Abstract
Shift work may adversely affect individuals’ health, thus, the current study aimed to investigate the association between shift work and health outcomes in the general population. A total of 41,061 participants were included in this online cross-sectional survey, among which 9612 (23.4%) individuals engaged in shift work and 31,449 (76.6%) individuals engaged in non-shift work. Multiple logistic regression analyses were conducted to explore the association between shift work and health outcomes (psychiatric disorders, mental health symptoms, and physical disorders). In addition, associations between the duration (≤1 year, 1–3 years, 3–5 years, 5–10 years, ≥10 years) and frequency of shift work (<1 or ≥1 night/week) and health outcomes were also explored. The results showed that compared to non-shift workers, shift workers had a higher likelihood of any psychiatric disorders (odds ratios [OR] = 1.80, 95% CI = 1.56–2.09, p < 0.001), mental health symptoms (OR = 1.76, 95% CI = 1.68–1.85, p < 0.001), and physical disorders (OR = 1.48, 95% CI = 1.39–1.57, p < 0.001). In addition, inverted U-shaped associations were observed between the duration of shift work and health outcomes. These results indicated that shift work was closely related to potential links with poor health outcomes. The findings highlighted the importance of paying attention to the health conditions of shift workers and the necessity of implementing comprehensive protective measures for shift workers to reduce the impact of shift work.
1. Introduction
With the development of the social economy, the working hours of some industries and factories have been extended to nighttime. Shift work usually involves work schedules inconsistent with customary daytime work, including regular morning, evening, and night work, as well as roster work and rotating three-shift work [1]. For example, in China and Korea, 36.1% of employees undertake shift work [2]. And in the United States, one-fifth of the population are shift workers or work night shifts outside of standard working hours (8:00–17:00) [3]. As time goes by, shift work has gradually been recognized as a serious occupational hazard, affecting about 15–20% of workers worldwide [4]. Recently, the impact of shift work on the long-term health and safety of staff and on social burdens has been emphasized [5].
Shift work may disturb an individual’s circadian system with alterations to sleep-activity patterns, suppression of melatonin production, and deregulation of circadian genes involved in multiple pathophysiological pathways [6,7]. As for now, shift work has been reported to increase the risk of cardiovascular diseases [5,8,9], metabolic diseases [3,10], cancer [11,12], cognitive disorders [13,14,15,16], mortality, and so on. Shift workers’ workplaces, relationships with coworkers, and individual characteristics are all factors that may influence their health conditions [17]. Some studies have found that shift work increases the risk of anxiety and depression [13,18], whereas others suggest that shift workers have better psychiatric well-being and mental health than non-shift workers [19]. In addition, many previous studies focus merely on specific occupation populations such as those from healthcare, industrial manufacturing, mining, transport, communication, leisure, and hospitality sectors, as well as on specific health outcomes such as coronary heart disease, asthma, diabetes, and breast cancer. Hence, there is a lack of study on the comprehensive health effects of shift work in the general population without limiting it to certain occupations.
Previous evidence showed that the frequency and duration of shift work had an impact on the relationship between shift work and some specific health outcomes. A study based on UK Biobank found that 3–8 nights/month, not more than 8 nights/month, of night shift work was associated with a higher risk of coronary heart disease [5]. As well, the risk of diabetes and breast cancer was shown to be associated with more frequent shift work [10,20]. In a cohort study of female nurses followed for 24 years, it was found that longer lifetime durations of night shift work were associated with decreased odds of healthy aging [21]. More research is needed on the inconsistent association between health outcomes and shift frequency [22,23].
Considering that most previous research on shift work and health outcomes focused only on specific diseases [24], this current cross-sectional study aimed to explore this relationship more comprehensively and systematically. We hypothesized that shift work would increase the risk of poor health outcomes (including psychiatric disorders, mental health symptoms, and physical disorders) in the general Chinese population. In addition, the frequency and duration of shift work would be associated with poor health outcomes in this population as well.
2. Methods
2.1. Study Design, Participants, and Data Collection
This cross-sectional study was approved by the Ethics Committee of the Sixth Hospital of Peking University (Institute of Mental Health). An online survey was conducted among the general population in 34 provinces in China from 12 June to 17 July 2022, and informed consent was obtained from all respondents. This self-designed online questionnaire was distributed on the health page of the Chinese website Joybuy; the survey link was posted on the website, and registered members received the link to the questionnaire and voluntarily filled out the questionnaire anonymously [25,26]. Convenience sampling was used to post the link to the questionnaire on the page.
2.2. Assessment of Shift Work
Participants who reported having a job were asked if their current job involved shift work. Shift work is a work schedule that falls outside of normal daytime working hours (9:00–17:00) or multiple shifts on a rotating basis (such as rotating between morning, afternoon, and evening). The answers included ‘never/rarely, sometimes shift work (<1 night/week), regular shift work (≥1 night/week)’.
Participants who answered ‘sometimes shift work (<1 night/week), regular shift work (≥1 night/week)’ were further asked the number of years they had been employed in shift work, with the following choices: ≤1 year, 1–3 years, 3–5 years, 5–10 years, and ≥10 years.
2.3. Assessment of Health Outcomes
Three types of health outcomes were assessed, including psychiatric disorders, mental health symptoms, and physical disorders. The presence of psychiatric disorders was assessed by a self-report questionnaire confirming the diagnosis by a psychiatrist of the following disorders: schizophrenia, anxiety, depression, obsessive compulsive disorder, and bipolar disorder.
Mental health symptoms, including anxiety, depression, and insomnia, were measured by the 2-item Patient Health Questionnaire (PHQ-2) [27,28], the 2-item Generalized Anxiety Disorder Scale (GAD-2) [29], and the 7-item Insomnia Severity Index (ISI) [30,31]. All measures were validated for use in Chinese [32,33,34]. Classification of the presence of poor mental health symptoms according to the total scale scores of measures was as follows: PHQ-2, normal (0–3) and abnormal (4–6) for depression [27], with a Cronbach’s alpha of 0.78 [33,35]; GAD-2, normal (0–3) and abnormal (4–6) for anxiety [36], with a Cronbach’s alpha of 0.82 [37]; and ISI, normal (0–7) and abnormal (≥28) for insomnia [30], with a Cronbach’s alpha of the Chinese version of 0.81 [34]. Scores of participants greater than the cutoff threshold indicate potential mental health symptoms.
Also, the following physical disorders were assessed with a self-reported questionnaire confirming the diagnosis by a physician of hypertension, coronary heart disease, hyperlipidemia, cerebrovascular disease or stroke, brain injury due to trauma, migraine, diabetes, chronic obstructive pulmonary disease, asthma, thyroid disease, arthritis, chronic pain, cancer, Parkinson’s disease, epilepsy, dementia, or mild cognitive impairment.
2.4. Covariates
Three aspects of covariates were considered, including demographic information, lifestyle, and COVID-19 status. Demographic information of the participants included age, sex, ethnicity (ethnic Han and ethnic minorities), living area (urban or rural), level of education, marital status, type of jobs, and monthly family income. Lifestyle included smoking, drinking, diet, body mass index (BMI), exercise habits, sedentary behavior, and napping habits. COVID-19 statuses include the infection status of participants and experience with quarantine during COVID-19 epidemics [16].
2.5. Statistical Analysis
Data analyses were performed using IBM SPSS Statistics, version 25 (IBM Corporation, Armonk, NY, USA). Descriptive statistics were used to represent demographic information, napping habits, and information related to COVID-19. The proportions of health outcomes were reported as the percentages of cases by shift work.
