Estimating Components and Costs of Standard Care for Children with Autism Spectrum Disorder in Europe from a Large International Sample
Abstract
:1. Introduction
1.1. Recommended Interventions for Children with ASD in Europe
1.2. Costs of Standard Care for Individuals with ASD Across the Lifespan
2. Materials and Methods
2.1. Study Design and Participants
2.2. Data Collected and Management
- Type of therapy or intervention (individual vs. group settings; number of sessions; average duration of one session; private costs per session);
- Institutional stay (number of admissions; number of days spent in facility; kind of facility/institution; private costs incurred);
- Outpatient treatment (number of visits of psychiatric/somatic services; number of visits of other specialized services; private costs incurred);
- Dietary supplement and medication (name of the drug/supplement, dosage, duration, private costs incurred);
- Special diet (kind; estimated extra cost);
- Care giver investment:
- Working hours spent on treatment as described above, including driving, of all private care givers (weekly average in hours);
- Work situation (working or not working);
- Reduced hours due to the child’s needs (in percentage);
- Employing anybody privately to help care for the child (if yes, private costs incurred);
- Any additional assistant/aide in school/at home for the child (if yes, number of hours per week);
2.3. Assessment of Costs
2.4. Statistical Analyses
2.4.1. Regression Analysis
2.4.2. Sensitivity Analysis
3. Results
3.1. Participant Characteristics
3.2. Services Used
3.3. Costs of Services
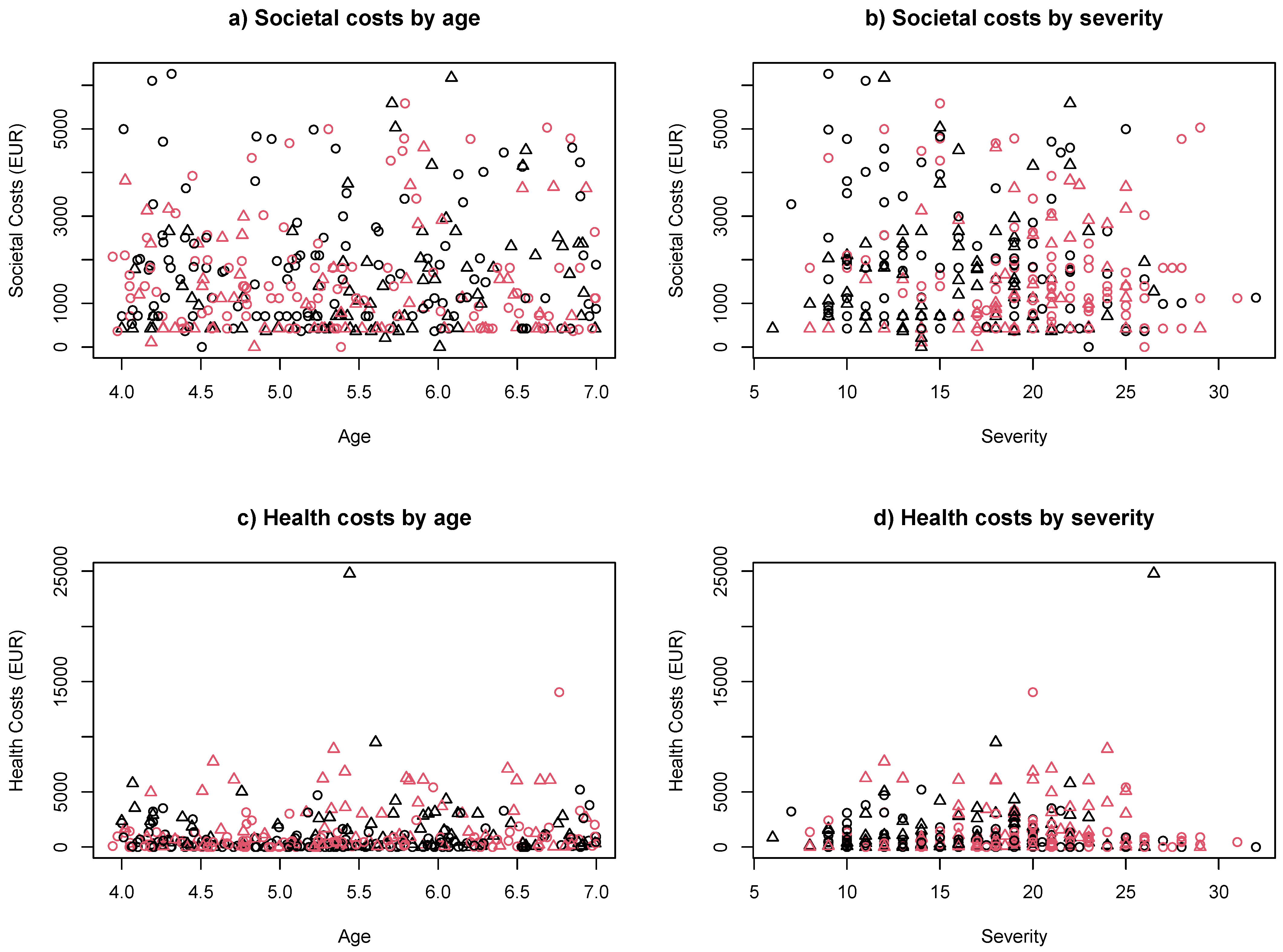
3.4. Regression Analysis
3.5. Sensitivity Analysis
4. Discussion
4.1. Main Finding
4.2. Health-Care Service Used
4.3. Costs of Health Care Services
4.4. Costs of Other Health Care Services
4.5. Costs of Indirect Societal Costs
4.6. Regression Analysis of the Predictors of Costs
4.7. Sensitivity Analysis of Health Services and Societal Costs
4.8. Limitation
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- World Health Organization. International Classification of Diseases for Mortality and Morbidity Statistics, 11th Revision ed; World Health Organization: Geneva, Switzerland, 2018; Available online: https://icd.who.int/browse11/l-m/en (accessed on 1 April 2020).
- Chiarotti, F.; Venerosi, A. Epidemiology of autism spectrum Disorders: A review of worldwide prevalence estimates since 2014. Brain Sci. 2020, 10, 274. [Google Scholar] [CrossRef] [PubMed]
- Fombonne, E. Epidemiological controversies in autism. Swiss Arch. Neurol. Psychiatry Psychother. 2020, 171, w03084. [Google Scholar] [CrossRef] [Green Version]
- Halladay, A.K.; Bishop, S.J.; Constantino, J.N.; Daniels, A.M.; Koenig, K.A.; Palmer, K.; Messinger, D.S.; Pelphrey, K.A.; Sanders, S.J.; Singer, A.T.; et al. Sex and gender differences in autism spectrum disorder: Summarizing evidence gaps and identifying emerging areas of priority. Mol. Autism 2015, 6, 36. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Messinger, D.S.; Young, G.S.; Webb, S.J.; Ozonoff, S.; Bryson, S.E.; Carter, A.; Carver, L.; Charman, T.; Chawarska, K.; Curtin, S.; et al. Early sex differences are not autism-specific: A Baby Siblings Research Consortium (BSRC) study. Mol. Autism 2015, 6, 32. [Google Scholar] [CrossRef] [Green Version]
