Network Analysis of Anxiety Symptoms in Front-Line Medical Staff during the COVID-19 Pandemic
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Research Tools
2.2.1. Questionnaire for Collecting General Information
2.2.2. GAD-7
2.3. Research Process
2.4. Statistical Analysis
2.5. RPCN
2.5.1. Network Construction and Visualisation
2.5.2. Centrality and Predictability
2.5.3. Network Accuracy and Stability
2.5.4. Community Test
2.5.5. Gender-Based Network Comparison
2.6. DAG
3. Results
3.1. Statistical Results for the Variables
3.2. RPCN
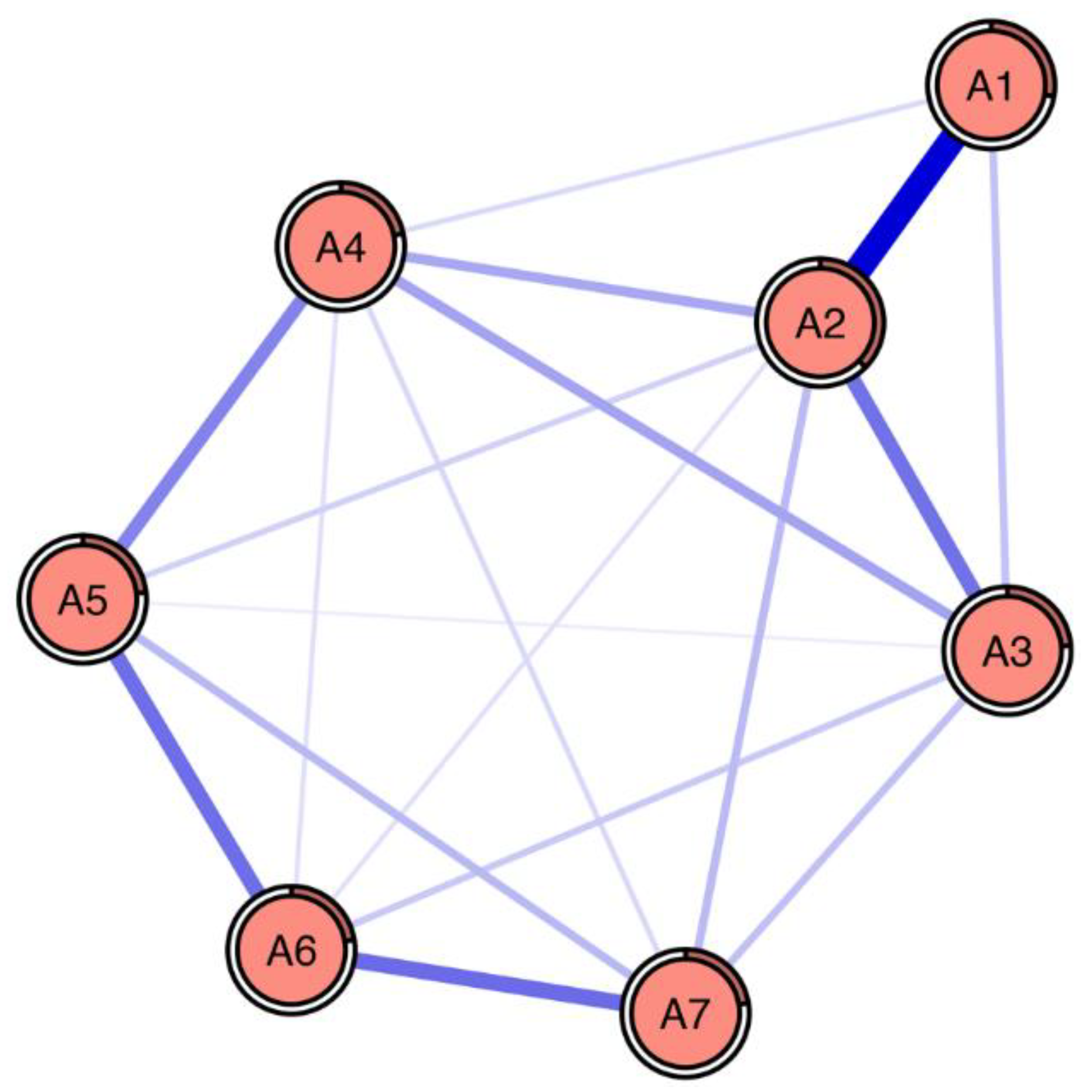
3.2.1. Network Structure
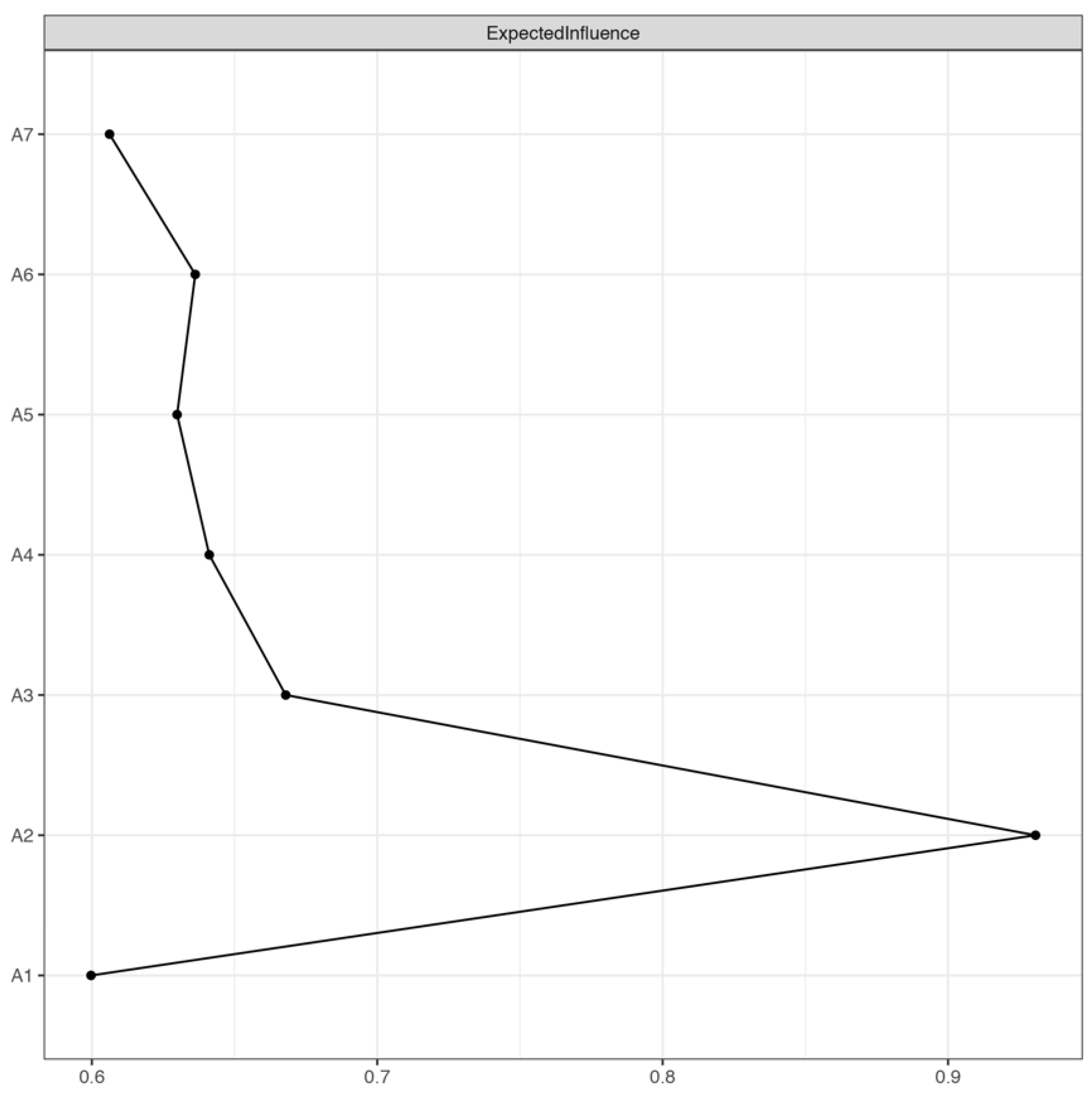
3.2.2. Centrality and Predictability of Nodes
3.2.3. Network Accuracy and Stability
3.2.4. Community Test
3.2.5. Gender-Based Network Comparison
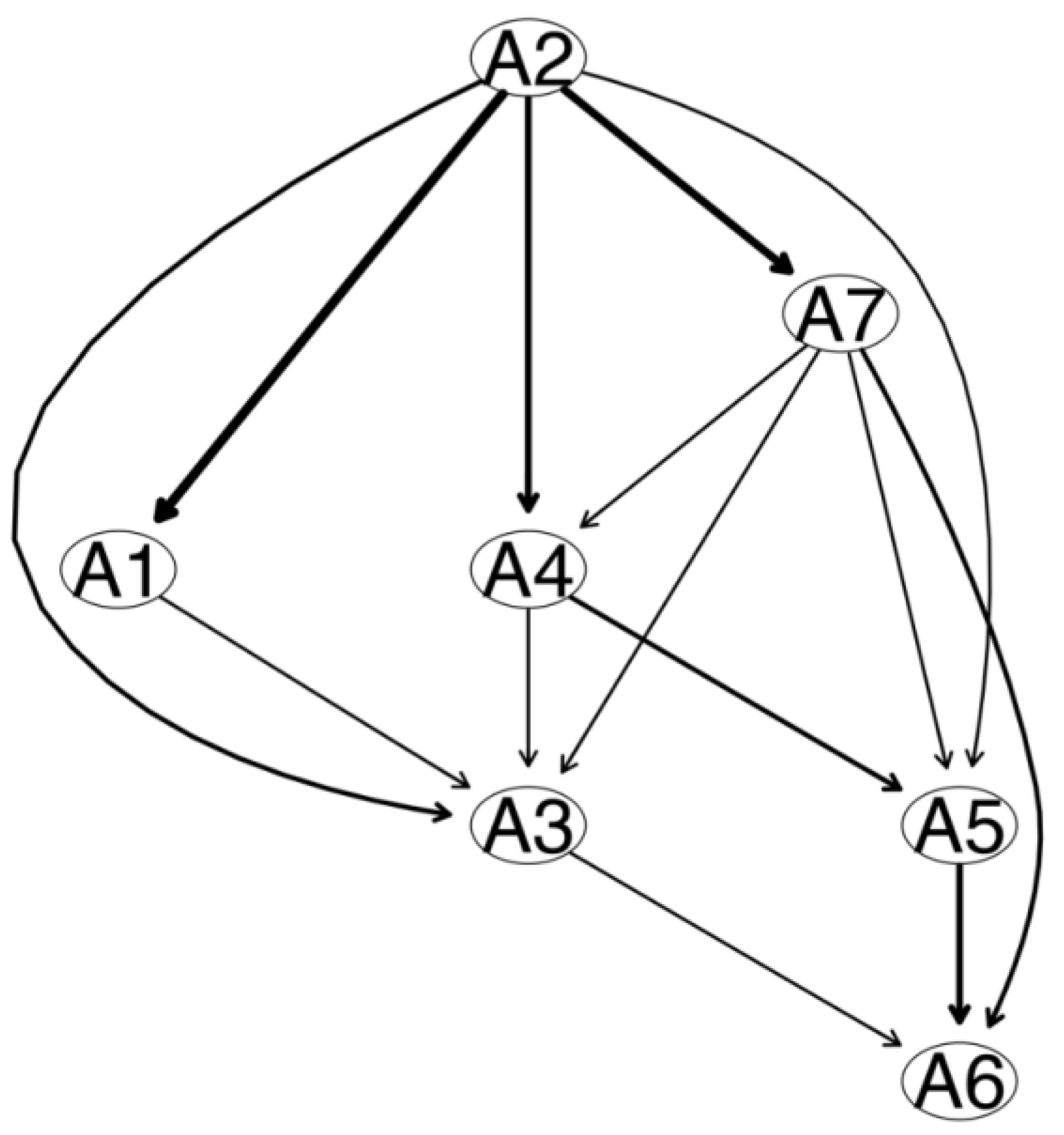
3.3. DAG
4. Discussion
4.1. RPCN
4.1.1. Network Structure
4.1.2. Centrality and Predictability of Item
4.1.3. Community Detection
4.1.4. Gender-Based Network Comparison
4.2. DAG
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wuhan Municipal Health Commission. Circular of Wuhan Municipal Health Committee on Pneumonia Caused by Novel Coronavirus. 2020. Available online: http://wjw.wuhan.gov.cn/front/wed/showDetail/2020011409039 (accessed on 3 February 2020).
- World Health Organization. Coronavirus Disease (COVID-19) Outbreak. Available online: https://www.who.int (accessed on 10 March 2022).
- Yue, Z.Y. Health Cognition, Behavior and Anxiety among Different Groups of People during the Epidemic of COVID-19; Shanxi Medical University: Taiyuan, China, 2021. [Google Scholar]
- Wang, H.; Zhou, X.; Jia, X.; Song, C.; Luo, X.; Zhang, H.; Wu, H.; Ye, J. Emotional exhaustion in front-line healthcare workers during the COVID-19 pandemic in Wuhan, China: The effects of time pressure, social sharing and cognitive appraisal. BMC Public Health 2021, 21, 829. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.W.; Di, J.; Jiang, S.F.; Liu, T.; Dai, Y.F.; Feng, C.Y.; Li, X.M. Knowledge, attitude, and practices of health care workers during COVID-19 epidemic. Chin. J. Med. Manag. Sci. 2021, 11, 66–71. [Google Scholar] [CrossRef]
