At the Crossroads between Eating Disorders and Body Dysmorphic Disorders—The Case of Bigorexia Nervosa
Abstract
:1. Introduction
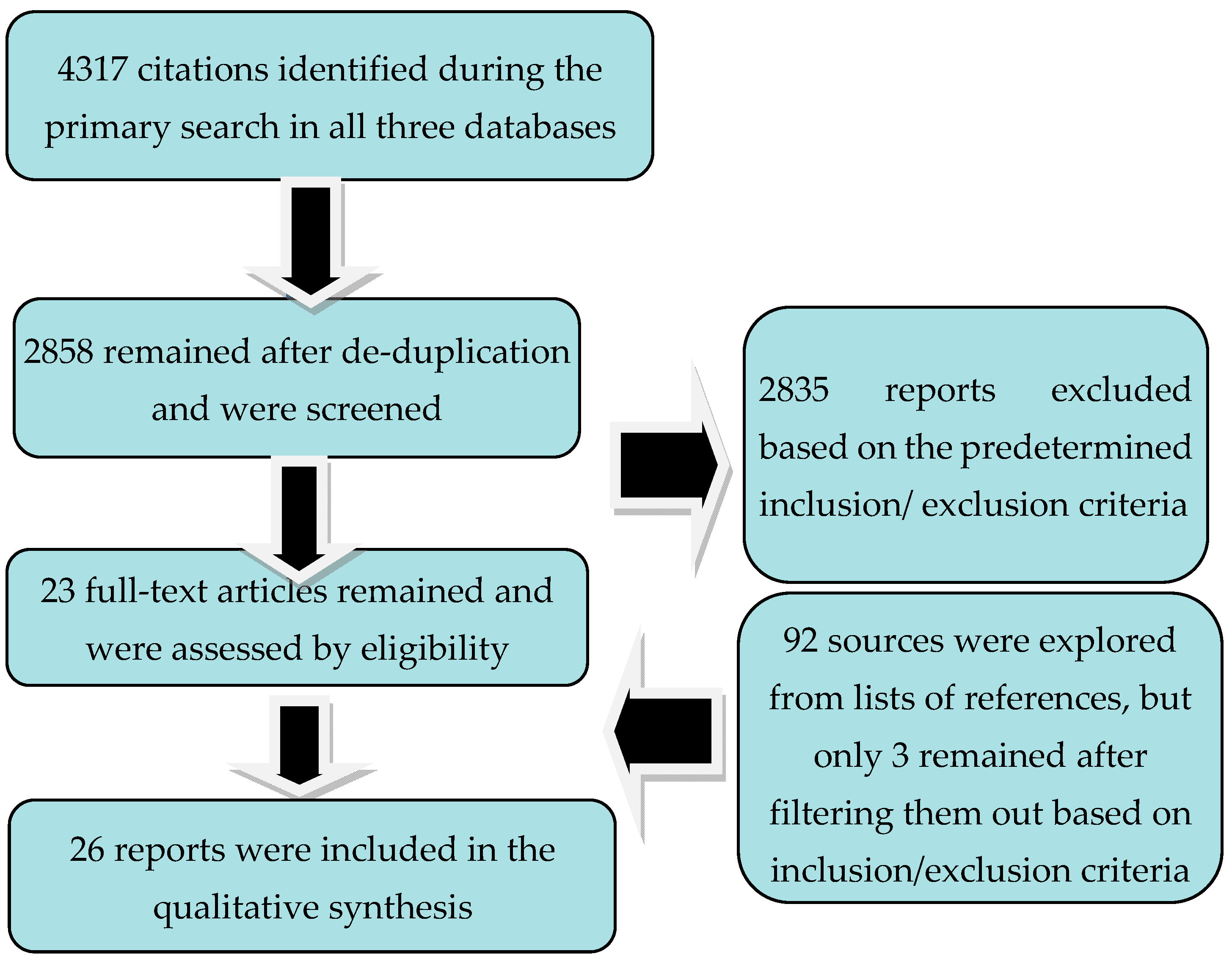
2. Objective and Methods
3. Results
3.1. Risk Factors, Pathophysiology, and Comorbid Conditions in Bigorexia Nervosa
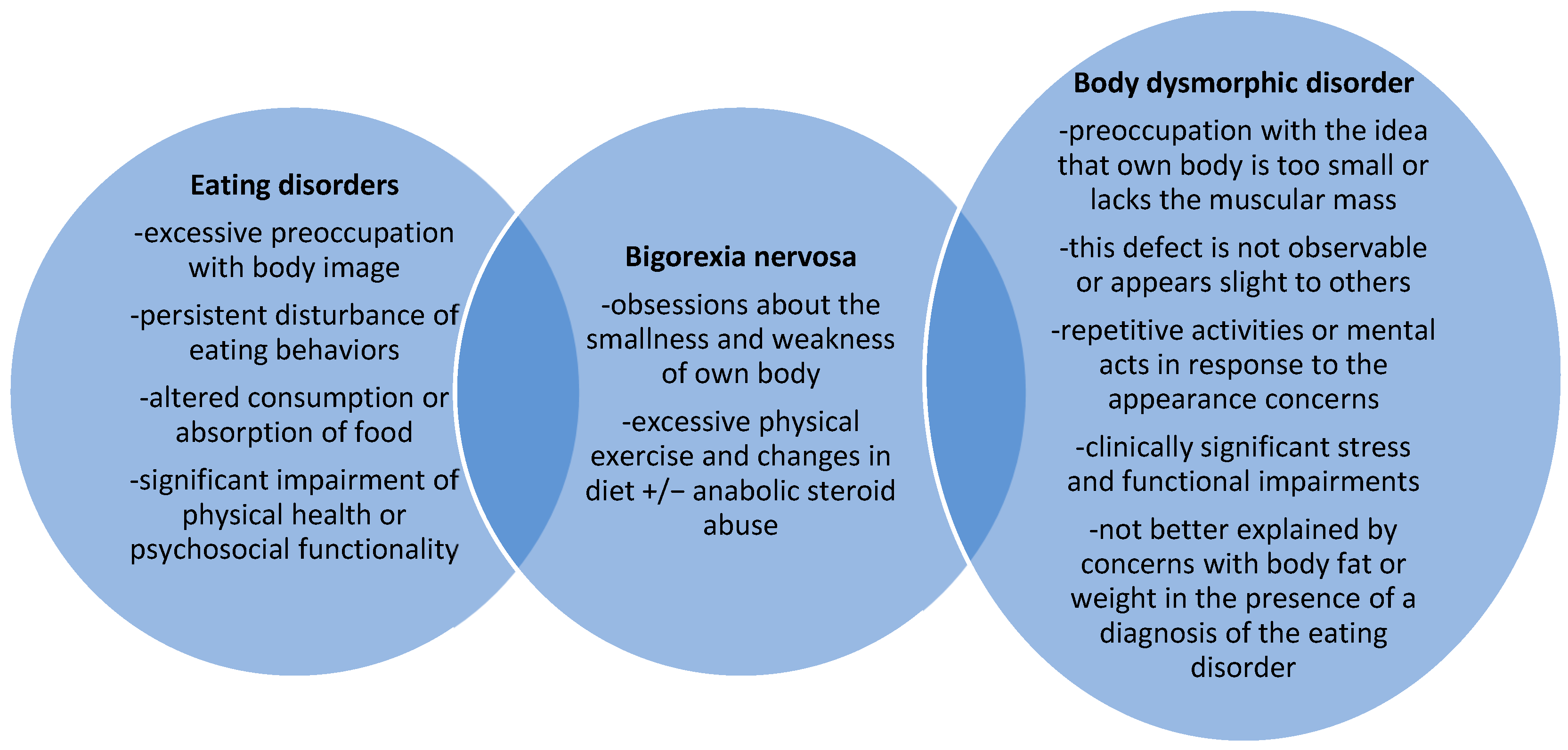
3.2. Positive and Differential Diagnosis
3.3. Epidemiology
3.4. Structured Evaluation
3.5. Available Treatments for Bigorexia Nervosa
4. Discussion
5. Conclusions
Funding
Data Availability Statement
Conflicts of Interest
References
- Fairburn, C.G.; Harrison, P.J. Eating disorders. Lancet 2003, 361, 407–416. [Google Scholar] [CrossRef] [PubMed]
- Treasure, J.; Duarte, T.A.; Schmidt, U. Eating disorders. Lancet 2020, 395, 899–911. [Google Scholar] [CrossRef]
- Berrettini, W. The genetics of eating disorders. Psychiatry 2004, 1, 18–25. [Google Scholar]
- Vander Wal, J.S.; Gibbons, J.L.; del Pilar Grazioso, M. The sociocultural model of eating disorder development: Application to a Guatemalan sample. Eat. Behav. 2008, 9, 277–284. [Google Scholar] [CrossRef] [PubMed]
- Izydorczyk, B.; Sitnik-Warchulska, K. Sociocultural appearance standards and risk factors for eating disorders in adolescents and women of various ages. Front. Psychol. 2018, 9, 429. [Google Scholar] [CrossRef]
- Bloch, M.H.; McGuire, J.; Landeros-Weisenberger, A.; Lechman, J.F.; Pittenger, C. Meta-analysis of the dose-response relationship of SSRI in obsessive-compulsive disorder. Mol. Psychiatry 2010, 15, 850–855. [Google Scholar] [CrossRef] [PubMed]
