Changes in Affective Behavior and Oxidative Stress after Binge Alcohol in Male and Female Rats
Abstract
1. Introduction
2. Materials and Methods
2.1. Animals
2.2. Alcohol Administration Paradigm
2.3. Behavioral Testing
2.4. Corticosterone Measurements
2.5. Tissue Preparation
2.6. Activity of Antioxidant Enzymes and Total Levels of Glutathione
2.7. Oxidative Damage Assays
2.8. Statistical Analyses
3. Results
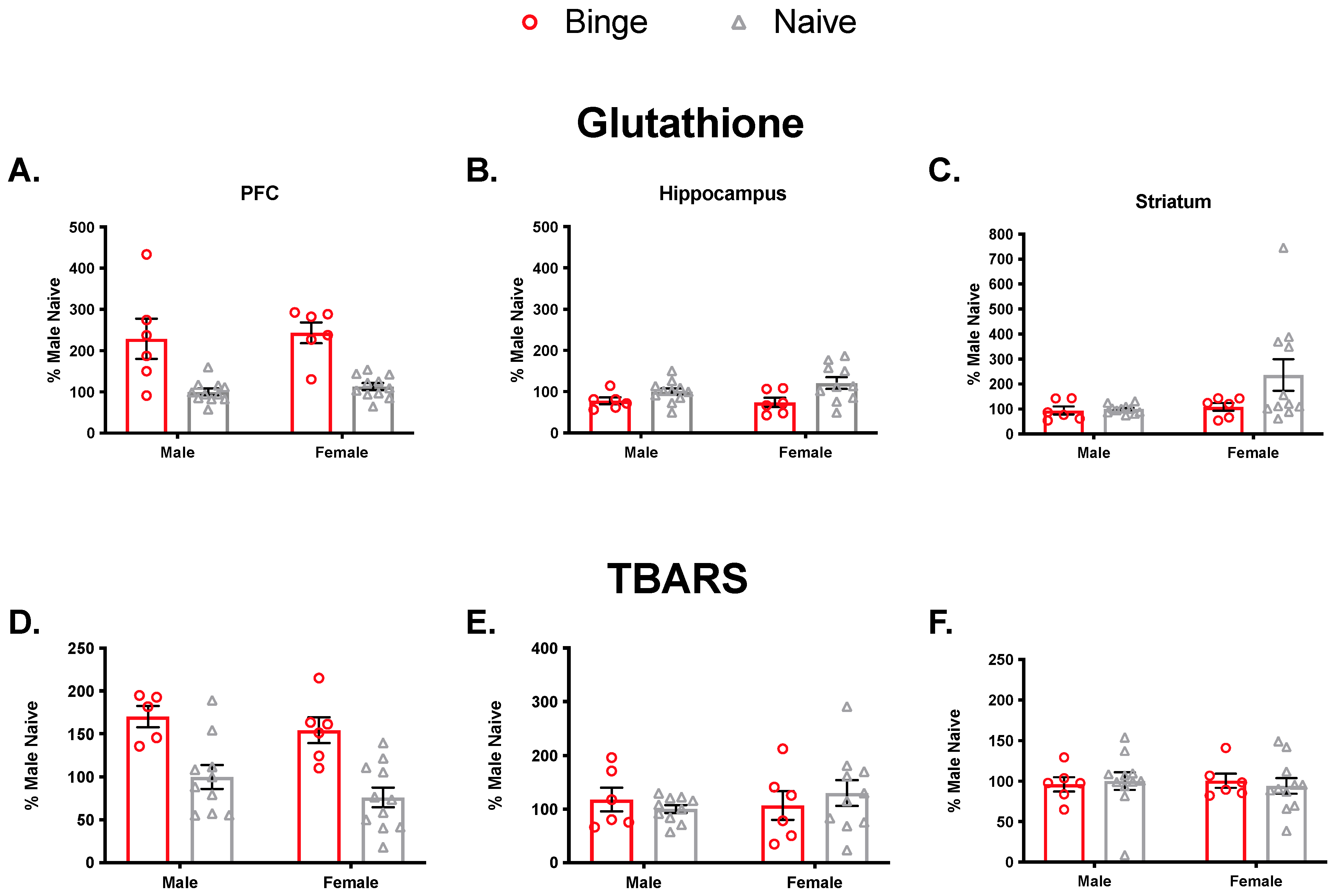
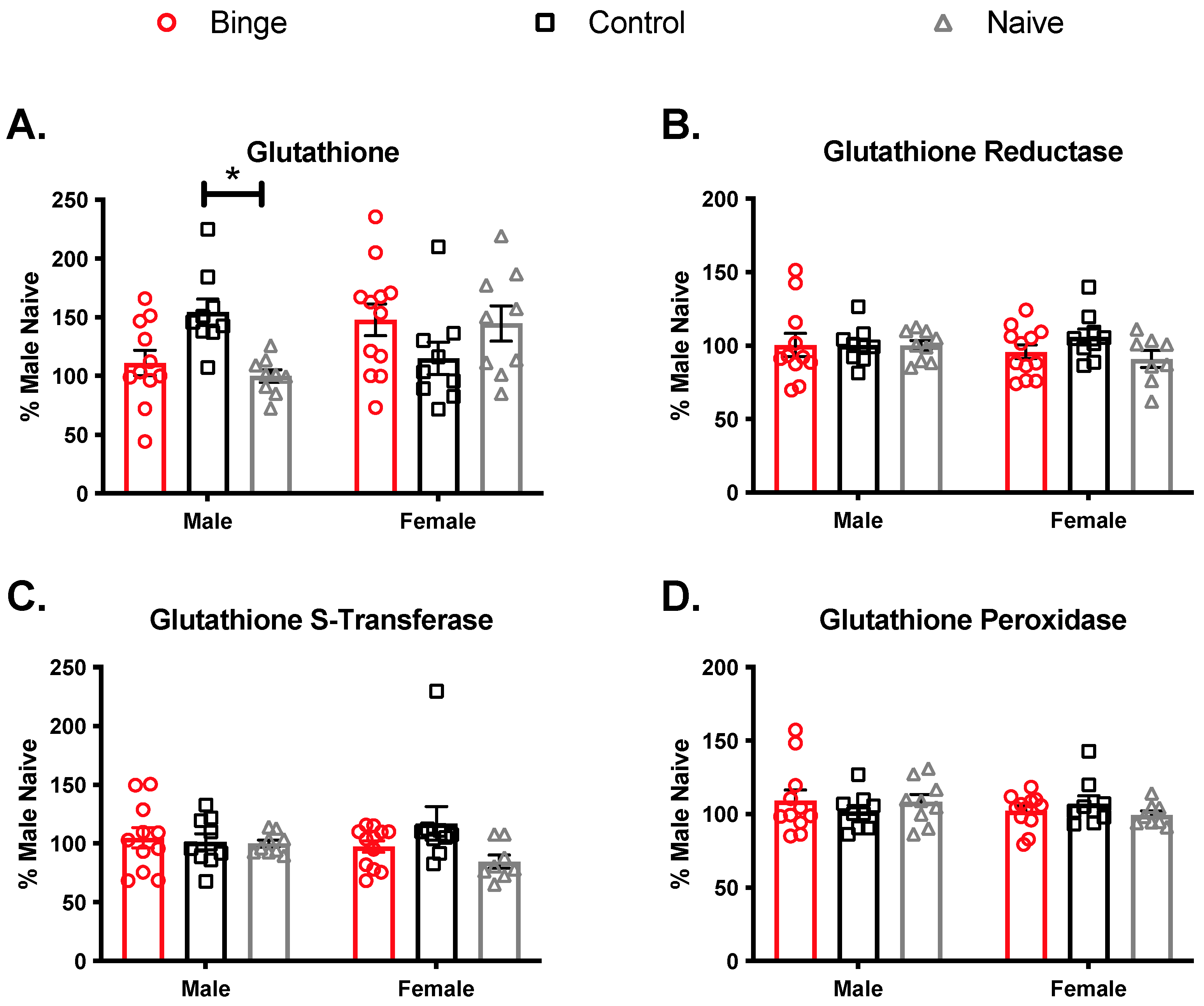
3.1. Single Binge
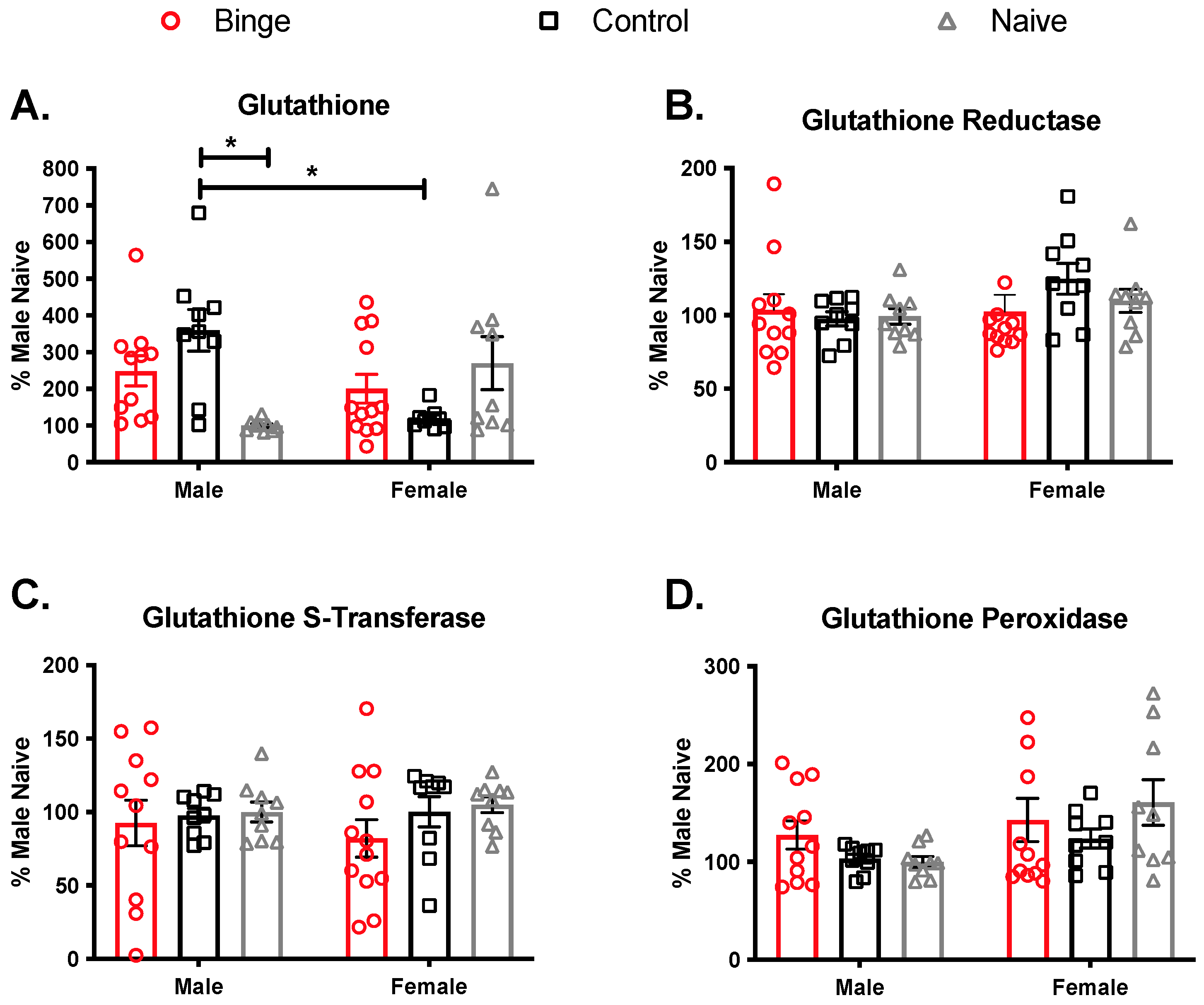
3.2. Multiple Binge
3.2.1. Body Weight, Blood Ethanol, and Corticosterone
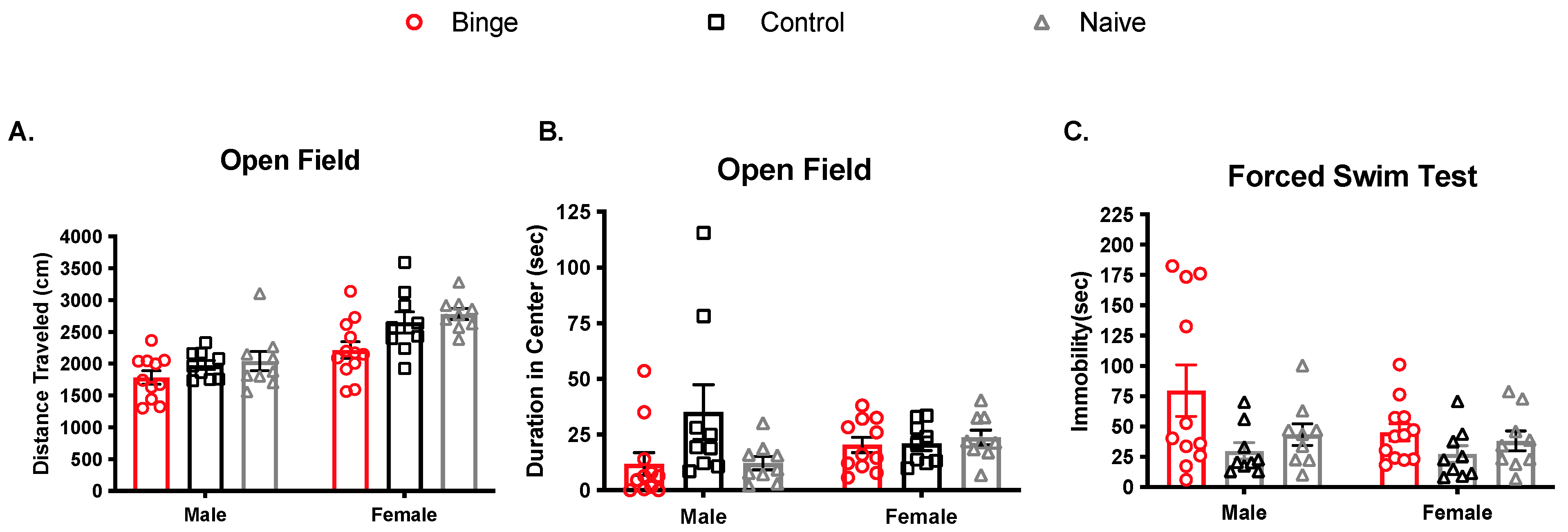
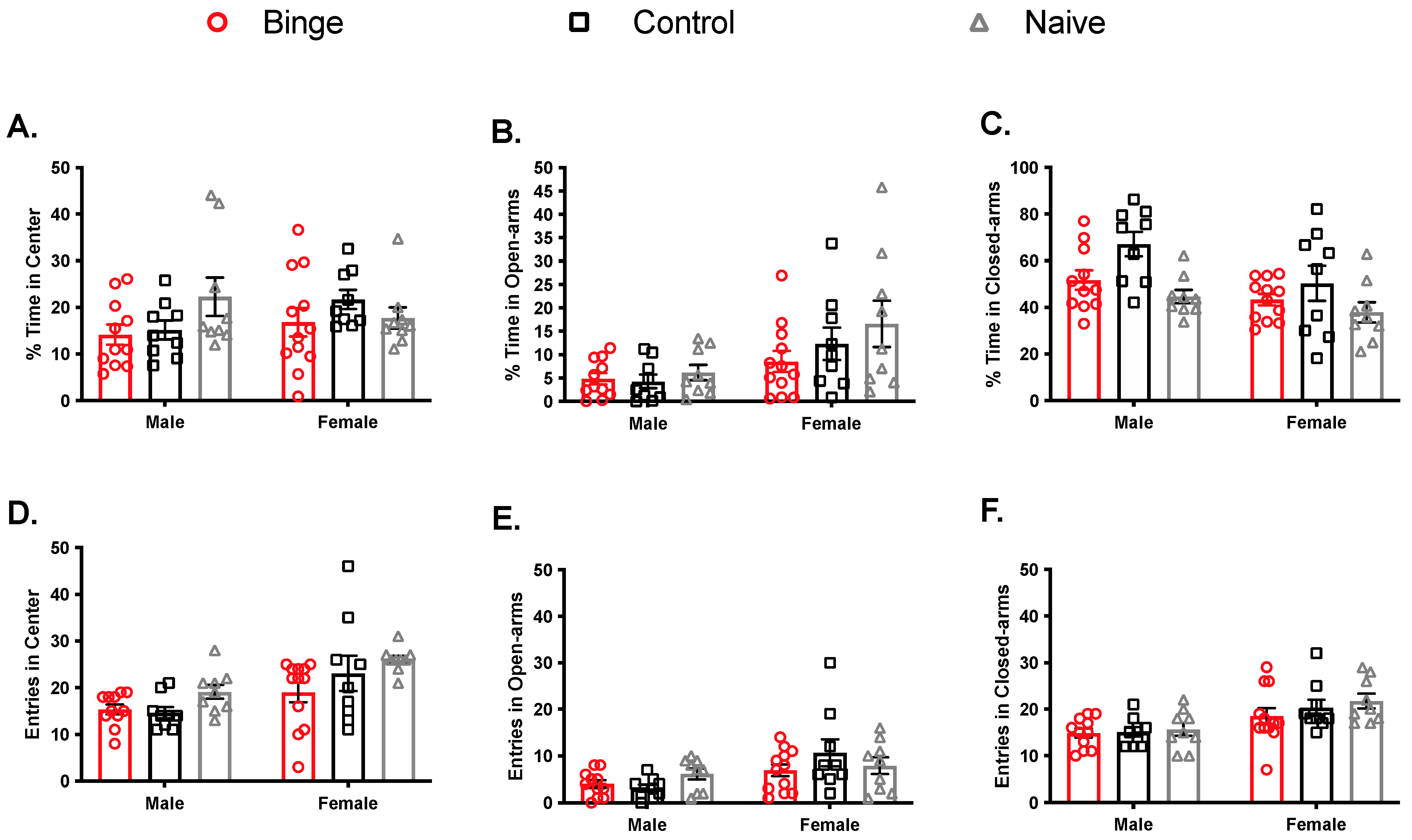
3.2.2. Effect of Multiple Binge on Locomotor Activity, Anxiety-Like Behavior, and Behavioral Despair