Participant characteristics were described using the mean (standard deviation, SD) for continuous variables and proportions for categorical variables. A t test and χ2 test were applied to examine the statistical significance of continuous variables with normal distribution and categorical variables in different shift work status groups, respectively. Multivariable logistic regression analysis was performed to explore the association between shift work and health outcomes (i.e., psychiatric disorders, mental health symptoms, and physical disorders), with all covariates mentioned above included in the model by Wald tests. Similarly, the association of frequency (<1 or ≥1 night/week) and years of shift work (≤1 year, 1–3 years, 3–5 years, 5–10 years, ≥10 years) with health outcomes were further explored using multivariable logistic regression analysis. Before using the multivariable logistic model, multicollinearity among the independent variables was assessed by calculating the variance inflation factor (VIF). A VIF greater than 5 indicates multicollinearity [38]. Separate models were performed when included independent variables were multicollinear, excluding highly correlated covariates [39]. For all logistic regression analyses, odds ratios (ORs) and 95% confidence intervals (CIs) were calculated. Two-sided Wald tests were used to determine the statistical significance of the ORs within the regression models. The level of significance was set to p < 0.05 for logistic regression, and Bonferroni correction was performed to adjust for multiple comparisons.
3. Results
3.1. Demographic Characteristics
A total of 42,368 participants from 34 provinces in China completed the consent and questionnaire. Data from participants with responses lasting less than 7 min, those under the age of 15, and any duplicate or impaired responses were excluded. Finally, 41,061 individuals were included in the study.
Of the 41,061 participants, 24,247 (59.1%) were female, and the mean (SD) age was 36.24 (9.51) years; 9612 (23.4%) engaged in shift work with 3821 (39.8%) being female. Shift workers reported higher rates of males (60.2% vs. 35.1%), lower education level (22.1% vs. 18.0%), manual work (22.5% vs. 16.6%), smoking (21.2% vs. 9.8%), alcohol consumption (10.5% vs. 5.2%), and low sedentary behavior (40.4% vs. 35.1%) than non-shift workers and lower rates of normal weight (50.1% vs. 56.5%), healthy diet (41.3% vs. 50.2%), regular exercise habit (23.7% vs. 25.8%), low income (27.7% vs. 30.6%), and frequent napping behavior (39.8% vs. 47.3%) compared to non-shift workers, with a p value < 0.001. In relation to COVID-19, a higher proportion of shift workers were infected (5.4% vs. 3.1%, p <0.001) and quarantined (9.4% vs. 6.7%, p < 0.001) than non-shift workers. Table 1 presents the demographic characteristics of the study population according to current shift status.

Table 1.
Demographic characteristics of the total sample stratified by shift work.
3.2. Association of Shift Work with Health Outcomes
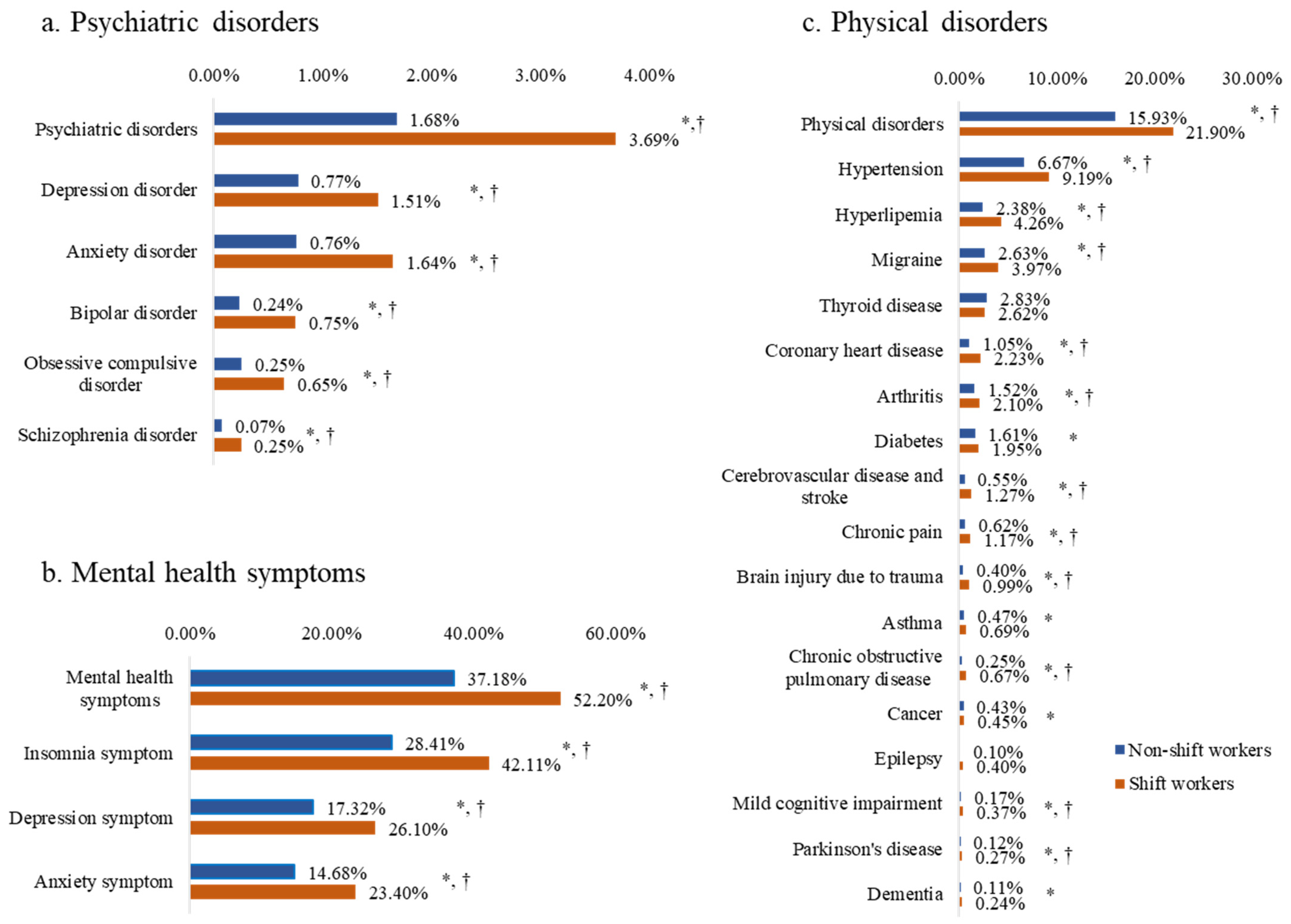
Figure 1 presents the proportions of each health outcome in shift workers and non-shift workers. For the entire sample, the proportion of participants practicing any psychiatric disorder, mental health symptom, and physical disorder were 2.2%, 40.7%, and 17.3%, respectively. Participants in the shift work group reported higher proportions of all three health outcomes when compared to the non-shift workers: psychiatric disorders (3.7% vs. 1.7%, p < 0.001), mental health symptoms (52.2% vs. 37.2%, p < 0.001), and physical disorders (21.9% vs. 15.9%, p < 0.001). The results for the number of detections and rates for health outcomes are shown in Table S1 in the Supplement.
