Comparison of the Effects of Constraint-Induced Movement Therapy and Unconstraint Exercise on Oxidative Stress and Limb Function—A Study on Human Patients and Rats with Cerebral Infarction
Abstract
:1. Introduction
2. Methods and Materials
2.1. Study Population of the RCT
2.2. Randomization and Allocation Concealment in the RCT
2.3. Interventions in the RCT
2.4. Models in the Animal Study
2.5. Interventions in the Animal Study
2.6. Modified Neurological Severity Scores (mNSS)
2.7. Magnetic Resonance Imaging (MRI) of Rats
2.8. Histology
2.9. QRT-PCR
2.10. Western Blot
2.11. ELISA
2.12. Statistical Analysis
3. Results
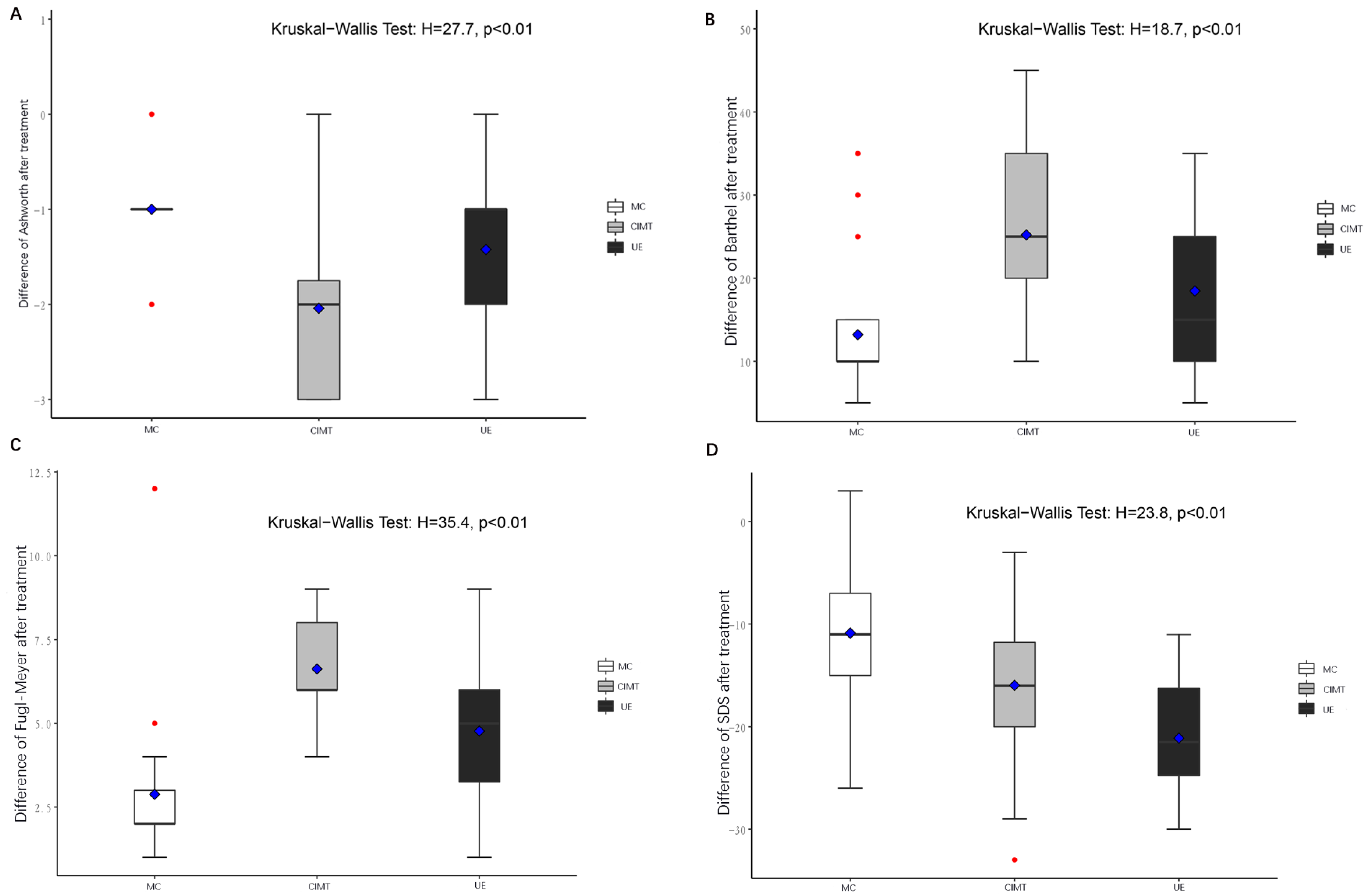
3.1. CIMT Was More Effective Than UE in Improving Limb Function in Stroke Patients
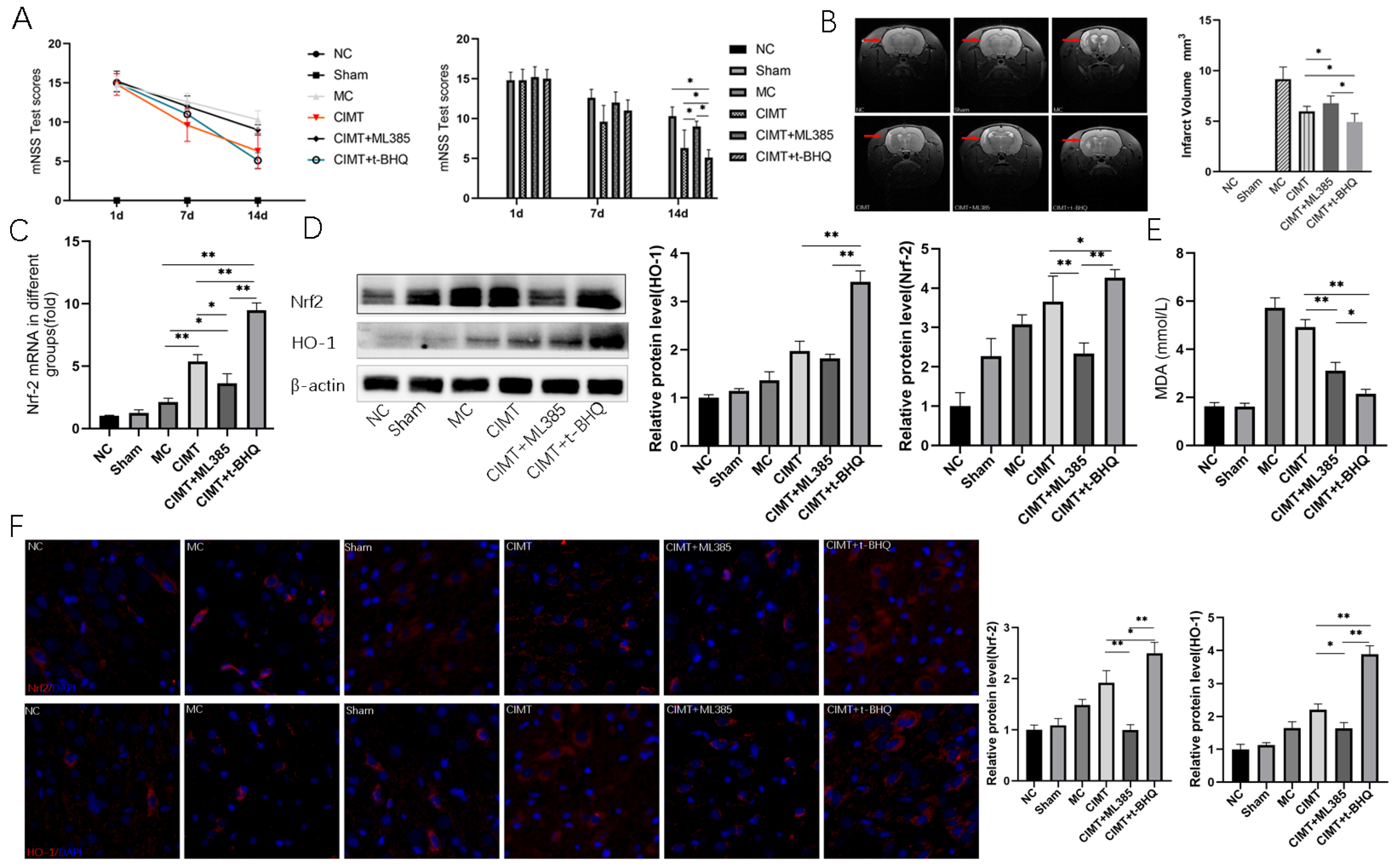
3.2. Keap1-Nrf2 Signaling Pathway Is Linked to the CIMT Induced Benefits
3.3. Nrf2 Plays a Pivotal Role in Regulating CIMT Induced Benefits
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Feigin, V.L.; Stark, B.A.; Johnson, C.O.; Roth, G.A.; Bisignano, C.; Abady, G.G.; Abbasifard, M.; Abbasi-Kangevari, M.; Abd-Allah, F.; Abedi, V.; et al. Global, regional, and national burden of stroke and its risk factors, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol. 2021, 20, 795–820. [Google Scholar] [CrossRef] [PubMed]
- Ekker, M.S.; Boot, E.M.; Singhal, A.B.; Tan, K.S.; Debette, S.; Tuladhar, A.M.; de Leeuw, F.-E. Epidemiology, aetiology, and management of ischaemic stroke in young adults. Lancet Neurol. 2018, 17, 790–801. [Google Scholar] [CrossRef] [PubMed]
- Lindsay, M.P.; Norrving, B.; Sacco, R.L.; Brainin, M.; Hacke, W.; Martins, S.; Pandian, J.; Feigin, V. World Stroke Organization (WSO): Global Stroke Fact Sheet 2019. Int. J. Stroke 2019, 14, 806–817. [Google Scholar] [CrossRef] [PubMed]
- Wu, S.; Wu, B.; Liu, M.; Chen, Z.; Wang, W.; Anderson, C.S.; Sandercock, P.; Wang, Y.; Huang, Y.; Cui, L.; et al. Stroke in China: Advances and challenges in epidemiology, prevention, and management. Lancet Neurol. 2019, 18, 394–405. [Google Scholar] [CrossRef]
