Update on How to Approach a Patient with Locked-In Syndrome and Their Communication Ability
Abstract
1. Introduction
2. Materials and Methods
Data Reporting
3. Establishing Communication
3.1. Overview of Solutions for Communication
3.2. Brain–Computer Interface (BCI)
Overview
3.3. Non-Invasive BCIs
3.3.1. Communication through Blinking
3.3.2. Electroencephalography (EEG)
3.3.3. Emerging Technologies
Functional Near-Infrared Spectroscopy
Functional Magnetic Resonance Imaging
Magnetoencephalography
P300
Summary of Risks and Benefits of Non-Invasive BCIs
3.4. Invasive
3.4.1. Electrocorticography
ECOG Point and Click Communication
3.4.2. Intracortical
Summary of Risks and Benefits of Invasive BCI’s
4. Limitations: Affordability, Usability, Access, Grants, Insurance, Social Worker
5. Caregiver Burden
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Kohnen, R.F.; Lavrijsen, J.C.M.; Bor, J.H.J.; Koopmans, R.T.C.M. The prevalence and characteristics of patients with classic locked-in syndrome in Dutch nursing homes. J. Neurol. 2013, 260, 1527–1534. [Google Scholar] [CrossRef] [PubMed]
- M Das, J.; Anosike, K.; Asuncion, R.M.D. Locked-in Syndrome. In StatPearls; Statpearls Publishing: Treasure Island, FL, USA, 2023. Available online: http://www.ncbi.nlm.nih.gov/books/NBK559026/ (accessed on 6 November 2023).
- Farr, E.; Altonji, K.; Harvey, R.L. Locked-In Syndrome: Practical Rehabilitation Management. PMR 2021, 13, 1418–1428. [Google Scholar] [CrossRef]
- Rousseau, M.-C.; Baumstarck, K.; Alessandrini, M.; Blandin, V.; Billette de Villemeur, T.; Auquier, P. Quality of life in patients with locked-in syndrome: Evolution over a 6-year period. Orphanet J. Rare Dis. 2015, 10, 88. [Google Scholar] [CrossRef] [PubMed]
- Corallo, F.; Bonanno, L.; Buono, V.L.; De Salvo, S.; Rifici, C.; Pollicino, P.; Allone, C.; Palmeri, R.; Todaro, A.; Alagna, A.; et al. Augmentative and Alternative Communication Effects on Quality of Life in Patients with Locked-in Syndrome and Their Caregivers. J. Stroke Cerebrovasc. Dis. 2017, 26, 1929–1933. [Google Scholar] [CrossRef] [PubMed]
- Elsahar, Y.; Hu, S.; Bouazza-Marouf, K.; Kerr, D.; Mansor, A. Augmentative and Alternative Communication (AAC) Advances: A Review of Configurations for Individuals with a Speech Disability. Sensors 2019, 19, 1911. [Google Scholar] [CrossRef] [PubMed]
- Vansteensel, M.J.; Jarosiewicz, B. Brain-computer interfaces for communication. In Handbook of Clinical Neurology; Elsevier: Amsterdam, The Netherlands, 2020; Volume 168, pp. 67–85. [Google Scholar] [CrossRef]
