Usefulness of a Mobile Application (Mentali) for Anxiety and Depression Screening in Medical Students and Description of the Associated Triggering Factors
Abstract
:1. Introduction
Objective
2. Materials and Methods
2.1. Study Design and Participants
2.2. Instruments and Scales
2.2.1. Mentali App
2.2.2. Beck Inventories
- Anxiety: 0–7 points, minimal anxiety; 8–15, mild anxiety; 16–25, moderate anxiety; 26–63, severe anxiety.
- Depression: 0–9 points, minimal depression; 10–16, mild depression; 17–29, moderate depression; 30–63, severe depression.
2.3. Psychological Intervention and Clinical History
2.3.1. Hamilton Anxiety Rating Scale (HARS)
2.3.2. Hamilton Depression Rating Scale (HDRS)
2.4. Data Analysis
2.5. Ethical Considerations
3. Results
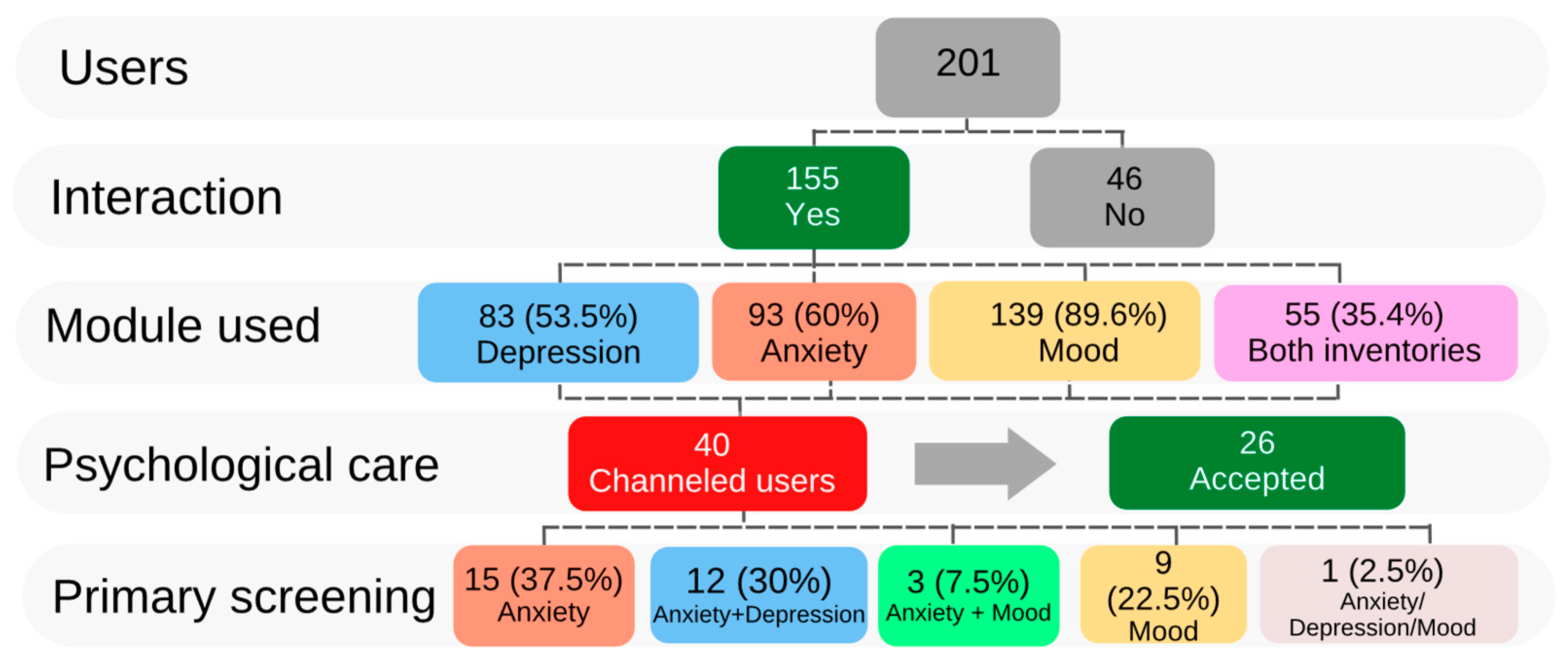
3.1. Description of the Characteristics of the Sample
3.2. Anxiety and Depression Primary Screening
3.3. Evaluation of Mood
3.4. Psychological Care
3.4.1. Psychological Medical History
3.4.2. Hamilton Scales
3.5. Psychiatric Care
3.6. Evaluation of Mentali as a Tool for Primary Screening of Anxiety and Depression
3.7. Mentali as a Tool for Monitoring Mental Health Conditions and Mood during School Periods
4. Discussion
Limitations
5. Conclusions
6. Patents
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rost, K. Disability from depression: The public health challenge to primary care. Nord. J. Psychiatry 2009, 63, 17–21. [Google Scholar] [CrossRef]
- World Health Organization. WHO-Convened Global Study of Origins of SARS-CoV-2: China Part; Joint WHO-China Study: Geneva, Switzerland, 2021. [Google Scholar]
- Brunier, A. COVID-19 Pandemic Triggers 25% Increase in Prevalence of Anxiety and Depression Worldwide; World Health Organization: Geneva, Switzerland, 2022. [Google Scholar]
- INEGI. Encuesta Nacional de Bienestar Autorreportado (ENBIARE) 2021; Instituto Nacional de Estadística y Geografía (INEGI): Ciudad de México, Mexico, 2021; p. 26. [Google Scholar]
- Association, A.P. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; Editorial Médica Panamericana: Madrid, Spain, 2014; Volume 21, pp. 591–643. [Google Scholar]
- Malllen, M.M.; Garza, D.N.L. Trastornos de ansiedad. Neurol. Neurocir. Psiquiatr. 2017, 44, 101–107. [Google Scholar]
- Tham, W.W.; Sojli, E.; Bryant, R.; McAleer, M. Common mental disorders and economic uncertainty: Evidence from the COVID-19 pandemic in the US. PLoS ONE 2021, 16, e0260726. [Google Scholar] [CrossRef] [PubMed]
