A Systematic Review of Treatment Outcome Predictors in Deep Brain Stimulation for Refractory Obsessive-Compulsive Disorder
Abstract
:1. Introduction
2. Methods
3. Results
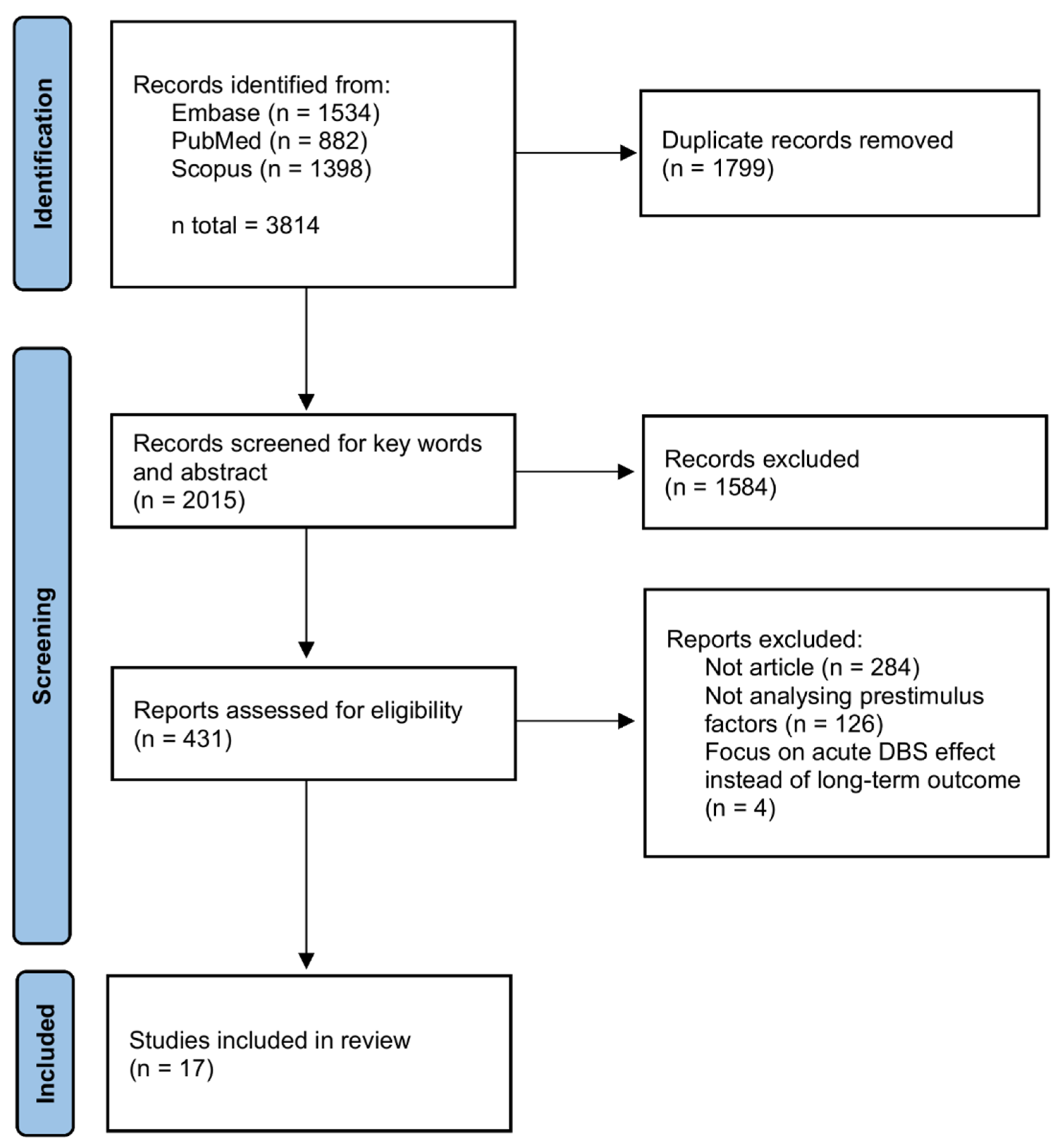
3.1. Study Selection
3.2. Main Characteristics
3.3. Outcome Predictors
3.3.1. Neuroimaging Data
3.3.2. Neural Activities
3.3.3. Clinical and Demographic Data
| # | Authors | Participants | Baseline Y-BOCS Scores | Last Follow-Up Date (Month) | Y-BOCS Reduction | Response Rate |
|---|---|---|---|---|---|---|
| 1 | Raymaekers, S., et al. [32] | 24 | 30~40 | 76.5 ± 44.85 | 5~95%, 45% for median 1 | 67% 2 |
| 2 | Mallet, L., et al. [46] | 14 | 31~36 | 46 3 | 19~86%, mean 51.2% | 75% |
| 3 | Graat, I., et al. [29] | 70 | 34 ± 3 | 12 | 13.5 ± 9.4 | 69% |
| 4 | de Koning, P.P., et al. [47] | 15 | 33.1 ± 3.4 | >12 | 17 ± 6.0 | 66.7% |
| 5 | Haq, I.U., et al. [48] | 6 | 33.2 ± 2.1 | 24 | 12.5 ± 11.3 | 66.7% |
| 6 | Schüller, T., et al. [43] | 17 4 | 25~37 | 12 | 33.33 ± 21.5% | 75% |
| 7 | Welter, M.L., et al. [45] | 12 | 31.8 ± 3.1 | 10 | 19.5 ± 9.5 5 | 41.7% |
| 8 | Hartmann, C.J., et al. [37] | 6 | 31~37 | 24 | −3~86% | 66.7% |
| 9 | Baldermann, J.C., et al. [35] | 22 | 31.3 ± 4.3 | 12 | 30.4 ± 20.1% | 63.6% |
| 10 | Li, N., et al. [34] | ALIC: 22 STN: 14 NAc: 8 6 Combined: 6 | ALIC: 31.3 ± 4.4 STN: 33.4 ± 3.7 NAc: 30 ± 7.75 Combined: 36.2 ± 1.8 | ALIC: 12 STN: 12 NAc: 3 Combined: optimized | ALIC: 31.0 ± 20.5% STN: 41.2 ± 31.7% NAc: 47.8 ± 23% Combined: 50.0 ± 12.6% | ALIC: 63.6% STN: 57.1% NAc: not mentioned Combined: 100% |
| 11 | van der Vlis, T., et al. [36] | 8 | 33.12 ± 3.34 | 10~74 | 10.5 ± 7.6 | 63% |
| 12 | Mosley, P.E., et al. [39] | 9 | 32.7 ± 2.6 | 12 | 17.4 ± 2.0 7 | 88.9% |
| 13 | Chen, X., et al. [38] | 11 | 28.5 ± 6.3 8 | 12 | 21.5 ± 6.7 | Not mentioned |
| 14 | Widge, A.S., et al. [41] | 8 | 28~35 | 2~4 | Not mentioned | 62.5% 9 |
| 15 | Liebrand, L.C., et al. [30] | 12 | 32.7 ± 4.1 | 12 | 14.2 ± 9.5 | 62.5% |
| 16 | Germann, J., et al. [40] | 5 | 33~38 | 12 | 39.4~72.7% | 100% |
| 17 | Sildatke, E., et al. [42] | 15 | 29.4 ± 5.4 | 6 or 12 | −54~35% | 33.3% 10 |
| # | Authors | Published Date | DBS Targets | Analyzed Factors | Main Results |
|---|---|---|---|---|---|
| 1 | Raymaekers, S., et al. [32] | 2017 | ALIC/BNST 1 | Clinical characteristics | The BDI at baseline was the only predictor inversely related to the evolution of the Y-BOCS |
| 2 | Mallet, L., et al. [46] | 2019 | STN | Clinical and demographic characteristics | A significant positive relationship between post-surgery OCD severity and the age at onset. |
| 3 | Graat, I., et al. [29] | 2021 | ALIC/NAc 2 | Clinical and demographic characteristics | Insight into illness was a significant predictor of response. |
| 4 | de Koning, P.P., et al. [47] | 2016 | ALIC/NAc | Neuroendocrine hormones 3 | No significant correlation between clinical symptoms and neuroendocrine outcomes. |
| 5 | Haq, I.U., et al. [48] | 2011 | ALIC/NAc | Induced laugh condition | Larger percentage of laugh conditions for individual patients correlated with greater reduction in YBOCS at 24-month follow-up |
| 6 | Schüller, T., et al. [43] | 2021 | ALIC/NAc | EEG | No significant correlation between medial frontal cortex theta modulations and DBS-induced symptom change |
| 7 | Sildatke, E., et al. [42] | 2022 | ALIC/NAc | EEG | Larger error-related negativity amplitude was correlated with attenuated symptom improvement. |
