Quality Control after Intracochlear Intralabyrinthine Schwannoma Resection and Cochlear Implantation
Abstract
:1. Introduction
2. Material and Methods
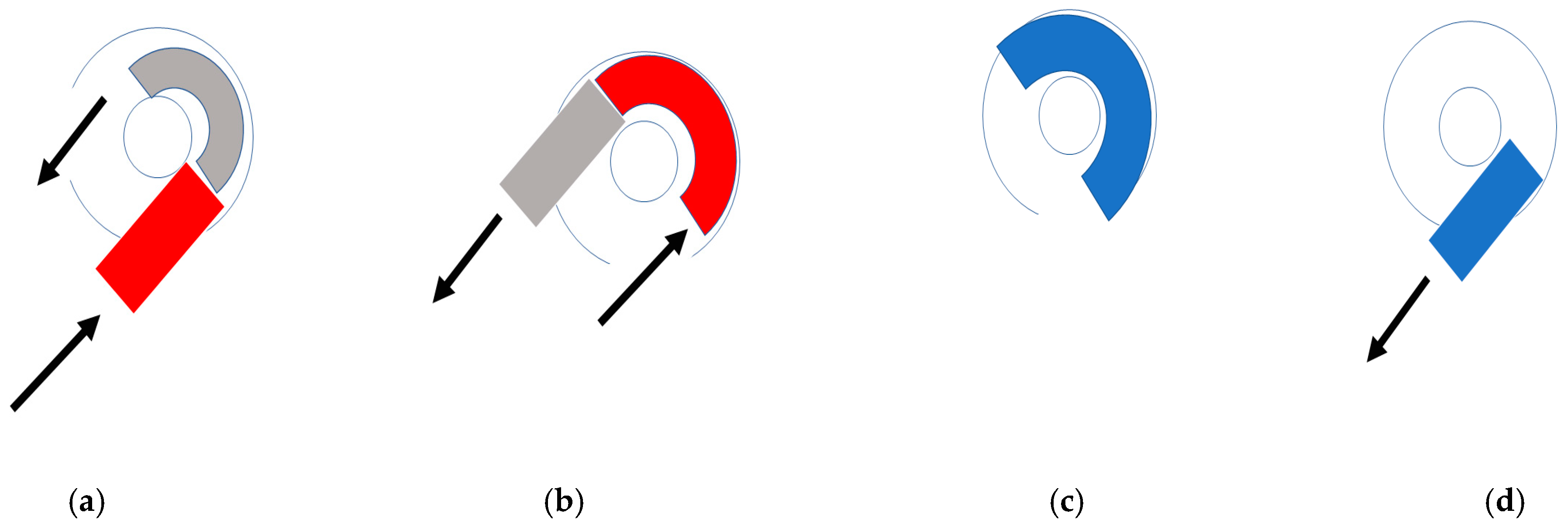
2.1. Surgical Approach
2.2. Sequence
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sanna, M.; Medina, M.D.; Macak, A.; Rossi, G.; Sozzi, V.; Prasad, S.C. Vestibular schwannoma resection with ipsilateral simultaneous cochlear implantation in patients with normal contralateral hearing. Audiol. Neurotol. 2016, 21, 286–295. [Google Scholar] [CrossRef] [PubMed]
- Wick, C.C.; Butler, M.J.; Yeager, L.H.; Kallogjeri, D.; Durakovic, N.; McJunkin, J.L.; Shew, M.A.; Herzog, J.A.; Buchman, C.A. Cochlear implant outcomes following vestibular schwannoma resection: Systematic review. Otol. Neurotol. 2020, 41, 1190–1197. [Google Scholar] [CrossRef] [PubMed]
- Kronenberg, J.; Horowitz, Z.; Hildesheimer, M. Intracochlear schwannoma and cochlear implantation. Ann. Otol. Rhinol. Laryngol. 1999, 108, 659–660. [Google Scholar] [CrossRef] [PubMed]
- Carlson, M.L.; Neff, B.A.; Sladen, D.P.; Link, M.J.; Driscoll, C.L. Cochlear implantation in patients with intracochlear and intralabyrinthine schwannomas. Otol. Neurotol. 2016, 37, 647–653. [Google Scholar] [CrossRef]
- Aschendorff, A.; Arndt, S.; Laszig, R.; Wesarg, T.; Hassepaß, F.; Beck, R. Treatment and auditory rehabilitation of intralabyrinthine schwannoma by means of cochlear implants: English version. HNO 2017, 65 (Suppl. 1), 46–51. [Google Scholar] [CrossRef]
- Plontke, S.K.; Rahne, T.; Pfister, M.; Götze, G.; Heider, C.; Pazaitis, N.; Strauss, C.; Caye-Thomasen, P.; Kösling, S. Intralabyrinthine schwannomas: Surgical management and hearing rehabilitation with cochlear implants. HNO 2017, 65 (Suppl. 2), 136–148. [Google Scholar] [CrossRef] [Green Version]
- Plontke, S.K.; Kösling, S.; Rahne, T. Cochlear implantation after partial or subtotal cochleoectomy for intracochlear schwannoma removal-a technical report. Otol. Neurotol. 2018, 39, 365–371. [Google Scholar] [CrossRef] [Green Version]
- Kennedy, R.; Shelton, C.; Salzman, K.; Davidson, H.; Harnsberger, H. Intralabyrinthine schwannomas: Diagnosis, management, and a new classification system. Otol. Neurotol. 2004, 25, 160–167. [Google Scholar] [CrossRef]
- Salzman, K.L.; Childs, A.M.; Davidson, H.C.; Kennedy, R.J.; Shelton, C.; Harnsberger, H.R. Intralabyrinthine schwannomas: Imaging diagnosis and classification. Am. J. Neuroradiol. 2012, 33, 104–109. [Google Scholar] [CrossRef] [Green Version]
- Plontke, S.K. An improved technique of subtotal cochleoectomy for removal of intracochlear schwannoma and single-stage cochlear implantation. Otol. Neurotol. 2020, 41, e891. [Google Scholar] [CrossRef]