- Sicras-Mainar, A.; Blanca-Tamayo, M.; Gutiérrez-Nicuesa, L.; Salvatella-Pasant, J.; Navarro-Artieda, y.R. Impacto de la morbilidad, uso de recursos y costes en el mantenimiento de la remisión de la depresión mayor en España: Estudio longitudinal de ámbito poblacional. Gac. Sanit. 2010, 24, 13–19. [Google Scholar] [CrossRef] [PubMed]
- De Jesús Moreno-Gordillo, G.; Trujillo-Olivera, L.E.; García-Chong, N.R.; Tapia-Garduño, F. Suicidio y depresión en adolescentes: Una revisión de la literatura. Rev. Chil. Salud Pública 2019, 23, 31–41. [Google Scholar] [CrossRef]
- Mascayano, F.; van der Ven, E.; Moro, M.F.; Schilling, S.; Alarcón, S.; Al Barathie, J.; Alnasser, L.; Asaoka, H.; Ayinde, O.; Balalian, A.A.; et al. The impact of the COVID-19 pandemic on the mental health of healthcare workers: Study protocol for the COVID-19 HEalth caRe wOrkErS (HEROES) study. Soc. Psychiatry Psychiatr. Epidemiol. 2022, 57, 633–645. [Google Scholar] [CrossRef]
- Susser, E.; Alvarado, R.; Mascayano, F. The COVID-19 Health Care Workers Study (HEROES); Organización Panamericana de la Salud: Washington, DC, USA, 2021. [Google Scholar]
- Capdevila-Gaudens, P.; García-Abajo, J.M.; Flores-Funes, D.; García-Barbero, M.; García-Estañ, J. Depression, anxiety, burnout and empathy among Spanish medical students. PLoS ONE. 2021, 16, e0260359. [Google Scholar] [CrossRef]
- Quek, T.T.; Tam, W.W.; Tran, B.X.; Zhang, M.; Zhang, Z.; Ho, C.S.; Ho, R.C. The Global Prevalence of Anxiety Among Medical Students: A Meta-Analysis. Int. J. Environ. Res. Public Health 2019, 16, 2735. [Google Scholar] [CrossRef]
- Murillo, O.G.; García, G.E.P.; Echegaray, R.M.; García, P.C.G.; Chávez, N.A. Estudio Comparatico: Trastorno De Ansiedad Generalizado (TAG) y Preocupación En Estudiantes De La Universidad Autónoma De Zacatecas. Integr. Académica En. Psicol. 2019, 7, 85–96. [Google Scholar]
- Azad, N.; Shahid, A.; Abbas, N.; Shaheen, A.; Munir, N. Anxiety And Depression In Medical Students Of A Private Medical College. J. Ayub Med. Coll. Abbottabad JAMC 2017, 29, 123–127. [Google Scholar]
- Grossman, J.T.; Frumkin, M.R.; Rodebaugh, T.L.; Lenze, E.J. mHealth Assessment and Intervention of Depression and Anxiety in Older Adults. Harv. Rev. Psychiatry 2020, 28, 203–214. [Google Scholar] [CrossRef] [PubMed]