- Langhorne, P.; Coupar, F.; Pollock, A. Motor recovery after stroke: A systematic review. Lancet Neurol. 2009, 8, 741–754. [Google Scholar] [CrossRef]
- Mead, G. Exercise after stroke. BMJ 2009, 339, b2795. [Google Scholar] [CrossRef]
- Legg, L.A.; Lewis, S.R.; Schofield-Robinson, O.J.; Drummond, A.; Langhorne, P. Occupational therapy for adults with problems in activities of daily living after stroke. Cochrane Database Syst. Rev. 2017, 7, Cd003585. [Google Scholar]
- Hasan, S.M.M.; Rancourt, S.N.; Austin, M.W.; Ploughman, M. Defining Optimal Aerobic Exercise Parameters to Affect Complex Motor and Cognitive Outcomes after Stroke: A Systematic Review and Synthesis. Neural Plast. 2016, 2016, 2961573. [Google Scholar] [CrossRef] [Green Version]
- Cooke, E.V.; Mares, K.; Clark, A.; Tallis, R.C.; Pomeroy, V.M. The effects of increased dose of exercise-based therapies to enhance motor recovery after stroke: A systematic review and meta-analysis. BMC Med. 2010, 8, 60. [Google Scholar] [CrossRef]
- Hornby, T.G.; Moore, J.L.; Lovell, L.; Roth, E.J. Influence of skill and exercise training parameters on locomotor recovery during stroke rehabilitation. Curr. Opin. Neurol. 2016, 29, 677–683. [Google Scholar] [CrossRef]
- Etoom, M.; Hawamdeh, M.; Hawamdeh, Z.; Alwardat, M.; Giordani, L.; Bacciu, S.; Scarpini, C.; Foti, C. Constraint-induced movement therapy as a rehabilitation intervention for upper extremity in stroke patients: Systematic review and meta-analysis. Int. J. Rehabil. Res. 2016, 39, 197–210. [Google Scholar] [CrossRef] [PubMed]
- Kwakkel, G.; Veerbeek, J.M.; Van Wegen, E.E.H.; Wolf, S.L. Constraint-induced movement therapy after stroke. Lancet Neurol. 2015, 14, 224–234. [Google Scholar] [CrossRef] [Green Version]
- Taub, E.; Uswatte, G.; Mark, V.W.; Morris, D.M.M. The learned nonuse phenomenon: Implications for rehabilitation. Eura Med. 2006, 42, 241–256. [Google Scholar]
- Darling, W.G.; Pizzimenti, M.A.; Rotella, D.L.; Ge, J.; Stilwell-Morecraft, K.S.; Morecraft, R.J. Greater Reduction in Contralesional Hand Use After Frontoparietal Than Frontal Motor Cortex Lesions in Macaca mulatta. Front. Syst. Neurosci. 2021, 15, 592235. [Google Scholar] [CrossRef] [PubMed]