- Liu, C.-Y.; Yang, Y.-Z.; Zhang, X.-M.; Xu, X.; Dou, Q.-L.; Zhang, W.-W.; Cheng, A.S.K. The prevalence and influencing factors in anxiety in medical workers fighting COVID-19 in China: A cross-sectional survey. Epidemiol. Infect. 2020, 148, e98. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.F.; Wang, Y.F.; Shi, K.; Chen, G.; Tang, S.Q.; Li, Y.Q.; Su, J.K.; Wu, S.J.; Zeng, Q. Analysis of psychological status and influencing factors of medical workers amid COVID 19 pandemic; analysis of influencing factors. Chin. J. Health Manag. 2021, 15, 167–172. [Google Scholar] [CrossRef]
- Xu, M.C.; Zhang, Y. Psychological status survey of first clinical first-line support nurses fighting against pneumonia caused by a 2019 novel coronavirus infection. Chin. Nurs. Res. 2020, 34, 368–370. [Google Scholar] [CrossRef]
- Wu, Y.; Zhu, S.; Chen, Z.L.; Chen, Z.K.; Hong, W.C.; Wang, Y.G. Mental health status among medical personnel in Ruian during the COVID-19 epidemic. J. Chin. Men. Health 2020, 34, 1056–1061. [Google Scholar] [CrossRef]
- Lai, J.; Ma, S.; Wang, Y.; Cai, Z.; Hu, J.; Wei, N.; Wu, J.; Du, H.; Chen, T.; Li, R.; et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw. Open 2020, 3, e203976. [Google Scholar] [CrossRef]
- Lu, W.; Wang, H.; Lin, Y.; Li, L. Psychological status of medical workforce during the COVID-19 pandemic: A cross-sectional study. Psychiatry Res. 2020, 288, 112936. [Google Scholar] [CrossRef]
- Lixia, W.; Xiaoming, X.; Lei, S.; Su, H.; Wo, W.; Xin, F.; Jianmei, C.; Qi, Z.; Ming, A.; Li, K. A cross-sectional study of the psychological status of 33,706 hospital workers at the late stage of the COVID-19 outbreak. J. Affect. Disord. 2022, 297, 156–168. [Google Scholar] [CrossRef]
- Pappa, S.; Ntella, V.; Giannakas, T.; Giannakoulis, V.G.; Papoutsi, E.; Katsaounou, P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav. Immun. 2020, 88, 901–907. [Google Scholar] [CrossRef]
- Marvaldi, M.; Mallet, J.; Dubertret, C.; Moro, M.R.; Guessoum, S.B. Anxiety, depression, trauma-related, and sleep disorders among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Neurosci. Biobehav. Rev. 2021, 126, 252–264. [Google Scholar] [CrossRef]
