Lower Serum Iron Level Predicts Postoperative Global Cerebral Edema Following Aneurysmal Subarachnoid Hemorrhage
Abstract
:1. Introduction
2. Materials and Methods
2.1. Inclusion and Exclusion Criteria
2.2. Laboratory and Clinical Data
2.3. Clinical Management
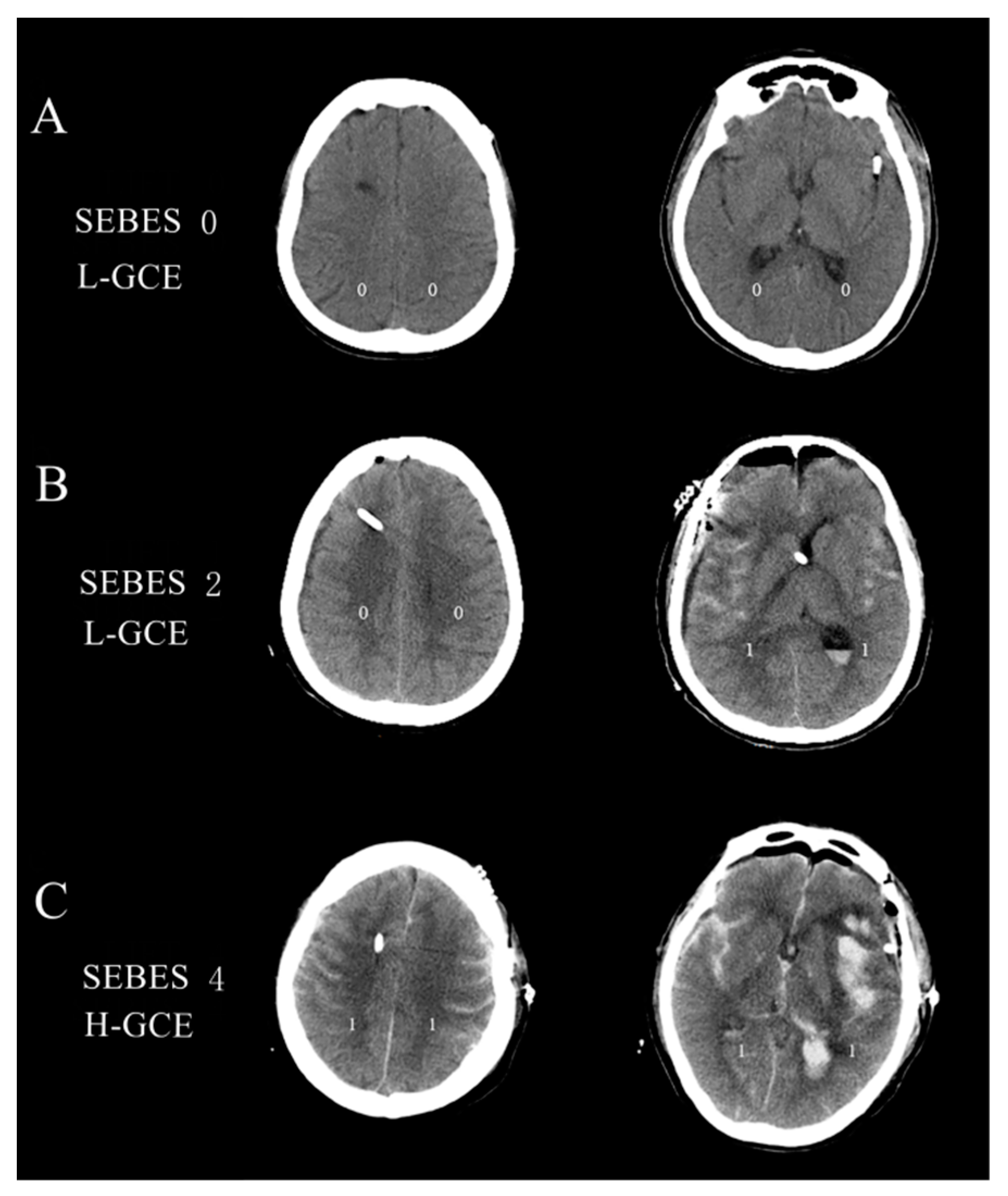
2.4. Clinical Outcome Assessment
3. Statistical Analysis
4. Results
4.1. Baseline Characteristics
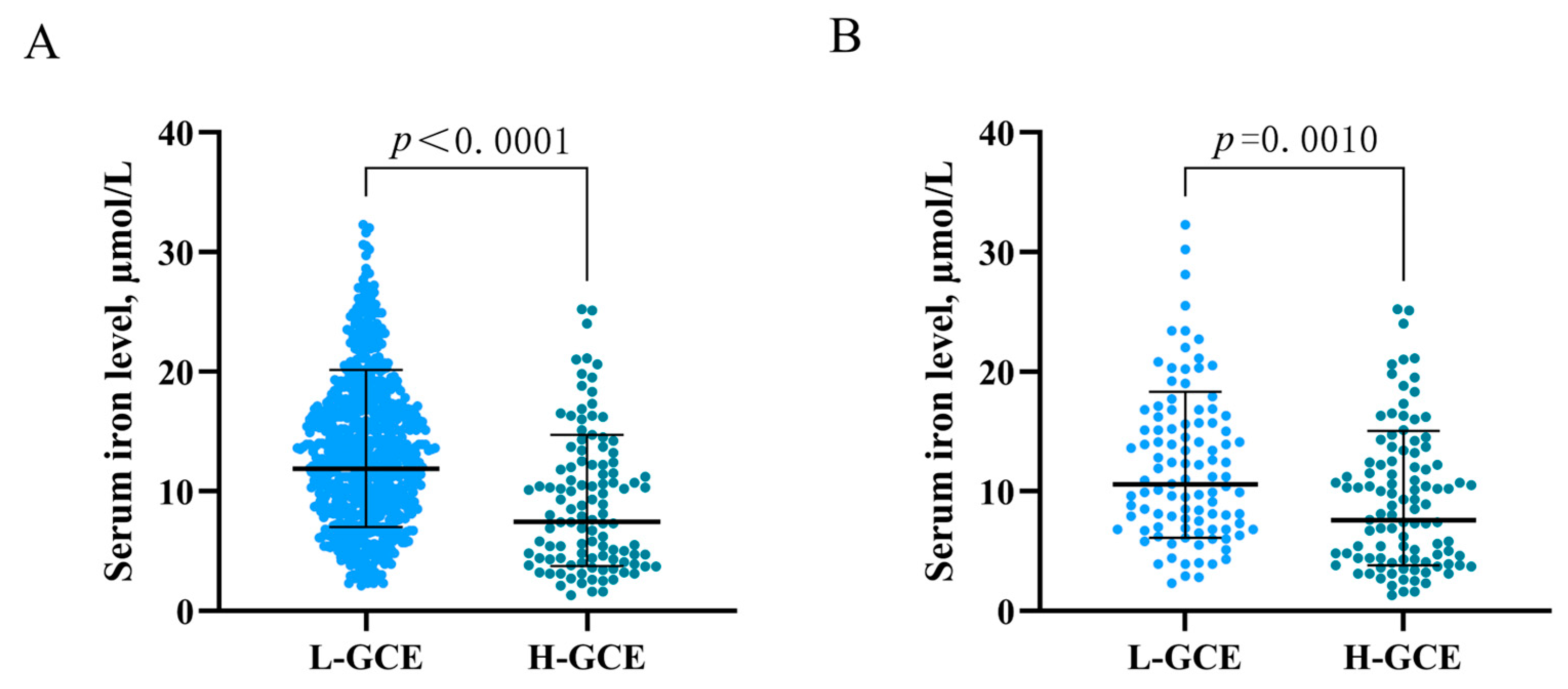
4.2. Risk Factors for H-GCE
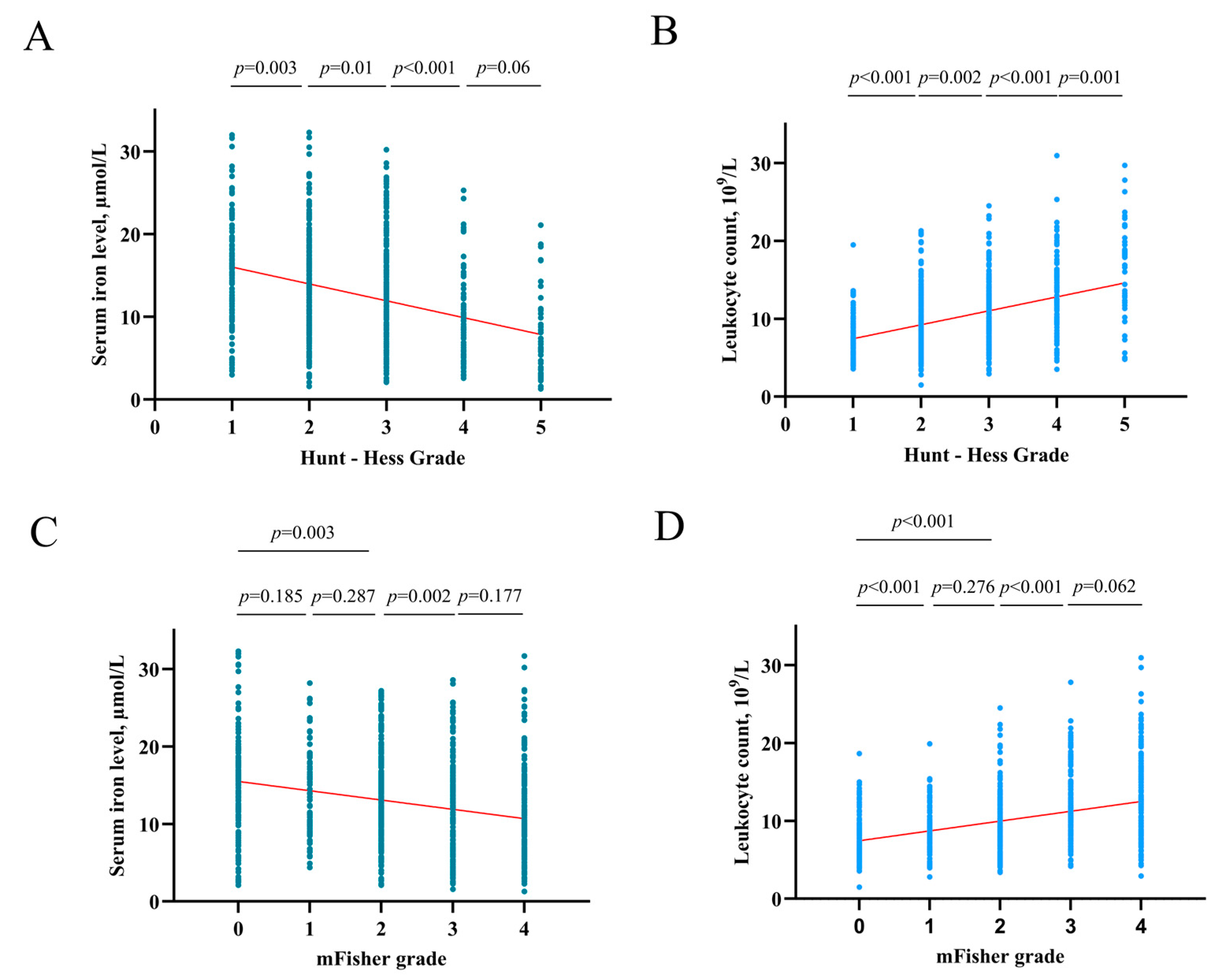
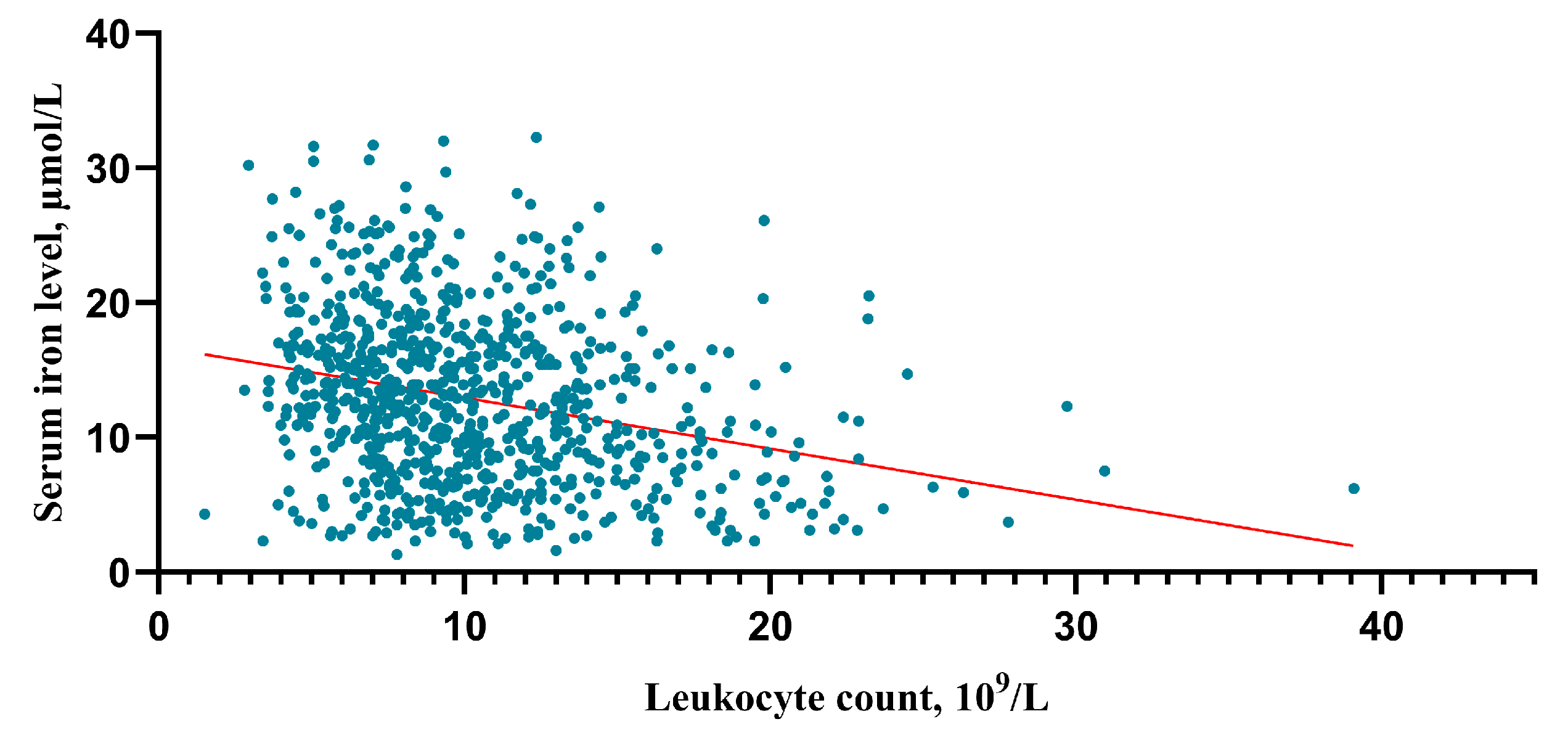
4.3. Association of Serum Iron with HHgrade and mFisher Grade
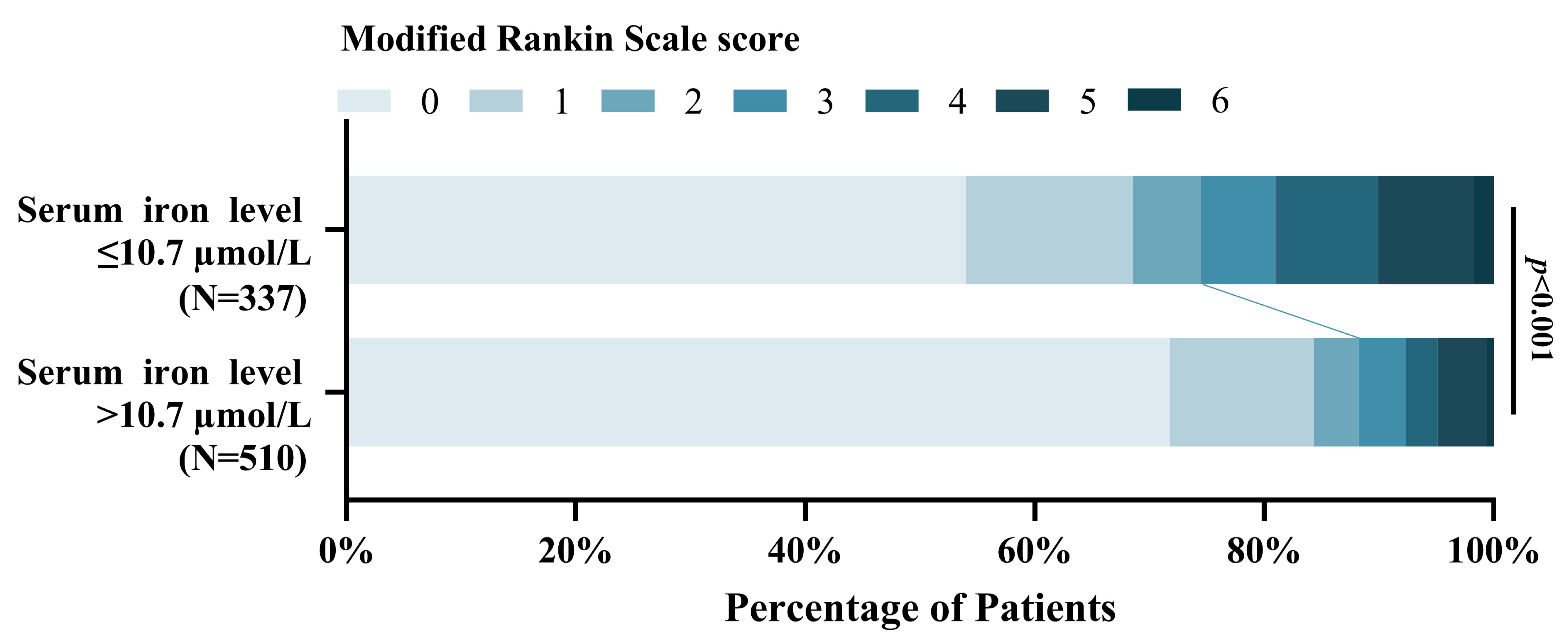
4.4. Association of Serum Iron with Poor 3-Month Functional Outcome
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Macdonald, R.L.; Schweizer, T.A. Spontaneous subarachnoid haemorrhage. Lancet 2017, 389, 655–666. [Google Scholar] [CrossRef]
- Hayman, E.G.; Wessell, A.; Gerzanich, V.; Sheth, K.N.; Simard, J.M. Mechanisms of Global Cerebral Edema Formation in Aneurysmal Subarachnoid Hemorrhage. Neurocrit. Care 2017, 26, 301–310. [Google Scholar] [CrossRef] [PubMed]
- Lantigua, H.; Ortega-Gutierrez, S.; Schmidt, J.M.; Lee, K.; Badjatia, N.; Agarwal, S.; Claassen, J.; Connolly, E.S.; Mayer, S.A. Subarachnoid hemorrhage: Who dies, and why? Crit. Care 2015, 19, 309. [Google Scholar] [CrossRef] [PubMed]
- Choi, H.A.; Bajgur, S.S.; Jones, W.H.; Savarraj, J.P.; Ko, S.B.; Edwards, N.J.; Chang, T.R.; Hergenroeder, G.W.; Dannenbaum, M.J.; Chen, P.R.; et al. Quantification of Cerebral Edema After Subarachnoid Hemorrhage. Neurocrit. Care 2016, 25, 64–70. [Google Scholar] [CrossRef] [PubMed]
- Rass, V.; Ianosi, B.A.; Wegmann, A.; Gaasch, M.; Schiefecker, A.J.; Kofler, M.; Lindner, A.; Addis, A.; Almashad, S.S.; Rhomberg, P.; et al. Delayed Resolution of Cerebral Edema Is Associated with Poor Outcome after Nontraumatic Subarachnoid Hemorrhage. Stroke 2019, 50, 828–836. [Google Scholar] [CrossRef]
- Ahn, S.H.; Burkett, A.; Paz, A.; Savarraj, J.P.; Hinds, S.; Hergenroeder, G.; Gusdon, A.M.; Ren, X.; Hong, J.H.; Choi, H.A. Systemic inflammatory markers of persistent cerebral edema after aneurysmal subarachnoid hemorrhage. J. Neuroinflamm. 2022, 19, 199. [Google Scholar] [CrossRef] [PubMed]