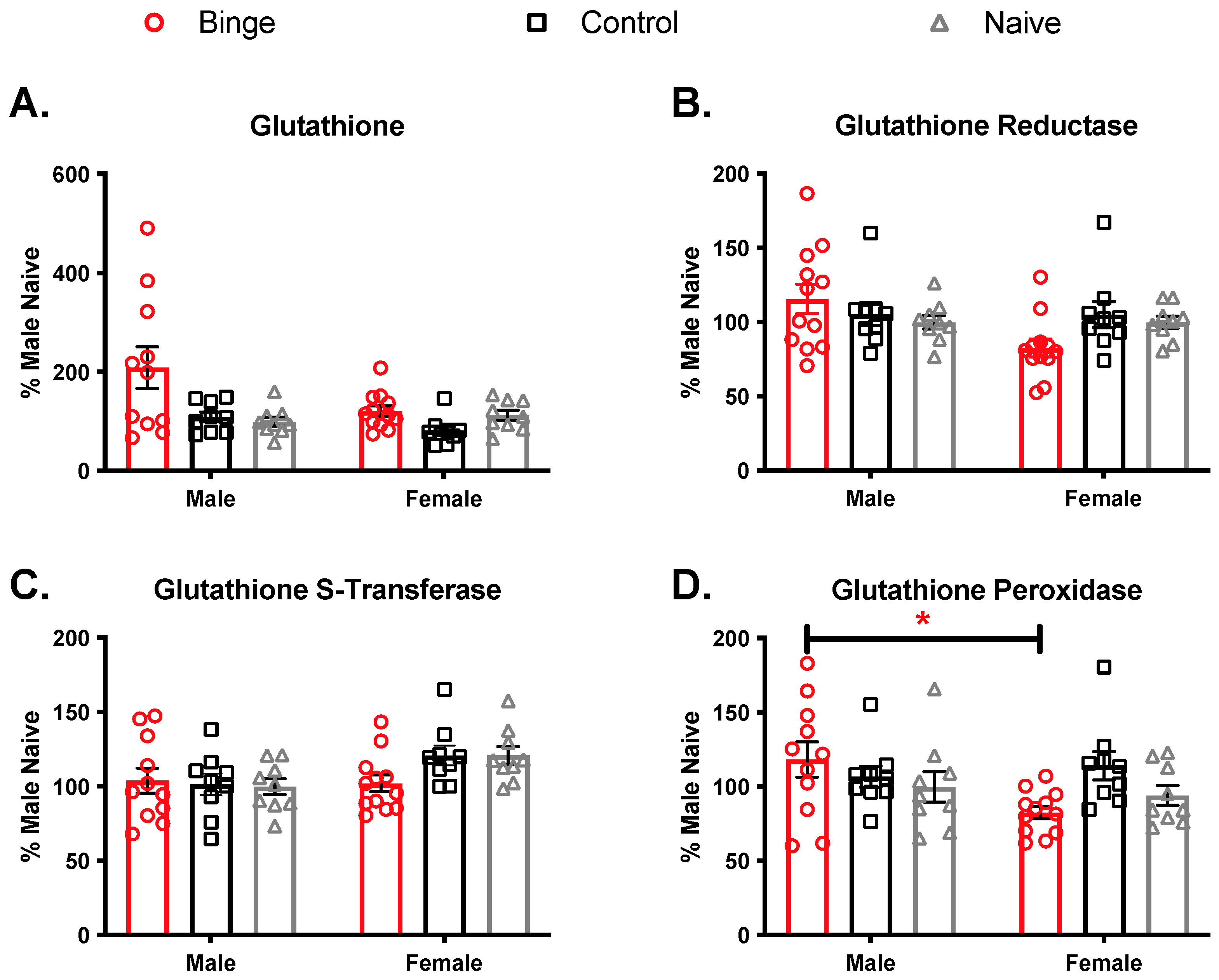
3.2.3. Effects of Repeated Binge on the Antioxidant Capacity of the Brain
3.2.4. Effects of Repeated Binge on Brain Levels of Oxidative Damage
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- NIAAA. Binge Drinking. 2021. Available online: https://www.niaaa.nih.gov/publications/brochures-and-fact-sheets/binge-drinking (accessed on 15 July 2021).
- NIAAA. Binge drinking defined. NIAAA Newsl. 2004, 3. [Google Scholar]
- Esser, M.B.; Hedden, S.L.; Kanny, D.; Brewer, R.D.; Gfroerer, J.C.; Naimi, T.S. Alcohol dependence among US adult drinkers, 2009–2011. Prev. Chronic Dis. 2014, 11, 140329. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Alcohol Use and Your Health. Available online: https://www.cdc.gov/alcohol/fact-sheets/alcohol-use.htm (accessed on 15 July 2021).