- Ozonoff, S.; Young, G.S.; Carter, A.; Messinger, D.; Yirmiya, N.; Zwaigenbaum, L.; Bryson, S.; Carver, L.J.; Constantino, J.N.; Dobkins, K.; et al. Recurrence risk for autism spectrum disorders: A baby siblings research consortium study. Pediatrics 2011, 128, e488–e495. [Google Scholar] [CrossRef] [Green Version]
- Sandin, S.; Lichtenstein, P.; Kuja-Halkola, R.; Larsson, H.; Hultman, C.M.; Reichenberg, A. The familial risk of autism. J. Am. Med. Assoc. 2014, 311, 1770–1777. [Google Scholar] [CrossRef] [PubMed]
- Tick, B.; Bolton, P.; Happé, F.; Rutter, M.; Rijsdijk, F. Heritability of autism spectrum disorders: A meta-analysis of twin studies. J. Child Psychol. Psychiatry 2016, 57, 585–595. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bieleninik, Ł.; Posserud, M.-B.; Geretsegger, M.; Thompson, G.; Elefant, C.; Gold, C. Tracing the temporal stability of autism spectrum diagnosis and severity as measured by the Autism Diagnostic Observation Schedule: A systematic review and meta-analysis. PLoS ONE 2017, 12, e0183160. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barthéémy, C.; Fuentes, J.; Howlin, P.; van der Gaag, R. People with Autism Spectrum Disorder. Identification, Understanding, Intervention, 3rd ed.; Autism Europe: Ghent, Brussels, 2019. [Google Scholar]
- Baxter, A.J.; Brugha, T.S.; Erskine, H.E.; Scheurer, R.W.; Vos, T.; Scott, J.G. The epidemiology and global burden of autism spectrum disorders. Psychol. Med. 2015, 45, 601–613. [Google Scholar] [CrossRef]
- Buescher, A.V.S.; Cidav, Z.; Knapp, M.; Mandell, D.S. Costs of autism spectrum disorders in the United Kingdom and the United States. JAMA Pediatr. 2014, 168, 721–728. [Google Scholar] [CrossRef]
- Lavelle, T.A.; Weinstein, M.C.; Newhouse, J.P.; Munir, K.; Kuhlthau, K.A.; Prosser, L.A. Economic burden of childhood autism spectrum disorders. Pediatrics 2014, 133, e520–e529. [Google Scholar] [CrossRef] [PubMed]
- Barrett, B.; Byford, S.; Sharac, J.; Hudry, K.; Leadbitter, K.; Temple, K.; Aldred, C.; Slonims, V.; Green, J.; PACT Consortium. Service and wider societal costs of very young children with autism in the UK. J. Autism Dev. Disord. 2012, 42, 797–804. [Google Scholar] [CrossRef] [PubMed]
- Knapp, M.; Romeo, R.; Beecham, J. Economic cost of autism in the UK. Autism 2009, 13, 317–336. [Google Scholar] [CrossRef] [PubMed]
- Peacock, G.; Amendah, D.D.; Ouyang, L.; Groose, S.D. Autism spectrum disorders and health care expenditures: The effects of co-occurring conditions. J. Dev. Behav. Pediatr. 2012, 33, 2–8. [Google Scholar] [CrossRef]
- Shimabukuro, T.T.; Grosse, S.D.; Rice, C. Medical expenditures for children with an autism spectrum disorder in a privately insured population. J. Autism Dev. Disord. 2007, 38, 546–552. [Google Scholar] [CrossRef] [Green Version]
