One Year of Outpatient Dialectical Behavioral Therapy and Its Impact on Neuronal Correlates of Attachment Representation in Patients with Borderline Personality Disorder Using a Personalized fMRI Task
Abstract
:1. Introduction
1.1. Characterization of BPD
1.2. Studies on Attachment
1.3. fMRI: Paradigms and Findings
1.4. Intervention Strategies
1.5. Study Aim and Hypotheses
2. Materials and Methods
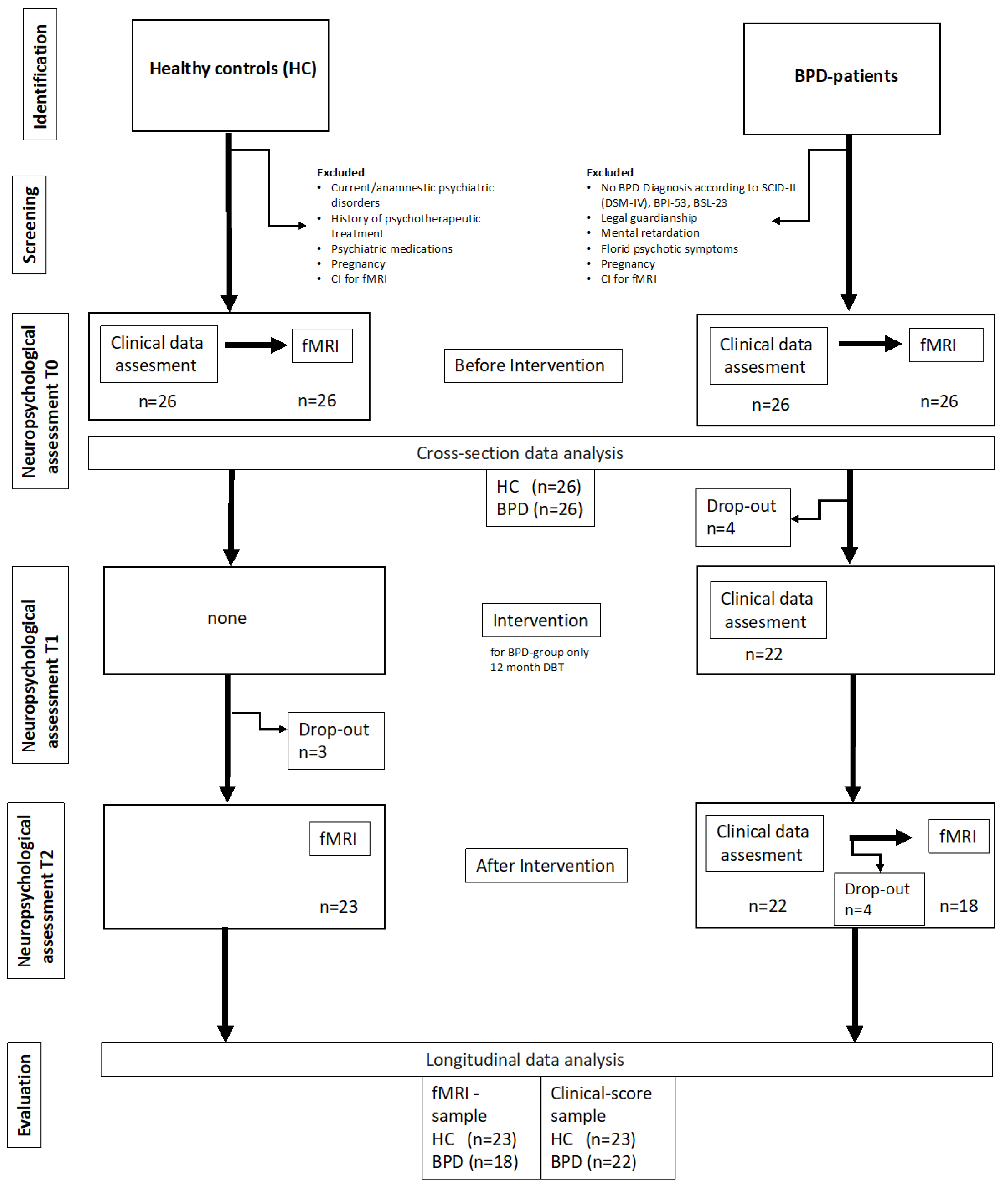
2.1. Procedure and Study Design
2.2. Sample
2.3. Measurements
2.3.1. Clinical Instruments
2.3.2. DBT-Intervention
2.3.3. Functional and Structural Imaging
2.3.4. Functional Imaging Paradigm and Personalized Core Sentences
2.3.5. Preprocessing of Imaging Data
2.3.6. Statistical Comparisons
3. Results
3.1. Sample Characteristics
3.2. Clinical Changes during Intervention
3.3. fMRI Data Results
3.3.1. Between Group Comparisons (Monadic Pictures with Personalized Sentences)
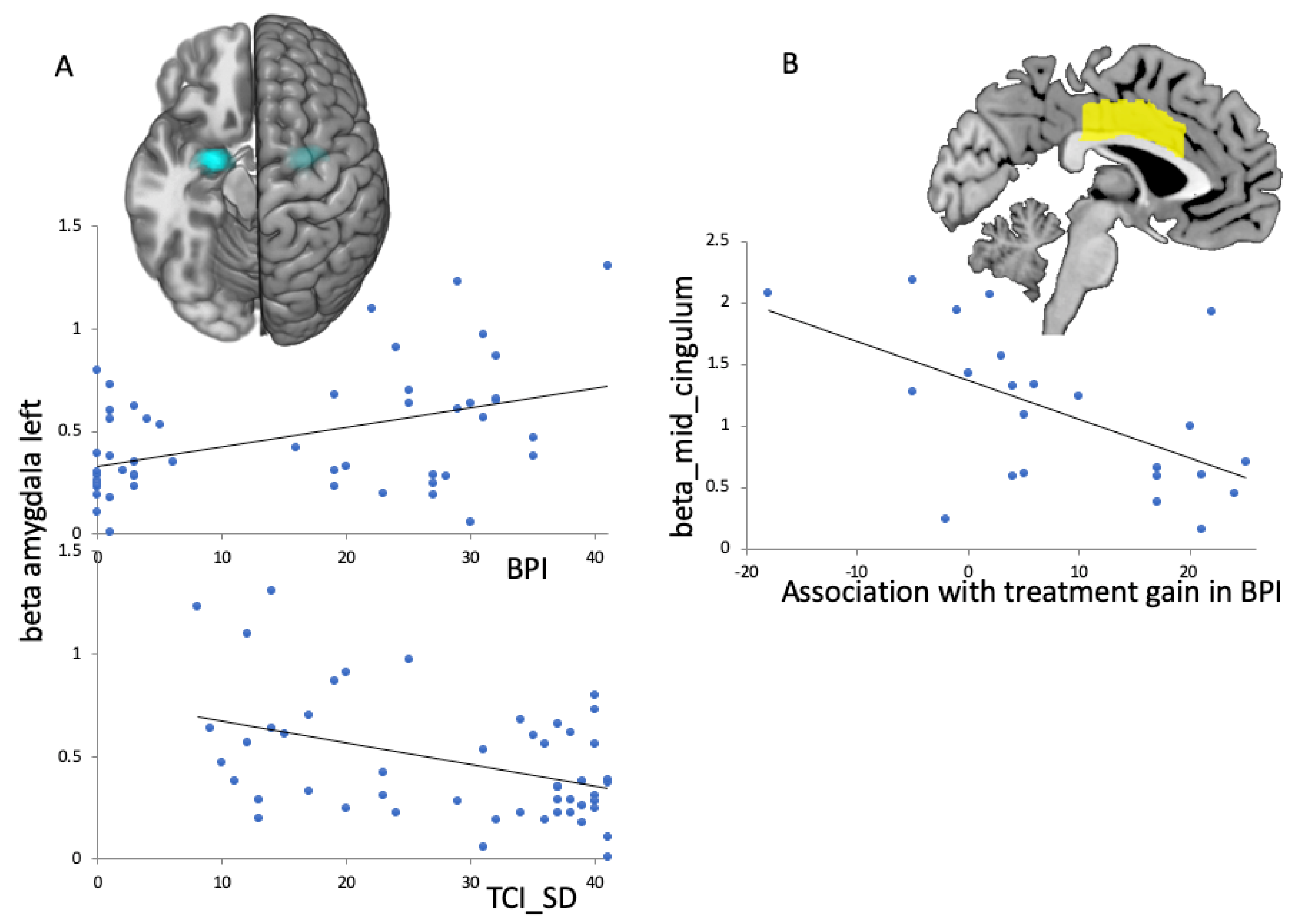
3.3.2. Association between BPD Group fMRI Images and Clinical BPD Scores
4. Discussion
4.1. Significance of the Study and Main Findings
4.2. Intervention Effects and fMRI Findings
4.3. fMRI-Effects in the aMCC
4.4. fMRI-Effects in the Amygdala
4.5. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gunderson, J.G. Borderline personality disorder: Ontogeny of a diagnosis. Am. J. Psychiatry 2009, 166, 530–539. [Google Scholar] [CrossRef]
- Leichsenring, F.; Leibing, E.; Kruse, J.; New, A.S.; Leweke, F. Borderline personality disorder. Lancet 2011, 377, 74–84. [Google Scholar] [CrossRef] [PubMed]
- Grant, B.F.; Chou, S.P.; Goldstein, R.B.; Huang, B.; Stinson, F.S.; Saha, T.D.; Smith, S.M.; Dawson, D.A.; Pulay, A.J.; Pickering, R.P.; et al. Prevalence, correlates, disability, and comorbidity of DSM-IV borderline personality disorder: Results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. J. Clin. Psychiatry 2008, 69, 533–545. [Google Scholar] [CrossRef] [PubMed]
- Schmahl, C.; Herpertz, S.C.; Bertsch, K.; Ende, G.; Flor, H.; Kirsch, P.; Lis, S.; Meyer-Lindenberg, A.; Rietschel, M.; Schneider, M.; et al. Mechanisms of disturbed emotion processing and social interaction in borderline personality disorder: State of knowledge and research agenda of the German Clinical Research Unit. Borderline Personal. Disord. Emot. Dysregul. 2014, 1, 12. [Google Scholar] [CrossRef] [Green Version]
