Discussing Personalized Prognosis Empowers Patients with Amyotrophic Lateral Sclerosis to Regain Control over Their Future: A Qualitative Study
Abstract
:1. Introduction
2. Methods
2.1. Design
2.2. Setting
2.3. Participants
2.3.1. Patients with ALS and Their Caregivers
2.3.2. Physicians
2.4. Data Collection
2.4.1. Patients and Caregivers
2.4.2. Physicians
2.5. Data Analysis
2.5.1. Patients and Caregivers
2.5.2. Physicians
3. Results
3.1. Participants
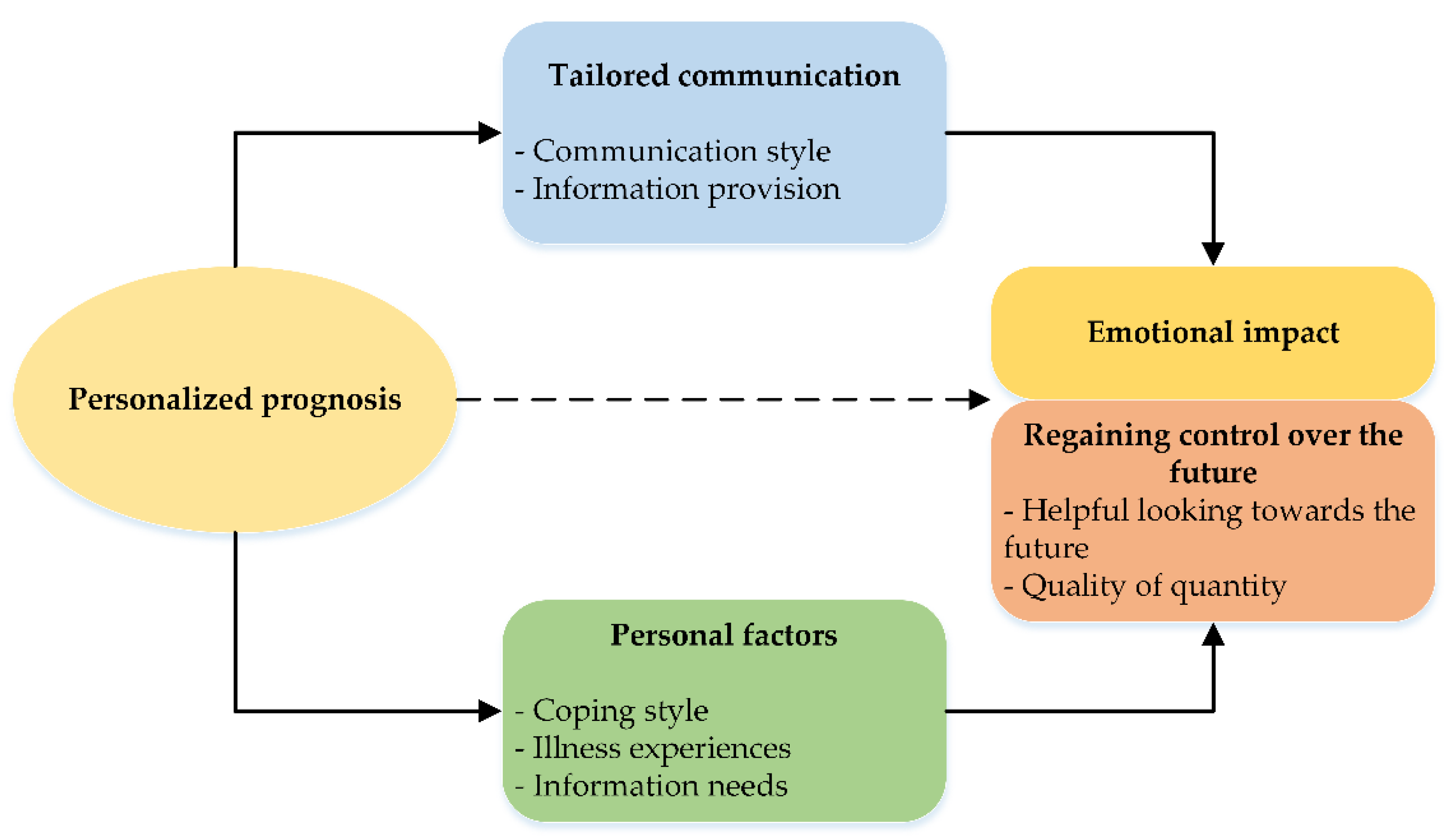
3.2. Patient and Caregiver Themes
3.2.1. Tailored Communication
3.2.2. Personal Factors
3.2.3. Emotional Impact
3.2.4. Regaining Control over the Future
3.3. Physician Focus Group
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Van Es, M.A.; Hardiman, O.; Chio, A.; Al-Chalabi, A.; Pasterkamp, R.J.; Veldink, J.H.; van den Berg, L.H. Amyotrophic Lateral Sclerosis. Lancet 2017, 390, 2084–2098. [Google Scholar] [CrossRef]
- Seeber, A.A.; Pols, A.J.; Hijdra, A.; Grupstra, H.F.; Willems, D.L.; de Visser, M. Experiences and Reflections of Patients with Motor Neuron Disease on Breaking the News in a Two-Tiered Appointment: A Qualitative Study. BMJ Support. Palliat. Care 2019, 9, e8. [Google Scholar] [CrossRef] [PubMed]
- Westeneng, H.-J.; Debray, T.P.A.; Visser, A.E.; van Eijk, R.P.A.; Rooney, J.P.K.; Calvo, A.; Martin, S.; McDermott, C.J.; Thompson, A.G.; Pinto, S.; et al. Prognosis for Patients with Amyotrophic Lateral Sclerosis: Development and Validation of a Personalised Prediction Model. Lancet Neurol. 2018, 17, 423–433. [Google Scholar] [CrossRef]
- O’Brien, M.R.; Whitehead, B.; Jack, B.A.; Mitchell, J.D. From Symptom Onset to a Diagnosis of Amyotrophic Lateral Sclerosis/Motor Neuron Disease (ALS/MND): Experiences of People with ALS/MND and Family Carers—A Qualitative Study. Amyotroph. Lateral Scler. 2011, 12, 97–104. [Google Scholar] [CrossRef]
- Sullivan, R.; Ugalde, A.; Sinclair, C.; Breen, L.J. Developing a Research Agenda for Adult Palliative Care: A Modified Delphi Study. J. Palliat. Med. 2019, 22, 480–488. [Google Scholar] [CrossRef]
- Holloway, R.G.; Gramling, R.; Kelly, A.G. Estimating and Communicating Prognosis in Advanced Neurologic Disease. Neurology 2013, 80, 764–772. [Google Scholar] [CrossRef] [Green Version]
- Gill, T.M. The Central Role of Prognosis in Clinical Decision Making. JAMA 2012, 30, 199. [Google Scholar] [CrossRef]
- Hancock, K.; Clayton, J.M.; Parker, S.M.; Der, S.W.; Butow, P.N.; Carrick, S.; Currow, D.; Ghersi, D.; Glare, P.; Hagerty, R.; et al. Truth-Telling in Discussing Prognosis in Advanced Life-Limiting Illnesses: A Systematic Review. Palliat. Med. 2007, 21, 507–517. [Google Scholar] [CrossRef]
- Mitsumoto, H. What If You Knew the Prognosis of Your Patients with ALS? Lancet Neurol. 2018, 17, 386–388. [Google Scholar] [CrossRef]
- Haaksma, M.L.; Eriksdotter, M.; Rizzuto, D.; Leoutsakos, J.M.S.; Olde Rikkert, M.G.M.; Melis, R.J.F.; Garcia-Ptacek, S. Survival Time Tool to Guide Care Planning in People with Dementia. Neurology 2020, 94, E538–E548. [Google Scholar] [CrossRef] [Green Version]
- Van Der Steen, J.T.; Albers, G.; Licht-Strunk, E.; Muller, M.T.; Ribbe, M.W. A Validated Risk Score to Estimate Mortality Risk in Patients with Dementia and Pneumonia: Barriers to Clinical Impact. Int. Psychogeriatr. 2011, 23, 31–43. [Google Scholar] [CrossRef]
- Schoenborn, N.L.; Bowman, T.L.; Cayea, D.; Pollack, C.E.; Feeser, S.; Boyd, C. Primary Care Practitioners’ Views on Incorporating Long-Term Prognosis in the Care of Older Adults. JAMA Intern. Med. 2016, 176, 671–678. [Google Scholar] [CrossRef] [PubMed]
- Van Eenennaam, R.M.; Kruithof, W.J.; van Es, M.A.; Kruitwagen-van Reenen, E.T.; Westeneng, H.J.; Visser-Meily, J.M.A.; van den Berg, L.H.; Beelen, A. Discussing Personalized Prognosis in Amyotrophic Lateral Sclerosis: Development of a Communication Guide. BMC Neurol. 2020, 20, 446. [Google Scholar] [CrossRef] [PubMed]
- Van der Velden, N.C.A.; Meijers, M.C.; Han, P.K.J.; van Laarhoven, H.W.M.; Smets, E.M.A.; Henselmans, I. The Effect of Prognostic Communication on Patient Outcomes in Palliative Cancer Care: A Systematic Review. Curr. Treat. Options Oncol. 2020, 21, 40. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Greenhalgh, T.; Annandale, E.; Ashcroft, R.; Barlow, J.; Black, N.; Bleakley, A.; Boaden, R.; Braithwaite, J.; Britten, N.; Carnevale, F.; et al. An Open Letter to The BMJ Editors on Qualitative Research. BMJ 2016, 352, i563. [Google Scholar] [CrossRef] [Green Version]
- Braun, V.; Clarke, V. Using Thematic Analysis in Psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef] [Green Version]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated Criteria for Reporting Qualitative Research (COREQ): A 32-Item Checklist for Interviews and Focus Groups. Int. J. Qual. Health Care 2007, 19, 349–357. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Butow, P.; Dowsett, S.; Hagerty, R.; Tattersall, M. Communicating Prognosis to Patients with Metastatic Disease: What Do They Really Want to Know? Support. Care Cancer 2002, 10, 161–168. [Google Scholar] [CrossRef] [PubMed]
