;100) | 57 (50;63) | 46 (38;53) | 98 (95;100) | 43 (37;50) | 4 (0.0;7) |
| Treated attack duration ≤ 3 h | 100 (100;100) | 77 (71;82) | 62 (54;70) | 100 (100;100) | 23 (18;29) | 0 (0.0;0.0) |
| Untreated attack duration ≤ 3 h | 100 (100;100) | 100 (100;100) | 100 (100;100) | 100 (100;100) | 0 (0.0;0.0) | 0 (0.0;0.0) |
| Test Item | Cut-off | Sensitivity (%) | Specificity (%) |
|---|---|---|---|
| Nature of pain | 3 (Stabbing/Burning) | 67.9 | 73.0 |
| Image preference | 5 (Image ‘e’) | 70.3 | 73.0 |
| Intensity of pain | 5 (Excruciating) | 82.7 | 82.7 |
| Pain scale | 9 (out of 10) | 83.9 | 67.9 |
| Total score | 25 (out of 32) | 86.4 | 92.0 |
| Total score (no images) | 20.5 (out of 32) | 92.6 | 93.9 |
| Statistics According to Gender | Nature of Pain | Image Preference | Intensity of Pain | Pain Scale | Total Score | Total Score (without Images) | |
|---|---|---|---|---|---|---|---|
| Cut off | Male | 3 | 5 | 5 | 9 | 23.6/32 | 20/32 |
| Female | 3 | 6 | 5 | 9 | 25.0/32 | 20.5/32 | |
| Sensitivity (%) | Male | 60.7 | 66.6 | 80.3 | 84.3 | 90.1 | 94.1 |
| Female | 80.0 | 73.3 | 86.6 | 83.3 | 90.0 | 93.3 | |
| Specificity (%) | Male | 68.5 | 77.1 | 91.4 | 77.1 | 94.2 | 94.2 |
| Female | 73.8 | 79.4 | 81.1 | 66.1 | 91.6 | 93.3 | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Buture, A.; Boland, J.W.; Dikomitis, L.; Huang, C.; Ahmed, F. Development and Evaluation of a Screening Tool to Aid the Diagnosis of Cluster Headache. Brain Sci. 2020, 10, 77. https://doi.org/10.3390/brainsci10020077
Buture A, Boland JW, Dikomitis L, Huang C, Ahmed F. Development and Evaluation of a Screening Tool to Aid the Diagnosis of Cluster Headache. Brain Sciences. 2020; 10(2):77. https://doi.org/10.3390/brainsci10020077
Chicago/Turabian StyleButure, Alina, Jason W Boland, Lisa Dikomitis, Chao Huang, and Fayyaz Ahmed. 2020. "Development and Evaluation of a Screening Tool to Aid the Diagnosis of Cluster Headache" Brain Sciences 10, no. 2: 77. https://doi.org/10.3390/brainsci10020077





