Association Between Glaucoma and Brain Structural Connectivity Based on Diffusion Tensor Tractography: A Bidirectional Mendelian Randomization Study
Abstract
:1. Introduction
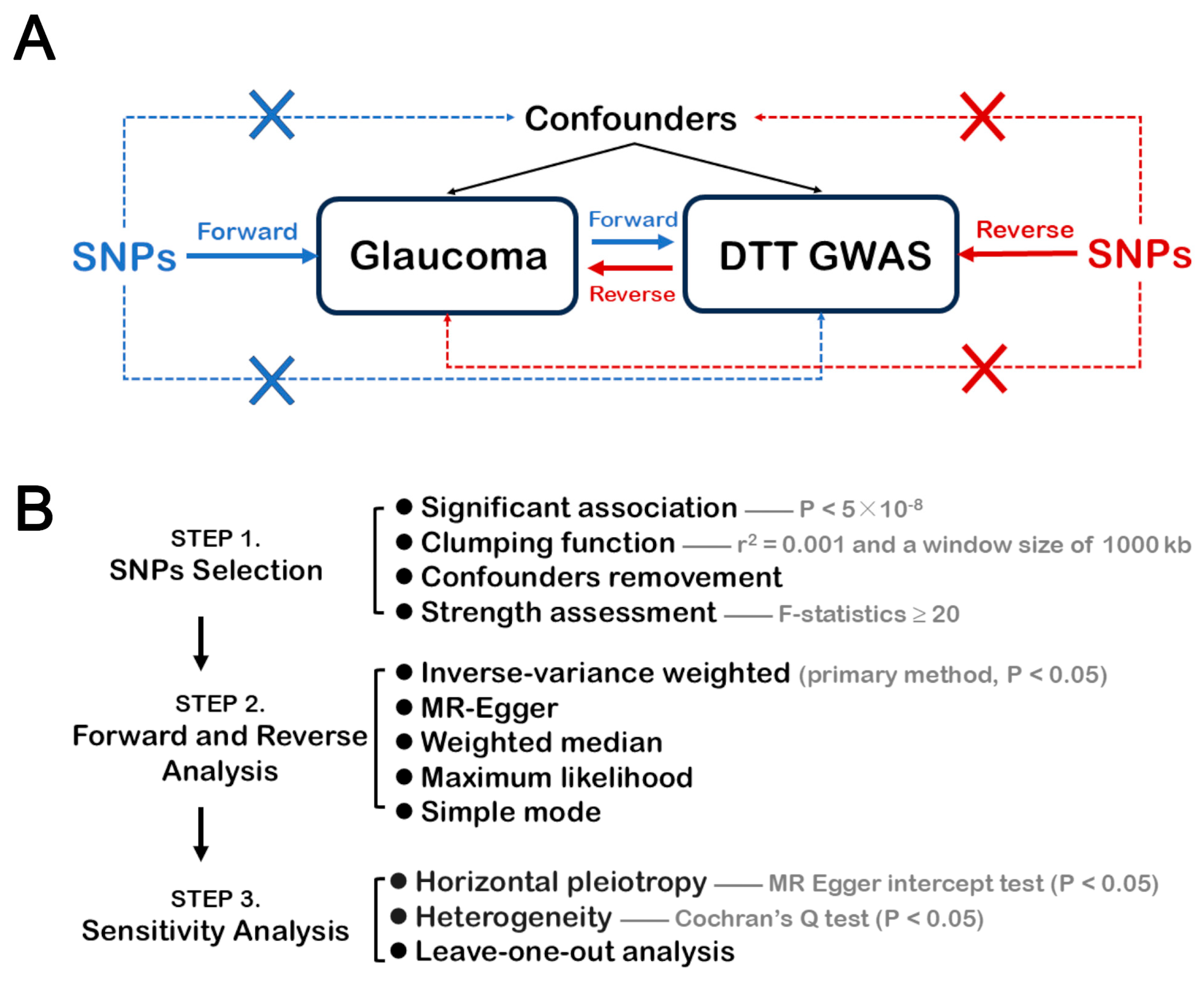
2. Materials and Methods
2.1. GWAS Data and Design of This Study
2.2. Selection of SNPs
2.3. Statistical Analysis
3. Results
3.1. Study Overview
3.2. Forward MR Analysis
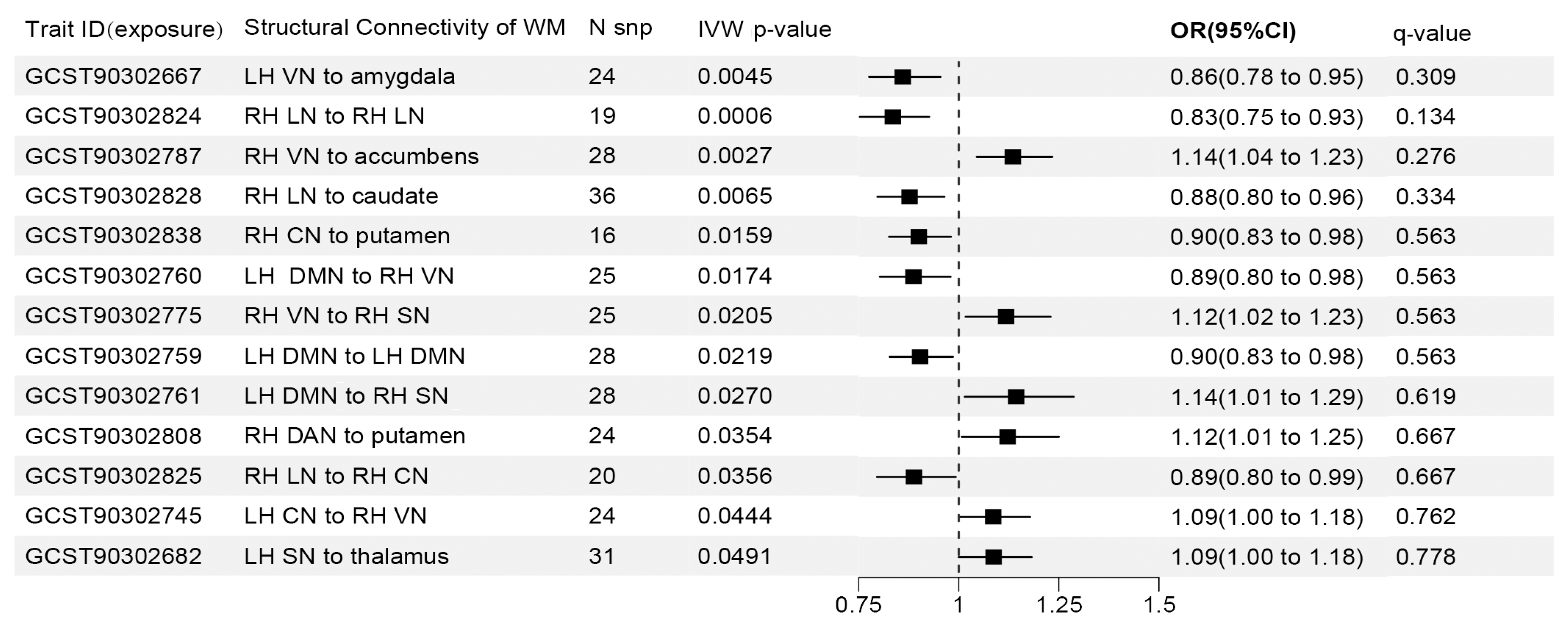
3.3. Reverse MR Analysis
3.4. Sensitivity Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kingman, S. Glaucoma Is Second Leading Cause of Blindness Globally. Bull. World Health Organ. 2004, 82, 887–888. [Google Scholar]
- Zhang, H.J.; Mi, X.S.; So, K.F. Normal Tension Glaucoma: From the Brain to the Eye or the Inverse? Neural Regen. Res. 2019, 14, 1845–1850. [Google Scholar] [CrossRef]
- Klugah-Brown, B.; Bore, M.C.; Liu, X.; Gan, X.; Biswal, B.B.; Kendrick, K.M.; Chang, D.H.; Zhou, B.; Becker, B. The Neurostructural Consequences of Glaucoma and Their Overlap with Disorders Exhibiting Emotional Dysregulations: A Voxel-Based Meta-Analysis and Tripartite System Model. J. Affect. Disord. 2024, 358, 487–499. [Google Scholar] [CrossRef]
- Zhong, T.; Zhou, J.; Yan, T.; Qiu, J.; Wang, Y.; Lu, W. Pseudo-Time Series Structural Mri Revealing Progressive Gray Matter Changes with Elevated Intraocular Pressure in Primary Open-Angle Glaucoma: A Preliminary Study. Acad. Radiol. 2024, 31, 3754–3763. [Google Scholar] [CrossRef]
- Yücel, Y. Central Nervous System Changes in Glaucoma. J. Glaucoma 2013, 22 (Suppl. S5), S24–S25. [Google Scholar] [CrossRef]
- Giorgio, A.; Zhang, J.; Costantino, F.; De Stefano, N.; Frezzotti, P. Diffuse Brain Damage in Normal Tension Glaucoma. Hum. Brain Mapp. 2018, 39, 532–541. [Google Scholar] [CrossRef]
- You, M.; Rong, R.; Zeng, Z.; Xia, X.; Ji, D. Transneuronal Degeneration in the Brain During Glaucoma. Front. Aging Neurosci. 2021, 13, 643685. [Google Scholar] [CrossRef]
- Mendoza, M.; Shotbolt, M.; Faiq, M.A.; Parra, C.; Chan, K.C. Advanced Diffusion Mri of the Visual System in Glaucoma: From Experimental Animal Models to Humans. Biology 2022, 11, 454. [Google Scholar] [CrossRef]
- Wang, J.; Zhang, Y.; Meng, X.; Liu, G. Application of Diffusion Tensor Imaging Technology in Glaucoma Diagnosis. Front. Neurosci. 2023, 17, 1125638. [Google Scholar] [CrossRef]
- Engelhorn, T.; Schmidt, M.A.; Dörfler, A.; Michelson, G. Diffusion Tensor Imaging of the Visual Pathway in Glaucomatous Optic Nerve Atrophy. Ophthalmologe 2017, 114, 906–921. [Google Scholar] [CrossRef]
- Rüber, T.; Elger, C.E.; Weber, B. Diffusion Tensor Imaging (Dti) and Tractography. In Neuroeconomics; Reuter, M., Montag, C., Eds.; Springer: Berlin/Heidelberg, Germany, 2016; pp. 411–442. [Google Scholar]
- Jeurissen, B.; Descoteaux, M.; Mori, S.; Leemans, A. Diffusion Mri Fiber Tractography of the Brain. NMR Biomed. 2019, 32, e3785. [Google Scholar] [CrossRef]
