Primary Care Clinician and Child Characteristics Impacting Autism Surveillance
Abstract
1. A Note on Terminology
2. Introduction
3. Materials and Methods
3.1. Participants
3.2. Measures
3.2.1. Screening
3.2.2. PCC Concern
3.2.3. PCC Characteristics and Beliefs Inventory
3.2.4. Practice Characteristics
3.3. Procedures
3.4. Analyses
4. Results
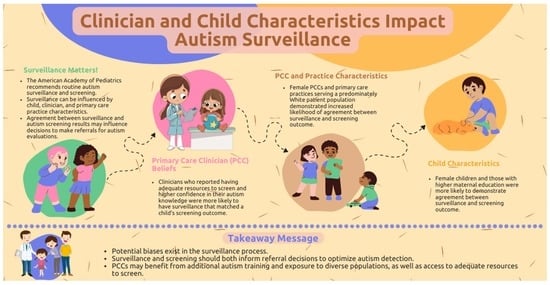
4.1. PCC Beliefs
4.2. PCC/Practice Characteristics
4.3. Child Characteristics
5. Discussion
6. Conclusions
Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bury, S.M.; Jellett, R.; Spoor, J.R.; Hedley, D. “It defines who I am” or “It’s something I have”: What language do [autistic] Australian adults [on the autism spectrum] prefer? J. Autism Dev. Disord. 2020, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Kenny, L.; Hattersley, C.; Molins, B.; Buckley, C.; Povey, C.; Pellicano, E. Which terms should be used to describe autism? Perspectives from the UK autism community. Autism Int. J. Res. Pract. 2016, 20, 442–462. [Google Scholar] [CrossRef]
- Anderson, D.K.; Liang, J.W.; Lord, C. Predicting young adult outcome among more and less cognitively able individuals with autism spectrum disorders. J. Child Psychol. Psychiatry 2014, 55, 485–494. [Google Scholar] [CrossRef] [PubMed]
- Dawson, G.; Rogers, S.; Munson, J.; Smith, M.; Winter, J.; Greenson, J.; Donaldson, A.; Varley, J. Randomized, controlled trial of an intervention for toddlers with autism: The Early Start Denver Model. Pediatrics 2010, 125, e17–e23. [Google Scholar] [CrossRef] [PubMed]
- Elder, J.H.; Kreider, C.M.; Brasher, S.N.; Ansell, M. Clinical impact of early diagnosis of autism on the prognosis and parent–child relationships. Psychol. Res. Behav. Manag. 2017, 10, 283–292. [Google Scholar] [CrossRef]
- Harris, S.L.; Handleman, J.S. Age and IQ at intake as predictors of placement for young children with autism: A four-to six-year follow-up. J. Autism Dev. Disord. 2000, 30, 137–142. [Google Scholar] [CrossRef]
- MacDonald, R.; Parry-Cruwys, D.; Dupere, S.; Ahearn, W. Assessing progress and outcome of early intensive behavioral intervention for toddlers with autism. Res. Dev. Disabil. 2014, 35, 3632–3644. [Google Scholar] [CrossRef]
- Orinstein, A.J.; Helt, M.; Troyb, E.; Tyson, K.E.; Barton, M.L.; Eigsti, I.M.; Naigles, L.; Fein, D.A. Intervention for optimal outcome in children and adolescents with a history of autism. J. Dev. Behav. Pediatr. 2014, 35, 247–256. [Google Scholar] [CrossRef]
- Rogers, S.J.; Vismara, L.A. Evidence-based comprehensive treatments for early autism. J. Clin. Child Adolesc. Psychol. 2008, 37, 8–38. [Google Scholar] [CrossRef]
- Rotholz, D.A.; Kinsman, A.M.; Lacy, K.K.; Charles, J. Improving early identification and intervention for children at risk for autism spectrum disorder. Pediatrics 2017, 139, e20161061. [Google Scholar] [CrossRef]
- Swanson, A.R.; Warren, Z.E.; Stone, W.L.; Vehorn, A.C.; Dohrmann, E.; Humberd, Q. The diagnosis of autism in community pediatric settings: Does advanced training facilitate practice change? Autism 2014, 18, 555–561. [Google Scholar] [CrossRef] [PubMed]