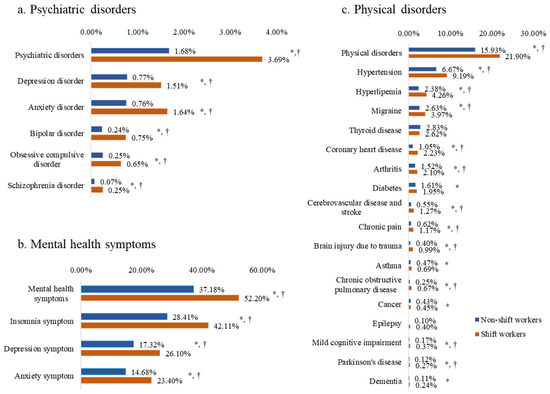
Figure 1.
Proportions of health outcomes in shift workers and non-shift workers. * p < 0.05 in uncorrected tests. † p < 0.0018 in Bonferroni correction tests for multiple comparisons.
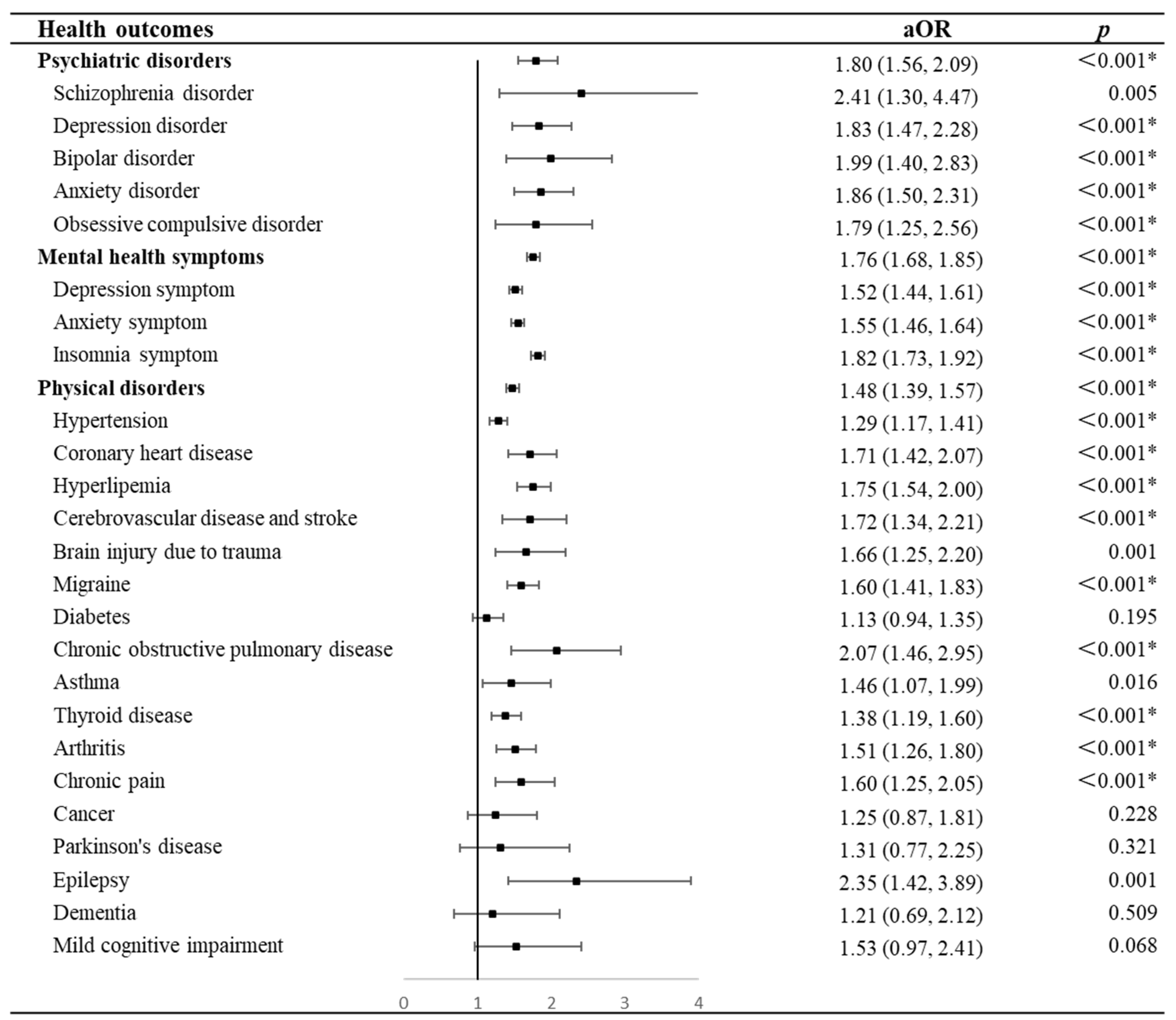
Figure 2 presents the association between shift work and health outcomes in the general population. Compared to non-shift workers, shift workers were more likely to have psychiatric disorders (OR = 1.80, 95% CI = 1.56–2.09, p < 0.001), mental health symptoms (OR = 1.76, 95% CI = 1.68–1.85, p < 0.001), or physical disorders (OR = 1.48, 95% CI = 1.39–1.57, p < 0.001) after adjusting covariates including nocturnal sleep characteristics, day napping, and insomnia, e.g., sleep disturbances. Specifically, shift work exhibited higher ORs of psychiatric disorders, including schizophrenia (OR = 2.41, 95% CI = 1.30–4.47, p = 0.005), bipolar disorder (OR = 1.99, 95% CI = 1.40–2.83, p < 0.001), anxiety (OR = 1.86, 95% CI = 1.50–2.31, p < 0.001), depression (OR = 1.83, 95% CI = 1.47–2.28, p < 0.001), and obsessive compulsive disorder (OR = 1.79, 95% CI = 1.25–2.56, p = 0.001). Similarly, shift workers were associated with increased ORs of depression symptoms (OR = 1.52, 95% CI = 1.44–1.61, p < 0.001), anxiety symptoms (OR = 1.55, 95% CI = 1.46–1.64, p < 0.001), and insomnia symptoms (OR = 1.82, 95% CI = 1.73–1.92, p < 0.001) when compared with non-shift workers. In addition, we have examined the collinearity and the VIF indicated that no collinearity existed. The detailed results of the VIF are shown in the Supplementary Materials (Table S2).
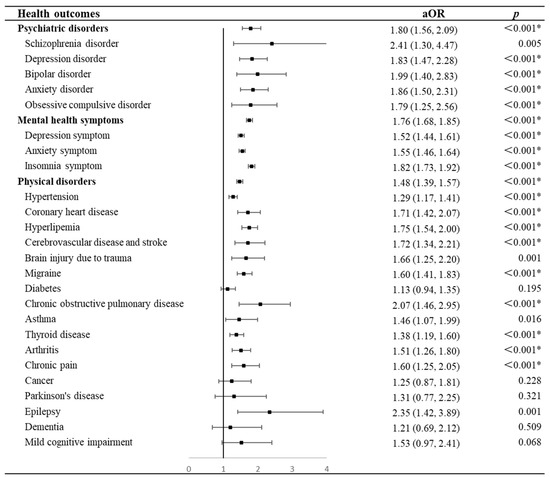
Figure 2.
Forest plots of results for odds ratios of health outcomes in shift workers compared with non-shift workers. * p < 0.0018 in Bonferroni correction tests for multiple comparisons. Abbreviations: aOR, adjusted odds ratio.