- Preti, E.; Di Mattei, V.; Perego, G.; Ferrari, F.; Mazzetti, M.; Taranto, P.; Di Pierro, R.; Madeddu, F.; Calati, R. The Psychological Impact of Epidemic and Pandemic Outbreaks on Healthcare Workers: Rapid Review of the Evidence. Curr. Psychiatry Rep. 2020, 22, 43. [Google Scholar] [CrossRef]
- Raoofi, S.; Kan, F.P.; Rafiei, S.; Khani, S.; Hosseinifard, H.; Tajik, F.; Masoumi, M.; Raoofi, N.; Ahmadi, S.; Aghalou, S.; et al. Anxiety during the COVID-19 pandemic in hospital staff: Systematic review plus meta-analysis. BMJ Support. Palliat. Care 2021, 13, 127–135. [Google Scholar] [CrossRef] [PubMed]
- Fang, P.; Shi, K.; Zhu, X.; Huang, P.; Miao, D.M.; Cui, D.; Liu, X.F.; Wu, S.J. Analysis on psychological characteristics of the public in the epidemic of COVID-19. Infect. Dis. Inf. 2020, 33, 30–35. [Google Scholar] [CrossRef]
- Xiong, J.; Lipsitz, O.; Nasri, F.; Lui, L.M.W.; Gill, H.; Phan, L.; Chen-Li, D.; Iacobucci, M.; Ho, R.; Majeed, A.; et al. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J. Affect. Disord. 2020, 277, 55–64. [Google Scholar] [CrossRef] [PubMed]
- Wu, L.; Shi, K.; Fang, P.; Huang, P.; Zhu, X.; Miao, D.M.; Wang, X.C.; Wang, C.X.; Cui, D.; Liu, X.F.; et al. Analysis on the characteristics and changing rules of the public mentality in the early stage of the epidemic of “COVID-19”. J. Prev. Med. Chin. PLA 2020, 38, 182–185+188. [Google Scholar] [CrossRef]
- Ma, C.; Yan, X.K. Research progress in psychological stress response and prevention and control strategies of COVID-19. J. Jilin Univ. (Med. Ed.) 2020, 46, 649–654. [Google Scholar] [CrossRef]
- Wu, P.; Fang, Y.Y.; Guan, Z.Q.; Fan, B.; Kong, J.H.; Yao, Z.L.; Liu, X.H.; Fuller, C.J.; Susser, E.; Lu, J.; et al. The Psychological Impact of the SARS Epidemic on Hospital Employees in China: Exposure, Risk Perception, and Altruistic Acceptance of Risk. Can. J. Psychiatry 2009, 54, 302–311. [Google Scholar] [CrossRef]
- Orrù, G.; Marzetti, F.; Conversano, C.; Vagheggini, G.; Miccoli, M.; Ciacchini, R.; Panait, E.; Gemignani, A. Secondary Traumatic Stress and Burnout in Healthcare Workers during COVID-19 Outbreak. Int. J. Environ. Res. Public Health 2021, 18, 337. [Google Scholar] [CrossRef]
- Boccaletti, S.; Latora, V.; Moreno, Y.; Chavez, M.; Hwang, D.-U. Complex networks: Structure and dynamics. Phys. Rep. 2006, 424, 175–308. [Google Scholar] [CrossRef]