- Croen, L.A.; Najjar, D.V.; Ray, G.T.; Lotspeich, L.; Bernal, P. A comparison of health care utilization and costs of children with and without autism spectrum disorders in a large group-model health plan. Pediatrics 2006, 118, e1203–e1211. [Google Scholar] [CrossRef] [PubMed]
- Mandell, D.S.; Cao, J.; Ittenbach, R.; Pinto-Martin, J. Medicaid expenditures for children with autistic spectrum disorders: 1994 to 1999. J. Autism Dev. Disord. 2006, 36, 475–485. [Google Scholar] [CrossRef]
- Liptak, G.S.; Stuart, T.; Auinger, P. Health care utilization and expenditures for children with autism: Data from U.S. National Samples. J. Autism Dev. Disord. 2006, 36, 871–879. [Google Scholar] [CrossRef] [PubMed]
- Ganz, M.L. The lifetime distribution of the incremental societal costs of autism. Arch. Pediatr. Adolesc. Med. 2007, 161, 343–349. [Google Scholar] [CrossRef] [Green Version]
- Leslie, D.L.; Martin, A. Health care expenditures associated with autism spectrum disorders. Arch. Pediatr. Adolesc. Med. 2007, 161, 350–355. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lokhandwala, T.; Khanna, R.; West-Strum, D. Hospitalization burden among individuals with autism. J. Autism Dev. Disord. 2011, 42, 95–104. [Google Scholar] [CrossRef] [PubMed]
- Vohra, R.; Madhavan, S.; Sambamoorthi, U. Comorbidity prevalence, healthcare utilization, and expenditures of Medicaid enrolled adults with autism spectrum disorders. Autism 2017, 21, 995–1009. [Google Scholar] [CrossRef] [Green Version]
- Järbrink, K.; Knapp, M. The economic impact of autism in Britain. Autism 2001, 5, 7–22. [Google Scholar] [CrossRef]
- Peters-Scheffer, N.; Didden, R.; Korzilius, H.; Matson, J. Cost comparison of early intensive behavioral intervention and treatment as usual for children with autism spectrum disorder in The Netherlands. Res. Dev. Disabil. 2012, 33, 1763–1772. [Google Scholar] [CrossRef]
- Roddy, A.; O’Neill, C. The economic costs and its predictors for childhood autism spectrum disorders in Ireland: How is the burden distributed? Autism 2019, 23, 1106–1118. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xiong, N.; Yang, L.; Yu, Y.; Hou, J.; Li, J.; Li, Y.; Liu, H.; Zhang, Y.; Jiao, Z. Investigation of raising burden of children with autism, physical disability and mental disability in China. Res. Dev. Disabil. 2011, 32, 306–311. [Google Scholar] [CrossRef] [PubMed]
- Horlin, C.; Falkmer, M.; Parsons, R.; Albrecht, M.A.; Falkmer, T. The Cost of autism spectrum disorders. PLoS ONE 2014, 9, e106552. [Google Scholar] [CrossRef] [Green Version]
- Hodgetts, S.; Zwaigenbaum, L.; Nicholas, D. Profile and predictors of service needs for families of children with autism spectrum disorders. Autism 2014, 19, 673–683. [Google Scholar] [CrossRef] [Green Version]
- Bieleninik, Ł.; Geretsegger, M.; Drscmus, K.M.; Assmus, J.; Thompson, G.; Gattino, G.; Elefant, C.; Gottfried, T.; Igliozzi, R.; Muratori, F.; et al. Effects of improvisational music therapy vs enhanced standard care on symptom severity among children with autism spectrum disorder: The TIME—A randomized clinical trial. J. Am. Med. Assoc. 2017, 318, 525–535. [Google Scholar] [CrossRef] [PubMed]