In addition, shift work was found to raise the likelihood of certain physical disorders, including hypertension (OR = 1.29, 95% CI = 1.17–1.41, p < 0.001), coronary heart disease (OR = 1.71, 95% CI = 1.42–2.07, p < 0.001), hyperlipidemia (OR = 1.75, 95% CI = 1.54–2.00, p < 0.001), cerebrovascular disease or stroke (OR = 1.72, 95% CI = 1.34–2.21, p < 0.001), brain injury due to trauma (OR = 1.66, 95% CI = 1.25–2.20, p < 0.001), migraine (OR = 1.60, 95% CI = 1.41–1.83, p < 0.001), chronic obstructive pulmonary disease (OR = 2.07, 95% CI = 1.46–2.95, p < 0.001), asthma (OR = 1.46, 95% CI = 1.07–1.99, p < 0.001), thyroid disease (OR = 1.38, 95% CI = 1.19–1.60, p < 0.001), arthritis (OR = 1.51, 95% CI = 1.26–1.80, p < 0.001), chronic pain (OR = 1.60, 95% CI = 1.25–2.05, p < 0.001), and epilepsy (OR = 2.35, 95% CI = 1.42–3.89, p < 0.001), but it was not significantly associated with the risk of diabetes (OR = 1.13, 95% CI = 0.94–1.35, p = 0.195), cancer (OR = 1.25, 95% CI = 0.87–1.81, p = 0.228), Parkinson’s disease (OR = 1.31, 95% CI = 0.77–2.25, p = 0.321), dementia (OR = 1.21, 95% CI = 0.69–2.12, p = 0.509), and mild cognitive impairment (OR = 1.53, 95% CI = 0.97–2.41, p = 0.068).
3.3. Association of Frequency of Shift Work with Health Outcomes
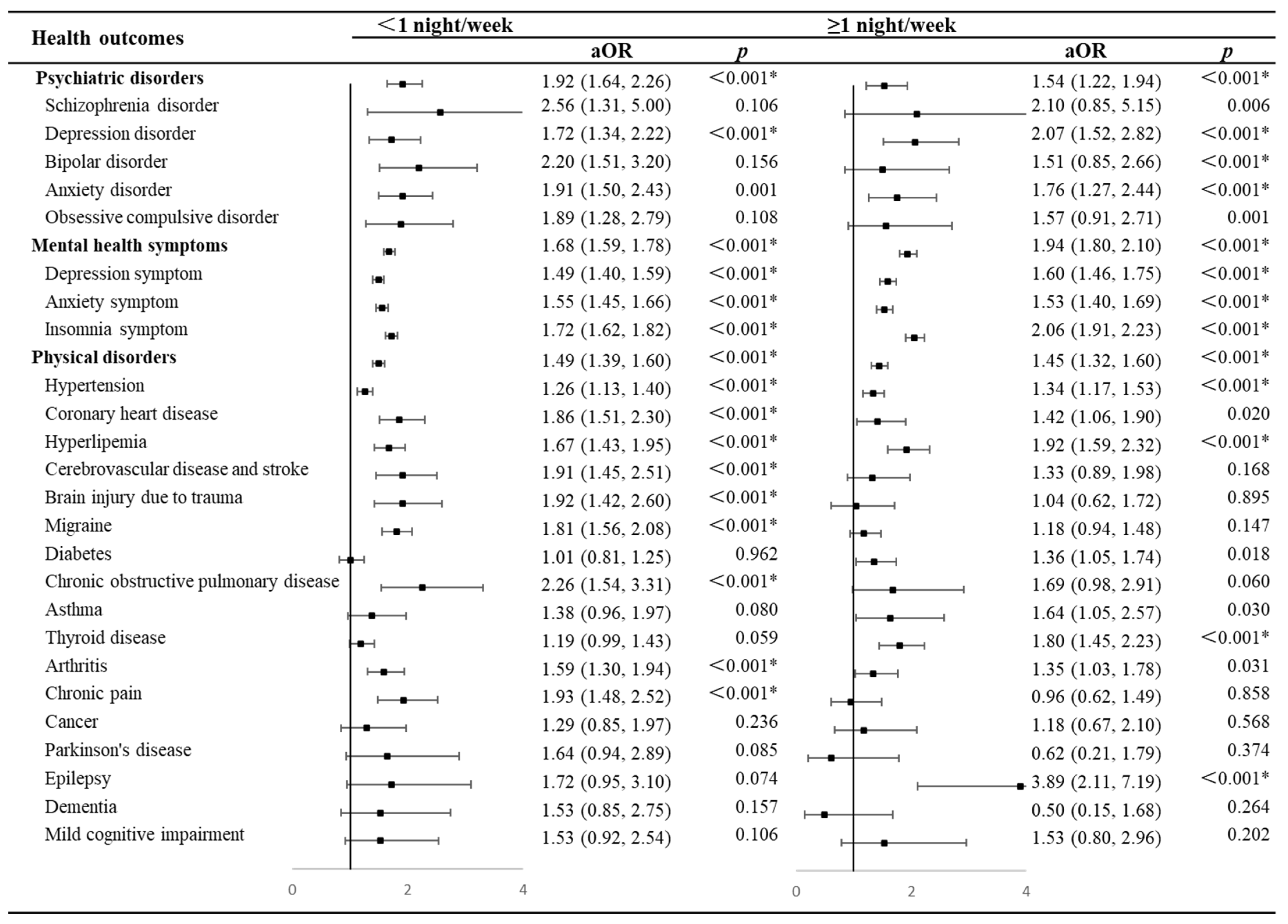
Figure 3 demonstrates the association between the frequency of shift work and each health outcome. Compared to non-shift workers, shift workers were associated with an increased likelihood of poor health outcomes regardless of shift frequency. Individuals with a shift frequency of <1 night/week had higher ORs for psychiatric disorders (OR = 1.92, 95% CI = 1.64–2.26, p < 0.001 vs. OR = 1.54, 95% CI = 1.22–1.94, p < 0.001) and physical disorders (OR = 1.49, 95% CI = 1.39–1.60, p < 0.001 vs. OR = 1.45, 95% CI = 1.32–1.60, p < 0.001) but lower ORs for mental health symptoms (OR = 1.68, 95% CI = 1.59–1.78, p <0.001 vs. OR = 1.94, 95% CI = 1.80–2.10, p <0.001) than those with a shift frequency of ≥1 night/week.
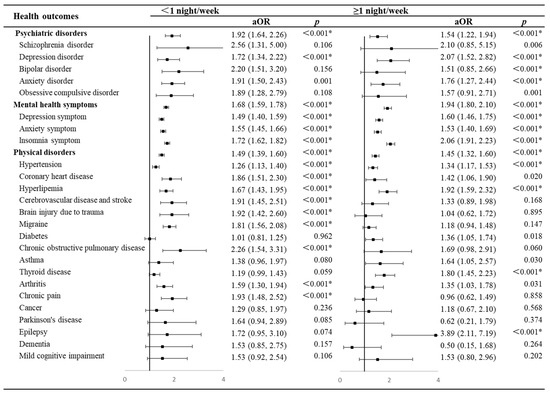
Figure 3.
Forest plots of results of odds ratios for health outcomes in different frequencies of shift work compared with non-shift workers. * p < 0.0018 in Bonferroni correction tests for multiple comparisons. Abbreviations: aOR, adjusted odds ratio.