- Clayton, J.M.; Butow, P.N.; Arnold, R.M.; Tattersall, M.H.N. Discussing Life Expectancy with Terminally Ill Cancer Patients and Their Carers: A Qualitative Study. Support. Care Cancer 2005, 13, 733–742. [Google Scholar] [CrossRef] [PubMed]
- Clayton, J.M.; Butow, P.N.; Tattersall, M.H.N. When and How to Initiate Discussion about Prognosis and End-of-Life Issues with Terminally Ill Patients. J. Pain Symptom Manag. 2005, 30, 132–144. [Google Scholar] [CrossRef] [PubMed]
- Curtis, J.R.; Engelberg, R.; Young, J.P.; Vig, L.K.; Reinke, L.F.; Wenrich, M.D.; McGrath, B.; McCown, E.; Back, A.L. An Approach to Understanding the Interaction of Hope and Desire for Explicit Prognostic Information among Individuals with Severe Chronic Obstructive Pulmonary Disease or Advanced Cancer. J. Palliat. Med. 2008, 11, 610–620. [Google Scholar] [CrossRef]
- Friedrichsen, M.; Lindholm, A.; Milberg, A. Experiences of Truth Disclosure in Terminally Ill Cancer Patients in Palliative Home Care. Palliat. Support. Care 2011, 9, 173–180. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hagerty, R.G.; Butow, P.N.; Ellis, P.M.; Lobb, E.A.; Pendlebury, S.C.; Leighl, N.; Mac Leod, C.; Tattersall, M.H.N. Communicating with Realism and Hope: Incurable Cancer Patients’ Views on the Disclosure of Prognosis. J. Clin. Oncol. 2005, 23, 1278–1288. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kirk, P.; Kirk, I.; Kristjanson, L.J. What Do Patients Receiving Palliative Care for Cancer and Their Families Want to Be Told? A Canadian and Australian Qualitative Study. BMJ 2004, 328, 1343. [Google Scholar] [CrossRef] [Green Version]
- Mitchison, D.; Butow, P.; Sze, M.; Aldridge, L.; Hui, R.; Vardy, J.; Eisenbruch, M.; Iedema, R.; Goldstein, D. Prognostic Communication Preferences of Migrant Patients and Their Relatives. Psychooncology 2012, 21, 496–504. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rohde, G.; Söderhamn, U.; Vistad, I. Reflections on Communication of Disease Prognosis and Life Expectancy by Patients with Colorectal Cancer Undergoing Palliative Care: A Qualitative Study. BMJ Open 2019, 9, e023463. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Clayton, J.M.; Butow, P.N.; Tattersall, M.H.N. The Needs of Terminally Ill Cancer Patients versus Those of Caregivers for Information Regarding Prognosis and End-of-Life Issues. Cancer 2005, 103, 1957–1964. [Google Scholar] [CrossRef]
- Clayton, J.M.; Butow, P.N.; Arnold, R.M.; Tattersall, M.H.N. Fostering Coping and Nurturing Hope When Discussing the Future with Terminally Ill Cancer Patients and Their Caregivers. Cancer 2005, 103, 1965–1975. [Google Scholar] [CrossRef]
- Coulourides Kogan, A.; Penido, M.; Enguidanos, S. Does Disclosure of Terminal Prognosis Mean Losing Hope? Insights from Exploring Patient Perspectives on Their Experience of Palliative Care Consultations. J. Palliat. Med. 2015, 18, 1019–1025. [Google Scholar] [CrossRef]
- Walczak, A.; Butow, P.N.; Davidson, P.M.; Bellemore, F.A.; Tattersall, M.H.N.; Clayton, J.M.; Young, J.; Mazer, B.; Ladwig, S.; Epstein, R.M. Patient Perspectives Regarding Communication about Prognosis and End-of-Life Issues: How Can It Be Optimised? Patient Educ. Couns. 2013, 90, 307–314. [Google Scholar] [CrossRef] [Green Version]
- Moser, A.; Korstjens, I. Series: Practical Guidance to Qualitative Research. Part 3: Sampling, Data Collection and Analysis. Eur. J. Gen. Pract. 2018, 24, 9–18. [Google Scholar] [CrossRef] [Green Version]
- Saldaña, J. The Coding Manual for Qualitative Researchers, 2nd ed.; SAGE Publications: Thousand Oaks, CA, USA, 2013. [Google Scholar]
- Hogden, A.V.; Greenfield, D.; Nugus, P.; Kiernan, M.C. What Influences Patient Decision-Making in Amyotrophic Lateral Sclerosis Multidisciplinary Care? A Study of Patient Perspectives. Patient Prefer. Adherence 2012, 6, 829–838. [Google Scholar] [CrossRef] [Green Version]
- Etkind, S.N.; Koffman, J. Approaches to Managing Uncertainty in People with Life-Limiting Conditions: Role of Communication and Palliative Care. Postgrad. Med. J. 2016, 92, 412–417. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Clayton, J.M.; Hancock, K.; Parker, S.; Butow, P.N.; Walder, S.; Carrick, S.; Currow, D.; Ghersi, D.; Glare, P.; Hagerty, R.; et al. Sustaining Hope When Communicating with Terminally Ill Patients and Their Families: A Systematic Review. Psychooncology 2008, 17, 641–659. [Google Scholar] [CrossRef] [PubMed]