- Kaufman, A.S.; Kaufman, N.L. Kaufman Assessment Battery for Children (K-ABC). Interpretive Manual; American Guidance Service: Circle Pines, MN, USA, 1983. [Google Scholar]
- Geretsegger, M.; Holck, U.; Gold, C. Randomised controlled trial of improvisational music therapy’s effectiveness for children with autism spectrum disorders (TIME-A): Study protocol. BMC Pediatr. 2012, 12, 2. [Google Scholar] [CrossRef] [Green Version]
- Kimman, M.; Dirksen, C.; Voogd, A.; Falger, P.; Gijsen, B.; Thuring, M.; Lenssen, A.; Van Der Ent, F.; Verkeyn, J.; Haekens, C.; et al. Economic evaluation of four follow-up strategies after curative treatment for breast cancer: Results of an RCT. Eur. J. Cancer 2011, 47, 1175–1185. [Google Scholar] [CrossRef] [PubMed]
- Roijen, L.H.-V.; Van Straten, A.; Al, M.; Rutten, F.; Donker, M. Cost-utility of brief psychological treatment for depression and anxiety. Br. J. Psychiatry 2006, 188, 323–329. [Google Scholar] [CrossRef] [Green Version]
- Curtis, L.; Burns, A. Unit Costs of Health and Social Care 2018; University of Kent: Canterbury, UK, 2018. [Google Scholar]
- Coleman, C.L.; Cottell, J. Childcare Survey 2019; Coram Family and Childcare: London, UK, 2019. [Google Scholar]
- Barrett, B.; Mosweu, I.; Jones, C.R.; Charman, T.; Baird, G.; Simonoff, E.; Pickles, A.; Happé, F.; Byford, S. Comparing service use and costs among adolescents with autism spectrum disorders, special needs and typical development. Autism 2015, 19, 562–569. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Drummond, M.F.; Sculpher, M.J.; Torrance, G.W. Methods for the Economic Evaluation of Healthcare Programmes, 3rd ed.; Oxford University Press: Oxford, UK, 2005. [Google Scholar]
- Glick, H.A.; Doshi, J.A.; Sonnad, S.S.; Polsky, D. Economic Evaluation in Clinical Trials; Oxford University Press: Oxford, UK, 2007. [Google Scholar]
- Tsiplova, K.; Ungar, W.J.; Flanagan, H.E.; Otter, J.D.; Waddell, C.; Murray, P.; D’Entremont, B.; Léger, N.; Garon, N.; Bryson, S.; et al. Types of services and costs of programs for preschoolers with autism spectrum disorder across sectors: A comparison of two canadian provinces. J. Autism Dev. Disord. 2019, 49, 2492–2508. [Google Scholar] [CrossRef] [PubMed]
- Ben-Sasson, A.; Gal, E.; Fluss, R.; Katz-Zetler, N.; Cermak, S.A. Update of a meta-analysis of sensory symptoms in ASD: A new decade of research. J. Autism Dev. Disord. 2019, 49, 4974–4996. [Google Scholar] [CrossRef]
- Fulceri, F.; Grossi, E.; Contaldo, A.; Narzisi, A.; Apicella, F.; Parrini, I.; Tancredi, R.; Calderoni, S.; Muratori, F. Motor skills as moderators of core symptoms in autism spectrum disorders: Preliminary data from an exploratory analysis with artificial neural networks. Front. Psychol. 2019, 9, 2683. [Google Scholar] [CrossRef]
- Reichow, B.; Barton, E.E.; Boyd, B.A.; Hume, K. Early intensive behavioral intervention (EIBI) for young children with autism spectrum disorders (ASD). Cochrane Database Syst. Rev. 2018, 10, CD009260. [Google Scholar] [CrossRef] [PubMed]
