Structural Cerebellar Abnormalities and Parkinsonism in Patients with 22q11.2 Deletion Syndrome
Abstract
:1. Introduction
Aims and Objectives
2. Methods
2.1. Study Design and Participants
2.2. Clinical and Neuropsychological Assessment
2.3. MRI Data Acquisition and Voxel-Based Morphometry (VBM)
2.4. Statistical Analyses
3. Results
3.1. Clinical Findings
3.2. VBM
3.3. Correlation Analyses
4. Discussion
4.1. GMV Alterations in Park+ and Park− Patients
4.2. Differences in GMV Alterations between Park+ and Park− Patients
4.3. Study Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Botto, L.D.; May, K.; Fernhoff, P.M.; Correa, A.; Coleman, K.; Rasmussen, S.A.; Merritt, R.K.; O’Leary, L.A.; Wong, L.-Y.; Elixson, E.M.; et al. A Population-Based Study of the 22q11.2 Deletion: Phenotype, Incidence, and Contribution to Major Birth Defects in the Population. Pediatrics 2003, 112, 101–107. [Google Scholar] [CrossRef]
- McDonald-McGinn, D.M.; Sullivan, K.E.; Marino, B.; Philip, N.; Swillen, A.; Vorstman, J.A.S.; Zackai, E.H.; Emanuel, B.S.; Vermeesch, J.R.; Morrow, B.E.; et al. 22q11.2 Deletion Syndrome. Nat. Rev. Dis. Primers 2015, 1, 15071. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sullivan, K.E. Chromosome 22q11.2 Deletion Syndrome and DiGeorge Syndrome. Immunol. Rev. 2019, 287, 186–201. [Google Scholar] [CrossRef] [PubMed]
- Philip, N.; Bassett, A. Cognitive, Behavioural and Psychiatric Phenotype in 22q11.2 Deletion Syndrome. Behav. Genet. 2011, 41, 403–412. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chow, E.W.C.; Watson, M.; Young, D.A.; Bassett, A.S. Neurocognitive Profile in 22q11 Deletion Syndrome and Schizophrenia. Schizoph.r Res. 2006, 87, 270–278. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Evers, L.J.M.; De Die-Smulders, C.E.M.; Smeets, E.E.J.; Clerkx, M.G.M.; Curfs, L.M.G. The Velo-Cardio-Facial Syndrome: The Spectrum of Psychiatric Problems and Cognitive Deterioration at Adult Age. Genet. Couns. 2009, 20, 307–315. [Google Scholar]
- Bearden, C.E.; Woodin, M.F.; Wang, P.P.; Moss, E.; McDonald-McGinn, D.; Zackai, E.; Emannuel, B.; Cannon, T.D. The Neurocognitive Phenotype of the 22q11.2 Deletion Syndrome: Selective Deficit in Visual-Spatial Memory. J. Clin. Exp. Neuropsychol. 2001, 23, 447–464. [Google Scholar] [CrossRef]
- Zinkstok, J.; van Amelsvoort, T. Neuropsychological Profile and Neuroimaging in Patients with 22Q11.2 Deletion Syndrome: A Review. Child Neuropsychol. 2005, 11, 21–37. [Google Scholar] [CrossRef]
- Fanella, M.; Frascarelli, M.; Lambiase, C.; Morano, A.; Unolt, M.; Liberati, N.; Fattouch, J.; Buzzanca, A.; Accinni, T.; Ceccanti, M.; et al. Myoclonic Epilepsy, Parkinsonism, Schizophrenia and Left-Handedness as Common Neuropsychiatric Features in 22q11.2 Deletion Syndrome. J. Med. Genet. 2020, 57, 151–159. [Google Scholar] [CrossRef]