- Volkmar, F.R. Editorial: The importance of early intervention. J. Autism Dev. Disord. 2014, 44, 2979–2980. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Zwaigenbaum, L.; Bauman, M.L.; Choueiri, R.; Kasari, C.; Carter, A.; Granpeesheh, D.; Mailloux, Z.; Roley, S.S.; Wagner, S.; Fein, D.; et al. Early intervention for children with autism spectrum disorder under 3 years of age: Recommendations for practice and research. Pediatrics 2015, 136, S60–S81. [Google Scholar] [CrossRef]
- Zwaigenbaum, L.; Bauman, M.L.; Stone, W.L.; Yirmiya, N.; Estes, A.; Hansen, R.L.; McPartland, J.C.; Natowicz, M.R.; Choueiri, R.; Fein, D.; et al. Early identification of autism spectrum disorder: Recommendations for practice and research. Pediatrics 2015, 136, S10–S40. [Google Scholar] [CrossRef]
- Zwaigenbaum, L.; Bryson, S.; Lord, C.; Rogers, S.; Carter, A.; Carver, L.; Chawarska, K.; Constantino, J.; Dawson, G.; Dobkins, K.; et al. Clinical assessment and management of toddlers with suspected autism spectrum disorder: Insights from studies of high-risk infants. Pediatrics 2009, 123, 1383–1391. [Google Scholar] [CrossRef] [PubMed]
- Landa, R.J.; Gross, A.L.; Stuart, E.A.; Faherty, A. Developmental trajectories in children with and without autism spectrum disorders: The first 3 years. Child Dev. 2013, 84, 429–442. [Google Scholar] [CrossRef]
- Ozonoff, S.; Young, G.S.; Landa, R.J.; Brian, J.; Bryson, S.; Charman, T.; Chawarska, K.; Macari, S.L.; Messenger, D.; Stone, W.L.; et al. Diagnostic stability in young children at risk for autism spectrum disorder: A baby siblings research consortium study. J. Child Psychol. Psychiatry 2015, 56, 988–998. [Google Scholar] [CrossRef]
- Pierce, K.; Gazestani, V.H.; Bacon, E.; Barnes, C.C.; Cha, D.; Nalabolu, S.; Lopez, L.; Moore, A.; Pence-Stophaeros, S.; Courchesne, E. Evaluation of the diagnostic stability of the early autism spectrum disorder phenotype in the general population starting at 12 months. JAMA Pediatr. 2019, 173, 578–587. [Google Scholar] [CrossRef] [PubMed]
- Zwaigenbaum, L.; Bryson, S.E.; Brian, J.; Smith, I.M.; Roberts, W.; Szatmari, P.; Roncadin, C.; Garon, N.; Vaillancourt, T. Stability of diagnostic assessment for autism spectrum disorder between 18 and 36 months in a high-risk cohort. Autism Res. 2016, 9, 790–800. [Google Scholar] [CrossRef]
- Wiggins, L.D.; Durkin, M.; Esler, A.; Lee, L.C.; Zahorodny, W.; Rice, C.; Yeargin-Allsopp, M.; Dowling, N.F.; Hall-Lande, J.; Morrier, M.J.; et al. Disparities in documented diagnoses of autism spectrum disorder based on demographic, individual, and service factors. Autism Res. 2020, 13, 464–473. [Google Scholar] [CrossRef]
- Duby, J.C.; Lipkin, P.H.; Macias, M.M.; Wegner, L.M.; Duncan, P.; Hagan, J.F.; Cooley, W.C.; Swigonski, N.; Biondich, P.G.; Lollar, D.; et al. Identifying infants and young children with developmental disorders in the medical home: An algorithm for developmental surveillance and screening. Pediatrics 2006, 118, 405–420. [Google Scholar] [CrossRef]
- Hyman, S.; Levy, S.E.; Myers, S.M. Identification, evaluation, and management of children with autism spectrum disorder. Pediatrics 2020, 145, e20193447. [Google Scholar] [CrossRef]
- American Academy of Pediatrics. Developmental Surveillance and Screening. Available online: https://www.aap.org/en/patient-care/developmental-surveillance-and-screening-patient-care/ (accessed on 1 November 2022).