- Oldham, J.M. Borderline personality disorder and suicidality. Am. J. Psychiatry 2006, 163, 20–26. [Google Scholar] [CrossRef] [PubMed]
- Gunderson, J.G.; Herpertz, S.C.; Skodol, A.E.; Torgersen, S.; Zanarini, M.C. Borderline personality disorder. Nat. Rev. Dis. Primers 2018, 4, 18029. [Google Scholar] [CrossRef] [Green Version]
- Cohen, P.; Chen, H.; Gordon, K.; Johnson, J.; Brook, J.; Kasen, S. Socioeconomic background and the developmental course of schizotypal and borderline personality disorder symptoms. Dev. Psychopathol. 2008, 20, 633–650. [Google Scholar] [CrossRef] [Green Version]
- Widom, C.S.; Czaja, S.J.; Paris, J. A prospective investigation of borderline personality disorder in abused and neglected children followed up into adulthood. J. Personal. Disord. 2009, 23, 433–446. [Google Scholar] [CrossRef]
- Gunderson, J.G. The borderline patient’s intolerance of aloneness: Insecure attachments and therapist availability. Am. J. Psychiatry 1996, 153, 752–758. [Google Scholar] [CrossRef]
- George, C.; Kaplan, N.; Main, M. Adult Attachment Interview: Unpublished Manuscript; Department of Psychology, University of California: Berkeley, CA, USA, 1996; p. 3. [Google Scholar]
- George, C.; West, M. The development and preliminary validation of a new measure of adult attachment: The adult attachment projective. Attach. Hum. Dev. 2001, 3, 30–61. [Google Scholar] [CrossRef]
- George, C.; West, M. The Adult Attachment Projective Picture System: Integrating attachment into clinical assessment. J. Pers. Assess. 2011, 93, 407–416. [Google Scholar] [CrossRef] [PubMed]
- Fonagy, P.; Leigh, T.; Steele, M.; Steele, H.; Kennedy, R.; Mattoon, G.; Target, M.; Gerber, A. The relation of attachment status, psychiatric classification, and response to psychotherapy. J. Consult. Clin. Psychol. 1996, 64, 22–31. [Google Scholar] [CrossRef]
- Agrawal, H.R.; Gunderson, J.; Holmes, B.M.; Lyons-Ruth, K. Attachment studies with borderline patients: A review. Harv. Rev. Psychiatry 2004, 12, 94–104. [Google Scholar] [CrossRef] [PubMed]
- Levy, K.N. The implications of attachment theory and research for understanding borderline personality disorder. Dev. Psychopathol. 2005, 17, 959–986. [Google Scholar] [CrossRef] [PubMed]
- Bakermans-Kranenburg, M.J.; van IJzendoorn, M.H. The first 10,000 Adult Attachment Interviews: Distributions of adult attachment representations in clinical and non-clinical groups. Attach. Hum. Dev. 2009, 11, 223–263. [Google Scholar] [CrossRef]