- Murphy, K.C. Schizophrenia and Velo-Cardio-Facial Syndrome. Lancet 2002, 359, 426–430. [Google Scholar] [CrossRef]
- Baker, K.; Vorstman, J.A.S. Is There a Core Neuropsychiatric Phenotype in 22q11.2 Deletion Syndrome? Curr. Opin. Neurol. 2012, 25, 131–137. [Google Scholar] [CrossRef]
- Antshel, K.M.; Aneja, A.; Strunge, L.; Peebles, J.; Fremont, W.P.; Stallone, K.; Abdulsabur, N.; Higgins, A.M.; Shprintzen, R.J.; Kates, W.R. Autistic Spectrum Disorders in Velo-Cardio Facial Syndrome (22q11.2 Deletion). J. Autism. Dev. Disord. 2007, 37, 1776–1786. [Google Scholar] [CrossRef]
- Schneider, M.; Debbané, M.; Bassett, A.S.; Chow, E.W.C.; Fung, W.L.A.; van den Bree, M.; Owen, M.; Murphy, K.C.; Niarchou, M.; Kates, W.R.; et al. Psychiatric Disorders from Childhood to Adulthood in 22q11.2 Deletion Syndrome: Results from the International Consortium on Brain and Behavior in 22q11.2 Deletion Syndrome. Am. J. Psychiatry 2014, 171, 627–639. [Google Scholar] [CrossRef] [PubMed]
- Antshel, K.M.; Fremont, W.; Roizen, N.J.; Shprintzen, R.; Higgins, A.M.; Dhamoon, A.; Kates, W.R. ADHD, Major Depressive Disorder, and Simple Phobias Are Prevalent Psychiatric Conditions in Youth with Velocardiofacial Syndrome. J. Am. Acad. Child Adolesc. Psychiatry 2006, 45, 596–603. [Google Scholar] [CrossRef] [PubMed]
- Fung, W.L.A.; McEvilly, R.; Fong, J.; Silversides, C.; Chow, E.; Bassett, A. Elevated Prevalence of Generalized Anxiety Disorder in Adults with 22q11.2 Deletion Syndrome. Am. J. Psychiatry 2010, 167, 998. [Google Scholar] [CrossRef] [PubMed]
- Bayat, M.; Bayat, A. Neurological Manifestation of 22q11.2 Deletion Syndrome. Neurol. Sci. 2022, 43, 1695–1700. [Google Scholar] [CrossRef] [PubMed]
- Krahn, L.E.; Maraganore, D.M.; Michels, V.V. Childhood-Onset Schizophrenia Associated With Parkinsonism in a Patient With a Microdeletion of Chromosome 22. Mayo Clin. Proc. 1998, 73, 956–959. [Google Scholar] [CrossRef] [Green Version]
- Zaleski, C.; Bassett, A.S.; Tam, K.; Shugar, A.L.; Chow, E.W.C.; McPherson, E. The Co-Occurrence of Early Onset Parkinson Disease and 22q11.2 Deletion Syndrome. Am. J. Med. Genet. A 2009, 149A, 525–528. [Google Scholar] [CrossRef] [Green Version]
- Booij, J.; van Amelsvoort, T.; Boot, E. Co-Occurrence of Early-Onset Parkinson Disease and 22q11.2 Deletion Syndrome: Potential Role for Dopamine Transporter Imaging. Am. J. Med. Genet. Part A 2010, 152A, 2937–2938. [Google Scholar] [CrossRef]
- Butcher, N.J.; Kiehl, T.-R.; Hazrati, L.-N.; Chow, E.W.C.; Rogaeva, E.; Lang, A.E.; Bassett, A.S. Association Between Early-Onset Parkinson Disease and 22q11.2 Deletion Syndrome. JAMA Neurol. 2013, 70, 1359–1366. [Google Scholar] [CrossRef]