- Burkett, K.; Morris, E.; Manning-Courtney, P.; Anthony, J.; Shambley-Ebron, D. African American families on autism diagnosis and treatment: The influence of culture. J. Autism Dev. Disord. 2015, 45, 3244–3254. [Google Scholar] [CrossRef]
- Donohue, M.R.; Childs, A.W.; Richards, M.; Robins, D.L. Race influences parent report of concerns about symptoms of autism spectrum disorder. Autism 2019, 23, 100–111. [Google Scholar] [CrossRef]
- Emerson, N.D.; Morrell, H.E.; Neece, C. Predictors of age of diagnosis for children with autism spectrum disorder: The role of a consistent source of medical care, race, and condition severity. J. Autism Dev. Disord. 2016, 46, 127–138. [Google Scholar] [CrossRef]
- Turner, E.A.; Jensen-Doss, A.; Heffer, R.W. Ethnicity as a moderator of how parents’ attitudes and perceived stigma influence intentions to seek child mental health services. Cult. Divers. Ethn. Minor. Psychol. 2015, 21, 613. [Google Scholar] [CrossRef]
- Zuckerman, K.E.; Lindly, O.J.; Reyes, N.M.; Chavez, A.E.; Cobian, M.; Macias, K.; Reynolds, A.M.; Smith, K.A. Parent perceptions of community autism spectrum disorder stigma: Measure validation and associations in a multi-site sample. J. Autism Dev. Disord. 2018, 48, 3199–3209. [Google Scholar] [CrossRef]
- Robins, D.L.; Fein, D.; Barton, M. The Modified Checklist for Autism in Toddlers, Revised, with Follow-up (M-CHAT-R/F). Available online: http://www.mchatscreen.com (accessed on 1 November 2022).
- Khowaja, M.K.; Hazzard, A.P.; Robins, D.L. Sociodemographic barriers to early detection of autism: Screening and evaluation using the M-CHAT, M-CHAT-R, and follow-up. J. Autism Dev. Disord. 2015, 45, 1797–1808. [Google Scholar] [CrossRef]
- Daniels, A.M.; Mandell, D.S. Explaining differences in age at autism spectrum disorder diagnosis: A critical review. Autism 2014, 18, 583–597. [Google Scholar] [CrossRef] [PubMed]
- Durkin, M.S.; Maenner, M.J.; Meaney, F.J.; Levy, S.E.; DiGuiseppi, C.; Nicholas, J.S.; Kirby, R.S.; Pinto-Martin, J.A.; Schieve, L.A. Socioeconomic inequality in the prevalence of autism spectrum disorder: Evidence from a US cross-sectional study. PLoS ONE 2010, 5, e11551. [Google Scholar] [CrossRef]
- Fountain, C.; King, M.D.; Bearman, P.S. Age of diagnosis for autism: Individual and community factors across 10 birth cohorts. J. Epidemiol. Community Health 2011, 65, 503–510. [Google Scholar] [CrossRef] [PubMed]
- Herlihy, L.E.; Brooks, B.; Dumont-Mathieu, T.; Barton, M.L.; Fein, D.; Chen, C.M.; Robins, D.L. Standardized screening facilitates timely diagnosis of autism spectrum disorders in a diverse sample of low-risk toddlers. J. Dev. Behav. Pediatr. 2014, 35, 85. [Google Scholar] [CrossRef] [PubMed]