- Rogge, N.; Janssen, J. The economic costs of autism spectrum disorder: A literature review. J. Autism Dev. Disord. 2019, 49, 2873–2900. [Google Scholar] [CrossRef]
- Chasson, G.S.; Harris, G.E.; Neely, W.J. Cost comparison of early intensive behavioral intervention and special education for children with autism. J. Child Fam. Stud. 2007, 16, 401–413. [Google Scholar] [CrossRef]
- Cidav, Z.; Munson, J.; Estes, A.; Dawson, G.; Rogers, S.; Mandell, D. Cost offset associated with early start denver model for children with autism. J. Am. Acad. Child Adolesc. Psychiatry 2017, 56, 777–783. [Google Scholar] [CrossRef]
- Sallows, G.O.; Graupner, T.D. Intensive behavioral treatment for children with autism: Four-year outcome and predictors. Am. J. Ment. Retard. 2005, 110, 417–438. [Google Scholar] [CrossRef]
- Butter, E.M.; Wynn, J.; Mulick, J.A. Early intervention critical to autism treatment. Pediatr. Ann. 2003, 32, 677–684. [Google Scholar] [CrossRef]
- Järbrink, K.; Fombonne, E.; Knapp, M. Measuring the parental, service and cost impacts of children with autistic spectrum disorder: A pilot study. J. Autism Dev. Disord. 2003, 33, 395–402. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Järbrink, K. The economic consequences of autism spectrum disorder among children in a Swedish municipality. J. Res. Pract. 2007, 11, 453–463. [Google Scholar]
- Motiwala, S.S.; Gupta, S.; Lilly, M.B.; Ungar, W.J.; Coyte, P.C. The cost-effectiveness of expanding intensive behavioural intervention to all autistic children in Ontario: In the past year, several court cases have been brought against provincial governments to increase funding for Intensive Behavioural Intervention (IBI). This economic evaluation examines the costs and consequences of expanding an IBI program. Healthc. Policy 2006, 1, 135–151. [Google Scholar] [PubMed] [Green Version]
- Byford, S.; The PACT Consortium; Cary, M.; Barrett, B.; Aldred, C.R.; Charman, T.; Howlin, P.; Hudry, K.; Leadbitter, K.; Le Couteur, A.; et al. Cost-effectiveness analysis of a communication-focused therapy for pre-school children with autism: Results from a randomised controlled trial. BMC Psychiatry 2015, 15, 316. [Google Scholar] [CrossRef] [Green Version]
- Cidav, Z.; Marcus, S.C.; Mandell, D.S. Implications of childhood autism for parental employment and earnings. Pediatrics 2012, 129, 617–623. [Google Scholar] [CrossRef] [Green Version]
- Peretti, S.; Mariano, M.; Mazzocchetti, C.; Mazza, M.; Pino, M.C.; Di Pianella, A.V.; Valenti, M. Diet: The keystone of autism spectrum disorder? Nutr. Neurosci. 2019, 22, 825–839. [Google Scholar] [CrossRef]
- Kogan, M.D.; Strickland, B.B.; Blumberg, S.J.; Singh, G.K.; Perrin, J.M.; Van Dyck, P.C. A National Profile of the Health Care Experiences and Family Impact of Autism Spectrum Disorder among Children in the United States, 2005–2006. Pediatrics 2008, 122, e1149–e1158. [Google Scholar] [CrossRef]