- Wright, A.A.; Zhang, B.; Ray, A.; Mack, J.W.; Trice, E.; Balboni, T.; Mitchell, S.L.; Jackson, V.A.; Block, S.D.; Maciejewski, P.K.; et al. Associations between End-of-Life Discussions, Patient Mental Health, Medical Care near Death, and Caregiver Bereavement Adjustment. JAMA 2008, 300, 1665–1673. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mack, J.W.; Weeks, J.C.; Wright, A.A.; Block, S.D.; Prigerson, H.G. End-of-Life Discussions, Goal Attainment, and Distress at the End of Life: Predictors and Outcomes of Receipt of Care Consistent with Preferences. J. Clin. Oncol. 2010, 28, 1203–1208. [Google Scholar] [CrossRef] [Green Version]
- McConigley, R.; Kristjanson, L.J.; Aoun, S.M.; Oldham, L.; Currow, D.; O’Connor, M.; Holloway, K. Staying Just One Step Ahead: Providing Care for Patients with Motor Neurone Disease: Table 1. BMJ Support. Palliat. Care 2014, 4, 38–42. [Google Scholar] [CrossRef] [PubMed]
- Hobson, E.V.; McDermott, C.J. Supportive and Symptomatic Management of Amyotrophic Lateral Sclerosis. Nat. Rev. Neurol. 2016, 12, 526–538. [Google Scholar] [CrossRef] [PubMed]
- Foley, G.; Timonen, V.; Hardiman, O. Exerting Control and Adapting to Loss in Amyotrophic Lateral Sclerosis. Soc. Sci. Med. 2014, 101, 113–119. [Google Scholar] [CrossRef]
- Soundy, A.; Condon, N. Patients Experiences of Maintaining Mental Well-Being and Hope within Motor Neuron Disease: A Thematic Synthesis. Front. Psychol. 2015, 6, 606. [Google Scholar] [CrossRef] [Green Version]
- Chiò, A.; Montuschi, A.; Cammarosano, S.; De Mercanti, S.; Cavallo, E.; Ilardi, A.; Ghiglione, P.; Mutani, R.; Calvo, A. ALS Patients and Caregivers Communication Preferences and Information Seeking Behaviour. Eur. J. Neurol. 2008, 15, 55–60. [Google Scholar] [CrossRef]
- Ozanne, A.; Graneheim, U.H. Understanding the Incomprehensible—Patients’ and Spouses’ Experiences of Comprehensibility before, at and after Diagnosis of Amyotrophic Lateral Sclerosis. Scand. J. Caring Sci. 2018, 32, 663–671. [Google Scholar] [CrossRef]
- Clayton, J.M.; Hancock, K.M.; Butow, P.N.; Tattersall, M.H.N.; Currow, D.C. Clinical Practice Guidelines for Communicating Prognosis and End-of-life Issues with Adults in the Advanced Stages of a Life-limiting Illness, and Their Caregivers. Med. J. Aust. 2007, 186, 478. [Google Scholar] [CrossRef]
- Gilligan, T.; Coyle, N.; Frankel, R.M.; Berry, D.L.; Bohlke, K.; Epstein, R.M.; Finlay, E.; Jackson, V.A.; Lathan, C.S.; Loprinzi, C.L.; et al. Patient-Clinician Communication: American Society of Clinical Oncology Consensus Guideline. J. Clin. Oncol. 2017, 35, 3618–3632. [Google Scholar] [CrossRef] [PubMed]
- Nierop-van Baalen, C.; Grypdonck, M.; van Hecke, A.; Verhaeghe, S. Hope Dies Last A Qualitative Study into the Meaning of Hope for People with Cancer in the Palliative Phase. Eur. J. Cancer Care 2016, 25, 570–579. [Google Scholar] [CrossRef]
- De Moree, S.; Smets, E.M.; Visser, L.N.; van Vliet, R.O.; Kruitwagen-van Reenen, E.T.; Grupstra, H.F.; Pieters, S.; De Visser, M.; De Haes, H.C.; Nollet, F.; et al. Silver Linings: The Experience of Hope in Dyads with Motor Neuron Disease. An Explorative Study. J. Palliat. Care Med. 2019, 9, 1–8. [Google Scholar] [CrossRef]
- Stutzki, R.; Weber, M.; Reiter-Theil, S.; Simmen, U.; Borasio, G.D.; Jox, R.J. Attitudes towards Hastened Death in ALS: A Prospective Study of Patients and Family Caregivers. Amyotroph. Lateral Scler. Front. Degener. 2014, 15, 68–76. [Google Scholar] [CrossRef] [PubMed]
- Hauswirth, A.G.; George, H.C.; Lomen-Hoerth, C. ALS Patient and Caregiver Attitudes toward Physician-Hastened Death in California. Muscle Nerve 2021, 64, 428–434. [Google Scholar] [CrossRef]
- Wang, L.H.; Elliott, M.A.; Jung Henson, L.; Gerena-Maldonado, E.; Strom, S.; Downing, S.; Vetrovs, J.; Kayihan, P.; Paul, P.; Kennedy, K.; et al. Death with Dignity in Washington Patients with Amyotrophic Lateral Sclerosis. Neurology 2016, 87, 2117–2122. [Google Scholar] [CrossRef] [Green Version]
- Maessen, M.; Veldink, J.H.; Onwuteaka-Philipsen, B.D.; de Vries, J.M.; Wokke, J.H.J.; van der Wal, G.; van den Berg, L.H. Trends and Determinants of End-of-Life Practices in ALS in the Netherlands. Neurology 2009, 73, 954–961. [Google Scholar] [CrossRef]
- Rietjens, J.A.C.; van der Maas, P.J.; Onwuteaka-Philipsen, B.D.; van Delden, J.J.M.; van der Heide, A. Two Decades of Research on Euthanasia from the Netherlands. What Have We Learnt and What Questions Remain? J. Bioethical Inq. 2009, 6, 271–283. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kappen, T.H.; van Klei, W.A.; van Wolfswinkel, L.; Kalkman, C.J.; Vergouwe, Y.; Moons, K.G.M. Evaluating the Impact of Prediction Models: Lessons Learned, Challenges, and Recommendations. Diagn. Progn. Res. 2018, 2, 11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wattanapisit, S.; Wagland, R.; Hunt, K. Prognostic Disclosure and Quality of Life in Palliative Care: A Systematic Review. BMJ Support. Palliat. Care 2021, 11, 361–370. [Google Scholar] [CrossRef]