- Galderisi, S.; Rucci, P.; Kirkpatrick, B.; Mucci, A.; Gibertoni, D.; Rocca, P.; Rossi, A.; Bertolino, A.; Strauss, G.P.; Aguglia, E.; et al. Italian Network for Research on Psychoses. Interplay among Psychopathologic Variables, Personal Resources, Context-Related Factors, and Real-life Functioning in Individuals with Schizophrenia: A Network Analysis. JAMA Psychiatry 2018, 75, 396–404. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Borsboom, D. A network theory of mental disorders. World Psychiatry 2017, 16, 5–13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Borsboom, D.; Cramer, A.O. Network Analysis: An Integrative Approach to the Structure of Psychopathology. Annu. Rev. Clin. Psychol. 2013, 9, 91–121. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Haslbeck, J.M.B.; Fried, E.I. How predictable are symptoms in psychopathological networks? A reanalysis of 18 published datasets. Psychol. Med. 2017, 47, 2767–2776. [Google Scholar] [CrossRef] [Green Version]
- Briganti, G.; Fried, E.I.; Linkowski, P. Network analysis of Contingencies of Self-Worth Scale in 680 university students. Psychiatry Res. 2019, 272, 252–257. [Google Scholar] [CrossRef] [Green Version]
- Briganti, G.; Linkowski, P. Item and domain network structures of the Resilience Scale for Adults in 675 university students. Epidemiol. Psychiatr. Sci. 2019, 29, e33. [Google Scholar] [CrossRef] [Green Version]
- Marcus, D.K.; Preszler, J.; Zeigler-Hill, V. A network of dark personality traits: What lies at the heart of darkness? J. Res. Pers. 2018, 73, 56–62. [Google Scholar] [CrossRef]
- Wei, Z.; Ren, L.; Liu, C.; Cao, M.; Yang, Q.; Deng, Y. The concept map of felt stigma in patient with epilepsy. Seizure 2020, 80, 138–142. [Google Scholar] [CrossRef]
- Peng, J.; Ren, L.; Yang, N.; Zhao, L.; Fang, P.; Shao, Y. The Network Structure of Decision-Making Competence in Chinese Adults. Front. Psychol. 2020, 11, 563023. [Google Scholar] [CrossRef]
- Ren, L.; Wang, Y.; Wu, L.; Wei, Z.; Cui, L.-B.; Wei, X.; Hu, X.; Peng, J.; Jin, Y.; Li, F.; et al. Network structure of depression and anxiety symptoms in Chinese female nursing students. BMC Psychiatry 2021, 21, 279. [Google Scholar] [CrossRef]