- Liptak, G.S.; Benzoni, L.B.; Mruzek, D.W.; Nolan, K.W.; Thingvoll, M.A.; Wade, C.M.; Fryer, G.E. Disparities in diagnosis and access to health services for children with autism: Data from the national survey of children’s health. J. Dev. Behav. Pediatr. 2008, 29, 152–160. [Google Scholar] [CrossRef]
- McCormack, G.; Dillon, A.C.; Healy, O.; Walsh, C.; Lydon, S. Primary care physicians’ knowledge of autism and evidence-based interventions for autism: A systematic review. Rev. J. Autism Dev. Disord. 2019, 7, 1–16. [Google Scholar] [CrossRef]
- Mazurek, M.O.; Harkins, C.; Menezes, M.; Chan, J.; Parker, R.A.; Kuhlthau, K.; Sohl, K. Primary care providers’ perceived barriers and needs for support in caring for children with autism. J. Pediatr. 2020, 221, 240–245. [Google Scholar] [CrossRef]
- Morris, R.; Greenblatt, A.; Saini, M. Healthcare Providers’ experiences with autism: A scoping review. J. Autism Dev. Disord. 2019, 49, 2374–2388. [Google Scholar] [CrossRef]
- Mandell, D.S.; Ittenbach, R.F.; Levy, S.E.; Pinto-Martin, J.A. Disparities in diagnoses received prior to a diagnosis of autism spectrum disorder. J. Autism Dev. Disord. 2007, 37, 1795–1802. [Google Scholar] [CrossRef]
- Mandell, D.S.; Listerud, J.; Levy, S.E.; Pinto-Martin, J.A. Race differences in the age at diagnosis among Medicaid-eligible children with autism. J. Am. Acad. Child Adolesc. Psychiatry 2002, 41, 1447–1453. [Google Scholar] [CrossRef]
- Carbone, P.S.; Campbell, K.; Wilkes, J.; Stoddard, G.J.; Huynh, K.; Young, P.C.; Gabrielsen, T.P. Primary care autism screening and later autism diagnosis. Pediatrics 2020, 146, e20192314. [Google Scholar] [CrossRef]
- Azim, A.; Rdesinski, R.E.; Phelps, R.; Zuckerman, K.E. Nonclinical factors in autism diagnosis: Results from a national health care provider survey. J. Dev. Behav. Pediatr. 2020, 41, 428–435. [Google Scholar] [CrossRef]
- Crais, E.R.; McComish, C.S.; Humphreys, B.P.; Watson, L.R.; Baranek, G.T.; Reznick, J.S.; Christian, R.B.; Earls, M. Pediatric healthcare professionals’ views on autism spectrum disorder screening at 12–18 months. J. Autism Dev. Disord. 2014, 44, 2311–2328. [Google Scholar] [CrossRef]
- Elder, J.H.; Brasher, S.; Alexander, B. Identifying the barriers to early diagnosis and treatment in underserved individuals with autism spectrum disorders (ASD) and their families: A qualitative study. Issues Ment. Health Nurs. 2016, 37, 412–420. [Google Scholar] [CrossRef]
- Barton, M.L.; Dumont-Mathieu, T.; Fein, D. Screening young children for autism spectrum disorders in primary practice. J. Autism Dev. Disord. 2012, 42, 1165–1174. [Google Scholar] [CrossRef] [PubMed]
- Martinez, M.; Thomas, K.C.; Williams, C.S.; Christian, R.; Crais, E.; Pretzel, R.; Hooper, S.R. Family experiences with the diagnosis of autism spectrum disorder: System barriers and facilitators of efficient diagnosis. J. Autism Dev. Disord. 2018, 48, 2368–2378. [Google Scholar] [CrossRef] [PubMed]
