Sleep Duration on Workdays Is Correlated with Subjective Workload and Subjective Impact of High Workload on Sleep in Young Healthy Adults
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethics and Participants
2.2. Study Design
2.3. Measures, Data Processing, and Statistics
3. Results
3.1. Sample Characteristics
3.2. Variables Assessed by Questionnaire
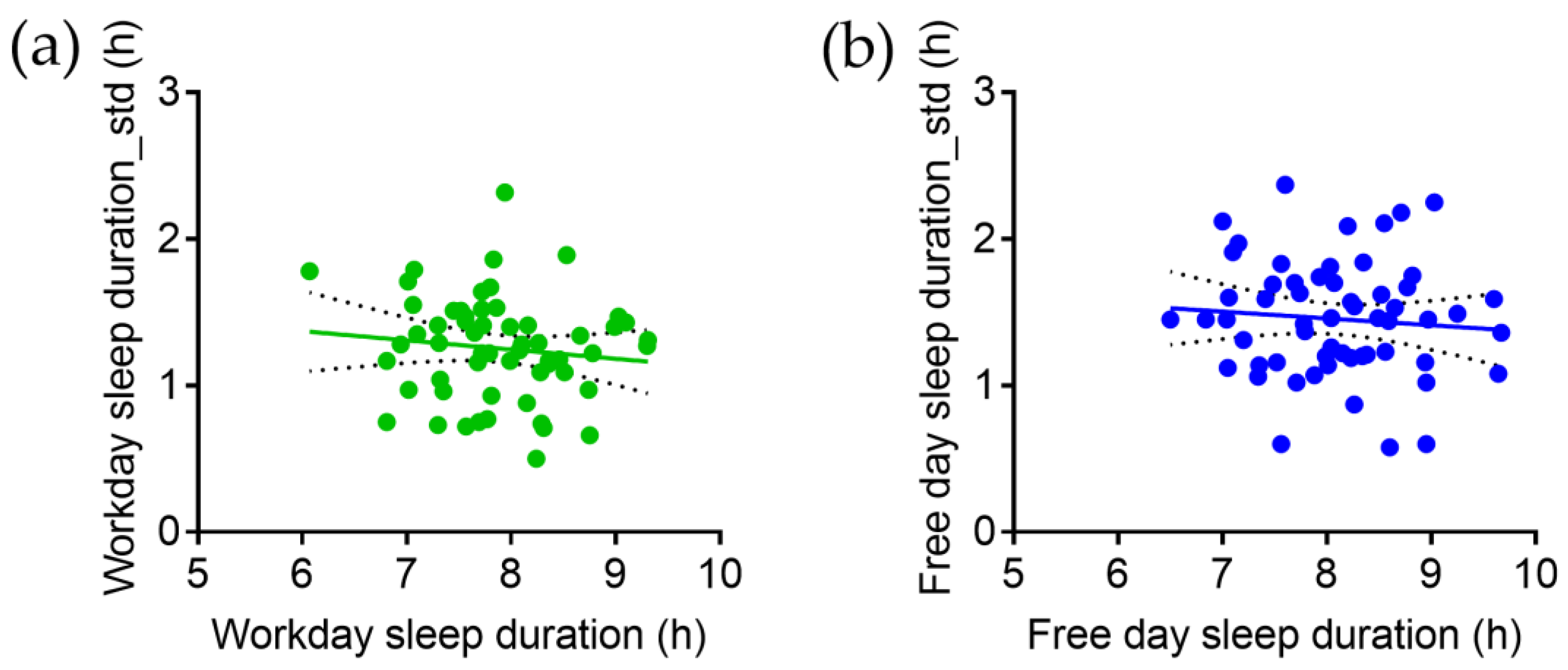
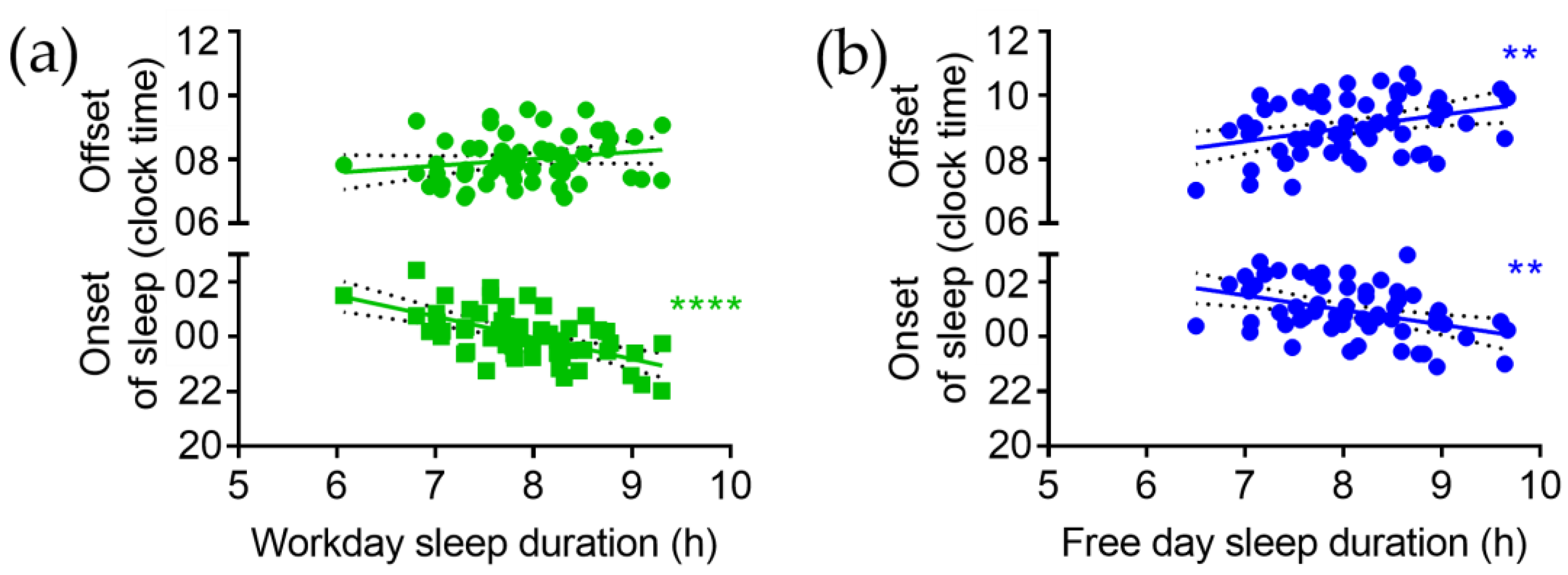
3.3. Objective Measures for Sleep Timing on Workdays and Free Days Longitudinally Assessed by Wearable Actigraphy
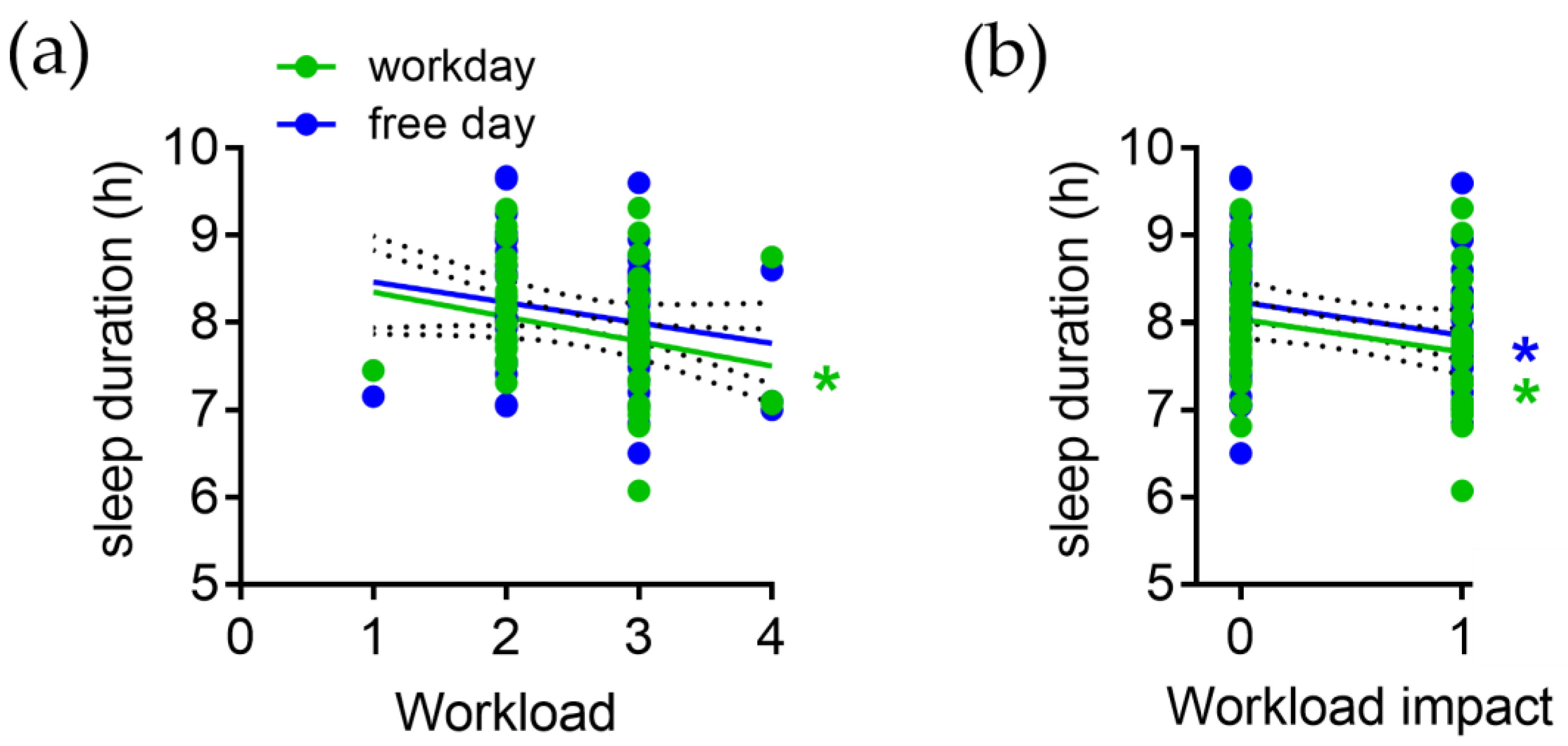
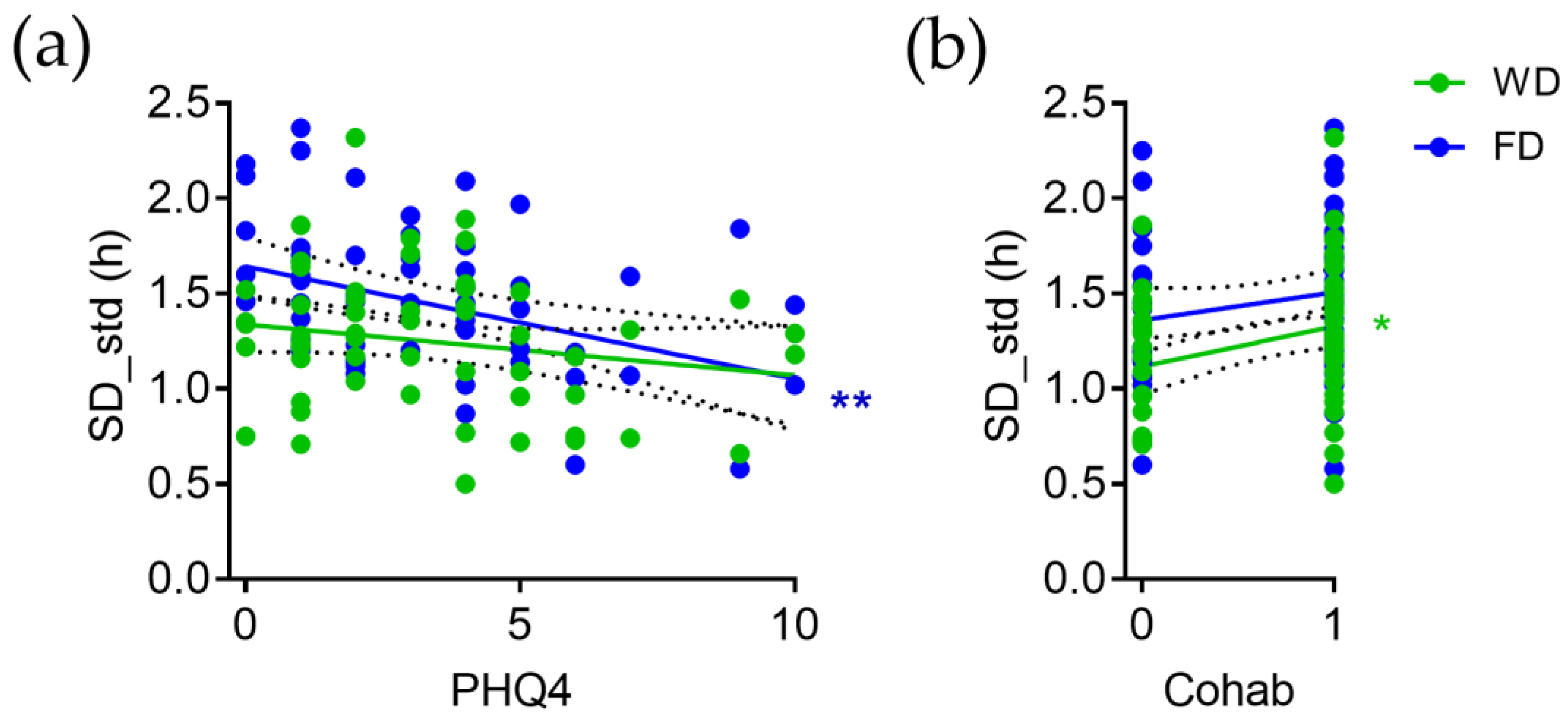
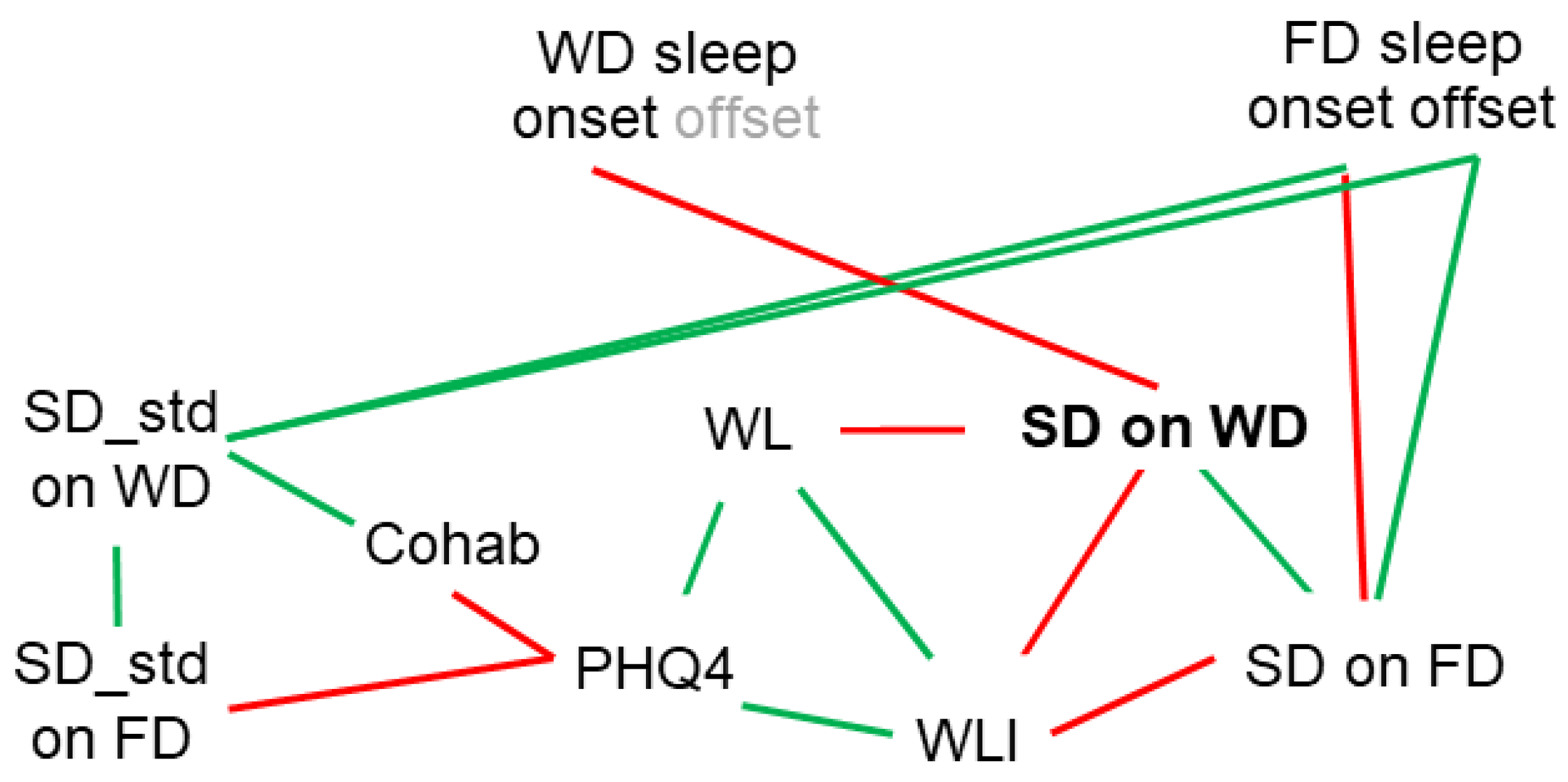
3.4. Correlations between Sleep Duration and Variables Assessed by Questionnaire
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Steel, Z.; Marnane, C.; Iranpour, C.; Chey, T.; Jackson, J.W.; Patel, V.; Silove, D. The global prevalence of common mental disorders: A systematic review and meta-analysis 1980–2013. Int. J. Epidemiol. 2014, 43, 476–493. [Google Scholar] [CrossRef] [PubMed]
- Son, C.; Hegde, S.; Smith, A.; Wang, X.; Sasangohar, F. Effects of COVID-19 on College Students’ Mental Health in the United States: Interview Survey Study. J. Med. Internet Res. 2020, 22, e21279. [Google Scholar] [CrossRef]