- Torné, R.; Hoyos, J.; Llull, L.; Rodríguez-Hernández, A.; Muñoz, G.; Mellado-Artigas, R.; Santana, D.; Pedrosa, L.; Di Somma, A.; San Roman, L.; et al. Edema Resolution and Clinical Assessment in Poor-Grade Subarachnoid Hemorrhage: Useful Indicators to Predict Delayed Cerebral Infarctions? J. Clin. Med. 2021, 10, 321. [Google Scholar] [CrossRef]
- Helbok, R.; Ko, S.B.; Schmidt, J.M.; Kurtz, P.; Fernandez, L.; Choi, H.A.; Connolly, E.S.; Lee, K.; Badjatia, N.; Mayer, S.A.; et al. Global cerebral edema and brain metabolism after subarachnoid hemorrhage. Stroke 2011, 42, 1534–1539. [Google Scholar] [CrossRef]
- Zetterling, M.; Hallberg, L.; Hillered, L.; Karlsson, T.; Enblad, P.; Ronne Engström, E. Brain energy metabolism in patients with spontaneous subarachnoid hemorrhage and global cerebral edema. Neurosurgery 2010, 66, 1102–1110. [Google Scholar] [CrossRef]
- Thal, S.C.; Sporer, S.; Klopotowski, M.; Thal, S.E.; Woitzik, J.; Schmid-Elsaesser, R.; Plesnila, N.; Zausinger, S. Brain edema formation and neurological impairment after subarachnoid hemorrhage in rats. Laboratory investigation. J. Neurosurg. 2009, 111, 988–994. [Google Scholar] [CrossRef]
- Claassen, J.; Carhuapoma, J.R.; Kreiter, K.T.; Du, E.Y.; Connolly, E.S.; Mayer, S.A. Global cerebral edema after subarachnoid hemorrhage: Frequency, predictors, and impact on outcome. Stroke 2002, 33, 1225–1232. [Google Scholar] [CrossRef] [PubMed]
- Loftspring, M.C. Iron and early brain injury after subarachnoid hemorrhage. J. Cereb. Blood Flow Metab. 2010, 30, 1791–1792. [Google Scholar] [CrossRef] [PubMed]
- Helbok, R.; Rass, V.; Kofler, M.; Talasz, H.; Schiefecker, A.; Gaasch, M.; Scherfler, C.; Pfausler, B.; Thome, C.; Beer, R.; et al. Intracerebral Iron Accumulation may be Associated with Secondary Brain Injury in Patients with Poor Grade Subarachnoid Hemorrhage. Neurocrit. Care 2022, 36, 171–179. [Google Scholar] [CrossRef] [PubMed]
- Bulters, D.; Gaastra, B.; Zolnourian, A.; Alexander, S.; Ren, D.; Blackburn, S.L.; Borsody, M.; Dore, S.; Galea, J.; Iihara, K.; et al. Haemoglobin scavenging in intracranial bleeding: Biology and clinical implications. Nat. Rev. Neurol. 2018, 14, 416–432. [Google Scholar] [CrossRef]