- Salinas-Rodríguez, A.; Manrique-Espinoza, B.; Acosta-Castillo, I.; Ma Téllez-Rojo, M.; Franco-Núñez, A.; Gutiérrez-Robledo, L.M.; Sosa-Ortiz, A.L. Validación de un punto de corte para la Escala de Depresión del Centro de Estudios Epidemiológicos, versión abreviada (CESD-7). Salud Publica Mex. 2013, 55, 267–274. [Google Scholar] [CrossRef]
- Becerra-García, J.A.; Sánchez-Gutiérrez, T.; Barbeito, S.; Calvo, A. COVID-19 pandemic and mental health in Spain: An analysis of their relationship using Google Trends. Rev. Psiquiatr. Salud Ment. 2021, 8. [Google Scholar]
- Grist, R.; Porter, J.; Stallard, P. Mental health mobile apps for preadolescents and adolescents: A systematic review. J. Med. Internet Res. 2017, 19, e7332. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wiljer, D.; Shi, J.; Lo, B.; Sanches, M.; Hollenberg, E.; Johnson, A.; Abi-Jaoudé, A.; Chaim, G.; Cleverley, K.; Henderson, J. Effects of a Mobile and Web App (Thought Spot) on Mental Health Help-Seeking Among College and University Students: Randomized Controlled Trial. J. Med. Internet Res. 2020, 22, e20790. [Google Scholar] [CrossRef]
- Donker, T.; Petrie, K.; Proudfoot, J.; Clarke, J.; Birch, M.-R.; Christensen, H. Smartphones for smarter delivery of mental health programs: A systematic review. J. Med. Internet Res. 2013, 15, e2791. [Google Scholar] [CrossRef]
- González, C.G.; Castán, J.P. Capítulo 8: Pruebas diagnósticas. Concordancia. SEMERGEN—Med. De Fam. 2007, 33, 509–519. [Google Scholar] [CrossRef]
- Medina, M.C. Generalidades de las pruebas diagnósticas, y su utilidad en la toma de decisiones médicas. Rev. Colomb. De Psiquiatr. 2011, 40, 787–797. [Google Scholar] [CrossRef]
- Wang, K.; Varma, D.S.; Prosperi, M. A systematic review of the effectiveness of mobile apps for monitoring and management of mental health symptoms or disorders. J. Psychiatr. Res. 2018, 107, 73–78. [Google Scholar] [CrossRef]
- Khademian, F.; Aslani, A.; Bastani, P. The effects of mobile apps on stress, anxiety, and depression: Overview of systematic reviews. Int. J. Technol. Assess. Health Care 2020, 37, e4. [Google Scholar] [CrossRef]
- Zhao, J.; Freeman, B.; Li, M. Can Mobile Phone Apps Influence People’s Health Behavior Change? An Evidence Review. J. Med. Internet Res. 2016, 18, e287. [Google Scholar] [CrossRef] [PubMed]
- Chandran, V.P.; Balakrishnan, A.; Rashid, M.; Pai Kulyadi, G.; Khan, S.; Devi, E.S.; Nair, S.; Thunga, G. Mobile applications in medical education: A systematic review and meta-analysis. PLoS ONE 2022, 17, e0265927. [Google Scholar] [CrossRef]