- Tally, Z.; Boetefuer, L.; Kauk, C.; Perez, G.; Schrand, L.; Hoder, J. The efficacy of treadmill training on balance dysfunction in individuals with chronic stroke: A systematic review. Top. Stroke. Rehabil. 2017, 24, 539–546. [Google Scholar] [CrossRef]
- Polese, J.C.; Ada, L.; Dean, C.; Nascimento, L.R.; Teixeira-Salmela, L.F. Treadmill training is effective for ambulatory adults with stroke: A systematic review. J. Physiother. 2013, 59, 73–80. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gebicki, J.M. Oxidative stress, free radicals and protein peroxides. Arch. Biochem. Biophys. 2016, 595, 33–39. [Google Scholar] [CrossRef] [PubMed]
- Orellana-Urzúa, S.; Rojas, I.; Líbano, L.; Rodrigo, R. Pathophysiology of Ischemic Stroke: Role of Oxidative Stress. Curr. Pharm. Des. 2020, 26, 4246–4260. [Google Scholar] [CrossRef]
- Cojocaru, I.M.; Cojocaru, M.; Sapira, V.; Ionescu, A. Evaluation of oxidative stress in patients with acute ischemic stroke. Rom. J. Intern. Med. 2013, 51, 97–106. [Google Scholar]
- Maciejczyk, M.; Bielas, M.; Zalewska, A.; Gerreth, K. Salivary Biomarkers of Oxidative Stress and Inflammation in Stroke Patients: From Basic Research to Clinical Practice. Oxidative Med. Cell. Longev. 2021, 2021, 5545330. [Google Scholar] [CrossRef]
- Gambassi, B.B.; Coelho-Junior, H.J.; Dos Santos, C.P.; Gonçalves, I.D.O.; Mostarda, C.T.; Marzetti, E.; Sotão, S.S.; Uchida, M.C.; De Angelis, K.; Rodrigues, B. Dynamic Resistance Training Improves Cardiac Autonomic Modulation and Oxidative Stress Parameters in Chronic Stroke Survivors: A Randomized Controlled Trial. Oxidative Med. Cell. Longev. 2019, 2019, 5382843. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xing, Y.; Yang, S.; Dong, F.; Wang, M.-M.; Feng, Y.-S.; Zhang, F. The beneficial role of early exercise training following stroke and possible mechanisms. Life Sci. 2018, 198, 32–37. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.; Chen, W.; Zhou, H.; Duan, W.; Huo, X.; Xu, W.; Huang, L.; Zheng, H.; Liu, J.; Shujuan Chinese Stroke Association Stroke Council Guideline Writing Committee; et al. Chinese Stroke Association guidelines for clinical management of cerebrovascular disorders: Executive summary and 2019 update of clinical management of ischaemic cerebrovascular diseases. Stroke Vasc. Neurol. 2020, 5, 159–176. [Google Scholar] [PubMed]