- Ezzat, M.; Maged, M.; Gamal, Y.; Adel, M.; Alrahmawy, M.; El-Metwally, S. Blink-To-Live eye-based communication system for users with speech impairments. Sci. Rep. 2023, 13, 7961. [Google Scholar] [CrossRef] [PubMed]
- Brumberg, J.S.; Pitt, K.M.; Mantie-Kozlowski, A.; Burnison, J.D. Brain–Computer Interfaces for Augmentative and Alternative Communication: A Tutorial. Am. J. Speech-Lang. Pathol. 2018, 27, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Luo, S.; Rabbani, Q.; Crone, N.E. Brain-Computer Interface: Applications to Speech Decoding and Synthesis to Augment Communication. Neurotherapeutics 2022, 19, 263–273. [Google Scholar] [CrossRef] [PubMed]
- Vansteensel, M.J.; Branco, M.P.; Leinders, S.; Freudenburg, Z.F.; Schippers, A.; Geukes, S.H.; Gaytant, M.A.; Gosselaar, P.H.; Aarnoutse, E.J.; Ramsey, N.F. Methodological Recommendations for Studies on the Daily Life Implementation of Implantable Communication-Brain–Computer Interfaces for Individuals with Locked-in Syndrome. Neurorehabilit. Neural Repair 2022, 36, 666–677. [Google Scholar] [CrossRef] [PubMed]
- Kopsky, D.J.; Winninghoff, Y.; Winninghoff, A.C.M.; Stolwijk-Swüste, J.M. A novel spelling system for locked-in syndrome patients using only eye contact. Disabil. Rehabil. 2014, 36, 1723–1727. [Google Scholar] [CrossRef] [PubMed]
- Park, S.-W.; Yim, Y.-L.; Yi, S.-H.; Kim, H.-Y.; Jung, S.-M. Augmentative and Alternative Communication Training Using Eye Blink Switch for Locked-in Syndrome Patient. Ann. Rehabil. Med. 2012, 36, 268–272. [Google Scholar] [CrossRef] [PubMed]
- Butler, L.K.; Kiran, S.; Tager-Flusberg, H. Functional Near-Infrared Spectroscopy in the Study of Speech and Language Impairment Across the Life Span: A Systematic Review. Am. J. Speech-Lang. Pathol. 2020, 29, 1674–1701. [Google Scholar] [CrossRef]
- Lugo, Z.R.; Quitadamo, L.R.; Bianchi, L.; Pellas, F.; Veser, S.; Lesenfants, D.; Real, R.G.L.; Herbert, C.; Guger, C.; Kotchoubey, B.; et al. Cognitive Processing in Non-Communicative Patients: What Can Event-Related Potentials Tell Us? Front. Hum. Neurosci. 2016, 10, 569. [Google Scholar] [CrossRef] [PubMed]
- Vansteensel, M.J.; Pels, E.G.M.; Bleichner, M.G.; Branco, M.P.; Denison, T.; Freudenburg, Z.V.; Gosselaar, P.; Leinders, S.; Ottens, T.H.; Boom, M.A.V.D.; et al. Fully Implanted Brain–Computer Interface in a Locked-In Patient with ALS. N. Engl. J. Med. 2016, 375, 2060–2066. [Google Scholar] [CrossRef] [PubMed]
- Bacher, D.; Jarosiewicz, B.; Masse, N.Y.; Stavisky, S.D.; Simeral, J.D.; Newell, K.; Oakley, E.M.; Cash, S.S.; Friehs, G.; Hochberg, L.R. Neural Point-and-Click Communication by a Person With Incomplete Locked-In Syndrome. Neurorehabilit. Neural Repair 2015, 29, 462–471. [Google Scholar] [CrossRef]