- Ogawa, S.; Takemura, H.; Horiguchi, H.; Miyazaki, A.; Matsumoto, K.; Masuda, Y.; Yoshikawa, K.; Nakano, T. Multi-Contrast Magnetic Resonance Imaging of Visual White Matter Pathways in Patients with Glaucoma. Investig. Ophthalmol. Vis. Sci. 2022, 63, 29. [Google Scholar] [CrossRef]
- Engelhorn, T.; Michelson, G.; Waerntges, S.; Hempel, S.; El-Rafei, A.; Struffert, T.; Doerfler, A. A New Approach to Assess Intracranial White Matter Abnormalities in Glaucoma Patients: Changes of Fractional Anisotropy Detected by 3t Diffusion Tensor Imaging. Acad. Radiol. 2012, 19, 485–488. [Google Scholar] [CrossRef]
- Li, K.; Lu, C.; Huang, Y.; Yuan, L.; Zeng, D.; Wu, K. Alteration of Fractional Anisotropy and Mean Diffusivity in Glaucoma: Novel Results of a Meta-Analysis of Diffusion Tensor Imaging Studies. PLoS ONE 2014, 9, e97445. [Google Scholar] [CrossRef]
- Li, M.; Ke, M.; Song, Y.; Mu, K.; Zhang, H.; Chen, Z. Diagnostic Utility of Central Damage Determination in Glaucoma by Magnetic Resonance Imaging: An Observational Study. Exp. Ther. Med. 2019, 17, 1891–1895. [Google Scholar] [CrossRef]
- Tellouck, L.; Durieux, M.; Coupé, P.; Cougnard-Grégoire, A.; Tellouck, J.; Tourdias, T.; Munsch, F.; Garrigues, A.; Helmer, C.; Malet, F.; et al. Optic Radiations Microstructural Changes in Glaucoma and Association with Severity: A Study Using 3tesla-Magnetic Resonance Diffusion Tensor Imaging. Investig. Ophthalmol. Vis. Sci. 2016, 57, 6539–6547. [Google Scholar] [CrossRef]
- Qu, X.; Wang, Q.; Chen, W.; Li, T.; Guo, J.; Wang, H.; Zhang, X.; Wang, Y.; Wang, N.; Xian, J. Combined Machine Learning and Diffusion Tensor Imaging Reveals Altered Anatomic Fiber Connectivity of the Brain in Primary Open-Angle Glaucoma. Brain Res. 2019, 1718, 83–90. [Google Scholar] [CrossRef]
- Di Ciò, F.; Garaci, F.; Minosse, S.; Passamonti, L.; Martucci, A.; Lanzafame, S.; Di Giuliano, F.; Picchi, E.; Cesareo, M.; Guerrisi, M.G.; et al. Reorganization of the Structural Connectome in Primary Open Angle Glaucoma. Neuroimage Clin. 2020, 28, 102419. [Google Scholar] [CrossRef]
- Wang, Y.; Guo, L.; Wang, R.; Wang, Y.; Duan, F.; Zhan, Y.; Cheng, J.; Sun, X.; Tang, Z. Abnormal Topological Organization of White Matter Structural Networks in Normal Tension Glaucoma Revealed via Diffusion Tensor Tractography. Brain Sci. 2023, 13, 1597. [Google Scholar] [CrossRef]
- Emdin, C.A.; Khera, A.V.; Kathiresan, S. Mendelian Randomization. JAMA 2017, 318, 1925–1926. [Google Scholar] [CrossRef]
- Birney, E. Mendelian Randomization. Cold Spring Harb. Perspect. Med. 2022, 12, a041302. [Google Scholar] [CrossRef]
- Zhang, X.; Liang, Y.; Huang, Y.; Liu, S.; Li, Q.; Wang, S.; Wu, G.; Du, Z.; Wang, Y.; Wang, J.; et al. Evaluation of the Observational Associations and Shared Genetics between Glaucoma with Depression and Anxiety. Investig. Ophthalmol. Vis. Sci. 2024, 65, 12. [Google Scholar] [CrossRef]
- Wu, Y.; Shi, R.; Chen, H.; Zhang, Z.; Bao, S.; Qu, J.; Zhou, M. Effect of the Gut Microbiome in Glaucoma Risk from the Causal Perspective. BMJ Open Ophthalmol. 2024, 9, e001547. [Google Scholar] [CrossRef]