- Takebayashi, T.; Takahashi, K.; Moriwaki, M.; Sakamoto, T.; Domen, K. Improvement of Upper Extremity Deficit after Constraint-Induced Movement Therapy Combined with and without Preconditioning Stimulation Using Dual-hemisphere Transcranial Direct Current Stimulation and Peripheral Neuromuscular Stimulation in Chronic Stroke Patients: A Pilot Randomized Controlled Trial. Front. Neurol. 2017, 8, 568. [Google Scholar]
- Rensink, M.; Schuurmans, M.; Lindeman, E.; Hafsteinsdóttir, T. Task-oriented training in rehabilitation after stroke: Systematic review. J. Adv. Nurs. 2009, 65, 737–754. [Google Scholar] [CrossRef]
- Ivey, F.M.; Hafer-Macko, C.E.; Macko, R.F. Task-oriented treadmill exercise training in chronic hemiparetic stroke. J. Rehabil. Res. Dev. 2008, 45, 249–259. [Google Scholar] [CrossRef]
- Corbetta, D.; Sirtori, V.; Moja, L.; Gatti, R. Constraint-induced movement therapy in stroke patients: Systematic review and meta-analysis. Eur. J. Phys. Rehabil. Med. 2010, 46, 537–544. [Google Scholar]
- Sirtori, V.; Corbetta, D.; Moja, L.; Gatti, R. Constraint-induced movement therapy for upper extremities in stroke patients. Cochrane Database Syst. Rev. 2009, 7, Cd004433. [Google Scholar]
- da Costa Daniele, T.M.; de Bruin, P.F.C.; de Matos, R.S.; de Bruin, G.S.; Junior, C.M.C.; de Bruin, V.M.S. Exercise effects on brain and behavior in healthy mice, Alzheimer’s disease and Parkinson’s disease model—A systematic review and meta-analysis. Behav. Brain Res. 2020, 383, 112488. [Google Scholar] [CrossRef]
- Hu, X.; Li, B.; Wang, X. Scalp acupuncture therapy combined with exercise can improve the ability of stroke patients to participate in daily activities. Complement. Ther. Clin. Pract. 2021, 43, 101343. [Google Scholar] [CrossRef]
