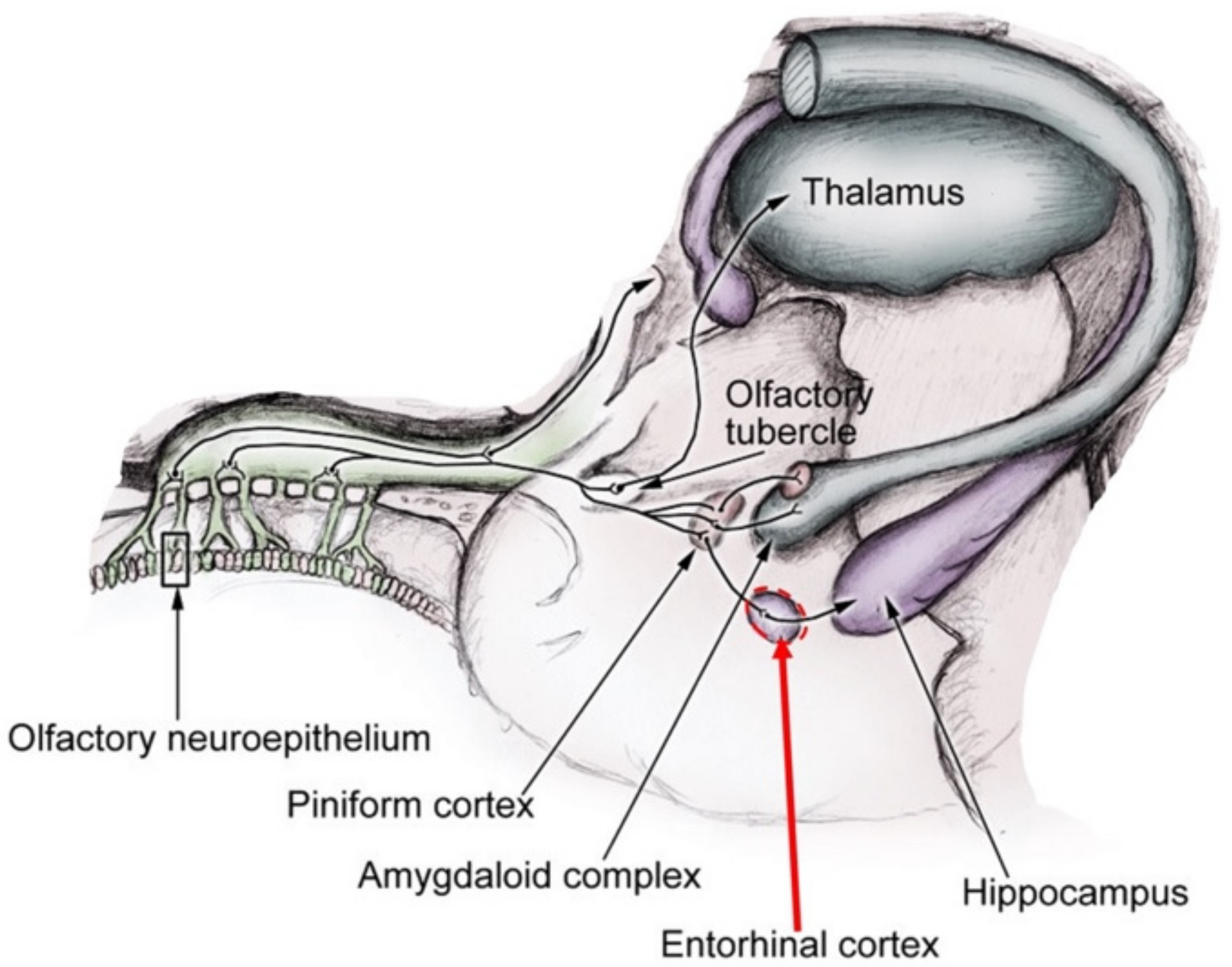
Entorhinal Cortex and Persistent Olfactory Loss in COVID-19 Patients: A Neuroanatomical Hypothesis. Comment on Fiorentino et al. Correlations between Persistent Olfactory and Semantic Memory Disorders after SARS-CoV-2 Infection. Brain Sci. 2022, 12, 714
Author Contributions
Funding
Conflicts of Interest
References
- Fiorentino, J.; Payne, M.; Cancian, E.; Plonka, A.; Dumas, L.-É.; Chirio, D.; Demonchy, É.; Risso, K.; Askenazy-Gittard, F.; Guevara, N.; et al. Correlations between Persistent Olfactory and Semantic Memory Disorders after SARS-CoV-2 Infection. Brain Sci. 2022, 12, 714. [Google Scholar] [CrossRef] [PubMed]
- Di Stadio, A.; Brenner, M.J.; De Luca, P.; Albanese, M.; D’Ascanio, L.; Ralli, M.; Roccamatisi, D.; Cingolani, C.; Vitelli, F.; Camaioni, A.; et al. Olfactory Dysfunction, Headache, and Mental Clouding in Adults with Long-COVID-19: What Is the Link between Cognition and Olfaction? A Cross-Sectional Study. Brain Sci. 2022, 12, 154. [Google Scholar] [CrossRef] [PubMed]
- Schwabenland, M.; Salié, H.; Tanevski, J.; Killmer, S.; Lago, M.S.; Schlaak, A.E.; Mayer, L.; Matschke, J.; Püschel, K.; Fitzek, A.; et al. Deep spatial profiling of human COVID-19 brains reveals neuroinflammation with distinct microanatomical microglia-T-cell interactions. Immunity 2021, 54, 1594–1610. [Google Scholar] [CrossRef] [PubMed]
- Poloni, T.E.; Medici, V.; Moretti, M.; Visonà, S.D.; Cirrincione, A.; Carlos, A.F.; Davin, A.; Gagliardi, S.; Pansarasa, O.; Cereda, C.; et al. COVID-19-related neuropathology and microglial activation in elderly with and without dementia. Brain Pathol. 2021, 31, e12997. [Google Scholar] [CrossRef] [PubMed]
- De Luca, P.; Scarpa, A.; Ralli, M.; Tassone, D.; Simone, M.; De Campora, L.; Cassandro, C.; Di Stadio, A. Auditory Disturbances and SARS-CoV-2 Infection: Brain Inflammation or Cochlear Affection? Systematic Review and Discussion of Potential Pathogenesis. Front. Neurol. 2021, 12, 1234. [Google Scholar] [CrossRef]
- Amin-Chowdhury, Z.; Harris, R.J.; Aiano, F.; Zavala, M.; Bertran, M.; Borrow, R.; Linley, E.; Ahmad, S.; Parker, B.; Horsley, A.; et al. Characterising post-COVID syndrome more than 6 months after acute infection in adults; prospective longitudinal cohort study, England. medRxiv 2021. [Google Scholar] [CrossRef]