- Wainberg, M.; Forde, N.J.; Mansour, S.; Kerrebijn, I.; Medland, S.E.; Hawco, C.; Tripathy, S.J. Genetic Architecture of the Structural Connectome. Nat. Commun. 2024, 15, 1962. [Google Scholar] [CrossRef]
- Sala, A.; Lizarraga, A.; Caminiti, S.P.; Calhoun, V.D.; Eickhoff, S.B.; Habeck, C.; Jamadar, S.D.; Perani, D.; Pereira, J.B.; Veronese, M.; et al. Brain Connectomics: Time for a Molecular Imaging Perspective? Trends Cogn. Sci. 2023, 27, 353–366. [Google Scholar] [CrossRef]
- Skrivankova, V.W.; Richmond, R.C.; Woolf, B.A.R.; Yarmolinsky, J.; Davies, N.M.; Swanson, S.A.; VanderWeele, T.J.; Higgins, J.P.T.; Timpson, N.J.; Dimou, N.; et al. Strengthening the Reporting of Observational Studies in Epidemiology Using Mendelian Randomization: The Strobe-Mr Statement. JAMA 2021, 326, 1614–1621. [Google Scholar] [CrossRef]
- Hemani, G.; Zheng, J.; Elsworth, B.; Wade, K.H.; Haberland, V.; Baird, D.; Laurin, C.; Burgess, S.; Bowden, J.; Langdon, R.; et al. The Mr-Base Platform Supports Systematic Causal Inference across the Human Phenome. eLife 2018, 7, e34408. [Google Scholar] [CrossRef]
- Burgess, S.; Butterworth, A.; Thompson, S.G. Mendelian Randomization Analysis with Multiple Genetic Variants Using Summarized Data. Genet. Epidemiol. 2013, 37, 658–665. [Google Scholar] [CrossRef]
- Bowden, J.; Davey Smith, G.; Burgess, S. Mendelian Randomization with Invalid Instruments: Effect Estimation and Bias Detection through Egger Regression. Int. J. Epidemiol. 2015, 44, 512–525. [Google Scholar] [CrossRef]
- Greco, M.F.; Minelli, C.; Sheehan, N.A.; Thompson, J.R. Detecting Pleiotropy in Mendelian Randomisation Studies with Summary Data and a Continuous Outcome. Stat. Med. 2015, 34, 2926–2940. [Google Scholar] [CrossRef]
- Maier-Hein, K.H.; Neher, P.F.; Houde, J.-C.; Côté, M.-A.; Garyfallidis, E.; Zhong, J.; Chamberland, M.; Yeh, F.-C.; Lin, Y.-C.; Ji, Q.; et al. The Challenge of Mapping the Human Connectome Based on Diffusion Tractography. Nat. Commun. 2017, 8, 1349. [Google Scholar] [CrossRef]
- Cio, F.D.; Garaci, F.; Minosse, S.; Passamonti, L.; Martucci, A.; Lanzafame, S.; Di Giuliano, F.; Picchi, E.; Mancino, R.; Guerrisi, M.; et al. Disruption of Structural Brain Networks in Primary Open Angle Glaucoma. Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. 2020, 2020, 1705–1708. [Google Scholar] [CrossRef]
- Boucard, C.C.; Hanekamp, S.; Ćurčić-Blake, B.; Ida, M.; Yoshida, M.; Cornelissen, F.W. Neurodegeneration Beyond the Primary Visual Pathways in a Population with a High Incidence of Normal-Pressure Glaucoma. Ophthalmic Physiol. Opt. 2016, 36, 344–353. [Google Scholar] [CrossRef]
- Li, T.; Liu, Z.; Li, J.; Tang, Z.; Xie, X.; Yang, D.; Wang, N.; Tian, J.; Xian, J. Altered Amplitude of Low-Frequency Fluctuation in Primary Open-Angle Glaucoma: A Resting-State Fmri Study. Investig. Ophthalmol. Vis. Sci. 2014, 56, 322–329. [Google Scholar] [CrossRef]
