A Cross-Sectional Survey on the Clinical Management of Emergence Delirium in Adults: Knowledge, Attitudes, and Practice in Mainland China
Abstract
:1. Introduction
2. Materials and Methods
2.1. Survey Design and Target Population
2.2. Data Sampling
2.3. Statistical Analysis
3. Results
3.1. General Data of Respondents
3.2. Indicated Importance of ED
3.3. Risk Factors and Intervention Measures
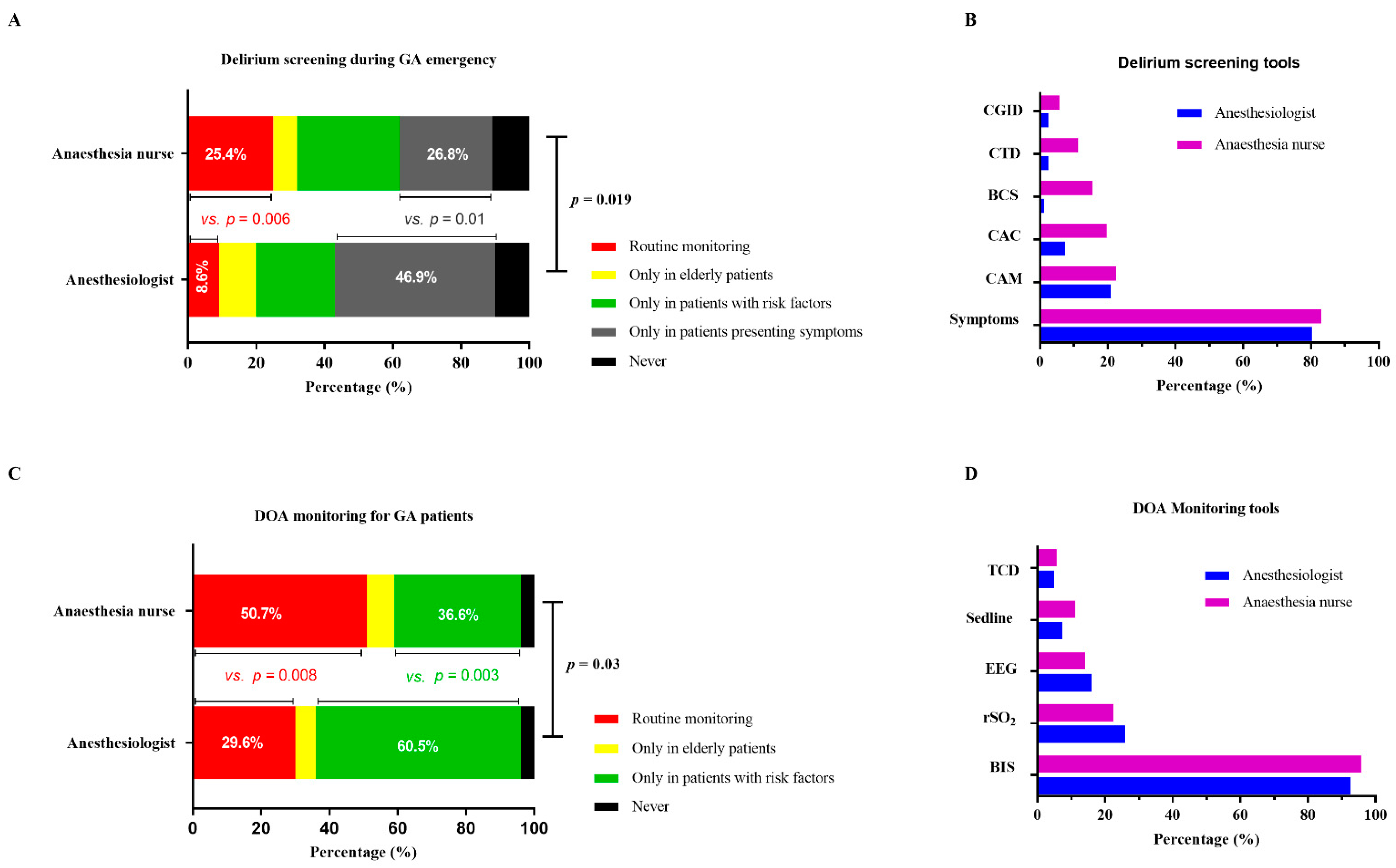
3.4. Assessment of ED
3.5. Monitoring Depth of Anesthesia (DOA)
3.6. Treatment for Delirium
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Aldecoa, C.; Bettelli, G.; Bilotta, F.; Sanders, R.D.; Audisio, R.; Borozdina, A.; Cherubini, A.; Jones, C.; Kehlet, H.; MacLullich, A.; et al. European Society of Anaesthesiology evidence-based and consensus-based guideline on postoperative delirium. Eur. J. Anaesthesiol. 2017, 34, 192–214. [Google Scholar] [CrossRef]
- Xara, D.; Silva, A.; Mendonca, J.; Abelha, F. Inadequate emergence after anesthesia: Emergence delirium and hypoactive emergence in the Postanesthesia Care Unit. J. Clin. Anesth. 2013, 25, 439–446. [Google Scholar] [CrossRef]
- Wang, Q.; Zhou, J.; Liu, T.; Yang, N.; Mi, X.; Han, D.; Han, Y.; Chen, L.; Liu, K.; Zheng, H.; et al. Predictive Value of Preoperative Profiling of Serum Metabolites for Emergence Agitation After General Anesthesia in Adult Patients. Front Mol. Biosci. 2021, 8, 739227. [Google Scholar] [CrossRef] [PubMed]
- Robinson, T.N.; Raeburn, C.D.; Tran, Z.V.; Brenner, L.A.; Moss, M. Motor subtypes of postoperative delirium in older adults. Arch. Surg. 2011, 146, 295–300. [Google Scholar] [CrossRef] [Green Version]
- Juliebo, V.; Bjoro, K.; Krogseth, M.; Skovlund, E.; Ranhoff, A.H.; Wyller, T.B. Risk factors for preoperative and postoperative delirium in elderly patients with hip fracture. J. Am. Geriatr. Soc. 2009, 57, 1354–1361. [Google Scholar] [CrossRef] [PubMed]
- Lepouse, C.; Lautner, C.A.; Liu, L.; Gomis, P.; Leon, A. Emergence delirium in adults in the post-anesthesia care unit. Br. J. Anaesth. 2006, 96, 747–753. [Google Scholar] [CrossRef] [Green Version]