- Lutter, M. Emerging treatments in eating disorders. Neurotherapeutics 2017, 14, 614–622. [Google Scholar] [CrossRef]
- Birmingham, C.L.; Su, J.; Hlynsky, J.A.; Goldner, E.M.; Gao, M. The mortality rate from anorexia nervosa. Int. J. Eat. Disord. 2005, 38, 143–146. [Google Scholar] [CrossRef]
- Strother, E.; Lemberg, R.; Stanford, S.C.; Turbeville, D. Eating disorders in men: Underdiagnosed, undertreated, and misunderstood. Eat. Disord. 2012, 20, 346–355. [Google Scholar] [CrossRef]
- Carlat, D.J.; Camargo, C.A., Jr.; Herzog, D.B. Eating disorders in males: A report on 135 patients. Am. J. Psychiatry 1997, 154, 1127–1132. [Google Scholar] [CrossRef]
- Morgan, J. The Invisible Man: A Self-Help Guide for Men with Eating Disorders, Compulsive Exercise, and Bigorexia; Routledge: New York, NY, USA, 2008. [Google Scholar]
- Halliwell, E.; Dittmar, H.; Orsborn, A. The effects of exposure to muscular male models among men: Exploring the moderating role of gym use and exercise motivation. Body Image 2007, 4, 278–287. [Google Scholar] [CrossRef]
- Mosley, P.E. Bigorexia: Bodybuilding and muscle dysmorphia. Eur. Eat. Disord. Rev. 2009, 17, 191–198. [Google Scholar] [CrossRef] [PubMed]
- Pope, H.G., Jr.; Katz, D.L.; Hudson, J.I. Anorexia nervosa and „reverse anorexia” among 108 male bodybuilders. Compr. Psychiatry 1993, 34, 406–409. [Google Scholar] [CrossRef]
- Pope, H.G.; Phillips, K.A.; Olivardia, R. The Adonis Complex: How to Identify, Treat and Prevent Body Obsession in Men and Boys; Touchstone: New York, NY, USA, 2000. [Google Scholar]