- Dederichs, M.; Weber, J.; Muth, T.; Angerer, P.; Loerbroks, A. Students’ perspectives on interventions to reduce stress in medical school: A qualitative study. PLoS ONE 2020, 15, e0240587. [Google Scholar] [CrossRef] [PubMed]
- Rotenstein, L.S.; Ramos, M.A.; Torre, M.; Segal, J.B.; Peluso, M.J.; Guille, C.; Sen, S.; Mata, D.A. Prevalence of Depression, Depressive Symptoms, and Suicidal Ideation among Medical Students A Systematic Review and Meta-Analysis. JAMA-J. Am. Med. Assoc. 2016, 316, 2214–2236. [Google Scholar] [CrossRef] [PubMed]
- Guse, J.; Heinen, I.; Kurre, J.; Mohr, S.; Bergelt, C. Perception of the study situation and mental burden during the COVID-19 pandemic among undergraduate medical students with and without mentoring. GMS J. Med. Educ. 2020, 37, Doc72. [Google Scholar] [CrossRef]
- Dyrbye, L.N.; Harper, W.; Durning, S.J.; Moutier, C.; Thomas, M.R.; Massie, F.S., Jr.; Eacker, A.; Power, D.V.; Szydlo, D.W.; Sloan, J.A.; et al. Patterns of distress in US medical students. Med. Teach. 2011, 33, 834–839. [Google Scholar] [CrossRef]
