“Build Your Village”—Conducting the Village Test on Cognitively Impaired Patients: A First Journey into Alzheimerland
Abstract
1. Introduction
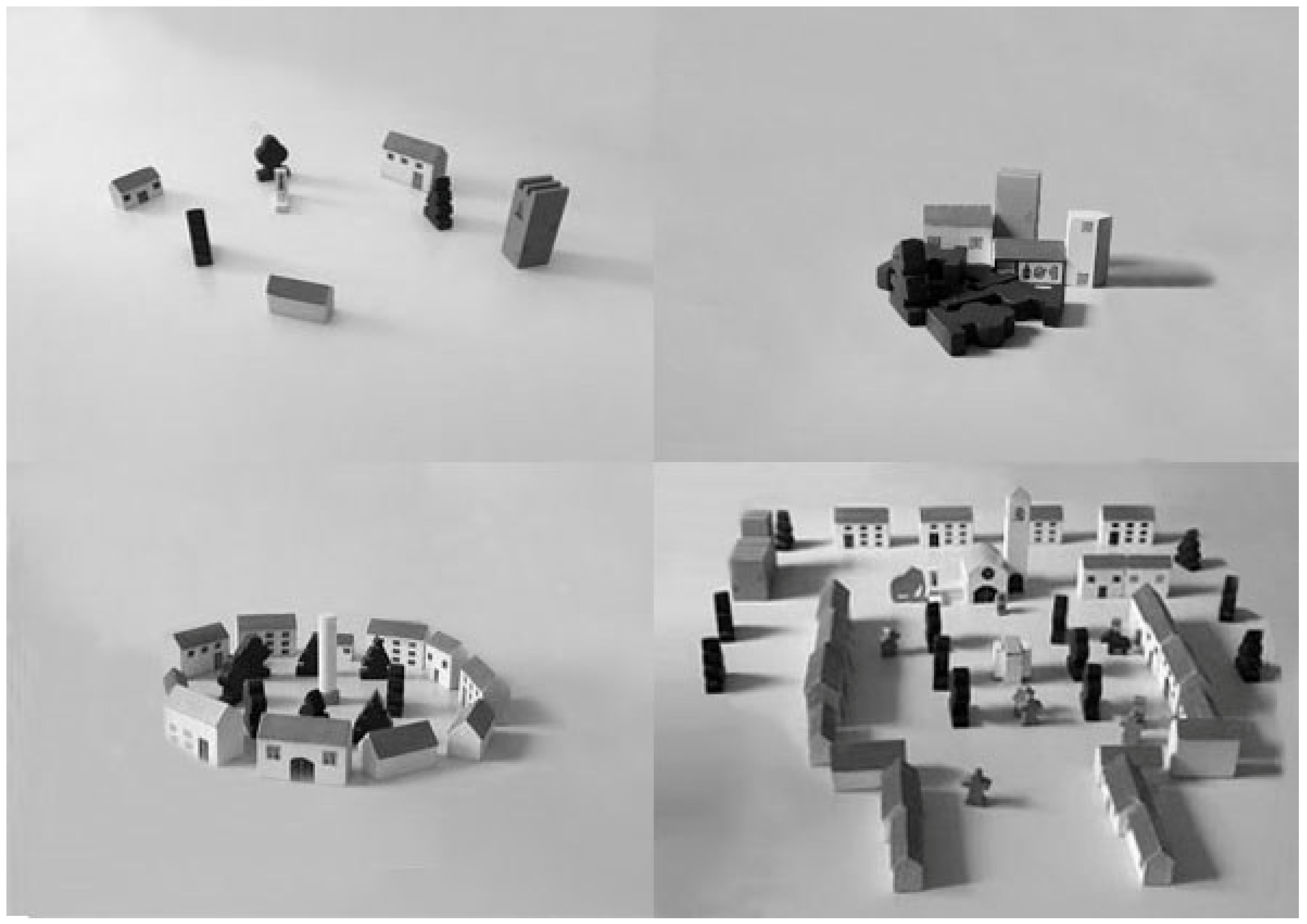
2. Materials and Methods
2.1. Inclusion and Exclusion Criteria
2.2. Procedures
2.3. Statistical Analysis
3. Results
3.1. VT Quantitative Analysis
3.2. VT Qualitative Analysis
3.3. Neuropsychological Assessment
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Alzheimer’s Association. 2023 Alzheimer’s Disease Facts and Figures. Alzheimers Dement 2023, 19, 1598–1695. [Google Scholar] [CrossRef]
- Larner, A.J. The Usage of Cognitive Screening Instruments: Test Characteristics and Suspected Diagnosis. In Cognitive Screening Instruments: A Practical Approach; Larner, A.J., Ed.; Springer: Berlin/Heidelberg, Germany, 2017; pp. 315–339. [Google Scholar]
- Stanzani Maserati, M.; Matacena, C.; Sambati, L.; Oppi, F.; Poda, R.; De Matteis, M.; Gallassi, R. The Tree-Drawing Test (Koch’s Baum Test): A Useful Aid to Diagnose Cognitive Impairment. Behav. Neurol. 2015, 2015, 534681. [Google Scholar] [CrossRef] [PubMed]
- Stanzani Maserati, M.; D’Onofrio, R.; Matacena, C.; Sambati, L.; Oppi, F.; Poda, R.; De Matteis, M.; Naldi, I.; Liguori, R.; Capellari, S. Human figure drawing distinguishes Alzheimer’s patients: A cognitive screening test study. Neurol. Sci. 2018, 39, 851–855. [Google Scholar] [CrossRef] [PubMed]
- Stanzani Maserati, M.; Mitolo, M.; Medici, F.; D’Onofrio, R.; Oppi, F.; Poda, R.; De Matteis, M.; Tonon, C.; Lodi, R.; Liguori, R.; et al. Color Choice Preference in Cognitively Impaired Patients: A Look Inside Alzheimer’s Disease through the Use of Lüscher Color Diagnostic. Front. Psychol. 2019, 10, 1951. [Google Scholar] [CrossRef]
- Stanzani Maserati, M.; Matacena, M.; Baccari, F.; Zenesini, C.; Gallassi, R.; Capellari, S.; Matacena, C. The Tree Drawing Test in Evolution: An Explorative Longitudinal Study in Alzheimer’s Disease. Am. J. Alzheimers Dis. Other Dement. 2022, 37, 15333175221129381. [Google Scholar] [CrossRef]
- Bonnet, M.; Belot, R.A.; Sanahuja, A.; Vandel, P. The House-Drawing Test: Using a projective test in assessment to differentiate normal from pathological ageing. Mediterr. J. Clin. Psychol. 2019, 7. [Google Scholar] [CrossRef]
- Robens, S.; Heymann, P.; Gienger, R.; Hett, A.; Müller, S.; Laske, C.; Loy, R.; Ostermann, T.; Elbing, U. The digital tree drawing test for screening of early dementia: An explorative study comparing healthy controls, patients with mild cognitive impairment, and patients with early dementia of the Alzheimer type. J. Alzheimers Dis. 2019, 68, 1561–1574. [Google Scholar] [CrossRef] [PubMed]