- Pope, C.G.; Pope, H.G.; Menard, W.; Fay, C.; Olivardia, R.; Phillips, K.A. Clinical features of muscle dysmorphia among males with body dysmorphic disorder. Body Image 2005, 2, 395–400. [Google Scholar] [CrossRef]
- Murray, S.B.; Rieger, E.; Touyz, S.W.; De la Garza García, Y. Muscle dysmorphia and the DSM-V conundrum: Where does it belong? A review paper. Int. J. Eat. Disord. 2010, 43, 483–491. [Google Scholar] [CrossRef]
- Murray, S.B.; Rieger, E.; Hildebrandt, T.; Karlov, L.; Russell, J.; Boon, E.; Touyz, S.W. A comparison of eating, exercise, shape, and weight related symptomatology in males with muscle dysmorphia and anorexia nervosa. Body Image 2012, 9, 193–200. [Google Scholar] [CrossRef] [PubMed]
- Pope, H.G., Jr.; Gruber, A.J.; Choi, P.; Olivardia, R.; Phillips, K.A. Muscle dysmorphia. An underrecognized form of body dysmorphic disorder. Psychosomatics 1997, 38, 548–557. [Google Scholar] [CrossRef]
- Olivardia, R.; Pope, H.G., Jr.; Hudson, J.I. Muscle dysmorphia in male weightlifters: A case-control study. Am. J. Psychiatry 2000, 157, 1291–1296. [Google Scholar] [CrossRef]
- American Psychiatric Association. Feeding and Eating Disorders. In Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; Arlington, American Psychiatric Publishing: Arlington, VA, USA, 2022; Available online: https://dsm.psychiatryonline.org/doi/10.1176/appi.books.9780890425787.x10_Feeding_and_Eating_Disorder (accessed on 19 February 2023).