- Beck, E.; Sharp, C.; Poulsen, S.; Bo, S.; Pedersen, J.; Simonsen, E. The mediating role of mentalizing capacity between parents and peer attachment and adolescent borderline personality disorder. Borderline Personal. Disord. Emot. Dysregul. 2017, 4, 23. [Google Scholar] [CrossRef] [Green Version]
- Buchheim, A.; Diamond, D. Attachment and Borderline Personality Disorder. Psychiatr. Clin. N. Am. 2018, 41, 651–668. [Google Scholar] [CrossRef]
- Keinänen, M.T.; Johnson, J.G.; Richards, E.S.; Courtney, E.A. A systematic review of the evidence-based psychosocial risk factors for understanding of borderline personality disorder. Psychoanal. Psychother. 2012, 26, 65–91. [Google Scholar] [CrossRef]
- Buchheim, A.; George, C. Attachment disorganization in borderline personality disorder and anxiety disorder. In Disorganization of Attachment and Caregiving; Solomon, J., George, C., Eds.; The Guilford Press: New York, NY, USA, 2011; pp. 343–382. [Google Scholar]
- Buchheim, A.; Erk, S.; George, C.; Kächele, H.; Kircher, T.; Martius, P.; Pokorny, D.; Ruchsow, M.; Spitzer, M.; Walter, H. Neural correlates of attachment trauma in borderline personality disorder: A functional magnetic resonance imaging study. Psychiatry Res. 2008, 163, 223–235. [Google Scholar] [CrossRef]
- Buchheim, A.; George, C.; Gündel, H.; Viviani, R. Editorial: Neuroscience of Human Attachment. Front. Hum. Neurosci. 2017, 11, 136. [Google Scholar] [CrossRef] [Green Version]
- Barbour, R.F. Attachment and Loss. Vol. 1. Attachment. By John Bowlby. London: The Hogarth Press and Institute of Psycho-Analysis. 1969. Pp. 428. Price 63 s. Br. J. Psychiatry 1970, 116, 102–103. [Google Scholar] [CrossRef] [Green Version]
- Gander, M.; Buchheim, A. Attachment classification, psychophysiology and frontal EEG asymmetry across the lifespan: A review. Front. Hum. Neurosci. 2015, 9, 79. [Google Scholar] [CrossRef] [Green Version]
- Spitoni, G.F.; Zingaretti, P.; Giovanardi, G.; Antonucci, G.; Galati, G.; Lingiardi, V.; Cruciani, G.; Titone, G.; Boccia, M. Disorganized Attachment pattern affects the perception of Affective Touch. Sci. Rep. 2020, 10, 9658. [Google Scholar] [CrossRef]
- Iskric, A.; Barkley-Levenson, E. Neural Changes in Borderline Personality Disorder After Dialectical Behavior Therapy—A Review. Front. Psychiatry 2021, 12, 2382. [Google Scholar] [CrossRef] [PubMed]