- Wu, L.; Ren, L.; Wang, Y.; Zhang, K.; Fang, P.; Liu, X.; Yang, Q.; Wang, X.; Wu, S.; Peng, J. The item network and domain network of burnout in Chinese nurses. BMC Nurs. 2021, 20, 147. [Google Scholar] [CrossRef] [PubMed]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.; Monahan, P.O.; Löwe, B. Anxiety Disorders in Primary Care: Prevalence, Impairment, Comorbidity, and Detection. Ann. Intern. Med. 2007, 146, 317–325. [Google Scholar] [CrossRef] [PubMed]
- Plummer, F.; Manea, L.; Trepel, D.; McMillan, D. Screening for anxiety disorders with the GAD-7 and GAD-2: A systematic review and diagnostic metaanalysis. Gen. Hosp. Psychiatry 2016, 39, 24–31. [Google Scholar] [CrossRef] [PubMed]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.W.; Löwe, B. A Brief Measure for Assessing Generalized Anxiety Disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef] [Green Version]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Publishing: Arlingon, VA, USA, 2013. [Google Scholar]
- Epskamp, S.; Fried, E.I. A tutorial on regularized partial correlation networks. Psychol. Methods 2018, 23, 617–634. [Google Scholar] [CrossRef] [Green Version]
- Liu, H.; Han, F.; Yuan, M.; Lafferty, J.; Wasserman, L. High-dimensional semiparametric Gaussian copula graphical models. Ann. Stat. 2012, 40, 2293–2326. [Google Scholar] [CrossRef]
- Heeren, A.; McNally, R.J. Social Anxiety Disorder as a Densely Interconnected Network of Fear and Avoidance for Social Situations. Cogn. Ther. Res. 2018, 42, 103–113. [Google Scholar] [CrossRef]
- Heeren, A.; Hanseeuw, B.; Cougnon, L.-A.; Lits, G. Excessive Worrying as a Central Feature of Anxiety during the First COVID-19 Lockdown-Phase in Belgium: Insights from a Network Approach. Psychol. Belg. 2021, 61, 401–418. [Google Scholar] [CrossRef]
- Blanchard, M.A.; Roskam, I.; Mikolajczak, M.; Heeren, A. A network approach to parental burnout. Child. Abus. Negl. 2021, 111, 104826. [Google Scholar] [CrossRef]
- Jones, P.J. Networktools: Tools for Identifying Important Nodes in Networks, R Package Version 1.5.0; 2022. Available online: https://cran.r-project.org/web/packages/networktools/networktools.pdf (accessed on 26 July 2023).
