1. Introduction
In the 1970s, Warrington’s description of three individuals with a selective and profound inability to name and recognise objects [
1] laid the foundation for what years later, in 1989, would be coined “semantic dementia” [
2]. Semantic dementia, now widely referred to as semantic variant primary progressive aphasia (svPPA), is a neurodegenerative syndrome characterised by progressive loss of semantic knowledge in the context of otherwise well-preserved language and cognitive abilities [
3,
4]. Current consensus criteria require language impairment to be the most salient clinical symptom and the main cause of impairment in daily living activities [
3,
5]. Clinically, individuals with svPPA present with fluent speech (preserved repetition and speech production) and loss of semantic knowledge across all modalities of testing (e.g., picture naming, single-word comprehension and visual association tasks). As the disease progresses, behavioural features emerge, and speech becomes increasingly empty, culminating with mutism in the final stages [
6]. An illustrative example is provided by the response of one woman with svPPA who, when asked about her symptoms, pointed to the trees in the hospital’s courtyard and said, “I don’t know what those green things are anymore”.
SvPPA is estimated to account for one-third of all cases of frontotemporal dementia [
7] with an average age at symptom onset of 60 years (64 years for diagnosis to be established). The prognosis for length of survival following diagnosis is highly variable, with a median of 12 years [
8]. MRI brain scans typically reveal bilateral and asymmetric temporal pole atrophy (greater on the left) and asymmetric anterior hippocampal atrophy [
9]. Furthermore, the anterior portion of the fusiform gyrus and adjacent regions are also critical areas systematically affected in svPPA and appear to play a pivotal role in semantic degradation [
10,
11,
12,
13]. Between 75% and 100% of all svPPA cases are associated with underlying TDP-43-C pathology, with the remainder mostly involving FTD tau [
8,
14,
15,
16] and a small proportion of cases showing concomitant Alzheimer’s disease pathology [
8,
17].
There is no curative or disease-modifying treatment for svPPA. However, a growing body of research on non-pharmacological interventions has shown that people with svPPA may relearn lost vocabulary and benefit from other behavioural therapies. The first rehabilitation reports emerged in the literature in the late 1990s, inspired by patients who spontaneously engaged in self-practice as an attempted remedy for their anomia [
18,
19]. The proliferation of single case studies and small group studies over the next decades have demonstrated that people with svPPA who receive naming therapy can improve their recall of object labels in the short term, that the gains might be retained over time and that at least partial restoration of semantic knowledge may be possible (see reviews by Carthery-Gouland et al. [
20], Jokel et al., [
21], Cotelli et al., [
22] and Pagnoni et al. [
23] for an overview). Furthermore, the breadth of research into non-pharmacological interventions has by no means remained restricted to word retrieval. Therapeutic approaches targeting conversation [
24], tasks and activities of daily living [
25,
26,
27], psychoeducation programmes [
28,
29] and peer support groups [
30] have made headway and are on the increase. Altogether they have set the stage for an integrative framework of clinical treatment and care in svPPA that combines rehabilitation interventions, compensatory approaches and provision of education and support, addressing the language impairment in svPPA within the context of dementia [
31]. This article aimed to synthesise the learnings from 20 years of research in the non-pharmacological treatment and management of svPPA and lay out evidence-based recommendations for clinical practice and future research. For the purposes of education and dissemination beyond an academic audience, this article includes a lay summary available in English, Spanish and French (
Supplementary Materials S1–S3).
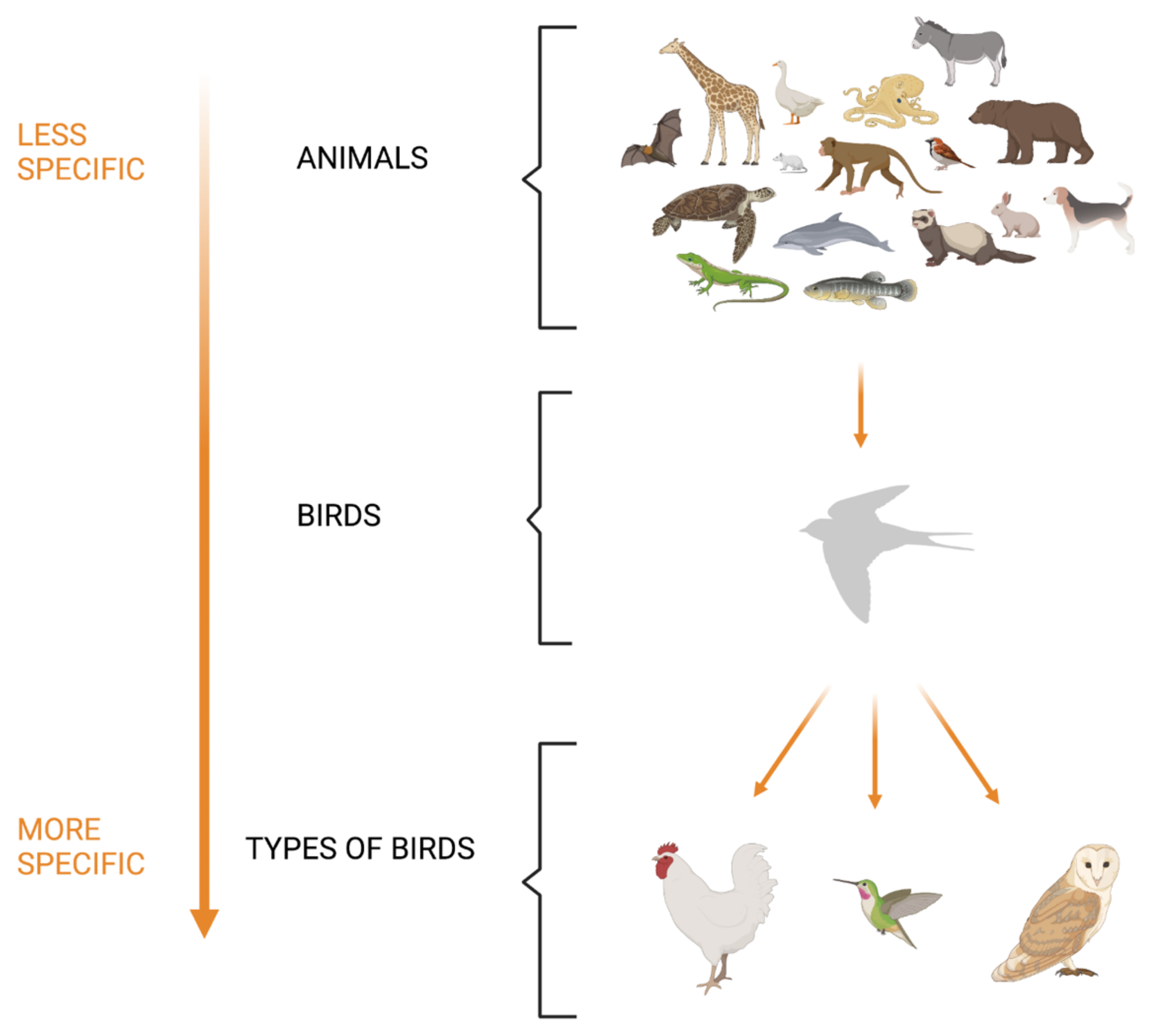
2. Anomia in svPPA as a Sign of Semantic Breakdown
There is evidence that the anomia seen in svPPA stems from impairment in semantic knowledge [
32]. This is different from the word retrieval impairments shown in the other PPA variants that arise at the lexical/phonological (logopenic variant PPA) or post-lexical (non-fluent/agrammatic PPA) [
33] stages. A basic understanding of how semantic memory architecture works is therefore required to develop effective treatments. A common theory is that semantic knowledge is organised in a hierarchy of specificity [
1,
34], ranging from very specific attributes at the bottom (e.g., the hummingbird is a small bird that can hover) to very general knowledge at the top (e.g., a hummingbird is an animal) (see
Figure 1).
Specific attributes are hypothesised to degrade first in a continuum of progressive degeneration that continues with the loss of general attributes and culminates in the disappearance of the concept. For instance, a person may identify a hummingbird as a living thing without being able to identify its specific properties (e.g., that it can fly and feeds on flower’s nectar). This means that, during cognitive and language assessment, partial provision of information should not be interpreted as unequivocal proof of complete semantic preservation. Further investigation of semantic integrity should always be pursued in people with svPPA in preparation for therapy.