- Vijayakumar, N.; Cheng, T.W.; Pfeifer, J.H. Neural correlates of social exclusion across ages: A coordinate-based meta-analysis of functional MRI studies. Neuroimage 2017, 153, 359–368. [Google Scholar] [CrossRef] [PubMed]
- Eisenberger, N.I.; Lieberman, M.D.; Williams, K.D. Does rejection hurt? An FMRI study of social exclusion. Science 2003, 302, 290–292. [Google Scholar] [CrossRef]
- Gillath, O.; Bunge, S.A.; Shaver, P.R.; Wendelken, C.; Mikulincer, M. Attachment-style differences in the ability to suppress negative thoughts: Exploring the neural correlates. Neuroimage 2005, 28, 835–847. [Google Scholar] [CrossRef]
- DeWall, C.N.; Masten, C.L.; Powell, C.; Combs, D.; Schurtz, D.R.; Eisenberger, N.I. Do neural responses to rejection depend on attachment style? An fMRI study. Soc. Cogn. Affect. Neurosci. 2012, 7, 184–192. [Google Scholar] [CrossRef] [Green Version]
- Buchheim, A.; Erk, S.; George, C.; Kachele, H.; Ruchsow, M.; Spitzer, M.; Kircher, T.; Walter, H. Measuring attachment representation in an FMRI environment: A pilot study. Psychopathology 2006, 39, 144–152. [Google Scholar] [CrossRef]
- Somma, A.; Ferrara, M.; Terrinoni, A.; Frau, C.; Ardizzone, I.; Sharp, C.; Fossati, A. Hypermentalizing as a marker of borderline personality disorder in Italian adolescents: A cross-cultural replication of Sharp and colleagues’ (2011) findings. Borderline Personal. Disord. Emot. Dysregul. 2019, 6, 5. [Google Scholar] [CrossRef]
- Buchheim, A.; Viviani, R.; Kessler, H.; Kächele, H.; Cierpka, M.; Roth, G.; George, C.; Kernberg, O.F.; Bruns, G.; Taubner, S. Changes in prefrontal-limbic function in major depression after 15 months of long-term psychotherapy. PLoS ONE 2012, 7, e33745. [Google Scholar] [CrossRef]
- Domsalla, M.; Koppe, G.; Niedtfeld, I.; Vollstädt-Klein, S.; Schmahl, C.; Bohus, M.; Lis, S. Cerebral processing of social rejection in patients with borderline personality disorder. Soc. Cogn. Affect. Neurosci. 2014, 9, 1789–1797. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Olié, E.; Doell, K.C.; Corradi-Dell’Acqua, C.; Courtet, P.; Perroud, N.; Schwartz, S. Physical pain recruits the nucleus accumbens during social distress in borderline personality disorder. Soc. Cogn. Affect. Neurosci. 2018, 13, 1071–1080. [Google Scholar] [CrossRef] [Green Version]
- Herpertz, S.C.; Dietrich, T.M.; Wenning, B.; Krings, T.; Erberich, S.G.; Willmes, K.; Thron, A.; Sass, H. Evidence of abnormal amygdala functioning in borderline personality disorder: A functional MRI study. Biol. Psychiatry 2001, 50, 292–298. [Google Scholar] [CrossRef] [PubMed]
