Effects of Acupuncture-Related Therapies in the Rehabilitation of Patients with Post-Stroke Aphasia—A Network Meta-Analysis of Randomized Controlled Trials
Abstract
:1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Inclusion Criteria
2.3. Exclusion Criteria
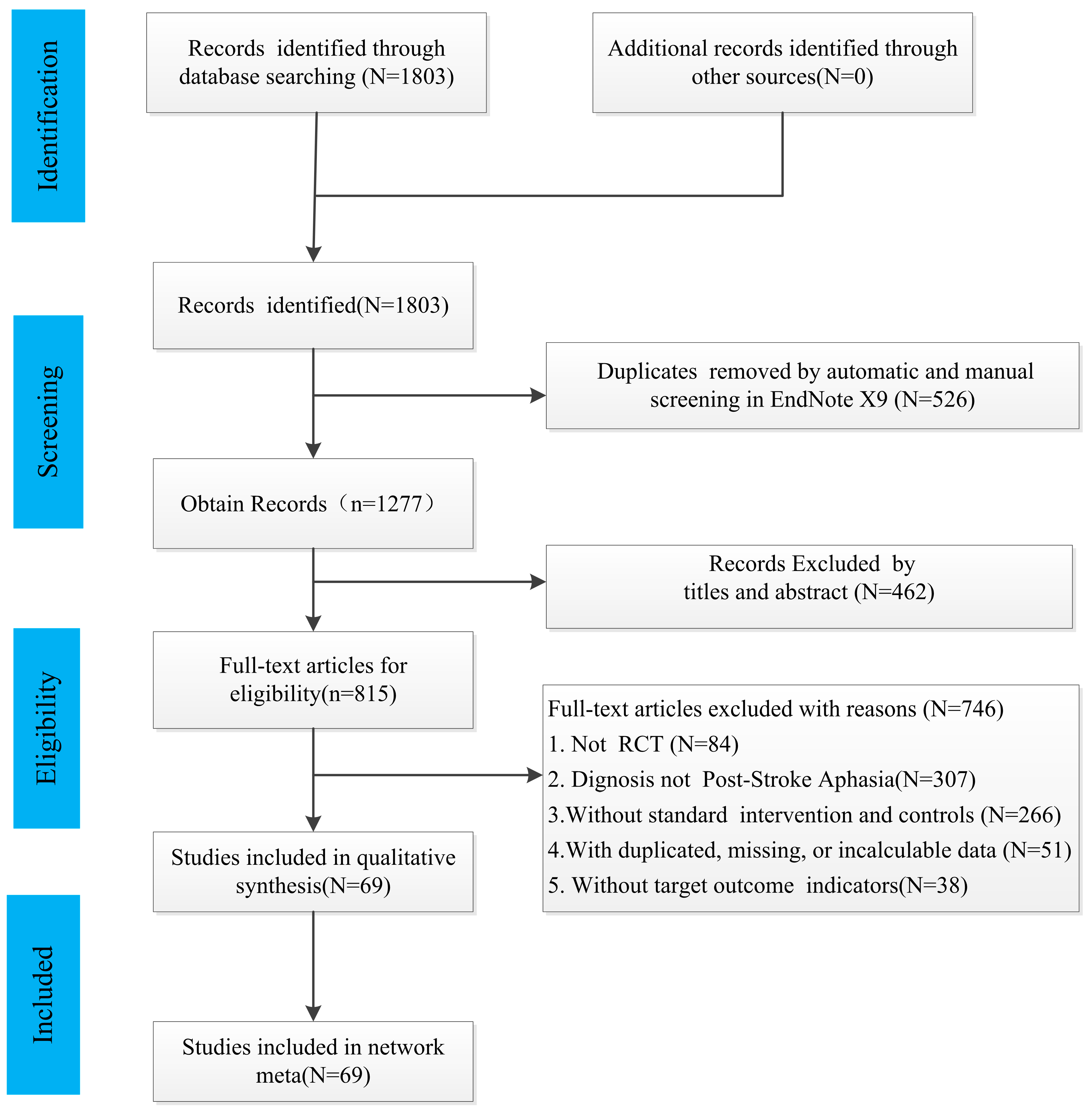
2.4. Study Selection
2.5. Data Extraction
2.6. Assessment of the Risk of Bias
2.7. Statistical Analysis
3. Results
3.1. Results of Study Identification and Selection
3.2. Characteristics of the Included Studies
3.3. Quality Assessment of the Included Studies
3.4. Results of Network Meta-Analysis
3.4.1. Evidence Network Diagram
3.4.2. Results of Total Effective Rate

3.4.3. Results of the Comprehension Score

3.4.4. Results of the Oral Expression Score

3.4.5. Results of the Repetition Score

3.4.6. Results of the Denomination Score

3.5. Presence of Adverse Effects
3.6. Publication Bias and Consistency Assessment
4. Discussion
4.1. This Work
4.2. Strengths and Limitations
4.3. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- GBD 2016 Stroke Collaborators. Global, regional, and national burden of stroke, 1990−2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019, 18, 439–458. [Google Scholar] [CrossRef]
- Shah-Basak, P.P.; Sivaratnam, G.; Teti, S.; Francois-Nienaber, A.; Yossofzai, M.; Armstrong, S.; Nayar, S.; Jokel, R.; Meltzer, J. High definition transcranial direct current stimulation modulates abnormal neurophysiological activity in post-stroke aphasia. Sci. Rep. 2020, 10, 19625. [Google Scholar] [CrossRef] [PubMed]
- Stefaniak, J.D.; Halai, A.D.; Lambon, R.M. The neural and neurocomputational bases of recovery from post-stroke aphasia. Nat. Rev. Neurol. 2020, 16, 43–55. [Google Scholar] [CrossRef] [PubMed]
- Fridriksson, J.; Hillis, A.E. Current approaches to the treatment of post-stroke aphasia. J. Stroke 2021, 23, 183–201. [Google Scholar] [CrossRef]
- Picano, C.; Quadrini, A.; Pisano, F.; Marangolo, P. Adjunctive approaches to aphasia rehabilitation: A review on efficacy and safety. Brain Sci. 2021, 11, 41. [Google Scholar] [CrossRef] [PubMed]
- Saxena, S.; Hillis, A.E. An update on medications and noninvasive brain stimulation to augment language rehabilitation in post-stroke aphasia. Expert Rev. Neurother. 2017, 17, 1091–1107. [Google Scholar] [CrossRef]
- Bhogal, S.K.; Teasell, R.; Speechley, M. Intensity of aphasia therapy, impact on recovery. Stroke 2003, 34, 987–993. [Google Scholar] [CrossRef]
- Allen, L.; Mehta, S.; Mcclure, J.A.; Teasell, R. Therapeutic interventions for aphasia initiated more than six months post stroke: A review of the evidence. Top. Stroke Rehabil. 2012, 19, 523–535. [Google Scholar] [CrossRef]
- Breitenstein, C.; Grewe, T.; Floel, A.; Ziegler, W.; Springer, L.; Martus, P.; Huber, W.; Willmes, K.; Ringelstein, E.B.; Haeusler, K.G.; et al. Intensive speech and language therapy in patients with chronic aphasia after stroke: A randomised, open-label, blinded-endpoint, controlled trial in a health-care setting. Lancet 2017, 389, 1528–1538. [Google Scholar] [CrossRef]
- Lin, Q.; Lu, J.; Chen, Z.; Yan, J.; Wang, H.; Ouyang, H.; Mou, Z.; Huang, D.; O’Young, B. A survey of speech-language-hearing therapists’ career situation and challenges in mainland china. Folia Phoniatr. Logop. 2016, 68, 10–15. [Google Scholar] [CrossRef]
- Zumbansen, A.; Thiel, A. Recent advances in the treatment of post-stroke aphasia. Neural Regen. Res. 2014, 9, 703–706. [Google Scholar] [CrossRef] [PubMed]
- Cramer, S.C. Repairing the human brain after stroke. II. Restorative therapies. Ann. Neurol. 2008, 63, 549–560. [Google Scholar] [CrossRef] [PubMed]
- Berthier, M.L.; Pulvermuller, F. Neuroscience insights improve neurorehabilitation of poststroke aphasia. Nat. Rev. Neurol. 2011, 7, 86–97. [Google Scholar] [CrossRef]
- Small, S.L.; Llano, D.A. Biological approaches to aphasia treatment. Curr. Neurol. Neurosci. Rep. 2009, 9, 443–450. [Google Scholar] [CrossRef]
- Zhang, X.; Shu, B.; Zhang, D.; Huang, L.; Fu, Q.; Du, G. The efficacy and safety of pharmacological treatments for post-stroke aphasia. CNS Neurol. Disord. Drug Targets 2018, 17, 509–521. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Wei, R.; Chen, Z.; Luo, B. Piracetam for aphasia in post-stroke patients: A systematic review and meta-analysis of randomized controlled trials. CNS Drugs 2016, 30, 575–587. [Google Scholar] [CrossRef] [PubMed]
- Gungor, L.; Terzi, M.; Onar, M.K. Does long term use of piracetam improve speech disturbances due to ischemic cerebrovascular diseases? Brain Lang. 2011, 117, 23–27. [Google Scholar] [CrossRef]
- Gill, S.K.; Leff, A.P. Dopaminergic therapy in aphasia. Aphasiology 2012, 28, 155–170. [Google Scholar] [CrossRef]
- Breitenstein, C.; Korsukewitz, C.; Baumgartner, A.; Floel, A.; Zwitserlood, P.; Dobel, C.; Knecht, S. L-dopa does not add to the success of high-intensity language training in aphasia. Restor. Neurol. Neurosci. 2015, 33, 115–120. [Google Scholar] [CrossRef]
- Ashtary, F.; Janghorbani, M.; Chitsaz, A.; Reisi, M.; Bahrami, A. A randomized, double-blind trial of bromocriptine efficacy in nonfluent aphasia after stroke. Neurology 2006, 66, 914–916. [Google Scholar] [CrossRef]
- Whiting, E.; Chenery, H.J.; Chalk, J.; Copland, D.A. Dexamphetamine boosts naming treatment effects in chronic aphasia. J. Int. Neuropsychol. Soc. 2007, 13, 972–979. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Yang, J.W.; Lin, L.T.; Huang, J.; Wang, X.R.; Su, X.T.; Cao, Y.; Fisher, M.; Liu, C.Z. Acupuncture attenuates inflammation in microglia of vascular dementia rats by inhibiting mir-93-mediated tlr4/myd88/nf-kappab signaling pathway. Oxid. Med. Cell. Longev. 2020, 2020, 8253904. [Google Scholar] [CrossRef] [PubMed]
- He, X.K.; Liu, H.H.; Chen, S.J.; Sun, Q.Q.; Yu, G.; Lei, L.; Niu, Z.Y.; Chen, L.D.; Hsieh, T.H. Subsequent acupuncture reverses the aftereffects of intermittent theta-burst stimulation. Front. Neural Circuits 2021, 15, 675365. [Google Scholar] [CrossRef] [PubMed]
- Zhang, B.; Han, Y.; Huang, X.; Liu, Z.; Li, S.; Chang, J.; Gao, Y. Acupuncture is effective in improving functional communication in post-stroke aphasia: A systematic review and meta-analysis of randomized controlled trials. Wien. Klin. Wochenschr. 2019, 131, 221–232. [Google Scholar] [CrossRef]
- Zhang, Y.; Wang, Z.; Jiang, X.; Lv, Z.; Wang, L.; Lu, L. Effectiveness of acupuncture for poststroke aphasia: A systematic review and meta-analysis of randomized controlled trials. Complement. Med. Res. 2021, 28, 545–556. [Google Scholar] [CrossRef] [PubMed]
- Li, G.; Yang, E.S. An fmri study of acupuncture-induced brain activation of aphasia stroke patients. Complement. Ther. Med. 2011, 19 (Suppl. S1), S49–S59. [Google Scholar] [CrossRef] [PubMed]
- Lumley, T. Network meta-analysis for indirect treatment comparisons. Stat. Med. 2002, 21, 2313–2324. [Google Scholar] [CrossRef]
- Rouse, B.; Chaimani, A.; Li, T. Network meta-analysis: An introduction for clinicians. Intern. Emerg. Med. 2017, 12, 103–111. [Google Scholar] [CrossRef]
- Watt, J.; Tricco, A.C.; Straus, S.; Veroniki, A.A.; Naglie, G.; Drucker, A.M. Research techniques made simple: Network meta-analysis. J. Investig. Dermatol. 2019, 139, 4–12. [Google Scholar] [CrossRef]
- Zhang, X.; Cheng, B.; Zhang, Y. A hands-on tutorial for systematic review and meta-analysis with example data set and codes. J. Speech Lang. Hear. Res. 2022, 65, 3217–3238. [Google Scholar] [CrossRef]
- Phillips, M.R.; Steel, D.H.; Wykoff, C.C.; Busse, J.W.; Bannuru, R.R.; Thabane, L.; Bhandari, M.; Chaudhary, V. A clinician’s guide to network meta-analysis. Eye 2022, 36, 1523–1526. [Google Scholar] [CrossRef]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A. Preferred reporting items for systematic review and meta-analysis protocols (prisma-p) 2015 statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef] [PubMed]
- Gao, S.; Chu, Y.; Shi, S.; Peng, Y.; Dai, S.; Wang, Y.; Zhao, S.; Zhou, Y.; Rao, B.; Zeng, G.; et al. A standardization research of the aphasia battery of chinese. Chin. Ment. Health J. 1992, 6, 125–128. [Google Scholar] [CrossRef]
- Yuan, B.; Zhang, N.; Yan, J.; Cheng, J.; Lu, J.; Wu, J. Resting-state functional connectivity predicts individual language impairment of patients with left hemispheric gliomas involving language network. Neuroimage Clin. 2019, 24, 102023. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health of the People’s Republic of China. Guiding Principles for Clinical Study of New Chinese Medicines; China Medico-Pharmaceutical Science & Technology Publishing House: Beijing, China, 2002; pp. 99–104.