Leveraging Episodic Memory
Episodic memory (e.g., the ability to remember where you parked your car, what you did yesterday evening, or the plumage of a bird that is new to you) is a main entry point of semantic information into the memory system. This new information is integrated into existing bodies of knowledge by a dual system supported by the hippocampus (allowing quick capture of episodes) and neocortical structures (allowing a slower but effective integration into a long-term database) [
35]. More specifically, in this second neocortical stage, information is consolidated in integrated, generalisable representations across a network distributed along the neocortex, tapping into the sensory, motor and linguistic systems [
36]. Cross-modal interaction of these areas has been hypothesised to be anatomically supported by the anterior temporal lobes (ATLs) that operate as a hub where different forms of semantic information converge and connect [
37,
38]. This ATL region is affected at an early stage by the bilateral pathological aggregation of proteins associated with svPPA. However, the brain structures supporting episodic memory, such as the posterior area of the hippocampus and posterior cingulate cortex [
39], are usually reasonably preserved. This suggests that, in principle, the episodic memory gateway to inputs that will eventually transform into re-learned concepts may remain functional. Consequently, this mechanism may be used, in conjunction with partially degraded neocortical structures, to the advantage of rehabilitation goals [
40].
3. Differences between Left and Right Variants: Implications for Practice
The usual pattern of brain atrophy in svPPA (left greater than right) is reversed in approximately 30% of cases (i.e., right greater than left), giving rise to left and right-sided variants (left-svPPA and right-svPPA respectively) [
41,
42,
43] (see
Figure 2). Left-svPPA is characterised by poorer performance on verbal tasks compared to right-svPPA [
13,
43,
44]. At the time of presentation, the prevalence of word-finding difficulties in left-svPPA is reported to be 94%, compared to 36% in right-svPPA, while impairments in single-word comprehension are reported in 67% of left-svPPA and 18% of right [
43]. In contrast, individuals with right-svPPA show greater impairment of non-verbal semantics [
38,
42,
43]. In up to 91% of cases with right-svPPA, the clinical picture is characterised by prosopagnosia (a difficulty in recognising faces) that for these individuals is associated with person-specific semantic knowledge breakdown [
42,
45,
46,
47,
48,
49]. Behavioural changes, although reported in both variants, seem to be more pronounced and appear earlier in right-svPPA, with social awkwardness and loss of insight are commonly reported (present in 64% and 55% of individuals respectively) [
43] along with loss of empathy, disinhibition, apathy and compulsiveness [
42,
45,
48].
Analysis of the types of naming errors produced by each group suggests that individuals with right-svPPA might have more difficulty accessing semantic knowledge through visual than verbal modalities (e.g., more difficulty recognising a famous face by looking at a photograph than by listening to a description of the person) (see
Table 1). Individuals with left-svPPA show a larger proportion of circumlocutions in response to naming difficulties (e.g., “when it rains” for umbrella) and omissions [
44,
50] compared to right-svPPA, while those with right-svPPA make more coordinate and superordinate semantic errors (e.g., coordinate: “cat” for “dog” and superordinate: “animal” for “dog”) [
44,
50]. The reduced ability of these individuals to access knowledge through visual features has been proposed as a possible mechanism that contributes to their greater difficulty in producing semantic associations, predisposing them to production of more taxonomic (coordinated and superordinate) semantic errors [
44].
In light of this evidence, clinicians should pay particular attention to a few factors. First, whether verbal material (e.g., audio recordings, verbal descriptions and sounds) may be preferable to visual (e.g., photographs and real objects) should be considered when treating individuals with right-svPPA. Second, individuals with left-svPPA seem better able to access residual associated semantic knowledge and use this to describe the target when attempting to name. This can be used as a therapeutic opportunity, for instance, by encouraging the individual to retrieve this residual knowledge and relink it with the label.
4. The Current Evidence Informing Treatment and Management of Anomia and Word Comprehension Deficits
4.1. How Should Therapies for Anomia Be Designed and Administered?
Typically, lexical training therapies have consisted of a set of items given to individuals to practice. Therapy in svPPA should focus on maintaining or improving access to both names and semantic representations. Below, we present a summary of how these therapies should be planned and administered in svPPA based on a synthesis of current evidence.
4.2. Who Benefits from Anomia Therapy?
Benefits of therapy have been shown across a range of severities of anomia, provided some level of spoken language is preserved (i.e., there are no studies of individuals who are mute). This suggests that, in principle, the level of severity should not prevent any individual with svPPA from being considered for treatment, although the nature of the intervention would differ based on the level of severity. People in the early stages may have the advantage of retaining more semantic knowledge on which to build the therapy. They are also more likely to be free of other cognitive or behavioural symptoms that may impact successful engagement with therapy and, in fact, circumscribed semantic impairments longer than 6 years post-onset have been reported in some individuals [
51,
52,
53,
54].
4.3. How Many Sessions, of What Length and How Many Items per Session?
Current evidence suggests that 20–60 min of daily (or almost daily) practice is effective to produce short-term benefits [
51,
52,
55,
56,
57], although some individuals have also shown benefits from less. Significant improvements should be expected within the first month of consistent practice [
40,
52,
53,
58,
59,
60,
61,
62,
63,
64] but may be evident sooner. Most studies to date have combined face-to-face sessions with the therapist with self-administered home programmes. Usual set size is between 15 and 30 items per session [
51,
52,
53,
54,
58,
60,
63,
65].
4.4. What Kind of Items and Naming Therapy?
Two kinds of words have been targeted in therapy: those that still are associated with some residual semantic knowledge and those that are not. A word is considered to have residual knowledge when the person can produce or comprehend at least partial information about it (e.g., “it’s food” for an egg, without being able to connect the association between an egg and a hen). These words are by far the most investigated in the lexical retrieval literature. Words where meaning is completely lost have, on the contrary, been less investigated and the few studies looking at the use of conceptual enrichment therapies to treat words destitute of semantic knowledge have produced mixed results [
66,
67]. A list of the techniques used in the svPPA rehabilitation literature is shown in
Table 2.
One of the most common approaches to improving naming is the “Look, listen and repeat” (LLR) or “Repetition (and reading) in the presence of the picture (RRIPP)”. A picture of the target concept is presented, along with the name as a spoken and/or written word for the individual to repeat/read aloud, sometimes preceded by an attempt at naming, with or without (semantic or phonological) cues. Multiple variations of this approach have proven effective for improving production of vocabulary that the person with svPPA can still comprehend (see
Table 2). However, this technique can lead to rote-learning (rigid and context-specific) and poor generalisation when semantic knowledge of the trained item is very impaired (e.g., the person can no longer comprehend either the lexical label or a picture of the object). Restitutive training of words/concepts that the person can no longer comprehend has been less explored in the literature. The suitability of a semantic approach to treating these items (e.g., working on characteristics of an object’s usage and location and linking it with other related memories) is supported by two types of studies. The first consists of studies looking at the direct restoration of semantic knowledge [
66,
67,
70] and the second capitalising on residual semantic information to boost word retrieval [
18,
40,
52,
53,
55,
58,
60,
62,
63,
66,
68,
69,
70,
71]. Both contribute to understanding the importance of the semantic system in the rehabilitation of svPPA. For instance, the naming of items with residual semantic knowledge appears to be easier to rehabilitate than that of items completely devoid of meaning [
53,
58]. Likewise, greater success is achieved with familiar items—familiar concepts degrade slower due to the larger and stronger network of semantic connections that are regularly reinforced with use (e.g., the concept of a toaster, used daily for breakfast, will be retained for longer than a hammer that is borrowed from a neighbour and used occasionally) [
53,
58,
60,
84]. In this same vein, some authors have introduced photos of individuals’ own items within their therapy material (rather than generic exemplars), to harness familiarity and personal significance [
51,
54,
65,
82]. Others have identified semantic attributes of exemplars [
76] or sorted items within semantic categories [
18,
51,
54,
65] to further reinforce the semantic concept (but randomise the order of items with each presentation to avoid rote learning).