- Sheldrick, R.C.; Breuer, D.J.; Hassan, R.; Chan, K.; Polk, D.E.; Benneyan, J. A system dynamics model of clinical decision thresholds for the detection of developmental-behavioral disorders. Implement. Sci. 2016, 11, 156. [Google Scholar] [CrossRef] [PubMed]
- Wetherby, A.; Prizant, B. Communication and Symbolic Behavior Scales Developmental Profile Preliminary Normed Edition; Paul, H., Ed.; Brookes Publishing Co.: Baltimore, MD, USA, 2001. [Google Scholar]
- Wetherby, A.M.; Brosnan-Maddox, S.; Peace, V.; Newton, L. Validation of the Infant—Toddler Checklist as a broadband screener for autism spectrum disorders from 9 to 24 months of age. Autism Int. J. Res. Pract. 2008, 12, 487–511. [Google Scholar] [CrossRef]
- Pierce, K.; Carter, C.; Weinfeld, M.; Desmond, J.; Hazin, R.; Bjork, R.; Gallagher, N. Detecting, studying, and treating autism early: The one-year well-baby check-up approach. J. Pediatr. 2011, 159, 458–465. [Google Scholar] [CrossRef]
- Reznick, J.S.; Baranek, G.T.; Reavis, S.; Watson, L.R.; Crais, E.R. A parent-report instrument for identifying one-year-olds at risk for an eventual diagnosis of autism: The first year inventory. J. Autism Dev. Disord. 2007, 37, 1691–1710. [Google Scholar] [CrossRef]
- Turner-Brown, L.M.; Baranek, G.T.; Reznick, J.S.; Watson, L.R.; Crais, E.R. The First Year Inventory: A longitudinal follow-up of 12-month-old to 3-year-old children. Autism Int. J. Res. Pract. 2013, 17, 527–540. [Google Scholar] [CrossRef]
- Robins, D.L.; Casagrande, K.; Barton, M.; Chen, C.-M.A.; Dumont-Mathieu, T.; Fein, D. Validation of the modified check- list for autism in toddlers, revised with follow-up (M-CHAT-R/F). Pediatrics 2014, 133, 37–45. [Google Scholar] [CrossRef]
- Sices, L.; Feudtner, C.; McLaughlin, J.; Drotar, D.; Williams, M. How do primary care physicians identify young children with developmental delays? A national survey. J. Dev. Behav. Pediatr. 2003, 24, 409–417. [Google Scholar] [CrossRef]
- RStudio Team. RStudio: Integrated Development Environment for R. RStudio, PBC, Boston, MA. Available online: http://www.rstudio.com/ (accessed on 1 November 2022).
- Lunardon, N.; Menardi, G.; Torelli, N. ROSE: A Package for binary imbalanced learning. R J. 2014, 6, 79–89. [Google Scholar] [CrossRef]
- Monteiro, S.A.; Dempsey, J.; Berry, L.N.; Voigt, R.G.; Goin-Kochel, R.P. Screening and referral practices for autism spectrum disorder in primary pediatric care. Pediatrics 2019, 144, e20183326. [Google Scholar] [CrossRef] [PubMed]
- Association of American Medical Colleges. Association of American Medical Colleges (AAMC) 2021 Report on Residents. Available online: https://www.aamc.org/data-reports/students-residents/interactive-data/report-residents/2021/table-b3-number-active-residents-type-medical-school-gme-specialty-and-sex (accessed on 5 November 2022).