- World Health Organisation (WHO). ICD-11 Clinical Descriptions and Diagnostic Guidelines for Mental and Behavioral Disorders. 2019. Available online: https://icd.who.int/browse11/l-m/en (accessed on 12 February 2023).
- Rohman, L. The relationship between anabolic androgenic steroids and muscle dysmorphia: A review. Eat. Disord. 2009, 17, 187–199. [Google Scholar] [CrossRef] [PubMed]
- Kanayama, G.; Barry, S.; Hudson, J.I.; Pope, H.G., Jr. Body image and attitudes towards male roles in anabolic-androgenic steroid users. Am. J. Psychiatry 2006, 163, 697–703. [Google Scholar] [CrossRef]
- Cole, J.C.; Smith, R.; Halford, J.C.G.; Wagstaff, G.F. A preliminary investigation into the relationship between anabolic-androgenic steroid use and the symptoms of reverse anorexia in both current and ex-users. Psychopharmacology 2003, 166, 424–429. [Google Scholar] [CrossRef]
- Bo, S.; Zoccali, R.; Ponzo, V.; Soldati, L.; De Carli, L.; Benso, A.; Abbate-Daga, G. University courses, eating problems and muscle dysmorphia: Are there any associations? J. Transl. Med. 2014, 12, 221. [Google Scholar] [CrossRef]
- Foster, A.C.; Shorter, G.W.; Griffiths, M.D. Muscle dysmorphia: Could it be classified as an addiction to body image? J. Behav. Addict. 2015, 4, 1–5. [Google Scholar] [CrossRef]
- Cooper, M.; Eddy, K.T.; Thomas, J.J.; Franko, D.L.; Carron-Arthur, B.; Keshishian, A.C.; Griffiths, K.M. Muscle dysmorphia: A systematic and meta-analytic review of the literature to assess diagnostic validity. Int. J. Eat. Disord. 2020, 53, 1583–1604. [Google Scholar] [CrossRef]
- Matenstyn, J.A.; Touyz, S.; Maguire, S. Treatment of compulsive exercise in eating disorders and muscle dysmorphia: Protocol for a systematic review. J. Eat. Disord. 2021, 9, 19. [Google Scholar] [CrossRef] [PubMed]
- Dalle Grave, R. Features and management of compulsive exercising in eating disorders. Physician Sportsmed. 2015, 37, 20–28. [Google Scholar] [CrossRef]
- Noetel, M.; Dawson, L.; Hay, P.; Touyz, S. The assessment and treatment of unhealthy exercise in adolescents with anorexia nervosa: A Delphi study to synthesize clinical knowledge. Int. J. Eat. Disord. 2017, 50, 378–388. [Google Scholar] [CrossRef]
- dos Santo Filho, C.A.; Tirico, P.P.; Stefano, S.C.; Touyz, S.W.; Claudino, A.M. Systematic review of the diagnostic category muscle dysmorphia. Austr. N. Zeal. J. Psychiatry 2015, 50, 322–333. [Google Scholar] [CrossRef]
- Applewhite, B.; Olivola, M.; Tweed, C.; Wesemann, U.; Himmerich, H. Body dysmorphic disorder, muscle dysmorphia, weight and shape dissatisfaction and the use of appearance-enhancing drugs in the military: A systematic review. BMJ Mil. Health 2022, e002135. [Google Scholar] [CrossRef] [PubMed]
- McCreary, D.R.; Sasse, D.K. An exploration of the drive for muscularity in adolescent boys and girls. J. Am. Coll. Health. 2000, 48, 297–304. [Google Scholar] [CrossRef] [PubMed]
- Hildebrandt, T.; Walker, D.C.; Alfano, L.; Delinsky, S.; Bannon, K. Development and validation of a male specific Body Checking Questionnaire. Int. J. Eat. Disord. 2010, 43, 77–87. [Google Scholar] [CrossRef]
- Hildebrandt, T.; Langenbucher, J.; Schlundt, D.G. Muscularity concerns among men: Development of attitudinal and perceptual measures. Body Image 2004, 1, 169–181. [Google Scholar] [CrossRef]
- Cunningham, M.L.; Griffiths, S.; Mitchison, D.; Mond, J.M.; Castle, D.; Murray, S.B. Muscle dysmorphia: An overview of clinical features and treatment options. J. Cogn. Psychother. 2017, 31, 255–271. [Google Scholar] [CrossRef] [PubMed]