4.5. Are These Therapies Well Accepted by People with svPPA?
Most studies of word retrieval therapy in svPPA have shown good adherence of people to practice. In many cases, participants completed home programmes consistently for many months. The first lexical retrieval therapy studies were prompted by individuals who started self-practice on their own initiative, evidencing their keenness to play an active role in their treatment [
18]. Inevitably, individuals reported in the literature are those who volunteered for research and are probably particularly motivated to pursue therapy, which may not be the case when extrapolating to the broader clinical population. It has been reported that, in clinical settings, individuals with PPA who receive lexical retrieval therapy show a rate of adherence of 60% [
85]. The authors of that study found that adherence was more likely when the treatment commenced in the year after diagnosis and when the patient was motivated, and mood was stable. Clearly, there will be people with svPPA who may prefer not to engage in lexical therapy for various reasons. In these cases, there is still a wide range of therapeutic options that can be offered (e.g., use of compensatory techniques, environmental adaptations, partner training and psychological support).
4.6. Are People with svPPA Aware of Their Deficits?
People with svPPA typically recognise that their language performance has weakened. However, some individuals appear to have difficulties evaluating their past knowledge of words (even in realising that certain words ever existed) and the extent of the impoverishment of their language content. For instance, Savage et al. [
86] reported that people with svPPA who have mild to moderate semantic impairments showed no awareness of obvious mislabelling errors when naming components of objects. The authors of the study warn about the implications that this may have regarding patients’ role and input into rehabilitation planning and recommend that rehabilitation programmes should not be based on patients’ judgment alone and instead also involve family members and friends.
4.7. How Long Does the Effect of Therapy Last?
Many studies have demonstrated that the significant improvements in naming are often very well maintained over the first month after ceasing practice [
40,
52,
54,
56,
59,
63,
81]. Outcomes beyond this, however, are variable. For some people with svPPA, a high proportion (73–82%) of the words named at the end of treatment can still be successfully named 3 to 6 months later [
54,
60,
63,
82]. In others, levels of retention in that time window are modest (e.g., around 65% of trained words) [
53,
62,
65] or low (e.g., only 10–40% of words are maintained) [
58,
68]. Encouragingly, the majority of studies report performance that continues to be above baseline levels for up to 6 months after completing treatment [
87]. These benefits have also been observed 12 months post-treatment in a small number of studies [
82].
The extent of retention may be influenced by the degree of semantic knowledge still retained for an item (i.e., meaningful items persist longer [
58]) and the opportunity to continue rehearsing items in everyday life [
54,
60,
68]. This is consistent with observations that autobiographical experience and subsequent conversations regarding such experiences, may enhance semantic knowledge and preserve these words over time [
81,
82,
84]. While this integration of the use of words in everyday life plays an important role in retaining vocabulary, many words (e.g., stove, plate) may not be used often enough in everyday conversation to allow regular practice, requiring alternative strategies for ongoing reinforcement. One feasible alternative is maintaining regular revision of the re-learned words. While daily practice may be needed in the early phases of an intervention, successful maintenance revisions (to maintain at least 80% of therapy items) require less practice [
54]. For instance, when monitored over a 6 month period, people with svPPA with a moderate level of impairment needed less than 10 revision sessions over 6 months to maintain their naming. For those with more severe semantic impairment, Savage et al. [
51,
54] found that regular, weekly practice was needed to restore the benefits of the initial intense training. In particular, performance at around 2 months post-intervention appears to be a useful indicator of the frequency of revision that could be required for sustained maintenance—implying that this is a useful time point for clinicians to monitor and then formulate the revision programme for those people with mild to moderate svPPA.
A practical consideration for people with svPPA and their families then becomes how long to continue with interventions. In some cases [
54,
68], the practice simply becomes part of the usual routine or there may be enjoyment gained from it. Consistent with this, some studies have reported ongoing practice persisting for 1–2 years [
55,
88]. For some individuals, however, where declines in performance may become upsetting or practice becomes stressful, it may not be desirable to continue. In these circumstances, individuals with PPA and their families should be prepared for declines to emerge over the months that follow.
4.8. Does This Learning Generalise?
An important aspect of any rehabilitation programme is the degree to which improvements extend from the intervention to assist the person in their daily living. The generalisation of benefits in svPPA has been usually evaluated in two ways: (1) whether naming improvements extend from trained to untrained words and (2) whether words can be used by the person with svPPA in contexts that differ from the training format. Generalisation of naming improvements, extending from trained to untrained words, have been observed in some individuals with non-progressive aphasia, but usually only when the impairment is one of phonological encoding, in the absence of significant semantic or lexical deficits [
89]. A consistent finding across most svPPA treatment studies is that untrained words do not improve [
21,
25] with very few exceptions showing the opposite result [
81,
82].
An alternative way of considering the generalisation of naming therapies is to evaluate the extent to which trained words can be used by the person with svPPA in contexts that differ from the training format. Broadly, this may be divided into “near transfer”—wherein the demonstration of knowledge is highly similar to the original training context (e.g., asking the person to produce the word in response to a different exemplar of the stimulus—see
Figure 2 in Heredia et al. [
60]) or “far transfer”—where knowledge must be applied more flexibly (e.g., by completing a different kind of language task such as verbal comprehension) [
90]. Successful naming has been observed when people with svPPA are tested on alternative versions of trained items [
52,
63] or photographs of target items taken from different views [
60,
66] but much less when they are required to name visually dissimilar versions of the trained item [
40,
60,
72,
91]. Encouragingly, evidence of producing trained words in other contexts after word training, such as fluency tasks (in one individual [
63], naming to description [
66], describing short videos of everyday scenes [
51] or in production of a simple sentence construction, have also been observed [
91].
To increase the chances of people with svPPA being able to correctly use the trained words in their everyday lives, it is helpful to tailor training stimuli to visually match the objects found within a person’s home (likewise in actual object use, which was found to depend on personal familiarity with object exemplars [
92]).
4.9. What Evidence Do We Have about Prophylactic Treatment in svPPA?
Prophylactic/preventative treatment aims to help retain current abilities by practising intact skills or items. There is some evidence suggesting that such preventative interventions may hold value in svPPA [
73,
78]. Several studies have found that treatment of items that could already be successfully named may slow the progression of semantic loss and anomia for those items [
52,
53,
54,
56].
4.10. Can We Deliver These Therapies Remotely? What Evidence Do We Have?
Digital technologies in treatment programmes provide opportunities to increase access for those with svPPA and their families who struggle to access expert care because of geographic location. Delivery of treatment via telehealth is highly relevant given the limited access to services for many individuals with PPA [
78,
83,
93,
94]. Significant improvements in word retrieval have been achieved after completing home-based programmes using either hardcopy or computer-mediated materials [
18,
40,
53,
54,
58,
60,
65,
66,
68,
95]. Rogalski and colleagues examined the feasibility of teletherapy for 28 individuals with PPA [
96] showing that treatment delivered via video conferencing has the potential to improve access to care for people with PPA. Two studies conducted on people with svPPA show that lexical retrieval therapy can be delivered in-person or by teletherapy with similar results [
78,
83].
4.11. What Are the Barriers and Facilitators of Online Therapy?
Recognition of the barriers to, and facilitators of, successful implementation of remote digital therapy, however, is extremely important in both the research and clinical setting. Disease severity has been noted by several studies to be a contraindication for remote therapy and there is a recommendation that individuals participating in remote therapy should preferably be in the early to mid-stages of disease progression [
83,
91,
96]. The inherent requirements of a technology can also be a barrier with the quality of audio and the stability of the internet connection being a prerequisite to successful participation online. In addition, the individual must possess adequate computer skills or a suitable support person to facilitate participation, particularly when carrying out intervention independently at home rather than supervised over the internet.
An example of these barriers, acting in concert, is provided by Taylor-Rubin et al. [
91], reporting a series of single-case design treatment studies where lexical retrieval treatment was delivered via a computer-mediated home programme. Two of three svPPA participants had significant improvement in verb and noun production, following lexical retrieval treatment. However, a third participant, Nsv, showed only marginal gains over two blocks of lexical retrieval treatment. The authors hypothesised that as Nsv was five years post-onset, the severity of impairment may have contributed to less positive treatment results. Practice logs indicated poor adherence with computer operating difficulties preventing completion of all treatment schedule sessions in the second block of treatment [
91].
