Complexity Analysis of the Default Mode Network Using Resting-State fMRI in Down Syndrome: Relationships Highlighted by a Neuropsychological Assessment
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Instruments
- (1)
- Ad hoc questionnaires were used to assess the clinical and educational history, and the following variables were collected: age, sex, place of residence and degree of intellectual disability.
- (2)
- Dementia Screening Questionnaire for Individuals with Intellectual Disabilities (DSQIID): with an internal consistency estimated with Cronbach’s α of 0.91 [39]. This questionnaire was useful for ruling out signs of dementia. As it only affected the application of the exclusion criteria, a version adapted to Spanish was used without a study of its psychometric properties.
- Frontal Assessment Battery (FAB): This consisted of tasks exploring the functions of the frontal lobes through six subtests: similarities (concept formation), verbal fluidity (mental flexibility), motor series (programming), interference (carrying out conflicting instructions), control (inhibition of responses) and autonomy (independence from the external environment). The cutoff point for frontal-subcortical deficits was 16–15, and the cutoff point for frontal-subcortical dementia was 13–12. The Frontal Assessment Battery scores showed a correlation with the Mattis Dementia Rating Scale scores (rho = 0.82, p < 0.01) [40].
- Intelligence Quotient (IQ) was assessed using the Kaufman Brief Test of Intelligence (KBIT), a screening test that evaluates crystallized intelligence (learning and problem solving) based on formal schooling and cultural experience, from two levels of conceptualization: verbal intelligence with an expressive vocabulary and definitions subtest and nonverbal intelligence with a master’s subtest. This test is valid for use by people from 4 to 90 years of age and generates standard scores (verbal, nonverbal and IQ composite) [41].
2.3. Procedure
2.4. MRI Acquisition and Preprocessing
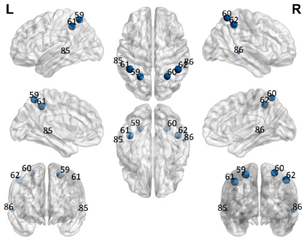
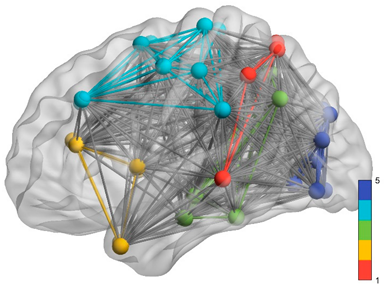
2.5. Regions of Interest
2.6. Estimation of Mental Age in the DS Group
2.7. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Pennington, B.F.; Moon, J.; Edgin, J.; Stedron, J.; Nadel, L. The neuropsychology of Down syndrome: Evidence for hippocampal dysfunction. Child. Dev. 2003, 74, 75–93. [Google Scholar] [CrossRef]
- Næss, K.A.B.; Lyster, S.A.H.; Hulme, C.; Melby-Lervåg, M. Language and Verbal Short-Term Memory Skills in children with Down syndrome: A metanalytic review. Res. Dev. Disabil. 2011, 32, 2225–2234. [Google Scholar] [CrossRef]
- Vicario, S. Motor development and neuropsychological patterns in persons with Down syndrome. Behav. Genet. 2006, 36, 355–364. [Google Scholar] [CrossRef] [PubMed]
- Gandy, K.C.; Castillo, H.A.; Ouellette, L.; Castillo, J.; Lupo, P.J.; Jacola, L.M.; Gramatges, M.M. The relationship between chronic health conditions and cognitive deficits in children, adolescents, and young adults with down syndrome: A systematic review. PLoS ONE 2020, 15, e0239040. [Google Scholar] [CrossRef] [PubMed]
- Wilcock, D.M.; Griffin, W.S.T. Down’s syndrome, neuroinflammation, and Alzheimer neuropathogenesis. J. Neuroinflamm. 2013, 10, 864. [Google Scholar] [CrossRef] [Green Version]
- Hartley, D.; Blumenthal, T.; Carrillo, M.; DiPaolo, G.; Esralew, L.; Gardiner, K.; Lott, I. Down syndrome and Alzheimer’s disease: Common pathways, common goals. Alzheimers Dement. 2015, 11, 700–709. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lott, I.T.; Head, E. Dementia in Down syndrome: Unique insights for Alzheimer disease research. Nat. Rev. Neurol. 2019, 15, 135–147. [Google Scholar] [CrossRef]