- Sterne, J.; Savovic, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. Rob 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef]
- Jackson, D.; Riley, R.; White, I.R. Multivariate meta-analysis: Potential and promise. Stat. Med. 2011, 30, 2481–2498. [Google Scholar] [CrossRef]
- Xu, C.; Niu, Y.; Wu, J.; Gu, H.; Zhang, C. Software and package applicating for network meta-analysis: A usage-based comparative study. J. Evid. Based Med. 2018, 11, 176–183. [Google Scholar] [CrossRef]
- Aziz, M.; Tan, L.E.; Wu, D.B.; Pearce, F.; Chua, G.; Lin, L.; Tan, P.T.; Ng, K. Comparative efficacy of inhaled medications (ics/laba, lama, lama/laba and sama) for copd: A systematic review and network meta-analysis. Int. J. Chron. Obstruc. Pulmon. Dis. 2018, 13, 3203–3231. [Google Scholar] [CrossRef]
- Greco, T.; Edefonti, V.; Biondi-Zoccai, G.; Decarli, A.; Gasparini, M.; Zangrillo, A.; Landoni, G. A multilevel approach to network meta-analysis within a frequentist framework. Contemp. Clin. Trials 2015, 42, 51–59. [Google Scholar] [CrossRef]
- Veroniki, A.A.; Vasiliadis, H.S.; Higgins, J.P.; Salanti, G. Evaluation of inconsistency in networks of interventions. Int. J. Epidemiol. 2013, 42, 332–345. [Google Scholar] [CrossRef] [Green Version]
- Guyot, P.; Ades, A.E.; Ouwens, M.J.; Welton, N.J. Enhanced secondary analysis of survival data: Reconstructing the data from published kaplan-meier survival curves. BMC Med. Res. Methodol. 2012, 12, 9. [Google Scholar] [CrossRef] [PubMed]
- Chaimani, A.; Higgins, J.P.; Mavridis, D.; Spyridonos, P.; Salanti, G. Graphical tools for network meta-analysis in stata. PLoS ONE 2013, 8, e76654. [Google Scholar] [CrossRef]
- Marotta, N.; Demeco, A.; Moggio, L.; Marinaro, C.; Pino, I.; Barletta, M.; Petraroli, A.; Pepe, D.; Lavano, F.; Ammendolia, A. Comparative effectiveness of breathing exercises in patients with chronic obstructive pulmonary disease. Complement. Ther. Clin. Pract. 2020, 41, 101260. [Google Scholar] [CrossRef]
- Hou, W.; Chang, D.; Yang, C.; Shi, G.; Zhou, L. Observation on clinical effect of scalp electroacupuncture on motor aphasia after stroke. J. Clin. Acupunct. Moxibustion 2012, 28, 29–31. [Google Scholar] [CrossRef]
- Liu, J.; Liu, Y.; Ma, Z.; Yang, Y.; Zheng, H. Clinical observation on 50 cases of aphasia after ischemic stroke treated by Jiaotong Xinshen acupuncture. Health Guide 2018, 123, 102. [Google Scholar] [CrossRef]
- Liu, J.; Liu, Y.; Ma, Z.; Yang, Y.; Zheng, H.; Liu, J.; Song, Z.; Li, H. Clinical observation on 36 cases of aphasia after stroke treated by acupuncture from the theory of lung and kindey. Chinese Baby 2018, 19, 46. [Google Scholar]
- Liu, J.; Song, Z.; Li, H.; Liu, J.; Liu, Y.; Ma, Z.; Yang, Y.; Zheng, H. Randomized controlled trial of jianpi-yangxin-tongluo acupuncture in treatment of motor aphasia after cerebral infarction due to qi deficiency and blood stasis. J. Chengdu Univ. Tradit. Chin. Med. 2018, 41, 44–47. [Google Scholar] [CrossRef]
- Wang, S.; Liang, X.; Huo, X. Clinical observation on 39 cases of post-stroke aphasia treated by acupuncture. J. Chengdu Univ. Tradit. Chin. Med. 2006, 29, 23–24. [Google Scholar] [CrossRef]
- Wu, H. Observations of the efficacy of acupuncture on apoplectic aphasia. China Health Ind. 2011, 8, 104. [Google Scholar] [CrossRef]
- Li, L.; Wang, Z.; Yi, R.; Ding, L.; Guo, C. Clinical observation on 30 aphasia patients after ischemic stroke treated by guan’s tongue acupuncture. Yunnan J. Tradit. Chin. Med. Mater. Med. 2019, 40, 38–41. [Google Scholar] [CrossRef]
- Li, Z.; Li, Y.; Fu, W. Observation on clinical effect of tongue acupuncture in the treatment of 32 post-stroke aphaisia patients. J. New Chin. Med. 2004, 36, 47–48. [Google Scholar] [CrossRef]
- Li, Z.; Fu, W. Treatment of anandia after apoplexy by tongue acupuncture therapy: A clinical observation of 46 cases. J. New Chin. Med. 2005, 37, 61–62. [Google Scholar] [CrossRef]
- Liu, X. Summary of 32 cases of poststroke speech disorder treated by acupuncture on the tip of the tongue. Hunan J. Tradit. Chin. Med. 2011, 27, 12–13. [Google Scholar] [CrossRef]
- Mi, J.; Zhu, X. Clinical observations on the treatment of 46 apoplectic aphasia patients by tongue acupuncture as a main method. Shanghai J. Acupunct. Moxibustion 2004, 23, 8–9. [Google Scholar] [CrossRef]
- Wang, P.; Huang, Y. Tongue acupuncture in the treatment of 30 cases of apoplectic aphasia. Jiangsu J. Tradit. Chin. Med. 1999, 20, 40. [Google Scholar]
- Jiang, G.; Li, X. Observations on the efficacy of jin’s tongue three needles in treating apoplectic motor aphasia. Shanghai J. Acupunct. Moxibustion 2008, 27, 5–6. [Google Scholar] [CrossRef]
- Li, L.; Huang, P.; Luan, S.; Xiao, X.; Fan, M.; Wang, Z.; Wang, J. Clinical study on the treatment of aphasia after ischemic stroke with guans’ tongue needle combined with seven points of sknll base. China J. Tradit. Chin. Med. Pharm. 2020, 35, 5851–5854. [Google Scholar]
- Li, X.; Cai, J.; Jiang, G. Observation on clinical effect of tongue triple acupuncture in the treatment of aphasia after stroke. J. Clin. Acupunct. Moxibustion 2009, 25, 6–8. [Google Scholar] [CrossRef]
- Wu, M.; Wan, T.; Hong, K.; Li, L.; Chen, L. Acupuncture combined with the bloodletting in pointes of jinjin and yuye in the treatment of 58 cases of aphasia after stroke. Fujian J. Tradit. Chin. Med. 2008, 39, 29–30. [Google Scholar] [CrossRef]
- Cheng, X.; Lai, J.; Wang, Z. Observation on the effect of speech training under acupuncture therapy on motor aphasia after stroke. Asia-Pac. Tradit. Med. 2018, 14, 153–154. [Google Scholar] [CrossRef]
- Dong, X.; Qin, L.; Fan, X.; Zhang, C. Influence of micro-needle intervention combined with rehabilitation training on language function of patients with aphasia after stroke. Liaoning J. Tradit. Chin. Med. 2020, 47, 153–156. [Google Scholar] [CrossRef]
- Huang, H. Effect of scalp acupuncture combined with speech therapy on ischemic stroke. Chin. J. Rehabil. Theory Pr. 2009, 15, 1180–1182. [Google Scholar] [CrossRef]
- Qiu, L.; Yu, Y.; Lu, J.; Lin, W.; Chen, L.; Liao, Y. Effects of acupuncture combined with response elaboration training on language efficacy of patients with chronic aphasia after stroke. China Med. Pharm. 2020, 10, 1–4. [Google Scholar] [CrossRef]
- Song, Z.; Zheng, H.; Liu, Y.; Ma, Z.; Yang, Y.; Liu, J.; Liu, J.; Li, H. Clinical study on treatment of aphasia after ischemic stroke by electroacupuncturing nonverbal eight points in shenying jing. J. Sichuan Tradit. Chin. Med. 2019, 37, 177–179. [Google Scholar]
- Wang, W.; Yang, S.; Li, J. Effects of joined puncture on head points combined with rehabilitation technique on motor aphasia. J. Clin. Acupunct. Moxibustion 2009, 25, 30–31. [Google Scholar] [CrossRef]
- Wang, Y. Effect of scalp acupuncture combined with speech rehabilitation in patients with motor aphasia after stroke. World Latest Med. Inf. 2021, 21, 106–107. [Google Scholar] [CrossRef]
- Zhang, R.; Sun, S. Treatment of motor aphasia after stroke with scalp acupuncture and speech rehabilitation. J. Chang. Univ. Tradit. Chin. Med. 2020, 36, 339–342. [Google Scholar] [CrossRef]
- Zhang, Y. Effect of scalp acupuncture on the recovery of language function in patients with aphasia after stroke. Healthmust-Readmagazine 2020, 28, 279. [Google Scholar]