| 8 | Welter, M.L., et al. [45] | 2011 | STN | Local neural activity | Y-BOCS improvement was significantly correlated with STN neuronal activities. |
| 9 | Hartmann, C.J., et al. [37] | 2016 | ALIC/NAc | DTI | Modulation of the right dorsolateral prefrontal cortex was associated with an excellent response. |
| 10 | Baldermann, J.C., et al. [35] | 2019 | ALIC/NAc | dMRI | A network was identified and was predictive of beneficial effects in DBS for OCD. |
| 11 | Li, N., et al. [34] | 2020 | ALIC/NAc, STN | dMRI | A bundle connected frontal regions to the STN was associated with clinical response in cohorts targeting either structure. |
| 12 | van der Vlis, T., et al. [36] | 2021 | VC/VS | dMRI | A subpart of the ALIC that connects PFC with the STN and medial nucleus of the thalamus is associated with optimal clinical response. |
| 13 | Mosley, P.E., et al. [39] | 2021 | NAc | dMRI | A right-hemispheric tract connected the BNST to the amygdala was associated with YBOCS reduction. |
| 14 | Chen, X., et al. [38] | 2021 | ALIC/NAc | fMRI | Presurgical communication at ventrolateral PFC could differentiate mood improvements of DBS. |
| 15 | Widge, A.S., et al. [41] | 2021 | VC/VS | dMRI | No tract could reliably predict clinical response or complications. |
| 16 | Liebrand, L.C., et al. [30] | 2019 | ALIC/NAc 2 | dMRI | Stimulation closer to the MFB was significantly correlated with better outcome. |
| 17 | Germann, J., et al. [40] | 2022 | ITP | fMRI and dMRI | A network composed of the bilateral amygdala and prefrontal region 24 and 46 was associated with symptom improvement. |
3.4. Quality Assessment
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ruscio, A.M.; Stein, D.J.; Chiu, W.T.; Kessler, R.C. The epidemiology of obsessive-compulsive disorder in the National Comorbidity Survey Replication. Mol. Psychiatry 2010, 15, 53–63. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bloch, M.H.; Green, C.; Kichuk, S.A.; Dombrowski, P.A.; Wasylink, S.; Billingslea, E.; Landeros-Weisenberger, A.; Kelmendi, B.; Goodman, W.K.; Leckman, J.F.; et al. Long-term outcome in adults with obsessive-compulsive disorder. Depress. Anxiety 2013, 30, 716–722. [Google Scholar] [CrossRef] [Green Version]
- Cherian, A.V.; Math, S.B.; Kandavel, T.; Reddy, Y.C.J. A 5-year prospective follow-up study of patients with obsessive-compulsive disorder treated with serotonin reuptake inhibitors. J. Affect. Disord. 2014, 152–154, 387–394. [Google Scholar] [CrossRef] [PubMed]
- Yang, W.; Tang, Z.; Wang, X.; Ma, X.; Cheng, Y.; Wang, B.; Sun, P.; Tang, W.; Luo, J.; Wang, C.; et al. The cost of obsessive-compulsive disorder (OCD) in China: A multi-center cross-sectional survey based on hospitals. Gen. Psychiatry 2021, 34, e100632. [Google Scholar] [CrossRef] [PubMed]
- Soomro, G.M.; Altman, D.; Rajagopal, S.; Oakley-Browne, M. Selective serotonin re-uptake inhibitors (SSRIs) versus placebo for obsessive compulsive disorder (OCD). Cochrane Database Syst. Rev. 2008, 2008, CD001765. [Google Scholar] [CrossRef] [PubMed]
- Skapinakis, P.; Caldwell, D.M.; Hollingworth, W.; Bryden, P.; Fineberg, N.A.; Salkovskis, P.; Welton, N.J.; Baxter, H.; Kessler, D.; Churchill, R.; et al. Pharmacological and psychotherapeutic interventions for management of obsessive-compulsive disorder in adults: A systematic review and network meta-analysis. Lancet Psychiatry 2016, 3, 730–739. [Google Scholar] [CrossRef] [Green Version]