- Bakhshayesh, B.; Hosseininezhad, M.; Nazanin Seyed Saadat, S.; Moien Ansar, M.; Ramezani, H.; Mohammad Seyed Saadat, S. Iron Overload is Associated with Perihematoma Edema Growth Following Intracerebral Hemorrhage that may Contribute to In-hospital Mortality and Long-term Functional Outcome. Curr. Neurovasc. Res. 2014, 11, 248–253. [Google Scholar] [CrossRef]
- Zhang, Y.B.; Zheng, S.F.; Shang-Guan, H.C.; Kang, D.Z.; Chen, G.R.; Yao, P.S. Lower Iron Levels Predict Acute Hydrocephalus Following Aneurysmal Subarachnoid Hemorrhage. World Neurosurg. 2019, 126, e907–e913. [Google Scholar] [CrossRef]
- Zhang, Y.B.; Zheng, F.; Stavrinou, L.; Wang, H.J.; Fan, W.J.; Yao, P.S.; Lin, Y.X.; Goldbrunner, R.; Zheng, S.F.; Stavrinou, P.; et al. Admission Serum Iron as an Independent Risk Factor for Postoperative Delayed Cerebral Ischemia Following Aneurysmal Subarachnoid Hemorrhage: A Propensity-Matched Analysis. Brain Sci. 2022, 12, 1183. [Google Scholar] [CrossRef]
- Wang, D.L.; Lin, P.; Lin, Z.Y.; Zheng, S.F.; Shang-Guan, H.C.; Kang, D.Z.; Chen, G.R.; Zhang, Y.B.; Wen, C.S.; Lin, Y.X.; et al. Lower Hemoglobin Levels Are Associated with Acute Seizures in Patients with Ruptured Cerebral Aneurysms. World Neurosurg. 2019, 127, e1237–e1241. [Google Scholar] [CrossRef]
- Zhang, Y.; Zheng, S.; Wang, H.; Chen, G.; Li, C.; Lin, Y.; Yao, P.; Kang, D. Admission Lower Serum Phosphate Ion Levels Predict Acute Hydrocephalus of Aneurysmal Subarachnoid Hemorrhage. Front. Neurol. 2021, 12, 759963. [Google Scholar] [CrossRef]
- English, S.W.; Chasse, M.; Turgeon, A.F.; Lauzier, F.; Griesdale, D.; Garland, A.; Fergusson, D.; Zarychanski, R.; van Walraven, C.; Montroy, K.; et al. Anemia prevalence and incidence and red blood cell transfusion practices in aneurysmal subarachnoid hemorrhage: Results of a multicenter cohort study. Crit. Care 2018, 22, 169. [Google Scholar] [CrossRef]
- Jabbarli, R.; Pierscianek, D.; Rolz, R.; Darkwah Oppong, M.; Kaier, K.; Shah, M.; Taschner, C.; Monninghoff, C.; Urbach, H.; Beck, J.; et al. Endovascular treatment of cerebral vasospasm after subarachnoid hemorrhage: More is more. Neurology 2019, 93, e458–e466. [Google Scholar] [CrossRef]