- Donegan, N.H.; Sanislow, C.A.; Blumberg, H.P.; Fulbright, R.K.; Lacadie, C.; Skudlarski, P.; Gore, J.C.; Olson, I.R.; McGlashan, T.H.; Wexler, B.E. Amygdala hyperreactivity in borderline personality disorder: Implications for emotional dysregulation. Biol. Psychiatry 2003, 54, 1284–1293. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sharp, C.; Wright, A.G.C.; Fowler, J.C.; Frueh, B.C.; Allen, J.G.; Oldham, J.; Clark, L.A. The structure of personality pathology: Both general (‘g’) and specific (‘s’) factors? J. Abnorm. Psychol. 2015, 124, 387–398. [Google Scholar] [CrossRef] [Green Version]
- Bernheim, D.; Buchheim, A.; Domin, M.; Mentel, R.; Lotze, M. Neural Correlates of Attachment Representation in Patients With Borderline Personality Disorder Using a Personalized Functional Magnet Resonance Imaging Task. Front. Hum. Neurosci. 2022, 16, 810417. [Google Scholar] [CrossRef] [PubMed]
- Schnell, K.; Herpertz, S.C. Effects of dialectic-behavioral-therapy on the neural correlates of affective hyperarousal in borderline personality disorder. J. Psychiatr. Res. 2007, 41, 837–847. [Google Scholar] [CrossRef]
- Linehan, M.M. Dialectical behavior therapy for treatment of borderline personality disorder: Implications for the treatment of substance abuse. NIDA Res. Monogr. 1993, 137, 201–216. [Google Scholar]
- Choi-Kain, L.W.; Albert, E.B.; Gunderson, J.G. Evidence-Based Treatments for Borderline Personality Disorder: Implementation, Integration, and Stepped Care. Harv. Rev. Psychiatry 2016, 24, 342–356. [Google Scholar] [CrossRef] [Green Version]
- Stoffers, J.M.; Völlm, B.A.; Rücker, G.; Timmer, A.; Huband, N.; Lieb, K. Psychological therapies for people with borderline personality disorder. Cochrane Database Syst. Rev. 2012, 2012, CD005652. [Google Scholar] [CrossRef]
- DeCou, C.R.; Comtois, K.A.; Landes, S.J. Dialectical Behavior Therapy Is Effective for the Treatment of Suicidal Behavior: A Meta-Analysis. Behav. Ther. 2019, 50, 60–72. [Google Scholar] [CrossRef]
- Stoffers-Winterling, J.M.; Storebø, O.J.; Kongerslev, M.T.; Faltinsen, E.; Todorovac, A.; Sedoc Jørgensen, M.; Sales, C.P.; Edemann Callesen, H.; Pereira Ribeiro, J.; Völlm, B.A.; et al. Psychotherapies for borderline personality disorder: A focused systematic review and meta-analysis. Br. J. Psychiatry 2022, 221, 538–552. [Google Scholar] [CrossRef] [PubMed]