- Wang, Q.; Qu, X.; Chen, W.; Wang, H.; Huang, C.; Li, T.; Wang, N.; Xian, J. Altered Coupling of Cerebral Blood Flow and Functional Connectivity Strength in Visual and Higher Order Cognitive Cortices in Primary Open Angle Glaucoma. J. Cereb. Blood Flow Metab. 2021, 41, 901–913. [Google Scholar] [CrossRef]
- Litwińczuk, M.C.; Muhlert, N.; Cloutman, L.; Trujillo-Barreto, N.; Woollams, A. Combination of Structural and Functional Connectivity Explains Unique Variation in Specific Domains of Cognitive Function. NeuroImage 2022, 262, 119531. [Google Scholar] [CrossRef]
- Ha, Y.W.; Jang, H.; Koh, S.-B.; Noh, Y.; Lee, S.-K.; Seo, S.W.; Cho, J.; Kim, C. Reduced Brain Subcortical Volumes in Patients with Glaucoma: A Pilot Neuroimaging Study Using the Region-of-Interest-Based Approach. BMC Neurol. 2022, 22, 277. [Google Scholar] [CrossRef]
- Zikou, A.K.; Kitsos, G.; Tzarouchi, L.C.; Astrakas, L.; Alexiou, G.A.; Argyropoulou, M.I. Voxel-Based Morphometry and Diffusion Tensor Imaging of the Optic Pathway in Primary Open-Angle Glaucoma: A Preliminary Study. Am. J. Neuroradiol. 2012, 33, 128–134. [Google Scholar] [CrossRef]
- Smith, J.C.; Zhang, K.Y.; Sladek, A.; Thompson, J.; Bierlein, E.R.; Bhandari, A.; Van Hook, M.J. Loss of Retinogeniculate Synaptic Function in the Dba/2j Mouse Model of Glaucoma. eNeuro 2022, 9, ENEURO.0421-22.2022. [Google Scholar] [CrossRef]
- Van Hook, M.J.; McCool, S. Enhanced Synaptic Inhibition in the Dorsolateral Geniculate Nucleus in a Mouse Model of Glaucoma. eNeuro 2024, 11, ENEURO.0263-24.2024. [Google Scholar] [CrossRef]
- Keun, J.T.B.; van Heese, E.M.; Laansma, M.A.; Weeland, C.J.; de Joode, N.T.; van den Heuvel, O.A.; Gool, J.K.; Kasprzak, S.; Bright, J.K.; Vriend, C.; et al. Structural Assessment of Thalamus Morphology in Brain Disorders: A Review and Recommendation of Thalamic Nucleus Segmentation and Shape Analysis. Neurosci. Biobehav. Rev. 2021, 131, 466–478. [Google Scholar] [CrossRef]
- You, Y.; Joseph, C.; Wang, C.; Gupta, V.; Liu, S.; Yiannikas, C.; Chua, B.E.; Chitranshi, N.; Shen, T.; Dheer, Y.; et al. Demyelination Precedes Axonal Loss in the Transneuronal Spread of Human Neurodegenerative Disease. Brain 2019, 142, 426–442. [Google Scholar] [CrossRef]
- Haykal, S.; Jansonius, N.M.; Cornelissen, F.W. Progression of Visual Pathway Degeneration in Primary Open-Angle Glaucoma: A Longitudinal Study. Front. Hum. Neurosci. 2021, 15, 630898. [Google Scholar] [CrossRef]
- Haykal, S.; Curcic-Blake, B.; Jansonius, N.M.; Cornelissen, F.W. Fixel-Based Analysis of Visual Pathway White Matter in Primary Open-Angle Glaucoma. Investig. Ophthalmol. Vis. Sci. 2019, 60, 3803–3812. [Google Scholar] [CrossRef]
- Prins, D.; Hanekamp, S.; Cornelissen, F.W. Structural Brain Mri Studies in Eye Diseases: Are They Clinically Relevant? A Review of Current Findings. Acta Ophthalmol. 2016, 94, 113–121. [Google Scholar] [CrossRef]
- Garner, C. Upward Bias in Odds Ratio Estimates from Genome-Wide Association Studies. Genet. Epidemiol. 2007, 31, 288–295. [Google Scholar] [CrossRef]
- Wang, K. Interval Estimate of Causal Effect in Summary Data Based Mendelian Randomization in the Presence of Winner’s Curse. Genet. Epidemiol. 2024, 48, 74–84. [Google Scholar] [CrossRef]