- Del Casale, A.; Sorice, S.; Padovano, A.; Simmaco, M.; Ferracuti, S.; Lamis, D.A.; Rapinesi, C.; Sani, G.; Girardi, P.; Kotzalidis, G.D.; et al. Psychopharmacological Treatment of Obsessive-Compulsive Disorder (OCD). Curr. Neuropharmacol. 2019, 17, 710–736. [Google Scholar] [CrossRef]
- Beaulieu, A.M.; Tabasky, E.; Osser, D.N. The psychopharmacology algorithm project at the Harvard South Shore Program: An algorithm for adults with obsessive-compulsive disorder. Psychiatry Res. 2019, 281, 112583. [Google Scholar] [CrossRef]
- Thamby, A.; Jaisoorya, T.S. Antipsychotic augmentation in the treatment of obsessive-compulsive disorder. Indian J. Psychiatry 2019, 61, s51–s57. [Google Scholar] [CrossRef]
- Zhou, D.D.; Zhou, X.X.; Li, Y.; Zhang, K.F.; Lv, Z.; Chen, X.R.; Wan, L.Y.; Wang, W.; Wang, G.M.; Li, D.Q.; et al. Augmentation agents to serotonin reuptake inhibitors for treatment-resistant obsessive-compulsive disorder: A network meta-analysis. Prog. Neuropsychopharmacol. Biol. Psychiatry 2019, 90, 277–287. [Google Scholar] [CrossRef]
- Robbins, T.W.; Vaghi, M.M.; Banca, P. Obsessive-Compulsive Disorder: Puzzles and Prospects. Neuron 2019, 102, 27–47. [Google Scholar] [CrossRef] [PubMed]
- Kohl, S.; Baldermann, J.C. Progress and challenges in deep brain stimulation for obsessive-compulsive disorder. Pharmacol. Ther. 2018, 186, 168–175. [Google Scholar] [CrossRef] [PubMed]
- Alonso, P.; Cuadras, D.; Gabriëls, L.; Denys, D.; Goodman, W.; Greenberg, B.D.; Jimenez-Ponce, F.; Kuhn, J.; Lenartz, D.; Mallet, L.; et al. Deep Brain Stimulation for Obsessive-Compulsive Disorder: A Meta-Analysis of Treatment Outcome and Predictors of Response. PLoS ONE 2015, 10, e0133591. [Google Scholar] [CrossRef] [Green Version]
- Haber, S.N.; Yendiki, A.; Jbabdi, S. Four Deep Brain Stimulation Targets for Obsessive-Compulsive Disorder: Are They Different? Biol. Psychiatry 2021, 90, 667–677. [Google Scholar] [CrossRef]
- Kisely, S.; Hall, K.; Siskind, D.; Frater, J.; Olson, S.; Crompton, D. Deep brain stimulation for obsessive-compulsive disorder: A systematic review and meta-analysis. Psychol. Med. 2014, 44, 3533–3542. [Google Scholar] [CrossRef]
- Martinho, F.P.; Duarte, G.S.; Couto, F.S.D. Efficacy, Effect on Mood Symptoms, and Safety of Deep Brain Stimulation in Refractory Obsessive-Compulsive Disorder: A Systematic Review and Meta-Analysis. J. Clin. Psychiatry 2020, 81, 19r12821. [Google Scholar] [CrossRef] [PubMed]
- Holland, M.T.; Trapp, N.T.; McCormick, L.M.; Jareczek, F.J.; Zanaty, M.; Close, L.N.; Beeghly, J.; Greenlee, J.D.W. Deep Brain Stimulation for Obsessive-Compulsive Disorder: A Long Term Naturalistic Follow Up Study in a Single Institution. Front. Psychiatry 2020, 11, 55. [Google Scholar] [CrossRef] [PubMed]
- Steketee, G.; Siev, J.; Yovel, I.; Lit, K.; Wilhelm, S. Predictors and Moderators of Cognitive and Behavioral Therapy Outcomes for OCD: A Patient-Level Mega-Analysis of Eight Sites. Behav. Ther. 2019, 50, 165–176. [Google Scholar] [CrossRef] [PubMed]
- Olatunji, B.O.; Davis, M.L.; Powers, M.B.; Smits, J.A. Cognitive-behavioral therapy for obsessive-compulsive disorder: A meta-analysis of treatment outcome and moderators. J. Psychiatr. Res. 2013, 47, 33–41. [Google Scholar] [CrossRef] [PubMed]
- Carey, P.D.; Lochner, C.; Kidd, M.; Van Ameringen, M.; Stein, D.J.; Denys, D. Quetiapine augmentation of serotonin reuptake inhibitors in treatment-refractory obsessive-compulsive disorder: Is response to treatment predictable? Int. Clin. Psychopharmacol. 2012, 27, 321–325. [Google Scholar] [CrossRef]