- Hittner, J.B.; May, K.; Silver, N.C. A Monte Carlo Evaluation of Tests for Comparing Dependent Correlations. J. Gen. Psychol. 2003, 130, 149–168. [Google Scholar] [CrossRef]
- Epskamp, S.; Waldorp, L.J.; Mõttus, R.; Borsboom, D. The Gaussian Graphical Model in Cross-Sectional and Time-Series Data. Multivar. Behav. Res. 2018, 53, 453–480. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Friedman, J.; Hastie, T.; Tibshirani, R. Sparse inverse covariance estimation with the graphical lasso. Biostatistics 2008, 9, 432–441. [Google Scholar] [CrossRef] [Green Version]
- Chen, J.; Chen, Z. Extended Bayesian information criteria for model selection with large model spaces. Biometrika 2008, 95, 759–771. [Google Scholar] [CrossRef] [Green Version]
- Beard, C.; Millner, A.J.; Forgeard, M.J.C.; Fried, E.I.; Hsu, K.J.; Treadway, M.T.; Leonard, C.V.; Kertz, S.J.; Björgvinsson, T. Network analysis of depression and anxiety symptom relationships in a psychiatric sample. Psychol. Med. 2016, 46, 3359–3369. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Foygel, R.; Drton, M. Extended Bayesian information criteria for Gaussian graphical models. Adv. Neural Inf. Process. Syst. 2010, 23, 2020–2028. [Google Scholar]
- Chang, W.C.; Wong, C.S.M.; Or, P.C.F.; Chu, A.O.K.; Hui, C.L.M.; Chan, S.K.W.; Lee, E.M.H.; Suen, Y.N.; Chen, E.Y.H. Inter-relationships among psychopathology, premorbid adjustment, cognition and psychosocial functioning in first-episode psychosis: A network analysis approach. Psychol. Med. 2019, 50, 2019–2027. [Google Scholar] [CrossRef] [PubMed]
- Epskamp, S.; Cramer, A.O.J.; Waldorp, L.J.; Schmittmann, V.D.; Borsboom, D. qgraph: Network Visualizations of Relationships in Psychometric Data. J. Stat. Softw. 2012, 48, 1–18. [Google Scholar] [CrossRef] [Green Version]
- Fruchterman, T.M.J.; Reingold, E.M. Graph drawing by force-directed placement. Softw. Pract. Exp. 1991, 21, 1129–1164. [Google Scholar] [CrossRef]
- Costantini, G.; Epskamp, S.; Borsboom, D.; Perugini, M.; Mõttus, R.; Waldorp, L.J.; Cramer, A.O. State of the aRt personality research: A tutorial on network analysis of personality data in R. J. Res. Pers. 2015, 54, 13–29. [Google Scholar] [CrossRef]
- Robinaugh, D.J.; Millner, A.J.; McNally, R.J. Identifying highly influential nodes in the complicated grief network. J. Abnorm. Psychol. 2016, 125, 747–757. [Google Scholar] [CrossRef] [Green Version]
- Ren, L.; Yang, Z.; Wang, Y.D.; Cui, L.B.; Jin, Y.C.; Ma, Z.J.; Zhang, Q.T.; Wu, Z.Y.; Wang, H.N.; Yang, Q. The relations among worry, meta-worry, intolerance of uncertainty and attentional bias for threat in men at high risk for generalized anxiety disorder: A network analysis. BMC Psychiatry 2020, 20, 452–462. [Google Scholar] [CrossRef] [PubMed]
- Haslbeck, J.M.B.; Waldorp, L.J. How well do network models predict observations? On the importance of predictability in network models. Behav. Res. Methods 2018, 50, 853–861. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Epskamp, S.; Borsboom, D.; Fried, E.I. Estimating psychological networks and their accuracy: A tutorial paper. Behav. Res. Methods 2018, 50, 195–212. [Google Scholar] [CrossRef] [Green Version]
- Borsboom, D.; Robinaugh, D.J.; The Psychosystems Group; Rhemtulla, M.; Cramer, A.O. Robustness and replicability of psychopathology networks. World Psychiatry 2018, 17, 143–144. [Google Scholar] [CrossRef] [Green Version]
- Csardi, G.; Nepusz, T. The igraph software package for complex network research. Int. J. Complex Syst. 2006, 1695. Available online: https://www.researchgate.net/publication/221995787_The_Igraph_Software_Package_for_Complex_Network_Research (accessed on 26 July 2023).
- Yang, Z.; Algesheimer, R.; Tessone, C.J. A Comparative Analysis of Community Detection Algorithms on Artificial Networks. Sci. Rep. 2016, 6, 30750. [Google Scholar] [CrossRef] [Green Version]
- van Borkulo, C.D.; van Bork, R.; Boschloo, L.; Kossakowski, J.J.; Tio, P.; Schoevers, R.A.; Borsboom, D.; Waldorp, L.J. Comparing network structures on three aspects: A permutation test. Psychol. Methods, 2022; advance online publication. [Google Scholar] [CrossRef]