- Cortez, I.; Rodgers, S.P.; Kosten, T.A.; Leasure, J.L. Sex and Age Effects on Neurobehavioral Toxicity Induced by Binge Alcohol. Brain Plast. 2020, 6, 5–25. [Google Scholar] [CrossRef]
- Geisner, I.M.; Trager, B.M.; Hultgren, B.A.; Larimer, M.E.; Mallett, K.A.; Turrisi, R. Examining parental monitoring as a moderator of the relationship between depressed mood and alcohol use and problems. Addict. Behav. 2018, 81, 117–124. [Google Scholar] [CrossRef]
- Peltier, M.R.; Verplaetse, T.L.; Mineur, Y.S.; Petrakis, I.L.; Cosgrove, K.P.; Picciotto, M.R.; McKee, S.A. Sex differences in stress-related alcohol use. Neurobiol. Stress 2019, 10, 100149. [Google Scholar] [CrossRef]
- Adan, A.; Navarro, J.F.; Forero, D.A. Personality profile of binge drinking in university students is modulated by sex. A study using the Alternative Five Factor Model. Drug Alcohol Depend. 2016, 165, 120–125. [Google Scholar] [CrossRef] [PubMed]
- Keyes, K.M.; Jager, J.; Mal-Sarkar, T.; Patrick, M.E.; Rutherford, C.; Hasin, D. Is There a Recent Epidemic of Women’s Drinking? A Critical Review of National Studies. Alcohol. Clin. Exp. Res. 2019, 43, 1344–1359. [Google Scholar] [CrossRef]
- Squeglia, L.M.; Schweinsburg, A.D.; Pulido, C.; Tapert, S.F. Adolescent binge drinking linked to abnormal spatial working memory brain activation: Differential gender effects. Alcohol. Clin. Exp. Res. 2011, 35, 1831–1841. [Google Scholar] [CrossRef]
- Squeglia, L.M.; Sorg, S.F.; Schweinsburg, A.D.; Wetherill, R.R.; Pulido, C.; Tapert, S.F. Binge drinking differentially affects adolescent male and female brain morphometry. Psychopharmacology 2012, 220, 529–539. [Google Scholar] [CrossRef] [PubMed]
- Caldwell, L.C.; Schweinsburg, A.D.; Nagel, B.J.; Barlett, V.C.; Brown, S.A.; Tapert, S.F. Gender and adolescent alcohol use disorders on BOLD (blood oxygen level dependent) response to spatial working memory. Alcohol Alcohol. 2005, 40, 194–200. [Google Scholar] [CrossRef]
- Hoppenbrouwers, S.S.; Hofman, D.; Schutter, D.J. Alcohol breaks down interhemispheric inhibition in females but not in males: Alcohol and frontal connectivity. Psychopharmacology 2010, 208, 469–474. [Google Scholar] [CrossRef] [PubMed]
- Ide, J.S.; Zhang, S.; Hu, S.; Matuskey, D.; Bednarski, S.R.; Erdman, E.; Farr, O.M.; Li, C.S. Gray matter volume correlates of global positive alcohol expectancy in non-dependent adult drinkers. Addict. Biol. 2014, 19, 895–906. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ide, J.S.; Zhornitsky, S.; Hu, S.; Zhang, S.; Krystal, J.H.; Li, C.R. Sex differences in the interacting roles of impulsivity and positive alcohol expectancy in problem drinking: A structural brain imaging study. Neuroimage Clin. 2017, 14, 750–759. [Google Scholar] [CrossRef] [PubMed]
- Pfefferbaum, A.; Rosenbloom, M.; Rohlfing, T.; Sullivan, E.V. Degradation of association and projection white matter systems in alcoholism detected with quantitative fiber tracking. Biol. Psychiatry 2009, 65, 680–690. [Google Scholar] [CrossRef]
- Alfonso-Loeches, S.; Pascual, M.; Guerri, C. Gender differences in alcohol-induced neurotoxicity and brain damage. Toxicology 2013, 311, 27–34. [Google Scholar] [CrossRef]
- Jung, M.E.; Metzger, D.B. A sex difference in oxidative stress and behavioral suppression induced by ethanol withdrawal in rats. Behav. Brain Res. 2016, 314, 199–214. [Google Scholar] [CrossRef]
- Wu, D.; Cederbaum, A.I. Alcohol, oxidative stress, and free radical damage. Alcohol Res. Health J. Natl. Inst. Alcohol Abuse Alcohol. 2003, 27, 277–284. [Google Scholar]
- Jung, M.E.; Metzger, D.B. Alcohol withdrawal and brain injuries: Beyond classical mechanisms. Molecules 2010, 15, 4984–5011. [Google Scholar] [CrossRef] [PubMed]
- Hernandez, J.A.; Lopez-Sanchez, R.C.; Rendon-Ramirez, A. Lipids and Oxidative Stress Associated with Ethanol-Induced Neurological Damage. Oxid. Med. Cell Longev. 2016, 2016, 1543809. [Google Scholar] [CrossRef]
- Floyd, R.A. Neuroinflammatory processes are important in neurodegenerative diseases: An hypothesis to explain the increased formation of reactive oxygen and nitrogen species as major factors involved in neurodegenerative disease development. Free Radic. Biol. Med. 1999, 26, 1346–1355. [Google Scholar] [CrossRef]
- Floyd, R.A.; Carney, J.M. Free radical damage to protein and DNA: Mechanisms involved and relevant observations on brain undergoing oxidative stress. Ann. Neurol. 1992, 32, S22–S27. [Google Scholar] [CrossRef] [PubMed]