- Wallis, K.E.; Guthrie, W.; Bennett, A.E.; Gerdes, M.; Levy, S.E.; Mandell, D.S.; Miller, J.S. Adherence to screening and referral guidelines for autism spectrum disorder in toddlers in pediatric primary care. PLoS ONE 2020, 15, e0232335. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Male | Female | Total |
|---|---|---|---|
| N (%) | N (%) | N | |
| Race | |||
| White | 1654 (52.1) | 1521 (47.9) | 3175 |
| Black | 473 (48.9) | 495 (51.1) | 968 |
| Maternal Education | |||
| High School or Less | 358 (54.1) | 304 (45.9) | 662 |
| Technical School/Some College | 373 (51.2) | 356 (48.8) | 729 |
| Bachelor’s Degree or More | 1396 (50.7) | 1356 (49.3) | 2752 |
| Characteristics | M (SD) |
|---|---|
| PCC Confidence | 3.28 (0.34) |
| PCC Resources | 2.95 (0.39) |
| Use of Formal Autism Screeners | 3.70 (0.48) |
| n(%) | Positive Screen | Negative Screen | All Screens |
|---|---|---|---|
| PCC Concern | 94 (2%) | 77 (2%) | 171 (4%) |
| No PCC Concern | 429 (10%) | 3543 (86%) | 3972 (96%) |
| Total | 523 (12%) | 3620 (88%) | 4143 (100%) |
| Predictor | Beta | p | F1 |
|---|---|---|---|
| (Intercept) | −2.96 ** | 0.001 | 0.703 |
| Confidence | 0.499 ** | 0.002 | |
| Resources | 0.431 * | 0.010 | |
| Formal Screening | 0.026 | 0.477 |
| Predictor | Beta | p | F1 |
|---|---|---|---|
| (Intercept) | 0.970 | 0.000 *** | 0.681 |
| Patient Demographics 1: Majority White vs. Equal Majority-Minority | −0.89 | 0.000 *** | |
| Patient Demographics 2: Majority White vs. Minoritized | −0.472 | 0.001 ** | |
| Years in Practice | 0.011 | 0.301 | |
| PCC Sex | −2.28 | 0.000 *** | |
| PCC Race | −0.21 | 0.379 |
| Predictor | Beta | p | F1 |
|---|---|---|---|
| (Intercept) | 0.099 | 0.220 | 0.754 |
| Child Race | −0.104 | 0.347 | |
| Child Sex | 0.443 | 0.000 *** | |
| Maternal Education 1: Bachelor’s vs. Some College | −0.701 | 0.000 *** | |
| Maternal Education 2: Bachelor’s vs. High School | −0.655 | 0.000 *** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Williams, L.N.; Wieckowski, A.T.; Dieckhaus, M.F.S.; Dai, Y.G.; Zhang, F.; Dumont-Mathieu, T.; Barton, M.; Fein, D.; Robins, D.L. Primary Care Clinician and Child Characteristics Impacting Autism Surveillance. Brain Sci. 2023, 13, 18. https://doi.org/10.3390/brainsci13010018
Williams LN, Wieckowski AT, Dieckhaus MFS, Dai YG, Zhang F, Dumont-Mathieu T, Barton M, Fein D, Robins DL. Primary Care Clinician and Child Characteristics Impacting Autism Surveillance. Brain Sciences. 2023; 13(1):18. https://doi.org/10.3390/brainsci13010018
Chicago/Turabian StyleWilliams, Lashae N., Andrea Trubanova Wieckowski, Mary F. S. Dieckhaus, Yael G. Dai, Fengqing Zhang, Thyde Dumont-Mathieu, Marianne Barton, Deborah Fein, and Diana L. Robins. 2023. "Primary Care Clinician and Child Characteristics Impacting Autism Surveillance" Brain Sciences 13, no. 1: 18. https://doi.org/10.3390/brainsci13010018
APA StyleWilliams, L. N., Wieckowski, A. T., Dieckhaus, M. F. S., Dai, Y. G., Zhang, F., Dumont-Mathieu, T., Barton, M., Fein, D., & Robins, D. L. (2023). Primary Care Clinician and Child Characteristics Impacting Autism Surveillance. Brain Sciences, 13(1), 18. https://doi.org/10.3390/brainsci13010018