- Ahn, S.H.; Savarraj, J.P.; Pervez, M.; Jones, W.; Park, J.; Jeon, S.B.; Kwon, S.U.; Chang, T.R.; Lee, K.; Kim, D.H.; et al. The Subarachnoid Hemorrhage Early Brain Edema Score Predicts Delayed Cerebral Ischemia and Clinical Outcomes. Neurosurgery 2018, 83, 137–145. [Google Scholar] [CrossRef]
- Hemphill, J.C., 3rd; Greenberg, S.M.; Anderson, C.S.; Becker, K.; Bendok, B.R.; Cushman, M.; Fung, G.L.; Goldstein, J.N.; Macdonald, R.L.; Mitchell, P.H.; et al. Guidelines for the Management of Spontaneous Intracerebral Hemorrhage: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke 2015, 46, 2032–2060. [Google Scholar] [CrossRef] [PubMed]
- Claassen, J.; Park, S. Spontaneous subarachnoid haemorrhage. Lancet 2022, 400, 846–862. [Google Scholar] [CrossRef]
- Zheng, S.F.; Lin, P.; Lin, Z.Y.; Shang-Guan, H.C.; Chen, G.R.; Zhang, Y.B.; Lin, Y.X.; Kang, D.Z.; Yao, P.S. Lower Serum Iron and Hemoglobin Levels are Associated with Acute Seizures in Patients with Ruptured Cerebral Aneurysms. Neurocrit. Care 2019, 31, 501–506. [Google Scholar] [CrossRef]
- Xia, F.; Keep, R.F.; Ye, F.; Holste, K.G.; Wan, S.; Xi, G.; Hua, Y. The Fate of Erythrocytes after Cerebral Hemorrhage. Transl. Stroke Res. 2022, 13, 655–664. [Google Scholar] [CrossRef]
- Xi, G.; Keep, R.F.; Hoff, J.T. Mechanisms of brain injury after intracerebral haemorrhage. Lancet Neurol. 2006, 5, 53–63. [Google Scholar] [CrossRef] [PubMed]
- Gomes, J.A.; Selim, M.; Cotleur, A.; Hussain, M.S.; Toth, G.; Koffman, L.; Asi, K.; Provencio, J.J. Brain iron metabolism and brain injury following subarachnoid hemorrhage: iCeFISH-pilot (CSF iron in SAH). Neurocrit. Care 2014, 21, 285–293. [Google Scholar] [CrossRef] [PubMed]
- Heinsberg, L.W.; Alexander, S.A.; Crago, E.A.; Minster, R.L.; Poloyac, S.M.; Weeks, D.E.; Conley, Y.P. Genetic Variability in the Iron Homeostasis Pathway and Patient Outcomes After Aneurysmal Subarachnoid Hemorrhage. Neurocrit. Care 2020, 33, 749–758. [Google Scholar] [CrossRef]