- Li, S. Observation on the curative effect of tongue three-needle, temporal three-needle combined with language rehabilitation training in the treatment of post-stroke language disorder. Chin. J. Clin. Ration. Drug Use 2014, 7, 135–136. [Google Scholar] [CrossRef]
- Tong, X. Clinical outcomes of the application of temporal three needling and tongue three needling combined with language rehabilitation training in treating aphasia after stroke. Chin. Sci. J. Hear. Speech Rehabil. 2017, 15, 107–110. [Google Scholar] [CrossRef]
- Wang, M. Clinical study of scalp acupuncture and tongue acupuncture combined with language rehabilitation training in the intervention of aphasia after acute stroke. J. Bethune Mil. Med. Coll. 2016, 14, 740–741. [Google Scholar] [CrossRef]
- Wen, Z. Clinical study of temporal three needling and tongue three needling combined with language rehabilitation training in post-stroke aphaisa. Healthmust-Readmagaz. 2019, 27, 191. [Google Scholar]
- Zhang, H. Effect of tongue three needles and temporal three needles combined with speech training on aphasia after intracerebral hemorrhage. Chin. Med. Mod. Distance Educ. China 2022, 20, 126–128. [Google Scholar] [CrossRef]
- Chen, X.; Wang, Y.; Wang, G.; Huang, Y. Observation on the curative effect of “Xingnao Kaiqiao” acupuncture combined with speech training in the treatment of post-stroke aphasia. Chin. J. Integr. Med. Cardio/Cerebrovasc. Dis. 2021, 19, 1194–1196. [Google Scholar] [CrossRef]
- Dong, Y.; Liu, G.; Wang, T. The treatment of 30 cases of post-stroke aphasia patients with “Tongdu Kaiyin” acupuncture. J. Anhui Univ. Chin. Med. 2009, 28, 34–36. [Google Scholar] [CrossRef]
- He, J. Analysis of the curative effect of acupuncture combined with schuell’s stimulation therapy in the treatment of aphasia after stroke. J. Pract. Tradit. Chin. Med. 2021, 37, 2103–2105. [Google Scholar]
- Huang, S.; Huang, K. Effect of acupuncture with speech training on speech function recovery of aphasia patients after stroke. World Chin. Med. 2016, 11, 1074–1076. [Google Scholar] [CrossRef]
- Li, G.; Zhao, X. Clinical observations on treatment of apoplectic aphasia by acupuncture plus rehabilitation. Shanghai J. Acupunct. Moxibustion 2006, 25, 13–14. [Google Scholar] [CrossRef]
- Liu, L.; Guo, R.; Pang, S.; Li, X.; Dai, S.; Li, X.; Su, L.; Sun, W.; Zhang, G. Clinical study on acupuncture combined with language training in the treatment of aphasia in the early stage of stroke. Chin. Arch. Tradit. Chin. Med. 2006, 24, 2256–2259. [Google Scholar] [CrossRef]
- Luo, W.; Tan, J.; Huang, H. Clinical observation on treatment of cerebral infarction-induced broca aphasia by tiaoshen fuyin acupuncture therapy combined with language training. Chin. Acupunct. Moxibustion 2008, 28, 171–175. [Google Scholar] [CrossRef]
- Qin, L. Effect analysis of acupuncture combined with speech training in the treatment of speech impairment after cerebral infarction. Diet Health 2018, 5, 117–118. [Google Scholar] [CrossRef]
- Shi, L.; Huang, H. Clinical effect of acupuncture on aphasia after stroke. Shenzhen J. Integr. Tradit. Chin. West. Med. 2021, 31, 78–79. [Google Scholar] [CrossRef]
- Tian, H. Clinical observation of acupuncture combined with language training on 58 cases of stroke aphasia. China Med. Eng. 2012, 20, 169. [Google Scholar]
- Wei, J.; Jiang, T.; Xu, M.; Li, J.; Hong, Y. Effects of acupuncture plus language training on language function and cerebral blood flow in patients with motor aphasia after ischemic stroke. J. Acupunct. Tuina Sci. 2021, 19, 378–383. [Google Scholar] [CrossRef]
- Xu, M.; Qiu, L.; Zhu, X.; Wang, S.; Wang, R.; Luo, W.; Zhang, J. Discussion on the therapeutic effect of acupuncture combined with schuell on aphasia after stroke. World Latest Med. Inf. 2021, 21, 30–31. [Google Scholar] [CrossRef]
- Yu, Q.; He, S. Evaluation of curative effect of acupuncture combined with shure stimulation therapy on post-stroke aphasia based on the theory of biaoben genjie. Hebei J. Tradit. Chin. Med. 2018, 40, 608–611. [Google Scholar] [CrossRef]
- Zhao, C.; Zheng, Y.; Zhang, Y. Observations on the effect of acupuncture for treatment of 46 patients with apoplectic aphasia. Shanghai J. Acupunct. Moxibustion 2004, 23, 13–14. [Google Scholar] [CrossRef]
- Zhao, D.; Zhao, Y.; Yang, X. Effect of du mai acupoint acupuncture combined with schuell language rehabilitation training on the speech function, moca and the function of language center in aphasia patients after stroke. J. Clin. Exp. Med. 2021, 20, 886–890. [Google Scholar] [CrossRef]
- Feng, X.; Gu, J. Analysis of therapeutic effect of acupuncture combined with rehabilitation training on aphasia. Chin. J. Otorhinolaryngol. Integr. Med. 2007, 15, 315, 276. [Google Scholar] [CrossRef]
- Hou, B.; Zhang, Z.; Sun, J.; Yang, H.; Yang, L. Effect of acupuncture combined with speech rehabilitation on language function score and clinical efficacy of post-stroke aphasia patients. J. Hebei Tradit. Chin. Med. Pharmacol. 2018, 33, 50–51. [Google Scholar] [CrossRef]
- Li, Q. Clinical effect of scalp acupuncture and abdominal acupuncture combined with language rehabilitation training on aphasia after stroke and its influence on language function. Nei Mong. J. Tradit. Chin. Med. 2017, 36, 88–89. [Google Scholar] [CrossRef]
- Li, Y.; Liu, W. Effect of tongdu tiaoshen acupuncture combined with language rehabilitation training on the rehabilitation of language function in patients with post-stroke aphasia. Hebei J. Tradit. Chin. Med. 2019, 41, 757–761. [Google Scholar] [CrossRef]
- Lu, Q.; Kang, B. Clinical observation on 32 cases of aphasia after stroke by acupuncture therapy combined with language training. Henan Tradit. Chin. Med. 2010, 30, 179–181. [Google Scholar] [CrossRef]
- Wang, G.; Liu, L.; Li, L.; Dong, B.; Wang, S. Clinic observation on motor aphasia after stroke by acupuncture and psychological intervention combined with rehabilitation training. J. Liaoning Univ. Tradit. Chin. Med. 2015, 17, 5–8. [Google Scholar] [CrossRef]
- Yang, X. Treatment with acupuncture and speech rehabilitation for post-stroke aphasia. China Contin. Med. Educ. 2015, 7, 251–252. [Google Scholar] [CrossRef]
- Zhang, S.; Liu, Y.; Li, Q. Effect of acupuncture combined with language training on motor aphasia of stroke patients. J. Pract. Tradit. Chin. Intern. Med. 2010, 24, 107–108. [Google Scholar] [CrossRef]
- Zhang, Y.; Yu, Z.; Zhang, Y.; Zhao, X.; Lin, C. Therapeutic observation on acupuncture and rehabilitation in treating motor aphasia after cerebral apoplexy. Shanghai J. Acupunct. Moxibustion 2012, 31, 781–783. [Google Scholar] [CrossRef]
- Chen, J. Effect of acupuncture combined with speech therapy on post-stroke aphasia. J. Clin. Acupunct. Moxibustion 2006, 22, 24–25. [Google Scholar] [CrossRef]
- Wang, L.; Liu, S.; Liu, M.; Li, B.; Hui, Z.; Gao, X. Post-stroke speech disorder treated with acupuncture and psychological intervention combined with rehabilitation training: A randomized controlled trial. Chin. Acupunct. Moxibustion 2011, 31, 481–486. [Google Scholar] [CrossRef]
- Wei, T.; Tang, Q.; Chen, J. Clinical study of acupuncture combined with speech therapy in the treatment of aphasia after stroke. Chin. Prim. Health Care 2005, 19, 88–89. [Google Scholar] [CrossRef]