3.4. Association of Years of Shift Work with Health Outcomes
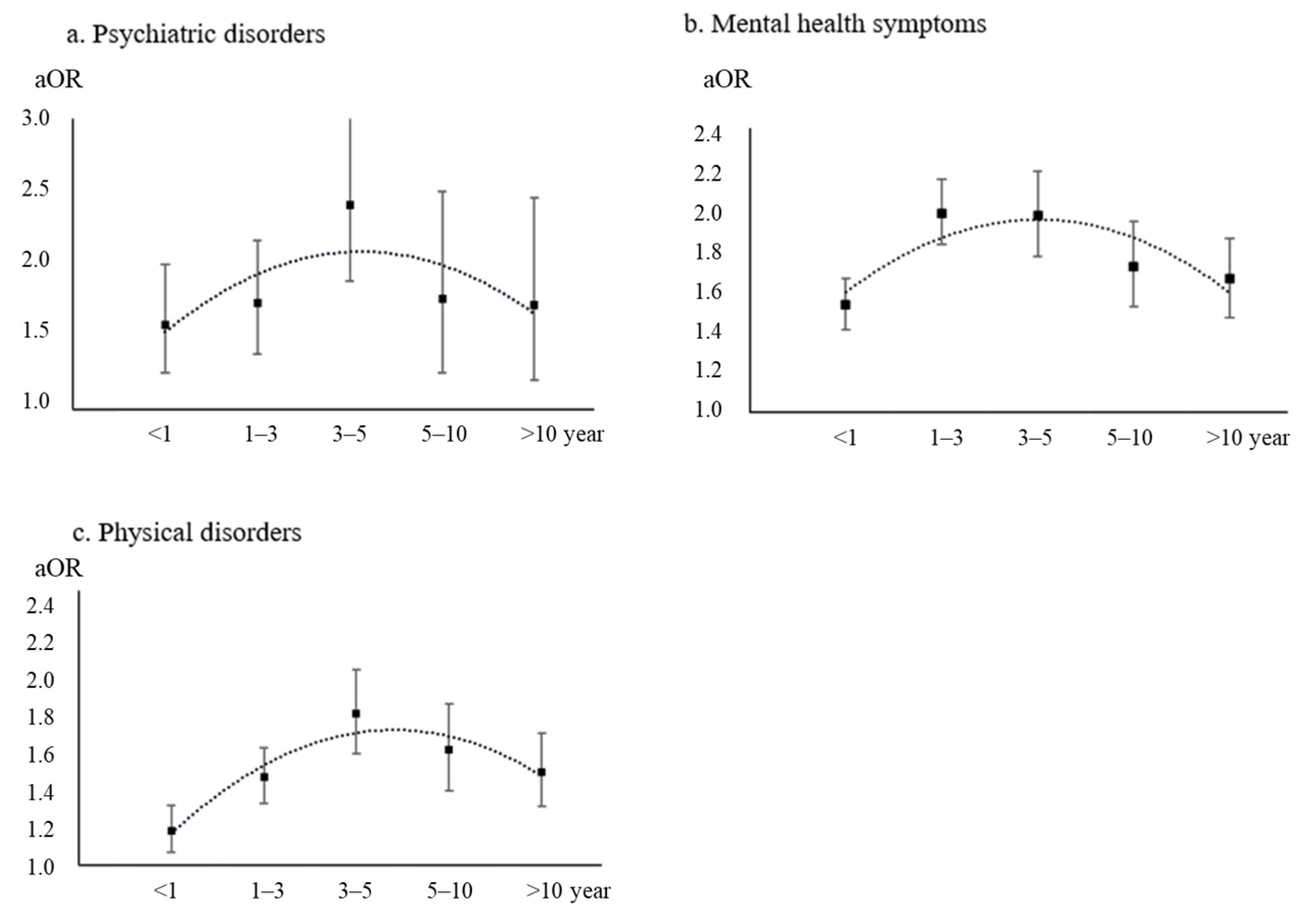
Figure 4 presents the results of associations between years of shift work and any health outcomes. Overall, inverted U-shaped associations between years of shift work and health outcomes were observed after adjusting for covariates. The ORs of poor health outcomes associated with shift work rose within 3 years, reached peaks at 3–5 years (psychiatric disorders: OR = 2.41, 95% CI = 1.88–3.10, p < 0.001; physical disorders: OR = 1.83, 95% CI = 1.61–2.07, p < 0.001), and then declined after more than 5 years of shift work. A similar trend was found for mental health symptoms, with a peak OR at 1–3 years (OR = 1.98, 95% CI = 1.83–2.15, p < 0.001), after which the OR began to decline.
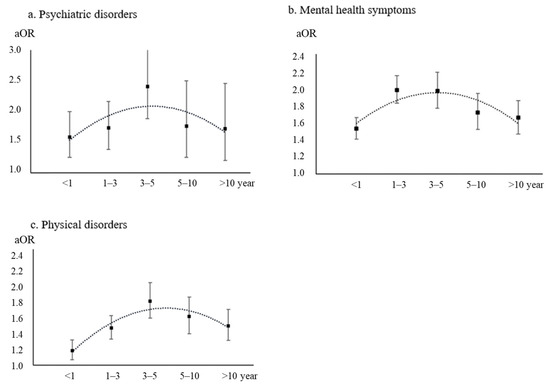
Figure 4.
Associations between years of shift work and health outcomes. Abbreviations: aOR, adjusted odds ratio.
4. Discussion
This cross-sectional study based on a large national sample focused on the health outcomes of shift workers in China, including mental health status and physical health condition. A total of 23.4% of the respondents had been engaging in shift work in this study. Shift workers were more associated with potential links to poor health outcomes than non-shift workers, neglecting shift frequency. In addition, inverted U-shaped associations were observed between years of shift work and health outcomes. This study provides insight into enhancing the health of shift workers by adjusting their work schedules.
There is a growing interest in the study of shift workers’ status and their health outcomes. A meta-analysis that evaluated seven studies with a total of 28,431 participants pointed out that shift workers were at an increased risk of poor mental health, particularly depression symptoms [13]. In addition, shift work, especially night shift work, was shown to be associated with a higher risk of chronic physical disorders, including diabetes, cardiovascular disease, and cancer [1,40]. Consistent with the findings of previous studies [41,42,43], current results also suggested that shift work was significantly associated with an increased risk of poor health outcomes among the general population in China.
Current research on the mechanisms by which shift work affects health is divided, including the interruption of the normal sleep–wake circadian cycle [44] and shift work tolerance [45,46]. In general speaking, shift work alters the circadian rhythm, causing significant adverse effects on biological functions [5,47]. Moreover, individual differences in tolerance to shift work may also cause distinct results of health outcomes [48]. Individual differences and baseline needs, especially neuroticism and autonomy, have been found to be strongly relevant to the tolerance of shift work in different occupations [49,50]. Irregular work reduces an individual’s ability to adapt to changes in the environment [51], these may be the mechanisms that lead to the link between shift work and chronic disease [22,52,53]. A fuller understanding of how shift work affects physical health remains to be explored.