- Yucel, Y.H.; Gupta, N. A Framework to Explore the Visual Brain in Glaucoma with Lessons from Models and Man. Exp. Eye Res. 2015, 141, 171–178. [Google Scholar] [CrossRef]
- Liu, K.; Wu, P.; Chen, B.; Cai, Y.; Yuan, R.; Zou, J. Implicating Causal Brain Magnetic Resonance Imaging in Glaucoma Using Mendelian Randomization. Front. Med. 2022, 9, 956339. [Google Scholar] [CrossRef]
- Phelps, E.A.; LeDoux, J.E. Contributions of the Amygdala to Emotion Processing: From Animal Models to Human Behavior. Neuron 2005, 48, 175–187. [Google Scholar] [CrossRef]
- Mukherjee, P.; Vilgis, V.; Rhoads, S.; Chahal, R.; Fassbender, C.; Leibenluft, E.; Dixon, J.F.; Pakyurek, M.; van den Bos, W.; Hinshaw, S.P.; et al. Associations of Irritability with Functional Connectivity of Amygdala and Nucleus Accumbens in Adolescents and Young Adults with Adhd. J. Atten. Disord. 2022, 26, 1040–1050. [Google Scholar] [CrossRef]
- Chen, Y.; Wang, Y.; Chen, L.; Ouyang, F.; Yin, M.; Lv, L.; Xu, Z.; Liu, J.; Zeng, X. Altered Resting-State Amygdalar Functional Connectivity in Primary Angle-Closure Glaucoma Patients. J. Integr. Neurosci. 2024, 23, 75. [Google Scholar] [CrossRef]
- Greicius, M.D.; Kimmel, D.L. Neuroimaging Insights into Network-Based Neurodegeneration. Curr. Opin. Neurol. 2012, 25, 727–734. [Google Scholar] [CrossRef]
- Drzezga, A. The Network Degeneration Hypothesis: Spread of Neurodegenerative Patterns along Neuronal Brain Networks. J. Nucl. Med. 2018, 59, 1645–1648. [Google Scholar] [CrossRef]
- Liu, Q.; Zhou, X.; Liu, K.; Wang, Y.; Liu, C.; Gao, C.; Cai, Q.; Sun, C. Exploring Risk Factors for Autoimmune Diseases Complicated by Non-Hodgkin Lymphoma through Regulatory T Cell Immune-Related Traits: A Mendelian Randomization Study. Front. Immunol. 2024, 15, 1374938. [Google Scholar] [CrossRef]
- Xu, J.; Chen, R.; Yang, Y.; Xu, S.; Yao, L. Genetically Predicted 91 Circulating Inflammatory Proteins in Relation to Risk of Urological Malignancies: A Mendelian Randomization Study. Aging 2024, 16, 10366–10379. [Google Scholar] [CrossRef]
- Lou, A.R.; Madsen, K.H.; Julian, H.O.; Toft, P.B.; Kjaer, T.W.; Paulson, O.B.; Prause, J.U.; Siebner, H.R. Postoperative Increase in Grey Matter Volume in Visual Cortex after Unilateral Cataract Surgery. Acta Ophthalmol. 2013, 91, 58–65. [Google Scholar] [CrossRef]
- Rosengarth, K.; Keck, I.; Brandl-Rühle, S.; Frolo, J.; Hufendiek, K.; Greenlee, M.W.; Plank, T. Functional and Structural Brain Modifications Induced by Oculomotor Training in Patients with Age-Related Macular Degeneration. Front. Psychol. 2013, 4, 428. [Google Scholar] [CrossRef]
- Sharma, S.; Chitranshi, N.; Wall, R.V.; Basavarajappa, D.; Gupta, V.; Mirzaei, M.; Graham, S.L.; Klistorner, A.; You, Y. Trans-Synaptic Degeneration in the Visual Pathway: Neural Connectivity, Pathophysiology, and Clinical Implications in Neurodegenerative Disorders. Surv. Ophthalmol. 2022, 67, 411–426. [Google Scholar] [CrossRef]