- Radtke, F.M.; Franck, M.; Schneider, M.; Luetz, A.; Seeling, M.; Heinz, A.; Wernecke, K.D.; Spies, C.D. Comparison of three scores to screen for delirium in the recovery room. Br. J. Anaesth. 2008, 101, 338–343. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Delp, S.; Mei, W.; Spies, C.D.; Neuner, B.; Aldecoa, C.; Bettelli, G.; Bilotta, F.; Sanders, R.D.; Kramer, S.; Weiss, B. Clinical practice in the management of postoperative delirium by Chinese anesthesiologists: A cross-sectional survey designed by the European Society of Anesthesiology. J. Int. Med. Res. 2020, 48, 300060520927207. [Google Scholar] [CrossRef]
- Chen, K.; Yang, Y.L.; Li, H.L.; Xiao, D.; Wang, Y.; Zhang, L.; Zhou, J.X. A gap existed between physicians’ perceptions and performance of pain, agitation-sedation and delirium assessments in Chinese intensive care units. BMC Anesthesiol. 2021, 21, 61. [Google Scholar] [CrossRef]
- Wu, J.; Gao, S.; Zhang, S.; Yu, Y.; Liu, S.; Zhang, Z.; Mei, W. Perioperative risk factors for recovery room delirium after elective non-cardiovascular surgery under general anesthesia. Perioper. Med. 2021, 10, 3. [Google Scholar] [CrossRef]
- Fong, T.G.; Tulebaev, S.R.; Inouye, S.K. Delirium in elderly adults: Diagnosis, prevention and treatment. Nat. Rev. Neurol. 2009, 5, 210–220. [Google Scholar] [CrossRef] [PubMed]
- Detroyer, E.; Clement, P.M.; Baeten, N.; Pennemans, M.; Decruyenaere, M.; Vandenberghe, J.; Menten, J.; Milisen, K. Detection of delirium in palliative care unit patients: A prospective descriptive study of the Delirium Observation Screening Scale administered by bedside nurses. Palliat. Med. 2014, 28, 79–86. [Google Scholar] [CrossRef] [PubMed]
- Yuhas, R.; O’Brien, J.; Cotton, S. Delirium Detection and Treatment in the Intensive Care Unit. Crit. Care Nurse. 2021, 41, 15. [Google Scholar] [CrossRef] [PubMed]
- Bergjan, M.; Zilezinski, M.; Schwalbach, T.; Franke, C.; Erdur, H.; Audebert, H.J.; Hauss, A. Validation of two nurse-based screening tools for delirium in elderly patients in general medical wards. BMC Nurs. 2020, 19, 72. [Google Scholar] [CrossRef]
- Yang, F.; Ji, M.; Wu, Y.; Feng, Y.; Li, J.; Ren, D.; Ely, E.W. Delirium screening for patients in the intensive care unit: A prospective validation study of the iCAM-ICU by nurse researchers and bedside nurses in routine practice. Int. J. Nurs. Stud. 2021, 117, 103886. [Google Scholar] [CrossRef]
- Koebrugge, B.; Koek, H.L.; van Wensen, R.J.; Dautzenberg, P.L.; Bosscha, K. Delirium after abdominal surgery at a surgical ward with a high standard of delirium care: Incidence, risk factors and outcomes. Dig. Surg. 2009, 26, 63–68. [Google Scholar] [CrossRef]