- Perelman, H.; Schwartz, N.; Yeoward-Dodson, J.; Quiñones, I.C.; Murray, M.F.; Dougherty, E.N.; Townsel, R.; Arthur-Cameselle, J.; Haedt-Matt, A.A. Reducing eating disorder risk among male athletes: A randomized controlled trial investigating the male athlete body project. Int. J. Eat. Disord. 2022, 55, 193–206. [Google Scholar] [CrossRef]
- Linardon, J.; Wade, T.D.; de la Piedad Garcia, X.; Brennan, L. The efficacy of cognitive-behavioral therapy for eating disorders: A systematic review and meta-analysis. J. Consult. Clin. Psychol. 2017, 85, 1080–1094. [Google Scholar] [CrossRef]
- Galsworthy-Francis, L.; Allan, S. Cognitive behavioral therapy for anorexia nervosa: A systematic review. Clin. Psychol. Rev. 2014, 34, 54–72. [Google Scholar] [CrossRef] [PubMed]
- Murray, S.B.; Griffiths, S. Adolescent muscle dysmorphia and family-based treatment: A case report. Clin. Child. Psychol. Psychiatry 2015, 20, 324–330. [Google Scholar] [CrossRef]
- Vasiliu, O. Therapeutic management of buying/shopping disorder: A systematic literature review and evidence-based recommendations. Front. Psychiatry 2022, 13, 1047280. [Google Scholar] [CrossRef]
- Budisteanu, M.; Andrei, E.; Lica, F.; Hulea, D.S.; Velicu, A.C.; Mihailescu, I.; Rad, F. Predictive factors in early onset schizophrenia. Exp. Ther. Med. 2020, 20, 210. [Google Scholar] [CrossRef]
- Sîrbu, C.A.; Manole, A.M.; Vasile, M.; Toma, G.S.; Dobrican, L.R.; Vîrvara, D.G.; Vasiliu, O. Cannabinoids- a new therapeutic strategy in neurology. RJMM 2022, 125, 349–355. [Google Scholar] [CrossRef]
- Vasiliu, O.; Vasile, D.; Mangalagiu, A.G.; Petrescu, M.B.; Candea, C.A.; Tudor, C.; Ungureanu, D.; Miclos, M.; Draghici, A.; Florescu, C.; et al. Current treatment of posttraumatic stress disorder—A review of therapeutic guidelines and good practice recommendations. RJMM. 2020, 123, 241–248. [Google Scholar] [CrossRef]
- Hasin, D.S.; O’brien, C.P.; Auriacombe, M.; Borges, G.; Bucholz, K.; Budney, A.; Compton, W.M.; Crowley, T.; Ling, W.; Petry, N.M.; et al. DSM-5 criteria for substance use disorders: Recommendations and rationale. Am. J. Psychiatry 2013, 170, 834–851. [Google Scholar] [CrossRef]
- Issari, Y.; Jakubovski, E.; Bartley, C.A.; Pittenger, C.; Bloch, M.H. Early onset of response with selective serotonin reuptake inhibitors in obsessive-compulsive disorder: A meta-analysis. J. Clin. Psychiatry 2016, 77, e605-11. [Google Scholar] [CrossRef] [PubMed]
- Marvanova, M.; Gramith, K. Role of antidepressants in the treatment of adults with anorexia nervosa. Ment. Health Clin. 2018, 8, 127–137. [Google Scholar] [CrossRef]
- Holtkamp, K.; Konrad, K.; Kaiser, N.; Ploenes, Y.; Heussen, N.; Grzella, I.; Herpertz-Dahlmann, B. A retrospective study of SSRI treatment in adolescent anorexia nervosa: Insufficient evidence for efficacy. J. Psychiatr. Res. 2005, 39, 303–310. [Google Scholar] [CrossRef] [PubMed]
- Petrescu, B.; Vasile, D.; Vasiliu, O.; Tudor, C.; Mangalagiu, A.; Ungureanu, D. SSRI dose escalation versus duloxetine in treatment of major depressive disorder not responding to initial SSRI. Eur. Neuropsychopharmacol. 2014, 24, S455–S456. [Google Scholar] [CrossRef]
- Emsley, R.; Ahokas, A.; Suarez, A.; Marinescu, D.; Dóci, I.; Lehtmets, A.; Milanova, V.; Lee, M.S.; Didi, R.; Araszkiewicz, A.; et al. Efficacy of tianeptine 25–50 mg in elderly patients with recurrent major depressive disorder: An 8-week placebo- and escitalopram-controlled study. J. Clin. Psychiatry 2018, 79, 17m11741. [Google Scholar] [CrossRef]
- Phillips, K.A. Pharmacotherapy for body dysmorphic disorder. Psychiatr. Ann. 2010, 40, 325–332. [Google Scholar] [CrossRef] [PubMed]