- Halliwell, B. Oxidative stress and neurodegeneration: Where are we now? J. Neurochem. 2006, 97, 1634–1658. [Google Scholar] [CrossRef] [PubMed]
- Krohne-Ehrich, G.; Schirmer, R.H.; Untucht-Grau, R. Glutathione reductase from human erythrocytes. Isolation of the enzyme and sequence analysis of the redox-active peptide. Eur. J. Biochem. 1977, 80, 65–71. [Google Scholar] [CrossRef] [PubMed]
- Jakoby, W.B. The glutathione S-transferases: A group of multifunctional detoxification proteins. Adv. Enzymol. Relat. Areas Mol. Biol. 1978, 46, 383–414. [Google Scholar] [CrossRef] [PubMed]
- Brocardo, P.S.; Gil-Mohapel, J.; Wortman, R.; Noonan, A.; McGinnis, E.; Patten, A.R.; Christie, B.R. The Effects of Ethanol Exposure During Distinct Periods of Brain Development on Oxidative Stress in the Adult Rat Brain. Alcohol. Clin. Exp. Res. 2017, 41, 26–37. [Google Scholar] [CrossRef] [PubMed]
- Maes, M.; Galecki, P.; Chang, Y.S.; Berk, M. A review on the oxidative and nitrosative stress (O&NS) pathways in major depression and their possible contribution to the (neuro)degenerative processes in that illness. Prog. Neuropsychopharmacol. Biol. Psychiatry 2011, 35, 676–692. [Google Scholar] [CrossRef]
- Crews, F.T.; Nixon, K. Mechanisms of neurodegeneration and regeneration in alcoholism. Alcohol Alcohol. 2009, 44, 115–127. [Google Scholar] [CrossRef]
- Balmus, I.M.; Ciobica, A.; Antioch, I.; Dobrin, R.; Timofte, D. Oxidative Stress Implications in the Affective Disorders: Main Biomarkers, Animal Models Relevance, Genetic Perspectives, and Antioxidant Approaches. Oxid. Med. Cell Longev. 2016, 2016, 3975101. [Google Scholar] [CrossRef] [PubMed]
- Liu, T.; Zhong, S.; Liao, X.; Chen, J.; He, T.; Lai, S.; Jia, Y. A Meta-Analysis of Oxidative Stress Markers in Depression. PLoS ONE 2015, 10, e0138904. [Google Scholar] [CrossRef] [PubMed]
- Michel, T.M.; Frangou, S.; Thiemeyer, D.; Camara, S.; Jecel, J.; Nara, K.; Brunklaus, A.; Zoechling, R.; Riederer, P. Evidence for oxidative stress in the frontal cortex in patients with recurrent depressive disorder—A postmortem study. Psychiatry Res. 2007, 151, 145–150. [Google Scholar] [CrossRef]
- Tsuboi, H.; Tatsumi, A.; Yamamoto, K.; Kobayashi, F.; Shimoi, K.; Kinae, N. Possible connections among job stress, depressive symptoms, lipid modulation and antioxidants. J. Affect. Disord. 2006, 91, 63–70. [Google Scholar] [CrossRef]
- Hovatta, I.; Juhila, J.; Donner, J. Oxidative stress in anxiety and comorbid disorders. Neurosci. Res. 2010, 68, 261–275. [Google Scholar] [CrossRef] [PubMed]
- Hovatta, I.; Tennant, R.S.; Helton, R.; Marr, R.A.; Singer, O.; Redwine, J.M.; Ellison, J.A.; Schadt, E.E.; Verma, I.M.; Lockhart, D.J.; et al. Glyoxalase 1 and glutathione reductase 1 regulate anxiety in mice. Nature 2005, 438, 662–666. [Google Scholar] [CrossRef] [PubMed]
- Salim, S.; Asghar, M.; Taneja, M.; Hovatta, I.; Chugh, G.; Vollert, C.; Vu, A. Potential contribution of oxidative stress and inflammation to anxiety and hypertension. Brain Res. 2011, 1404, 63–71. [Google Scholar] [CrossRef]
- Tenkorang, M.A.; Snyder, B.; Cunningham, R.L. Sex-related differences in oxidative stress and neurodegeneration. Steroids 2018, 133, 21–27. [Google Scholar] [CrossRef]
- Bilici, M.; Efe, H.; Koroglu, M.A.; Uydu, H.A.; Bekaroglu, M.; Deger, O. Antioxidative enzyme activities and lipid peroxidation in major depression: Alterations by antidepressant treatments. J. Affect. Disord. 2001, 64, 43–51. [Google Scholar] [CrossRef]
- Ozcan, M.E.; Gulec, M.; Ozerol, E.; Polat, R.; Akyol, O. Antioxidant enzyme activities and oxidative stress in affective disorders. Int. Clin. Psychopharmacol. 2004, 19, 89–95. [Google Scholar] [CrossRef]
- Krieger, H.; Young, C.M.; Anthenien, A.M.; Neighbors, C. The Epidemiology of Binge Drinking Among College-Age Individuals in the United States. Alcohol Res. 2018, 39, 23–30. [Google Scholar]
- West, R.K.; Rodgers, S.P.; Leasure, J.L. Neural Perturbations Associated With Recurrent Binge Alcohol in Male and Female Rats. Alcohol. Clin. Exp. Res. 2021, 45, 365–374. [Google Scholar] [CrossRef]
- Walf, A.A.; Frye, C.A. The use of the elevated plus maze as an assay of anxiety-related behavior in rodents. Nat. Protoc. 2007, 2, 322–328. [Google Scholar] [CrossRef]
- Paljarvi, T.; Koskenvuo, M.; Poikolainen, K.; Kauhanen, J.; Sillanmaki, L.; Makela, P. Binge drinking and depressive symptoms: A 5-year population-based cohort study. Addiction 2009, 104, 1168–1178. [Google Scholar] [CrossRef] [PubMed]