A further barrier can be the lack of contact with the therapist. Caregivers in Rogalski’s study reported that less than optimum opportunities for face-to-face support for the person with PPA, in times of distress, was a limitation of participation in the web-based treatment programme [
96]. Similarly, caregivers of people with PPA, including svPPA, reported, in a study of treatment adherence, that home treatment programmes can be lonely and socially isolating and this would be anticipated to reduce adherence, “It is easier to fall off the wagon with a programme at home” [
85]. Finally, the barrier of social isolation could be minimised by innovative networking; pairing peers with svPPA in small online groups, thus incorporating support, increased social participation and positive experiences [
30].
5. Compensatory Approaches to Support Communication in svPPA
Aside from the direct treatment of language, a number of single-case studies have explored the benefit of using a compensatory approach to support language difficulties, particularly naming, in svPPA [
26,
97,
98,
99]. Compensatory approaches include the use of external devices to support communication, such as compensatory augmentative and alternative communication (AAC) systems [
100]. These can be based on low (e.g., paper communication board or notebooks) or high technology (e.g., smartphones or tablets and computers); people with svPPA may use them in conjunction with verbal communication in a multi-modal way, multiplying the communication options available to them [
100].
In two case studies, Bier and collaborators [
26,
97] explored the potential of using smartphone applications to help two people with svPPA learn how to search for information related to lost concepts through Internet search engines or a visual dictionary application named ARCUS
©. This application aimed to support the retrieval of people’s names from a virtual name directory using clues or information chosen by the person with svPPA. ARCUS
© was successfully used by ND, a recreation therapist in a senior living facility with early svPPA [
97]. In his work, ND had to identify a large number of people by name each day. At the start of the study, he used a paper notebook to do this, organised into several columns, each linked to a different piece of information (e.g., resident’s room number or employee’s job type). The authors converted ND’s notebook into a smartphone application to ease its use and reduce the stigma associated with it. ND phased out his paper-based compensatory system in favour of this new, more flexible name retrieval system. Four years later, ND had extended the use of ARCUS
© by adapting it to record information about grocery stores and food items to buy before he went shopping.
Another recent study has combined the classical use of mobile technology to develop CoChat, an app constructed on natural language processing (NLP) features, social media use, and just-in-time principles that was tested in two people with svPPA [
98]. In this app the user takes a photograph with the tablet’s built-in camera, shares the pictures with the person’s simulated social network (e.g., family and friends) and sees comments to the images in real time. Results suggest that CoChat may improve word retrieval in a natural conversational context making conversations easier when using the app. As AAC devices and systems are becoming common practice in aphasia, further studies will have to deepen our understanding of how these types of tools can be optimised in svPPA.
Semantic deficits may sometimes prevent people with svPPA from understanding task requirements and limit their ability to learn certain functions of assistive technological devices [
26,
97] (e.g., being able to remember the series of actions required to obtain an Internet connection, but not understanding why). Nevertheless, taken together, these case studies suggest that it is possible to teach the use of practical, portable solutions to compensate for semantic memory deficits. Considering the degenerative nature of svPPA, it is important to integrate AAC with other treatment approaches as early as possible in the disease process so that they are well practised before the skills to acquire their use are lost [
98,
100]. Finally, although strategies of functional communication have been explored in individuals with PPA in general, there is a lack of studies examining non-AAC compensatory strategies targeting svPPA in particular.
6. Interventions to Support Activities of Daily Living
Complementary approaches that support engagement or re-engagement in meaningful activities of daily living are also important. Participation in meaningful activity is the primary focus of these kinds of interventions, without special consideration for language skills—although these may also benefit. They are oriented toward two objectives: (1) capitalising upon preserved episodic (e.g., what you had for lunch) and procedural memory functions (e.g., how to perform different skills, such as tying your shoes); (2) focusing on significant and meaningful everyday activities that will have immediate results and a potential impact on well-being.
To our knowledge, only two studies have explored the engagement, or re-engagement, in meaningful daily living activities in svPPA [
27,
101]. In the first study, Bier et al. [
27] did so by combining the repeated practice of an activity that the person had stopped doing (e.g., meal preparation) with a step-by-step cognitive assistive technology (SemAssist
©). The objective was to support EC, a woman with left svPPA, to relearn how to prepare a specific recipe of her choice. This study showed that EC mainly used SemAssist
© to follow the current steps during the activity. While she made many mistakes before the therapy sessions began, she was able to complete the recipe without error by the end of the process. Interestingly, EC also resumed spontaneous preparation of other recipes, showing that she had acquired new “knowledge” about the ingredients from the recipes she practised (e.g., “goes in the shrimp recipe”) and did not overgeneralise. In the second study, O’Connor et al. [
101] applied the Tailored Activity Program (TAP) with a person with svPPA who had highly repetitive routine behaviours. The TAP intervention resulted in this person engaging well in prescribed activities, with scores reflecting reduced carer distress regarding challenging behaviours and improved caregiver vigilance.
It therefore seems appropriate and promising to combine traditional language-based approaches with an interdisciplinary intervention that also incorporates a participatory approach such as occupational therapy or other meaningful activity interventions in svPPA.
7. Support Groups and Educational Programmes
One of the most recent developments in therapy for primary progressive aphasia is in group-based programmes offering education and support. While none of the published reports are specific to a particular PPA variant, they do include individuals with svPPA. In 2017, Jokel and colleagues published the first report of a group intervention programme that included both individuals with PPA and their caregivers [
102]. The group members not only shared the intervention focus but, importantly, actively participated in defining it. Half of each session was spent on education, counselling and/or training communication strategies in dyads. The other half was separated into language activities for people with PPA and networking activities for caregivers. All participants reported valuing learning about the nature, progression and types of PPA, becoming familiar with current research in PPA, and several other aspects of the intervention. Components that were reported to be beneficial included receiving information on nutrition and lifestyle to support brain health, learning strategies for managing stress and depression, feeling understood by others in the group when experiencing difficulties during verbal communication, and getting support from multiple disciplines.
Although not specific to svPPA, to date, three more group interventions for PPA have also been reported [
29,
30,
98]. Mooney and colleagues [
98] developed a PPA group treatment model that incorporated elements of three methodologies used in language rehabilitation: communication strategies from augmentative and alternative communication, communication partner training from aphasia rehabilitation, and systematic instruction from dementia management. Morhardt et al. [
29] describe the development of a programme that offered education, communication strategies, strategies to “live well” with PPA and non-language-based activities (e.g., watercolour painting and horticultural therapy). Finally, Taylor-Rubin et al. [
30] delivered PPA education and support for a group of people with PPA and their caregivers in the early post-diagnostic period. In the post-intervention interview, participants highlighted the reduced feelings of isolation, increased feelings of support, increased knowledge of coping strategies and improved understanding of PPA as a result of participating in the programme soon after the receipt of the PPA diagnosis.
Based on the outcomes of these group interventions in PPA, several factors have emerged that may be critical to PPA care. First and foremost, the needs of both patients and caregivers should be addressed, preferably simultaneously [
28,
30]. A successful intervention programme for PPA should provide not just language activities and education but also a safe forum for discussing important and difficult issues, for sharing successes and failures, and for peer education. Such a programme is likely to ultimately result in improvements in confidence and well-being for both individuals with PPA and their caregivers. Published studies underline that PPA-specific education and ecologically valid context (i.e., group format) are positive elements highlighted by all participants. In addition, having consistent peer support helps to “normalise” daily challenges. It has been suggested that self-help groups may be beneficial in maintaining the group intervention benefits and they are recommended even in the absence of professional input [
103].
As more and more services are being offered online, the support for individuals dealing with svPPA may also migrate to virtual space. A review of virtual support groups for dementia caregivers [
104] suggests that weekly or monthly sessions can provide participants with knowledge about dementia, caregiving skills, coping strategies and access to resources. While occasional barriers, such as technology and access, were identified, there are also numerous economic and geographical advantages to online group sessions. Extrapolating from the broad dementia field, we may predict that the trend towards virtual care in svPPA will continue.