- Vieira, E.V.; Arantes, P.R.; Hamani, C.; Iglesio, R.; Duarte, K.P.; Teixeira, M.J.; Miguel, E.C.; Lopes, A.C.; Godinho, F. Neurocircuitry of Deep Brain Stimulation for Obsessive-Compulsive Disorder as Revealed by Tractography: A Systematic Review. Front. Psychiatry 2021, 12, 680484. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- NIH. Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies. National Heart, Lung, and Blood Institute. Available online: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (accessed on 23 May 2022).
- Dougherty, D.D.; Chou, T.; Corse, A.K.; Arulpragasam, A.R.; Widge, A.S.; Cusin, C.; Evans, K.C.; Greenberg, B.D.; Haber, S.N.; Deckersbach, T. Acute deep brain stimulation changes in regional cerebral blood flow in obsessive-compulsive disorder. J. Neurosurg. 2016, 125, 1087–1093. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tsai, H.C.; Chang, C.H.; Pan, J.I.; Hsieh, H.J.; Tsai, S.T.; Hung, H.Y.; Chen, S.Y. Acute stimulation effect of the ventral capsule/ventral striatum in patients with refractory obsessive-compulsive disorder—A double-blinded trial. Neuropsychiatr. Dis. Treat. 2014, 10, 63–69. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Winter, L.; Heitland, I.; Saryyeva, A.; Lütjens, G.; Schwabe, K.; Heissler, H.E.; Alam, M.; Kahl, K.G.; Krauss, J.K. Acute Effects of Electrical Stimulation of the Bed Nucleus of the Stria Terminalis/Internal Capsule in Obsessive-Compulsive Disorder. World Neurosurg. 2018, 111, e471–e477. [Google Scholar] [CrossRef] [PubMed]
- Rauch, S.L.; Dougherty, D.D.; Malone, D.; Rezai, A.; Friehs, G.; Fischman, A.J.; Alpert, N.M.; Haber, S.N.; Stypulkowski, P.H.; Rise, M.T.; et al. A functional neuroimaging investigation of deep brain stimulation in patients with obsessive-compulsive disorder. J. Neurosurg. 2006, 104, 558–565. [Google Scholar] [CrossRef] [PubMed]
- Graat, I.; Mocking, R.; Figee, M.; Vulink, N.; de Koning, P.; Ooms, P.; Mantione, M.; van den Munckhof, P.; Schuurman, R.; Denys, D. Long-term Outcome of Deep Brain Stimulation of the Ventral Part of the Anterior Limb of the Internal Capsule in a Cohort of 50 Patients With Treatment-Refractory Obsessive-Compulsive Disorder. Biol. Psychiatry 2021, 90, 714–720. [Google Scholar] [CrossRef]
- Graat, I.; Mocking, R.J.T.; de Koning, P.; Vulink, N.; Figee, M.; van den Munckhof, P.; Schuurman, P.R.; Denys, D. Predicting Response to vALIC Deep Brain Stimulation for Refractory Obsessive-Compulsive Disorder. J. Clin. Psychiatry 2021, 82, 37759. [Google Scholar] [CrossRef]
- Liebrand, L.C.; Caan, M.W.A.; Schuurman, P.R.; van den Munckhof, P.; Figee, M.; Denys, D.; van Wingen, G.A. Individual white matter bundle trajectories are associated with deep brain stimulation response in obsessive-compulsive disorder. Brain Stimul. 2019, 12, 353–360. [Google Scholar] [CrossRef] [Green Version]
- Huys, D.; Kohl, S.; Baldermann, J.C.; Timmermann, L.; Sturm, V.; Visser-Vandewalle, V.; Kuhn, J. Open-label trial of anterior limb of internal capsule-nucleus accumbens deep brain stimulation for obsessive-compulsive disorder: Insights gained. J. Neurol. Neurosurg. Psychiatry 2019, 90, 805–812. [Google Scholar] [CrossRef]