- Obeidat, R.F.; Homish, G.G.; Lally, R.M. Shared Decision Making Among Individuals with Cancer in Non-Western Cultures: A Literature Review. Oncol. Nurs. Forum 2013, 40, 454–463. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- O’Connor, M.; Aoun, S.M.; Breen, L.J. Australian Family Carer Responses When a Loved One Receives a Diagnosis of Motor Neurone Disease Our Life Has Changed Forever. Health Soc. Care Community 2018, 26, e415–e421. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Case | Participant | Sex | Age | Education | Initiative to Discuss | Prognostic Group | Location Interview | Participation |
|---|---|---|---|---|---|---|---|---|
| C1 * | Patient 1 | Male | 64 | High | Physician | Long | No | |
| Partner 1 | Female | 50 | Intermediate | Clinic (face to face) | Yes | |||
| C2 | Patient 2 | Female | 57 | Intermediate | Physician | Very long | Home (face to face) | Yes |
| C3 | Patient 3 | Female | 69 | High | Physician | Short | Home (telephone) | Yes |
| C4 | Patient 4 | Female | 73 | High | Patient-caregiver | Long | Home (face to face) | Yes (separate) |
| Daughter 4 | Female | 49 | High | Home (telephone) | Yes (separate) | |||
| C5 | Patient 5 | Male | 71 | Intermediate | Physician | Short | Home (telephone) | Yes |
| C6 ** | Patient 6 | Male | 65 | High | Physician | Long | Home (face to face) | Yes (together) |
| Partner 6 | Female | - | High | Home (face to face) | Yes (together) | |||
| C7 | Patient 7 | Male | 59 | High | Physician | Intermediate | Clinic (face to face) | Yes |
| C8 | Patient 8 | Male | 52 | High | Patient-caregiver | Long | Home (Video) | Yes |
| C9 | Patient 9 | Male | 55 | High | Physician | Long | Home (telephone) | Yes (together) |
| Partner 9 | Female | 54 | High | Home (telephone) | Yes (together) | |||
| C10 | Patient 10 | Female | 68 | High | Physician | Very long | Home (telephone) | Yes (together) |
| Partner 10 | Male | 72 | High | Home (telephone) | Yes (together) | |||
| C11 | Patient 11 | Male | 56 | Intermediate | Physician | Short | Home (Video) | Yes (together) |
| Partner 11 | Female | 54 | Intermediate | Home (Video) | Yes (together) | |||
| Daughter 11 | Female | 24 | High | Home (Video) | Yes (separate) | |||
| C12 | Patient 12 | Male | 57 | High | Physician | Short | Home (Video) | Yes (together) |
| Partner 12 | Female | 47 | High | Home (Video) | Yes (together) | |||
| C13 | Patient 13 | Male | 79 | High | Physician | Intermediate | Home (Video and telephone) | Yes (together) |
| Partner 13 | Female | 81 | High | Home (Video and telephone) | Yes (together) | |||
| C14 | Patient 14 | Female | 77 | High | Patient-caregiver | Short | Home (Video) | Yes (together) |
| Partner 14 | Male | 81 | High | Home (Video) | Yes (together) |
| Physician | Sex | Age | Years of Experience with ALS | Number of Times Physician Has Discussed Personalized Prognosis * | Medical Discipline |
|---|---|---|---|---|---|
| Physician 1 | Female | 53 | 15 | 15 | Rehabilitation |
| Physician 2 | Female | 47 | 15 | 15 | Rehabilitation |
| Physician 3 | Female | 34 | 5 | 10–15 | Rehabilitation |
| Physician 4 | Female | 32 | 1.5 | 5 | Rehabilitation |
| Physician 5 | Male | 30 | 3 | 10–15 | Neurology |
| Themes and Subthemes | Quotes |
|---|---|
| Tailored communication | |
| Communication style | Patient 4: “It was a pleasant conversation, yes a bit cheerful though. I was fine with it and we did leave there happy… First, that the life expectancy was obviously longer than we originally thought. And also just the way the [the rehabilitation physician] handled the situation, yes with humor… I [thought] it was special how [the rehabilitation physician did her] best to assess what type of person I am and how I’m handling it all. It was apparent that that was important to her.” Quote 1. Patient 4 (73 years old); Long prognosis |
| Patient 8: “I think that is very important in a conversation like that that you are unburdened in the sense of … we are there to constantly assist you throughout this whole process and you are not alone… That combination of life expectancy combined with the fact that you are not facing it alone, I do find that essential. That combination, that gave me a sense of calm.” Quote 2. Patient 8 (52 years old); Long prognosis | |
| Patient 12: “It really just comes down to the person giving you the news… That might also be because this doctor is less empathetic than another doctor… I had the impression that she found it harder to tell me than I found dealing with it…” Partner 12: “We have no idea what’s on the computer because she’s looking at her computer screen and we’re sitting there… Either let us see what’s on your computer screen or turn off your screen and write it on a piece of paper.” Quote 3. Patient 12 (57 years old) and Partner 12 (47 years old); Short prognosis | |