- Yildizeli, B.; Ozyurtkan, M.O.; Batirel, H.F.; Kuscu, K.; Bekiroglu, N.; Yuksel, M. Factors associated with postoperative delirium after thoracic surgery. Ann. Thorac. Surg. 2005, 79, 1004–1009. [Google Scholar] [CrossRef]
- Breitbart, W.; Alici, Y. Agitation and delirium at the end of life: “We couldn’t manage him”. JAMA 2008, 300, 2898–2910. [Google Scholar]
- Zakriya, K.J.; Christmas, C.; Wenz, J.F., Sr.; Franckowiak, S.; Anderson, R.; Sieber, F.E. Preoperative factors associated with postoperative change in confusion assessment method score in hip fracture patients. Anesth. Analg. 2002, 94, 1628–1632. [Google Scholar] [CrossRef]
- Devlin, J.W.; Marquis, F.; Riker, R.R.; Robbins, T.; Garpestad, E.; Fong, J.J.; Didomenico, D.; Skrobik, Y. Combined didactic and scenario-based education improves the ability of intensive care unit staff to recognize delirium at the bedside. Crit. Care 2008, 12, R19. [Google Scholar] [CrossRef] [Green Version]
- Hosker, C.; Ward, D. Hypoactive delirium. BMJ 2017, 357, j2047. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boord, M.S.; Moezzi, B.; Davis, D.; Ross, T.J.; Coussens, S.; Psaltis, P.J.; Bourke, A.; Keage, H.A.D. Investigating how electroencephalogram measures associate with delirium: A systematic review. Clin. Neurophysiol. 2021, 132, 246–257. [Google Scholar] [CrossRef]
- Hesse, S.; Kreuzer, M.; Hight, D.; Gaskell, A.; Devari, P.; Singh, D.; Taylor, N.B.; Whalin, M.K.; Lee, S.; Sleigh, J.W.; et al. Association of electroencephalogram trajectories during emergence from anesthesia with delirium in the postanesthesia care unit: An early sign of postoperative complications. Br. J. Anaesth. 2019, 122, 622–634. [Google Scholar] [CrossRef] [PubMed]
- Su, X.; Meng, Z.T.; Wu, X.H.; Cui, F.; Li, H.L.; Wang, D.X.; Zhu, X.; Zhu, S.N.; Maze, M.; Ma, D. Dexmedetomidine for prevention of delirium in elderly patients after non-cardiac surgery: A andomized, double-blind, placebo-controlled trial. Lancet. 2016, 388, 1893–1902. [Google Scholar] [CrossRef] [Green Version]
- Khajavi, M.R.; Saffarian, A.; Majidi, F.; Moharari, R.S.; Pourfakhr, P.; Parhiz, S.A. Prophylactic administration of diphenhydramine/paracetamol reduced emergence agitation and postoperative pain following maxillofacial surgeries: A randomized controlled trial. Eur. Arch. Otorhinolaryngol. 2021, 279, 1467–1471. [Google Scholar] [CrossRef] [PubMed]