- Sabel, B.A.; Gao, Y.; Antal, A. Reversibility of Visual Field Defects through Induction of Brain Plasticity: Vision Restoration, Recovery and Rehabilitation Using Alternating Current Stimulation. Neural Regen. Res. 2020, 15, 1799–1806. [Google Scholar] [CrossRef]
- Prabhakaran, G.T.; Al-Nosairy, K.O.; Tempelmann, C.; Wagner, M.; Thieme, H.; Hoffmann, M.B. Functional Dynamics of Deafferented Early Visual Cortex in Glaucoma. Front. Neurosci. 2021, 15, 653632. [Google Scholar] [CrossRef]
- Haykal, S.; Invernizzi, A.; Carvalho, J.; Jansonius, N.M.; Cornelissen, F.W. Microstructural Visual Pathway White Matter Alterations in Primary Open-Angle Glaucoma: A Neurite Orientation Dispersion and Density Imaging Study. Am. J. Neuroradiol. 2022, 43, 756–763. [Google Scholar] [CrossRef]
- El-Rafei, A.; Engelhorn, T.; Wärntges, S.; Dörfler, A.; Hornegger, J.; Michelson, G. Glaucoma Classification Based on Visual Pathway Analysis Using Diffusion Tensor Imaging. Magn. Reson. Imaging 2013, 31, 1081–1091. [Google Scholar] [CrossRef]
- Sidek, S.; Ramli, N.; Rahmat, K.; Ramli, N.M.; Abdulrahman, F.; Tan, L.K. Glaucoma Severity Affects Diffusion Tensor Imaging (Dti) Parameters of the Optic Nerve and Optic Radiation. Eur. J. Radiol. 2014, 83, 1437–1441. [Google Scholar] [CrossRef]
- Wang, R.; Tang, Z.; Sun, X.; Wu, L.; Wang, J.; Zhong, Y.; Xiao, Z. White Matter Abnormalities and Correlation with Severity in Normal Tension Glaucoma: A Whole Brain Atlas-Based Diffusion Tensor Study. Investig. Ophthalmol. Vis. Sci. 2018, 59, 1313–1322. [Google Scholar] [CrossRef]
- Mastropasqua, R.; Agnifili, L.; Mattei, P.A.; Caulo, M.; Fasanella, V.; Navarra, R.; Mastropasqua, L.; Marchini, G. Advanced Morphological and Functional Magnetic Resonance Techniques in Glaucoma. BioMed Res. Int. 2015, 2015, 160454. [Google Scholar] [CrossRef]
- Gracitelli, C.P.B.; Gerente, V.M.; Furlanetto, R.L.; Amaro, E., Jr.; Paranhos, A., Jr. Magnetic Resonance Imaging for Glaucoma Evaluation. J. Glaucoma 2020, 29, 622–626. [Google Scholar] [CrossRef]
- Yoshimine, S.; Ogawa, S.; Horiguchi, H.; Terao, M.; Miyazaki, A.; Matsumoto, K.; Tsuneoka, H.; Nakano, T.; Masuda, Y.; Pestilli, F. Age-Related Macular Degeneration Affects the Optic Radiation White Matter Projecting to Locations of Retinal Damage. Brain Struct. Funct. 2018, 223, 3889–3900. [Google Scholar] [CrossRef]
- Allen, B.; Schmitt, M.A.; Kushner, B.J.; Rokers, B. Retinothalamic White Matter Abnormalities in Amblyopia. Investig. Ophthalmol. Vis. Sci. 2018, 59, 921–929. [Google Scholar] [CrossRef]
- Wang, H.; Wen, H.; Li, J.; Chen, Q.; Li, S.; Wang, Z. Disrupted Topological Organization of White Matter Structural Networks in High Myopia Patients Revealed by Diffusion Kurtosis Imaging and Tractography. Front. Neurosci. 2023, 17, 1158928. [Google Scholar] [CrossRef]
- Zhao, B.; Li, Y.; Fan, Z.; Wu, Z.; Shu, J.; Yang, X.; Yang, Y.; Wang, X.; Li, B.; Wang, X.; et al. Eye-Brain Connections Revealed by Multimodal Retinal and Brain Imaging Genetics. Nat. Commun. 2024, 15, 6064. [Google Scholar] [CrossRef]