| Information provision | Patient 8: “We had a quick look at the screen together and I was able to get a look at the parameters… So that immediately gave me a sense of how that information is structured and what are, say, the key features… With that, to my mind, the matter was over and done with [laughs]… I think she [rehabilitation doctor] understood very well that I was interested, including in the scientific background of that life expectancy curve.” Quote 4. Patient 8 (52 years old); Long prognosis |
| Partner 11: “Actually, the model is not clear to us… Yeah, and then when it’s said from 18 to 30 months that’s also, yeah, I think it’s almost like trying to read tea leaves. Patient 11: “I mean look, I’m pretty happy about it [consultation], but my wife and my daughter not so much [laughs].” Partner 11: “If she [the rehabilitation physician] herself already indicates that you have to look at that broadly then I think, so, is this false hope? False information? … I’m like yeah, but what are we taking with a grain of salt here? The 18 months or the 30 months, or the whole story?” Quote 5. Patient 11 (56 years old) and Partner 11 (54 years old); Short prognosis | |
| Daughter 11: “She said she was going to discuss it and then the computer didn’t work and then she had logged in somewhere else. And I think it’s pretty tough when you start giving information like that to someone, with a model like that and then that it’s not ready and then you’re waiting for it to be ready.” Quote 6. Daughter 11 (24 years old); Short prognosis | |
| Patient 7: “I went to [local hospital] first. That’s where I got the diagnosis: ALS. And, uh, yeah they were already talking about, well, several years… So then I was referred here [ALS Centre diagnosis day]. And then I was told 3 to 5 years. And yesterday [at the rehabilitation physician] … then it was 3 years. So, uh, that really has an impact… It’s gotten worse three times.” Quote 7. Patient 7 (59 years old); Intermediate prognosis | |
| Patient 8: “Here I was actually told three to five years, which already sounds a little better. And um, actually you don’t know anything then, because of course it’s a statistic, and then of course you have a spread and who knows, maybe I’m in the 96th percentile. And then I might end up with ten years. You never know.” Quote 8. Patient 8 (52 years old); Long prognosis | |
| Themes and Subthemes | Quotes |
|---|---|
| Personal factors | |
| Coping style | Patient 7: “It was a bit intense at first, and also emotional. But then again, I’m so down-to-earth that yes, I resigned myself to it pretty quickly… [My wife], she’s a little more emotional than I am. She’s a little less down-to-earth… I accept that things are the way they are more easily.” Quote 9. Patient 7 (59 years old); Intermediate prognosis |
| Patient 11: “I like things to be clear… then you can take action, do things you still want or take care of things… [With such a short life expectancy] you’re going to get started with things sooner and find things out a little faster to see what needs to get done… You distract yourself a little bit that way.” Partner 11: “Yeah, I was in denial. In particular, not being ready to get this news… I’m just like, we’ll see what’s coming and then we’ll just deal with it and I don’t need to know when that will be.” Quote 10. Patient 11 (56 years old) and Partner 11 (54 years old); Short prognosis | |
| Patient 13: “I’m not afraid to die, that’s a very important principle. I don’t think it’s time to die yet, but once you get to 80, we do say ‘up to 80 is wonderful, but 80 to 100 sucks’ [laughs]. Once you reach your 80th birthday, you’re increasingly faced with deterioration… It’s not dramatic that my life is finite.” Partner 13: “It’s just the way it is and I’m not going to worry about it… I want to take care of him for as much as I can and I will do that with love… So, we’ll just live for now and enjoy life every day.” Quote 11. Patient 13 (79 years old) and Partner 13 (81 years old); Intermediate prognosis | |
| Patient 14: “Our oldest son passed away very suddenly just before he turned 20. That’s the biggest disaster that can happen to you. After that all disasters pale in comparison… I’m 77 and I’ve had a very long life. A lot of people don’t even get that old. I have wonderful memories so it’s been nice.” Quote 12. Patient 14 (77 years old); Short prognosis | |
| Partner 12: “I am an extreme control freak [laughs] both in my work and in my personal life … and I don’t function as well when I know that there are unanswered [issues].” Quote 13. Partner 12 (47 years old); Short prognosis | |
| Illness experiences | Patient 8: “I was like, ‘I’m going to make it those three years,’ because I’m actually feeling incredibly good right now. Very fit and spry. I actually have no complaints right now. So I feel like I can last a while. Well, that was kind of confirmed by this news. So in that sense, of course, that’s only positive.” Quote 14. Patient 8 (52 years old); Long prognosis |
