Motives for Cannabis Use and Risky Decision Making Influence Cannabis Use Trajectories in Teens
Abstract
:1. Introduction
Aims and Hypotheses
2. Materials and Methods
2.1. Participants and Procedure
2.2. Measures
2.3. Data Analytic Plan
3. Results
3.1. Substance Use Characteristics
3.2. The Unconditional Linear Growth Model
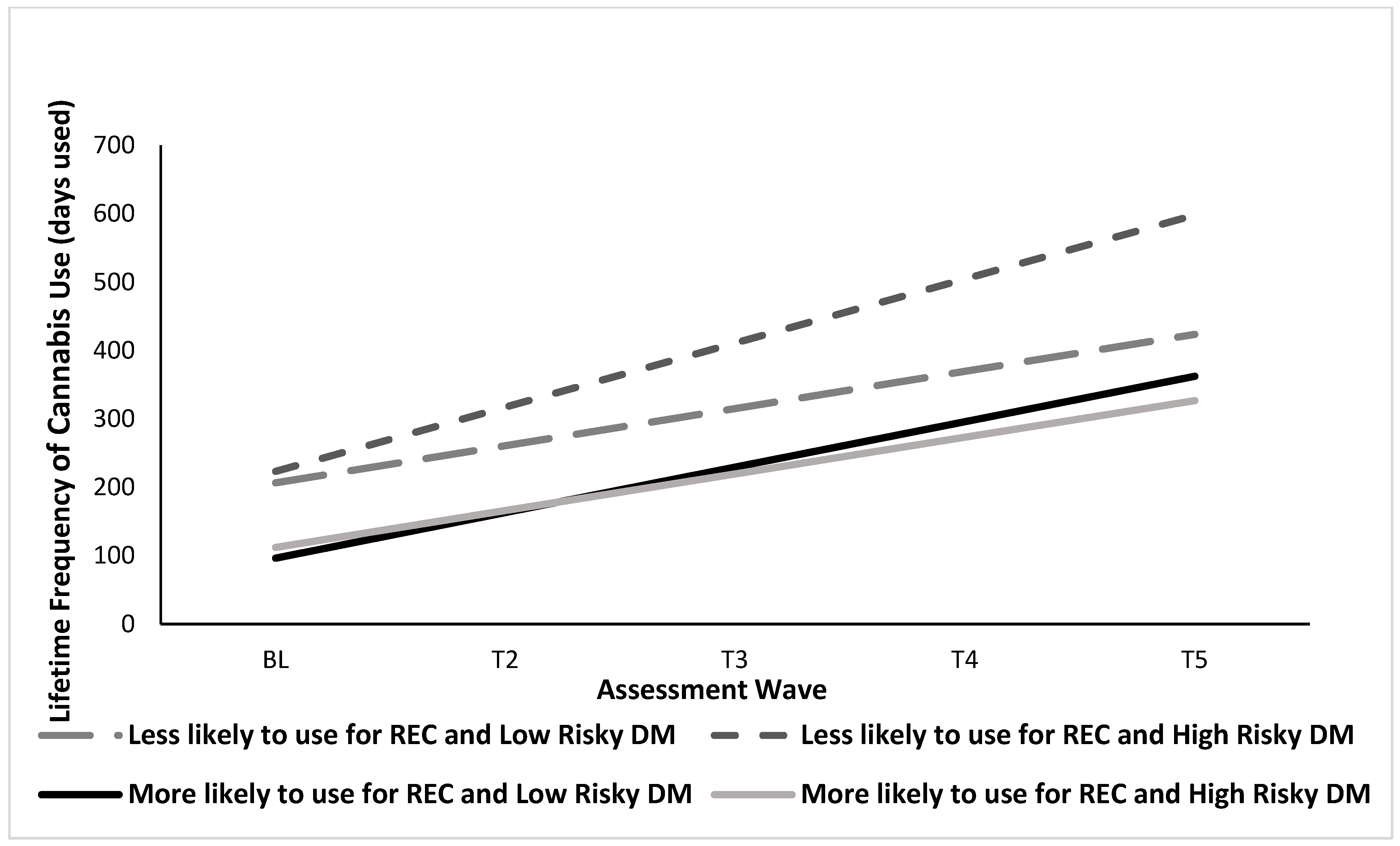
3.3. The Conditional Latent Growth Curve Model
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Miech, R.A.; Johnston, L.D.; Patrick, M.E.; O’Malley, P.M.; Bachman, J.G.; Schulenberg, J.E. Monitoring the Future National Survey Results on Drug Use, 1975–2022: Secondary School Students; Institute for Social Research, The University of Michigan: Ann Arbor, MI, USA, 2023; Available online: http://monitoringthefuture.org (accessed on 15 May 2023).