8. Future Directions in Behavioural Therapies in svPPA
We have shown in this synthesis of evidence that there has been relatively little research on intervention for words and concepts that the person with svPPA can no longer understand, and that therapy gains for such words show limited generalisation. Far from indicating that conceptual restoration or generalisation is not possible, we argue that optimal treatments may not yet have been found, and that this should motivate future research. On the other hand, the use of compensatory approaches to supporting communication and activities of daily living (e.g., assistive technologies) is promising and has the potential to make a difference to the lives of people with svPPA. The next steps should therefore be directed towards: (1) the development of more precise naming therapies, tailored to the level of semantic degradation of the words and concepts treated; (2) finding ways to guarantee transfer and generalisation of therapy gains to daily life; (3) expanding research into the use of assistive technologies, compensatory strategies, programmes to support daily living and how and when to combine these components.
9. Conclusions
The last two decades have witnessed rapid advances in the understanding and treatment of svPPA. The current body of research suggests that people with svPPA who have access to non-pharmacological therapies show favourable outcomes and long-lasting effects that can have benefits for health outcomes. Moreover, these treatments are generally well accepted. Although there is a lack of empirical research examining what the optimal combination and timing for treatments are, there are general guidelines for delivering language therapy at different stages of PPA that offer pragmatic advice about how to combine different therapy approaches in a meaningful way [
105]. Current ongoing research around the staging of PPA (including svPPA) will make it easier to match therapies to impairments in the future. We therefore advocate for the svPPA care pathway to include a wide range of therapeutic options including both restorative and compensatory strategies and educational and support groups for people with svPPA as well as their care partners. These therapeutic options have the potential to become more accessible due to the advent of telemedicine, which has overcome geographical barriers and can provide care of similar efficacy to face-to-face therapy. Finally, to facilitate dissemination beyond an academic audience we have included a lay summary in English, Spanish and French (
Supplementary Materials S1–S3).
Supplementary Materials
The following are available online at
https://www.mdpi.com/article/10.3390/brainsci11121552/s1. Supplementary 1 (English). Semantic Variant Primary Progressive Aphasia (svPPA): evidence-based recommendations for therapy and management; Supplementary 2 (French). Variante sémantique de l’aphasie progressive primaire (vsAPP): indications fondées sur les données probantes pour le traitement et la prise en charge; Supplementary 3 (Spanish). Variante semántica de la afasia progresiva primaria (APP-s): recomendaciones basadas en evidencia para el manejo terapéutico.
Author Contributions
A.S.-G. and C.T.-R. contributed to the conceptualisation, original draft preparation, critical review and editing. S.A.S., N.B. and R.J. contributed to the original draft preparation, critical review and editing. M.L.H. and L.N. contributed to the critical review and editing. All authors have read and agreed to the published version of the manuscript.
Funding
A.S.-G. was funded by a UKRI Healthy Ageing Challenge Catalyst Award (ES/W006405/1) and a grant jointly funded by the Economic and Social Research Council (UK) and the National Institute for Health Research (UK) (ES/S010467/1). N.B. was supported by a research scholarship from the Fonds de la recherche du Québec-Santé. M.H. was funded by the National Institutes of Health (NIDCD R01DC016291) and by the Darrell K Royal Research Fund for Alzheimer’s Disease.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Warrington, E.K. The Selective Impairment of Semantic Memory. Q. J. Exp. Psychol. 1975, 27, 635–657. [Google Scholar] [CrossRef] [PubMed]
- Julie, S.; Goulding, P.J.; Neary, D. Semantic dementia: A form of circumscribed cerebral atrophy. Behav. Neurol. 1989, 2, 167–182. [Google Scholar] [CrossRef]
- Gorno-Tempini, M.L.; Hillis, A.E.; Weintraub, S.; Kertesz, A.; Mendez, M.; Cappa, S.F.; Ogar, J.M.; Rohrer, J.D.; Black, S.; Boeve, B.F.; et al. Classification of primary progressive aphasia and its variants. Neurology 2011, 76, 1006–1014. [Google Scholar] [CrossRef] [Green Version]
- Neary, D.; Snowden, J.; Gustafson, L.; Passant, U.; Stuss, D.; Black, S.; Freedman, M.; Kertesz, A.; Robert, P.H.; Albert, M.; et al. Frontotemporal lobar degeneration: A consensus on clinical diagnostic criteria. Neurology 1998, 51, 1546–1554. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mesulam, M.M. Primary progressive aphasia. Ann. Neurol. 2001, 49, 425–432. [Google Scholar] [CrossRef] [PubMed]
- Harciarek, M.; Sitek, E.J.; Kertesz, A. The patterns of progression in primary progressive aphasia—Implications for assessment and management. Aphasiology 2014, 28, 964–980. [Google Scholar] [CrossRef]
- Coyle-Gilchrist, I.T.; Dick, K.M.; Patterson, K.; Rodríquez, P.V.; Wehmann, E.; Wilcox, A.; Lansdall, C.J.; Dawson, K.E.; Wiggins, J.; Mead, S.; et al. Prevalence, characteristics, and survival of frontotemporal lobar degeneration syndromes. Neurology 2016, 86, 1736–1743. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hodges, J.R.; Mitchell, J.; Dawson, K.; Spillantini, M.G.; Xuereb, J.H.; McMonagle, P.; Nestor, P.J.; Patterson, K. Semantic dementia: Demography, familial factors and survival in a consecutive series of 100 cases. Brain 2010, 133, 300–306. [Google Scholar] [CrossRef] [Green Version]
- Chan, D.; Fox, N.C.; Scahill, R.I.; Crum, W.R.; Whitwell, J.L.; Leschziner, G.; Rossor, A.M.; Stevens, J.M.; Cipolotti, L.; Rossor, M.N. Patterns of temporal lobe atrophy in semantic dementia and Alzheimer’s disease. Ann. Neurol. 2001, 49, 433–442. [Google Scholar] [CrossRef]
- Chen, K.; Ding, J.; Lin, B.; Huang, L.; Tang, L.; Bi, Y.; Han, Z.; Lv, Y.; Guo, Q. The neuropsychological profiles and semantic-critical regions of right semantic dementia. NeuroImage Clin. 2018, 19, 767–774. [Google Scholar] [CrossRef]
- Ding, J.; Chen, K.; Chen, Y.; Fang, Y.; Yang, Q.; Lv, Y.; Lin, N.; Bi, Y.; Guo, Q.; Han, Z. The Left Fusiform Gyrus is a Critical Region Contributing to the Core Behavioral Profile of Semantic Dementia. Front. Hum. Neurosci. 2016, 10, 215. [Google Scholar] [CrossRef] [Green Version]
- Yang, J.; Pan, P.; Song, W.; Shang, H.-F. Quantitative Meta-Analysis of Gray Matter Abnormalities in Semantic Dementia. J. Alzheimers Dis. 2012, 31, 827–833. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mion, M.; Patterson, K.; Acosta-Cabronero, J.; Pengas, G.; Izquierdo-Garcia, D.; Hong, Y.T.; Fryer, T.D.; Williams, G.B.; Hodges, J.R.; Nestor, P. What the left and right anterior fusiform gyri tell us about semantic memory. Brain 2010, 133, 3256–3268. [Google Scholar] [CrossRef] [Green Version]