- Ganann, R.; Ciliska, D.; Thomas, H. Expediting systematic reviews: Methods and implications of rapid reviews. Implement. Sci. 2010, 5, 56. [Google Scholar] [CrossRef]
- Rathbone, J.; Albarqouni, L.; Bakhit, M.; Beller, E.; Byambasuren, O.; Hoffmann, T.; Scott, A.M.; Glasziou, P. Expediting citation screening using PICo-based title-only screening for identifying studies in scoping searches and rapid reviews. Syst. Rev. 2017, 6, 233. [Google Scholar] [CrossRef]
- Saracci, C.; Mahamat, M.; Jacquérioz, F. How to write a narrative literature review article? Rev. Med. Suisse 2019, 15, 1694–1698. [Google Scholar] [PubMed]
| Operational Criteria | Inclusion Criteria | Exclusion Criteria |
|---|---|---|
| Population | All age groups were allowed. The diagnoses explored were “bigorexia (nervosa)”, “muscle dysmorphia”, or “reverse anorexia”. Diagnoses made according to the DSM or ICD nosographic systems (no limitations regarding the edition) were permitted, but also original criteria constructed by authors of the respective reports. | Unspecified diagnoses or reports that included various EDs or BDDs without clarifying what criteria were used during the research. |
| Intervention | Any type of study, such as clinical or preclinical research, epidemiological or clinical, prospective or retrospective, etc. Any type of review, such as systematic, narrative, scoping, meta-analysis, umbrella review, etc. | Studies with undetermined methodology and reviews with unspecified design. |
| Environment | Inpatient, outpatient, daycare, and general population. | Unspecified environment. |
| Primary and secondary variables | Prevalence, incidence, risk factors, clinical diagnosis, pathophysiological data, psychological evaluation, and treatment. | Imprecisely defined or poorly characterized variables and reports without pre-defined outcomes. |
| Study design | Primary and secondary reports, clinical and preclinical research. | Unspecified or insufficiently defined designs. |
| Language | Any language of publication was admitted if the in extenso version of the paper could be retrieved. |
| Reference | Type of Paper | Main Outcomes | Results and Observations |
|---|---|---|---|
| [13] | CR, a male practicing BB | Pathophysiological considerations about BN, bodybuilding as a predisposing factor to BN, analysis of BN as a type of ED | Psychological vulnerability for BN—a young man reports experiencing concerns about his appearance or muscularity. Predisposing factors—physical exercise motivated primarily by the need to improve one’s own physical aspect. |
| [14] | A case–control study (AAS-abusing males practicing BB vs. non-AAS-abusing males practicing BB), N = 108 participants | SCID-III-based evaluation for detection of AN, Bn, BN + medical history, family history of psychiatric disorders and violent behavior + physical examination | BB is a risk factor for BN and AN. BN may precipitate or perpetuate AAS use in vulnerable individuals. |
| [16] | Retrospective, case–control study (BDD + BN vs. BDD without BN), N = 63 patients | The detection of characteristics in patients with BDD + BN at the clinical level | Demographic variables, BDD severity, delusionality, and number of non-muscle-related body parts of concern were similar between the two groups. Attempted suicide, poorer quality of life, and higher rates of SUDs and AAS abuse were more frequent in the BN + BDD group. |
| [19] | NR + CR (four patients—two male and two female) | Diagnostic features, differential diagnosis, epidemiology, and etiology | Tentative diagnosis criteria are suggested, and case reports are presented. |