- Choi, N.G.; Dinitto, D.M. Heavy/binge drinking and depressive symptoms in older adults: Gender differences. Int. J. Geriatr. Psychiatry 2011, 26, 860–868. [Google Scholar] [CrossRef] [PubMed]
- Briere, F.N.; Rohde, P.; Seeley, J.R.; Klein, D.; Lewinsohn, P.M. Comorbidity between major depression and alcohol use disorder from adolescence to adulthood. Compr. Psychiatry 2014, 55, 526–533. [Google Scholar] [CrossRef] [PubMed]
- Pettinati, H.M.; Oslin, D.W.; Kampman, K.M.; Dundon, W.D.; Xie, H.; Gallis, T.L.; Dackis, C.A.; O’Brien, C.P. A double-blind, placebo-controlled trial combining sertraline and naltrexone for treating co-occurring depression and alcohol dependence. The Am. J. Psychiatry 2010, 167, 668–675. [Google Scholar] [CrossRef] [PubMed]
- Castagne, V.; Moser, P.; Roux, S.; Porsolt, R.D. Rodent models of depression: Forced swim and tail suspension behavioral despair tests in rats and mice. Curr. Protoc. Neurosci. 2011, 8, Unit 8.10A. [Google Scholar] [CrossRef]
- Porsolt, R.D.; Anton, G.; Blavet, N.; Jalfre, M. Behavioural despair in rats: A new model sensitive to antidepressant treatments. Eur. J. Pharmacol. 1978, 47, 379–391. [Google Scholar] [CrossRef]
- Borsini, F.; Meli, A. Is the forced swimming test a suitable model for revealing antidepressant activity? Psychopharmacology 1988, 94, 147–160. [Google Scholar] [CrossRef]
- Akerboom, T.P.; Sies, H. Assay of glutathione, glutathione disulfide, and glutathione mixed disulfides in biological samples. Methods Enzymol. 1981, 77, 373–382. [Google Scholar] [CrossRef]
- Tietze, F. Enzymic method for quantitative determination of nanogram amounts of total and oxidized glutathione: Applications to mammalian blood and other tissues. Anal. Biochem. 1969, 27, 502–522. [Google Scholar] [CrossRef]
- Wendel, A. Glutathione peroxidase. Methods Enzymol. 1981, 77, 325–333. [Google Scholar] [CrossRef]
- Carlberg, I.; Mannervik, B. Glutathione reductase. Methods Enzymol. 1985, 113, 484–490. [Google Scholar] [CrossRef]
- Habig, W.H.; Jakoby, W.B. Assays for differentiation of glutathione S-transferases. Methods Enzymol. 1981, 77, 398–405. [Google Scholar] [CrossRef] [PubMed]
- Xiang, X.; Huang, W.; Haile, C.N.; Kosten, T.A. Hippocampal GluR1 associates with behavior in the elevated plus maze and shows sex differences. Behav. Brain Res. 2011, 222, 326–331. [Google Scholar] [CrossRef]
- Hare, B.D.; Duman, R.S. Prefrontal cortex circuits in depression and anxiety: Contribution of discrete neuronal populations and target regions. Mol. Psychiatry 2020, 25, 2742–2758. [Google Scholar] [CrossRef]
- Lovinger, D.M.; Alvarez, V.A. Alcohol and basal ganglia circuitry: Animal models. Neuropharmacology 2017, 122, 46–55. [Google Scholar] [CrossRef]
- Shukla, V.; Mishra, S.K.; Pant, H.C. Oxidative stress in neurodegeneration. Adv. Pharmacol. Sci. 2011, 2011, 572634. [Google Scholar] [CrossRef]
- Maas, D.A.; Eijsink, V.D.; van Hulten, J.A.; Panic, R.; De Weerd, P.; Homberg, J.R.; Valles, A.; Nait-Oumesmar, B.; Martens, G.J.M. Antioxidant treatment ameliorates prefrontal hypomyelination and cognitive deficits in a rat model of schizophrenia. Neuropsychopharmacology 2021, 46, 1161–1171. [Google Scholar] [CrossRef] [PubMed]
- Nascimento, C.P.; Luz, D.A.; da Silva, C.C.S.; Malcher, C.M.R.; Fernandes, L.M.P.; Dalla Santa, H.S.; Gomes, A.R.Q.; Monteiro, M.C.; Ribeiro, C.; Fontes-Junior, E.A.; et al. Ganoderma lucidum Ameliorates Neurobehavioral Changes and Oxidative Stress Induced by Ethanol Binge Drinking. Oxid. Med. Cell Longev. 2020, 2020, 2497845. [Google Scholar] [CrossRef] [PubMed]
- Uysal, M.; Kutalp, G.; Ozdemirler, G.; Aykac, G. Ethanol-induced changes in lipid peroxidation and glutathione content in rat brain. Drug Alcohol Depend. 1989, 23, 227–230. [Google Scholar] [CrossRef]
- Rendon-Ramirez, A.; Cortes-Couto, M.; Martinez-Rizo, A.B.; Muniz-Hernandez, S.; Velazquez-Fernandez, J.B. Oxidative damage in young alcohol drinkers: A preliminary study. Alcohol 2013, 47, 501–504. [Google Scholar] [CrossRef]
- Haorah, J.; Ramirez, S.H.; Floreani, N.; Gorantla, S.; Morsey, B.; Persidsky, Y. Mechanism of alcohol-induced oxidative stress and neuronal injury. Free Radic. Biol. Med. 2008, 45, 1542–1550. [Google Scholar] [CrossRef]