- Hodges, J.R.; Davies, R.R.; Xuereb, J.H.; Casey, B.; Broe, M.; Bak, T.H.; Kril, J.J.; Halliday, G.M. Clinicopathological correlates in frontotemporal dementia. Ann. Neurol. 2004, 56, 399–406. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Davies, R.R.; Hodges, J.R.; Kril, J.J.; Patterson, K.; Halliday, G.M.; Xuereb, J.H. The pathological basis of semantic dementia. Brain 2005, 128, 1984–1995. [Google Scholar] [CrossRef]
- Grossman, M.; Wood, E.M.; Moore, P.; Neumann, M.; Kwong, L.; Forman, M.S.; Clark, C.M.; McCluskey, L.F.; Miller, B.L.; Lee, V.M.; et al. TDP-43 Pathologic Lesions and Clinical Phenotype in Frontotemporal Lobar Degeneration with Ubiquitin-Positive Inclusions. Arch. Neurol. 2007, 64, 1449. [Google Scholar] [CrossRef] [Green Version]
- Santos-Santos, M.A.; Rabinovici, G.D.; Iaccarino, L.; Ayakta, N.; Tammewar, G.; Lobach, I.; Henry, M.L.; Hubbard, I.; Mandelli, M.L.; Spinelli, E.; et al. Rates of Amyloid Imaging Positivity in Patients with Primary Progressive Aphasia. JAMA Neurol. 2018, 75, 342. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Graham, K.S.; Patterson, K.; Pratt, K.H.; Hodges, J.R. Relearning and subsequent forgetting of semantic category exemplars in a case of semantic dementia. Neuropsychology 1999, 13, 359–380. [Google Scholar] [CrossRef]
- Funnell, E. A case of forgotten knowledge. In Broken Memories: Case Studies in Memory Impairment; Campbell, R., Conway, M.A., Eds.; Wiley-Blackwell: Oxford, UK, 1995; pp. 225–236. [Google Scholar]
- Carthery-Goulart, M.T.; Silveira, A.D.; Machado, T.H.; Mansur, L.L.; Parente, M.A.; Senaha, M.L.; Brucki, S.M.; Nitrini, R. Nonpharmacological interventions for cognitive impairments following primary progressive aphasia: A systematic review of the literature. Dement. Neuropsychol. 2013, 7, 122–131. [Google Scholar] [CrossRef] [Green Version]
- Jokel, R.; Graham, N.L.; Rochon, E.; Leonard, C. Word retrieval therapies in primary progressive aphasia. Aphasiology 2014, 28, 1038–1068. [Google Scholar] [CrossRef]
- Cotelli, M.; Manenti, R.; Ferrari, C.; Gobbi, E.; Macis, A.; Cappa, S.F. Effectiveness of language training and non-invasive brain stimulation on oral and written naming performance in Primary Progressive Aphasia: A meta-analysis and systematic review. Neurosci. Biobehav. Rev. 2020, 108, 498–525. [Google Scholar] [CrossRef] [PubMed]
- Pagnoni, I.; Gobbi, E.; Premi, E.; Borroni, B.; Binetti, G.; Cotelli, M.; Manenti, R. Language training for oral and written naming impairment in primary progressive aphasia: A review. Transl. Neurodegener. 2021, 10, 24. [Google Scholar] [CrossRef] [PubMed]
- Taylor-Rubin, C.; Croot, K.; Power, E.; Savage, S.A.; Hodges, J.R.; Togher, L. Communication behaviors associated with successful conversation in semantic variant primary progressive aphasia. Int. Psychogeriatr. 2017, 29, 1619–1632. [Google Scholar] [CrossRef] [PubMed]
- Croot, K.; Nickels, L.; Laurence, F.; Manning, M. Impairment- and activity/participation-directed interventions in progressive language impairment: Clinical and theoretical issues. Aphasiology 2009, 23, 125–160. [Google Scholar] [CrossRef]
- Bier, N.; Brambati, S.; Macoir, J.; Paquette, G.; Schmitz, X.; Belleville, S.; Faucher, C.; Joubert, S. Relying on procedural memory to enhance independence in daily living activities: Smartphone use in a case of semantic dementia. Neuropsychol. Rehabil. 2015, 25, 913–915. [Google Scholar] [CrossRef]
- Bier, N.; Macoir, J.; Joubert, S.; Bottari, C.; Chayer, C.; Pigot, H.; Giroux, S.; Team, S. Cooking “Shrimp à la Créole”: A pilot study of an ecological rehabilitation in semantic dementia. Neuropsychol. Rehabil. 2011, 21, 455–483. [Google Scholar] [CrossRef] [PubMed]
- Jokel, R.; Meltzer, J. Group intervention for individuals with primary progressive aphasia and their spouses: Who comes first? J. Commun. Disord. 2017, 66, 51–64. [Google Scholar] [CrossRef]
- Morhardt, D.J.; O’Hara, M.C.; Zachrich, K.; Wieneke, C.; Rogalski, E.J. Development of a Psycho-Educational Support Program for Individuals with Primary Progressive Aphasia and their Care-Partners. Dementia 2019, 18, 1310–1327. [Google Scholar] [CrossRef]
- Taylor-Rubin, C.; Azizi, L.; Croot, K.; Nickels, L. Primary Progressive Aphasia Education and Support Groups: A Clinical Evaluation. Am. J. Alzheimers Dis. Demen. 2020, 35, 1533317519895638. [Google Scholar] [CrossRef] [Green Version]
- Taylor-Rubin, C.; Croot, K.; Nickels, L. Speech and language therapy in primary progressive aphasia: A critical review of current practice. Expert Rev. Neurother. 2021, 21, 419–430. [Google Scholar] [CrossRef]
- Lambon Ralph, M.A.; McClelland, J.L.; Patterson, K.; Galton, C.J.; Hodges, J.R. No right to speak? The relationship between object naming and semantic impairment: Neuropsychological evidence and a computational model. J. Cogn. Neurosci. 2001, 13, 341–356. [Google Scholar] [CrossRef]
- Rohrer, J.D.; Knight, W.D.; Warren, J.E.; Fox, N.C.; Rossor, M.N.; Warren, J.D. Word-finding difficulty: A clinical analysis of the progressive aphasias. Brain J. Neurol. 2008, 131 Pt 1, 8–38. [Google Scholar] [CrossRef] [Green Version]
- Hodges, J.R.; Graham, N.; Patterson, K. Charting the progression in semantic dementia: Implications for the organisation of semantic memory. Memory 1995, 3, 463–495. [Google Scholar] [CrossRef] [PubMed]
- O’Reilly, R.C.; Bhattacharyya, R.; Howard, M.D.; Ketz, N. Complementary learning systems. Cogn. Sci. 2014, 38, 1229–1248. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Patterson, K.; Nestor, P.J.; Rogers, T.T. Where do you know what you know? The representation of semantic knowledge in the human brain. Nat. Rev. Neurosci. 2007, 8, 976–987. [Google Scholar] [CrossRef]
- Patterson, K.; Lambon Ralph, M.A. The Hub-and-Spoke Hypothesis of Semantic Memory. In Neurobiology of Language; Elsevier: Amsterdam, The Netherlands, 2016; pp. 765–775. [Google Scholar]
- Ralph, M.A.L.; Jefferies, E.; Patterson, K.; Rogers, T.T. The neural and computational bases of semantic cognition. Nat. Rev. Neurosci. 2017, 18, 42–55. [Google Scholar] [CrossRef]
- Irish, M.; Bunk, S.; Tu, S.; Kamminga, J.; Hodges, J.R.; Hornberger, M.; Piguet, O. Preservation of episodic memory in semantic dementia: The importance of regions beyond the medial temporal lobes. Neuropsychologia 2016, 81, 50–60. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mayberry, E.J.; Sage, K.; Ehsan, S.; Ralph, M.A.L. Relearning in semantic dementia reflects contributions from both medial temporal lobe episodic and degraded neocortical semantic systems: Evidence in support of the complementary learning systems theory. Neuropsychologia 2011, 49, 3591–3598. [Google Scholar] [CrossRef]
- Kumfor, F.; Landin-Romero, R.; Devenney, E.; Hutchings, R.; Grasso, R.; Hodges, J.R.; Piguet, O. On the right side? A longitudinal study of left- versus right-lateralized semantic dementia. Brain 2016, 139, 986–998. [Google Scholar] [CrossRef] [Green Version]
- Thompson, S.A.; Patterson, K.; Hodges, J.R. Left/right asymmetry of atrophy in semantic dementia: Behavioral-cognitive implications. Neurology 2003, 61, 1196–1203. [Google Scholar] [CrossRef]