- Leichsenring, F. Borderline-Persönlichkeits-Inventar (BPI): Manual; Hogrefe: Göttingen, Germany, 1997. [Google Scholar]
- Cloninger, C.R.; Svrakic, D.M.; Przybeck, T.R. A psychobiological model of temperament and character. Arch. Gen. Psychiatry 1993, 50, 975–990. [Google Scholar] [CrossRef]
- Bernheim, D.; Gander, M.; Keller, F.; Becker, M.; Lischke, A.; Mentel, R.; Freyberger, H.J.; Buchheim, A. The role of attachment characteristics in dialectical behavior therapy for patients with borderline personality disorder. Clin. Psychol. Psychother. 2019, 26, 339–349. [Google Scholar] [CrossRef]
- Wittchen, H.-U.; Zaudig, M.; Fydrich, T. SKID Strukturiertes Klinisches Interview für DSM-IV. Achse I und II. In Zeitschrift für Klinische Psychologie und Psychotherapie; Hogrefe: Göttingen, Germany, 1997. [Google Scholar] [CrossRef]
- Bohus, M.; Limberger, M.F.; Frank, U.; Sender, I.; Gratwohl, T.; Stieglitz, R.D. Entwicklung der Borderline-Symptom-Liste. Psychother. Psychosom. Med. Psychol. 2001, 51, 201–211. [Google Scholar] [CrossRef] [PubMed]
- Richter, J.; Eisemann, M.; Richter, G.; Cloninger, C.R. Das Temperament und Charakter Inventar (TCI): Ein Leitfaden über seine Entwicklung und Anwendung; Swets Test Services mbH: Frankfurt am Main, Germany, 1999. [Google Scholar]
- Cloninger, C.R. Feeling Good: The Science of Well-Being; Oxford University Press: Oxford, UK, 2004; ISBN 9780195051377. [Google Scholar]
- Bernheim, D.; Becker, M.; Gander, M.; Lischke, A.; Mentel, R.; Buchheim, A.; Freyberger, H.J. Einfluss und Veränderung der Selbstlenkungsfähigkeit in der Dialektisch-Behavioralen Therapie (DBT). Psychiatr. Prax. 2017, 44, 266–273. [Google Scholar] [CrossRef]
- Linehan, M.M.; Armstrong, H.E.; Suarez, A.; Allmon, D.; Heard, H.L. Cognitive-behavioral treatment of chronically parasuicidal borderline patients. Arch. Gen. Psychiatry 1991, 48, 1060–1064. [Google Scholar] [CrossRef]
- Bohus, M.; Wolf-Arehult, M.; Kienast, T. Interaktives Skillstraining für Borderline-Patienten: Das Therapeutenmanual: Inklusive Keycard zum Freischalten der Software “Interaktives Skillstraining für Borderline-Patienten”; 2., Aktualisierte und Erweiterte Auflage, 2. Nachdruck; Schattauer; EBSCO: Stuttgart/Ipswich, UK, 2020; ISBN 978-3-608-42827-8. [Google Scholar]
- George, C.; West, M. The Adult Attachment Projective Picture System: Attachment Theory and Assessment in Adults; Guilford Press: New York, NY, USA, 2012. [Google Scholar]