- Chassin, L.; Colder, C.R.; Hussong, A.; Sher, K. Substance use and substance use disorders. In Developmental Psychopathology: Maladaptation and Psychopathology; Cicchetti, D., Ed.; John Wiley & Sons: Hoboken, NJ, USA, 2016; Volume 3, pp. 833–897. [Google Scholar]
- Chen, C.Y.; Storr, C.L.; Anthony, J.C. Early-onset drug use and risk for drug dependence problems. Addict. Behav. 2009, 34, 319–322. [Google Scholar] [CrossRef] [PubMed]
- King, K.M.; Chassin, L. A prospective study of the effects of age of initiation of alcohol and drug use on young adult substance dependence. J. Stud. Alcohol Drugs 2007, 68, 256–265. [Google Scholar] [CrossRef] [PubMed]
- Hammond, C.J.; Chaney, A.; Hendrickson, B.; Sharma, P. Cannabis use among U.S. adolescents in the era of marijuana legalization: A review of changing use patterns, comorbidity, and health correlates. Int. Rev. Psychiatry 2020, 32, 221–234. [Google Scholar] [CrossRef]
- Bresin, K.; Mekawi, Y. Do marijuana use motives matter? Meta-analytic associations with marijuana use frequency and problems. Addict. Behav. 2019, 99, 106102. [Google Scholar] [CrossRef] [PubMed]
- Chabrol, H.; Beck, C.; Laconi, S. Contribution of health motive to cannabis use among high-school students. Addict. Behav. 2017, 64, 54–56. [Google Scholar] [CrossRef]
- Patrick, M.E.; Evans-Polce, R.J.; Kloska, D.D.; Maggs, J.L. Reasons High School Students Use Marijuana: Prevalence and Correlations With Use Across Four Decades. J. Stud. Alcohol Drugs 2019, 80, 15–25. [Google Scholar] [CrossRef]
- De Bellis, M.D.; Wang, L.; Bergman, S.R.; Yaxley, R.H.; Hooper, S.R.; Huettel, S.A. Neural mechanisms of risky decision-making and reward response in adolescent onset cannabis use disorder. Drug Alcohol Depend. 2013, 133, 134–145. [Google Scholar] [CrossRef]
- Solowij, N.; Jones, K.A.; Rozman, M.E.; Davis, S.M.; Ciarrochi, J.; Heaven, P.C.; Pesa, N.; Lubman, D.I.; Yücel, M. Reflection impulsivity in adolescent cannabis users: A comparison with alcohol-using and non-substance-using adolescents. Psychopharmacology 2012, 219, 575–586. [Google Scholar] [CrossRef]
- Thompson, E.L.; Adams, A.R.; Pacheco-Colón, I.; Lopez-Quintero, C.; Limia, J.M.; Pulido, W.; Granja, K.; Paula, D.C.; Gonzalez, I.; Ross, J.M.; et al. An exploratory follow-up study of cannabis use and decision-making under various risk conditions within adolescence. Neuropsychology 2023, 37, 544–556. [Google Scholar] [CrossRef]
- Anderson, K.G.; Sitney, M.; White, H.R. Marijuana motivations across adolescence: Impacts on use and consequences. Subst. Use Misuse 2015, 50, 292–301. [Google Scholar] [CrossRef]
- Johnston, L.D.; O’Malley, P.M. Why do the nation’s students use drugs and alcohol? Self-reported reasons from nine national surveys. J. Drug Issues 1986, 16, 29–66. [Google Scholar] [CrossRef]
- Patrick, M.E.; Bray, B.C.; Berglund, P.A. Reasons for Marijuana Use Among Young Adults and Long-Term Associations with Marijuana Use and Problems. J. Stud. Alcohol Drugs 2016, 77, 881–888. [Google Scholar] [CrossRef]
- Patrick, M.E.; Schulenberg, J.E.; O’Malley, P.M.; Johnston, L.D.; Bachman, J.G. Adolescents’ reported reasons for alcohol and marijuana use as predictors of substance use and problems in adulthood. J. Stud. Alcohol Drugs 2011, 72, 106–116. [Google Scholar] [CrossRef] [PubMed]