| Patient 14: “Well, I made an estimate myself by looking at how fast things are deteriorating and since that was pretty fast, I thought, well, it’s not going to take very long then. I’m not going to make it four years, but I probably won’t make it one year either… It makes little difference to me…” Partner 14: “I have now received confirmation of what [my partner] thought. So there’s also no reason to let anything give us false hope or anything… I have to arrange all kinds of things for the future. I actually need to stay just one step ahead of her disease, which is worsening, for example with aids. That’s why I wanted to know. It makes a big difference whether you have to take care of someone who has four years left or someone who has one year left.” Quote 15. Patient 14 (77 years old) and Partner 14 (81 years old); Short prognosis | |
| Patient 11: “You’re also sick, but you don’t have the idea yet of being so bad that within a short period of time you end up in such bad shape that all the muscles stop working… It’s like it’s so far from your daily life because you’re still so healthy.” Quote 16. Patient 11 (56 years old); Short prognosis | |
| Patient 9: “I had a brother who died [of ALS] within three-and-a-half months… Fear absolutely, it’s of course burying your head in the sand.” Partner 9: “The fear that it would be four months for you too… So on the one hand you were very afraid… And when it was done, … you got a completely different result and that was a relief.” Quote 17. Patient 9 (55 years old) and Partner 9 (54 years old); Long prognosis | |
| Patient 4: “I myself also cared for my mother with dementia and for a husband with Alzheimer’s for 10 years… In the case of Alzheimer’s, you have no idea how long it will last, and to what degree, and how it will all end. This is actually a pretty well-defined situation, clear cut, I would say. At a certain point it ends. Done… It doesn’t have to take very long for me though.” Quote 18. Patient 4 (73 years old); Long prognosis | |
| Information needs | Patient 8: “So I asked that rehabilitation physician ‘let’s hear it’ [laughs]. Yeah! I was like, what do I have to lose? And that also came as a big shock to those around me, I think… I was mainly very curious about which of those five curves you can wind up in. And I was also a little curious to know why. I was raised in a very scientific way.” Quote 19. Patient 8 (52 years old); Long prognosis |
| Patient 2: “Seven years. Two more years after all… He also said that it’s a slow variant. And so, with that my questions were basically answered [laughs].” Quote 20. Patient 2 (57 years old); Very long prognosis | |
| Patient 1: “I would also like to have clarity to have a certain grasp on things. Every time I think, okay this is it, then we’re already a step further… He’s obsessive-compulsive [due to frontotemporal dementia] and I have to deal with it 24/7. So I would like clarity.” Quote 21. Partner 1 (64 years old); Long prognosis | |
| Patient 13: “I don’t really want to know how long I have left to live, but rather … how long I will be able to function as I function now… And that’s a burning question: what will my life be like in a year’s time? Statistically speaking, I’m still alive, but what will my quality of life be then?” Quote 22. Patient 13 (79 years old); Intermediate prognosis | |
| Themes and Subthemes | Quotes |
|---|---|
| Emotional impact | |
| Patient 4: “Three years seems like a very short time, but now you have a bit more space and that gives some room to breathe. It just gave us room to breathe.” Daughter 4: “It does feel like we were given some time in a way.” Quote 23. Patient 4 (73 years old) and Daughter 4 (49 years old); Long prognosis | |
| Patient 7: “If they have given me a diagnosis of 10 years, okay, that would have been nice. So this prognosis of three years, that makes it extra difficult. Definitely. Also in the whole processing of it… Yes, it’s a bit of [short pause] an emotional rollercoaster right now.” Quote 24. Patient 7 (57 years old); Intermediate prognosis | |
| Patient 5: “[I was] a bit confused. So I went back to [the diagnosis day at the ALS Centre] where they had given three to four years… How can she [rehabilitation physician] say two years? That’s a difference of almost half! … If I had known beforehand that the result would be so bad, I wouldn’t even have started. Because I would rather live with the thought of three to four years than two.” Quote 25. Patient 5 (71 years old); Short prognosis | |
| Patient 3: “Suppose I have another six months or so. Then we’ll have been so good to each other, it must hurt a lot less to say goodbye. And it’s easier for them [children], as well, not to see their mother deteriorate.” Quote 26. Patient 3 (69 years old); Short prognosis | |