- Bao, W.; Mu, Y.; Xie, C.; Huang, X.; Cheng, M.; Ding, Q. Therapeutic effect and action mechanism of du meridian acupuncture combined with three-needle tongue acupuncture and speech rehabilitation training in treating post-stroke aphasia. J. Clin. Acupunct. Moxibustion 2020, 36, 32–35. [Google Scholar] [CrossRef]
- Li, Z.; Sun, S. Clinical observation of tongue three-needle combined with language rehabilitation training in the treatment of stroke aphasia. J. Liaoning Univ. Tradit. Chin. Med. 2019, 21, 167–170. [Google Scholar] [CrossRef]
- Xie, M.; Diao, J.; Zeng, K. Clinical observation on 22 cases of aphasia after stroke treated by acupuncture combined with speech training. Chinese Journal of Ethnomedicine and Ethnopharmacy 2015, 24, 64. [Google Scholar]
- He, A.; An, J. Therapeutic observation of tongue acupuncture plus schuell’s stimulation approach for post-stroke motor aphasia. Shanghai J. Acupunct. Moxibustion 2014, 33, 103–104. [Google Scholar] [CrossRef]
- Li, Z. Effect analysis of xingnaokaiqiao acupuncture combined with speech training in the treatment of aphasia after stroke. Henan Med. Res. 2019, 28, 2040–2042. [Google Scholar] [CrossRef]
- Luo, W.; Huang, H.; Song, J. Acupuncture combined with language training for treatment of motor aphasia caused by ischemic apoplex. World J. Acupunct. -Moxibustion 2008, 18, 9–16. [Google Scholar] [CrossRef]
- Song, C.; Li, S.; Xue, S.; Chen, G.; Xie, Z.; Lin, J. Clinical research on broca aphasia after stroke by jin’s three needles therapy combined with schuell stimulation method. Chin. J. Pract. Nerv. Dis. 2017, 20, 35–38. [Google Scholar] [CrossRef]
- Wang, Q.; Xu, Z. Clinical observation of modified tongue acupuncture combined with schuell stimulation therapy in the treatment of mild-to-moderate motor aphasia after stroke. Hebei J. Tradit. Chin. Med. 2018, 40, 589–592. [Google Scholar] [CrossRef]
- Wang, T.; Liu, Q.; Zhao, L.; Gao, Y.; Zhao, B. Clinical observations on tongue acupuncture combined with language therapy in motor aphasia after stroke. Shandong J. Tradit. Chin. Med. 2016, 35, 36–37. [Google Scholar] [CrossRef]
- Xu, Q.; Liu, J.; Wang, T.; Tan, C. Clinical effect of tongdu kaiyin acupuncture combined with scalp acupuncture in treating post-stroke motor aphasia of qi deficiency and blood stasis and its influence to serum levels of cgrp and et. J. Clin. Acupunct. Moxibustion 2021, 37, 11–15. [Google Scholar] [CrossRef]
- Zhou, L.; Zheng, S. Acupuncture combined with language rehabilitation in the treatment of sensory aphasia after stroke. J. Clin. Acupunct. Moxibustion 2012, 28, 21–23. [Google Scholar] [CrossRef]
- Yang, D.; Han, B. Observation on 35 cases of aphasia after stroke treated by acupuncture of scalp words area. Shanxi J. Tradit. Chin. Med. 2011, 27, 33–34. [Google Scholar] [CrossRef]
- Hope, T.; Leff, A.P.; Prejawa, S.; Bruce, R.; Haigh, Z.; Lim, L.; Ramsden, S.; Oberhuber, M.; Ludersdorfer, P.; Crinion, J.; et al. Right hemisphere structural adaptation and changing language skills years after left hemisphere stroke. Brain 2017, 140, 1718–1728. [Google Scholar] [CrossRef]
- Landrigan, J.F.; Zhang, F.; Mirman, D. A data-driven approach to post-stroke aphasia classification and lesion-based prediction. Brain 2021, 144, 1372–1383. [Google Scholar] [CrossRef] [PubMed]
- Pisano, F.; Giachero, A.; Rugiero, C.; Calati, M.; Marangolo, P. Does covid−19 impact less on post-stroke aphasia? This is not the case. Front. Psychol. 2020, 11, 564717. [Google Scholar] [CrossRef]
- Ren, C.; Zhang, G.; Xu, X.; Hao, J.; Fang, H.; Chen, P.; Li, Z.; Ji, Y.; Cai, Q.; Gao, F. The effect of rtms over the different targets on language recovery in stroke patients with global aphasia: A randomized sham-controlled study. Biomed Res. Int. 2019, 2019, 4589056. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Lee, Y.; Choi, H.; Pyun, S.B. Community integration and quality of life in aphasia after stroke. Yonsei Med. J. 2015, 56, 1694–1702. [Google Scholar] [CrossRef]
- Pompon, R.H.; Smith, A.N.; Baylor, C.; Kendall, D. Exploring associations between a biological marker of chronic stress and reported depression and anxiety in people with aphasia. J. Speech Lang. Hear. Res. 2019, 62, 4119–4130. [Google Scholar] [CrossRef]
- Baker, C.; Worrall, L.; Rose, M.; Ryan, B. Stroke health professionals’ management of depression after post-stroke aphasia: A qualitative study. Disabil. Rehabil. 2021, 43, 217–228. [Google Scholar] [CrossRef]
- Berthier, M.L. Poststroke aphasia: Epidemiology, pathophysiology and treatment. Drugs Aging 2005, 22, 163–182. [Google Scholar] [CrossRef]
- Zhang, Y.; Wang, Y.; Wang, C.; Zhao, X.; Gong, X.; Sun, X.; Chen, H.; Wang, Y. Study on the pathogenic mechanism of broca’s and wernicke’s aphasia. Neurol. Res. 2006, 28, 59–65. [Google Scholar] [CrossRef]
- Shimogawa, T.; Morioka, T.; Sayama, T.; Haga, S.; Kanazawa, Y.; Murao, K.; Arakawa, S.; Sakata, A.; Iihara, K. The initial use of arterial spin labeling perfusion and diffusion-weighted magnetic resonance images in the diagnosis of nonconvulsive partial status epileptics. Epilepsy Res. 2017, 129, 162–173. [Google Scholar] [CrossRef] [PubMed]
- Wilson, S.M.; Schneck, S.M. Neuroplasticity in post-stroke aphasia: A systematic review and meta-analysis of functional imaging studies of reorganization of language processing. Neurobiol. Lang. 2021, 2, 22–82. [Google Scholar] [CrossRef] [PubMed]
- Cichon, N.; Wlodarczyk, L.; Saluk-Bijak, J.; Bijak, M.; Redlicka, J.; Gorniak, L.; Miller, E. Novel advances to post-stroke aphasia pharmacology and rehabilitation. J. Clin. Med. 2021, 10, 3778. [Google Scholar] [CrossRef]
- Tang, H.Y.; Tang, W.; Yang, F.; Wu, W.W.; Shen, G.M. Efficacy of acupuncture in the management of post-apoplectic aphasia: A systematic review and meta-analysis of randomized controlled trials. BMC Complement. Altern. Med. 2019, 19, 282. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Xue, S.A.; Zuo, Z. Acupuncture therapy on apoplectic aphasia rehabilitation. J. Tradit. Chin. Med. 2012, 32, 314–321. [Google Scholar] [CrossRef]
- Wong, V.C.; Sun, J.G.; Yeung, D.W. Pilot study of efficacy of tongue and body acupuncture in children with visual impairment. J. Child Neurol. 2006, 21, 463–473. [Google Scholar] [CrossRef]
- Wong, V.C.; Sun, J.G.; Yeung, D.W. Pilot study of positron emission tomography (pet) brain glucose metabolism to assess the efficacy of tongue and body acupuncture in cerebral palsy. J. Child Neurol. 2006, 21, 456–462. [Google Scholar] [CrossRef]
- Bono, D.; Belyk, M.; Longo, M.R.; Dick, F. Beyond language: The unspoken sensory-motor representation of the tongue in non-primates, non-human and human primates. Neurosci. Biobehav. Rev. 2022, 139, 104730. [Google Scholar] [CrossRef]
- Zhang, J.; Lu, C.; Wu, X.; Nie, D.; Yu, H. Neuroplasticity of acupuncture for stroke: An evidence-based review of mri. Neural Plast. 2021, 2021, 2662585. [Google Scholar] [CrossRef]
- Xie, Z.; Cui, F.; Zou, Y.; Bai, L. Acupuncture enhances effective connectivity between cerebellum and primary sensorimotor cortex in patients with stable recovery stroke. Evid. Based Complement. Altern. Med. 2014, 2014, 603909. [Google Scholar] [CrossRef]
- Ratmansky, M.; Levy, A.; Messinger, A.; Birg, A.; Front, L.; Treger, I. The effects of acupuncture on cerebral blood flow in post-stroke patients: A randomized controlled trial. J. Altern. Complement. Med. 2016, 22, 33–37. [Google Scholar] [CrossRef] [PubMed]