- Shrier, L.A.; Walls, C.; Rhoads, A.; Blood, E.A. Individual and contextual predictors of severity of marijuana use events among young frequent users. Addictive behaviors 2013, 38, 1448–1456. [Google Scholar] [CrossRef] [PubMed]
- Fox, C.L.; Towe, S.L.; Stephens, R.S.; Walker, D.D.; Roffman, R.A. Motives for cannabis use in high-risk adolescent users. Psychol. Addict. Behav. J. Soc. Psychol. Addict. Behav. 2011, 25, 492–500. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.M.; Neighbors, C.; Hendershot, C.S.; Grossbard, J.R. Development and preliminary validation of a comprehensive marijuana motives questionnaire. J. Stud. Alcohol Drugs 2009, 70, 279–287. [Google Scholar] [CrossRef]
- Noël, X.; Brevers, D.; Bechara, A. A neurocognitive approach to understanding the neurobiology of addiction. Curr. Opin. Neurobiol. 2013, 23, 632–638. [Google Scholar] [CrossRef]
- Shulman, E.P.; Smith, A.R.; Silva, K.; Icenogle, G.; Duell, N.; Chein, J.; Steinberg, L. The dual systems model: Review, reappraisal, and reaffirmation. Dev. Cogn. Neurosci. 2016, 17, 103–117. [Google Scholar] [CrossRef]
- Brand, M.; Grabenhorst, F.; Starcke, K.; Vandekerckhove, M.M.; Markowitsch, H.J. Role of the amygdala in decisions under ambiguity and decisions under risk: Evidence from patients with Urbach-Wiethe disease. Neuropsychologia 2007, 45, 1305–1317. [Google Scholar] [CrossRef]
- Bava, S.; Tapert, S.F. Adolescent brain development and the risk for alcohol and other drug problems. Neuropsychol. Rev. 2010, 20, 398–413. [Google Scholar] [CrossRef]
- Shannon, E.E.; Mathias, C.W.; Dougherty, D.M.; Liguori, A. Cognitive impairments in adolescent cannabis users are related to THC levels. Addict. Disord. Their Treat. 2010, 9, 158–163. [Google Scholar] [CrossRef]
- Arain, M.; Haque, M.; Johal, L.; Mathur, P.; Nel, W.; Rais, A.; Sandhu, R.; Sharma, S. Maturation of the adolescent brain. Neuropsychiatr. Dis. Treat. 2013, 9, 449–461. [Google Scholar] [CrossRef] [PubMed]
- Chein, J.; Albert, D.; O’Brien, L.; Uckert, K.; Steinberg, L. Peers increase adolescent risk taking by enhancing activity in the brain’s reward circuitry. Dev. Sci. 2011, 14, F1–F10. [Google Scholar] [CrossRef] [PubMed]
- Cascio, C.N.; Carp, J.; O’Donnell, M.B.; Tinney, F.J.; Bingham, C.R.; Shope, J.T.; Ouimet, M.C.; Pradhan, A.K.; Simons-Morton, B.G.; Falk, E.B. Buffering Social Influence: Neural Correlates of Response Inhibition Predict Driving Safety in the Presence of a Peer. J. Cogn. Neurosci. 2015, 27, 83–95. [Google Scholar] [CrossRef]
- Vorobyev, V.; Kwon, M.S.; Moe, D.; Parkkola, R.; Hämäläinen, H. Risk-taking behavior in a computerized driving task: Brain activation correlates of decision-making, outcome, and peer influence in male adolescents. PLoS ONE 2015, 10, e0129516. [Google Scholar] [CrossRef]
- Brand, M.; Roth-Bauer, M.; Driessen, M.; Markowitsch, H.J. Executive functions and risky decision-making in patients with opiate dependence. Drug Alcohol Depend. 2008, 97, 64–72. [Google Scholar] [CrossRef]
- Starcke, K.; Pawlikowski, M.; Wolf, O.T.; Altstötter-Gleich, C.; Brand, M. Decision-making under risk conditions is susceptible to interference by a secondary executive task. Cogn. Process. 2011, 12, 177–182. [Google Scholar] [CrossRef]