- García, A.S.; Casas, J.M.M. Apps de salud: Nuevas herramientas para el cuidado del paciente cardiológico. Enferm Cardiol. 2015, 22, 28–34. [Google Scholar]
- Jackson-Koku, G. Beck depression inventory. Occup. Med. 2016, 66, 174–175. [Google Scholar] [CrossRef] [PubMed]
- Wiebe, J.S.; Penley, J.A. A psychometric comparison of the Beck Depression Inventory-II in English and Spanish. Psychol. Assess. 2005, 17, 481–485. [Google Scholar] [CrossRef]
- Araneda, R.M.; Solar, F.C.; González, P.R.; Peralta, M.V. Propiedades psicométricas del Inventario de Depresión de Beck-II en adolescentes chilenos. Ter. Psicológica 2008, 26, 59–69. [Google Scholar]
- Cuba, M.A.S.; Espinoza, M.A. APGAR familiar: Una herramienta para detectar disfunción familiar. Rev. Méd. La Paz 2014, 20, 53–57. [Google Scholar]
- Shao, R.; He, P.; Ling, B.; Tan, L.; Xu, L.; Hou, Y.; Kong, L.; Yang, Y. Prevalence of depression and anxiety and correlations between depression, anxiety, family functioning, social support and coping styles among Chinese medical students. BMC Psychol. 2020, 8, 38. [Google Scholar] [CrossRef]
- Bruss, G.S.; Gruenberg, A.M.; Goldstein, R.D.; Barber, J.P. Hamilton anxiety rating scale interview guide: Joint interview and test-retest methods for interrater reliability. Psychiatry Res. 1994, 53, 191–202. [Google Scholar] [CrossRef]
- Teutli, A.; Escala de Ansiedad de Hamilton. Alejandra Teutli: Servicio Andaluz de Salud. Consejeria de Salud. Available online: https://www.huvn.es/archivos/cms/enfermeria-en-huvn/archivos/publico/cuestionarios/Cuestionarios-2/escala_de_ansiedad_de_hamilton.pdf (accessed on 3 March 2022).
- Sharp, R. The Hamilton Rating Scale for Depression. J. Occup. Med. 2015, 65, 340. [Google Scholar] [CrossRef]
- Black, D.W.; Andreasen, N.C. Texto Introductorio de Psiquiatría; Editorial El Manual Moderno: Mexico City, Mexico, 2015. [Google Scholar]
- Manyari, M.V.; Salinas, I.M.; Andrade-González, N.; Lahera, G. Tratamiento farmacológico de la depresión: Comparación entre las principales Guías de Práctica Clínica. Revista de Investivación y Educación en Ciencias de la Salud 2017, 2, 72–84. [Google Scholar] [CrossRef]
- Martin, G.H.; Segura, P.C. Guía clínica para el manejo de la ansiedad; Instituto nacional de psiquiatría Ramon de la Fuente: Ciudad de México, México, 2010.