- Head, E.; Lott, I.T.; Patterson, D.; Doran, E.; Haier, R.J. Possible compensatory events in adult Down syndrome brain prior to the development of Alzheimer disease neuropathology: Targets for nonpharmacological intervention. J. Alzheimers Dis. 2007, 11, 61–76. [Google Scholar] [CrossRef] [Green Version]
- Oliver, C.; Crayton, L.; Holland, A.; Hall, S.; Bradbury, J. A four year prospective study of age-related cognitive change in adults with Down’s syndrome. Psychol. Med. 1998, 28, 1365–1377. [Google Scholar] [CrossRef] [Green Version]
- De Sola, S.; de la Torre, R.; Sánchez-Benavides, G.; Benejam, B.; Cuenca-Royo, A.; Del Hoyo, L.; Hernandez, G. A new cognitive evaluation battery for Down syndrome and its relevance for clinical trials. Front. Psychol. 2015, 6, 708. [Google Scholar] [CrossRef] [Green Version]
- Edgin, J.O.; Mason, G.M.; Allman, M.J.; Capone, G.T.; DeLeon, I.; Maslen, C.; Nadel, L. Development and validation of the Arizona Cognitive Test Battery for Down syndrome. J. Neurodev. Disord. 2010, 2, 149–164. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Edgin, J.O.; Anand, P.; Rosser, T.; Pierpont, E.I.; Figueroa, C.; Hamilton, D.; Nguyen-Driver, M. The Arizona Cognitive Test Battery for Down syndrome: Test-retest reliability and practice effects. Am. J. Intellect. Dev. Disabil. 2017, 122, 215–234. [Google Scholar] [CrossRef]
- Powell, D.; Caban-Holt, A.; Jicha, G.; Robertson, W.; Davis, R.; Gold, B.T.; Head, E. Frontal white matter integrity in adults with Down syndrome with and without dementia. Neurobiol. Aging 2014, 35, 1562–1569. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lao, P.J.; Gutierrez, J.; Keator, D.; Rizvi, B.; Banerjee, A.; Igwe, K.C.; Krinsky-McHale, S. Alzheimer-Related Cerebrovascular Disease in Down Syndrome. Ann. Neurol. 2020, 88, 1165–1177. [Google Scholar] [CrossRef] [PubMed]
- Carbó-Carreté, M.; Cañete-Massé, C.; Peró-Cebollero, M.; Guàrdia-Olmos, J. Using FMRI to Assess Brain Activity in People with Down Syndrome: A systematic Review. Front. Hum. Neurosci. 2020, 14, 147. [Google Scholar] [CrossRef] [PubMed]
- Strogatz, S.H. Exploring Complex Networks. Nature 2001, 410, 268–276. [Google Scholar] [CrossRef] [Green Version]
- Newman, M.E. The Structure and Function of Complex Networks. SIAM Rev. 2003, 45, 167–256. [Google Scholar] [CrossRef] [Green Version]
- Boccaletti, S.; Latora, V.; Moreno, Y.; Chavez, M.; Hwang, D.U. Complex Networks: Structure and Dynamics. Phys. Rep. 2006, 424, 175–308. [Google Scholar] [CrossRef]
- Bullmore, E.; Sporns, O. Complex brain networks: Graph theoretical analysis of structural and functional systems. Nat. Rev. Neurosci. 2009, 10, 186–198. [Google Scholar] [CrossRef]
- Farahani, F.V.; Karwowski, W.; Lighthall, N.R. Application of Graph Theory for Identifying Connectivity Patterns in Human Brain Networks: A Systematic Review. Front. Neurosci. 2019, 13, 585. [Google Scholar] [CrossRef] [PubMed]
- Rubinov, M.; Sporns, O. Complex network measures of brain connectivity: Uses and interpretations. Neuroimage 2010, 52, 1059–1069. [Google Scholar] [CrossRef]
- Sporns, O. The human connectome: Origins and challenges. Neuroimage 2013, 80, 53–61. [Google Scholar] [CrossRef]
- Wang, Y.; Zuo, C.; Xu, Q.; Liao, S.; Kanji, M.; Wang, D. Altered resting functional network topology assessed using graph theory in youth with attention-deficit/hyperactivity disorder. Prog. Neuropsychopharmacol. Biol. Psychiatry 2020, 98, 109796. [Google Scholar] [CrossRef] [PubMed]
- Khazaee, A.; Ebrahimzadeh, A.; Babajani-Feremi, A. Identifying patients with Alzheimer’s disease using resting-state fMRI and graph theory. Clin. Neurophysiol. 2015, 126, 2132–2141. [Google Scholar] [CrossRef]