- Heinen, I.; Bullinger, M.; Kocalevent, R.D. Perceived stress in first year medical students—Associations with personal resources and emotional distress. BMC Med. Educ. 2017, 17, 4. [Google Scholar] [CrossRef]
- Thun-Hohenstein, L.; Hobinger-Ablasser, C.; Geyerhofer, S.; Lampert, K.; Schreuer, M.; Fritz, C. Burnout in medical students. Neuropsychiatrie 2021, 35, 17–27. [Google Scholar] [CrossRef]
- Harvey, S.B.; Modini, M.; Joyce, S.; Milligan-Saville, J.S.; Tan, L.; Mykletun, A.; Bryant, R.A.; Christensen, H.; Mitchell, P.B. Can work make you mentally ill? A systematic meta-review of work-related risk factors for common mental health problems. Occup. Environ. Med. 2017, 74, 301–310. [Google Scholar] [CrossRef]
- van der Molen, H.F.; Nieuwenhuijsen, K.; Frings-Dresen, M.H.W.; de Groene, G. Work-related psychosocial risk factors for stress-related mental disorders: An updated systematic review and meta-analysis. BMJ Open 2020, 10, e034849. [Google Scholar] [CrossRef]
- Atalay, K.D.; Can, G.F.; Erdem, S.R.; Muderrisoglu, I.H. Assessment of mental workload and academic motivation in medical students. J. Pak. Med. Assoc. 2016, 66, 574–578. [Google Scholar] [PubMed]
- Steptoe, A.; Kivimaki, M. Stress and cardiovascular disease. Nat. Rev. Cardiol. 2012, 9, 360–370. [Google Scholar] [CrossRef] [PubMed]