- Scutari, M. Learning Bayesian networks with the bnlearn R package. J. Stat. Softw. 2010, 35, 1–22. [Google Scholar] [CrossRef] [Green Version]
- Scutari, M.; Denis, J. Bayesian Networks: With Examples in R; CRC Press: Boca Raton, FL, USA, 2015. [Google Scholar]
- Heeren, A.; Bernstein, E.E.; McNally, R.J. Bridging maladaptive social self-beliefs and social anxiety: A network perspective. J. Anxiety Disord. 2020, 74, 102267. [Google Scholar] [CrossRef]
- Bernstein, E.E.; Heeren, A.; McNally, R.J. Unpacking Rumination and Executive Control: A Network Perspective. Clin. Psychol. Sci. 2017, 5, 816–826. [Google Scholar] [CrossRef]
- Li, K.L.; Ren, L.; Zhang, L.; Liu, C.; Zhao, M.X.; Zhan, X.Q.; Li, L.; Luo, X.; Feng, Z.Z. Social anxiety and depression symptoms in Chinese left-behind children after the lifting of COVID-19 lockdown: A network analysis. Int J Soc Psychiatry 2023, 4, 916–927. [Google Scholar] [CrossRef] [PubMed]
- Scutari, M.; Nagarajan, R. Identifying significant edges in graphical models of molecular networks. Artif. Intell. Med. 2013, 57, 207–217. [Google Scholar] [CrossRef] [Green Version]
- Wang, Y.; Hu, Z.; Feng, Y.; Wilson, A.; Chen, R. Changes in network centrality of psychopathology symptoms between the COVID-19 outbreak and after peak. Mol. Psychiatry 2020, 25, 3140–3149. [Google Scholar] [CrossRef] [PubMed]
- Bai, W.; Cai, H.; Liu, S.; Chen, X.; Sha, S.; Cheung, T.; Lin, J.J.; Cui, X.; Ng, C.H.; Xiang, Y.-T. Anxiety and depressive symptoms in college students during the late stage of the COVID-19 outbreak: A network approach. Transl. Psychiatry 2021, 11, 638. [Google Scholar] [CrossRef]
- Hoffart, A.; Johnson, S.U.; Ebrahimi, O.V. The network of stress-related states and depression and anxiety symptoms during the COVID-19 lockdown. J. Affect. Disord. 2021, 294, 671–678. [Google Scholar] [CrossRef]
- Zavlis, O.; Butter, S.; Bennett, K.; Hartman, T.K.; Hyland, P.; Mason, L.; McBride, O.; Murphy, J.; Gibson-Miller, J.; Levita, L.; et al. How does the COVID-19 pandemic impact on population mental health? A network analysis of COVID influences on depression, anxiety and traumatic stress in the UK population. Psychol. Med. 2021, 52, 3825–3833. [Google Scholar] [CrossRef]
- Noreen, F.; Shehzadi, K.; Mehmood, K.; Mulfqar, M.; Maqsood, S.; Khalid, K. A Research on SARS-COVID-19 and mental health. J. Depress. Anxiety 2021, 10, 411. [Google Scholar]
- Wei, Z.; Ren, L.; Wang, X.; Liu, C.; Cao, M.; Hu, M.; Jiang, Z.; Hui, B.; Xia, F.; Yang, Q.; et al. Network of depression and anxiety symptoms in patients with epilepsy. Epilepsy Res. 2021, 175, 106696. [Google Scholar] [CrossRef] [PubMed]
- Osborn, T.L.; Campbell, S.; Weisz, J.R.; Ndetei, D.M. Network Analysis Reveals Central Symptoms of Adolescent Depression and Anxiety in Sub-Saharan Africa. PsyArXix 2020. [Google Scholar] [CrossRef] [Green Version]
- Cheung, T.; Wong, S.Y.; Wong, K.Y.; Law, L.Y.; Ng, K.; Tong, M.T.; Wong, K.Y.; Ng, M.Y.; Yip, P.S. Depression, Anxiety and Symptoms of Stress among Baccalaureate Nursing Students in Hong Kong: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2016, 13, 779–803. [Google Scholar] [CrossRef] [Green Version]
- Ruscio, A.M.; Hallion, L.S.; Lim, C.C.W.; Aguilar-Gaxiola, S.; Al-Hamzawi, A.; Alonso, J.; Andrade, L.H.; Borges, G.; Bromet, E.J.; Bunting, B.; et al. Cross-sectional Comparison of the Epidemiology of DSM-5 Generalized Anxiety Disorder across the Globe. JAMA Psychiatry 2017, 74, 465–475. [Google Scholar] [CrossRef] [Green Version]
- Craske, M.G.; Stein, M.B. Anxiety. Lancet 2016, 388, 3048–3059. [Google Scholar] [CrossRef]
- Blanchard, M.A.; Heeren, A. Ongoing and future challenges of the network approach to psychopathology: From theoretical conjectures to clinical translations. In Comprehensive Clinical Psychology, 2nd ed.; Asmundson, G., Ed.; Elsevier: Amsterdam, The Netherlands, 2022. [Google Scholar]
- Bonchi, F.; Hajian, S.; Mishra, B.; Ramazzotti, D. Exposing the probabilistic causal structure of discrimination. Int. J. Data Sci. Anal. 2017, 3, 1–21. [Google Scholar] [CrossRef] [Green Version]