- Arthus, H. Il Villaggio. Test di Attività Creativa; Giunti O. S. Organizzazioni Speciali: Firenze, Italy, 1968. [Google Scholar]
- Marchisa, E.; Terenzio, G. Il Villaggio di H. Arthus nella Diagnosi di Strutture della Personalità; Giunti O. S. Organizzazioni Speciali: Firenze, Italy, 1968. [Google Scholar]
- Bosco, L.; Grandi, L.G. La Tecnica del Villaggio Nella Psicoterapia Infantile; Psiconline: Francavilla al Mare, Italy, 2014. [Google Scholar]
- Bosco, L. I luoghi del sé. Il Test del Villaggio. Applicazione del Metodo Evolutivo-Elementale Dall’infanzia All’età Adulta; Psiconline: Francavilla al Mare, Italy, 2018. [Google Scholar]
- Bosco, L. Principi di teoria adleriana applicati al Test del Villaggio. Simbolismo spaziale e psicodinamica nella Psicologia Individuale e nel Modello Evolutivo-Elementale. Riv. Psicol. Indiv. 2022, 92, 105–131. [Google Scholar]
- Nguyen, K.C. La création projective: Qu’est-ce que cela dit de l’intériorité? Psychol. Clin. 1989, 2, 80. [Google Scholar]
- Malandain, C.; Chambellan, S. Corps et configuration de l’espace dans une construction ludique. Bull. Psychol. 1999, 52, 21–25. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Arlington, VA, USA, 2013. [Google Scholar]
- Petersen, R.C.; Roberts, R.O.; Knopman, D.S.; Boeve, B.F.; Geda, Y.E.; Ivnik, R.J.; Smith, G.E.; Jack, C.R. Mild cognitive impairment: Ten years later. Arch. Neurol. 2009, 66, 1447–1455. [Google Scholar] [CrossRef]
- McKhann, G.M.; Knopman, D.S.; Chertkow, H.; Hyman, B.T.; Jack, C.R., Jr.; Kawas, C.H.; Klunk, W.E.; Koroshetz, W.J.; Manly, J.J.; Mayeux, R.; et al. The diagnosis of dementia due to Alzheimer’s disease: Recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011, 7, 263–269. [Google Scholar] [CrossRef]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. Mini-mental state. A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Measso, G.; Cavarzeran, F.; Zappalà, G.; Lebowitz, B.D.; Crook, T.H.; Pirozzolo, F.J.; Amaducci, L.A.; Massari, D.; Grigoletto, F. The Mini-Mental State Examination: Normative study of an Italian random sample. Dev. Neuropsychol. 1993, 9, 77–85. [Google Scholar] [CrossRef]
- Gallassi, R.; Lenzi, P.; Stracciari, A.; Lorusso, S.; Ciardulli, C.; Morreale, A.; Mussuto, V. Neuropsychological assessment of mental deterioration: Purpose of a brief battery and a probabilistic definition of ‘normality’ and ‘non-normality’. Acta Psychiatr. Scan. 1986, 75, 62–67. [Google Scholar] [CrossRef]
- Gallassi, R.; Morreale, A.; Di Sarro, R.; Lorusso, S. Value of clinical data and neuropsychological measures in probable Alzheimer’s disease. Arch. Gerontol. Geriatr. 2002, 34, 123–134. [Google Scholar] [CrossRef] [PubMed]