- Homer, M.L.; Nurmikko, A.V.; Donoghue, J.P.; Hochberg, L.R. Sensors and Decoding for Intracortical Brain Computer Interfaces. Annu. Rev. Biomed. Eng. 2013, 15, 383–405. [Google Scholar] [CrossRef] [PubMed]
- Elliott, C.; Sutherland, D.; Gerhard, D.; Theys, C. An Evaluation of the P300 Brain–Computer Interface, EyeLink Board, and Eye-Tracking Camera as Augmentative and Alternative Communication Devices. J. Speech Lang. Hear. Res. 2022, 65, 4280–4290. [Google Scholar] [CrossRef]
- Pitt, K.M.; Brumberg, J.S. Evaluating person-centered factors associated with brain–computer interface access to a commercial augmentative and alternative communication paradigm. Assist. Technol. 2022, 34, 468–477. [Google Scholar] [CrossRef] [PubMed]
- Pitt, K.M.; Brumberg, J.S.; Pitt, A.R. Considering Augmentative and Alternative Communication Research for Brain-Computer Interface Practice. Assist. Technol. Outcomes Benefits 2019, 13, 1–20. [Google Scholar]
- Zinkevich, A.; Uthoff, S.A.K.; Wirtz, M.A.; Boenisch, J.; Sachse, S.K.; Bernasconi, T.; Feldhaus, M.; Ansmann, L. Burden of informal caregivers of people without natural speech: A mixed-methods intervention study. BMC Health Serv. Res. 2022, 22, 1549. [Google Scholar] [CrossRef]
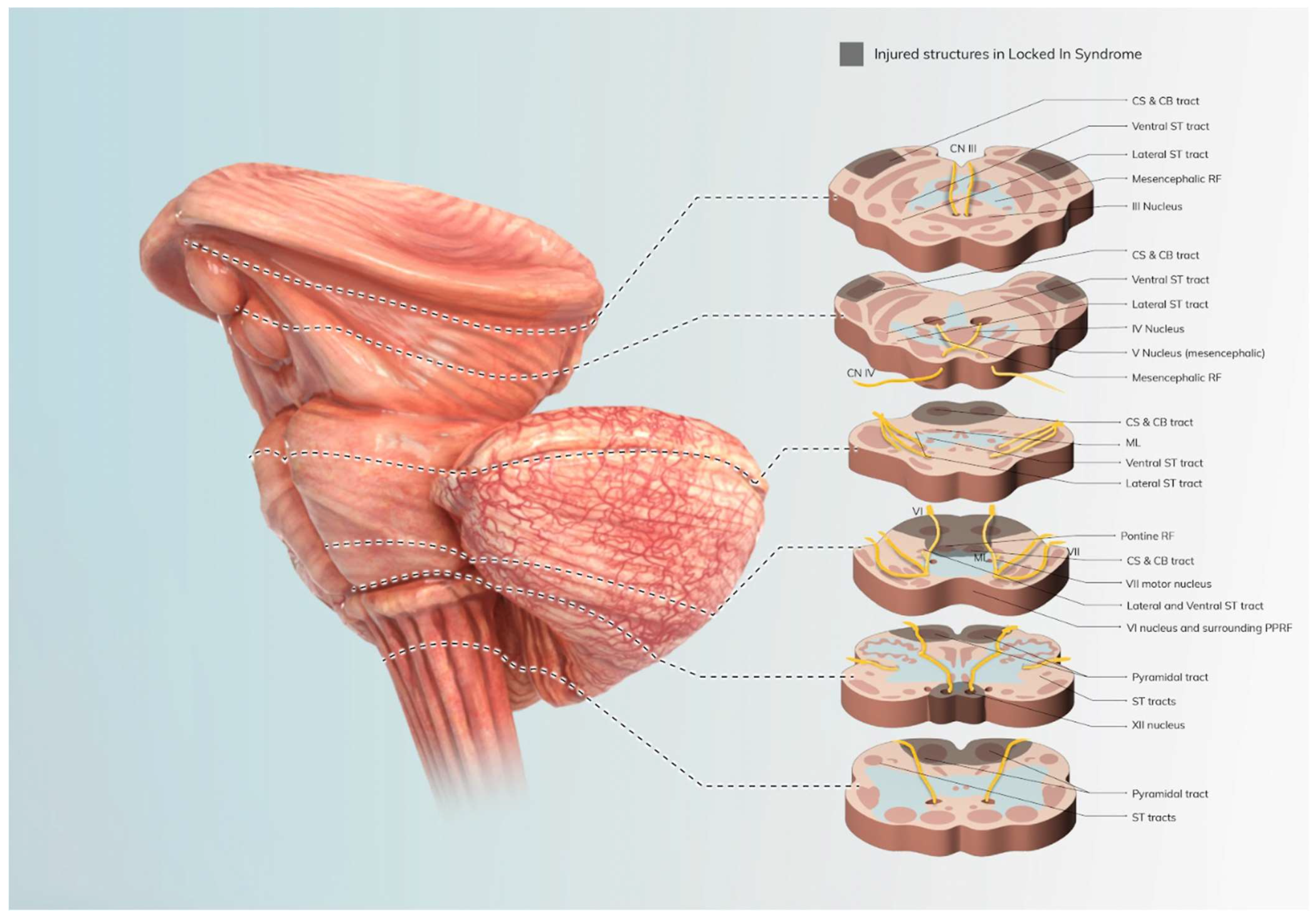



| Structure (s) | Function | Status in Classical LIS |
|---|---|---|
| CN 3, 4 | Vertical eye movement, pupillary reflex, eyelid control data | Intact |
| CN 6, paramedian pontine reticular formation | Bilateral horizontal gaze | Injured |
| Corticobulbar tracts (CN 5, 7, 9, 10, 11, 12) | Respiratory function | Variable |
| Corticospinal tracts | Limb and truncal motor functions | Injured |
| Medial lemniscus and spinothalamic pathways | Sensation | Intact |
| Reticular activating system | Arousal, consciousness, awareness | Intact |
| Reference | Communication Involved |
|---|---|
| Kopsky et al. (2014) (Disabil Rehabil, 36(20), 1723–1727, doi:10.3109/09638288.2013.866700) [12]. | Through utilizing the maintained eye movement in LIS, a specialized spelling system was tried to see if it helped make communication with blinking more user-friendly. |
| Park et al. (2012) (Ann Rehabil Med, 36(2), 268–272, doi:10.5535/arm.2012.36.2.268) [13]. | After eye blinking therapy (AAC), there was a benefit seen in patients’ communication ability. |
| Luo et al. (2022) (Neurother J Am Soc Exp Neurother, 19(1), 263–273, doi:10.1007/s13311-022-01190-2) [10]. | With the use of EEG, brain activity was able to be tracked before and during communication to see the areas most involved. |