- Heinsberg, L.W.; Arockiaraj, A.I.; Crago, E.A.; Ren, D.; Shaffer, J.R.; Sherwood, P.R.; Sereika, S.M.; Weeks, D.E.; Conley, Y.P. Genetic Variability and Trajectories of DNA Methylation May Support a Role for HAMP in Patient Outcomes After Aneurysmal Subarachnoid Hemorrhage. Neurocrit. Care 2020, 32, 550–563. [Google Scholar] [CrossRef]
- Muñoz, M.; Romero, A.; Morales, M.; Campos, A.; García-Erce, J.A.; Ramírez, G. Iron metabolism, inflammation and anemia in critically ill patients. A cross-sectional study. Nutr. Hosp. 2005, 20, 115–120. [Google Scholar] [PubMed]
- Chaudhry, S.R.; Kahlert, U.D.; Kinfe, T.M.; Lamprecht, A.; Niemela, M.; Hanggi, D.; Muhammad, S. Elevated Systemic IL-10 Levels Indicate Immunodepression Leading to Nosocomial Infections after Aneurysmal Subarachnoid Hemorrhage (SAH) in Patients. Int. J. Mol. Sci. 2020, 21, 1569. [Google Scholar] [CrossRef] [PubMed]
- Simon, M.; Grote, A. Interleukin 6 and Aneurysmal Subarachnoid Hemorrhage. A Narrative Review. Int. J. Mol. Sci. 2021, 22, 4133. [Google Scholar] [CrossRef] [PubMed]
- Ma, X.; Lan, F.; Zhang, Y. Associations between C-reactive protein and white blood cell count, occurrence of delayed cerebral ischemia and poor outcome following aneurysmal subarachnoid hemorrhage: A systematic review and meta-analysis. Acta Neurol. Belg. 2021, 121, 1311–1324. [Google Scholar] [CrossRef] [PubMed]
- Tombini, M.; Squitti, R.; Cacciapaglia, F.; Ventriglia, M.; Assenza, G.; Benvenga, A.; Pellegrino, G.; Campana, C.; Assenza, F.; Siotto, M.; et al. Inflammation and iron metabolism in adult patients with epilepsy: Does a link exist? Epilepsy Res. 2013, 107, 244–252. [Google Scholar] [CrossRef]
- Panther, E.J.; Zelmanovich, R.; Hernandez, J.; Dioso, E.R.; Foster, D.; Lucke-Wold, B. Ferritin and Neurotoxicity: A Contributor to Deleterious Outcomes for Subarachnoid Hemorrhage. Eur. Neurol. 2022, 85, 415–423. [Google Scholar] [CrossRef]
- Hua, Y.; Keep, R.F.; Hoff, J.T.; Xi, G. Brain injury after intracerebral hemorrhage: The role of thrombin and iron. Stroke 2007, 38, 759–762. [Google Scholar] [CrossRef]
- Mehta, P.J.; Chapman, S.; Jayam-Trouth, A.; Kurukumbi, M. Acute ischemic stroke secondary to iron deficiency anemia: A case report. Case Rep. Neurol. Med. 2012, 2012, 487080. [Google Scholar] [CrossRef]