- Alaerts, K.; Geerlings, F.; Herremans, L.; Swinnen, S.P.; Verhoeven, J.; Sunaert, S.; Wenderoth, N. Functional organization of the action observation network in autism: A graph theory approach. PLoS ONE 2015, 10, e0137020. [Google Scholar] [CrossRef]
- Buckner, R.L.; Andrews-Hanna, J.R.; Schacter, D.L. The brain’s default network-anatomy, function, and relevance to disease. Ann. N. Y. Acad. Sci. 2008, 1124, 1–38. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gusnard, D.A.; Raichle, M.E. Searching for a baseline: Functional imaging and the resting human brain. Nat. Rev. Neurosci. 2001, 2, 685–694. [Google Scholar] [CrossRef] [PubMed]
- Figueroa-Jiménez, M.D.; Cañete-Massé, C.; Carbó-Carreté, M.; Zarabozo-Hurtado, D.; Peró-Cebollero, M.; Salazar-Estrada, J.G.; Guàrdia-Olmos, J. Resting state default-mode network connectivity in Down Syndrome. Brain Behav. 2021, 11, e01905. [Google Scholar] [CrossRef]
- Lloyd, S. Measures of complexity: A nonexhaustive list. Control. Syst. Mag. IEEE 2001, 21, 7–8. [Google Scholar]
- Anderson, J.S.; Nielsen, J.A.; Ferguson, M.A.; Burback, M.C.; Cox, E.T.; Dai, L.; Gerig, G.; Edgin, J.O.; Korenberg, J.R. Abnormal brain synchrony in Down Syndrome. NeuroImage Clin. 2013, 2, 703–715. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vega, J.N.; Hohman, T.J.; Pryweller, J.R.; Dykens, E.M.; Thornton-Wells, T.A. Resting-state functional connectivity in individuals with Down syndrome and Williams syndrome compared with typically developing controls. Brain Connect. 2015, 5, 461–475. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wilson, L.R.; Vatansever, D.; Annus, T.; Williams, G.B.; Hong, Y.T.; Fryer, T.D.; Nestor, P.J.; Holland, A.J.; Zaman, S.H. Differential effects of Down’s syndrome and Alzheimer’s neuropathology on default mode connectivity. Hum. Brain Mapp. 2019, 40, 4551–4563. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Supekar, K.; Menon, V.; Rubin, D.; Musen, M.; Greicius, M.D. Network analysis of intrinsic functional brain connectivity in Alzheimer’s disease. PLoS Comput. Biol. 2008, 4, e1000100. [Google Scholar] [CrossRef]
- Sporns, O.; Honey, C.J. Small worlds inside big brains. Proc. Natl. Acad. Sci. USA 2006, 103, 19219–19220. [Google Scholar] [CrossRef] [Green Version]
- Xu, X.; Li, W.; Tao, M.; Xie, Z.; Gao, X.; Yue, L.; Wang, P. Effective and Accurate Diagnosis of Subjective Cognitive Decline Based on Functional Connection and Graph Theory View. Front. Neurosci. 2020, 14, 577887. [Google Scholar] [CrossRef] [PubMed]
- Mancho-Fora, N.; Montalà-Flaquer, M.; Farràs-Permanyer, L.; Bartrés-Faz, D.; Vaqué-Alcázar, L.; Peró-Cebollero, M.; Guàrdia-Olmos, J. Resting-State Functional Connectivity Dynamics in Healthy Aging: An Approach Through Network Change Point Detection. Brain Connect. 2020, 10, 134–142. [Google Scholar] [CrossRef]
- Andrews-Hanna, J.R.; Snyder, A.Z.; Vincent, J.L.; Lustig, C.; Head, D.; Raichle, M.E.; Buckner, R.L. Disruption of large-scale brain systems in advanced aging. Neuron 2007, 56, 924–935. [Google Scholar] [CrossRef] [Green Version]
- Antonenko, D.; Flöel, A. Healthy Aging by Staying Selectively Connected: A Mini-Review. Gerontology 2014, 60, 3–9. [Google Scholar] [CrossRef] [Green Version]
- Deb, S.; Hare, M.; Prior, L.; Bhaumik, S. Dementia Screening Questionnaire for Individuals with Intellectual disabilities. Br. J. Psychiatry 2007, 190, 440–444. [Google Scholar] [CrossRef] [Green Version]
- Dubois, B.; Slachevsky, A.; Litvan, I.; Pillon, B.F.A.B. The FAB: A Frontal Assessment Battery at Bedside. Neurology 2000, 55, 1621–1626. [Google Scholar] [CrossRef] [Green Version]
- Kaufman, A.S. Kaufman Brief. Intelligence Test.: KBIT; AGS, American Guidance Service: Circle Pines, MN, USA, 1990. [Google Scholar]
- FMRIB Software Library v5.0. Available online: https://fsl.fmrib.ox.ac.uk/fsl/fslwiki (accessed on 2 March 2019).