In this study, we also explored the association between the frequency of shift work and health outcomes. Our results suggested that shift work participation, even with low frequency, may be associated with higher ORs of poor health outcomes. Previous studies have also found that shift work increased the risk of anxiety, depression, and coronary heart disease, neglecting shift frequency [5,54]. However, some studies have found that poor health outcomes increased following more frequent shift work [53]. Notably, we found that some health outcomes did not show a consistent linear relationship with shift frequency, such as cerebrovascular disease, chronic pain, and Parkinson’s disease, which had higher odds with lower shift frequency compared to more frequent shift work. Sleep, circadian rhythms, individual personality, neuroticism, and autonomy are all potential contributing factors to this outcome [49]. In addition, variations in study design, sample size, and work intensity may also be responsible [5,53,55]. In the meantime, it should be pointed out that the frequency of shift work in this study was not concise (merely divided into <1 and ≥1 night/week), and a precise estimate of the average number of shifts per month was needed.
When exploring the relationship between years of shift work and health outcomes, U-shaped associations were observed. Similarly, one study found that the relationship between shift work and cardiovascular disease risk appeared to emerge only after the first 5 years of exposure to shift work, after which it would gradually decrease [41]. Meanwhile, a study on the healthy age of female nurses in the U.S. also found that 1–5 years of shift work was a risk factor for healthy aging [21]. Work tolerance may be an explanation. The research has shown that shift work can lead to fatigue at the start of a shift, but an increased work capacity can help reduce fatigue and promote recovery from poor health outcomes [56]. Although the ORs for poor health outcomes decreased after five or more years, the risks still remained, suggesting that the structure of shift work needs to be improved to mitigate these hazards.
Our study has some strengths. To our knowledge, this cross-sectional study with a large sample of the general Chinese population provided an opportunity to observe the association between shift work and health outcomes more comprehensively. Our results suggested that there was no consistent linear relationship between shift frequency and health outcomes, and inverted U-shaped associations were observed between years of shift work and health outcomes. Our findings may provide more helpful information for policy making of shift work and recognition of high-risk disease progression in shift workers. Nonetheless, the study has several limitations as well. First, this was an online survey, and we used a convenience sampling method. Although the questionnaire was collected nationally, internet users are mostly highly educated young people, and the representativeness of our sample may be limited. Second, some other aspects of shift work such as the relationship with rotation work, overtime on holidays, frequency, pattern, or work type were not well detected in the current study. Third, this study was cross-sectional; hence, we were not able to explore the causal relationship between the frequency of shift work and adverse health outcomes. Fourth, the health outcomes we collected, including mental health and physical health, were derived from respondents’ self-reports rather than clinical diagnoses, which are subject to recall bias and may lead to error. And we investigated only common physical and mental illnesses, and a more detailed history of the disease was not explored among our participants.
5. Conclusions
Shift work is associated with a higher likelihood of poor health outcomes in the general population in China. The current research findings emphasize the necessity of paying attention to the health status of shift workers and it is encouraged to take effective measures to mitigate the negative impact of shift work and promote public health. The frequency, intensity, and duration of shift work, as well as the type of shift, need to be further considered in the following cohort studies in order to obtain a full picture of shift work.
Supplementary Materials
The following supporting information can be downloaded at https://www.mdpi.com/article/10.3390/brainsci14020145/s1: Table S1 Proportions of health outcomes and X2 in shift workers and non-shift workers. Table S2: The variance inflation factors of variables in the model.
Author Contributions
L.L., Z.Z. (Zhaohui Zhang), W.Y. and Y.B., proposed the topic and main idea. Y.H., L.S. and Y.B. designed the questionnaire and conducted the survey. N.G., Y.Z., Y.Y., Y.H., S.N., S.W. (Shuilin Wu) and N.Z. performed the data analysis and wrote the initial draft. N.G., Y.Z., Y.Y., Y.H., Y.G., S.W. (Sanwang Wang), S.N., N.Z., Z.Z. (Zhibo Zhang), S.S., K.Y., Z.Z. (Zhaohui Zhang), W.Y., Y.B. and L.L. commented on and revised the manuscript. L.L., Y.B., L.S., S.W. (Sanwang Wang), Y.G., Y.Z. and N.G. made the final version. All authors have read and agreed to the published version of the manuscript.
Funding
This study is supported by grants from National Programs for Brain Science and Brain-like Intelli-gence Technology of China: 2021ZD0200800; National Programs for Brain Science and Brain-like Intelligence Technology of China: 2021ZD0200700; the National Natural Science Foundation of China: 82288101; the National Natural Science Foundation of China: 82171514; Postgraduate Edu-cation Reform and Quality Improvement Project of Henan Province: YJS2021JD12.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of the Sixth Hospital of Peking University. (protocol code 2022-6-10-1 and date of approval: 10 June 2022).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data and statistical analysis plan in this study are available to others after publication. To access this data, please email one of the corresponding authors.
Conflicts of Interest
This is not an industry-supported study. None of the authors have potential conflicts of interest to be disclosed.
References
- Kecklund, G.; Axelsson, J. Health consequences of shift work and insufficient sleep. BMJ 2016, 355, i5210. [Google Scholar] [CrossRef] [PubMed]
- Liu, Q.; Shi, J.; Duan, P.; Liu, B.; Li, T.; Wang, C.; Li, H.; Yang, T.; Gan, Y.; Wang, X.; et al. Is shift work associated with a higher risk of overweight or obesity? A systematic review of observational studies with meta-analysis. Int. J. Epidemiol. 2018, 47, 1956–1971. [Google Scholar] [PubMed]
- Shan, Z.; Li, Y.; Zong, G.; Guo, Y.; Li, J.; Manson, J.E.; Hu, F.B.; Willett, W.C.; Schernhammer, E.S.; Bhupathiraju, S.N. Rotating night shift work and adherence to unhealthy lifestyle in predicting risk of type 2 diabetes: Results from two large US cohorts of female nurses. BMJ 2018, 363, k4641. [Google Scholar]
- Number of People Working Night Shifts up by More than 150,000 in 5 Years. Trade Union Congress. 12 July 2023. Available online: https://www.tuc.org.uk/news/number-people-working-night-shifts-more-150000-5-years (accessed on 12 October 2023).