| Regaining control over the future | |
| Helpful in looking towards the future | Patient 2: “It’s just nice to know that I have some more time. You know, that does take away some of the uncertainty.” Quote 27. Patient 2 (57 years old); Very long prognosis |
| Partner 12: “I find that I get a lot of peace from that, that I know … where I stand, where we stand as a family, and that we also have to make every day a celebration. Every day that [patient] is well, we have a party. Strange as it might be, we have no time left… So you just live a much more active lifestyle and you grab everything you can get your hands on … ” Patient 12: “Of course it [life expectancy] is a disappointment, but on the other hand it offers clarity. So you’re going to have to get up more focused every day with that knowledge.” Quote 28. Patient 12 (57 years old) and partner 12 (47 years old); Short prognosis | |
| Patient 7: “I have an appointment with the company doctor on Monday and I think I’m just going to say, ‘y’know, with this life expectancy, I just want to stop working’. I just want to spend time regularly with the grandchildren and with my wife…If you know this [life expectancy], then of course you aren’t completely in control, but you can start planning something. What I actually couldn’t do before, when I had just been diagnosed.” Quote 29. Patient 7 (59 years old); Intermediate prognosis | |
| Partner 12: “Both of us talk with social services in which [patient] talks up until death and I talk after the death … that I shouldn’t really be looking about afterwards, but rather that I should live more NOW, do things with [patient] now. And [patient] also gets advice to look further ahead, because that’s where [the question] arises for me, because how am I going to support my children or our children when he’s gone?” Quote 30. Partner 12 (47 years old); Short prognosis | |
| Quality over quantity | Patient 8: “I especially hope that I will remain ambulant, that I can keep walking for example. And minimally to be able to use my hands even if they become weaker… That means that I can mail, so I can communicate, voice my own wishes. For me that is fundamental to quality of life, that you are able to communicate your own wishes… If that is not possible anymore, I think, life will end for me.” Quote 31. Patient 8 (52 years old); Long prognosis |
| Patient 3: “Suppose it were a year and a half. Then I think I would divide it into a year and six months and I think that the last six months is no longer acceptable to me… So my life expectancy is then one and a half years minus half a year, let’s say. I’m just going to take charge of that myself… That does give me peace of mind.” Quote 32. Patient 3 (69 years old); Short prognosis | |
| Patient 7: “It’s not just life expectancy, it’s also when you look at ALS: how it progresses. Then the quality of life, that deteriorates rapidly… And I’m really going to look into euthanasia. Because I really don’t want to keep going until the very last moment… Look. I’ve resigned myself to the fact that it may be 3 years. Yeah, you hope that the quality of life will be good for a little while longer, or that it will be good for at least three years.” Quote 33. Patient 7 (57 years old); Intermediate prognosis | |
| Partner 11: “The result is still between 18 to 30 months, then you hope for 30, that’s the hope, yeah.”Patient 11: “Yeah, you just hope that you can stay mobile and do things normally for as long as possible.” Quote 34. Patient 11 (56 years old) and Partner 11 (54 years old); Short prognosis) | |
| Themes and Subthemes | Quotes |
|---|---|
| Tailored communication | |
| Communication style | “And I think it’s very important HOW you discuss it with the patient, and that you feel how someone is receiving that message. Can someone accept that message, or are you just stirring up a lot of resistance? And if that’s the case, how can you change your tone of voice or the way you present something so that it is well understood; so that the patient and the partner or close relative who is there can go along with it?” Quote p1. Physician 2 |
| Information provision | “Of course, you always try in a conversation to get a clear idea in advance of the degree to which both parties wish to have the conversation. And what their expectations are and what thoughts they have about it. Yes and you know, you do try to reflect back those emotions that you notice or feel or see.” Quote p2. Physician 3 |
| “But I also think it depends very much on how you tell people. If you just present that statistic not as fact and reality and truth, but just as very much the relativity of the statistic and that it does not come down to the month or the day.” Quote p3. Physician 1 | |