- Buonsenso, D.; Munblit, D.; De Rose, C.; Sinatti, D.; Ricchiuto, A.; Carfi, A.; Valentini, P. Preliminary evidence on long COVID in children. Acta Paediatr. 2021, 110, 2208–2211. [Google Scholar] [CrossRef]
- Cirulli, E.T.; Barrett, K.M.S.; Riffle, S.; Bolze, A.; Neveux, I.; Dabe, S.; Grzymski, J.J.; Lu, J.T.; Washington, N.L. Long-term COVID-19 symptoms in a large unselected population. medrxiv 2020. [Google Scholar] [CrossRef]
- Woo, M.S.; Malsy, J.; Pöttgen, J.; Zai, S.S.; Ufer, F.; Hadjilaou, A.; Schmiedel, S.; Addo, M.M.; Gerloff, C.; Heesen, C.; et al. Frequent neurocognitive deficits after recovery from mild COVID-19. Brain Commun. 2020, 2, fcaa205. [Google Scholar] [CrossRef]
- Di Stadio, A.; D’Ascanio, L.; De Luca, P.; Roccamatisi, D.; La Mantia, I.; Brenner, M.J. Hyperosmia after COVID-19: Hedonic perception or hypersensitivity? Eur. Rev. Med. Pharmacol. Sci. 2022, 26, 2196–2200. [Google Scholar] [CrossRef]
- Porcherot, C.; Delplanque, S.; Raviot-Derrien, S.; Le Calvé, B.; Chrea, C.; Gaudreau, N.; Cayeux, I. How do you feel when you smell this? Optimization of a verbal measurement of odor-elicited emotions. Food Qual. Prefer. 2010, 21, 938–947. [Google Scholar] [CrossRef]
- Leichnetz, G.; Astruc, J. The squirrel monkey entorhinal cortex: Architecture and medial frontal afferents. Brain Res. Bull. 1976, 1, 351–358. [Google Scholar] [CrossRef]
- Insausti, R. Comparative anatomy of the entorhinal cortex and hippocampus in mammals. Hippocampus 1993, 3, 19–26. [Google Scholar] [CrossRef]
- Witter, M.P.; Doan, T.P.; Jacobsen, B.; Nilssen, E.S.; Ohara, S. Architecture of the Entorhinal Cortex A Review of Entorhinal Anatomy in Rodents with Some Comparative Notes. Front. Syst. Neurosci. 2017, 11, 46. [Google Scholar] [CrossRef]
- Wilson, D.A.; Xu, W.; Sadrian, B.; Courtiol, E.; Cohen, Y.; Barnes, D.C. Cortical Odor Processing in Health and Disease. Prog. Brain Res. 2014, 208, 275–305. [Google Scholar] [CrossRef] [Green Version]