- Rehman, A.F.; Dhamija, R.; Williams, E.S.; Barrett, M.J. 22q11.2 Deletion Syndrome Presenting with Early-Onset Parkinson’s Disease. Mov. Disord. 2015, 30, 1289–1290. [Google Scholar] [CrossRef] [PubMed]
- Mok, K.Y.; Sheerin, U.; Simón-Sánchez, J.; Salaka, A.; Chester, L.; Escott-Price, V.; Mantripragada, K.; Doherty, K.M.; Noyce, A.J.; Mencacci, N.E.; et al. Deletions at 22q11.2 in Idiopathic Parkinson’s Disease: A Combined Analysis of Genome-Wide Association Data. Lancet Neurol. 2016, 15, 585–596. [Google Scholar] [CrossRef] [Green Version]
- Dufournet, B.; Nguyen, K.; Charles, P.; Grabli, D.; Jacquette, A.; Borg, M.; Danaila, T.; Mutez, E.; Drapier, S.; Colin, O.; et al. Parkinson’s Disease Associated with 22q11.2 Deletion: Clinical Characteristics and Response to Treatment. Rev. Neurol. (Paris) 2017, 173, 406–410. [Google Scholar] [CrossRef]
- Butcher, N.J.; Merico, D.; Zarrei, M.; Ogura, L.; Marshall, C.R.; Chow, E.W.C.; Lang, A.E.; Scherer, S.W.; Bassett, A.S. Whole-Genome Sequencing Suggests Mechanisms for 22q11.2 Deletion-Associated Parkinson’s Disease. PLoS ONE 2017, 12, e0173944. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Oldfield, R.C. The Assessment and Analysis of Handedness: The Edinburgh Inventory. Neuropsychologia 1971, 9, 97–113. [Google Scholar] [CrossRef]
- Postuma, R.B.; Berg, D.; Stern, M.; Poewe, W.; Olanow, C.W.; Oertel, W.; Obeso, J.; Marek, K.; Litvan, I.; Lang, A.E.; et al. MDS Clinical Diagnostic Criteria for Parkinson’s Disease. Mov. Disord. 2015, 30, 1591–1601. [Google Scholar] [CrossRef]
- Antonini, A.; Abbruzzese, G.; Ferini-Strambi, L.; Tilley, B.; Huang, J.; Stebbins, G.T.; Goetz, C.G.; Barone, P.; MDS-UPDRS Italian Validation Study Group; Bandettini di Poggio, M.; et al. Validation of the Italian Version of the Movement Disorder Society--Unified Parkinson’s Disease Rating Scale. Neurol. Sci. 2013, 34, 683–687. [Google Scholar] [CrossRef]
- Goetz, C.G.; Tilley, B.C.; Shaftman, S.R.; Stebbins, G.T.; Fahn, S.; Martinez-Martin, P.; Poewe, W.; Sampaio, C.; Stern, M.B.; Dodel, R.; et al. Movement Disorder Society-Sponsored Revision of the Unified Parkinson’s Disease Rating Scale (MDS-UPDRS): Scale Presentation and Clinimetric Testing Results. Mov. Disord. 2008, 23, 2129–2170. [Google Scholar] [CrossRef]
- Nasreddine, Z.S.; Phillips, N.A.; Bédirian, V.; Charbonneau, S.; Whitehead, V.; Collin, I.; Cummings, J.L.; Chertkow, H. The Montreal Cognitive Assessment, MoCA: A Brief Screening Tool for Mild Cognitive Impairment. J. Am. Geriatr. Soc. 2005, 53, 695–699. [Google Scholar] [CrossRef]