- Lovestrand, D.; Beaumont, C.D.; Calder, M.S.; Schmidt, M.; Calaro, R. Simulation Training Exercise to Improve Outcomes of Emergence Delirium in Patients with Posttraumatic Stress Disorder. AANA J. 2021, 89, 187–193. [Google Scholar]

| General Data | |
|---|---|
| Profession of respondents | |
| Anesthesiologist | 243 (87.10%) |
| Nurse | 213 (76.34%) |
| Years in anesthesiology | |
| <5 years | 29 (11.93%) |
| 5–10 years | 81 (33.33%) |
| 10–15 years | 85 (34.97%) |
| 15–20 years | 27 (11.11%) |
| >20 years | 21 (8.64%) |
| Years in nursing | |
| <3 years | 18 (8.45%) |
| 3–5 years | 33 (15.49%) |
| 5–7 years | 51 (23.94%) |
| 7–10 years | 30 (14.08%) |
| >10 years | 81 (38.03%) |
| Beds in hospital | |
| <1000 | 15 (6.17%) |
| 1000–2999 | 117 (48.15%) |
| 3000–4999 | 78 (32.10%) |
| 5000–9999 | 27 (11.11%) |
| ≥10,000 | 6 (2.47%) |
| Surgeries/year | |
| <10,000 | 9 (3.70%) |
| 10,000–29,999 | 72 (29.63%) |
| 30,000–49,999 | 42 (17.28%) |
| 50,000–79,999 | 78 (32.10%) |
| ≥80,000 | 42 (17.28%) |
| General anesthetics/year | |
| <10,000 | 33 (13.58%) |
| 10,000–29,999 | 78 (32.10%) |
| 30,000–49,999 | 63 (25.93%) |
| 50,000–79,999 | 36 (14.81%) |
| ≥80,000 | 33 (13.58%) |
| Risk Factors | Anesthesiologists (n = 243) | Anesthesia Nurses (n = 213) | p-Value |
|---|---|---|---|
| Advanced age | 234 (96.30%) | 195 (91.55%) | 0.032 |
| Comorbidities | 213 (87.65%) | 177 (83.10%) | 0.17 |
| Postoperative pain | 198 (81.48%) | 159 (74.65%) | 0.07 |
| Duration of surgery | 186 (76.54%) | 150 (70.42%) | 0.14 |
| Alcohol-related disorders | 180 (74.07%) | 153 (71.83%) | 0.59 |
| Catheter-related discomfort | 174 (71.60%) | 147 (69.01%) | 0.55 |
| Anticholinergic drug | 165 (67.90%) | 120 (56.34%) | 0.01 |
| Hyponatremia or hypernatraemia | 156 (64.20%) | 132 (61.97%) | 0.62 |
| Intraoperative bleeding | 156 (64.20%) | 123 (57.75%) | 0.16 |
| ASA status | 153 (62.96%) | 135 (63.38%) | 0.93 |
| Preoperative fluid fasting | 132 (54.32%) | 102 (47.89%) | 0.56 |
| Site of surgery | 117 (48.15%) | 90 (42.25%) | 0.041 |
| Prevention Measures | Anesthesiologists (n = 243) | Anesthesia Nurses (n = 213) | p-Value |
|---|---|---|---|
| Adequate perioperative pain management | 228 (93.83%) | 180 (84.50%) | 0.05 |