- Althubaiti, A. Information bias in health research: Definition, pitfalls, and adjustment methods. J. Multidiscip. Health 2016, 9, 211–217. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Byford, S.; Leese, M.; Knapp, M.; Seivewright, H.; Cameron, S.; Jones, V.; Davidson, K.; Tyrer, P. Comparison of alternative methods of collection of service use data for the economic evaluation of health care interventions. Health Econ. 2006, 16, 531–536. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | No. | Value | |
|---|---|---|---|
| Age, mean (SD), y | 357 | 5.4 (0.9) | |
| Sex, No. (%) | Boys | 295 (82.6) | |
| Girls | 62 (17.4) | ||
| Diagnosis, No. (%) | 357 | ||
| Childhood autism (ICD-10 code F84.0) | 295 (82.6) | ||
| Atypical autism (ICD-10 code F84.1) | 3 (0.8) | ||
| Asperger syndrome (ICD-10 code F84.5) | 14 (3.9) | ||
| PDD (ICD-10 code F84.9) | 45 (12.6) | ||
| ADOS 1, No. (%) | 357 | ||
| Module 1 | 218 (61.1) | ||
| Module 2 | 128 (35.9) | ||
| Module 3 | 11 (3.1) | ||
| ADOS score, mean (SD) | |||
| Total | 356 | 17.7 (5.3) | |
| Social affect | 357 | 13.8 (4.4) | |
| Language and communication | 357 | 3.3 (1.5) | |
| Reciprocal social interaction | 357 | 10.5 (3.6) | |
| Restricted and repetitive behavior | 356 | 3.9 (2) | |
| ADI-R score 2, mean (SD) | |||
| Reciprocal social interaction | 357 | 18.2 (5.8) | |
| Language and communication | 357 | 13 (4.2) | |
| Repetitive behaviors and interests | 357 | 5.8 (2.4) | |
| Early onset | 357 | 3.9 (1.1) | |
| IQ source 3, No. (%) | 357 | ||
| KABC | 8 (2.2) | ||
| Other standardized test | 209 (58.5) | ||
| Clinical judgment | 140 (39.2) | ||
| IQ, standardized test 4, mean (SD) | 210 | 75.5 (26.3) | |
| Intellectual disability (IQ < 70), No. (%) | 349 | 163 (46.7) | |
| Child care, No. (%) | 357 | ||
| Attends school | 222 (62.2) | ||
| Full-time care (≥7 h/d) | 80 (22.4) | ||
| Part-time care (<7 h/d) | 38 (10.6) | ||
| None of the above | 17 (4.8) | ||
| Maternal education, No. (%) | 351 | ||
| <12 y (less than high school) | 35 (10) | ||
| ≥12 y (equivalent to high school) | 130 (37) | ||
| University | 161 (45.9) | ||
| Unknown | 25 (7.1) | ||
| Paternal education, No. (%) | 347 | ||
| <12 y (less than high school) | 50 (14.4) | ||
| ≥12 y (equivalent to high school) | 112 (32.3) | ||
| University | 149 (42.9) | ||
| Unknown | 36 (10.4) | ||
| Maternal employment, No. (%) | 351 | ||
| Unemployed or social support | 47 (13.4) | ||
| Working part time | 90 (25.6) | ||
| Working full time | 67 (19.1) | ||
| Homemaker | 119 (33.9) | ||
| Other | 7 (2) | ||
| Unknown | 21 (6) | ||
| Paternal employment, No. (%) | 349 | ||
| Unemployed or social support | 18 (5.2) | ||
| Working part time | 18 (5.2) | ||
| Working full time | 259 (74.2) | ||
| Homemaker | 5 (1.4) | ||
| Other | 11 (3.2) | ||
| Unknown | 38 (10.9) | ||
| Adults in household, No. (%) | 338 | ||
| 1 | 45 (13.3) | ||
| 2 | 267 (79) | ||
| >2 | 26 (7.7) | ||
| Siblings in family, No. (%) | 335 | ||
| None | 90 (26.9) | ||
| 1 | 158 (47.2) | ||
| >1 | 87 (26) | ||
| Service Type | N (%) | Number of Sessions 1, M (SD) | Total Number of Hours 1, M (SD) |
|---|---|---|---|
| Interventions | |||
| Specialist autism services 2 | 122 (34) | 13.39 (15.55) | 47.24 (91.14) |