| Vansteensel et al. (2022) (Neurorehabil Neural Repair, 36(10–11), 666–677, doi:10.1177/15459683221125788) [11]. | fNRI and fMRI are both emerging technologies in the area of communication, but the one downside is implanting them in daily life. They allow for the tracking and amplification of neural signals. |
| Butler et al. (2020) (Am J Speech Lang Pathol, 29(3), 1674–1701, doi:10.1044/2020_AJSLP-19-00050) [14]. | fNRI may not only help with augmenting communication but also show promise in assisting with diagnosing communication ability. |
| Lugo et al. (2016) (Front Hum Neurosci, 10, 569, doi:10.3389/fnhum.2016.00569) [15] | P300 allows for better diagnosis in baseline communication ability for patients with LIS while looking at event potentials when presented with a task or stimuli. |
| Reference | Communication Involved |
|---|---|
| Bacher et al. (2015) (Neurorehabil Neural Repair, 29(5), 462–471, doi:10.1177/1545968314554624) [17]. | In the clinical trial of the BrainGate Neural Interface System, this system, featuring the BrainGate Radial Keyboard, was compared to a standard QWERTY keyboard. The results showed a significant improvement in communication ability. The participant effectively used this interface for face-to-face communication with research staff through text-to-speech conversion and remote communication via an internet chat application. |
| Homer et al. (2013) (Annu Rev Biomed Eng, 15, 383–405, doi:10.1146/annurev-bioeng-071910-124640) [18]. | Central components of intracortical BCIs include implanted sensors capturing neural signals and the decoding software extracting the user’s intended movements from these signals. These innovations can enhance the technology’s capacity, precision, and durability. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Voity, K.; Lopez, T.; Chan, J.P.; Greenwald, B.D. Update on How to Approach a Patient with Locked-In Syndrome and Their Communication Ability. Brain Sci. 2024, 14, 92. https://doi.org/10.3390/brainsci14010092
Voity K, Lopez T, Chan JP, Greenwald BD. Update on How to Approach a Patient with Locked-In Syndrome and Their Communication Ability. Brain Sciences. 2024; 14(1):92. https://doi.org/10.3390/brainsci14010092
Chicago/Turabian StyleVoity, Kaitlyn, Tara Lopez, Jessie P. Chan, and Brian D. Greenwald. 2024. "Update on How to Approach a Patient with Locked-In Syndrome and Their Communication Ability" Brain Sciences 14, no. 1: 92. https://doi.org/10.3390/brainsci14010092
APA StyleVoity, K., Lopez, T., Chan, J. P., & Greenwald, B. D. (2024). Update on How to Approach a Patient with Locked-In Syndrome and Their Communication Ability. Brain Sciences, 14(1), 92. https://doi.org/10.3390/brainsci14010092