- Chapuis, J.; Cohen, Y.; He, X.; Zhang, Z.; Jin, S.; Xu, F.; Wilson, N.A. Lateral Entorhinal Modulation of Piriform Cortical Activity and Fine Odor Discrimination. J. Neurosci. 2013, 33, 13449–13459. [Google Scholar] [CrossRef] [Green Version]
- Khan, U.A.; Liu, L.; Provenzano, F.A.; Berman, D.E.; Profaci, C.; Sloan, R.P.; Mayeux, R.; Duff, K.; Small, S.A. Molecular drivers and cortical spread of lateral entorhinal cortex dysfunction in preclinical Alzheimer’s disease. Nat. Neurosci. 2013, 17, 304–311. [Google Scholar] [CrossRef] [Green Version]
- Leitner, F.C.; Melzer, S.; Lütcke, H.; Pinna, R.; Seeburg, P.H.; Helmchen, F.; Monyer, H. Spatially segregated feedforward and feed-back neurons support differential odor processing in the lateral entorhinal cortex. Nat. Neurosci. 2016, 19, 935–944. [Google Scholar] [CrossRef]
- Douaud, G.; Lee, S.; Alfaro-Almagro, F.; Arthofer, C.; Wang, C.; McCarthy, P.; Lange, F.; Andersson, J.L.R.; Griffanti, L.; Duff, E.; et al. SARS-CoV-2 is associated with changes in brain structure in UK Biobank. Nature 2022, 604, 697–707. [Google Scholar] [CrossRef]
- Brann, D.H.; Tsukahara, T.; Weinreb, C.; Lipovsek, M.; Van Den Berge, K.; Gong, B.; Chance, R.; Macaulay, I.C.; Chou, H.-J.; Fletcher, R.B.; et al. Non-neuronal expression of SARS-CoV-2 entry genes in the olfactory system suggests mechanisms underlying COVID-19-associated anosmia. Sci. Adv. 2020, 6, eabc5801. [Google Scholar] [CrossRef]
- Pennanen, C.; Kivipelto, M.; Tuomainen, S.; Hartikainen, P.; Hänninen, T.; Laakso, M.; Hallikainen, M.; Vanhanen, M.; Nissinen, A.; Helkala, E.-L.; et al. Hippocampus and entorhinal cortex in mild cognitive impairment and early AD. Neurobiol. Aging 2004, 25, 303–310. [Google Scholar] [CrossRef]
- Varon, D.; Loewenstein, D.A.; Potter, E.; Greig, M.T.; Agron, J.; Shen, Q.; Zhao, W.; Celeste Ramirez, M.; Santos, I.; Barker, W.; et al. Minimal atrophy of the entorhinal cortex and hippocampus: Progression of cogni-tive impairment. Dement. Geriatr. Cogn. Disord. 2011, 31, 276–283. [Google Scholar] [CrossRef] [Green Version]
- Di Stadio, A.; Bernitsas, E.; Ralli, M.; Severini, C.; Brenner, M.J.; Angelini, C. OAS1 gene, Spike protein variants and persistent COVID-19-related anosmia: May the olfactory disfunction be a harbinger of future neurodegenerative disease? Eur. Rev. Med. Pharmacol. Sci. 2022, 26, 347–349. [Google Scholar]