| Sensory/motor therapy | 149 (42) | 13.01 (10.62) | 9.16 (8.28) |
| Speech/language therapy | 205 (57) | 11.35 (9.04) | 7.29 (5.23) |
| Play therapy | 35 (10) | 12.71 (10.28) | 8.78 (5.47) |
| Behavioural intervention | 55 (15) | 24.2 (17.4) | 33.11 (35.82) |
| Social skills training | 31 (9) | 9.42 (6.65) | 8.88 (9.62) |
| Therapeutic recreational activities | 47 (13) | 9.3 (7.15) | 11.23 (27.06) |
| Other services (see text) | 59 (17) | 11.39 (12.31) | 11.88 (20.29) |
| Schooling | |||
| Attends school | 222 (62) | ||
| Full-time child care (7 h or more per day) | 80 (22) | ||
| Part-time child care (Less than 7 h per day) | 38 (11) | ||
| None of the above | 17 (5) | ||
| Other services | |||
| Institutional stay 3 | 12 (3) | 1.42 (0.67) | 1.58 (1.38) |
| Outpatient services 4 | 37 (10) | 1.22 (0.75) | |
| Medication 5 | 109 (31) | ||
| Diet | 59 (17) | ||
| Caregiver time investment | |||
| Caregiver time spent on services (hours/week) | 175 (49) | 8.74 (13.24) | |
| Reduction in working hours (percent of full-time) | 191 (54) | 63.85 (34.19) | |
| Child care help | 47 (13) | ||
| Additional aide at school or home (hours/week) | 108 (30) | 19.16 (11.04) |
| Service Type | M (SD) | Range |
|---|---|---|
| Health services costs | ||
| Specialist autism services | 314.91 (976.21) | 0 to 6048 |
| Sensory/motor therapy | 213.18 (459.5) | 0 to 3360 |
| Speech/language therapy | 251.42 (405.33) | 0 to 2016 |
| Play therapy | 31.54 (194.23) | 0 to 2184 |
| Behavioural intervention | 283.64 (1363.25) | 0 to 16,800 |
| Social skills training | 12.36 (63.85) | 0 to 672 |
| Therapeutic recreational activities | 22.53 (178.11) | 0 to 3024 |
| Other services | 62.69 (347.51) | 0 to 4200 |
| Institutional stay | 2.75 (51.9) | 0 to 980.61 |
| Outpatient services | 1.18 (10.23) | 0 to 131.64 |
| Medication | 6.17 (29.45) | 0 to 289.62 |
| Diet | 7.22 (35.49) | 0 to 455.14 |
| Sum of all health services costs | 1209.59 (2159.84) | 0 to 24,780 |
| Societal costs | ||
| Childcare/school | 460.59 (160.32) | 0 to 707.57 |
| Reduction in working hours | 523.86 (642.82) | 0 to 1946.08 |
| Child care help (private) | 18.24 (124.99) | 0 to 1645.54 |
| Additional aide at school or home | 621.28 (1145.96) | 0 to 4288 |
| Sum of all societal costs | 1623.96 (1316.7) | 0 to 6263.26 |
| Sum of all costs | 2833.56 (2497.5) | 84 to 26,050.54 |
| Source | Health Costs (All Participants) | Health Costs (Outlier Excluded) | Societal Costs (All Participants) | |||
|---|---|---|---|---|---|---|
| b (SE) | p | b (SE) | p | b (SE) | p | |
| Age (continuous) | 207.63 (133.38) | 0.120 | 213.20 (107.64) | 0.048 * | 32.99 (79.46) | 0.678 |
| Severity (continuous) | 14.74 (23.55) | 0.532 | −15.47 (19.13) | 0.419 | −16.68 (14.03) | 0.235 |
| Intellectual disability (binary) | 320.40 (249.90) | 0.201 | 566.11 (202.48) | 0.005 ** | −71.95 (148.88) | 0.629 |
| Service Type | n (%) | Number of Sessions 1, M (SD) | Total Number of Hours 1, M (SD) |
|---|---|---|---|
| Interventions | |||
| Specialist autism services 2 | 50 (14) | 7.48 (5.04) | 14.94 (16.76) |