- Hodges, J.R.; Patterson, K. Semantic dementia: A unique clinicopathological syndrome. Lancet Neurol. 2007, 6, 1004–1014. [Google Scholar] [CrossRef]
- Woollams, A.M.; Patterson, K. Cognitive consequences of the left-right asymmetry of atrophy in semantic dementia. Cortex. 2018, 107, 64–77. [Google Scholar] [CrossRef]
- Ulugut Erkoyun, H.; Groot, C.; Heilbron, R.; Nelissen, A.; van Rossum, J.; Jutten, R.; Koene, T.; van der Flier, W.M.; Wattjes, M.P.; Scheltens, P.; et al. A clinical-radiological framework of the right temporal variant of frontotemporal dementia. Brain J. Neurol. 2020, 143, 2831–2843. [Google Scholar] [CrossRef]
- Josephs, K.A.; Whitwell, J.L.; Vemuri, P.; Senjem, M.L.; Boeve, B.F.; Knopman, D.S.; Smith, G.E.; Ivnik, R.J.; Petersen, R.C.; Jack, C.R. The anatomic correlate of prosopagnosia in semantic dementia. Neurology 2008, 71, 1628–1633. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nakachi, R.; Muramatsu, T.; Kato, M.; Akiyama, T.; Saito, F.; Yoshino, F.; Mimura, M.; Kashima, H. Progressive prosopagnosia at a very early stage of frontotemporal lobar degeneration. Psychogeriatrics 2007, 7, 155–162. [Google Scholar] [CrossRef]
- Henry, M.L.; Wilson, S.M.; Ogar, J.M.; Sidhu, M.S.; Rankin, K.P.; Cattaruzza, T.; Miller, B.L.; Gorno-Tempini, M.L.; Seeley, W.W. Neuropsychological, behavioral, and anatomical evolution in right temporal variant frontotemporal dementia: A longitudinal and post-mortem single case analysis. Neurocase 2014, 20, 100–109. [Google Scholar] [CrossRef] [PubMed]
- Suárez-González, A.; Crutch, S.J. Relearning knowledge for people in a case of right variant frontotemporal dementia. Neurocase 2016, 22, 130–134. [Google Scholar] [CrossRef] [PubMed]
- Snowden, J.S.; Harris, J.M.; Thompson, J.; Kobylecki, C.; Jones, M.; Richardson, A.M.; Neary, D. Semantic dementia and the left and right temporal lobes. Cortex 2018, 107, 188–203. [Google Scholar] [CrossRef] [PubMed]
- Savage, S.A.; Piguet, O.; Hodges, J.R. Giving words new life: Generalization of word retraining outcomes in Semantic Dementia. J. Alzheimers Dis. 2014, 40, 309–317. [Google Scholar] [CrossRef]
- Jokel, R.; Anderson, N.D. Quest for the best: Effects of errorless and active encoding on word re-learning in semantic dementia. Neuropsychol. Rehabil. 2012, 22, 187–214. [Google Scholar] [CrossRef]
- Jokel, R.; Rochon, E.; Leonard, C. Treating anomia in semantic dementia: Improvement, maintenance, or both? Neuropsychol. Rehabil. 2006, 16, 241–256. [Google Scholar] [CrossRef]
- Savage, S.A.; Piguet, O.; Hodges, J.R. Cognitive Intervention in Semantic Dementia: Maintaining Words Over Time. Alzheimers Dis. Assoc. Disord. 2015, 29, 55–62. [Google Scholar] [CrossRef]
- Senaha, M.L.H.; Brucki, S.M.D.; Nitrini, R. Rehabilitation in semantic dementia: Study of effectiveness of lexical reacquisition in three patients. Dement. Neuropsychol. 2010, 4, 306–312. [Google Scholar] [CrossRef]
- Macoir, J.; Leroy, M.; Routhier, S.; Auclair-Ouellet, N.; Houde, M.; Laforce, R. Improving verb anomia in the semantic variant of primary progressive aphasia: The effectiveness of a semantic-phonological cueing treatment. Neurocase 2015, 21, 448–456. [Google Scholar] [CrossRef]
- Jokel, R.; Kielar, A.; Anderson, N.; Black, S.E.; Rochon, E.; Graham, S.; Freedman, M.; Tang-Wai, D.F. Behavioural and neuroimaging changes after naming therapy for semantic variant primary progressive aphasia. Neuropsychologia 2016, 89, 191–216. [Google Scholar] [CrossRef] [PubMed]
- Snowden, J.S.; Neary, D. Relearning of verbal labels in semantic dementia. Neuropsychologia 2002, 40, 1715–1728. [Google Scholar] [CrossRef]
- Bier, N.; Macoir, J.; Gagnon, L.; Van der Linden, M.; Louveaux, S.; Desrosiers, J. Known, lost, and recovered: Efficacy of formal-semantic therapy and spaced retrieval method in a case of semantic dementia. Aphasiology 2009, 23, 210–235. [Google Scholar] [CrossRef]
- Heredia, C.G.; Sage, K.; Ralph, M.A.L.; Berthier, M.L. Relearning and retention of verbal labels in a case of semantic dementia. Aphasiology 2009, 23, 192–209. [Google Scholar] [CrossRef]
- Robinson, S.; Druks, J.; Hodges, J.; Garrard, P. The treatment of object naming, definition, and object use in semantic dementia: The effectiveness of errorless learning. Aphasiology 2009, 23, 749–775. [Google Scholar] [CrossRef]
- Dressel, K.; Huber, W.; Frings, L.; Kümmerer, D.; Saur, D.; Mader, I.; Hüll, M.; Weiller, C.; Abel, S. Model-oriented naming therapy in semantic dementia: A single-case fMRI study. Aphasiology 2010, 24, 1537–1558. [Google Scholar] [CrossRef]
- Jokel, R.; Rochon, E.; Anderson, N.D. Errorless learning of computer-generated words in a patient with semantic dementia. Neuropsychol. Rehabil. 2010, 20, 16–41. [Google Scholar] [CrossRef]
- Beales, A.; Cartwright, J.; Whitworth, A.; Panegyres, P.K. Exploring generalisation processes following lexical retrieval intervention in primary progressive aphasia. Int. J. Speech Lang. Pathol. 2016, 18, 299–314. [Google Scholar] [CrossRef] [PubMed]
- Savage, S.A.; Ballard, K.J.; Piguet, O.; Hodges, J.R. Bringing words back to mind—Improving word production in semantic dementia. Cortex 2013, 49, 1823–1832. [Google Scholar] [CrossRef] [PubMed]
- Suárez-González, A.; Heredia, C.G.; Savage, S.A.; Gil-Néciga, E.; García-Casares, N.; Franco-Macías, E.; Berthier, M.L.; Caine, D. Restoration of conceptual knowledge in a case of semantic dementia. Neurocase 2014, 21, 309–321. [Google Scholar] [CrossRef]
- Krajenbrink, T.; Croot, K.; Taylor-Rubin, C.; Nickels, L. Treatment for spoken and written word retrieval in the semantic variant of primary progressive aphasia. Neuropsychol. Rehabil. 2020, 30, 915–947. [Google Scholar] [CrossRef] [PubMed]
- Graham, K.S.; Patterson, K.; Pratt, K.H.; Hodges, J.R. Can repeated exposure to ‘forgotten’ vocabulary help alleviate word-finding difficulties in semantic dementia? An illustrative case study. Neuropsychol. Rehabil. 2001, 11, 429–454. [Google Scholar] [CrossRef]
- Hoffman, P.; Clarke, N.; Jones, R.W.; Noonan, K.A. Vocabulary relearning in semantic dementia: Positive and negative consequences of increasing variability in the learning experience. Neuropsychologia 2015, 76, 240–253. [Google Scholar] [CrossRef] [PubMed]
- Suárez-González, A.; Savage, S.A.; Caine, D. Successful short-term re-learning and generalisation of concepts in semantic dementia. Neuropsychol. Rehabil. 2018, 28, 1095–1109. [Google Scholar] [CrossRef] [Green Version]
- Montagut, N.; Borrego-Écija, S.; Castellví, M.; Rico, I.; Reñé, R.; Balasa, M.; Lladó, A.; Sánchez-Valle, R. Errorless Learning Therapy in Semantic Variant of Primary Progressive Aphasia. J. Alzheimers Dis. 2021, 79, 415–422. [Google Scholar] [CrossRef]
- Croot, K.; Raiser, T.; Taylor-Rubin, C.; Ruggero, L.; Ackl, N.; Wlasich, E.; Danek, A.; Scharfenberg, A.; Foxe, D.; Hodges, J.R.; et al. Lexical retrieval treatment in primary progressive aphasia: An investigation of treatment duration in a heterogeneous case series. Cortex 2019, 115, 133–158. [Google Scholar] [CrossRef]
- Flurie, M.; Ungrady, M.; Reilly, J. Evaluating a Maintenance-Based Treatment Approach to Preventing Lexical Dropout in Progressive Anomia. J. Speech Lang. Hear Res. 2020, 63, 4082–4095. [Google Scholar] [CrossRef]