- Sherrington, C.; Michaleff, Z.A.; Fairhall, N.; Paul, S.S.; Tiedemann, A.; Whitney, J.; Cumming, R.G.; Herbert, R.D.; Close, J.C.T.; Lord, S.R. Exercise to prevent falls in older adults: An updated systematic review and meta-analysis. Br. J. Sports Med. 2017, 51, 1750–1758. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Han, P.; Zhang, W.; Kang, L.; Ma, Y.; Fu, L.; Jia, L.; Yu, H.; Chen, X.; Hou, L.; Wang, L.; et al. Clinical Evidence of Exercise Benefits for Stroke. Adv. Exp. Med. Biol. 2017, 1000, 131–151. [Google Scholar]
- An, M.; Shaughnessy, M. The effects of exercise-based rehabilitation on balance and gait for stroke patients: A systematic review. J. Neurosci. Nurs. 2011, 43, 298–307. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Austin, M.W.; Ploughman, M.; Glynn, L.; Corbett, D. Aerobic exercise effects on neuroprotection and brain repair following stroke: A systematic review and perspective. Neurosci. Res. 2014, 87, 8–15. [Google Scholar] [CrossRef] [PubMed]
- Ammann, B.C.; Knols, R.H.; Baschung, P.; De Bie, R.A.; de Bruin, E.D. Application of principles of exercise training in sub-acute and chronic stroke survivors: A systematic review. BMC Neurol. 2014, 14, 167. [Google Scholar] [CrossRef] [Green Version]
- Schimidt, H.L.; Vieira, A.; Altermann, C.; Martins, A.; Sosa, P.; Santos, F.W.; Mello-Carpes, P.B.; Izquierdo, I.; Carpes, F.P. Memory deficits and oxidative stress in cerebral ischemia-reperfusion: Neuroprotective role of physical exercise and green tea supplementation. Neurobiol. Learn. Mem. 2014, 114, 242–250. [Google Scholar] [CrossRef] [Green Version]
- Radak, Z.; Kumagai, S.; Taylor, A.W.; Naito, H.; Goto, S. Effects of exercise on brain function: Role of free radicals. Appl. Physiol. Nutr. Metab. 2007, 32, 942–946. [Google Scholar] [CrossRef]
- Quindry, J.C.; Stone, W.L.; King, J.; Broeder, C.E. The effects of acute exercise on neutrophils and plasma oxidative stress. Med. Sci. Sports Exerc. 2003, 35, 1139–1145. [Google Scholar] [CrossRef] [PubMed]
- Clanton, T.L.; Zuo, L.; Klawitter, P. Oxidants and skeletal muscle function: Physiologic and pathophysiologic implications. Proc. Soc. Exp. Biol. Med. 1999, 222, 253–262. [Google Scholar] [CrossRef]