- Marchioni, D.; De Rossi, S.; Soloperto, D.; Presutti, L.; Sacchetto, L.; Rubini, A. Intralabyrinthine schwannomas: A new surgical treatment. Eur. Arch. Otorhinolaryngol. 2018, 275, 1095–1102. [Google Scholar] [CrossRef]
- Sudhoff, H.; Gehl, H.B.; Scholtz, L.U.; Todt, I. MRI observation after intralabyrinthine and vestibular schwannoma resection and cochlear implantation. Front. Neurol. 2020, 11, 759. [Google Scholar] [CrossRef] [PubMed]
- Deux, J.F.; Marsot-Dupuch, K.; Ouayoun, M.; Huy, P.T.B.; Sterkers, J.M.; Meyer, B.; Tubiana, J.M. Slow-growing labyrinthine masses: Contribution of MRI to diagnosis, follow-up and treatment. Neuroradiology 1998, 40, 684–689. [Google Scholar] [CrossRef] [PubMed]
- Magliulo, G.; Colicchio, G.; Romana, A.F.; Stasolla, A. Intracochlear schwannoma. Skull Base. 2010, 20, 115–118. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jiang, Z.Y.; Kutz, J.W., Jr.; Roland, P.S.; Isaacson, B. Intracochlear schwannomas confined to the otic capsule. Otol Neurotol. 2011, 32, 1175–1179. [Google Scholar] [CrossRef] [Green Version]
- Van Abel, K.M.; Carlson, M.L.; Link, M.J.; Neff, B.A.; Beatty, C.W.; Lohse, C.M.; Eckel, L.J.; Lane, J.I.; Driscoll, C.L. Primary inner ear schwannomas: A case series and systematic review of the literature. Laryngoscope 2013, 123, 1957–1966. [Google Scholar] [CrossRef]
- Tieleman, A.; Casselman, J.W.; Somers, T. Imaging of intralabyrinthine schwannomas: A retrospective study of 52 cases with emphasis on lesion growth. Am. J. Neuroradiol. 2008, 29, 898–905. [Google Scholar] [CrossRef] [Green Version]
- Todt, I.; Rademacher, G.; Mittmann, P.; Wagner, J.; Mutze, S.; Ernst, A. MRI artifacts and cochlear implant positioning at 3 T in vivo. Otol. Neurotol. 2015, 36, 972–976. [Google Scholar] [CrossRef]
- Gantz, B.J.; McCabe, B.F.; Tyler, R.S. Use of multichannel cochlear implants in obstructed and obliterated cochleas. Otolaryngol. Head Neck Surg. 1988, 98, 72–81. [Google Scholar] [CrossRef]
- Balkany, T.; Luntz, M.; Telischi, F.F.; Hodges, A.V. Intact canal wall drill-out procedure for implantation of the totally ossified cochlea. Am. J. Otol. 1997, 18 (Suppl. 6), S58–S559. [Google Scholar]
- Lenarz, T.; Battmer, R.D.; Lesinski, A.; Parker, J. Nucleus double electrode array: A new approach for ossified cochleae. Am. J. Otol. 1997, 18 (Suppl. 6), S39–S41. [Google Scholar] [PubMed]
- Arriaga, M.A.; Marks, S. Simultaneous cochlear implantation and acoustic neuroma resection: Imaging considerations, technique and functional outcome. Otolaryngol. Head Neck Surg. 1995, 112, 325–328. [Google Scholar] [CrossRef]
- Walton, J.; Donnelly, N.P.; Tam, Y.C.; Joubert, I.; Durie-Gair, J.; Jackson, C.; Mannion, R.A.; Tysome, J.R.; Axon, P.R.; Scoffings, D.J. MRI without magnet removal in neurofibromatosis type 2 patients with cochlear and auditory brainstem implants. Otol. Neurotol. 2014, 35, 821–825. [Google Scholar] [CrossRef] [PubMed]