- Nagababu, E.; Gulyani, S.; Earley, C.J.; Cutler, R.G.; Mattson, M.P.; Rifkind, J.M. Iron-deficiency anaemia enhances red blood cell oxidative stress. Free Radic. Res. 2008, 42, 824–829. [Google Scholar] [CrossRef]
- Sabri, M.; Ai, J.; Lass, E.; D’Abbondanza, J.; Macdonald, R.L. Genetic elimination of eNOS reduces secondary complications of experimental subarachnoid hemorrhage. J. Cereb. Blood Flow. Metab. 2013, 33, 1008–1014. [Google Scholar] [CrossRef]
- Deng, X.; Wu, Y.; Hu, Z.; Wang, S.; Zhou, S.; Zhou, C.; Gao, X.; Huang, Y. The mechanism of ferroptosis in early brain injury after subarachnoid hemorrhage. Front. Immunol. 2023, 14, 1191826. [Google Scholar] [CrossRef] [PubMed]
- Zetterling, M.; Hallberg, L.; Ronne-Engström, E. Early global brain oedema in relation to clinical admission parameters and outcome in patients with aneurysmal subarachnoid haemorrhage. Acta Neurochir. 2010, 152, 1527–1533. [Google Scholar] [CrossRef] [PubMed]
- Eibach, M.; Won, S.Y.; Bruder, M.; Keil, F.; Herrmann, E.; Berkefeld, J.; Seifert, V.; Konczalla, J. Age dependency and modification of the Subarachnoid Hemorrhage Early Brain Edema Score. J. Neurosurg. 2020, 134, 946–952. [Google Scholar] [CrossRef] [PubMed]


| Before Propensity-Score Matching | |||
|---|---|---|---|
| Characteristics | High-Grade Global Cerebral Edema | Low-Grade Global Cerebral Edema | p-Value |
| N = 110 | N = 737 | ||
| Age, mean (SD) y | 54.75 (11.874) | 54.51 (11.643) | 0.841 |
| Gender, female (N, %) | 62 (56.36%) | 444 (60.24%) | 0.439 |
| Medical history (N, %) | |||
| Smoking | 18 (16.36%) | 131 (17.77%) | 0.717 |
| Drinking | 14 (12.73%) | 76 (10.31%) | 0.443 |
| Hypertension | 81 (73.64%) | 353 (47.90%) | <0.001 |
| diabetes | 18 (16.36%) | 83 (11.26%) | 0.124 |
| Hyperlipidemia | 24 (21.82%) | 141 (19.13%) | 0.507 |
| Coronary heart disease | 6 (5.45%) | 22 (2.99%) | 0.177 |
| Hunt-Hess grade (N, %) | <0.001 | ||
| Grade I–III | 63 (57.27%) | 638 (86.57%) | |
| Grade IV, V | 47 (42.73%) | 99 (13.43%) | |
| mFisher grade (N, %) | <0.001 | ||
| Grade 0–2 | 54 (49.09%) | 599 (81.28%) | |
| Grade 3–4 | 56 (50.91%) | 138 (18.72%) | |