| [20] | A case–control study (men with BN vs. healthy weightlifters), N = 54 participants | Demographic, psychiatric, and physical measures | BN was associated with body dissatisfaction, dysfunctional eating attitudes, higher prevalence of AAS use, and higher lifetime prevalence of mood disorders, anxiety disorders, and ED vs. controls. |
| [21] | Nosological classification | Diagnostic and epidemiological data on muscle dysmorphia | BN is a subtype of BDD, and it is included in the OCD spectrum. Specific diagnostic criteria were formulated. |
| [22] | Nosological classification | Diagnostic data on muscle dysmorphia | BN is a form of BDD. |
| [23] | NR | Relationship between AAS use and BN | AAS use is considered secondary to the need to compensate body image pathology, BN included. AAS use is frequently detected in patients with BN; therefore, this SUD is a part of the diagnostic criteria for BN. |
| [24] | A case–control study (AAS users vs. non-users), N = 89 male weightlifter participants | Relationship between AAS use and body image distortions and attitudes toward male roles | Body image pathology and rigid stereotypic views on masculinity are prominent in men with long-term AAS use. However, the causality is still uncertain. |
| [25] | A case–control study included current, ex-, and non-AAS BB, N = 137 male participants who practiced regular aerobic exercises | Relationship between AAS use and reverse anorexia | AAS users had an ideal image of an exaggerated mesomorphic body shape. Current and ex-AAS users had higher scores on eating behavior pathology vs. non-AAS users. AAS use, but not BB as an independent variable, was associated with higher severity of BN. |
| [26] | A case–control study (students in Dietetics/Exercise and Sport Sciences vs. Biology), N = 440 participants | Prevalence of orthorexia and BN in students following courses on nutrition and body care vs. those following Biology classes | The selection of the university courses may be, at least partially, under the influence of eating behavior pathology. |
| [27] | NR | Exploration of an alternative model for BN—”the addiction to body ideal” paradigm | Maintaining a body image through bodybuilding, exercise, eating behaviors, AAS use, etc., is addictive; therefore, BN may be considered a behavioral addiction. |
| [28] | SR and MTA (n = 40 papers) | Clinical diagnosis of BN | Using cluster analysis, two distinct patterns of BN were identified—the cognitive type and the behavioral variant. The data analyzed did not prove to be sufficient for determining if BN is a specifier for BDD or a unique psychiatric disorder. |
| [29] | SR protocol | Exploration of compulsive exercise in EDs and BN | Not yet disclosed. |
| [30] | NR | Exploration of compulsive exercising in EDs, especially restrictive type AN | Compulsive exercising is a negative prognosis factor in EDs, and it is associated with higher ED psychopathology, dietary restraint, general psychopathology, and personality features (perfectionism, persistence, and lower novelty seeking). Enhanced CBT may be useful for hospitalized patients with this pathology. |
| [31] | Delphi study (N = 25 participants, experts in AN treatment) | Exploration of unhealthy exercise in adolescents with AN | Exercise restriction practices and initiating healthy exercise behaviors in patients who are medically stable. |