- Schaper, S.J.; Stengel, A. Emotional stress responsivity of patients with IBS—A systematic review. J. Psychosom. Res. 2022, 153, 110694. [Google Scholar] [CrossRef] [PubMed]
- Zielinski, G.; Ginszt, M.; Zawadka, M.; Rutkowska, K.; Podstawka, Z.; Szkutnik, J.; Majcher, P.; Gawda, P. The Relationship between Stress and Masticatory Muscle Activity in Female Students. J. Clin. Med. 2021, 10, 3459. [Google Scholar] [CrossRef]
- Consensus Conference Panel; Watson, N.F.; Badr, M.S.; Belenky, G.; Bliwise, D.L.; Buxton, O.M.; Buysse, D.; Dinges, D.F.; Gangwisch, J.; Grandner, M.A.; et al. Joint Consensus Statement of the American Academy of Sleep Medicine and Sleep Research Society on the Recommended Amount of Sleep for a Healthy Adult: Methodology and Discussion. Sleep 2015, 38, 1161–1183. [Google Scholar] [CrossRef]
- Medic, G.; Wille, M.; Hemels, M.E. Short- and long-term health consequences of sleep disruption. Nat. Sci. Sleep 2017, 9, 151–161. [Google Scholar] [CrossRef]
- Nelson, K.L.; Davis, J.E.; Corbett, C.F. Sleep quality: An evolutionary concept analysis. Nurs. Forum 2022, 57, 144–151. [Google Scholar] [CrossRef]
- Killgore, W.D. Effects of sleep deprivation on cognition. Prog. Brain Res. 2010, 185, 105–129. [Google Scholar] [CrossRef]