- Diez, I.; Bonifazi, P.; Escudero, I.; Mateos, B.; Muñoz, M.A.; Stramaglia, S.; Cortes, J.M. A novel brain partition highlights the modular skeleton shared by structure and function. Sci. Rep. 2015, 5, 10532. [Google Scholar] [CrossRef]
- Ashburner, J.; Friston, K.J. Nonlinear spatial normalization using basis functions. Hum. Brain Mapp. 1999, 7, 254–266. [Google Scholar] [CrossRef]
- Tzourio-Mazoyer, N.; Landeau, B.; Papathanassiou, D.; Crivello, F.; Etard, O.; Delcroix, N.; Mazoyer, B.; Joliot, M. Automated Anatomical Labeling of Activations in SPM Using a Macroscopic Anatomical Parcellation of the MNI MRI Single-Subject Brain. Neuroimage 2002, 15, 273–289. [Google Scholar] [CrossRef]
- Huang, C.C.; Hsieh, W.J.; Lee, P.L.; Peng, L.N.; Liu, L.K.; Lee, W.J.; Huang, J.K.; Chen, L.K.; Lin, C.P. Age-related changes in resting-state networks of a large sample size of healthy elderly. CNS Neurosci. Ther. 2015, 21, 817–825. [Google Scholar]
- Dierssen, M. Down Syndrome: The Brain in Trisomic Mode. Nat. Rev. Neurosci. 2012, 13, 844–858. [Google Scholar] [PubMed]
- Lanfranchi, S.; Berteletti, I.; Torrisi, E.; Vianello, R.; Zorzi, M. Numerical Estimation in Individuals with Down syndrome. Res. Dev. Disabil. 2015, 36, 222–229. [Google Scholar] [CrossRef] [PubMed]
- Hamburg, S.; Lowe, B.; Startin, C.M.; Padilla, C.; Coppus, A.; Silverman, W.; Lott, I. Assessing general cognitive and adaptive abilities in adults with Down syndrome: A systematic review. J. Neurodev. Disord. 2019, 11, 20. [Google Scholar] [CrossRef] [Green Version]
- Ripoll, S.B. Algunos Problemas de Los Test de Inteligencia En La Evaluación de Los Alumnos/as Con Retraso Mental: El caso WISC-R. Siglo Cero Rev. Española Sobre Discapac. Intelect. 2001, 32, 21–25. [Google Scholar]
- Sinai, A.; Hassiotis, A.; Rantell, K.; Strydom, A. Assessing Specific Cognitive Deficits Associated with Dementia in older adults with Down syndrome: Use and validity of the Arizona Cognitive Test Battery (ACTB). PLoS ONE 2016, 11, e0153917. [Google Scholar] [CrossRef] [Green Version]
- Esbensen, A.J.; Hoffman, E.K.; Shaffer, R.; Chen, E.; Patel, L.; Jacola, L. Reliability of parent report measures of behaviour in children with Down syndrome. J. Intellect. Disabil. Res. 2018, 62, 785–797. [Google Scholar] [CrossRef]
- Key, A.P.; Dykens, E.M. Event-Related Potential Index of Age-Related Differences in Memory Processes in Adults with Down syndrome. Neurobiol. Aging 2014, 35, 247–253. [Google Scholar] [CrossRef] [Green Version]
- Pujol, J.; Del Hoyo, L.; Blanco-Hinojo, L.; de Sola, S.; Macià, D.; Martínez-Vilavella, G.; Dierssen, M. Anomalous brain functional connectivity contributing to poor adaptive behavior in Down syndrome. Cortex 2015, 64, 148–156. [Google Scholar] [CrossRef]
- Santarnecchi, E.; Emmendorfer, A.; Tadayon, S.; Rossi, S.; Rossi, A.; Pascual-Leone, A. Network Connectivity correlates of variability in fluid intelligence performance. Intelligence 2017, 65, 35. [Google Scholar] [CrossRef]
- Stam, C.J.; Jones, B.F.; Nolte, G.; Breakspear, M.; Scheltens, P. Small-World Networks and Functional Connectivity in Alzheimer’s disease. Cereb. Cortex 2007, 17, 92–99. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stam, C.J.; De Haan, W.; Daffertshofer, A.B.F.J.; Jones, B.F.; Manshanden, I.; van Cappellen van Walsum, A.M.; Montez, T.; Verbunt, J.P.A.; Munck, J.C.; van Dijk, B.W.; et al. Graph theoretical analysis of magnetoencephalographic functional connectivity in Alzheimer’s disease. Brain 2009, 132, 213–224. [Google Scholar] [CrossRef] [PubMed]