| Aneurysm characteristics (N, %) | 0.767 | ||
| Anterior circulation | 85 (77.27%) | 560(75.98%) | |
| Posterior circulation | 25 (22.73%) | 177(24.02%) | |
| Time from onset to admission, mean (SD) h | 11.78 (6.205) | 13.01 (5.733) | 0.039 |
| Admission laboratory mean (SD) | |||
| Leukocyte,109/L | 12.835 (5.297) | 9.826 (4.194) | <0.001 |
| Hemoglobin, g/L | 131.91 (17.090) | 129.24 (17.319) | 0.131 |
| Serum potassium, mmol/L | 3.851 (0.469) | 3.915 (0.464) | 0.183 |
| Serum sodium, mmol/L | 140.999 (4.284) | 140.466 (4.645) | 0.258 |
| Serum calcium, mmol/L | 2.136 (0.196) | 2.171 (0.139) | 0.018 |
| Serum iron, µmol/L | 9.186 (5.726) | 13.425 (6.139) | <0.001 |
| Serum phosphorus, mmol/L | 0.842 (0.344) | 1.007 (0.347) | <0.001 |
| Treatment (N, %) | 0.278 | ||
| Clipping | 69 (62.73%) | 422 (57.26%) | |
| Coiling | 41 (37.27%) | 315 (42.74%) | |
| Characteristics | Univariable | Multivariable | ||
|---|---|---|---|---|
| Odds Ratio (95% CI) | p Value | Odds Ratio (95% CI) | p Value | |
| Hypertension (N, %) | 3.038 (1.941–4.756) | <0.001 | 2.130 (1.312–3.458) | 0.002 |
| Hunt-Hess grade (N, %) | 4.808 (3.118–7.413) | <0.001 | 1.528 (0.900–2.593) | 0.116 |
| mFisher grade (N, %) | 4.501 (2.966–6.831) | <0.001 | 2.292 (1.428–3.679) | <0.001 |
| Time from onset to admission, h | 0.965 (0.932–0.998) | 0.039 | 1.031 (0.994–1.069) | 0.099 |
| Leukocyte,109/L | 1.136 (1.090–1.183) | <0.001 | 0.951 (0.908–0.997) | 0.035 |
| Serum calcium, mmol/L | 0.187 (0.047–0.746) | 0.018 | 1.410 (0.306–6.499) | 0.659 |
| Serum iron, µmol/L | 0.875 (0.840–0.911) | <0.001 | 1.091 (1.043–1.141) | <0.001 |
| Serum phosphorus, mmol/L | 0.147 (0.071–0.304) | <0.001 | 1.860 (0.815–4.241) | 0.140 |
| After Propensity Score Matching | |||
|---|---|---|---|
| Characteristics | High-Grade Global Cerebral Edema | Low-Grade Global Cerebral Edema | p-Value |
| N = 103 | N = 103 | ||
| Age, mean (SD) y | 54.22 (11.893) | 55.83 (11.301) | 0.323 |
| Gender, female (N, %) | 57 (55.34%) | 62 (60.19%) | 0.481 |
| Medical history (N, %) | |||
| Smoking | 17 (16.50%) | 15 (14.56%) | 0.700 |
| Drinking | 14 (13.59%) | 8 (7.77%) | 0.176 |
| Hypertension | 76 (73.79%) | 74 (71.84%) | 0.754 |