- Triantafillou, S.; Saeb, S.; Lattie, E.G.; Mohr, D.C.; Kording, K.P. Relationship between Sleep Quality and Mood: Ecological Momentary Assessment Study. JMIR Ment. Health 2019, 6, e12613. [Google Scholar] [CrossRef]
- Dijk, D.J.; von Schantz, M. Timing and consolidation of human sleep, wakefulness, and performance by a symphony of oscillators. J. Biol. Rhythms 2005, 20, 279–290. [Google Scholar] [CrossRef]
- Borbely, A.A.; Daan, S.; Wirz-Justice, A.; Deboer, T. The two-process model of sleep regulation: A reappraisal. J. Sleep Res. 2016, 25, 131–143. [Google Scholar] [CrossRef] [PubMed]
- Roenneberg, T.; Wirz-Justice, A.; Merrow, M. Life between clocks: Daily temporal patterns of human chronotypes. J. Biol. Rhythm. 2003, 18, 80–90. [Google Scholar] [CrossRef] [PubMed]
- Roenneberg, T. The human sleep project. Nature 2013, 498, 427–428. [Google Scholar] [CrossRef]
- Pilz, L.K.; Keller, L.K.; Lenssen, D.; Roenneberg, T. Time to rethink sleep quality: PSQI scores reflect sleep quality on workdays. Sleep 2018, 41, zsy029. [Google Scholar] [CrossRef] [PubMed]