| Sensory/motor therapy | 72 (20) | 10 (7.13) | 7.92 (5.38) |
| Speech/language therapy | 109 (31) | 8.72 (5.31) | 6.16 (4.11) |
| Play therapy | 21 (6) | 15.52 (12.29) | 10.63 (6.04) |
| Behavioural intervention | 19 (5) | 26.53 (22.14) | 35.61 (34.62) |
| Social skills training | 15 (4) | 12.6 (7.73) | 9.84 (9.98) |
| Therapeutic recreational activities | 25 (7) | 7.64 (4.68) | 4.8 (2.62) |
| Other services | 25 (7) | 11.88 (12.3) | 14.47 (28.14) |
| Schooling | |||
| Attends school | 121 (34) | ||
| Full-time child care (7 h or more per day) | 65 (18) | ||
| Part-time child care (Less than 7 h per day) | 26 (7) | ||
| None of the above | 5 (1) | ||
| Other services | |||
| Institutional stay 3 | 10 (3) | 1.5 (0.71) | 1.8 (1.4) |
| Outpatient services 4 | 24 (7) | 1.12 (0.45) | |
| Medication 5 | 55 (15) | ||
| Diet | 38 (11) | ||
| Caregiver time investment | |||
| Caregiver time spent on services (hours/week) | 85 (24) | 6.54 (14.84) | |
| Reduction in working hours (percent of full-time) | 111 (31) | 65.37 (32.24) | |
| Child care help | 26 (7) | ||
| Additional aide at school or home (hours/week) | 77 (22) | 19.81 (10.59) |
| Service Type | M (SD) | Range |
|---|---|---|
| Health services costs | ||
| Specialist autism services | 98.29 (244.31) | 0 to 1512 |
| Sensory/motor therapy | 122.28 (283.22) | 0 to 1960 |
| Speech/language therapy | 200.77 (337.66) | 0 to 2016 |
| Play therapy | 48.39 (247.19) | 0 to 2184 |
| Behavioural intervention | 186.79 (1102.81) | 0 to 13,440 |
| Social skills training | 13.8 (74.46) | 0 to 672 |
| Therapeutic recreational activities | 7.19 (35.73) | 0 to 336 |
| Other services | 53.01 (252) | 0 to 2436 |
| Institutional stay | 0 (0) | 0 to 0 |
| Outpatient services | 0.28 (4.12) | 0 to 60.69 |
| Medication | 1.73 (16.12) | 0 to 228.97 |
| Diet | 7.68 (38.99) | 0 to 455.14 |
| Sum of all health services costs | 740.19 (1322.7) | 0 to 14,042 |
| Societal costs | ||
| Childcare/school | 491.63 (155.58) | 0 to 707.57 |
| Reduction in working hours | 486.91 (589.6) | 0 to 1946.08 |
| Child care help (private) | 16.53 (110.73) | 0 to 1320.9 |
| Additional aide at school or home | 753.36 (1220.87) | 0 to 4288 |
| Sum of all societal costs | 1748.43 (1344.59) | 0 to 6263.26 |
| Sum of all costs | 2488.62 (1951.48) | 101.14 to 15,856.9 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bieleninik, Ł.; Gold, C. Estimating Components and Costs of Standard Care for Children with Autism Spectrum Disorder in Europe from a Large International Sample. Brain Sci. 2021, 11, 340. https://doi.org/10.3390/brainsci11030340
Bieleninik Ł, Gold C. Estimating Components and Costs of Standard Care for Children with Autism Spectrum Disorder in Europe from a Large International Sample. Brain Sciences. 2021; 11(3):340. https://doi.org/10.3390/brainsci11030340
Chicago/Turabian StyleBieleninik, Łucja, and Christian Gold. 2021. "Estimating Components and Costs of Standard Care for Children with Autism Spectrum Disorder in Europe from a Large International Sample" Brain Sciences 11, no. 3: 340. https://doi.org/10.3390/brainsci11030340