- Carlesimo, G.A.; Caltagirone, C.; Gainotti, G. The Mental Deterioration Battery: Normative data, diagnostic reliability and qualitative analyses of cognitive impairment. The Group for the Standardization of the Mental Deterioration Battery. Eur. Neurol. 1996, 36, 378–384. [Google Scholar] [CrossRef] [PubMed]
- Orsini, A.; Grossi, D.; Capitani, E.; Laiacona, M.; Papagno, C.; Vallar, G. Verbal and spatial immediate memory span: Normative data from 1355 adults and 1112 children. Ital. J. Neurol. Sci. 1987, 8, 539–548. [Google Scholar] [CrossRef]
- Spinnler, H.; Tognoni, G. Standardizzazione e taratura italiana di test neuropsicologici. Ital. J. Neurol. Sci. 1987, 6, 1–120. [Google Scholar]
- Caffarra, P.; Vezzadini, G.; Dieci, F.; Zonato, F. Una versione abbreviata del test di Stroop: Dati normativi nella popolazione italiana. Nuova Riv. Neurol. 2002, 12, 111–115. [Google Scholar]
- Caffarra, P.; Vezzadini, G.; Dieci, F.; Zonato, F.; Venneri, A. Rey-Osterrieth complex figure: Normative values in an Italian population sample. Neurol. Sci. 2002, 22, 443–447. [Google Scholar] [CrossRef] [PubMed]
- Monaco, M.; Costa, A.; Caltagirone, C.; Carlesimo, G.A. Forward and backward span for verbal and visuo-spatial data: Standardization and normative data from an Italian adult population. Neurol. Sci. 2013, 34, 749–754. [Google Scholar] [CrossRef] [PubMed]
- Gallassi, R.; Sambati, L.; Stanzani Maserati, M.; Poda, R.; Oppi, F.; De Matteis, M.; Marano, G. Simple verbal analogies test: Normative data on a short task exploring abstract thinking. Aging Clin. Exp. Res. 2014, 26, 67–71. [Google Scholar] [CrossRef] [PubMed]
- Novelli, G.; Papagno, C.; Capitani, E.; Laiacona, M. Tre test clinici di ricerca e produzione lessicale. Taratura su soggetti normali. Arch. Psicol. Neurol. Psichiatr. 1986, 47, 279–296. [Google Scholar]
- Ferracuti, S.; Cannoni, E.; Sacco, R.; Hufty, A.M. Contributi per un Assessment Neuropsicologico. Manuale Clinico; Giunti O. S. Organizzazioni Speciali: Firenze, Italy, 2007. [Google Scholar]
- Yu, K.; Lu, Z.; Stander, J. Quantile regression: Applications and current research areas. J. R. Stat. Soc. Ser. D Stat. 2003, 52, 331–350. [Google Scholar] [CrossRef]
- Benjamini, Y.; Yekutieli, D. The control of the false discovery rate in multiple hypothesis testing under dependency. Ann. Stat. 2001, 29, 1165–1188. [Google Scholar] [CrossRef]
| Cognitive Functions | Test |
|---|---|
| Global cognitive function indices | MMSE (range: 0–30) [19], MMSE corrected for age and education (range: 0–30; cut-off: <23.8) [20] |
| Brief Mental Deterioration Battery (BBDM) with Final Result (FR) (cut-off: <0) [21,22] | |
| Memory | Rey’s 15 Words *: immediate recall (range: 0–75; cut-off: <28.53); delayed recall * (range: 0–15; cut-off: <4.69) [23] |