- Raymaekers, S.; Vansteelandt, K.; Luyten, L.; Bervoets, C.; Demyttenaere, K.; Gabriëls, L.; Nuttin, B. Long-term electrical stimulation of bed nucleus of stria terminalis for obsessive-compulsive disorder. Mol. Psychiatry 2017, 22, 931–934. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Luyten, L.; Hendrickx, S.; Raymaekers, S.; Gabriëls, L.; Nuttin, B. Electrical stimulation in the bed nucleus of the stria terminalis alleviates severe obsessive-compulsive disorder. Mol. Psychiatry 2016, 21, 1272–1280. [Google Scholar] [CrossRef] [PubMed]
- Li, N.; Baldermann, J.C.; Kibleur, A.; Treu, S.; Akram, H.; Elias, G.J.B.; Boutet, A.; Lozano, A.M.; Al-Fatly, B.; Strange, B.; et al. A unified connectomic target for deep brain stimulation in obsessive-compulsive disorder. Nat. Commun. 2020, 11, 3364. [Google Scholar] [CrossRef] [PubMed]
- Baldermann, J.C.; Melzer, C.; Zapf, A.; Kohl, S.; Timmermann, L.; Tittgemeyer, M.; Huys, D.; Visser-Vandewalle, V.; Kühn, A.A.; Horn, A.; et al. Connectivity Profile Predictive of Effective Deep Brain Stimulation in Obsessive-Compulsive Disorder. Biol. Psychiatry 2019, 85, 735–743. [Google Scholar] [CrossRef]
- van der Vlis, T.; Ackermans, L.; Mulders, A.E.P.; Vrij, C.A.; Schruers, K.; Temel, Y.; Duits, A.; Leentjens, A.F.G. Ventral Capsule/Ventral Striatum Stimulation in Obsessive-Compulsive Disorder: Toward a Unified Connectomic Target for Deep Brain Stimulation? Neuromodulation 2021, 24, 316–323. [Google Scholar] [CrossRef]
- Hartmann, C.J.; Lujan, J.L.; Chaturvedi, A.; Goodman, W.K.; Okun, M.S.; McIntyre, C.C.; Haq, I.U. Tractography activation patterns in dorsolateral prefrontal cortex suggest better clinical responses in OCD DBS. Front. Neurosci. 2016, 9, 519. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, X.; Wang, Z.; Lv, Q.; Lv, Q.; van Wingen, G.; Fridgeirsson, E.A.; Denys, D.; Voon, V.; Wang, Z. Common and differential connectivity profiles of deep brain stimulation and capsulotomy in refractory obsessive-compulsive disorder. Mol. Psychiatry 2021, 27, 1020–1030. [Google Scholar] [CrossRef] [PubMed]
- Mosley, P.E.; Windels, F.; Morris, J.; Coyne, T.; Marsh, R.; Giorni, A.; Mohan, A.; Sachdev, P.; O’Leary, E.; Boschen, M.; et al. A randomised, double-blind, sham-controlled trial of deep brain stimulation of the bed nucleus of the stria terminalis for treatment-resistant obsessive-compulsive disorder. Transl. Psychiatry 2021, 11, 190. [Google Scholar] [CrossRef]
- Germann, J.; Boutet, A.; Elias, G.J.B.; Gouveia, F.V.; Loh, A.; Giacobbe, P.; Bhat, V.; Kucharczyk, W.; Lozano, A.M. Brain Structures and Networks Underlying Treatment Response to Deep Brain Stimulation Targeting the Inferior Thalamic Peduncle in Obsessive-Compulsive Disorder. Stereotact. Funct. Neurosurg. 2022, 1–8. [Google Scholar] [CrossRef]
- Widge, A.S.; Zhang, F.; Gosai, A.; Papadimitrou, G.; Wilson-Braun, P.; Tsintou, M.; Palanivelu, S.; Noecker, A.M.; McIntyre, C.C.; O’Donnell, L.; et al. Patient-specific connectomic models correlate with, but do not reliably predict, outcomes in deep brain stimulation for obsessive-compulsive disorder. Neuropsychopharmacology 2021, 47, 965–972. [Google Scholar] [CrossRef] [PubMed]
- Sildatke, E.; Gruendler, T.O.J.; Ullsperger, M.; Dembek, T.A.; Baldermann, J.C.; Kohl, S.; Visser-Vandewalle, V.; Huys, D.; Kuhn, J.; Schüller, T. Deep Brain Stimulation Reduces Conflict-Related Theta and Error-Related Negativity in Patients with Obsessive-Compulsive Disorder. Neuromodulation 2022, 25, 245–252. [Google Scholar] [CrossRef] [PubMed]