- Liu, Q. Effects of acupuncture on hemorheology, blood lipid content and nail fold microcirculation in multiple infarct dementia patients. J. Tradit. Chin. Med. 2004, 24, 219–223. [Google Scholar] [PubMed]
- Cao, J.; Huang, Y.; Meshberg, N.; Hodges, S.A.; Kong, J. Neuroimaging-based scalp acupuncture locations for dementia. J. Clin. Med. 2020, 9, 2477. [Google Scholar] [CrossRef]
- Yau, C.H.; Ip, C.L.; Chau, Y.Y. The therapeutic effect of scalp acupuncture on natal autism and regressive autism. Chin. Med. 2018, 13, 30. [Google Scholar] [CrossRef]
- Allam, H.; Eldine, N.G.; Helmy, G. Scalp acupuncture effect on language development in children with autism: A pilot study. J. Altern. Complement. Med. 2008, 14, 109–114. [Google Scholar] [CrossRef]
- Liu, C.; Li, T.; Wang, Z.; Zhou, R.; Zhuang, L. Scalp acupuncture treatment for children’s autism spectrum disorders: A systematic review and meta-analysis. Medicine 2019, 98, e14880. [Google Scholar] [CrossRef]
- Liu, H.; Jiang, Y.; Wang, N.; Yan, H.; Chen, L.; Gao, J.; Zhang, J.; Qu, S.; Liu, S.; Liu, G.; et al. Scalp acupuncture enhances local brain regions functional activities and functional connections between cerebral hemispheres in acute ischemic stroke patients. Anat. Rec. 2021, 304, 2538–2551. [Google Scholar] [CrossRef]
- Li, B.; Deng, S.; Sang, B.; Zhu, W.; Zhuo, B.; Zhang, M.; Qin, C.; Lyu, Y.; Du, Y.; Meng, Z. Revealing the neuroimaging mechanism of acupuncture for poststroke aphasia: A systematic review. Neural Plast. 2022, 2022, 5635596. [Google Scholar] [CrossRef]

| Study | Sample Number | Gender (M/F) | Age | Therapy | Outcome | Reference | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| T | C | T | C | T | C | T | C | |||
| Bao W., 2020 | 40 | 40 | 25/15 | 13/17 | 61.30 | 62.48 | SLT + BA + TA | SLT | 1 | [102] |
| Chen J., 2006 | 30 | 30 | 17/13 | 16/14 | 63.12 | 61.71 | SLT + BA + SA + TA | SLT | 1 | [99] |
| Chen X., 2021 | 41 | 41 | 24/17 | 25/16 | 56.22 | 56.24 | SLT + BA | SLT | 1/2/4/5 | [75] |
| Cheng X., 2018 | 20 | 20 | 14/6 | 13/7 | 63.15 | 63.34 | SLT + SA | SLT | 3/4/5 | [61] |
| Dong X., 2020 | 56 | 56 | 30/26 | 33/23 | 60.85 | 62.57 | SLT + SA | SLT | 1 | [62] |
| Dong Y., 2009 | 30 | 30 | 18/12 | 17/13 | - | - | SLT + BA | SLT | 1 | [76] |
| Feng X., 2007 | 30 | 30 | 19/11 | 21/9 | 61 | 65 | SLT + BA + SA | SLT | 1 | [90] |
| He J., 2021 | 56 | 56 | 26/30 | 31/25 | 55.67 | 56.12 | SLT + BA | SLT | 1 | [77] |
| He A., 2014 | 30 | 30 | 14/16 | 13/17 | 55 | 54 | SLT + TA | SLT | 1 | [105] |
| Hou B., 2018 | 50 | 50 | 26/24 | 24/26 | 33.6 | 34.2 | SLT + BA + SA | SLT | 1 | [91] |
| Hou W., 2012 | 30 | 30 | 13/17 | 15/15 | 57.1 | 56.7 | BA | SLT | 1/2/3/4/5 | [45] |
| Huang H., 2009 | 48 | 48 | 24/24 | 26/22 | 60.96 | 60.42 | SLT + SA | SLT | 1 | [63] |
| Huang S., 2016 | 42 | 42 | 21/21 | 22/20 | 62 | 62 | SLT + BA | BA | 1 | [78] |
| Jiang G., 2008 | 40 | 36 | 23/17 | 23/13 | 61.5 | 59.2 | BA + TA | BA | 1/2/3/4/5 | [57] |
| Li L., 2019 | 30 | 30 | 19/11 | 17/13 | 63 | 64 | TA | BA | 3/4 | [51] |
| Li L., 2020 | 30 | 30 | 17/13 | 16/14 | 56.07 | 54.47 | BA + TA | BA | 1/2/3/4/5 | [58] |
| Li G., 2006 | 30 | 30 | 12/18 | 14/16 | 57.6 | 58.3 | SLT + BA | SLT | 1 | [79] |
| Li Q., 2017 | 38 | 38 | 21/17 | 22/16 | 62.1 | 61.7 | SLT + BA + SA | SLT | 1 | [92] |
| Li S., 2014 | 60 | 53 | 32/28 | 27/26 | 61.5 | 62.2 | SLT + SA + TA | SLT | 1 | [70] |
| Li X., 2009 | 30 | 30 | 18/12 | 20/10 | 61.5 | 59.2 | BA + TA | BA | 1/2/3/4/5 | [59] |
| Li Y., 2019 | 45 | 45 | 28/17 | 29/16 | 56.5 | 56.9 | SLT + BA + SA | SLT | 1 | [93] |
| Li Z., 2019 | 40 | 40 | 23/17 | 25/15 | 57.7 | 58.03 | SLT + BA + TA | SLT | 1/2/3/4/5 | [103] |
| Li Z.Z., 2019 | 41 | 41 | 21/20 | 24/17 | 66.49 | 67.05 | SLT + TA | SLT | 1 | [106] |
| Li Z.P., 2004 | 32 | 30 | 20/12 | 18/12 | 60.5 | 61.8 | TA | BA | 1 | [52] |
| Li Z.P., 2005 | 46 | 36 | 28/18 | 24/12 | 61.5 | 59.2 | TA | BA | 1 | [53] |
| Liu J., 2018 | 50 | 50 | 27/23 | 31/19 | 57.98 | 58.05 | BA | SLT | 1 | [46] |
| Liu J., 2018 | 36 | 36 | 20/16 | 18/18 | 57.68 | 58.01 | BA | SLT | 1 | [47] |
| Liu J., 2018 | 36 | 36 | 19/17 | 18/18 | 56.87 | 58.01 | BA | SLT | 1/2/3/4/5 | [48] |
| Liu L., 2006 | 30 | 28 | 22/8 | 18/10 | - | - | SLT + BA | SLT | 1 | [80] |
| Liu X., 2011 | 32 | 32 | 19/13 | 21/11 | 65 | 65 | TA | BA | 1 | [54] |
| Lu Q., 2010 | 32 | 32 | 22/10 | 26/6 | 50.5 | 45.3 | SLT + BA + SA | SLT | 1/2/3 | [94] |
| Luo W., 2008 | 30 | 30 | 19/11 | 16/14 | 60.0 | 62.2 | SLT + TA | SLT | 2/3/4/5 | [107] |
| Luo W., 2008 | 30 | 30 | 18/12 | 15/15 | 63.21 | 64.24 | SLT + BA | SLT | 2/3/4/5 | [81] |
| Mi J., 2004 | 46 | 38 | 26/20 | 20/18 | - | - | TA | BA | 1 | [55] |
| Qin L., 2018 | 40 | 40 | - | - | - | - | SLT + BA | SLT | 2/4/5 | [82] |
| Qiu L., 2020 | 30 | 30 | 21/9 | 24/6 | 52.0 | 53.0 | SLT + SA | SLT | 1 | [64] |
| Shi L., 2021 | 40 | 40 | 22/18 | 24/16 | 65.69 | 64.80 | SLT + BA | SLT | 1 | [83] |
| Song C., 2017 | 31 | 30 | 20/11 | 18/12 | 61.0 | 60.1 | SLT + TA | SLT | 1 | [108] |
| Song Z., 2019 | 35 | 35 | 16/19 | 15/20 | 58.35 | 57.25 | SLT + SA | SLT | 1/2/3/4/5 | [65] |
| Tian H., 2012 | 58 | 40 | 30/28 | 20/20 | - | - | SLT + BA | SLT | 1 | [84] |
| Tong X., 2017 | 42 | 42 | 24/18 | 22/20 | 61.8 | 61.0 | SLT + SA + TA | SLT | 1/2/4/5 | [71] |
| Wang G., 2015 | 40 | 40 | 22/18 | 23/17 | 51.67 | 53.33 | SLT + BA + SA | SLT | 1/2/3/4/5 | [95] |
| Wang L., 2011 | 40 | 40 | 20/20 | 22/18 | 63.4 | 64.5 | SLT + BA + SA + TA | SLT | 1/2/3/4/5 | [100] |
| Wang M., 2016 | 40 | 40 | 24/16 | 25/15 | 63.6 | 63.5 | SLT + SA + TA | SLT | 1 | [72] |
| Wang P., 1999 | 30 | 20 | 18/12 | - | 63 | - | TA | BA | 1 | [56] |
| Wang Q., 2018 | 39 | 32 | 24/15 | 19/13 | 67.54 | 66.22 | SLT + TA | SLT | 2/3/4/5 | [109] |
| Wang S., 2006 | 39 | 39 | - | - | - | - | BA | SLT | 1 | [49] |
| Wang T., 2016 | 30 | 30 | 18/12 | 17/13 | 59.2 | 58.7 | SLT + TA | SLT | 1 | [110] |
| Wang W., 2009 | 26 | 26 | 14/12 | 15/11 | 60.8 | 59.36 | SLT + SA | SA | 1/2/3 | [66] |
| Wang Y., 2021 | 33 | 33 | 18/15 | 16/17 | 56.36 | 56.32 | SLT + SA | SLT | 1 | [67] |
| Wei J., 2021 | 41 | 40 | 24/17 | 22/18 | 60.0 | 58.3 | SLT + BA | SLT | 1/2/3/4/5 | [85] |
| Wei T., 2005 | 30 | 30 | 18/12 | 16/14 | 56.7 | 58.4 | SLT + BA + SA + TA | SLT | 1 | [101] |
| Wen Z., 2019 | 45 | 45 | 21/24 | 23/22 | 60.41 | 60.36 | SLT + SA + TA | SLT | 1/2/3/4/5 | [73] |
| Wu H., 2011 | 41 | 41 | - | - | - | - | BA | SLT | 1 | [50] |
| Wu M., 2008 | 58 | 58 | 38/20 | 36/22 | 61 | 63 | BA + TA | SLT | 1 | [60] |
| Xie M., 2015 | 22 | 22 | 12/10 | 14/8 | 52.1 | 50.4 | SLT + BA + TA | SLT | 1 | [104] |
| Xu M., 2021 | 41 | 41 | 22/19 | 23/18 | 58.82 | 58.68 | BA + SA | SA | 1/2/3/4/5 | [111] |
| Xu M., 2021 | 30 | 30 | 17/13 | 18/12 | 56.4 | 56.8 | SLT + BA | SLT | 1 | [86] |
| Yang D., 2011 | 35 | 32 | 25/10 | 20/12 | - | - | SA | BA | 1/2/3/4/5 | [113] |
| Yang X., 2015 | 35 | 35 | - | - | - | - | SLT + BA + SA | SLT | 1 | [96] |
| Yu Q., 2018 | 30 | 30 | 18/12 | 17/13 | 57.06 | 58.52 | SLT + BA | SLT | 1 | [87] |
| Zhang H., 2022 | 40 | 40 | 25/15 | 26/14 | 54.08 | 54.26 | SLT + SA + TA | SLT | 1 | [74] |
| Zhang R., 2020 | 38 | 38 | 21/17 | 23/15 | 57.32 | 59.16 | SLT + SA | SLT | 1 | [68] |
| Zhang S., 2010 | 24 | 23 | 15/9 | 13/10 | 62.7 | 63.2 | SLT + BA + SA | SLT | 1 | [97] |