- Vincent, H.K.; Powers, S.K.; Demirel, H.A.; Coombes, J.S.; Naito, H. Exercise training protects against contraction-induced lipid peroxidation in the diaphragm. Eur. J. Appl. Physiol. Occup. Physiol. 1999, 79, 268–273. [Google Scholar] [CrossRef]
- Powers, S.K.; Deminice, R.; Ozdemir, M.; Yoshihara, T.; Bomkamp, M.P.; Hyatt, H. Exercise-induced oxidative stress: Friend or foe? J. Sport Health Sci. 2020, 9, 415–425. [Google Scholar] [CrossRef] [PubMed]
- Shi, Y.X.; Tian, J.H.; Yang, K.H.; Zhao, Y. Modified constraint-induced movement therapy versus traditional rehabilitation in patients with upper-extremity dysfunction after stroke: A systematic review and meta-analysis. Arch. Phys. Med. Rehabil. 2011, 92, 972–982. [Google Scholar] [CrossRef] [PubMed]
- Rudilosso, S.; Rodríguez-Vázquez, A.; Urra, X.; Arboix, A. The Potential Impact of Neuroimaging and Translational Research on the Clinical Management of Lacunar Stroke. Int. J. Mol. Sci. 2022, 23, 1497. [Google Scholar] [CrossRef] [PubMed]



| Genes | Directions | Sequences |
|---|---|---|
| cap3 | Forward | CTACCGCACCCGGTTACTAT |
| Reverse | TTCCGGTTAACACGAGTGAG | |
| catenin | Forward | GACAAGCCACAGGACTACAAGAA |
| Reverse | CGTATCCACCAGAGTGAAAAGAA | |
| wnt3a | Forward | GAATGGTCTCTCGGGAGTTTGC |
| Reverse | CAGCAGGTCTTCACTTCGCAAC | |
| Nrf2 | Forward | GCCTTCCTCTGCTGCCATTAGTC |
| Reverse | TCATTGAACTCCACCGTGCCTTC | |
| keap1 | Forward | TGCTCAACCGCTTGCTGTATGC |
| Reverse | TCATCCGCCACTCATTCCTCTCC |
| N | Sex | Age (Years) | Disease Duration (Months) | Time between Disease Onset and Rehabilitation Treatment (Months) | ||
|---|---|---|---|---|---|---|
| F | M | |||||
| Control | 25 | 9 | 16 | 61.72 ± 9.09 | 4.04 ± 1.74 | 2.56 ± 1.56 |
| CIMT | 24 | 9 | 15 | 61.38 ± 10.15 | 3.33 ± 1.71 | 2.17 ± 1.13 |
| UE | 26 | 8 | 18 | 60.12 ± 11.31 | 3.12 ± 1.66 | 1.96 ± 1.28 |
| p | 0.706 | 0.848 | 0.141 | 0.318 | ||
| FMA-UE | Barthel | SDS | |
|---|---|---|---|
| Control | 57.36 ± 1.32 | 56.80 ± 10.50 | 58.24 ± 5.25 |
| CIMT | 57.23 ± 1.21 | 56.73 ± 10.38 | 59.08 ± 6.95 |