- Eickhoff, S.B.; Stephan, K.E.; Mohlberg, H.; Grefkes, C.; Fink, G.R.; Amunts, K.; Zilles, K. A new SPM toolbox for combining probabilistic cytoarchitectonic maps and functional imaging data. Neuroimage 2005, 25, 1325–1335. [Google Scholar] [CrossRef]
- Klepzig, K.; Horn, U.; König, J.; Holtz, K.; Wendt, J.; Hamm, A.O.; Lotze, M. Brain imaging of chill reactions to pleasant and unpleasant sounds. Behav. Brain Res. 2020, 380, 112417. [Google Scholar] [CrossRef] [PubMed]
- Kröger, C.; Kosfelder, J. Eine Meta-Analyse zur Wirksamkeit der Dialektisch Behavioralen Therapie bei Borderline-Persönlichkeitsstörungen. Z. Klin. Psychol. Psychother. 2007, 36, 11–17. [Google Scholar] [CrossRef] [Green Version]
- Kernberg, O. Borderline personality organization. J. Am. Psychoanal. Assoc. 1967, 15, 641–685. [Google Scholar] [CrossRef] [PubMed]
- Cloninger, C.R. The Temperament and Character Inventory (TCI): A Guide to Its Development and Use, 1st ed.; Center for Psychobiology of Personality, Washington University: St. Louis, MO, USA, 1994; ISBN 978-0-9642917-1-3. [Google Scholar]
- Buchheim, A.; Hörz-Sagstetter, S.; Doering, S.; Rentrop, M.; Schuster, P.; Buchheim, P.; Pokorny, D.; Fischer-Kern, M. Change of Unresolved Attachment in Borderline Personality Disorder: RCT Study of Transference-Focused Psychotherapy. Psychother. Psychosom. 2017, 86, 314–316. [Google Scholar] [CrossRef]
- Wilcox, C.E.; Mayer, A.R.; Teshiba, T.M.; Ling, J.; Smith, B.W.; Wilcox, G.L.; Mullins, P.G. The Subjective Experience of Pain: An FMRI Study of Percept-Related Models and Functional Connectivity. Pain Med. 2015, 16, 2121–2133. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schulze, L.; Schmahl, C.; Niedtfeld, I. Neural Correlates of Disturbed Emotion Processing in Borderline Personality Disorder: A Multimodal Meta-Analysis. Biol. Psychiatry 2016, 79, 97–106. [Google Scholar] [CrossRef]
- Schmitgen, M.M.; Niedtfeld, I.; Schmitt, R.; Mancke, F.; Winter, D.; Schmahl, C.; Herpertz, S.C. Individualized treatment response prediction of dialectical behavior therapy for borderline personality disorder using multimodal magnetic resonance imaging. Brain Behav. 2019, 9, e01384. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Anders, S.; Lotze, M.; Erb, M.; Grodd, W.; Birbaumer, N. Brain activity underlying emotional valence and arousal: A response-related fMRI study. Hum. Brain Mapp. 2004, 23, 200–209. [Google Scholar] [CrossRef]