| Zhang Y., 2012 | 34 | 34 | 20/14 | 18/16 | 52 | 55 | SLT + BA + SA | SLT | 1 | [98] |
| Zhang Y.J., 2020 | 40 | 40 | - | - | - | - | SLT + SA | SLT | 1 | [69] |
| Zhao C., 2004 | 46 | 35 | 25/21 | 23/12 | 69 | 66 | SLT + BA | SLT | 1 | [88] |
| Zhao D., 2021 | 48 | 48 | 26/22 | 27/21 | 61.79 | 62.42 | SLT + BA | SLT | 1 | [89] |
| Zhou L., 2012 | 32 | 34 | 17/15 | 18/16 | 58.40 | 58.75 | BA + SA + TA | SLT | 1/2/3/4/5 | [112] |
| N | B | D | H | L | J | G | I | C | M | K | A | E | F |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | 1.04 (0.12, 8.76) | 0.74 (0.29, 1.93) | 0.69 (0.26, 1.78) | 0.62 (0.22, 1.76) | 0.58 (0.18, 1.89) | 0.55 (0.23, 1.31) | 0.48 (0.13, 1.85) | 0.48 (0.11, 2.12) | 0.37 (0.13, 1.06) | 0.37 (0.14, 0.95) | 0.29 (0.15, 0.55) | 0.22 (0.05, 0.88) | 0.12 (0.06, 0.28) |
| 0.96 (0.11, 8.14) | B | 0.72 (0.08, 6.12) | 0.66 (0.08, 5.35) | 0.60 (0.07, 5.06) | 0.56 (0.06, 5.10) | 0.53 (0.07, 4.16) | 0.47 (0.05, 4.64) | 0.46 (0.04, 4.99) | 0.36 (0.04, 3.03) | 0.36 (0.05, 2.65) | 0.28 (0.04, 2.14) | 0.21 (0.04, 1.07) | 0.12 (0.02, 0.91) |
| 1.34 (0.52, 3.49) | 1.39 (0.16, 11.89) | D | 0.92 (0.35, 2.40) | 0.83 (0.29, 2.38) | 0.79 (0.24, 2.55) | 0.74 (0.31, 1.78) | 0.65 (0.17, 2.50) | 0.64 (0.14, 2.85) | 0.50 (0.17, 1.43) | 0.50 (0.19, 1.29) | 0.39 (0.19, 0.79) | 0.29 (0.07, 1.20) | 0.17 (0.08, 0.37) |
| 1.46 (0.56, 3.78) | 1.51 (0.19, 12.25) | 1.09 (0.42, 2.82) | H | 0.91 (0.39, 2.12) | 0.85 (0.31, 2.33) | 0.80 (0.42, 1.54) | 0.71 (0.21, 2.34) | 0.69 (0.18, 2.72) | 0.54 (0.23, 1.28) | 0.54 (0.26, 1.14) | 0.42 (0.21, 0.86) | 0.32 (0.08, 1.21) | 0.18 (0.11, 0.31) |
| 1.61 (0.57, 4.56) | 1.67 (0.20, 14.11) | 1.20 (0.42, 3.41) | 1.10 (0.47, 2.58) | L | 0.94 (0.32, 2.80) | 0.88 (0.41, 1.92) | 0.78 (0.22, 2.78) | 0.77 (0.18, 3.20) | 0.60 (0.23, 1.55) | 0.59 (0.25, 1.40) | 0.47 (0.21, 1.06) | 0.35 (0.09, 1.42) | 0.20 (0.10, 0.39) |
| 1.71 (0.53, 5.53) | 1.77 (0.20, 16.03) | 1.27 (0.39, 4.13) | 1.17 (0.43, 3.21) | 1.06 (0.36, 3.17) | J | 0.94 (0.36, 2.42) | 0.83 (0.21, 3.30) | 0.81 (0.18, 3.75) | 0.63 (0.21, 1.90) | 0.63 (0.23, 1.74) | 0.50 (0.19, 1.33) | 0.38 (0.08, 1.67) | 0.21 (0.09, 0.50) |
| 1.82 (0.76, 4.36) | 1.89 (0.24, 14.84) | 1.36 (0.56, 3.27) | 1.25 (0.65, 2.39) | 1.13 (0.52, 2.46) | 1.06 (0.41, 2.74) | G | 0.88 (0.28, 2.78) | 0.87 (0.23, 3.25) | 0.67 (0.31, 1.48) | 0.67 (0.35, 1.31) | 0.53 (0.29, 0.96) | 0.40 (0.11, 1.43) | 0.23 (0.15, 0.34) |
| 2.06 (0.54, 7.89) | 2.14 (0.22, 21.24) | 1.54 (0.40, 5.89) | 1.41 (0.43, 4.68) | 1.28 (0.36, 4.56) | 1.21 (0.30, 4.80) | 1.13 (0.36, 3.57) | I | 0.98 (0.19, 5.16) | 0.76 (0.21, 2.74) | 0.76 (0.23, 2.54) | 0.60 (0.18, 1.94) | 0.45 (0.09, 2.31) | 0.26 (0.09, 0.76) |
| 2.10 (0.47, 9.35) | 2.18 (0.20, 23.72) | 1.56 (0.35, 6.98) | 1.44 (0.37, 5.64) | 1.31 (0.31, 5.45) | 1.23 (0.27, 5.66) | 1.15 (0.31, 4.33) | 1.02 (0.19, 5.36) | C | 0.78 (0.19, 3.27) | 0.78 (0.20, 3.06) | 0.61 (0.16, 2.35) | 0.46 (0.08, 2.67) | 0.26 (0.07, 0.93) |
| 2.70 (0.94, 7.72) | 2.80 (0.33, 23.76) | 2.01 (0.70, 5.77) | 1.85 (0.78, 4.37) | 1.68 (0.64, 4.37) | 1.58 (0.53, 4.74) | 1.48 (0.67, 3.26) | 1.31 (0.36, 4.69) | 1.28 (0.31, 5.40) | M | 1.00 (0.42, 2.38) | 0.78 (0.34, 1.80) | 0.59 (0.15, 2.40) | 0.34 (0.17, 0.67) |
| 2.71 (1.05, 7.00) | 2.81 (0.38, 20.94) | 2.02 (0.78, 5.24) | 1.86 (0.88, 3.92) | 1.68 (0.71, 3.97) | 1.58 (0.57, 4.37) | 1.49 (0.77, 2.89) | 1.31 (0.39, 4.38) | 1.29 (0.33, 5.08) | 1.00 (0.42, 2.40) | K | 0.79 (0.39, 1.58) | 0.59 (0.18, 1.96) | 0.34 (0.20, 0.58) |
| 3.45 (1.82, 6.54) | 3.58 (0.47, 27.37) | 2.57 (1.26, 5.21) | 2.36 (1.17, 4.78) | 2.14 (0.94, 4.87) | 2.02 (0.75, 5.39) | 1.89 (1.05, 3.43) | 1.67 (0.51, 5.43) | 1.64 (0.43, 6.32) | 1.28 (0.56, 2.94) | 1.27 (0.63, 2.56) | A | 0.76 (0.22, 2.60) | 0.43 (0.27, 0.69) |
| 4.56 (1.13, 18.33) | 4.73 (0.94, 23.82) | 3.39 (0.83, 13.85) | 3.12 (0.83, 11.77) | 2.83 (0.70, 11.40) | 2.67 (0.60, 11.87) | 2.50 (0.70, 8.98) | 2.21 (0.43, 11.26) | 2.17 (0.37, 12.55) | 1.69 (0.42, 6.84) | 1.68 (0.51, 5.53) | 1.32 (0.38, 4.55) | E | 0.57 (0.17, 1.92) |
| 8.03 (3.62, 17.81) | 8.32 (1.10, 63.13) | 5.97 (2.68, 13.33) | 5.50 (3.27, 9.25) | 4.99 (2.55, 9.75) | 4.69 (1.98, 11.10) | 4.41 (2.98, 6.52) | 3.89 (1.32, 11.44) | 3.82 (1.08, 13.49) | 2.97 (1.50, 5.89) | 2.96 (1.73, 5.06) | 2.33 (1.45, 3.74) | 1.76 (0.52, 5.97) | F |
| D | B | A | N | G | E | L | J | M | H | K | C | I | F |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| D | 0.06 (−48.01, 48.13) | −4.97 (−26.16, 16.22) | −3.78 (−40.58, 33.01) | −11.11 (−44.49, 22.28) | −10.95 (−48.64, 26.73) | −12.46 (−51.45, 26.52) | −16.23 (−58.38, 25.92) | −16.55 (−53.11, 20.01) | −18.76 (−55.36, 17.84) | −20.45 (−57.48, 16.59) | −24.60 (−66.62, 17.42) | −29.97 (−71.98, 12.04) | −26.19 (−56.09, 3.71) |
| −0.06 (−48.13, 48.01) | B | −5.03 (−48.19, 38.12) | −3.84 (−56.45, 48.76) | −11.17 (−56.97, 34.64) | −11.01 (−40.90, 18.88) | −12.52 (−62.54, 37.50) | −16.29 (−68.83, 36.25) | −16.61 (−64.77, 31.55) | −18.82 (−67.03, 29.38) | −20.51 (−60.21, 19.19) | −24.66 (−77.10, 27.78) | −30.03 (−82.46, 22.40) | −26.25 (−69.59, 17.08) |
| 4.97 (−16.22, 26.16) | 5.03 (−38.12, 48.19) | A | 1.19 (−28.89, 31.27) | −6.13 (−31.93, 19.67) | −5.98 (−37.14, 25.19) | −7.49 (−40.21, 25.24) | −11.26 (−47.69, 25.18) | −11.57 (−41.37, 18.22) | −13.79 (−43.63, 16.06) | −15.47 (−45.85, 14.90) | −19.63 (−55.92, 16.66) | −25.00 (−61.28, 11.28) | −21.22 (−42.32, −0.12) |
| 3.78 (−33.01, 40.58) | 3.84 (−48.76, 56.45) | −1.19 (−31.27, 28.89) | N | −7.32 (−46.95, 32.31) | −7.17 (−50.48, 36.14) | −8.68 (−53.13, 35.77) | −12.45 (−59.69, 34.80) | −12.76 (−55.10, 29.58) | −14.98 (−57.35, 27.39) | −16.66 (−59.41, 26.09) | −20.82 (−67.95, 26.32) | −26.19 (−73.31, 20.94) | −22.41 (−59.15, 14.33) |
| 11.11 (−22.28, 44.49) | 11.17 (−34.64, 56.97) | 6.13 (−19.67, 31.93) | 7.32 (−32.31, 46.95) | G | 0.15 (−34.58, 34.89) | −1.36 (−30.47, 27.75) | −5.12 (−38.36, 28.11) | −5.44 (−31.22, 20.34) | −7.66 (−33.50, 18.18) | −9.34 (−40.00, 21.31) | −13.49 (−46.57, 19.58) | −18.86 (−51.93, 14.20) | −15.09 (−29.96, −0.21) |
| 10.95 (−26.73, 48.64) | 11.01 (−18.88, 40.90) | 5.98 (−25.19, 37.14) | 7.17 (−36.14, 50.48) | −0.15 (−34.89, 34.58) | E | −1.51 (−41.64, 38.62) | −5.28 (−48.51, 37.96) | −5.59 (−43.38, 32.20) | −7.81 (−45.65, 30.03) | −9.49 (−35.64, 16.65) | −13.65 (−56.75, 29.46) | −19.02 (−62.12, 24.08) | −15.24 (−46.64, 16.17) |
| 12.46 (−26.52, 51.45) | 12.52 (−37.50, 62.54) | 7.49 (−25.24, 40.21) | 8.68 (−35.77, 53.13) | 1.36 (−27.75, 30.47) | 1.51 (−38.62, 41.64) | L | −3.77 (−42.62, 35.08) | −4.09 (−36.78, 28.61) | −6.30 (−39.05, 26.45) | −7.98 (−44.65, 28.68) | −12.14 (−50.85, 26.58) | −17.51 (−56.21, 21.20) | −13.73 (−38.75, 11.29) |
| 16.23 (−25.92, 58.38) | 16.29 (−36.25, 68.83) | 11.26 (−25.18, 47.69) | 12.45 (−34.80, 59.69) | 5.12 (−28.11, 38.36) | 5.28 (−37.96, 48.51) | 3.77 (−35.08, 42.62) | J | −0.32 (−36.74, 36.10) | −2.53 (−39.00, 33.93) | −4.22 (−44.24, 35.81) | −8.37 (−50.28, 33.53) | −13.74 (−55.64, 28.16) | −9.96 (−39.68, 19.76) |
| 16.55 (−20.01, 53.11) | 16.61 (−31.55, 64.77) | 11.57 (−18.22, 41.37) | 12.76 (−29.58, 55.10) | 5.44 (−20.34, 31.22) | 5.59 (−32.20, 43.38) | 4.09 (−28.61, 36.78) | 0.32 (−36.10, 36.74) | M | −2.21 (−32.04, 27.61) | −3.90 (−37.98, 30.18) | −8.05 (−44.33, 28.22) | −13.42 (−49.69, 22.84) | −9.65 (−30.70, 11.41) |