| Preoperative risk factors evaluation | 225 (92.59%) | 201 (94.37%) | 0.45 |
| Promptly diagnosing POD | 213 (87.65%) | 186 (87.32%) | 0.92 |
| Monitor depth of anesthesia | 195 (80.25%) | 183 (85.92%) | 0.11 |
| No premedication with benzodiazepines | 153 (62.96%) | 138 (64.79%) | 0.69 |
| Fast-track surgery | 135 (55.56%) | 111 (52.11%) | 0.10 |
| Treatment Strategies for ED | Anesthesiologists (n = 243) | Anesthesia Nurses (n = 213) | p-Value |
|---|---|---|---|
| Pain management | 207 (85.19%) | 150 (70.42%) | 0.001 |
| Sedation | 168 (69.14%) | 156 (73.24%) | 0.34 |
| Shout to inhibit aggressive behavior | 141 (58.02%) | 162 (76.06%) | 0.001 |
| Restraint | 132 (54.32%) | 164 (76.06%) | 0.001 |
| Artery blood gas analysis | 123 (50.62%) | 129 (60.56%) | 0.03 |
| Noting | 0 (0%) | 9 (4.23%) | 0.001 |
| Medications for ED | Anesthesiologists (n = 243) | Anesthesia Nurses (n = 213) | p-Value |
|---|---|---|---|
| Dexamedetomidine | 93 (38.27%) | 66 (30.99%) | 0.15 |
| Propofol | 84 (34.57%) | 75 (35.21%) | 0.89 |
| Intravenous analgesic | 42 (17.28%) | 45 (21.13%) | 0.30 |
| Midazolam | 6 (2.47%) | 12 (5.63%) | 0.08 |
| Haloperidol | 9 (3.70%) | 6 (2.82%) | 0.60 |
| Droperidol | 6 (2.47%) | 3 (1.41%) | 0.42 |
| Don’t know | 3 (1.23%) | 6 (2.82%) | 0.23 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yuan, Y.; Lei, B.; Li, Z.; Wang, X.; Zhao, H.; Gao, M.; Xue, Y.; Zhang, W.; Xiao, R.; Meng, X.; et al. A Cross-Sectional Survey on the Clinical Management of Emergence Delirium in Adults: Knowledge, Attitudes, and Practice in Mainland China. Brain Sci. 2022, 12, 989. https://doi.org/10.3390/brainsci12080989
Yuan Y, Lei B, Li Z, Wang X, Zhao H, Gao M, Xue Y, Zhang W, Xiao R, Meng X, et al. A Cross-Sectional Survey on the Clinical Management of Emergence Delirium in Adults: Knowledge, Attitudes, and Practice in Mainland China. Brain Sciences. 2022; 12(8):989. https://doi.org/10.3390/brainsci12080989
Chicago/Turabian StyleYuan, Yi, Bao Lei, Zhengqian Li, Xiaoxiao Wang, Huiling Zhao, Meng Gao, Yingying Xue, Wenchao Zhang, Rui Xiao, Xue Meng, and et al. 2022. "A Cross-Sectional Survey on the Clinical Management of Emergence Delirium in Adults: Knowledge, Attitudes, and Practice in Mainland China" Brain Sciences 12, no. 8: 989. https://doi.org/10.3390/brainsci12080989