- Liu, W.; Kato, M.; Akhand, A.A.; Hayakawa, A.; Suzuki, H.; Miyata, T.; Kurokawa, K.; Hotta, Y.; Ishikawa, N.; Nakashima, I. 4-hydroxynonenal induces a cellular redox status-related activation of the caspase cascade for apoptotic cell death. J. Cell Sci. 2000, 113 Pt 4, 635–641. [Google Scholar] [CrossRef]
- Nakamura-Palacios, E.M.; Souza, R.S.; Zago-Gomes, M.P.; de Melo, A.M.; Braga, F.S.; Kubo, T.T.; Gasparetto, E.L. Gray matter volume in left rostral middle frontal and left cerebellar cortices predicts frontal executive performance in alcoholic subjects. Alcohol. Clin. Exp. Res. 2014, 38, 1126–1133. [Google Scholar] [CrossRef] [PubMed]
- Crews, F.T.; Boettiger, C.A. Impulsivity, frontal lobes and risk for addiction. Pharmacol. Biochem. Behav. 2009, 93, 237–247. [Google Scholar] [CrossRef]
- Luo, L.; Min, X.L.; He, X.; Shang, F.F. Broad and dynamic neurochemical alterations in the brain of alcoholic rats. J. Integr. Neurosci. 2021, 20, 33–41. [Google Scholar] [CrossRef]
- Shiwalkar, N.; Zuo, W.; Bekker, A. The Role of the Lateral Habenula Circuitries in Alcohol Use Disorders. In Neuroscience of Alcohol; Preedy, V.R., Ed.; Academic Press: Cambridge, MA, USA, 2019; pp. 153–161. [Google Scholar]
- Shah, A.; Zuo, W.; Kang, S.; Li, J.; Fu, R.; Zhang, H.; Bekker, A.; Ye, J.H. The lateral habenula and alcohol: Role of glutamate and M-type potassium channels. Pharmacol. Biochem. Behav. 2017, 162, 94–102. [Google Scholar] [CrossRef]
- Glover, E.J.; Starr, E.M.; Chao, Y.; Jhou, T.C.; Chandler, L.J. Inhibition of the rostromedial tegmental nucleus reverses alcohol withdrawal-induced anxiety-like behavior. Neuropsychopharmacology 2019, 44, 1896–1905. [Google Scholar] [CrossRef]
- Lushchak, V.I. Glutathione homeostasis and functions: Potential targets for medical interventions. J. Amino Acids 2012, 2012, 736837. [Google Scholar] [CrossRef]
- Anjum, I.; Jaffery, S.S.; Fayyaz, M.; Wajid, A.; Ans, A.H. Sugar Beverages and Dietary Sodas Impact on Brain Health: A Mini Literature Review. Cureus 2018, 10, e2756. [Google Scholar] [CrossRef]
- Kanny, D.; Naimi, T.S.; Liu, Y.; Lu, H.; Brewer, R.D. Annual Total Binge Drinks Consumed by U.S. Adults, 2015. Am. J. Prev. Med. 2018, 54, 486–496. [Google Scholar] [CrossRef] [PubMed]
- Crews, F.T.; Collins, M.A.; Dlugos, C.; Littleton, J.; Wilkins, L.; Neafsey, E.J.; Pentney, R.; Snell, L.D.; Tabakoff, B.; Zou, J.; et al. Alcohol-induced neurodegeneration: When, where and why? Alcohol. Clin. Exp. Res. 2004, 28, 350–364. [Google Scholar] [CrossRef]
- Ogilvie, K.M.; Rivier, C. Gender difference in hypothalamic-pituitary-adrenal axis response to alcohol in the rat: Activational role of gonadal steroids. Brain Res. 1997, 766, 19–28. [Google Scholar] [CrossRef]

| BEC (mg/dL) | Binge 1 | Binge 2 | Binge 3 | Binge 4 |
| male | 199.6 ± 5.2 | 141.7 ± 17.9 | 172.0 ± 8.4 | 162.4 ± 18.2 |
| female | 198.1 ± 17.4 | 157.8 ± 5.7 | 151.2 ± 14.1 | 228.1 ± 13.2 |
| Corticosterone (ng/mL) | Binge | Control | Naive | |
| male | 70.3 ± 7.8 | 75.7 ± 7.6 | 54.5 ± 15.2 | |
| female | 95.7 ± 20.3 | 58.1 ± 6.6 | 49.3 ± 5.8 |
| TBARS | PFC | Hippocampus | Striatum | |||
|---|---|---|---|---|---|---|
| Binge | Control | Binge | Control | Binge | Control | |
| Male Female | 138.3 ± 27.3 119.7 ± 17.2 | 107.2 ± 22.1 108.6 ± 22.0 | 121.9 ± 9.4 106.6 ± 9.8 | 152.0 ± 30.1 93.3 + 15.3 | 73.3 ± 14.4 47.7 + 10.1 | 83.8 ± 13.3 64.1 ± 12.2 |
| Protein Carbonyls Male Female | 103.7 ± 8.8 117.0 ± 7.2 | 86.2 ± 8.8 107.4 ± 7.5 | 111.3 ± 8.9 104.3 ± 6.4 | 113.3 ± 3.4 111.6 ± 6.0 | 106.81 ± 5.1 91.0 ± 7.9 | 100.3 ± 6.5 90.6 ± 6.0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cortez, I.; Brocardo, P.S.; Leasure, J.L. Changes in Affective Behavior and Oxidative Stress after Binge Alcohol in Male and Female Rats. Brain Sci. 2021, 11, 1250. https://doi.org/10.3390/brainsci11091250
Cortez I, Brocardo PS, Leasure JL. Changes in Affective Behavior and Oxidative Stress after Binge Alcohol in Male and Female Rats. Brain Sciences. 2021; 11(9):1250. https://doi.org/10.3390/brainsci11091250
Chicago/Turabian StyleCortez, Ibanelo, Patricia S. Brocardo, and J. Leigh Leasure. 2021. "Changes in Affective Behavior and Oxidative Stress after Binge Alcohol in Male and Female Rats" Brain Sciences 11, no. 9: 1250. https://doi.org/10.3390/brainsci11091250
APA StyleCortez, I., Brocardo, P. S., & Leasure, J. L. (2021). Changes in Affective Behavior and Oxidative Stress after Binge Alcohol in Male and Female Rats. Brain Sciences, 11(9), 1250. https://doi.org/10.3390/brainsci11091250