- Mehlum, L. Mechanisms of change in dialectical behaviour therapy for people with borderline personality disorder. Curr. Opin. Psychol. 2021, 37, 89–93. [Google Scholar] [CrossRef]
- Kazdin, A.E. Understanding how and why psychotherapy leads to change. Psychother. Res. 2009, 19, 418–428. [Google Scholar] [CrossRef]



| Healthy Controls | BPD Patients | Statistics | |
|---|---|---|---|
| Participants (n) | 23 | 18 | |
| Age in years | 27.3 (6.83) | 27.5 (7.97) | t = −0.78, p = 0.939 |
| IQ (MWT-B) | 108.4 (9.29) | 111.7 (14.88) | t = −0.82, p = 0.419 |
| TCI_SD | 38.43 (2.66) | 19.67 (9.81) | t = 7.893, p = 0.000 |
| AAP_CLASS | 2.70 (1.063) | 1.83 (0.924) | t = 2.775, p = 0.008 |
| BSL_total_score | 2.0 (2.8) | 44.2 (21.82) | t = −8.147, p = 0.000 |
| BPI_sum | 1.55 (1.82) | 27.78 (5.86) | t = −18.295, p = 0.000 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Flechsig, A.; Bernheim, D.; Buchheim, A.; Domin, M.; Mentel, R.; Lotze, M. One Year of Outpatient Dialectical Behavioral Therapy and Its Impact on Neuronal Correlates of Attachment Representation in Patients with Borderline Personality Disorder Using a Personalized fMRI Task. Brain Sci. 2023, 13, 1001. https://doi.org/10.3390/brainsci13071001
Flechsig A, Bernheim D, Buchheim A, Domin M, Mentel R, Lotze M. One Year of Outpatient Dialectical Behavioral Therapy and Its Impact on Neuronal Correlates of Attachment Representation in Patients with Borderline Personality Disorder Using a Personalized fMRI Task. Brain Sciences. 2023; 13(7):1001. https://doi.org/10.3390/brainsci13071001
Chicago/Turabian StyleFlechsig, Ariane, Dorothee Bernheim, Anna Buchheim, Martin Domin, Renate Mentel, and Martin Lotze. 2023. "One Year of Outpatient Dialectical Behavioral Therapy and Its Impact on Neuronal Correlates of Attachment Representation in Patients with Borderline Personality Disorder Using a Personalized fMRI Task" Brain Sciences 13, no. 7: 1001. https://doi.org/10.3390/brainsci13071001
APA StyleFlechsig, A., Bernheim, D., Buchheim, A., Domin, M., Mentel, R., & Lotze, M. (2023). One Year of Outpatient Dialectical Behavioral Therapy and Its Impact on Neuronal Correlates of Attachment Representation in Patients with Borderline Personality Disorder Using a Personalized fMRI Task. Brain Sciences, 13(7), 1001. https://doi.org/10.3390/brainsci13071001