- Carlson, M.L.; Neff, B.A.; Link, M.J.; Lane, J.I.; Watson, R.E.; McGee, K.P.; Bernstein, M.A.; Driscoll, C.L.W. Magnetic resonance imaging with cochlear implant magnet in place. Otol. Neurotol. 2015, 36, 965–971. [Google Scholar] [CrossRef]
- Ay, N.; Gehl, H.B.; Sudhoff, H.; Todt, I. Effect of head position on cochlear implant MRI artifact. Eur. Arch. Otorhinolaryngol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Todt, I.; Tittel, A.; Ernst, A.; Mittmann, P.; Mutze, S. Pain free 3 T MRI scans in cochlear implantees. Otol. Neurotol. 2017, 38, e401–e404. [Google Scholar] [CrossRef] [PubMed]
- Edmonson, H.; Carlson, M.; Patton, A.; Watson, R. MR imaging and cochlear implants with retained internal magnets: Reducing artifacts near highly inhomogeneous magnetic fields. RadioGraphics. 2018, 38, 94–106. [Google Scholar] [CrossRef] [Green Version]
- Bagattini, M.; Quesnel, A.M.; Röösli, C. Histopathologic Evaluation of Intralabyrinthine Schwannoma. Audiol Neurootol. 2021, 26, 265–272. [Google Scholar] [CrossRef]



| No. | Month between Surgery and MRI | ILS Form | Surgical Access | Implant | Specific Information | Monosyllabic Understanding at 65 dB |
|---|---|---|---|---|---|---|
| 1 | 3 | vestibulo cochlear | cochleostomy | 512 | 70 | |
| 2 | 21 | cochlear | drill out | Synchrony | 30 | |
| 3 | 14 | cochlear | double access | Synchrony | testelectrode | 45 |
| 4 | 19 | vestibulo cochlear | labyrinthectomy and double access | 622 | testelectrode | 60 |
| 5 | 15 | vestibulo cochlear | labyrinthectomy and double access | Synchrony | gelfoam pusher | 55 |
| 6 | 14 | cochlear | Double access | AB 3D | gelfoam pusher | 65 |
| 7 | 8 | cochlear | cochleostomy | Synchrony | apical ossification | Lost follow up |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sudhoff, H.; Scholtz, L.U.; Gehl, H.B.; Todt, I. Quality Control after Intracochlear Intralabyrinthine Schwannoma Resection and Cochlear Implantation. Brain Sci. 2021, 11, 1221. https://doi.org/10.3390/brainsci11091221
Sudhoff H, Scholtz LU, Gehl HB, Todt I. Quality Control after Intracochlear Intralabyrinthine Schwannoma Resection and Cochlear Implantation. Brain Sciences. 2021; 11(9):1221. https://doi.org/10.3390/brainsci11091221
Chicago/Turabian StyleSudhoff, Holger, Lars Uwe Scholtz, Hans Björn Gehl, and Ingo Todt. 2021. "Quality Control after Intracochlear Intralabyrinthine Schwannoma Resection and Cochlear Implantation" Brain Sciences 11, no. 9: 1221. https://doi.org/10.3390/brainsci11091221
APA StyleSudhoff, H., Scholtz, L. U., Gehl, H. B., & Todt, I. (2021). Quality Control after Intracochlear Intralabyrinthine Schwannoma Resection and Cochlear Implantation. Brain Sciences, 11(9), 1221. https://doi.org/10.3390/brainsci11091221