- Tzourio-Mazoyer, N.; Landeau, B.; Papathanassiou, D.; Crivello, F.; Etard, O.; Delcroix, N.; Mazoyer, B.; Joliot, M. Automated Anatomical Labeling of Activations in SPM Using a Macroscopic Anatomical Parcellation of the MNI MRI Single-Subject Brain. Neuroimage 2002, 15, 273–289. [Google Scholar] [CrossRef]
- Stoodley, C.J.; Schmahmann, J.D. Functional Topography in the Human Cerebellum: A Meta-Analysis of Neuroimaging Studies. Neuroimage 2009, 44, 489–501. [Google Scholar] [CrossRef]
- Mitnick, R.J.; Bello, J.A.; Shprintzen, R.J. Brain Anomalies in Velo-Cardio-Facial Syndrome. Am. J. Med. Genet. 1994, 54, 100–106. [Google Scholar] [CrossRef]
- Lynch, D.R.; McDonald-McGinn, D.M.; Zackai, E.H.; Emanuel, B.S.; Driscoll, D.A.; Whitaker, L.A.; Fischbeck, K.H. Cerebellar Atrophy in a Patient with Velocardiofacial Syndrome. J. Med. Genet. 1995, 32, 561–563. [Google Scholar] [CrossRef]
- van Amelsvoort, T.; Daly, E.; Robertson, D.; Suckling, J.; Ng, V.; Critchley, H.; Owen, M.J.; Henry, J.; Murphy, K.C.; Murphy, D.G. Structural Brain Abnormalities Associated with Deletion at Chromosome 22q11: Quantitative Neuroimaging Study of Adults with Velo-Cardio-Facial Syndrome. Br. J. Psychiatry 2001, 178, 412–419. [Google Scholar] [CrossRef] [Green Version]
- Eliez, S.; Schmitt, J.E.; White, C.D.; Wellis, V.G.; Reiss, A.L. A Quantitative MRI Study of Posterior Fossa Development in Velocardiofacial Syndrome. Biol. Psychiatry 2001, 49, 540–546. [Google Scholar] [CrossRef]
- Bish, J.P.; Pendyal, A.; Ding, L.; Ferrante, H.; Nguyen, V.; McDonald-McGinn, D.; Zackai, E.; Simon, T.J. Specific Cerebellar Reductions in Children with Chromosome 22q11.2 Deletion Syndrome. Neurosci. Lett. 2006, 399, 245–248. [Google Scholar] [CrossRef]
- Schmitt, J.E.; DeBevits, J.J.; Roalf, D.R.; Ruparel, K.; Gallagher, R.S.; Gur, R.C.; Alexander-Bloch, A.; Eom, T.-Y.; Alam, S.; Steinberg, J.; et al. A Comprehensive Analysis of Cerebellar Volumes in the 22q11.2 Deletion Syndrome. Biol. Psychiatry: Cogn. Neurosci. Neuroimaging, 2021, in press. [CrossRef]
- O’Reilly, J.X.; Beckmann, C.F.; Tomassini, V.; Ramnani, N.; Johansen-Berg, H. Distinct and Overlapping Functional Zones in the Cerebellum Defined by Resting State Functional Connectivity. Cereb. Cortex 2010, 20, 953–965. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stoodley, C.J.; Valera, E.M.; Schmahmann, J.D. Functional Topography of the Cerebellum for Motor and Cognitive Tasks: An FMRI Study. Neuroimage 2012, 59, 1560–1570. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guell, X.; Schmahmann, J. Cerebellar Functional Anatomy: A Didactic Summary Based on Human FMRI Evidence. Cerebellum 2020, 19, 1–5. [Google Scholar] [CrossRef] [Green Version]