- Bassett, D.S.; Bullmore, E.; Verchinski, B.A.; Mattay, V.S.; Weinberger, D.R.; Meyer-Lindenberg, A. Hierarchical organization of human cortical networks in health and schizophrenia. J. Neurosci. 2008, 28, 9239–9248. [Google Scholar] [CrossRef] [Green Version]
- Leistedt, S.J.; Coumans, N.; Dumont, M.; Lanquart, J.P.; Stam, C.J.; Linkowski, P. Altered sleep brain functional connectivity in acutely depressed patients. Hum. Brain Mapp. 2009, 30, 2207–2219. [Google Scholar] [CrossRef]
- Ponten, S.C.; Douw, L.; Bartolomei, F.; Reijneveld, J.C.; Stam, C.J. Indications for Network Regularization during absence seizures: Weighted and unweighted graph theoretical analyses. Exp. Neurol. 2009, 217, 197–204. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Zhu, C.; He, Y.; Zang, Y.; Cao, Q.; Zhang, H.; Zhong, Q.; Wang, Y. Altered Small-world Brain Functional Networks in children with attention-deficit/hyperactivity disorder. Hum. Brain Mapp. 2009, 30, 638–649. [Google Scholar] [CrossRef]
- Chen, H.; Sheng, X.; Luo, C.; Qin, R.; Ye, Q.; Zhao, H.; Xu, Y.; Bai, F. Alzheimer’s Disease Neuroimaging Initiative. The compensatory phenomenon of the functional connectome related to pathological biomarkers in individuals with subjective cognitive decline. Transl. Neurodegener. 2020, 9, 1–14. [Google Scholar] [CrossRef]

| DMN Partial | DMN Anterior | DMN Ventral | Sensorimotor | Visual | |||||
|---|---|---|---|---|---|---|---|---|---|
| Number in the AAL90 Atlas | Region Name | Number in the AAL90 Atlas | Region Name | Number in the AAL90 Atlas | Region Name | Number in the AAL90 Atlas | Region Name | Number in the AAL90 Atlas | Region Name |
| 59 | Parietal_Sup_L | 29 | Insula_L | 35 | Cingulum_Post_L | 1 | Precentral_L | 43 | Calcarine_L |
| 60 | Parietal_Sup_R | 30 | Insula_R | 36 | Cingulum_Post_R | 2 | Precentral_R | 44 | Calcarine_R |
| 61 | Parietal_Inf_L | 31 | Cingulum_Ant_L | 37 | Hippocampus_L | 7 | Frontal_Mid_L | 45 | Cuneus_L |
| 62 | Parietal_Inf_R | 32 | Cingulum_Ant_R | 38 | Hippocampus_R | 8 | Frontal_Mid_R | 46 | Cuneus_R |
| 85 | Temporal_Mid_L | 87 | Temporal_Pole_Mid_L | 39 | ParaHippocampal_L | 19 | Supp_Motor_Area_L | 47 | Lingual_L |
| 86 | Temporal_Mid_R | 88 | Temporal_Pole_Mid_R | 40 | ParaHippocampal_R | 20 | Supp_Motor_Area_R | 48 | Lingual_R |
| 55 | Fusiform_L | 57 | PostcentralL | 49 | Occipital_Sup_L | ||||
| 56 | Fusiform_R | 58 | Postcentral_R | 50 | Occipital_Sup_R | ||||
| 65 | Angular_L | 63 | SupraMarginal_L | 51 | Occipital_Mid_L | ||||
| 66 | Angular_R | 64 | SupraMarginal_R | 52 | Occipital_Mid_R | ||||
| 67 | Precuneus_L | 69 | Paracentral_Lobule_L | 53 | Occipital_Inf_L | ||||
| 68 | Precuneus_R | 70 | Paracentral_Lobule_R | 54 | Occipital_Inf_R | ||||
| Description | Calculations | |
|---|---|---|
| Functional Integration (FI) | ||
| Number of communities | Number of independent communities detected in a group of specific ROIs. Estimated maximum number of statistically significant clusters in a random network. | |
| Mean of the path lengths | The path length of a node i (Li) is the average number of edges that must be crossed to go from node i to the remaining nodes in the network | where N is the total number of nodes in the network, n is the number of nodes involved and dij is the shortest path length between node i and j. |
| Standard deviation of the path lengths | The characteristic path length is a global measure of the network, i.e., there is only one value for the entire network. It consists of the average path length of each node in the network. | |
| Functional Segregation (FS) | ||
| Global clustering coefficient | This is the average value of the clustering coefficients, which is the fraction of triangles around a node, and is equivalent to the fraction of neighbors of the node that are neighbors among them. | |