- Schüller, T.; Gruendler, T.O.J.; Smith, E.E.; Baldermann, J.C.; Kohl, S.; Fischer, A.G.; Visser-Vandewalle, V.; Ullsperger, M.; Kuhn, J.; Huys, D. Performance monitoring in obsessive-compulsive disorder: Insights from internal capsule/nucleus accumbens deep brain stimulation. Neuroimage Clin. 2021, 31, 102746. [Google Scholar] [CrossRef]
- Rappel, P.; Marmor, O.; Bick, A.S.; Arkadir, D.; Linetsky, E.; Castrioto, A.; Tamir, I.; Freedman, S.A.; Mevorach, T.; Gilad, M.; et al. Subthalamic theta activity: A novel human subcortical biomarker for obsessive compulsive disorder. Transl. Psychiatry 2018, 8, 118. [Google Scholar] [CrossRef]
- Welter, M.L.; Burbaud, P.; Fernandez-Vidal, S.; Bardinet, E.; Coste, J.; Piallat, B.; Borg, M.; Besnard, S.; Sauleau, P.; Devaux, B.; et al. Basal ganglia dysfunction in OCD: Subthalamic neuronal activity correlates with symptoms severity and predicts high-frequency stimulation efficacy. Transl. Psychiatry 2011, 1, e5. [Google Scholar] [CrossRef]
- Mallet, L.; Du Montcel, S.T.; Clair, A.H.; Arbus, C.; Bardinet, E.; Baup, N.; Chabardès, S.; Chéreau, I.; Czernecki, V.; Fontaine, D.; et al. Long-term effects of subthalamic stimulation in Obsessive-Compulsive Disorder: Follow-up of a randomized controlled trial. Brain Stimul. 2019, 12, 1080–1082. [Google Scholar] [CrossRef] [Green Version]
- de Koning, P.P.; Figee, M.; Endert, E.; van den Munckhof, P.; Schuurman, P.R.; Storosum, J.G.; Denys, D.; Fliers, E. Rapid effects of deep brain stimulation reactivation on symptoms and neuroendocrine parameters in obsessive-compulsive disorder. Transl. Psychiatry 2016, 6, e722. [Google Scholar] [CrossRef] [Green Version]
- Haq, I.U.; Foote, K.D.; Goodman, W.G.; Wu, S.S.; Sudhyadhom, A.; Ricciuti, N.; Siddiqui, M.S.; Bowers, D.; Jacobson, C.E.; Ward, H.; et al. Smile and laughter induction and intraoperative predictors of response to deep brain stimulation for obsessive-compulsive disorder. Neuroimage 2011, 54, S247–S255. [Google Scholar] [CrossRef] [Green Version]
- Sheth, S.A.; Goodman, W. Connectomic approaches to deep brain stimulation for OCD. Neuropsychopharmacology 2022, 47, 801–802. [Google Scholar] [CrossRef]
- Senova, S.; Clair, A.H.; Palfi, S.; Yelnik, J.; Domenech, P.; Mallet, L. Deep Brain Stimulation for Refractory Obsessive-Compulsive Disorder: Towards an Individualized Approach. Front. Psychiatry 2019, 10, 905. [Google Scholar] [CrossRef]
- Bragdon, L.B.; Gibb, B.E.; Coles, M.E. Does neuropsychological performance in OCD relate to different symptoms? A meta-analysis comparing the symmetry and obsessing dimensions. Depress. Anxiety 2018, 35, 761–774. [Google Scholar] [CrossRef]
- Nakao, T.; Okada, K.; Kanba, S. Neurobiological model of obsessive-compulsive disorder: Evidence from recent neuropsychological and neuroimaging findings. Psychiatry Clin. Neurosci. 2014, 68, 587–605. [Google Scholar] [CrossRef] [PubMed]
- Via, E.; Cardoner, N.; Pujol, J.; Alonso, P.; López-Solà, M.; Real, E.; Contreras-Rodríguez, O.; Deus, J.; Segalàs, C.; Menchón, J.M.; et al. Amygdala activation and symptom dimensions in obsessive-compulsive disorder. Br. J. Psychiatry 2014, 204, 61–68. [Google Scholar] [CrossRef] [Green Version]
- Menzies, L.; Chamberlain, S.R.; Laird, A.R.; Thelen, S.M.; Sahakian, B.J.; Bullmore, E.T. Integrating evidence from neuroimaging and neuropsychological studies of obsessive-compulsive disorder: The orbitofronto-striatal model revisited. Neurosci. Biobehav. Rev. 2008, 32, 525–549. [Google Scholar] [CrossRef] [Green Version]