- World Medical Association. World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef]
- De Salud, S. Norma Oficial Mexicana NOM-004-SSA3-2012; Del Expediente Clinico. Diario Oficial de la Federación: Ciudad de México, Mexico, 2012. [Google Scholar]
- Bassols, A.M.; Okabayashi, L.S.; Silva, A.B.; Carneiro, B.B.; Feijó, F.; Guimarães, G.C.; Cortes, G.N.; Rohde, L.A.; Eizirik, C.L. First- and last-year medical students: Is there a difference in the prevalence and intensity of anxiety and depressive symptoms? Rev. Bras. De Psiquiatr. 2014, 36, 233–240. [Google Scholar] [CrossRef] [PubMed]
- Cheng, H.L.; Wang, C.; McDermott, R.C.; Kridel, M.; Rislin, J.L. Self-stigma, mental health literacy, and attitudes toward seeking psychological help. J. Couns. Dev. 2018, 96, 64–74. [Google Scholar] [CrossRef]
- Ding, Y.; Dai, J. Advance in stress for depressive disorder. Adv. Exp. Med. Biol. 2019, 1180, 147–178. [Google Scholar] [CrossRef] [PubMed]
- Hammen, C. Risk Factors for Depression: An Autobiographical Review. Annu. Rev. Clin. Psychol. 2018, 14, 1–28. [Google Scholar] [CrossRef]
- Newman, M.G.; Shin, K.E.; Zuellig, A.R. Developmental risk factors in generalized anxiety disorder and panic disorder. J. Affect. Disord. 2016, 206, 94–102. [Google Scholar] [CrossRef] [Green Version]
- Roman Sanchez, J.; Martin Anton, L.; Carbonero Martin, M. Tipos de familia y satisfacción de necesidades de los hijos. Int. J. Dev. Educ. Psychol. 2009, 2, 549–558. [Google Scholar]
- Andrade, J.J.d.C.; Silva, A.C.O.; Frazão, I.D.S.; Perrelli, J.G.A.; Silva, T.T.D.M.; Cavalcanti, A.M.T.S. Family functionality and burden of family caregivers of users with mental disorders. Rev. Bras. Enferm. 2021, 74, 9. [Google Scholar] [CrossRef]
- Carreras, A. Recursos, Funcionalidad y Disfuncionalidad Familiar. Recur. Func. Y Disfuncionalidad Fam. 2014, 1, 1–12. Available online: https://www.academia.edu/36332513/Recursos_Funcionalidad_y_Disfuncionalidad_Familiar (accessed on 25 August 2022).
- Firth, J.; Ward, P.; Stubbs, B. Editorial: Lifestyle Psychiatry. Front. Psychiatry 2019, 10, 597. [Google Scholar] [CrossRef] [PubMed]
- Balanzá-Martínez, V.; Kapczinski, F.; Cardoso, T.D.A.; Atienza-Carbonell, B.; Rosa, A.R.; Mota, J.C.; De Boni, R.B. The assessment of lifestyle changes during the COVID-19 pandemic using a multidimensional scale. Rev. Psiquiatr. Salud. Ment. 2021, 14, 16–26. [Google Scholar] [CrossRef] [PubMed]
- Robertson, M.; Duffy, F.; Newman, E.; Bravo, C.P.; Ates, H.H.; Sharpe, H. Exploring changes in body image, eating and exercise during the COVID-19 lockdown: A UK survey. Appetite 2021, 159, 105062. [Google Scholar] [CrossRef] [PubMed]
- Ehryhorczuk, C.; Esharma, S.; Fulton, S.E. Metabolic disturbances connecting obesity and depression. Front. Neurosci. 2013, 7, 177. [Google Scholar] [CrossRef]
- Liu, J.; Garza, J.C.; Bronner, J.; Kim, C.S.; Zhang, W.; Lu, X.-Y. Acute administration of leptin produces anxiolytic-like effects: A comparison with fluoxetine. Psychopharmacology 2010, 207, 535–545. [Google Scholar] [CrossRef]
- Yamada, N.; Katsuura, G.; Ochi, Y.; Ebihara, K.; Kusakabe, T.; Hosoda, K.; Nakao, K. Impaired CNS leptin action is implicated in depression associated with obesity. Endocrinology 2011, 152, 2634–2643. [Google Scholar] [CrossRef]