- Pacheco-Colón, I.; Lopez-Quintero, C.; Coxe, S.; Limia, J.M.; Pulido, W.; Granja, K.; Paula, D.C.; Gonzalez, I.; Ross, J.M.; Duperrouzel, J.C.; et al. Risky decision-making as an antecedent or consequence of adolescent cannabis use: Findings from a 2-year longitudinal study. Addiction 2022, 117, 392–410. [Google Scholar] [CrossRef]
- Barch, D.M.; Harms, M.P.; Tillman, R.; Hawkey, E.; Luby, J.L. Early childhood depression, emotion regulation, episodic memory, and hippocampal development. J. Abnorm. Psychol. 2019, 128, 81–95. [Google Scholar] [CrossRef]
- Blest-Hopley, G.; Giampietro, V.; Bhattacharyya, S. A Systematic Review of Human Neuroimaging Evidence of Memory-Related Functional Alterations Associated with Cannabis Use Complemented with Preclinical and Human Evidence of Memory Performance Alterations. Brain Sci. 2020, 10, 102. [Google Scholar] [CrossRef]
- Figueiredo, P.R.; Tolomeo, S.; Steele, J.D.; Baldacchino, A. Neurocognitive consequences of chronic cannabis use: A systematic review and meta-analysis. Neurosci. Biobehav. Rev. 2020, 108, 358–369. [Google Scholar] [CrossRef] [PubMed]
- Wilkinson, G.S.; Robertson, G.J. WRAT 4: Wide Range Achievement Test; Professional Manual; Psychological Assessment Resources: Lutz, FL, USA, 2006. [Google Scholar]
- Gonzalez, R.; Schuster, R.M.; Mermelstein, R.J.; Vassileva, J.; Martin, E.M.; Diviak, K.R. Performance of young adult cannabis users on neurocognitive measures of impulsive behavior and their relationship to symptoms of cannabis use disorders. J. Clin. Exp. Neuropsychol. 2012, 34, 962–976. [Google Scholar] [CrossRef] [PubMed]
- Rippeth, J.D.; Heaton, R.K.; Carey, C.L.; Marcotte, T.D.; Moore, D.J.; Gonzalez, R.; Wolfson, T.; Grant, I.; HNRC Group. Methamphetamine dependence increases risk of neuropsychological impairment in HIV infected persons. J. Int. Neuropsychol. Soc. JINS 2004, 10, 1–14. [Google Scholar] [CrossRef]
- First, M.B.; Spitzer, R.L.; Gibbon, M.; Williams, J.B.W. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Non-Patient Edition. (SCID-I/NP); New York State Psychiatric Institute: New York, NY, USA, 2002. [Google Scholar]
- Fagerström, K.O. Measuring degree of physical dependence to tobacco smoking with reference to individualization of treatment. Addict. Behav. 1978, 3, 235–241. [Google Scholar] [CrossRef] [PubMed]
- Babson, K.A.; Bonn-Miller, M.O. Sleep Disturbances: Implications for Cannabis Use, Cannabis Use Cessation, and Cannabis Use Treatment. Curr. Addict. Rep. 2014, 1, 109–114. [Google Scholar] [CrossRef]
- Walsh, Z.; Callaway, R.; Belle-Isle, L.; Capler, R.; Kay, R.; Lucas, P.; Holtzman, S. Cannabis for therapeutic purposes: Patient characteristics, access, and reasons for use. Int. J. Drug Policy 2013, 24, 511–516. [Google Scholar] [CrossRef]
- Brand, M.; Fujiwara, E.; Borsutzky, S.; Kalbe, E.; Kessler, J.; Markowitsch, H.J. Decision-making deficits of Korsakoff patients in a new gambling task with explicit rules: Associations with executive functions. Neuropsychology 2005, 19, 267–277. [Google Scholar] [CrossRef]
- Muthén, L.K.; Muthén, B.O. Mplus User’s Guid, 8th ed.; Muthén & Muthén: Los Angeles, CA, USA, 2017. [Google Scholar]