- Wang, N.; Sun, Y.; Zhang, H.; Wang, B.; Chen, C.; Wang, Y.; Chen, J.; Tan, X.; Zhang, J.; Xia, F.; et al. Long-term night shift work is associated with the risk of atrial fibrillation and coronary heart disease. Eur. Heart J. 2021, 42, 4180–4188. [Google Scholar] [PubMed]
- Lunn, R.M.; Blask, D.E.; Coogan, A.N.; Figueiro, M.G.; Gorman, M.R.; Hall, J.E.; Hansen, J.; Nelson, R.J.; Panda, S.; Smolensky, M.H.; et al. Health consequences of electric lighting practices in the modern world: A report on the National Toxicology Program’s workshop on shift work at night, artificial light at night, and circadian disruption. Sci. Total Environ. 2017, 607–608, 1073–1084. [Google Scholar] [CrossRef]
- Jaradat, Y.; Birkeland Nielsen, M.; Kristensen, P.; Bast-Pettersen, R. Job satisfaction and mental health of Palestinian nurses with shift work: A cross-sectional study. Lancet 2018, 391, S50. [Google Scholar] [CrossRef]
- Xu, C.; Weng, Z.; Liang, J.; Liu, Q.; Zhang, X.; Xu, J.; Li, Q.; Zhou, Y.; GU, A. Shift work, genetic factors, and the risk of heart failure: A prospective study of the UK biobank. Mayo Clin. Proc. 2022, 97, 1134–1144. [Google Scholar] [CrossRef]
- Wu, Q.-J.; Sun, H.; Wen, Z.-Y.; Zhang, M.; Wang, H.-Y.; He, X.-H.; Jiang, Y.-T.; Zhao, Y.-H. Shift work and health outcomes: An umbrella review of systematic reviews and meta-analyses of epidemiological studies. J. Clin. Sleep Med. 2022, 18, 653–662. [Google Scholar] [CrossRef]
- Vetter, C.; Dashti, H.S.; Lane, J.M.; Anderson, S.G.; Schernhammer, E.S.; Rutter, M.K.; Saxena, R.; Scheer, F.A. Night shift work, genetic risk, and type 2 diabetes in the UK biobank. Diabetes Care 2018, 41, 762–769. [Google Scholar] [CrossRef]
- Barul, C.; Richard, H.; Parent, M.-E. Night-shift work and risk of prostate cancer: Results from a canadian case-control study, the prostate cancer and environment study. Am. J. Epidemiol. 2019, 188, 1801–1811. [Google Scholar]
- Wegrzyn, L.R.; Tamimi, R.M.; Rosner, B.A.; Brown, S.B.; Stevens, R.G.; Eliassen, A.H.; Laden, F.; Willett, W.C.; Hankinson, S.E.; Schernhammer, E.S. Rotating Night-Shift Work and the Risk of Breast Cancer in the Nurses’ Health Studies. Am. J. Epidemiol. 2017, 186, 532–540. [Google Scholar] [PubMed]
- Torquati, L.; Mielke, G.I.; Brown, W.J.; Burton, N.W.; Kolbe-Alexander, T.L. Shift work and poor mental health: A meta-analysis of longitudinal studies. Am. J. Public Health 2019, 109, e13–e20. [Google Scholar] [CrossRef] [PubMed]
- Shi, L.; Chen, S.-J.; Ma, M.-Y.; Bao, Y.-P.; Han, Y.; Wang, Y.-M.; Shi, J.; Vitiello, M.V.; Lu, L. Sleep disturbances increase the risk of dementia: A systematic review and meta-analysis. Sleep Med. Rev. 2018, 40, 4–16. [Google Scholar] [CrossRef] [PubMed]
- Kervezee, L.; Kosmadopoulos, A.; Boivin, D.B. Metabolic and cardiovascular consequences of shift work: The role of circadian disruption and sleep disturbances. Eur. J. Neurosci. 2020, 51, 396–412. [Google Scholar]
- Shi, J.; Bao, Y.; Lu, L.; Yan, W.; Ni, S.; Liu, C.; Yuan, J.; Zhao, Y.; Zeng, N.; Mei, H.; et al. Pattern and Associated Factors of Cognitive Failures in the General Chinese Population during the Early Stages of the COVID-19 Pandemic: A Cross-Sectional Study. Heart Mind 2023, 7, 224. [Google Scholar] [CrossRef]
- Varytis, A.; Giannouli, V. Workplace mobbing, group cohesion and intraindividual variables in nurses from a rural hospital in Northern Greece: A correlation study. Work 2023, 76, 1255–1261. [Google Scholar] [CrossRef]
- Ho, F.K.; Celis-Morales, C.; Gray, S.R.; Demou, E.; Mackay, D.; Welsh, P.; Katikireddi, S.V.; Sattar, N.; Pell, J.P. Association and pathways between shift work and cardiovascular disease: A prospective cohort study of 238,661 participants from UK Biobank. Int. J. Epidemiol. 2022, 51, 579–590. [Google Scholar] [CrossRef]
- Nabe-Nielsen, K.; Garde, A.H.; Albertsen, K.; Diderichsen, F. The moderating effect of work-time influence on the effect of shift work: A prospective cohort study. Int. Arch. Occup. Environ. Health 2011, 84, 551–559. [Google Scholar] [CrossRef]
- Hansen, J.; Lassen, C.F. Nested case-control study of night shift work and breast cancer risk among women in the Danish military. Occup. Environ. Med. 2012, 69, 551–556. [Google Scholar]
- Shi, H.; Huang, T.; Schernhammer, E.S.; Sun, Q.; Wang, M. Rotating night shift work and healthy aging after 24 years of follow-up in the nurses’ health study. JAMA Netw. Open 2022, 5, e2210450. [Google Scholar] [CrossRef]
- Berthelsen, M.; Pallesen, S.; Magerøy, N.; Tyssen, R.; Bjorvatn, B.; Moen, B.E.; Knardahl, S. Effects of psychological and social factors in shiftwork on symptoms of anxiety and depression in nurses: A 1-year follow-up. J. Occup. Environ. Med. 2015, 57, 1127–1137. [Google Scholar] [PubMed]
- Lee, H.Y.; Kim, M.S.; Kim, O.; Lee, I.-H.; Kim, H.-K. Association between shift work and severity of depressive symptoms among female nurses: The Korea Nurses’ Health Study. J. Nurs. Manag. 2016, 24, 192–200. [Google Scholar]
- Wang, X.-S.; Armstrong, M.E.G.; Cairns, B.J.; Key, T.J.; Travis, R.C. Shift work and chronic disease: The epidemiological evidence. Occup. Med. 2011, 61, 78–89. [Google Scholar]
- Shi, L.; Lu, Z.-A.; Que, J.-Y.; Huang, X.-L.; Liu, L.; Ran, M.-S.; Gong, Y.-M.; Yuan, K.; Yan, W.; Sun, Y.-K.; et al. Prevalence of and risk factors associated with mental health symptoms among the general population in china during the coronavirus disease 2019 pandemic. JAMA Netw. Open 2020, 3, e2014053. [Google Scholar] [CrossRef] [PubMed]
- Zheng, Y.-B.; Shi, L.; Lu, Z.-A.; Que, J.-Y.; Yuan, K.; Huang, X.-L.; Liu, L.; Wang, Y.-H.; Lu, Q.-D.; Wang, Z.; et al. Mental health status of late-middle-aged adults in China during the coronavirus disease 2019 pandemic. Front. Public Health 2021, 9, 643988. [Google Scholar] [CrossRef] [PubMed]
- Narducci, D.M.; Bertasi, T.G.O.; Bertasi, R.A.O.; Primiani, C.; Salinas, M.; Pujalte, G.G.A. Correlation of pre-race anxiety using the generalized anxiety disorder 2-item scale. Psychiatr. Q. 2022, 93, 463–471. [Google Scholar] [PubMed]
- Yuan, K.; Zheng, Y.-B.; Wang, Y.-J.; Sun, Y.-K.; Gong, Y.-M.; Huang, Y.-T.; Chen, X.; Liu, X.-X.; Zhong, Y.; Su, S.-Z.; et al. A systematic review and meta-analysis on prevalence of and risk factors associated with depression, anxiety and insomnia in infectious diseases, including COVID-19: A call to action. Mol. Psychiatry 2022, 27, 3214–3222. [Google Scholar] [CrossRef]