- Martucci, A.; Di Giuliano, F.; Minosse, S.; Pocobelli, G.; Nucci, C.; Garaci, F. Mri and Clinical Biomarkers Overlap between Glaucoma and Alzheimer’s Disease. Int. J. Mol. Sci. 2023, 24, 14932. [Google Scholar] [CrossRef]
- Huh, M.G.; Kim, Y.K.; Lee, J.; Shin, Y.I.; Lee, Y.J.; Choe, S.; Kim, D.W.; Jeong, Y.; Jeoung, J.W.; Park, K.H. Relative Risks for Dementia among Individuals with Glaucoma: A Meta-Analysis of Observational Cohort Studies. Korean J. Ophthalmol. 2023, 37, 490–500. [Google Scholar] [CrossRef]
- Saccà, S.C.; Paluan, F.; Gandolfi, S.; Manni, G.; Cutolo, C.A.; Izzotti, A. Common Aspects between Glaucoma and Brain Neurodegeneration. Mutat. Res. Rev. Mutat. Res. 2020, 786, 108323. [Google Scholar] [CrossRef]
- Ngoo, Q.Z.; Wan Hitam, W.H.; Ab Razak, A. Evaluation of Retinal Nerve Fiber Layer Thickness, Electroretinogram and Visual Evoked Potential in Patients with Alzheimer’s Disease. J. Ophthalmol. 2019, 2019, 6248185. [Google Scholar] [CrossRef]
- Hu, Z.; Wang, L.; Zhu, D.; Qin, R.; Sheng, X.; Ke, Z.; Shao, P.; Zhao, H.; Xu, Y.; Bai, F. Retinal Alterations as Potential Biomarkers of Structural Brain Changes in Alzheimer’s Disease Spectrum Patients. Brain Sci. 2023, 13, 460. [Google Scholar] [CrossRef]
- Lee, J.Y.; Yoon, E.J.; Lee, W.W.; Kim, Y.K.; Lee, J.Y.; Jeon, B. Lateral Geniculate Atrophy in Parkinson’s with Visual Hallucination: A Trans-Synaptic Degeneration? Mov. Disord. 2016, 31, 547–554. [Google Scholar] [CrossRef]
- Larsson, S.C.; Butterworth, A.S.; Burgess, S. Mendelian Randomization for Cardiovascular Diseases: Principles and Applications. Eur. Heart J. 2023, 44, 4913–4924. [Google Scholar] [CrossRef]
- Gage, S.H.; Smith, G.D.; Ware, J.J.; Flint, J.; Munafò, M.R. G = E: What Gwas Can Tell Us about the Environment. PLoS Genet. 2016, 12, e1005765. [Google Scholar] [CrossRef]
- Zhang, X.; Olson, D.J.; Le, P.; Lin, F.C.; Fleischman, D.; Davis, R.M. The Association between Glaucoma, Anxiety, and Depression in a Large Population. Am. J. Ophthalmol. 2017, 183, 37–41. [Google Scholar] [CrossRef]
- Groff, M.L.; Choi, B.; Lin, T.; McLlraith, I.; Hutnik, C.; Malvankar-Mehta, M.S. Anxiety, Depression, and Sleep-Related Outcomes of Glaucoma Patients: Systematic Review and Meta-Analysis. Can. J. Ophthalmol. J. Can. D’ophtalmologie 2023, 58, 346–355. [Google Scholar] [CrossRef]
- Mu, C.; Dang, X.; Luo, X.J. Mendelian Randomization Analyses Reveal Causal Relationships between Brain Functional Networks and Risk of Psychiatric Disorders. Nat. Hum. Behav. 2024, 8, 1417–1428. [Google Scholar] [CrossRef]
- Della Santina, L.; Ou, Y. Who’s Lost First? Susceptibility of Retinal Ganglion Cell Types in Experimental Glaucoma. Exp. Eye Res. 2017, 158, 43–50. [Google Scholar] [CrossRef]
- Amin, D.; Kuwajima, T. Differential Retinal Ganglion Cell Vulnerability, a Critical Clue for the Identification of Neuroprotective Genes in Glaucoma. Front. Ophthalmol. 2022, 2, 905352. [Google Scholar] [CrossRef]