- Fang, Y.; Forger, D.B.; Frank, E.; Sen, S.; Goldstein, C. Day-to-day variability in sleep parameters and depression risk: A prospective cohort study of training physicians. Npj Digit. Med. 2021, 4, 28. [Google Scholar] [CrossRef] [PubMed]
- Weiss, C.; Woods, K.; Filipowicz, A.; Ingram, K.K. Sleep Quality, Sleep Structure, and PER3 Genotype Mediate Chronotype Effects on Depressive Symptoms in Young Adults. Front. Psychol. 2020, 11, 2028. [Google Scholar] [CrossRef]
- Bakotic, M.; Radosevic-Vidacek, B.; Bjelajac, A.K. Morningness-eveningness and daytime functioning in university students: The mediating role of sleep characteristics. J. Sleep Res. 2017, 26, 210–218. [Google Scholar] [CrossRef]
- Wefers, B.; Hitz, C.; Holter, S.M.; Trumbach, D.; Hansen, J.; Weber, P.; Putz, B.; Deussing, J.M.; de Angelis, M.H.; Roenneberg, T.; et al. MAPK signaling determines anxiety in the juvenile mouse brain but depression-like behavior in adults. PLoS ONE 2012, 7, e35035. [Google Scholar] [CrossRef]
- von Gall, C.; Holub, L.; Pfeffer, M.; Eickhoff, S. Chronotype-related sleep loss is associated with reduced amplitude in circadian rhythm and higher fragmentation of REM sleep in young health adults. J. Med. Internet Res. 2023. submitted. Available online: https://preprints.jmir.org/preprint/46361 (accessed on 26 April 2023).