| 18.76 (−17.84, 55.36) | 18.82 (−29.38, 67.03) | 13.79 (−16.06, 43.63) | 14.98 (−27.39, 57.35) | 7.66 (−18.18, 33.50) | 7.81 (−30.03, 45.65) | 6.30 (−26.45, 39.05) | 2.53 (−33.93, 39.00) | 2.21 (−27.61, 32.04) | H | −1.68 (−35.82, 32.45) | −5.84 (−42.16, 30.48) | −11.21 (−47.52, 25.10) | −7.43 (−28.56, 13.70) |
| 20.45 (−16.59, 57.48) | 20.51 (−19.19, 60.21) | 15.47 (−14.90, 45.85) | 16.66 (−26.09, 59.41) | 9.34 (−21.31, 40.00) | 9.49 (−16.65, 35.64) | 7.98 (−28.68, 44.65) | 4.22 (−35.81, 44.24) | 3.90 (−30.18, 37.98) | 1.68 (−32.45, 35.82) | K | −4.15 (−44.04, 35.74) | −9.52 (−49.40, 30.36) | −5.75 (−32.56, 21.07) |
| 24.60 (−17.42, 66.62) | 24.66 (−27.78, 77.10) | 19.63 (−16.66, 55.92) | 20.82 (−26.32, 67.95) | 13.49 (−19.58, 46.57) | 13.65 (−29.46, 56.75) | 12.14 (−26.58, 50.85) | 8.37 (−33.53, 50.28) | 8.05 (−28.22, 44.33) | 5.84 (−30.48, 42.16) | 4.15 (−35.74, 44.04) | C | −5.37 (−47.14, 36.40) | −1.59 (−31.13, 27.95) |
| 29.97 (−12.04, 71.98) | 30.03 (−22.40, 82.46) | 25.00 (−11.28, 61.28) | 26.19 (−20.94, 73.31) | 18.86 (−14.20, 51.93) | 19.02 (−24.08, 62.12) | 17.51 (−21.20, 56.21) | 13.74 (−28.16, 55.64) | 13.42 (−22.84, 49.69) | 11.21 (−25.10, 47.52) | 9.52 (−30.36, 49.40) | 5.37 (−36.40, 47.14) | I | 3.78 (−25.75, 33.31) |
| 26.19 (−3.71, 56.09) | 26.25 (−17.08, 69.59) | 21.22 (0.12, 42.32) | 22.41(−14.33, 59.15) | 15.09 (0.21, 29.96) | 15.24 (−16.17, 46.64) | 13.73 (−11.29, 38.75) | 9.96 (−19.76, 39.68) | 9.65 (−11.41, 30.70) | 7.43 (−13.70, 28.56) | 5.75 (−21.07, 32.56) | 1.59 (−27.95, 31.13) | −3.78 (−33.31, 25.75) | F |
| N | D | B | A | K | G | M | L | J | E | I | C | H | F |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | −3.64 (−26.07, 18.80) | −7.79 (−39.85, 24.26) | −12.70 (−32.23, 6.83) | −13.73 (−40.61, 13.15) | −14.57 (−41.47, 12.33) | −15.63 (−42.53, 11.27) | −16.61 (−46.74, 13.53) | −16.98 (−42.12, 8.15) | −17.30 (−42.82, 8.22) | −20.71 (−50.69, 9.27) | −21.05 (−50.98, 8.88) | −21.31 (−51.26, 8.64) | −21.71 (−44.86, 1.43) |
| 3.64 (−18.80, 26.07) | D | −4.16 (−31.86, 23.55) | −9.06 (−20.10, 1.97) | −10.09 (−31.61, 11.42) | −10.93 (−32.47, 10.61) | −11.99 (−33.53, 9.55) | −12.97 (−38.43, 12.49) | −13.35 (−32.63, 5.94) | −13.66 (−33.45, 6.12) | −17.07 (−42.35, 8.21) | −17.41 (−42.63, 7.81) | −17.67 (−42.92, 7.57) | −18.08 (−34.69, −1.46) |
| 7.79 (−24.26, 39.85) | 4.16 (−23.55, 31.86) | B | −4.91 (−30.32, 20.51) | −5.94 (−35.13, 23.26) | −6.78 (−35.98, 22.43) | −7.84 (−37.04, 21.37) | −8.82 (−41.03, 23.39) | −9.19 (−34.22, 15.84) | −9.51 (−28.91, 9.90) | −12.92 (−44.99, 19.15) | −13.26 (−45.28, 18.76) | −13.52 (−45.56, 18.52) | −13.92 (−39.71, 11.87) |
| 12.70 (−6.83, 32.23) | 9.06 (−1.97, 20.10) | 4.91 (−20.51, 30.32) | A | −1.03 (−19.50, 17.44) | −1.87 (−20.36, 16.63) | −2.93 (−21.42, 15.57) | −3.91 (−26.85, 19.04) | −4.28 (−20.10, 11.54) | −4.60 (−21.02, 11.82) | −8.01 (−30.75, 14.74) | −8.35 (−31.02, 14.33) | −8.61 (−31.31, 14.10) | −9.01 (−21.43, 3.41) |
| 13.73 (−13.15, 40.61) | 10.09 (−11.42, 31.61) | 5.94 (−23.26, 35.13) | 1.03 (−17.44, 19.50) | K | −0.84 (−20.20, 18.53) | −1.90 (−21.26, 17.47) | −2.88 (−26.53, 20.78) | −3.25 (−21.73, 15.22) | −3.57 (−25.39, 18.25) | −6.98 (−30.44, 16.48) | −7.32 (−30.71, 16.07) | −7.58 (−31.00, 15.84) | −7.98 (−21.66, 5.70) |
| 14.57 (−12.33, 41.47) | 10.93 (−10.61, 32.47) | 6.78 (−22.43, 35.98) | 1.87 (−16.63, 20.36) | 0.84 (−18.53, 20.20) | G | −1.06 (−20.45, 18.32) | −2.04 (−25.71, 21.63) | −2.42 (−20.91, 16.08) | −2.73 (−24.56, 19.10) | −6.14 (−29.62, 17.34) | −6.48 (−29.89, 16.93) | −6.74 (−30.18, 16.70) | −7.15 (−20.86, 6.56) |
| 15.63 (−11.27, 42.53) | 11.99 (−9.55, 33.53) | 7.84 (−21.37, 37.04) | 2.93 (−15.57, 21.42) | 1.90 (−17.47, 21.26) | 1.06 (−18.32, 20.45) | M | −0.98 (−24.65, 22.69) | −1.35 (−19.85, 17.14) | −1.67 (−23.50, 20.16) | −5.08 (−28.56, 18.40) | −5.42 (−28.83, 17.99) | −5.68 (−29.12, 17.76) | −6.09 (−19.79, 7.62) |
| 16.61 (−13.53, 46.74) | 12.97 (−12.49, 38.43) | 8.82 (−23.39, 41.03) | 3.91 (−19.04, 26.85) | 2.88 (−20.78, 26.53) | 2.04 (−21.63, 25.71) | 0.98 (−22.69, 24.65) | L | −0.37 (−23.32, 22.57) | −0.69 (−26.41, 25.02) | −4.10 (−31.22, 23.02) | −4.44 (−31.50, 22.62) | −4.70 (−31.79, 22.39) | −5.10 (−24.40, 14.19) |
| 16.98 (−8.15, 42.12) | 13.35 (−5.94, 32.63) | 9.19 (−15.84, 34.22) | 4.28 (−11.54, 20.10) | 3.25 (−15.22, 21.73) | 2.42 (−16.08, 20.91) | 1.35 (−17.14, 19.85) | 0.37 (−22.57, 23.32) | J | −0.32 (−16.13, 15.49) | −3.73 (−26.47, 19.02) | −4.07 (−26.74, 18.61) | −4.33 (−27.03, 18.38) | −4.73 (−17.15, 7.69) |
| 17.30 (−8.22, 42.82) | 13.66 (−6.12, 33.45) | 9.51 (−9.90, 28.91) | 4.60 (−11.82, 21.02) | 3.57 (−18.25, 25.39) | 2.73 (−19.10, 24.56) | 1.67 (−20.16, 23.50) | 0.69 (−25.02, 26.41) | 0.32 (−15.49, 16.13) | E | −3.41 (−28.95, 22.13) | −3.75 (−29.22, 21.72) | −4.01 (−29.51, 21.49) | −4.41 (−21.41, 12.58) |
| 20.71 (−9.27, 50.69) | 17.07 (−8.21, 42.35) | 12.92 (−19.15, 44.99) | 8.01 (−14.74, 30.75) | 6.98 (−16.48, 30.44) | 6.14 (−17.34, 29.62) | 5.08(−18.40, 28.56) | 4.10 (−23.02, 31.22) | 3.73 (−19.02, 26.47) | 3.41 (−22.13, 28.95) | I | −0.34 (−27.23, 26.55) | −0.60 (−27.52, 26.32) | −1.00 (−20.06, 18.06) |
| 21.05 (−8.88, 50.98) | 17.41 (−7.81, 42.63) | 13.26 (−18.76, 45.28) | 8.35 (−14.33, 31.02) | 7.32 (−16.07, 30.71) | 6.48 (−16.93, 29.89) | 5.42 (−17.99, 28.83) | 4.44 (−22.62, 31.50) | 4.07 (−18.61, 26.74) | 3.75 (−21.72, 29.22) | 0.34 (−26.55, 27.23) | C | −0.26 (−27.12, 26.60) | −0.66 (−19.64, 18.31) |
| 21.31 (−8.64, 51.26) | 17.67 (−7.57, 42.92) | 13.52 (−18.52, 45.56) | 8.61 (−14.10, 31.31) | 7.58 (−15.84, 31.00) | 6.74 (−16.70, 30.18) | 5.68 (−17.76, 29.12) | 4.70 (−22.39, 31.39) | 4.33 (−18.38, 27.03) | 4.01 (−21.49, 29.51) | 0.60 (−26.32, 27.52) | 0.26 (−26.60, 27.12) | H | −0.40 (−19.41, 18.61) |
| 21.71 (−1.43, 44.86) | 18.08 (1.46, 34.69) | 13.92 (−11.87, 39.71) | 9.01 (−3.41, 21.43) | 7.98 (−5.70, 21.66) | 7.15 (−6.56, 20.86) | 6.09 (−7.62, 19.79) | 5.10 (−14.19, 24.40) | 4.73 (−7.69, 17.15) | 4.41 (−12.58, 121.41) | 1.00 (−18.06, 20.06) | 0.66 (−18.31, 19.64) | 0.40 (−18.61, 19.41) | F |
| B | M | D | E | A | K | G | I | L | J | C | H | F |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | −4.06 (−27.23, 19.12) | −5.57 (−26.61, 15.46) | −11.11 (−22.75, 0.54) | −13.00 (−33.02, 7.02) | −13.97 (−37.32, 9.37) | −14.72 (−37.40, 7.96) | −17.40 (−40.71, 5.90) | −19.06 (−42.40, 4.28) | −23.53 (−47.22, 0.17) | −24.50 (−48.93, −0.07) | −24.60 (−49.21, 0.01) | −25.55 (−47.52, −3.59) |
| 4.06 (−19.12, 27.23) | M | −1.52 (−14.87, 11.83) | −7.05 (−27.09, 12.99) | −8.94 (−20.62, 2.74) | −9.92 (−26.67, 6.84) | −10.66 (−26.48, 5.15) | −13.35 (−30.04, 3.35) | −15.00 (−31.74, 1.74) | −19.47 (−36.70, −2.23) | −20.45 (−38.68, −2.21) | −20.55 (−39.02, −2.07) | −21.50 (−36.26, −6.74) |
| 5.57 (−15.46, 26.61) | 1.52 (−11.83, 14.87) | D | −5.53 (−23.06, 11.99) | −7.42 (−13.89, −0.96) | −8.40 (−22.04, 5.24) | −9.15 (−21.61, 3.32) | −11.83 (−25.39, 1.73) | −13.49 (−27.10, 0.13) | −17.95 (−32.17, −3.73) | −18.93 (−34.35, −3.51) | −19.03 (−34.73, −3.33) | −19.98 (−31.08, −8.88) |
| 11.11 (−0.54, 22.75) | 7.05 (−12.99, 27.09) | 5.53 (−11.99, 23.06) | E | −1.89 (−18.18, 14.39) | −2.87 (−23.11, 17.37) | −3.61 (−23.08, 15.85) | −6.30 (−26.48, 13.89) | −7.95 (−28.18, 12.27) | −12.42 (−33.05, 8.22) | −13.40 (−34.87, 8.08) | −13.50 (−35.18, 8.18) | −14.45 (−33.07, 4.17) |