| Coping style | “Yes, my patients were also fairly accepting of the news… But it is also perhaps a selection of the population that wants to know, let’s say, because they already want to know. They’re curious and they may already have an expectation of where they fall under.” Quote p4. Physician 5 |
| Personal factors | |
| Illness experiences | “So I’ve only discussed it twice and with both of them their reaction was actually ‘well, that’s the prognosis we were expecting’. So both of them weren’t that shocked by the news.” Quote p5. Physician 4 |
| Information needs | “I also had a patient once who couldn’t live with the fact that he didn’t know [the personalized prognosis] … The fact that he knew the model was there, for him, made him really want to know as well.” Quote p6. Physician 5 |
| Emotional impact | |
| “With others, you notice a very emotional reaction they are really shocked by what the results of the prediction model are, and then there it is in writing in black and white or visible on the computer. And the picture you share with them then is often different from what they heard at [the diagnosis].” Quote p7. Physician 2 | |
| Regaining control over the future | |
| Helpful in looking towards the future | “And some patients say that they like to know where they stand so they can make a plan and think, I have more time or less time to plan my life further, and giving them something to hold on to.” Quote p8. Physician 2 |
| Quality over quantity | “I’ve also had people who actually found it very interesting, but then turned around and said ‘but you still can’t tell me how it’s going to go’. So they actually found that much more interesting… Yes, that is much more relevant of course, so they already put the outcome and the conversation into perspective themselves.” Quote p9. Physician 1 |
| Potential benefits and barriers | |
| Benefits | “I think that also the way you present it and also if you include the patient in it, then it doesn’t have to be more difficult than any other important subject, for example, discussing the limits of treatment… It’s mainly about being able to talk to people about what their future looks like, even if it’s shortened, and what they find important in the short time they have left. Quote p10. Physician 2 |
| “There have also been a few times when I thought, ‘oh, this is worse than I thought’, based on my clinical view.” Quote p11. Physician 2 | |
| “If you take the time, you are talking about things that actually affect the patient deeply… And, that, I think is a very nice step towards very personal guidance… It can deepen your contact nicely, which is a nice basis for further conversations.” Quote p12. Physician 1 | |
| Barriers | “The preparation takes more time … [and] getting the concept right and explaining it well takes more time than getting the message across. And then it takes a lot of time to absorb the patient’s reaction and interpret it correctly.” Quote p13. Physician 2 |
| “Sometimes you really have doubts. I find, for example, in some patients, someone who has had cramps for five years or has had cramps all his life, has had cramps for four years and has had functional loss since December, explain to me when the symptoms started.” Quote p14. Physician 1 | |
| “ALS patients … who either did not speak Dutch at all or where both patient and family only spoke English, I notice that I find this a complicated subject… That takes a lot of time … I don’t get started with that…. How I should and can discuss this clearly with non-native speakers, which also often involves a whole cultural problem.” Quote p15. Physician 2 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
van Eenennaam, R.M.; Koppenol, L.S.; Kruithof, W.J.; Kruitwagen-van Reenen, E.T.; Pieters, S.; van Es, M.A.; van den Berg, L.H.; Visser-Meily, J.M.A.; Beelen, A. Discussing Personalized Prognosis Empowers Patients with Amyotrophic Lateral Sclerosis to Regain Control over Their Future: A Qualitative Study. Brain Sci. 2021, 11, 1597. https://doi.org/10.3390/brainsci11121597
van Eenennaam RM, Koppenol LS, Kruithof WJ, Kruitwagen-van Reenen ET, Pieters S, van Es MA, van den Berg LH, Visser-Meily JMA, Beelen A. Discussing Personalized Prognosis Empowers Patients with Amyotrophic Lateral Sclerosis to Regain Control over Their Future: A Qualitative Study. Brain Sciences. 2021; 11(12):1597. https://doi.org/10.3390/brainsci11121597
Chicago/Turabian Stylevan Eenennaam, Remko M., Loulou S. Koppenol, Willeke J. Kruithof, Esther T. Kruitwagen-van Reenen, Sotice Pieters, Michael A. van Es, Leonard H. van den Berg, Johanna M. A. Visser-Meily, and Anita Beelen. 2021. "Discussing Personalized Prognosis Empowers Patients with Amyotrophic Lateral Sclerosis to Regain Control over Their Future: A Qualitative Study" Brain Sciences 11, no. 12: 1597. https://doi.org/10.3390/brainsci11121597