- Barcia, J.A.; Reyes, L.; Arza, R.; Saceda, J.; Avecillas, J.; Yáñez, R.; García-Albea, J.; Ortiz, T.; López-Ibor, M.I.; López-Ibor, J.J. The search for an individualized target in deep brain stimulation for obsessive-compulsive disease: Is the side relevant? Stereotact. Funct. Neurosurg. 2012, 90, 170. [Google Scholar] [CrossRef]
- Barcia, J.A.; Avecillas-Chasín, J.M.; Nombela, C.; Arza, R.; García-Albea, J.; Pineda-Pardo, J.A.; Reneses, B.; Strange, B.A. Personalized striatal targets for deep brain stimulation in obsessive-compulsive disorder. Brain Stimul. 2019, 12, 724–734. [Google Scholar] [CrossRef]
- Coenen, V.A.; Schlaepfer, T.E.; Varkuti, B.; Schuurman, P.R.; Reinacher, P.C.; Voges, J.; Zrinzo, L.; Blomstedt, P.; Fenoy, A.J.; Hariz, M. Surgical decision making for deep brain stimulation should not be based on aggregated normative data mining. Brain Stimul. 2019, 12, 1345–1348. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thomas, C.; Ye, F.Q.; Irfanoglu, M.O.; Modi, P.; Saleem, K.S.; Leopold, D.A.; Pierpaoli, C. Anatomical accuracy of brain connections derived from diffusion MRI tractography is inherently limited. Proc. Natl. Acad. Sci. USA 2014, 111, 16574–16579. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Corroenne, R.; Arthuis, C.; Kasprian, G.; Mahallati, H.; Ville, Y.; Millischer Bellaiche, A.E.; Henry, C.; Grevent, D.; Salomon, L.J. Diffusion tensor imaging in fetal brain: Review to understand principles, potential and limitations of promising technique. Ultrasound Obstet. Gynecol. 2022. [Google Scholar] [CrossRef] [PubMed]
- Haber, S.N.; Tang, W.; Choi, E.Y.; Yendiki, A.; Liu, H.; Jbabdi, S.; Versace, A.; Phillips, M. Circuits, Networks, and Neuropsychiatric Disease: Transitioning From Anatomy to Imaging. Biol. Psychiatry 2020, 87, 318–327. [Google Scholar] [CrossRef]
- Tagliati, M.; Jankovic, J.; Pagan, F.; Susatia, F.; Isaias, I.U.; Okun, M.S. Safety of MRI in patients with implanted deep brain stimulation devices. Neuroimage 2009, 47 (Suppl. S2), T53–T57. [Google Scholar] [CrossRef]
- Boutet, A.; Chow, C.T.; Narang, K.; Elias, G.J.B.; Neudorfer, C.; Germann, J.; Ranjan, M.; Loh, A.; Martin, A.J.; Kucharczyk, W.; et al. Improving Safety of MRI in Patients with Deep Brain Stimulation Devices. Radiology 2020, 296, 250–262. [Google Scholar] [CrossRef] [PubMed]
- Boutet, A.; Rashid, T.; Hancu, I.; Elias, G.J.B.; Gramer, R.M.; Germann, J.; Dimarzio, M.; Li, B.; Paramanandam, V.; Prasad, S.; et al. Functional MRI Safety and Artifacts during Deep Brain Stimulation: Experience in 102 Patients. Radiology 2019, 293, 174–183. [Google Scholar] [CrossRef] [PubMed]
- Smith, E.E.; Schüller, T.; Huys, D.; Baldermann, J.C.; Andrade, P.; Allen, J.J.B.; Visser-Vandewalle, V.; Ullsperger, M.; Gruendler, T.O.J.; Kuhn, J. A brief demonstration of frontostriatal connectivity in OCD patients with intracranial electrodes. Neuroimage 2020, 220, 117138. [Google Scholar] [CrossRef]
- Xiong, B.; Wen, R.; Gao, Y.; Wang, W. Longitudinal Changes of Local Field Potential Oscillations in Nucleus Accumbens and Anterior Limb of the Internal Capsule in Obsessive-Compulsive Disorder. Biol. Psychiatry 2021, 21, S0006-3223(21)01366-4. [Google Scholar] [CrossRef] [PubMed]
- Priori, A.; Foffani, G.; Rossi, L.; Marceglia, S. Adaptive deep brain stimulation (aDBS) controlled by local field potential oscillations. Exp. Neurol. 2013, 245, 77–86. [Google Scholar] [CrossRef]
- Litvak, V.; Florin, E.; Tamás, G.; Groppa, S.; Muthuraman, M. EEG and MEG primers for tracking DBS network effects. Neuroimage 2021, 224, 117447. [Google Scholar] [CrossRef]