- Wittmann, M.; Dinich, J.; Merrow, M.; Roenneberg, T. Social jetlag: Misalignment of biological and social time. Chronobiol. Int. 2006, 23, 497–509. [Google Scholar] [CrossRef]
- Mahgoub, I.M.; Abdelrahman, A.; Abdallah, T.A.; Ahmed, K.A.H.M.; Omer, M.E.A.; Abdelrahman, E.; Salih, Z.M.A. Psychological effects of the COVID-19 pandemic: Perceived stress, anxiety, work-family imbalance, and coping strategies among healthcare professionals in Khartoum state hospitals, Sudan, 2021. Brain Behav. 2021, 11, e2318. [Google Scholar] [CrossRef]
- Xiong, J.; Lipsitz, O.; Nasri, F.; Lui, L.M.W.; Gill, H.; Phan, L.; Chen-Li, D.; Iacobucci, M.; Ho, R.; Majeed, A.; et al. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J. Affect. Disord. 2020, 277, 55–64. [Google Scholar] [CrossRef] [PubMed]
- Hu, J.; Huang, Y.; Liu, J.; Zheng, Z.; Xu, X.; Zhou, Y.; Wang, J. COVID-19 Related Stress and Mental Health Outcomes 1 Year After the Peak of the Pandemic Outbreak in China: The Mediating Effect of Resilience and Social Support. Front. Psychiatry 2022, 13, 828379. [Google Scholar] [CrossRef] [PubMed]
- Hopf, D.; Schneider, E.; Aguilar-Raab, C.; Scheele, D.; Morr, M.; Klein, T.; Ditzen, B.; Eckstein, M. Loneliness and diurnal cortisol levels during COVID-19 lockdown: The roles of living situation, relationship status and relationship quality. Sci. Rep. 2022, 12, 15076. [Google Scholar] [CrossRef]
- Qi, Y.; Lepe, A.; Almansa, J.; Ots, P.; de Kroon, M.L.A.; Lifelines Corona Research Initiative; Vrooman, J.C.; Reijneveld, S.A.; Brouwer, S. Increases in symptoms of depression and anxiety in adults during the initial phases of the COVID-19 pandemic are limited to those with less resources: Results from the Lifelines Cohort Study. J. Psychiatr. Res. 2022, 154, 151–158. [Google Scholar] [CrossRef] [PubMed]
- Brown, J.P.; Martin, D.; Nagaria, Z.; Verceles, A.C.; Jobe, S.L.; Wickwire, E.M. Mental Health Consequences of Shift Work: An Updated Review. Curr. Psychiatry Rep. 2020, 22, 7. [Google Scholar] [CrossRef] [PubMed]
- Angerer, P.; Schmook, R.; Elfantel, I.; Li, J. Night Work and the Risk of Depression. Dtsch. Arztebl. Int. 2017, 114, 404–411. [Google Scholar] [CrossRef]
- Wu, Q.J.; Sun, H.; Wen, Z.Y.; Zhang, M.; Wang, H.Y.; He, X.H.; Jiang, Y.T.; Zhao, Y.H. Shift work and health outcomes: An umbrella review of systematic reviews and meta-analyses of epidemiological studies. J. Clin. Sleep Med. 2022, 18, 653–662. [Google Scholar] [CrossRef]
- Van den Berg, J.F.; Kivela, L.; Antypa, N. Chronotype and depressive symptoms in students: An investigation of possible mechanisms. Chronobiol. Int. 2018, 35, 1248–1261. [Google Scholar] [CrossRef]
- Dimitrov, A.; Veer, I.M.; Kleeblatt, J.; Seyfarth, F.; Roenneberg, T.; Ising, M.; Uhr, M.; Keck, M.E.; Kramer, A.; Berger, M.; et al. Chronotype is associated with psychological well-being depending on the composition of the study sample. J. Health Psychol. 2018, 25, 1236–1247. [Google Scholar] [CrossRef]