- Lavoie, M.; Bier, N.; Laforce, R.; Macoir, J. Improvement in functional vocabulary and generalization to conversation following a self-administered treatment using a smart tablet in primary progressive aphasia. Neuropsychol. Rehabil. 2020, 30, 1224–1254. [Google Scholar] [CrossRef] [PubMed]
- Evans, W.S.; Quimby, M.; Dickey, M.W.; Dickerson, B.C. Relearning and Retaining Personally-Relevant Words using Computer-Based Flashcard Software in Primary Progressive Aphasia. Front. Hum. Neurosci. 2016, 10, 561. [Google Scholar] [CrossRef] [PubMed]
- Henry, M.; Beeson, P.; Rapcsak, S. Treatment for Anomia in Semantic Dementia. Semin Speech Lang. 2008, 29, 060–070. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Meyer, A.M.; Tippett, D.C.; Friedman, R.B. Prophylaxis and remediation of anomia in the semantic and logopenic variants of primary progressive aphasia. Neuropsychol. Rehabil. 2018, 28, 352–368. [Google Scholar] [CrossRef]
- Meyer, A.M.; Getz, H.R.; Brennan, D.M.; Hu, T.M.; Friedman, R.B. Telerehabilitation of anomia in primary progressive aphasia. Aphasiology 2016, 30, 483–507. [Google Scholar] [CrossRef] [Green Version]
- Meyer, A.M.; Tippett, D.C.; Turner, R.S.; Friedman, R.B. Long-Term maintenance of anomia treatment effects in primary progressive aphasia. Neuropsychol. Rehabil. 2019, 29, 1439–1463. [Google Scholar] [CrossRef]
- Newhart, M.; Davis, C.; Kannan, V.; Heidler-Gary, J.; Cloutman, L.; Hillis, A.E. Therapy for naming deficits in two variants of primary progressive aphasia. Aphasiology 2009, 23, 823–834. [Google Scholar] [CrossRef]
- Henry, M.L.; Rising, K.; DeMarco, A.T.; Miller, B.L.; Gorno-Tempini, M.L.; Beeson, P.M. Examining the value of lexical retrieval treatment in primary progressive aphasia: Two positive cases. Brain Lang. 2013, 127, 145–156. [Google Scholar] [CrossRef] [Green Version]
- Henry, M.L.; Hubbard, H.I.; Grasso, S.M.; Dial, H.R.; Beeson, P.M.; Miller, B.L.; Gorno-Tempini, M.L. Treatment for Word Retrieval in Semantic and Logopenic Variants of Primary Progressive Aphasia: Immediate and Long-Term Outcomes. J. Speech Lang. Hear Res. 2019, 62, 2723–2749. [Google Scholar] [CrossRef]
- Dial, H.R.; Hinshelwood, H.A.; Grasso, S.M.; Hubbard, H.I.; Gorno-Tempini, M.-L.; Henry, M.L. Investigating the utility of teletherapy in individuals with primary progressive aphasia. Clin. Interv. Aging 2019, 14, 453–471. [Google Scholar] [CrossRef] [Green Version]
- Snowden, J.S.; Griffiths, H.; Neary, D. Semantic dementia: Autobiographical contribution to preservation of meaning. Cogn. Neuropsychol. 1994, 11, 265–288. [Google Scholar] [CrossRef]
- Taylor-Rubin, C.; Croot, K.; Nickels, L. Adherence to lexical retrieval treatment in Primary Progressive Aphasia and implications for candidacy. Aphasiology 2019, 33, 1182–1201. [Google Scholar] [CrossRef]
- Savage, S.A.; Piguet, O.; Hodges, J.R. ‘Knowing What You Don’t Know’: Language Insight in Semantic Dementia. J. Alzheimers Dis. 2015, 46, 187–198. [Google Scholar] [CrossRef]
- Cadório, I.; Lousada, M.; Martins, P.; Figueiredo, D. Generalization and maintenance of treatment gains in primary progressive aphasia (PPA): A systematic review. Int. J. Lang. Commun. Disord. 2017, 52, 543–560. [Google Scholar] [CrossRef] [PubMed]
- Reilly, J. How to constrain and maintain a lexicon for the treatment of progressive semantic naming deficits: Principles of item selection for formal semantic therapy. Neuropsychol. Rehabil. 2016, 26, 126–156. [Google Scholar] [CrossRef] [Green Version]
- Best, W.; Greenwood, A.; Grassly, J.; Herbert, R.; Hickin, J.; Howard, D. Aphasia rehabilitation: Does generalisation from anomia therapy occur and is it predictable? A case series study. Cortex 2013, 49, 2345–2357. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Subedi, B.S. Emerging trends of research on transfer of learning. Int. Educ. J. 2004, 5, 591–599. [Google Scholar]
- Taylor-Rubin, C.; Nickels, L.; Croot, K. Exploring the effects of verb and noun treatment on verb phrase production in primary progressive aphasia: A series of single case experimental design studies. Neuropsychol. Rehabil. 2021, 1–43. [Google Scholar] [CrossRef]
- Bozeat, S.; Ralph, M.A.L.; Patterson, K.; Hodges, J.R. The Influence of Personal Familiarity and Context on Object Use in Semantic Dementia. Neurocase 2002, 8, 127–134. [Google Scholar] [CrossRef]
- Rutherford, S. Our journey with primary progressive aphasia. Aphasiology 2014, 28, 900–908. [Google Scholar] [CrossRef]
- Taylor, C.; Kingma, R.M.; Croot, K.; Nickels, L. Speech pathology services for primary progressive aphasia: Exploring an emerging area of practice. Aphasiology 2009, 23, 161–174. [Google Scholar] [CrossRef]
- Jokel, R.; Rochon, E.; Leonard, C. Therapy for anomia in semantic dementia. Brain Cogn. 2002, 49, 241–244. [Google Scholar] [PubMed]
- Rogalski, E.J.; Saxon, M.; McKenna, H.; Wieneke, C.; Rademaker, A.; Corden, M.E.; Borio, K.; Mesulam, M.-M.; Khayum, B. Communication Bridge: A pilot feasibility study of Internet-based speech-language therapy for individuals with progressive aphasia. Alzheimers Dement. Transl. Res. Clin. Interv. 2016, 2, 213–221. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bier, N.; Paquette, G.; Macoir, J. Smartphone for smart living: Using new technologies to cope with everyday limitations in semantic dementia. Neuropsychol. Rehabil. 2018, 28, 734–754. [Google Scholar] [CrossRef] [PubMed]
- Mooney, A.; Bedrick, S.; Noethe, G.; Spaulding, S.; Fried-Oken, M. Mobile technology to support lexical retrieval during activity retell in primary progressive aphasia. Aphasiology 2018, 32, 666–692. [Google Scholar] [CrossRef]
- Routhier, S.; Macoir, J.; Imbeault, H.; Jacques, S.; Pigot, H.; Giroux, S.; Cau, A.; Bier, N. From smartphone to external semantic memory device: The use of new technologies to compensate for semantic deficits. Non-Pharmacol. Ther. Dement. 2011, 2, 81. [Google Scholar]
- Fried-Oken, M.; Beukelman, D.R.; Hux, K. Current and future AAC research considerations for adults with acquired cognitive and communication impairments. Assist. Technol. 2011, 24, 56–66. [Google Scholar] [CrossRef] [Green Version]
- O’Connor, C.M.; Clemson, L.; Brodaty, H.; Gitlin, L.N.; Piguet, O.; Mioshi, E. Enhancing caregivers’ understanding of dementia and tailoring activities in frontotemporal dementia: Two case studies. Disabil. Rehabil. 2016, 38, 704–714. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lanyon, L.E.; Rose, M.L.; Worrall, L. The efficacy of outpatient and community-based aphasia group interventions: A systematic review. Int. J. Speech Lang. Pathol. 2013, 15, 359–374. [Google Scholar] [CrossRef]
- Davies, K.; Howe, T. Experiences of Living with Primary Progressive Aphasia: A Scoping Review of Qualitative Studies. Am. J. Alzheimers Dis. Dement. 2020, 35, 1533317519886218. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Armstrong, M.J.; Alliance, S. Virtual Support Groups for Informal Caregivers of Individuals with Dementia: A Scoping Review. Alzheimers Dis. Assoc. Disord. 2019, 33, 362–369. [Google Scholar] [CrossRef] [PubMed]
- Jokel, R. Planning for patient deterioration. ASHA Lead. 2021, 26, 32–41. [Google Scholar]
| Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).