| diabetes | 16 (15.53%) | 15 (14.56%) | 0.845 |
| Hyperlipidemia | 22 (21.36%) | 16 (15.53%) | 0.281 |
| Coronary heart disease | 6 (5.83%) | 2 (1.94%) | 0.149 |
| Hunt-Hess grade (N, %) | 0.886 | ||
| Grade I-III | 63 (61.17%) | 64 (62.14%) | |
| Grade IV, V | 40 (38.83%) | 39 (37.86%) | |
| mFisher grade (N, %) | 1.000 | ||
| Grade 0–2 | 54 (52.43%) | 54 (52.43%) | |
| Grade 3–4 | 49 (47.57%) | 49 (47.57%) | |
| Aneurysm characteristics (N, %) | 0.868 | ||
| Anterior circulation | 80 (77.67%) | 79 (76.70%) | |
| Posterior circulation | 23 (22.33%) | 24 (23.30%) | |
| Time from onset to admission, mean (SD) h | 11.93 (6.214) | 10.81 (6.326) | 0.199 |
| Admission laboratory mean (SD) | |||
| Leukocyte,109/L | 12.724 (5.344) | 13.123 (5.777) | 0.607 |
| Hemoglobin, g/L | 131.21 (17.255) | 130.86 (17.794) | 0.852 |
| Serum potassium, mmol/L | 3.864 (0.456) | 3.870 (0.460) | 0.920 |
| Serum sodium, mmol/L | 141.022 (4.322) | 140.571 (4.301) | 0.454 |
| Serum calcium, mmol/L | 2.144 (0.197) | 2.188 (0.119) | 0.560 |
| Serum iron, µmol/L | 9.358 (5.761) | 12.146 (6.258) | 0.001 |
| Serum phosphorus, mmol/L | 0.868 (0.339) | 0.912 (0.281) | 0.303 |
| Treatment (N, %) | 0.184 | ||
| Clipping | 64 (62.14%) | 73 (70.87%) | |
| Coiling | 39 (37.86%) | 30 (29.13%) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, H.; Zheng, S.; Zhang, Y.; Fan, W.; Xie, B.; Chen, F.; Lin, Y.; Kang, D. Lower Serum Iron Level Predicts Postoperative Global Cerebral Edema Following Aneurysmal Subarachnoid Hemorrhage. Brain Sci. 2023, 13, 1232. https://doi.org/10.3390/brainsci13091232
Wang H, Zheng S, Zhang Y, Fan W, Xie B, Chen F, Lin Y, Kang D. Lower Serum Iron Level Predicts Postoperative Global Cerebral Edema Following Aneurysmal Subarachnoid Hemorrhage. Brain Sciences. 2023; 13(9):1232. https://doi.org/10.3390/brainsci13091232
Chicago/Turabian StyleWang, Haojie, Shufa Zheng, Yibin Zhang, Wenjian Fan, Bingsen Xie, Fuxiang Chen, Yuanxiang Lin, and Dezhi Kang. 2023. "Lower Serum Iron Level Predicts Postoperative Global Cerebral Edema Following Aneurysmal Subarachnoid Hemorrhage" Brain Sciences 13, no. 9: 1232. https://doi.org/10.3390/brainsci13091232