- Stoodley, C.J.; Schmahmann, J.D. Evidence for Topographic Organization in the Cerebellum of Motor Control versus Cognitive and Affective Processing. Cortex 2010, 46, 831–844. [Google Scholar] [CrossRef] [PubMed]
- Guell, X.; Gabrieli, J.D.E.; Schmahmann, J.D. Triple representation of language, working memory, social and emotion processing in the cerebellum: Convergent evidence from task and seed-based resting-state fmri analyses in a single large cohort. Neuroimage 2018, 172, 437–449. [Google Scholar] [CrossRef] [PubMed]
- Sokolov, A.A.; Erb, M.; Gharabaghi, A.; Grodd, W.; Tatagiba, M.S.; Pavlova, M.A. Biological Motion Processing: The Left Cerebellum Communicates with the Right Superior Temporal Sulcus. Neuroimage 2012, 59, 2824–2830. [Google Scholar] [CrossRef] [PubMed]
- Yamaguchi, K.; Sakurai, Y. Inactivation of Cerebellar Cortical Crus II Disrupts Temporal Processing of Absolute Timing but Not Relative Timing in Voluntary Movements. Front. Syst. Neurosci. 2016, 10, 16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schlerf, J.E.; Verstynen, T.D.; Ivry, R.B.; Spencer, R.M.C. Evidence of a Novel Somatopic Map in the Human Neocerebellum during Complex Actions. J. Neurophysiol. 2010, 103, 3330–3336. [Google Scholar] [CrossRef] [Green Version]
- Rolland, A.-S.; Herrero, M.-T.; Garcia-Martinez, V.; Ruberg, M.; Hirsch, E.C.; François, C. Metabolic Activity of Cerebellar and Basal Ganglia-Thalamic Neurons Is Reduced in Parkinsonism. Brain 2007, 130, 265–275. [Google Scholar] [CrossRef] [PubMed]
- Bostan, A.C.; Dum, R.P.; Strick, P.L. The Basal Ganglia Communicate with the Cerebellum. Proc. Natl. Acad. Sci. USA 2010, 107, 8452–8456. [Google Scholar] [CrossRef] [Green Version]
- Camicioli, R.; Gee, M.; Bouchard, T.P.; Fisher, N.J.; Hanstock, C.C.; Emery, D.J.; Martin, W.R.W. Voxel-Based Morphometry Reveals Extra-Nigral Atrophy Patterns Associated with Dopamine Refractory Cognitive and Motor Impairment in Parkinsonism. Park. Relat. Disord. 2009, 15, 187–195. [Google Scholar] [CrossRef]
- Borghammer, P.; Østergaard, K.; Cumming, P.; Gjedde, A.; Rodell, A.; Hall, N.; Chakravarty, M.M. A Deformation-Based Morphometry Study of Patients with Early-Stage Parkinson’s Disease. Eur. J. Neurol. 2010, 17, 314–320. [Google Scholar] [CrossRef]
- Rascol, O.; Sabatini, U.; Fabre, N.; Brefel, C.; Loubinoux, I.; Celsis, P.; Senard, J.M.; Montastruc, J.L.; Chollet, F. The Ipsilateral Cerebellar Hemisphere Is Overactive during Hand Movements in Akinetic Parkinsonian Patients. Brain 1997, 120, 103–110. [Google Scholar] [CrossRef] [Green Version]
- Yu, H.; Sternad, D.; Corcos, D.M.; Vaillancourt, D.E. Role of Hyperactive Cerebellum and Motor Cortex in Parkinson’s Disease. Neuroimage 2007, 35, 222–233. [Google Scholar] [CrossRef]