- Di Stadio, A.; D’Ascanio, L.; Vaira, L.A.; Cantone, E.; De Luca, P.; Cingolani, C.; Motta, G.; De Riu, G.; Vitelli, F.; Spriano, G.; et al. Ultramicronized Palmitoylethanolamide and Luteolin Supplement Combined with Olfactory Training to Treat Post-COVID-19 Olfactory Impairment: A Multi-Center Double-Blinded Randomized Placebo-Controlled Clinical Trial. Curr. Neuropharmacol. 2022. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
De Luca, P.; Marra, P.; La Mantia, I.; Salzano, F.A.; Camaioni, A.; Di Stadio, A. Entorhinal Cortex and Persistent Olfactory Loss in COVID-19 Patients: A Neuroanatomical Hypothesis. Comment on Fiorentino et al. Correlations between Persistent Olfactory and Semantic Memory Disorders after SARS-CoV-2 Infection. Brain Sci. 2022, 12, 714. Brain Sci. 2022, 12, 850. https://doi.org/10.3390/brainsci12070850
De Luca P, Marra P, La Mantia I, Salzano FA, Camaioni A, Di Stadio A. Entorhinal Cortex and Persistent Olfactory Loss in COVID-19 Patients: A Neuroanatomical Hypothesis. Comment on Fiorentino et al. Correlations between Persistent Olfactory and Semantic Memory Disorders after SARS-CoV-2 Infection. Brain Sci. 2022, 12, 714. Brain Sciences. 2022; 12(7):850. https://doi.org/10.3390/brainsci12070850
Chicago/Turabian StyleDe Luca, Pietro, Pasquale Marra, Ignazio La Mantia, Francesco Antonio Salzano, Angelo Camaioni, and Arianna Di Stadio. 2022. "Entorhinal Cortex and Persistent Olfactory Loss in COVID-19 Patients: A Neuroanatomical Hypothesis. Comment on Fiorentino et al. Correlations between Persistent Olfactory and Semantic Memory Disorders after SARS-CoV-2 Infection. Brain Sci. 2022, 12, 714" Brain Sciences 12, no. 7: 850. https://doi.org/10.3390/brainsci12070850
APA StyleDe Luca, P., Marra, P., La Mantia, I., Salzano, F. A., Camaioni, A., & Di Stadio, A. (2022). Entorhinal Cortex and Persistent Olfactory Loss in COVID-19 Patients: A Neuroanatomical Hypothesis. Comment on Fiorentino et al. Correlations between Persistent Olfactory and Semantic Memory Disorders after SARS-CoV-2 Infection. Brain Sci. 2022, 12, 714. Brain Sciences, 12(7), 850. https://doi.org/10.3390/brainsci12070850