- Jansen, E.C.; Peterson, K.E.; O’Brien, L.; Hershner, S.; Boolani, A. Associations between Mental Workload and Sleep Quality in a Sample of Young Adults Recruited from a US College Town. Behav. Sleep Med. 2020, 18, 513–522. [Google Scholar] [CrossRef]
- Almojali, A.I.; Almalki, S.A.; Alothman, A.S.; Masuadi, E.M.; Alaqeel, M.K. The prevalence and association of stress with sleep quality among medical students. J. Epidemiol. Glob. Health 2017, 7, 169–174. [Google Scholar] [CrossRef] [PubMed]
- Rezaei, M.; Khormali, M.; Akbarpour, S.; Sadeghniiat-Hagighi, K.; Shamsipour, M. Sleep quality and its association with psychological distress and sleep hygiene: A cross-sectional study among pre-clinical medical students. Sleep Sci. 2018, 11, 274–280. [Google Scholar] [CrossRef]
- Han, K.S.; Kim, L.; Shim, I. Stress and sleep disorder. Exp. Neurobiol. 2012, 21, 141–150. [Google Scholar] [CrossRef] [PubMed]
- Ahrberg, K.; Dresler, M.; Niedermaier, S.; Steiger, A.; Genzel, L. The interaction between sleep quality and academic performance. J. Psychiatr. Res. 2012, 46, 1618–1622. [Google Scholar] [CrossRef] [PubMed]

| Variable | Score | Mean +/− std | Total (%) |
|---|---|---|---|
| Cohabitation | 0.64 +/− 0.48 | ||
| Living alone | 0 | 21 (36%) | |
| Living in the community | 1 | 40 (64%) | |
| Workload | 2.6 +/− 0.62 | ||
| Low | 1 | 1 (2%) | |
| Medium | 2 | 24 (41% | |
| High | 3 | 31 (52%) | |
| Very high | 4 | 3 (5%) | |
| Workload impact on sleep | 0.41 +/− 0.49 | ||
| No | 0 | 35 (59%) | |
| Yes | 1 | 24 (41%) | |
| Anxiety and depression | 3.18 +/− 2.56 | ||
| Normal | 0–2 | 29 (49%) | |
| Mild | 3–5 | 20 (34%) | |
| Moderate | 6–8 | 6 (10%) | |
| Severe | 9–12 | 4 (7%) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
von Gall, C.; Muth, T.; Angerer, P. Sleep Duration on Workdays Is Correlated with Subjective Workload and Subjective Impact of High Workload on Sleep in Young Healthy Adults. Brain Sci. 2023, 13, 818. https://doi.org/10.3390/brainsci13050818
von Gall C, Muth T, Angerer P. Sleep Duration on Workdays Is Correlated with Subjective Workload and Subjective Impact of High Workload on Sleep in Young Healthy Adults. Brain Sciences. 2023; 13(5):818. https://doi.org/10.3390/brainsci13050818
Chicago/Turabian Stylevon Gall, Charlotte, Thomas Muth, and Peter Angerer. 2023. "Sleep Duration on Workdays Is Correlated with Subjective Workload and Subjective Impact of High Workload on Sleep in Young Healthy Adults" Brain Sciences 13, no. 5: 818. https://doi.org/10.3390/brainsci13050818
APA Stylevon Gall, C., Muth, T., & Angerer, P. (2023). Sleep Duration on Workdays Is Correlated with Subjective Workload and Subjective Impact of High Workload on Sleep in Young Healthy Adults. Brain Sciences, 13(5), 818. https://doi.org/10.3390/brainsci13050818