- Hughes, A.J.; Dunn, K.M.; Chaffee, T.; Bhattarai, J.J.; Beier, M. Diagnostic and clinical utility of the GAD-2 for screening anxiety symptoms in individuals with multiple sclerosis. Arch. Phys. Med. Rehabil. 2018, 99, 2045–2049. [Google Scholar]
- Morin, C.M.; Belleville, G.; Bélanger, L.; Ivers, H. The insomnia severity index: Psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep 2011, 34, 601–608. [Google Scholar] [CrossRef]
- Bastien, C.H.; Vallières, A.; Morin, C.M. Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Med. 2001, 2, 297–307. [Google Scholar] [CrossRef]
- He, X.Y.L.C.; Qian, J.; Cui, H.S.; Wu, W.Y. Reliability and validity of a generalized anxiety scale in general hospital outpatients. Shanghai Arch. Psychiatry 2010, 22, 200–203. [Google Scholar]
- Zhang, Y.-L.; Liang, W.; Chen, Z.-M.; Zhang, H.-M.; Zhang, J.-H.; Weng, X.-Q.; Yang, S.-C.; Zhang, L.; Shen, L.-J.; Zhang, Y.-L. Validity and reliability of patient health questionnaire-9 and patient health questionnaire-2 to screen for depression among college students in China. Asia-Pac. Psychiatry 2013, 5, 268–275. [Google Scholar] [PubMed]
- Yu, D.S. Insomnia severity index: Psychometric properties with Chinese community-dwelling older people. J. Adv. Nurs. 2010, 66, 2350–2359. [Google Scholar]
- Löwe, B.; Wahl, I.; Rose, M.; Spitzer, C.; Glaesmer, H.; Wingenfeld, K.; Schneider, A.; Brähler, E. A 4-item measure of depression and anxiety: Validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population. J. Affect. Disord. 2010, 122, 86–95. [Google Scholar] [CrossRef] [PubMed]
- Luo, Z.; Li, Y.; Hou, Y.; Zhang, H.; Liu, X.; Qian, X.; Jiang, J.; Wang, Y.; Liu, X.; Dong, X.; et al. Adaptation of the two-item generalized anxiety disorder scale (GAD-2) to Chinese rural population: A validation study and meta-analysis. Gen. Hosp. Psychiatry 2019, 60, 50–56. [Google Scholar]
- Seo, J.G.; Park, S.P. Validation of the Generalized Anxiety Disorder-7 (GAD-7) and GAD-2 in patients with migraine. J. Headache Pain 2015, 16, 97. [Google Scholar]
- Kim, J.H. Multicollinearity and misleading statistical results. Korean J. Anesthesiol. 2019, 72, 558–569. [Google Scholar]
- Zheng, Y.-B.; Sun, J.; Liu, L.; Zhao, Y.-M.; Yan, W.; Yuan, K.; Su, S.-Z.; Lu, Z.-A.; Huang, Y.-T.; Zeng, N.; et al. COVID-19 Vaccine-Related Psychological Stress Among General Public in China. Front. Psychiatry 2021, 12, 774504. [Google Scholar] [CrossRef]
- Wang, F.; Zhang, L.; Zhang, Y.; Zhang, B.; He, Y.; Xie, S.; Li, M.; Miao, X.; Chan, E.Y.Y.; Tang, J.L.; et al. Meta-analysis on night shift work and risk of metabolic syndrome. Obes. Rev. 2014, 15, 709–720. [Google Scholar] [CrossRef]
- Torquati, L.; Mielke, G.I.; Brown, W.J.; Kolbe-Alexander, T. Shift work and the risk of cardiovascular disease. a systematic review and meta-analysis including dose-response relationship. Scand. J. Work Environ. Health 2018, 44, 229–238. [Google Scholar]
- Joshi, A.; Sundar, I.K. Circadian disruption in night shift work and its association with chronic pulmonary diseases. Adv. Biol. 2023, 7, e2200292. [Google Scholar]
- Maidstone, R.J.; Turner, J.; Vetter, C.; Dashti, H.S.; Saxena, R.; Scheer, F.A.; Shea, S.A.; Kyle, S.D.; Lawlor, D.A.; Loudon, A.S.I.; et al. Night shift work is associated with an increased risk of asthma. Thorax 2021, 76, 53–60. [Google Scholar] [PubMed]
- Ganesan, S.; Magee, M.; Stone, J.E.; Mulhall, M.D.; Collins, A.; Howard, M.E.; Lockley, S.W.; Rajaratnam, S.M.W.; Sletten, T.L. The impact of shift work on sleep, alertness and performance in healthcare workers. Sci. Rep. 2019, 9, 4635. [Google Scholar] [CrossRef]
- Rajaratnam, S.M.; Howard, M.E.; Grunstein, R.R. Sleep loss and circadian disruption in shift work: Health burden and management. Med. J. Aust. 2013, 199, S11–S15. [Google Scholar] [PubMed]
- Ritonja, J.; Aronson, K.J.; Matthews, R.W.; Boivin, D.B.; Kantermann, T. Working time society consensus statements: Individual differences in shift work tolerance and recommendations for research and practice. Ind. Health 2019, 57, 201–212. [Google Scholar] [CrossRef]
- Ferri, P.; Guadi, M.; Marcheselli, L.; Balduzzi, S.; Magnani, D.; Di Lorenzo, R. The impact of shift work on the psychological and physical health of nurses in a general hospital: A comparison between rotating night shifts and day shifts. Risk Manag. Health Policy 2016, 9, 203–211. [Google Scholar] [CrossRef]
- Saksvik, I.B.; Bjorvatn, B.; Hetland, H.; Sandal, G.M.; Pallesen, S. Individual differences in tolerance to shift work—A systematic review. Sleep Med. Rev. 2011, 15, 221–235. [Google Scholar] [CrossRef]
- Saksvik-Lehouillier, I.; Sørengaard, T.A. Comparing shift work tolerance across occupations, work arrangements, and gender. Occup. Med. 2023, 73, 427–433. [Google Scholar] [CrossRef]
- Foldal, V.S.; Langvik, E.; Saksvik-Lehouillier, I. Personal dispositions and shift-work tolerance: A longitudinal study of municipality shift workers. J. Employ. Couns. 2016, 53, 174–186. [Google Scholar]
- Charrier, A.; Olliac, B.; Roubertoux, P.; Tordjman, S. Clock genes and altered sleep-wake rhythms: Their role in the development of psychiatric disorders. Int. J. Mol. Sci. 2017, 18, 938. [Google Scholar] [CrossRef]
- Durrington, H.J.; Gioan-Tavernier, G.O.; Maidstone, R.J.; Krakowiak, K.; Loudon, A.S.I.; Blaikley, J.F.; Fowler, S.J.; Singh, D.; Simpson, A.; Ray, D.W. Time of day affects eosinophil biomarkers in asthma: Implications for diagnosis and treatment. Am. J. Respir. Crit. Care Med. 2018, 198, 1578–1581. [Google Scholar] [CrossRef] [PubMed]
- Vetter, C.; Devore, E.E.; Wegrzyn, L.R.; Massa, J.; Speizer, F.E.; Kawachi, I.; Rosner, B.; Stampfer, M.J.; Schernhammer, E.S. Association between rotating night shift work and risk of coronary heart disease among women. JAMA 2016, 315, 1726–1734. [Google Scholar] [CrossRef] [PubMed]
- Xu, M.; Yin, X.; Gong, Y. Lifestyle factors in the association of shift work and depression and anxiety. JAMA Netw. Open 2023, 6, e2328798. [Google Scholar] [CrossRef] [PubMed]
- Meng, S.; Lu, L.; Yuan, K.; Yang, D.; Zhang, I. Facing Sleep and Mental Health Problems in the Covid-19 Era: What Shall We Do? Heart Mind 2022, 6, 203–206. [Google Scholar] [CrossRef]
- Driesen, K.; Jansen, N.W.; van Amelsvoort, L.G.; Kant, I. The mutual relationship between shift work and depressive complaints—A prospective cohort study. Scand. J. Work. Environ. Health 2011, 37, 402–410. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).