- Myin-Germeys, I.; Kasanova, Z.; Vaessen, T.; Vachon, H.; Kirtley, O.; Viechtbauer, W.; Reininghaus, U. Experience sampling methodology in mental health research: New insights and technical developments. World Psychiatry 2018, 17, 123–132. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McNally, R.J.; Mair, P.; Mugno, B.L.; Riemann, B.C. Co-morbid obsessive–compulsive disorder and depression: A Bayesian network approach. Psychol. Med. 2017, 47, 1204–1214. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McNally, R.J.; Heeren, A.; Robinaugh, D.J. A Bayesian network analysis of posttraumatic stress disorder symptoms in adults reporting childhood sexual abuse. Eur. J. Psychotraumatol. 2017, 8 (Suppl. S3), 1341276. [Google Scholar] [CrossRef] [Green Version]
- Heeren, A.; Bernstein, E.E.; McNally, R.J. Deconstructing trait anxiety: A network perspective. Anxiety Stress. Coping 2018, 31, 262–276. [Google Scholar] [CrossRef]
- Ren, L. The Characteristics of Symptoms and Cognitions for Generalized Anxiety Disorder in Young Males: A Network Analysis; Air Force Medical University of the Chinese People’s Liberation Army: Xi’an, China, 2020. [Google Scholar]
- Everaert, J.; Joormann, J. Emotion Regulation Difficulties Related to Depression and Anxiety: A Network Approach to Model Relations Among Symptoms, Positive Reappraisal, and Repetitive Negative Thinking. Clin. Psychol. Sci. 2019, 7, 1304–1318. [Google Scholar] [CrossRef] [Green Version]

| Item | Number (n) | Percentage (%) |
|---|---|---|
| Gender | ||
| Male | 238 | 23.0 |
| Female | 796 | 77.0 |
| Marital status | ||
| Married | 825 | 79.8 |
| Unmarried | 189 | 18.3 |
| Other (Widowhood, divorce, etc.) | 20 | 1.9 |
| Education | ||
| Below bachelor’s degree | 340 | 32.9 |
| Bachelor’s degree or above | 694 | 67.1 |
| Job | ||
| Doctor | 302 | 29.2 |
| Nurse | 732 | 70.8 |
| Title | ||
| Non | 91 | 8.8 |
| Primary | 444 | 42.9 |
| Intermediate | 341 | 33.0 |
| Senior | 158 | 15.3 |
| Years of service | ||
| ≤3 years | 181 | 17.5 |
| 4–10 years | 346 | 33.5 |
| ≥10 years | 507 | 49.0 |
| ± s | Min | Max | Expected Influence (EI) | Predictability (Pre) | |
|---|---|---|---|---|---|
| A1 | 1.86 ± 0.81 | 0 | 3 | 0.60 | 0.28 |
| A2 | 1.69 ± 0.78 | 0 | 3 | 0.93 | 0.37 |
| A3 | 1.85 ± 0.75 | 0 | 3 | 0.67 | 0.24 |
| A4 | 1.80 ± 0.78 | 0 | 3 | 0.64 | 0.22 |
| A5 | 1.28 ± 0.78 | 0 | 3 | 0.63 | 0.23 |
| A6 | 1.76 ± 0.82 | 0 | 3 | 0.64 | 0.22 |
| A7 | 1.33 ± 0.78 | 0 | 3 | 0.61 | 0.22 |
| A1 | A2 | A3 | A4 | A5 | A6 | A7 | |
| A1 | 0 | ||||||
| A2 | 0.40 | 0 | |||||
| A3 | 0.10 | 0.22 | 0 | ||||
| A4 | 0.06 | 0.13 | 0.14 | 0 | |||
| A5 | 0 | 0.07 | 0.03 | 0.19 | 0 | ||
| A6 | 0.05 | 0 | 0.08 | 0.05 | 0.23 | 0 | |
| A7 | 0 | 0.11 | 0.10 | 0.06 | 0.11 | 0.23 | 0 |
| Arrow | Thickness Value of Arrow | ||
|---|---|---|---|
| From | To | BIC | Direction Probability |
| A1 | A3 | −3.24 | 0.57 |
| A2 | A1 | −152.35 | 0.55 |
| A2 | A3 | −25.17 | 0.65 |
| A2 | A4 | −41.62 | 0.62 |
| A2 | A5 | −3.34 | 0.64 |
| A2 | A7 | −41.76 | 0.64 |
| A3 | A6 | −3.22 | 0.63 |
| A4 | A3 | −10.62 | 0.51 |
| A4 | A5 | −27.35 | 0.55 |
| A5 | A6 | −35.22 | 0.65 |
| A7 | A3 | −7.78 | 0.52 |
| A7 | A4 | −13.05 | 0.53 |
| A7 | A5 | −22.93 | 0.50 |
| A7 | A6 | −33.83 | 0.65 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wu, L.; Ren, L.; Li, F.; Shi, K.; Fang, P.; Wang, X.; Feng, T.; Wu, S.; Liu, X. Network Analysis of Anxiety Symptoms in Front-Line Medical Staff during the COVID-19 Pandemic. Brain Sci. 2023, 13, 1155. https://doi.org/10.3390/brainsci13081155
Wu L, Ren L, Li F, Shi K, Fang P, Wang X, Feng T, Wu S, Liu X. Network Analysis of Anxiety Symptoms in Front-Line Medical Staff during the COVID-19 Pandemic. Brain Sciences. 2023; 13(8):1155. https://doi.org/10.3390/brainsci13081155
Chicago/Turabian StyleWu, Lin, Lei Ren, Fengzhan Li, Kang Shi, Peng Fang, Xiuchao Wang, Tingwei Feng, Shengjun Wu, and Xufeng Liu. 2023. "Network Analysis of Anxiety Symptoms in Front-Line Medical Staff during the COVID-19 Pandemic" Brain Sciences 13, no. 8: 1155. https://doi.org/10.3390/brainsci13081155
APA StyleWu, L., Ren, L., Li, F., Shi, K., Fang, P., Wang, X., Feng, T., Wu, S., & Liu, X. (2023). Network Analysis of Anxiety Symptoms in Front-Line Medical Staff during the COVID-19 Pandemic. Brain Sciences, 13(8), 1155. https://doi.org/10.3390/brainsci13081155