| [32] | SR (n = 34 papers) | Clinical criteria for diagnosing BN | There is insufficient data to support the validity, clinical utility, nosological classification, and inclusion of BN as a new disorder in the nosological systems of mental disorders. |
| [33] | SR (n = 20 papers) | Analysis of BDD, BN, weight and shape dissatisfaction, and the use of AAS in military personnel | BDD, BN, and AAS use are highly prevalent in military personnel. A preliminary tendency toward overvaluation of physical appearance and fitness may influence the decision to choose a military career. |
| [34] | Validation study for a psychological instrument | Creating and validating a psychometric tool to determine the severity of BN manifestations | A 15-item survey was administered to 197 adolescents, and the drive for muscularity displayed good reliability. This drive was related to lower self-esteem and a higher level of depression in boys, but not in girls. |
| [35] | Validation study for a psychological instrument | Convergent and divergent validity, factor structure, and reliability of a psychometric tool for BN | A 19-item, four-factor instrument was supported by analysis + a higher-order global checking factor for men only. Good concurrent and divergent validity and good short-term test–retest reliability. |
| [36] | Validation study for a psychological instrument | Psychometric properties of a new instrument for quantifying BN severity | A 13-item questionnaire with two subscales had good reliability, convergent and divergent validity, and test–retest validity. |
| [37] | NR | Overview of clinical features and treatment options for BN | Techniques applied with success for treating BDDs and EDs can be intuitively used for patients with BN. Cognitive restructuring of perfectionistic and egosyntonic beliefs and also DBT techniques may prove useful. |
| [38] | A case–control study (psychotherapy vs. assessment-only), N = 79 male participants | The effects of a psychotherapeutic, structured intervention (3-session group Male Athlete Body Project) in collegiate athletes with EDs | Satisfaction with specific body parts increased, and the drive for muscularity and body-ideal internalization decreased at post-treatment evaluation vs. controls. The results were preserved at the 1-month follow-up visit. Reductions in AAS use were also observed. |
| [39] | MTA (n = 72 trials) | Efficacy of CBT for EDs | CBT is efficacious for patients with EDs, and it outperformed all active psychological comparisons and ITP, specifically. Many trials were of poor quality. |
| [40] | SR (n = 16 articles) | Efficacy of CBT for AN | CBT improved treatment adherence and reduced the dropout risk in patients with AN. CBT was not significantly superior to dietary counseling, supportive management, ITP, or behavioral family therapy. |
| [41] | CR, a 15-year-old boy | The effects of family-based treatment for BN | This intervention may be efficient. MDDI score decreased significantly at the post-treatment visit vs. baseline. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vasiliu, O. At the Crossroads between Eating Disorders and Body Dysmorphic Disorders—The Case of Bigorexia Nervosa. Brain Sci. 2023, 13, 1234. https://doi.org/10.3390/brainsci13091234
Vasiliu O. At the Crossroads between Eating Disorders and Body Dysmorphic Disorders—The Case of Bigorexia Nervosa. Brain Sciences. 2023; 13(9):1234. https://doi.org/10.3390/brainsci13091234
Chicago/Turabian StyleVasiliu, Octavian. 2023. "At the Crossroads between Eating Disorders and Body Dysmorphic Disorders—The Case of Bigorexia Nervosa" Brain Sciences 13, no. 9: 1234. https://doi.org/10.3390/brainsci13091234