| Number of triangles | This is the number of connected triangles that can be estimated within a network in Euclidean space. | An ordered pair in which V is a nonempty set of vertices and E is a set of edges. Where E consists of unordered pairs of vertices such as {x, y} E, then x and y are said to be adjacent. |
| Other measures | ||
| Density | The network density (D) is the number of edges in the network in proportion to the total number of possible edges. | where K is the number of edges in the network and N is the total number of nodes in the network. |
| Small world (Watts–Strogatz) | Networks that present a higher clustering coefficient than expected by chance and that, in addition, have a characteristic shortest path length. | A network is said to represent this type of organization if the calculated index is greater than 1. |
| Complexity | The number of nodes and alternative paths that exist within a specific network | |
| Criteria Variables | Mean (Standard Deviation) | Bootstrap 95% CI | Symmetry | Kurtosis |
|---|---|---|---|---|
| Mental Age Vocabulary | 6.11 (2.51) | 4.97–7.26 | 0.967 | 0.034 |
| Mental Age Matrices | 5.42 (1.53) | 4.72–6.12 | 1.032 | 0.843 |
| FAB (Frontal Assessment Battery) Score | 9.62 (4.20) | 7.71–11.53 | 0.215 | 0.681 |
| Total Score Vocabulary | 23.71 (13.91) | 17.38–30.04 | 0.603 | −0.452 |
| Total Score Matrices | 47.47 (13.76) | 41.21–53.74 | −0.063 | 0.879 |
 | Network Indicators | DS Group | Control Group | ||
| Mean | SD | Mean | SD | ||
| Number of communities | 2.23 | 0.922 | 0.001 | 0.0001 | |
| Mean of the weighted path | 0.496 | 0.193 | 0.12 | 0.02 | |
| Standard deviation of the weighted path | 0.276 | 0.146 | 0.06 | 0.01 | |
| Density | 0.768 | 0.101 | 0.001 | 0.0001 | |
| Small-worldness | 1.027 | 0.088 | 0.0001 | 0.0001 | |
| Global clustering coefficient | 0.317 | 0.006 | 0.001 | 0.0001 | |
| Complexity | 0.822 | 0.238 | 0.11 | 0.02 | |
| Segregation (triangles) | 105.136 | 90.590 | 104.66 | 22.31 | |
| DMN Anterior (DMNa) partial network (6 ROIs) | |||||
 | Network Indicators | DS Group | Control Group | ||
| Mean | SD | Mean | SD | ||
| Number of communities | 2.41 | 0.194 | 0.21 | 0.04 | |
| Mean of the weighted path | 0.423 | 0.043 | 0.10 | 0.02 | |
| Standard deviation of the weighted path | 0.299 | 0.027 | 0.05 | 0.01 | |
| Density | 0.768 | 0.021 | 0.0001 | 0.0001 | |
| Small-worldness | 1.027 | 0.018 | 0.0001 | 0.0001 | |
| Global clustering coefficient | 0.318 | 0.001 | 0.0001 | 0.0001 | |
| Complexity | 0.868 | 0.046 | 0.11 | 0.02 | |
| Segregation (triangles) | 109.181 | 18.035 | 103.14 | 21.98 | |
| DMN Ventral (DMNv) partial network (12 ROIs) | |||||
 | Network Indicators | DS Group | Control Group | ||
| Mean | SD | Mean | SD | ||
| Number of communities | 2.409 | 0.107 | 0.59 | 0.12 | |
| Mean of the weighted path | 0.605 | 0.033 | 0.08 | 0.01 | |
| Standard deviation of the weighted path | 0.232 | 0.029 | 0.03 | 0.01 | |
| Density | 0.454 | 0.001 | 0.001 | 0.001 | |
| Small-worldness | 1.240 | 0.014 | 0.05 | 0.01 | |
| Global clustering coefficient | 0.316 | 0.001 | 0.001 | 0.001 | |
| Complexity | 0.871 | 0.031 | 0.071 | 0.0001 | |
| Segregation (triangles) | 209.818 | 38.25 | 209.27 | 44.61 | |
| Sensorimotor (SM) partial network (12 ROIs) | |||||
 | Network Indicators | DS Group | Control Group | ||
| Mean | SD | Mean | SD | ||
| Number of communities | 2.545 | 0.108 | 0.49 | 0.10 | |
| Mean of the weighted path | 0.677 | 0.027 | 0.08 | 0.01 | |
| Standard deviation of the weighted path | 0.202 | 0.032 | 0.22 | 0.04 | |
| Density | 0.454 | 0.001 | 0.001 | 0.001 | |