| 13.00 (−7.02, 33.02) | 8.94 (−2.74, 20.62) | 7.42 (0.96, 13.89) | 1.89 (−14.39, 18.18) | A | −0.98 (−12.99, 11.04) | −1.72 (−12.39, 8.94) | −4.41 (−16.33, 7.52) | −6.06 (−18.05, 5.93) | −10.53 (−23.20, 2.15) | −11.50 (−25.51, 2.50) | −11.60 (−25.92, 2.71) | −12.56 (−21.58, −3.53) |
| 13.97 (−9.37, 37.32) | 9.92 (−6.84, 26.67) | 8.40 (−5.24, 22.04) | 2.87 (−17.37, 23.11) | 0.98 (−11.04, 12.99) | K | −0.75 (−10.53, 9.04) | −3.43 (−14.59, 7.73) | −5.09 (−16.28, 6.11) | −9.55 (−21.46, 2.36) | −10.53 (−23.89, 2.83) | −10.63 (−24.31, 3.05) | −11.58 (−19.57, −3.59) |
| 14.72 (−7.96, 37.40) | 10.66 (−5.15, 26.48) | 9.15 (−3.32, 21.61) | 3.61 (−15.85, 23.08) | 1.72 (−8.94, 12.39) | 0.75 (−9.04, 10.53) | G | −2.68 (−12.31, 6.94) | −4.34 (−13.98, 5.30) | −8.80 (−19.27, 1.66) | −9.78 (−21.88, 2.32) | −9.88 (−22.34, 2.57) | −10.83 (−16.47, −5.19) |
| 17.40 (−5.90, 40.71) | 13.35 (−3.35, 30.04) | 11.83 (−1.73, 25.39) | 6.30 (−13.89, 26.48) | 4.41 (−7.52, 16.33) | 3.43 (−7.73, 14.59) | 2.68 (−6.94, 12.31) | I | −1.66 (−12.71, 9.39) | −6.12 (−17.89, 5.65) | −7.10 (−20.34, 6.15) | −7.20 (−20.77, 6.37) | −8.15 (−15.95, −0.35) |
| 19.06 (−4.28, 42.40) | 15.00 (−1.74, 31.74) | 13.49 (−0.13, 27.10) | 7.95 (−12.27, 28.18) | 6.06 (−5.93, 18.05) | 5.09 (−6.11, 16.28) | 4.34 (−5.30, 13.98) | 1.66 (−9.39, 12.71) | L | −4.46 (−16.24, 7.31) | −5.44 (−18.71, 7.82) | −5.54 (−19.13, 8.05) | −6.49 (−14.32, 1.33) |
| 23.53 (−0.17, 47.22) | 19.47 (2.23, 36.70) | 17.95 (3.73, 32.17) | 12.42 (−8.22, 33.05) | 10.53 (−2.15, 23.20) | 9.55 (−2.36, 21.46) | 8.80 (−1.66, 19.27) | 6.12 (−5.65, 17.89) | 4.46 (−7.31, 16.24) | J | −0.98 (−14.85, 12.89) | −1.08 (−15.26, 13.11) | −2.03 (−10.85, 6.79) |
| 24.50 (0.07, 48.93) | 20.45 (2.21, 38.68) | 18.93 (3.51, 34.35) | 13.40 (−8.08, 34.87) | 11.50 (−2.50, 25.51) | 10.53 (−2.83, 23.89) | 9.78 (−2.32, 21.88) | 7.10 (−6.15, 20.34) | 5.44 (−7.82, 18.71) | 0.98 (−12.89, 14.85) | C | −0.10 (−15.53, 15.33) | −1.05 (−11.76, 9.65) |
| 24.60 (−0.01, 49.21) | 20.55 (2.07, 39.02) | 19.03 (3.33, 34.73) | 13.50 (−8.18, 35.18) | 11.60 (−2.71, 25.92) | 10.63 (−3.05, 24.31) | 9.88 (−2.57, 22.34) | 7.20 (−6.37, 20.77) | 5.54 (−8.05, 19.13) | 1.08 (−13.11, 15.26) | 0.10 (−15.33, 15.53) | H | −0.95 (−12.06, 10.15) |
| 25.55 (3.59, 47.52) | 21.50 (6.74, 36.26) | 19.98 (8.88, 31.08) | 14.45 (−4.17, 33.07) | 12.56 (3.53, 21.58) | 11.58 (3.59, 19.57) | 10.83 (5.19, 16.47) | 8.15 (0.35, 15.95) | 6.49 (−1.33, 14.32) | 2.03 (−6.79, 10.85) | 1.05 (−9.65, 11.76) | 0.95 (−10.15, 12.06) | F |
| B | D | A | E | G | L | H | M | J | C | I | F | K |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | −6.81 (−28.94, 15.31) | −11.96 (−33.01, 9.09) | −10.07 (−22.66, 2.53) | −18.83 (−42.95, 5.30) | −19.63 (−44.45, 5.18) | −21.02 (−47.14, 5.09) | −22.30 (−47.27, 2.67) | −23.60 (−49.81, 2.60) | −28.08 (−54.15, −2.02) | −28.44 (−54.51, −2.38) | −28.65 (−52.01, −5.29) | −29.47 (−54.63, −4.32) |
| 6.81 (−15.31, 28.94) | D | −5.15 (−11.95, 1.66) | −3.25 (−21.44, 14.94) | −12.01 (−25.61, 1.59) | −12.82 (−27.61, 1.96) | −14.21 (−31.08, 2.66) | −15.49 (−30.53, −0.45) | −16.79 (−33.81, 0.23) | −21.27 (−38.08, −4.47) | −21.63 (−38.43, −4.83) | −21.83 (−34.02, −9.65) | −22.66 (−38.02, −7.31) |
| 11.96 (−9.09, 33.01) | 5.15 (−1.66, 11.95) | A | 1.89 (−14.98, 18.76) | −6.87 (−18.66, 4.92) | −7.68 (−20.81, 5.46) | −9.07 (−24.51, 6.38) | −10.34 (−23.77, 3.08) | −11.65 (−27.25, 3.96) | −16.13 (−31.50, −0.75) | −16.49 (−31.86, −1.11) | −16.69 (−26.81, −6.56) | −17.52 (−31.29, −3.74) |
| 10.07 (−2.53, 22.66) | 3.25 (−14.94, 21.44) | −1.89 (−18.76, 14.98) | E | −8.76 (−29.34, 11.82) | −9.57 (−30.95, 11.81) | −10.96 (−33.83, 11.92) | −12.23 (−33.79, 9.33) | −13.54 (−36.52, 9.45) | −18.02 (−40.84, 4.81) | −18.38 (−41.20, 4.45) | −18.58 (−38.25, 1.10) | −19.41 (−41.19, 2.37) |
| 18.83 (−5.30, 42.95) | 12.01 (−1.59, 25.61) | 6.87 (−4.92, 18.66) | 8.76 (−11.82, 29.34) | G | −0.81 (−11.12, 9.50) | −2.20 (−15.31, 10.92) | −3.47 (−14.01, 7.06) | −4.78 (−18.08, 8.53) | −9.26 (−22.29, 3.77) | −9.62 (−22.64, 3.41) | −9.82 (−15.81, −3.83) | −10.65 (−21.71, 0.42) |
| 19.63 (−5.18, 44.45) | 12.82 (−1.96, 27.61) | 7.68 (−5.46, 20.81) | 9.57 (−11.81, 30.95) | 0.81 (−9.50, 11.12) | L | −1.39 (−15.76, 12.98) | −2.67 (−14.74, 9.41) | −3.97 (−18.52, 10.58) | −8.45 (−22.74, 5.84) | −8.81 (−23.10, 5.48) | −9.01 (−17.40, −0.62) | −9.84 (−22.37, 2.69) |
| 21.02 (−5.09, 47.14) | 14.21 (−2.66, 31.08) | 9.07 (−6.38, 24.51) | 10.96 (−11.92, 33.83) | 2.20 (−10.92, 15.31) | 1.39 (−12.98, 15.76) | H | −1.28 (−15.82, 13.27) | −2.58 (−19.23, 14.07) | −7.06 (−23.49, 9.37) | −7.42 (−23.85, 9.01) | −7.62 (−19.29, 4.05) | −8.45 (−23.37, 6.48) |
| 22.30 (−2.67, 47.27) | 15.49 (0.45, 30.53) | 10.34 (−3.08, 23.77) | 12.23 (−9.33, 33.79) | 3.47 (−7.06, 14.01) | 2.67 (−9.41, 14.74) | 1.28 (−13.27, 15.82) | M | −1.30 (−16.02, 13.41) | −5.78 (−20.25, 8.68) | −6.14 (−20.60, 8.32) | −6.35 (−15.03, 2.33) | −7.17 (−19.89, 5.54) |
| 23.60 (−2.60, 49.81) | 16.79 (−0.23, 33.81) | 11.65 (−3.96, 27.25) | 13.54 (−9.45, 36.52) | 4.78 (−8.53, 18.08) | 3.97 (−10.58, 18.52) | 2.58 (−14.07, 19.23) | 1.30 (−13.41, 16.02) | J | −4.48 (−21.06, 12.10) | −4.84 (−21.42, 11.74) | −5.04 (−16.92, 6.84) | −5.87 (−20.96, 9.22) |
| 28.08 (2.02, 54.15) | 21.27 (4.47, 38.08) | 16.13 (0.75, 31.50) | 18.02 (−4.81, 40.84) | 9.26 (−3.77, 22.29) | 8.45 (−5.84, 22.74) | 7.06 (−9.37, 23.49) | 5.78 (−8.68, 20.25) | 4.48 (−12.10, 21.06) | C | −0.36 (−16.72, 16.00) | −0.56 (−12.13, 11.01) | −1.39 (−16.24, 13.46) |
| 28.44 (2.38, 54.51) | 21.63 (4.83, 38.43) | 16.49 (1.11, 31.86) | 18.38 (−4.45, 41.20) | 9.62 (−3.41, 22.64) | 8.81 (−5.48, 23.10) | 7.42 (−9.01, 23.85) | 6.14 (−8.32, 20.60) | 4.84 (−11.74, 21.42) | 0.36 (−16.00, 16.72) | I | −0.20 (−11.77, 11.36) | −1.03 (−15.87, 13.82) |
| 28.65 (5.29, 52.01) | 21.83 (9.65, 34.02) | 16.69 (6.56, 26.81) | 18.58 (−1.10, 38.25) | 9.82 (3.83, 15.81) | 9.01 (0.62, 17.40) | 7.62 (−4.05, 19.29) | 6.35 (−2.33, 15.03) | 5.04 (−6.84, 16.92) | 0.56 (−11.01, 12.13) | 0.20 (−11.36, 11.77) | F | −0.83 (−10.13, 8.48) |
| 29.47 (4.32, 54.63) | 22.66 (7.31, 38.02) | 17.52 (3.74, 31.29) | 19.41 (−2.37, 41.19) | 10.65 (−0.42, 21.71) | 9.84 (−2.69, 22.37) | 8.45 (−6.48, 23.37) | 7.17 (−5.54, 19.89) | 5.87 (−9.22, 20.96) | 1.39 (−13.46, 16.24) | 1.03 (−13.82, 15.87) | 0.83 (−8.48, 10.13) | K |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liang, P.; Li, Y.; Feng, Y.; Yin, G.; Chen, S.; Liu, X.; Zhang, F. Effects of Acupuncture-Related Therapies in the Rehabilitation of Patients with Post-Stroke Aphasia—A Network Meta-Analysis of Randomized Controlled Trials. Brain Sci. 2022, 12, 1282. https://doi.org/10.3390/brainsci12101282
Liang P, Li Y, Feng Y, Yin G, Chen S, Liu X, Zhang F. Effects of Acupuncture-Related Therapies in the Rehabilitation of Patients with Post-Stroke Aphasia—A Network Meta-Analysis of Randomized Controlled Trials. Brain Sciences. 2022; 12(10):1282. https://doi.org/10.3390/brainsci12101282
Chicago/Turabian StyleLiang, Pengpeng, Yufei Li, Yanan Feng, Guoliang Yin, Suwen Chen, Xiangyi Liu, and Fengxia Zhang. 2022. "Effects of Acupuncture-Related Therapies in the Rehabilitation of Patients with Post-Stroke Aphasia—A Network Meta-Analysis of Randomized Controlled Trials" Brain Sciences 12, no. 10: 1282. https://doi.org/10.3390/brainsci12101282