| HCs (N = 24) | 22q11.2DS (N = 29) | P * | Park+ (N = 15) | Park− (N = 14) | P * | |
|---|---|---|---|---|---|---|
| Demographic/ clinical features | ||||||
| Age | 29.8 ± 9.1 | 26.6 ± 8.1 | ns | 29.5 ± 9.8 | 23.5 ± 4.1 | ns |
| Female/male, n | 15/9 | 8/21 | 0.014 | 4/11 | 4/10 | ns |
| Left-handedness (yes/no) | 0/20 | 6/23 | 0.027 | 3/12 | 3/11 | ns |
| Neuroleptics (yes/no) | - | 12/17 | - | 7/8 | 5/9 | ns |
| Neuropsychological scores | ||||||
| MDS-UPDRS-III | - | 9.9 ± 8.6 § | - | 9.9 ± 8.6 | - | - |
| MoCA | - | 23.0 ± 4.0 | - | 22.3 ± 5.1 | 23.9 ± 1.8 | ns |
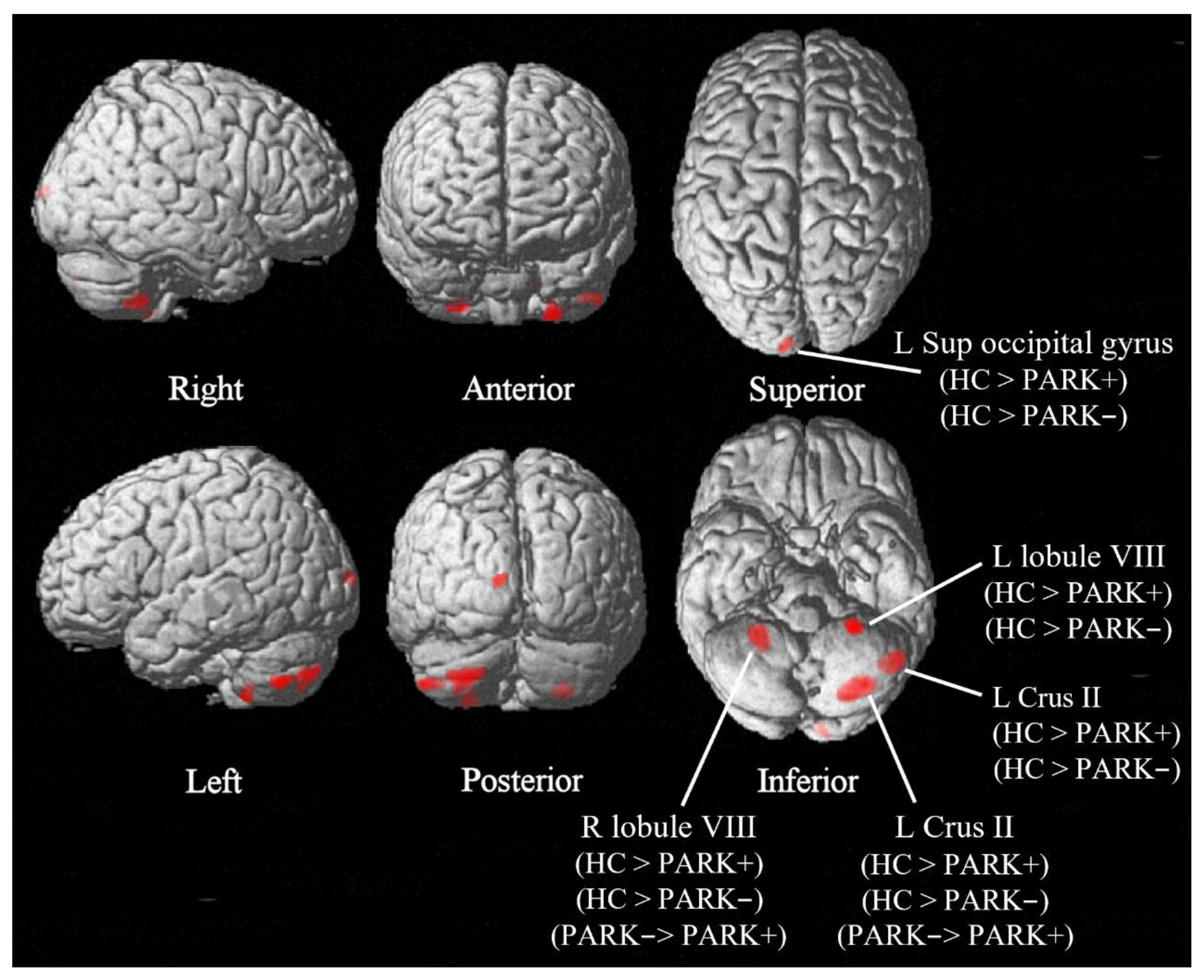
| K | F | P | MNI Coordinates (mm) | Brain region | Post hoc | ||
|---|---|---|---|---|---|---|---|
| x | y | Z | |||||
| 252 | 36.23 | <0.001 | 28 | −48 | −50 | R Cerebellum, lobule VIII | HCs > Park+ HCs > Park− Park− > Park+ |
| 172 | 32.83 | <0.001 | −24 | −42 | −58 | L Cerebellum, lobule VIII | HCs > Park+ HCs > Park− |
| 435 | 26.70 | <0.001 | −28 | −76 | −44 | L Cerebellum, Crus II | HCs > Park+ HCs > Park− Park− > Park+ |
| 78 | 24.54 | 0.001 | −8 | −99 | 9 | L Superior occipital gyrus | HCs > Park+ HCs > Park− |
| 195 | 24.53 | <0.001 | −48 | −62 | −48 | L Cerebellum, Crus II | HCs > Park+ HCs > Park− |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Piervincenzi, C.; Fanella, M.; Petsas, N.; Frascarelli, M.; Morano, A.; Accinni, T.; Di Fabio, F.; Di Bonaventura, C.; Berardelli, A.; Pantano, P. Structural Cerebellar Abnormalities and Parkinsonism in Patients with 22q11.2 Deletion Syndrome. Brain Sci. 2022, 12, 1533. https://doi.org/10.3390/brainsci12111533
Piervincenzi C, Fanella M, Petsas N, Frascarelli M, Morano A, Accinni T, Di Fabio F, Di Bonaventura C, Berardelli A, Pantano P. Structural Cerebellar Abnormalities and Parkinsonism in Patients with 22q11.2 Deletion Syndrome. Brain Sciences. 2022; 12(11):1533. https://doi.org/10.3390/brainsci12111533
Chicago/Turabian StylePiervincenzi, Claudia, Martina Fanella, Nikolaos Petsas, Marianna Frascarelli, Alessandra Morano, Tommaso Accinni, Fabio Di Fabio, Carlo Di Bonaventura, Alfredo Berardelli, and Patrizia Pantano. 2022. "Structural Cerebellar Abnormalities and Parkinsonism in Patients with 22q11.2 Deletion Syndrome" Brain Sciences 12, no. 11: 1533. https://doi.org/10.3390/brainsci12111533
APA StylePiervincenzi, C., Fanella, M., Petsas, N., Frascarelli, M., Morano, A., Accinni, T., Di Fabio, F., Di Bonaventura, C., Berardelli, A., & Pantano, P. (2022). Structural Cerebellar Abnormalities and Parkinsonism in Patients with 22q11.2 Deletion Syndrome. Brain Sciences, 12(11), 1533. https://doi.org/10.3390/brainsci12111533