| Small-worldness | 1.230 | 0.013 | 0.07 | 0.01 | |
| Global clustering coefficient | 0.313 | 0.007 | 0.003 | 0.0008 | |
| Complexity | 0.884 | 0.027 | 0.06 | 0.001 | |
| Segregation (triangles) | 217.090 | 37.303 | 208.28 | 44.40 | |
| Visual (VIS) partial network (12 ROIs) | |||||
 | Network Indicators | DS Group | Control Group | ||
| Mean | SD | Mean | SD | ||
| Number of communities | 2.500 | 0.109 | 0.35 | 0.07 | |
| Mean of the weighted path | 0.783 | 0.016 | 0.07 | 0.01 | |
| Standard deviation of the weighted path | 0.115 | 0.009 | 0.04 | 0.009 | |
| Density | 0.454 | 0.001 | 0.0001 | 0.0001 | |
| Small-worldness | 1.271 | 0.011 | 0.06 | 0.001 | |
| Global clustering coefficient | 0.316 | 0.005 | 0.002 | 0.0006 | |
| Complexity | 0.930 | 0.011 | 0.04 | 0.008 | |
| Segregation (triangles) | 220.001 | 37.549 | 199.05 | 42.43 | |
| GLOBAL NETWORK ANALYSIS (48 ROIs) | |||||
 | Network Indicators | DS Group | Control Group | ||
| Mean | SD | Mean | SD | ||
| Number of communities | 4.863 | 0.257 | 1.184 | 0.25 | |
| Mean of the weighted path | 0.690 | 0.022 | 0.07 | 0.01 | |
| Standard deviation of the weighted path | 0.248 | 0.030 | 0.08 | 0.01 | |
| Density | 0.152 | 0.020 | 0.001 | 0.0001 | |
| Small-worldness | 2.483 | 0.090 | 0.17 | 0.03 | |
| Global clustering coefficient | 0.312 | 0.001 | 0.001 | 0.0003 | |
| Complexity | 0.724 | 0.0617 | 0.03 | 0.008 | |
| Segregation (triangles) | 865,76 | 201.190 | 837.19 | 178.49 | |
| COMPLEXITY INDICATOR | DMN Partial | DMN Anterior | DMN Ventral | Sensorimotor | Visual | Observed Distribution | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| FAB | VOC | MAT | FAB | VOC | MAT | FAB | VOC. | MAT | FAB | VOC | MAT | FAB | VOC | MAT | FAB | VOC | MAT | |
| Number of communities | 0.221 | 0.333 ** | 0.572 ** | −0.051 | 0.018 | 0.070 | −0.026 | 0.110 | 0.328 ** | −0.193 * | −0.238 ** | 0.375 ** | 0.172 * | 0.247 ** | 0.510 ** | |||
| Mean of the path lengths | −0.365 ** | 0.184 * | −0.172 * | 0.065 | 0.372 ** | 0.000 | −0.241 ** | −0.024 | −0.275 ** | −0.190 | 0.516 ** | −0.127 | −0.362 ** | −0.435 * | −0.500 ** | |||
| SD of the path lengths | 0.132 | −0.164 * | 0.002 | −0.022 | −0.188 * | −0.206 ** | 0.297 ** | 0.075 | 0.166 * | 0.163 * | −0.047 | 0.001 | 0.376 ** | 0.644 ** | 0.491 ** | |||
| Density | −0.007 | −0.341 ** | −0.182 * | −0.007 | −0.341 ** | −0.182 * | 0.011 | 0.007 | 0.022 | 0.003 | 0.012 | 0.008 | 0.084 | 0.026 | 0.003 | |||
| Small-world | 0.007 | 0.341 ** | 0.182 * | 0.007 | 0.341 ** | 0.182 * | −0.143 * | -0.003 | −0.167 * | 0.155 | 0.012 | 0.090 | 0.317 ** | 0.448* | 0.197 | |||
| Global clustering coefficient | −0.105 | 0.022 | 0.033 | 0.017 | −0.008 | 0.105 | 0.068 | 0.092 | −0.311 * | 0.131 | −0.075 | −0.107 * | 0.245* | 0.325 ** | 0.091 | |||
| Complexity | 0.037 | 0.069 | −0.008 | 0.042 | −0.029 | 0.172 * | −0.175 * | −0.557 ** | −0.139 | −0.077 | 0.028 | −0.267 * | −0.404 ** | −0.436 ** | −0.409 ** | |||
| Number of triangles | −0.181 * | −0.418 | −0.457 * | −0.352 ** | −0.427 ** | −0.453 ** | −0.359 ** | −0.441 ** | −0.417 ** | −0.397 ** | −0.438 * | −0.452 * | −0.368 ** | −0.416 | −0.438 ** | |||
| Mental age vocabulary | 0.653 ** | 0.907 ** | 0.189 * | |||||||||||||||
| Mental age matrices | 0.305 ** | 0.693 ** | 0.346 ** | |||||||||||||||
| Criteria Variables | Predictor | Parameter | p | Effect Size | Observations | |
|---|---|---|---|---|---|---|
| FAB total score | Mental age estimated from the vocabulary score | 0.997 | 0.01 | 0.376 | AIC = 124.367 | Outliers: participant number 11 (Cook’s distance = 0.242) |
| Mean of the weighted path length of the DMN network | −8.361 | 0.034 | 0.241 | |||