- Maffei, Á.; Halaas, J.; Ravussin, E.; Pratley, R.; Lee, G.; Zhang, Y.; Fei, H.; Kim, S.; Lallone, R.; Ranganathan, S. Leptin levels in human and rodent: Measurement of plasma leptin and ob RNA in obese and weight-reduced subjects. Nat. Med. 1995, 1, 1155–1161. [Google Scholar] [CrossRef]
- Dantzer, R.; O’connor, J.C.; Freund, G.G.; Johnson, R.W.; Kelley, K.W. From inflammation to sickness and depression: When the immune system subjugates the brain. Nat. Rev. Neurosci. 2008, 9, 46–56. [Google Scholar] [CrossRef]
- Colin, A.; Reggers, J.; Castronovo, V.; Ansseau, M. Lipids, depression and suicide. L’Encephale 2003, 29, 49–58. [Google Scholar]
- Dêbska, E.; Janas, A.; Bañczyk, W.; Janas–Kozik, M. Depression or depressiveness in patients diagnosed with Anorexia Nervosa and Bulimia Nervosa–pilot research. Psychiatr. Danub. 2011, 23, 87–90. [Google Scholar]
- Ganança, L.; Galfalvy, H.C.; Cisneros-Trujillo, S.; Basseda, Z.; Cooper, T.B.; Ren, X.; Figueira, M.L.; Oquendo, M.A.; Mann, J.J.; Sublette, M.E. Relationships between inflammatory markers and suicide risk status in major depression. J. Psychiatr. Res. 2021, 134, 192–199. [Google Scholar] [CrossRef] [PubMed]
- Firth, J.; Marx, W.; Dash, S.; Carney, R.; Teasdale, S.B.; Solmi, M.; Stubbs, B.; Schuch, F.B.; Carvalho, A.F.; Jacka, F.; et al. The effects of dietary improvement on symptoms of depression and anxiety: A meta-analysis of randomized controlled trials. Psychosom. Med. 2019, 81, 265. [Google Scholar] [CrossRef]
- Casper, R.C. Depression and eating disorders. Depress. Anxiety 1998, 8, 96–104. [Google Scholar] [CrossRef]
- Fuentes, E.A.; Carvallo, P.R.; Poblete, S.R. Bullying as a risk factor for depression and suicide. Rev. Chil. Pediatr. 2020, 91, 432–439. [Google Scholar] [CrossRef]
- Janowsky, D.S. Introversion and extroversion: Implications for depression and suicidality. Curr. Psychiatry Rep. 2001, 3, 444–450. [Google Scholar] [CrossRef]
- Yan, Z.; Zeng, X.; Su, J.; Zhang, X. The dark side of empathy: Meta-analysis evidence of the relationship between empathy and depression. PsyCh J. 2021, 10, 794–804. [Google Scholar] [CrossRef] [PubMed]
- Moutinho, I.L.; Maddalena, N.C.; Roland, R.K.; Lucchetti, A.L.; Tibiriçá, S.H.; Ezequiel, O.D.; Lucchetti, G. Depression, stress and anxiety in medical students: A cross-sectional comparison between students from different semesters. Rev. Da Assoc. Med. Bras. 2017, 63, 21–28. [Google Scholar] [CrossRef]




| Variable | Factor | n (%) |
|---|---|---|
| Family | Conflicts | 12 (46.1) |
| Disapproval | 3 (11.5) | |
| Absence of relative | 3 (11.5) | |
| Distant relationship | 1 (3.8) | |
| Paternal alcoholism | 1 (3.8) | |
| Unknown | 6 (23) | |
| Couples | Conflicts | 4 (15.3) |
| Distrust | 2 (7.6) | |
| Lack of attention | 1 (3.8) | |
| Lack of communication | 1 (3.8) | |
| Transgender couple | 1 (3.8) | |
| Unknown | 17 (65) | |
| Friendship | Couple estrangement | 4 (15.3) |
| Trouble socializing | 2 (7.6) | |
| Lack of support | 1 (3.8) | |
| Unknown | 19 (73) | |
| School | Stress | 13 (50) |
| Lack of concentration | 3 (11.5) | |
| Frustration | 2 (7.6) | |
| Favoritism | 1 (3.8) | |
| Insecurity about choice career | 1 (3.8) | |