| UE | 57.58 ± 1.50 | 57.08 ± 8.59 | 57.58 ± 4.61 |
| p | 0.773 | 0.936 | 0.456 |
| The Baseline Scores | The Score after the Interventions | ||||||
|---|---|---|---|---|---|---|---|
| Scores | Control (n) | UE (n) | CIMT (n) | Scores | Control (n) | UE (n) | CIMT (n) |
| 0 | 0 | 0 | 0 | 0 | 5 | 4 | 4 |
| 1 | 0 | 0 | 0 | 1 | 6 | 8 | 16 |
| 2 | 6 | 5 | 5 | 2 | 15 | 13 | 4 |
| 3 | 17 | 13 | 12 | 3 | |||
| 4 | 3 | 7 | 7 | 4 | |||
| total (n) | 26 | 25 | 24 | total (n) | 26 | 25 | 24 |
| FMA-UE | Barthel | SDS | |||||||
|---|---|---|---|---|---|---|---|---|---|
| MC | CIMT | UE | MC | CIMT | UE | MC | CIMT | UE | |
| Baseline | 57.36 ± 1.32 | 57.23 ± 1.21 | 57.58 ± 1.50 | 56.80 ± 10.50 | 56.73 ± 10.38 | 57.08 ± 8.59 | 58.24 ± 5.25 | 59.08 ± 6.95 | 57.58 ± 4.61 |
| Week 3 | 60.24 ± 230 | 64.21 ± 0.78 | 62.00 ± 2.04 | 70.00 ± 8.660 | 82.29 ± 7.07 | 75.19 ± 5.91 | 47.36 ± 7.04 | 43.13 ± 5.05 | 36.46 ± 3.43 |
| Changes | 2.88 ± 2.128 | 6.63 ± 1.527 | 4.77 ± 2.006 | 13.20 ± 7.343 | 25.21 ± 9.264 | 18.46 ± 8.92 | −10.88 ± 6.65 | −15.96 ± 7.25 | −21.12 ± 5.36 |
| p | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, D.; Li, L.; Pan, H.; Huang, L.; Sun, X.; He, C.; Wei, Q. Comparison of the Effects of Constraint-Induced Movement Therapy and Unconstraint Exercise on Oxidative Stress and Limb Function—A Study on Human Patients and Rats with Cerebral Infarction. Brain Sci. 2023, 13, 4. https://doi.org/10.3390/brainsci13010004
Wang D, Li L, Pan H, Huang L, Sun X, He C, Wei Q. Comparison of the Effects of Constraint-Induced Movement Therapy and Unconstraint Exercise on Oxidative Stress and Limb Function—A Study on Human Patients and Rats with Cerebral Infarction. Brain Sciences. 2023; 13(1):4. https://doi.org/10.3390/brainsci13010004
Chicago/Turabian StyleWang, Dong, Lijuan Li, Hongxia Pan, Liyi Huang, Xin Sun, Chengqi He, and Quan Wei. 2023. "Comparison of the Effects of Constraint-Induced Movement Therapy and Unconstraint Exercise on Oxidative Stress and Limb Function—A Study on Human Patients and Rats with Cerebral Infarction" Brain Sciences 13, no. 1: 4. https://doi.org/10.3390/brainsci13010004