| Variables excluded | Step number 1: Number of communities in DMN partial; Number of triangles in the subnetworks DMN partial, DMN ventral, Sensoriomotor and Visual; SD of the path length of DMN ventral, Small-world in DMN ventral; Number of communities in Sensoriomotor network; mean and SD of the path lengths of Visual network; Small-world of the visual network, Global clustering coefficient of visual network; complexity of the visual network and Mental age derived from matrices subtest. | |||||
| Vocabulary subtest score | Mental age estimated from the vocabulary score | 5.156 | <0.001 | 0.950 | AIC = 112.556 | Outliers: participant number 16 (Cook’s distance = 0.388) and 19 (Cook’s distance = 0.264) |
| Mean of the weighted path length of the sensorimotor network | −15.069 | 0.004 | 0.026 | |||
| Small-worldness of the visual network | 25.226 | 0.029 | 0.013 | |||
| Complexity of the ventral DMN | −13.281 | 0.046 | 0.010 | |||
| Variables excluded | Step number 1: Number of communities, Mean and SD of the path lengths and number of triangles of DMN partial; Mean and SD of the path lengths, density and Small-world of the DMN anterior; Number of communities of DMN Ventral; Number of communities of Sensoriomotor and Visual networks. Step number 2: Density and Small-world of DMN partial; Number of triangles of DMN anterior; Complexity and Number of triangles of DMN ventral; Number of triangles of Sensoriomoto network a Mental Age derived from Matrices Test. Step number 3: Mean and SD of path lengths of Visual network; Global clustering coefficient, Complexity and Number of triangles of Visual network. | |||||
| Matrices subtest score | Number of communities in the visual network | 14.581 | 0.004 | 0.562 | AIC = 168.857 | Outliers: participant number 7 (Cook’s distance = 0.432) |
| Number of communities in the DMN networks | −24.149 | 0.042 | 0.247 | |||
| Variables excluded | Step number 1: Mean of the path lengths, Density, Small-world and Number of triangles of DMN partial; SD of path lengths, Density, Small-world, Complexity and Number of Triangles of DMN anterior; all the indicators (except Density) of the DMN ventral; Number of communities, Complexity and Number of triangles of Sensoriomotor network; Mean and SD of the path lengths, Small-world, Complexity and Number of triangles of Visual network. Step number 2: Mental age derived from vocabulary and matrices tests. | |||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Figueroa-Jimenez, M.D.; Carbó-Carreté, M.; Cañete-Massé, C.; Zarabozo-Hurtado, D.; Peró-Cebollero, M.; Salazar-Estrada, J.G.; Guàrdia-Olmos, J. Complexity Analysis of the Default Mode Network Using Resting-State fMRI in Down Syndrome: Relationships Highlighted by a Neuropsychological Assessment. Brain Sci. 2021, 11, 311. https://doi.org/10.3390/brainsci11030311
Figueroa-Jimenez MD, Carbó-Carreté M, Cañete-Massé C, Zarabozo-Hurtado D, Peró-Cebollero M, Salazar-Estrada JG, Guàrdia-Olmos J. Complexity Analysis of the Default Mode Network Using Resting-State fMRI in Down Syndrome: Relationships Highlighted by a Neuropsychological Assessment. Brain Sciences. 2021; 11(3):311. https://doi.org/10.3390/brainsci11030311
Chicago/Turabian StyleFigueroa-Jimenez, María Dolores, María Carbó-Carreté, Cristina Cañete-Massé, Daniel Zarabozo-Hurtado, Maribel Peró-Cebollero, José Guadalupe Salazar-Estrada, and Joan Guàrdia-Olmos. 2021. "Complexity Analysis of the Default Mode Network Using Resting-State fMRI in Down Syndrome: Relationships Highlighted by a Neuropsychological Assessment" Brain Sciences 11, no. 3: 311. https://doi.org/10.3390/brainsci11030311