| Discouragement | 1 (3.8) | |
| Unknown | 5 (19.2) | |
| Physical health | Weight gain | 2 (7.6) |
| Polycystic Ovary Syndrome | 2 (7.6) | |
| Anemia | 1 (3.8) | |
| Appendicitis | 1 (3.8) | |
| Hypochondria | 1 (3.8) | |
| Irritable Bowel Syndrome | 1 (3.8) | |
| Unknown | 18 (69.2) |
| User | Diagnosis | ||
|---|---|---|---|
| Mentali | Psychology | Psychiatry | |
| 1 | Severe anxiety and severe depression | Generalized anxiety and mild depression | Mixed anxious–depressive disorder |
| 2 | Severe anxiety and moderate depression | Generalized anxiety | Generalized anxiety disorder |
| 3 | Severe anxiety and mild depression | Moderate depression | Moderate depressive episode |
| 4 | Severe anxiety and moderate depression | Generalized anxiety | Generalized anxiety disorder |
| 5 | Severe anxiety | Generalized anxiety | Generalized anxiety disorder and moderate depressive episode |
| Time of Evaluation | Mood Report, n (%) | Total Responses | ||||
|---|---|---|---|---|---|---|
| Excellent a | Good b | Regular c | Bad d | Very Bad e | ||
| Beginning of the semester | 114 (36.7) | 130 (41.3) | 43 (13.8) | 15 (4.8) | 8 (2.5) | 310 |
| First academic test | 12 (4.6) | 72 (27.9) | 102 (39.5) | 44 (17) | 28 (10.8) | 258 |
| Final academic test | 5 (17.2) | 5 (17.2) | 9 (31.0) | 5 (17.2) | 5 (17.2) | 29 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martinez-Fierro, M.L.; Ayala-Haro, A.E.; Pinedo-Hurtado, M.E.; Solis-Galvan, J.A.; Garza-Veloz, I.; Velazquez-Lopez, Z.Y.; Camacho-Martinez, A.G.; Avila-Carrasco, L.; Vazquez-Reyes, S.; Velasco-Elizondo, P.; et al. Usefulness of a Mobile Application (Mentali) for Anxiety and Depression Screening in Medical Students and Description of the Associated Triggering Factors. Brain Sci. 2022, 12, 1223. https://doi.org/10.3390/brainsci12091223
Martinez-Fierro ML, Ayala-Haro AE, Pinedo-Hurtado ME, Solis-Galvan JA, Garza-Veloz I, Velazquez-Lopez ZY, Camacho-Martinez AG, Avila-Carrasco L, Vazquez-Reyes S, Velasco-Elizondo P, et al. Usefulness of a Mobile Application (Mentali) for Anxiety and Depression Screening in Medical Students and Description of the Associated Triggering Factors. Brain Sciences. 2022; 12(9):1223. https://doi.org/10.3390/brainsci12091223
Chicago/Turabian StyleMartinez-Fierro, Margarita L., Anayantzin E. Ayala-Haro, Martha E. Pinedo-Hurtado, Jorge A. Solis-Galvan, Idalia Garza-Veloz, Zihomara Y. Velazquez-Lopez, Antonio G. Camacho-Martinez, Lorena Avila-Carrasco, Sodel Vazquez-Reyes, Perla Velasco-Elizondo, and et al. 2022. "Usefulness of a Mobile Application (Mentali) for Anxiety and Depression Screening in Medical Students and Description of the Associated Triggering Factors" Brain Sciences 12, no. 9: 1223. https://doi.org/10.3390/brainsci12091223
APA StyleMartinez-Fierro, M. L., Ayala-Haro, A. E., Pinedo-Hurtado, M. E., Solis-Galvan, J. A., Garza-Veloz, I., Velazquez-Lopez, Z. Y., Camacho-Martinez, A. G., Avila-Carrasco, L., Vazquez-Reyes, S., Velasco-Elizondo, P., Mauricio-Gonzalez, A., & Ortiz-Castro, Y. (2022). Usefulness of a Mobile Application (Mentali) for Anxiety and Depression Screening in Medical Students and Description of the Associated Triggering Factors. Brain Sciences, 12(9), 1223. https://doi.org/10.3390/brainsci12091223