- Hu, L.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Aiken, L.S.; West, S.G.; Reno, R.R. Multiple Regression: Testing and Interpreting Interactions; Sage: Thousand Oaks, CA, USA, 1991. [Google Scholar]
- Wardell, J.D.; Rueda, S.; Elton-Marshall, T.; Mann, R.E.; Hamilton, H.A. Prevalence and Correlates of Medicinal Cannabis Use Among Adolescents. J. Adolesc. Health 2021, 68, 103–109. [Google Scholar] [CrossRef]
- Koob, G.F.; Le Moal, M. Drug abuse: Hedonic homeostatic dysregulation. Science 1997, 278, 52–58. [Google Scholar] [CrossRef]
- Simons, J.; Correia, C.J.; Carey, K.B.; Borsari, B.E. Validating a five-factor marijuana motives measure: Relations with use, problems, and alcohol motives. J. Couns. Psychol. 1998, 45, 265–273. [Google Scholar] [CrossRef]
- Thayer, R.E.; Feldstein Ewing, S.W. Adolescent psychotherapy for addiction medicine: From brain development to neurocognitive treatment mechanisms. Prog. Brain Res. 2016, 224, 305–322. [Google Scholar] [CrossRef] [PubMed]
- Hawes, S.W.; Pacheco-Colón, I.; Ross, J.M.; Gonzalez, R. Adolescent Cannabis Use and Conduct Problems: The Mediating Influence of Callous-Unemotional Traits. Int. J. Ment. Health Addict. 2020, 18, 613–627. [Google Scholar] [CrossRef] [PubMed]

| (N = 171) | BL | T2 | T3 | T4 | T5 |
|---|---|---|---|---|---|
| Demographics (% or M ± SD) | |||||
| % Female | 42.7 | - | - | - | - |
| Race and Ethnicity | |||||
| % Hispanic White | 70.2 | - | - | - | - |
| % Hispanic Black or African American | 2.9 | - | - | - | - |
| % Hispanic American Indian/Alaska Native | 1.2 | - | - | - | - |
| % Hispanic Native Hawaiian or Other Pacific Islander | 0.58 | - | - | - | - |
| % Hispanic More than One Race | 12.9 | - | - | - | - |
| % Hispanic Unknown Race | 3.5 | - | - | - | - |
| % Non-Hispanic White | 3.5 | - | - | - | - |
| % Non-Hispanic Black or African American | 4.1 | - | - | - | - |
| % Non-Hispanic More than one Race | 1.2 | - | - | - | - |
| WRAT-4 Reading Standard Score | 107.7 ± 14.7 | - | - | - | - |
| Years of Education | 9.0 ± 0.8 | 9.8 ± 0.9 | 10.3 ± 0.8 | 10.8 ± 0.8 | 11.3 ± 0.8 |
| Age | 15.5 ± 0.6 | 16.1 ± 0.8 | 16.5 ± 0.6 | 17.1 ± 0.7 | 17.5 ± 0.6 |
| Decision-Making Performance (M ± SD) | |||||
| Game of Dice Task (# of risky decisions) | 8.3 ± 5.2 | - | - | - | - |
| Prevalence Rate (%) | Estimate | S.E. | p-Value | |
|---|---|---|---|---|
| Health Motives | ||||
| To decrease pain | 26 | 0.72 | 0.06 | p < 0.001 |
| To sleep better | 49 | 0.77 | 0.07 | p < 0.001 |
| To reduce muscle spasms | 4 | 0.61 | 0.11 | p < 0.001 |
| To increase appetite | 27 | 0.67 | 0.08 | p < 0.001 |
| To reduce nausea | 11 | 0.72 | 0.08 | p < 0.001 |
| To reduce anxiety | 76 | 0.94 | 0.07 | p < 0.001 |
| To feel happier | 57 | 0.74 | 0.06 | p < 0.001 |
| To feel less sad | 31 | 0.58 | 0.08 | p < 0.001 |
| Recreational Motives | ||||
| To be more social | 84 | 0.39 | 0.13 | p < 0.01 |
| To get high | 92 | 0.65 | 0.12 | p < 0.001 |
| To have fun | 94 | 0.82 | 0.13 | p < 0.001 |
| To be less bored | 53 | 0.78 | 0.15 | p < 0.001 |
| (N = 171) | BL | T2 | T3 | T4 | T5 |
|---|---|---|---|---|---|
| Lifetime Days of Use [Md, IQR] | |||||
| Alcohol | 8 [2, 28] | 13 [3, 40] | 21 [7, 60] | 29 [10, 73] | 37 [14, 88] |
| Nicotine | 1 [0, 6] | 1 [0, 12] | 2 [0, 18] | 4 [0, 26] | 8 [1, 46] |