- Grassi, M.; Rickelt, J.; Caldirola, D.; Eikelenboom, M.; van Oppen, P.; Dumontier, M.; Perna, G.; Schruers, K. Prediction of illness remission in patients with Obsessive-Compulsive Disorder with supervised machine learning. J. Affect. Disord. 2022, 296, 117–125. [Google Scholar] [CrossRef]
- Öst, L.-G.; Havnen, A.; Hansen, B.; Kvale, G. Cognitive behavioral treatments of obsessive–compulsive disorder. A systematic review and meta-analysis of studies published 1993–2014. Clin. Psychol. Rev. 2015, 40, 156–169. [Google Scholar] [CrossRef]
- Wu, H.; Hariz, M.; Visser-Vandewalle, V.; Zrinzo, L.; Coenen, V.A.; Sheth, S.A.; Bervoets, C.; Naesström, M.; Blomstedt, P.; Coyne, T.; et al. Deep brain stimulation for refractory obsessive-compulsive disorder (OCD): Emerging or established therapy? Mol. Psychiatry 2021, 26, 60–65. [Google Scholar] [CrossRef] [PubMed]
- Goodman, W.K.; Foote, K.D.; Greenberg, B.D.; Ricciuti, N.; Bauer, R.; Ward, H.; Shapira, N.A.; Wu, S.S.; Hill, C.L.; Rasmussen, S.A.; et al. Deep brain stimulation for intractable obsessive compulsive disorder: Pilot study using a blinded, staggered-onset design. Biol. Psychiatry 2010, 67, 535–542. [Google Scholar] [CrossRef] [PubMed]
- Mallet, L.; Polosan, M.; Jaafari, N.; Baup, N.; Welter, M.L.; Fontaine, D.; du Montcel, S.T.; Yelnik, J.; Chéreau, I.; Arbus, C.; et al. Subthalamic nucleus stimulation in severe obsessive-compulsive disorder. New Engl. J. Med. 2008, 359, 2121–2134. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schruers, K.; Baldi, S.; van den Heuvel, T.; Goossens, L.; Luyten, L.; Leentjens, A.F.G.; Ackermans, L.; Temel, Y.; Viechtbauer, W. The effects of deep-brain non-stimulation in severe obsessive-compulsive disorder: An individual patient data meta-analysis. Transl. Psychiatry 2019, 9, 183. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Agne, N.A.; Tisott, C.G.; Ballester, P.; Passos, I.C.; Ferrão, Y.A. Predictors of suicide attempt in patients with obsessive-compulsive disorder: An exploratory study with machine learning analysis. Psychol. Med. 2020, 52, 715–725. [Google Scholar] [CrossRef] [PubMed]
- Hoexter, M.Q.; Miguel, E.C.; Diniz, J.B.; Shavitt, R.G.; Busatto, G.F.; Sato, J.R. Predicting obsessive-compulsive disorder severity combining neuroimaging and machine learning methods. J. Affect. Disord. 2013, 150, 1213–1216. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ruan, H.; Wang, Y.; Li, Z.; Tong, G.; Wang, Z. A Systematic Review of Treatment Outcome Predictors in Deep Brain Stimulation for Refractory Obsessive-Compulsive Disorder. Brain Sci. 2022, 12, 936. https://doi.org/10.3390/brainsci12070936
Ruan H, Wang Y, Li Z, Tong G, Wang Z. A Systematic Review of Treatment Outcome Predictors in Deep Brain Stimulation for Refractory Obsessive-Compulsive Disorder. Brain Sciences. 2022; 12(7):936. https://doi.org/10.3390/brainsci12070936
Chicago/Turabian StyleRuan, Hanyang, Yang Wang, Zheqin Li, Geya Tong, and Zhen Wang. 2022. "A Systematic Review of Treatment Outcome Predictors in Deep Brain Stimulation for Refractory Obsessive-Compulsive Disorder" Brain Sciences 12, no. 7: 936. https://doi.org/10.3390/brainsci12070936
APA StyleRuan, H., Wang, Y., Li, Z., Tong, G., & Wang, Z. (2022). A Systematic Review of Treatment Outcome Predictors in Deep Brain Stimulation for Refractory Obsessive-Compulsive Disorder. Brain Sciences, 12(7), 936. https://doi.org/10.3390/brainsci12070936