| Traits | Year | Database | Data Sources | Sample Sizes | Population |
|---|---|---|---|---|---|
| Glaucoma | 2021 | FinnGen.R10 | https://storage.googleapis.com/finngen-public-data-r10/summary_stats/finngen_R10_H7_GLAUCOMA.gz (accessed on 29 August 2024); | 20,906 cases and 391,275 controls | EUR |
| DTT traits | 2024 | UK Biobank | accession numbers GCST90302648 to GCST90302853; https://www.ebi.ac.uk/gwas (accessed on 29 August 2024); | 26,333 individuals | EUR |
| Traits ID | Structural Connectivity | N(SNPs) | Egger Intercept | p-Value of Egger Intercept | Cochran’s Q | p-Value of Cochran’s Q |
|---|---|---|---|---|---|---|
| Forward MR | ||||||
| GCST90302682 | LH SN to thalamus | 48 | −0.002973 | 0.536 | 31.50 | 0.960 |
| GCST90302808 | RH DAN to putamen | 48 | 0.002980 | 0.540 | 29.28 | 0.980 |
| GCST90302824 | RH LN to RH LN | 48 | 0.000211 | 0.966 | 34.11 | 0.920 |
| Reverse MR | ||||||
| GCST90302667 | LH VN to amygdala | 24 | 0.003648 | 0.677 | 16.09 | 0.851 |
| GCST90302824 | RH LN to RH LN | 19 | 0.010224 | 0.414 | 10.54 | 0.913 |
| GCST90302787 | RH VN to accumbens | 28 | 0.001613 | 0.830 | 17.22 | 0.926 |
| GCST90302828 | RH LN to caudate | 36 | 0.012419 | 0.086 | 32.93 | 0.568 |
| GCST90302838 | RH CN to putamen | 16 | 0.000023 | 0.998 | 6.68 | 0.966 |
| GCST90302760 | LH DMN to RH VN | 25 | −0.009642 | 0.197 | 19.19 | 0.742 |
| GCST90302775 | RH VN to RH SN | 25 | 0.010420 | 0.203 | 19.47 | 0.727 |
| GCST90302759 | LH DMN to LH DMN | 28 | 0.005086 | 0.425 | 17.46 | 0.919 |
| GCST90302761 | LH DMN to RH SN | 28 | 0.008127 | 0.296 | 25.46 | 0.549 |
| GCST90302808 | RH DAN to putamen | 24 | −0.010452 | 0.141 | 23.74 | 0.419 |
| GCST90302825 | RH LN to RH CN | 20 | 0.004533 | 0.569 | 13.98 | 0.785 |
| GCST90302745 | LH CN to RH VN | 24 | −0.002204 | 0.756 | 13.43 | 0.942 |
| GCST90302682 | LH SN to thalamus | 31 | 0.004978 | 0.504 | 19.85 | 0.920 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shu, L.; Chen, X.; Sun, X. Association Between Glaucoma and Brain Structural Connectivity Based on Diffusion Tensor Tractography: A Bidirectional Mendelian Randomization Study. Brain Sci. 2024, 14, 1030. https://doi.org/10.3390/brainsci14101030
Shu L, Chen X, Sun X. Association Between Glaucoma and Brain Structural Connectivity Based on Diffusion Tensor Tractography: A Bidirectional Mendelian Randomization Study. Brain Sciences. 2024; 14(10):1030. https://doi.org/10.3390/brainsci14101030
Chicago/Turabian StyleShu, Lian, Xiaoxiao Chen, and Xinghuai Sun. 2024. "Association Between Glaucoma and Brain Structural Connectivity Based on Diffusion Tensor Tractography: A Bidirectional Mendelian Randomization Study" Brain Sciences 14, no. 10: 1030. https://doi.org/10.3390/brainsci14101030
APA StyleShu, L., Chen, X., & Sun, X. (2024). Association Between Glaucoma and Brain Structural Connectivity Based on Diffusion Tensor Tractography: A Bidirectional Mendelian Randomization Study. Brain Sciences, 14(10), 1030. https://doi.org/10.3390/brainsci14101030