| Cannabis | 60 [14, 198] | 96 [24, 284] | 138 [36, 384] | 191 [48, 488] | 280 [65, 595] |
| Lifetime Reports of Substance Use | |||||
| % Reporting Alcohol Use in Lifetime | 88.9 | 94.2 | 97.1 | 98.2 | 98.8 |
| % Reporting Nicotine Use in Lifetime | 51.5 | 55.6 | 64.3 | 67.8 | 75.4 |
| Current Substance Dependence | |||||
| % Current Alcohol Dependence | 0 | 0 | 0 | 0.6 | 0 |
| % Current Cannabis Dependence | 4.1 | 4.1 | 4.1 | 5.3 | 2.9 |
| Current Substance Abuse | |||||
| % Current Alcohol Abuse | 0.6 | 2.9 | 0.6 | 0 | 2.9 |
| % Current Cannabis Abuse | 15.2 | 11.1 | 22.2 | 21.1 | 27.6 |
| Standardized Estimate | Standard Error | 95% CI | p-Value | |
|---|---|---|---|---|
| Health → Intercept | 0.52 | 0.08 | [0.37, 0.68] | p < 0.001 *** |
| Health → Slope | 0.47 | 0.09 | [0.30, 0.64] | p < 0.001 *** |
| Health × DM → Intercept | −0.12 | 0.09 | [−0.29, 0.05] | p = 0.16 |
| Health × DM → Slope | 0.07 | 0.08 | [−0.09, 0.22] | p = 0.39 |
| REC → Intercept | −0.29 | 0.12 | [−0.52, −0.06] | p = 0.01 * |
| REC → Slope | −0.11 | 0.13 | [−0.36, 0.14] | p = 0.38 |
| REC × DM → Intercept | −0.01 | 0.12 | [−0.24, 0.24] | p = 0.98 |
| REC × DM → Slope | −0.23 | 0.10 | [−0.43, −0.03] | p = 0.03 * |
| DM → Intercept | 0.04 | 0.06 | [−0.09, 0.17] | p = 0.52 |
| DM → Slope | 0.13 | 0.07 | [−0.01, 0.26] | p = 0.07 |
| Sex → Intercept | −0.14 | 0.06 | [−0.27, −0.02] | p = 0.03 * |
| Sex → Slope | −0.21 | 0.07 | [−0.35, −0.08] | p < 0.01 ** |
| Age → Intercept | 0.12 | 0.05 | [0.01, 0.22] | p = 0.03 * |
| Age → Slope | 0.03 | 0.07 | [−0.11, 0.18] | p = 0.65 |
| WRAT-4 → Intercept | −0.06 | 0.06 | [−0.17, 0.05] | p = 0.30 |
| WRAT-4 → Slope | −0.07 | 0.08 | [−0.22, 0.08] | p = 0.35 |
| Alc_BL → CU_BL | 0.18 | 0.09 | [0.01, 0.36] | p = 0.04 * |
| Nic_BL → CU_BL | −0.03 | 0.05 | [−0.12, 0.06] | p = 0.58 |
| Alc_T2 → CU_T2 | 0.15 | 0.07 | [0.00, 0.29] | p = 0.05 * |
| Nic_T2 → CU_T2 | −0.02 | 0.04 | [−0.09, 0.06] | p = 0.68 |
| Alc_T3 → CU_T3 | 0.11 | 0.06 | [−0.01, 0.23] | p = 0.06 |
| Nic_T3 → CU_T3 | 0.02 | 0.03 | [−0.03, 0.07] | p = 0.45 |
| Alc_T4 → CU_T4 | 0.09 | 0.06 | [−0.03, 0.21] | p = 0.12 |
| Nic_T4 → CU_T4 | 0.05 | 0.02 | [0.01, 0.09] | p = 0.03 * |
| Alc_T5 → CU_T5 | 0.09 | 0.06 | [−0.03, 0.20] | p = 0.14 |
| Nic_T5 → CU_T5 | 0.06 | 0.03 | [0.01, 0.11] | p = 0.02 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lehman, S.M.; Thompson, E.L.; Adams, A.R.; Hawes, S.W.; Pacheco-Colón, I.; Granja, K.; Paula, D.C.; Gonzalez, R. Motives for Cannabis Use and Risky Decision Making Influence Cannabis Use Trajectories in Teens. Brain Sci. 2023, 13, 1405. https://doi.org/10.3390/brainsci13101405
Lehman SM, Thompson EL, Adams AR, Hawes SW, Pacheco-Colón I, Granja K, Paula DC, Gonzalez R. Motives for Cannabis Use and Risky Decision Making Influence Cannabis Use Trajectories in Teens. Brain Sciences. 2023; 13(10):1405. https://doi.org/10.3390/brainsci13101405
Chicago/Turabian StyleLehman, Sarah M., Erin L. Thompson, Ashley R. Adams, Samuel W. Hawes, Ileana Pacheco-Colón, Karen Granja, Dayana C. Paula, and Raul Gonzalez. 2023. "Motives for Cannabis Use and Risky Decision Making Influence Cannabis Use Trajectories in Teens" Brain Sciences 13, no. 10: 1405. https://doi.org/10.3390/brainsci13101405