| Immediate Visual Memory * (range: 0–22; cut-off: <13.85) [23] | |
| Digit Span Forward (range: 0–9; cut-off: <3.75) [24] | |
| Corsi Block-tapping Test (range: 0-infinite; cut-off: <3.75) [25] | |
| Rey–Osterrieth Complex Figure Test: delayed recall (range: 0–36; cut-off: <6.20) [27] | |
| Attention/Executive functions | Barrage Test * (time cut-off: ≥90; score cut-off: ≤9; errors cut-off: ≥2; result cut-off: >2.5) [21,22] Digit Span Backward (range: 0–9; cut-off: <2.65) [28] |
| Stroop Test (time cut-off: >27.5; errors cut-off: >7.5) [26] | |
| Abstract/concrete thinking | Analogies * (range: 0–20; cut-off: <13.92) [29] |
| Language | Verbal Fluency: phonemic (range: 0–infinite; cut-off: <17.35) [23]; semantic (range: 0–infinite; cut-off: <25) [30] |
| Constructional praxis | Copy Design: simple (range: 0–12; cut-off: <7.18) [23] |
| Rey–Osterrieth Complex Figure Test: direct copy (range: 0–36; cut-off: <28) [27] | |
| Visuospatial and perceptual functions | Judgment of Line Orientation Test (range: 0–30; cut-off: <19) [31] Street’s Completion Test (range: 0–14; cut-off: <2.25) [25] |
| AD n = 50 | MCI n = 28 | Controls n = 38 | p-Value | p-Value AD vs. MCI | p-Value AD vs. Ctrl | p-Value MCI vs. Ctrl | ||
|---|---|---|---|---|---|---|---|---|
| Age years | Mean (SD) Median [IQR] | 74.4 (9.5) 76 [70; 82] | 74 (6.1) 75.5 [72; 77.5] | 70.2 (8.4) 70 [63; 74] | 0.022 | 0.387 | 0.004 | 0.022 |
| Sex f | N (%) | 22 (44) | 12 (42.9) | 20 (52.6) | 0.654 | 0.922 | 0.422 | 0.432 |
| Education years | Mean (SD) Median [IQR] | 10.1 (4.5) 8 [5; 13] | 8.4 (3.6) 8 [5; 12.5] | 11.5 (3.8) 13 [8; 13] | 0.013 | 0.050 | 0.042 | 0.001 |
| AD n = 50 | MCI n = 28 | Controls n = 38 | p-Value | p-Value AD vs. MCI | p-Value AD vs. Ctrl | p-Value MCI vs. Ctrl | |
|---|---|---|---|---|---|---|---|
| Time of execution (s) Median [IQR] | 339 [188; 549] | 312.5 [209; 477.5] | 513.5 [368; 657] | 0.007 | 0.422 | 0.003 | 0.005 |
| Latency time (s) Median [IQR] | 3 [2; 5] | 3 [1.5; 7] | 2 [1; 3] | 0.273 | 0.424 | 0.077 | 0.079 |
| Village area Median [IQR] | 1009.5 [736; 1947] | 1705.5 [885; 2964] | 3350 [2303; 4543] | <0.001 | 0.025 | <0.001 | <0.001 |
| % used pieces/total Median [IQR] | 12.5 [6; 24] | 19 [12.5; 33] | 37 [24; 47] | <0.001 | 0.018 | <0.001 | <0.001 |
| Human figures Median [IQR] | 0 [0; 1] | 1.5 [0; 8] | 6 [3; 10] | <0.001 | 0.007 | <0.001 | 0.002 |
| Living pieces Median [IQR] | 8 [2; 20] | 16 [9.5; 30] | 36 [26; 46] | <0.001 | 0.008 | <0.001 | <0.001 |
| Non-living pieces Median [IQR] | 14.5 [8; 25] | 21 [15.5; 43] | 35 [21; 50] | <0.001 | 0.028 | <0.001 | 0.029 |
| Living/non-living ratio Median [IQR] | 0.5 [0.2; 1] | 0.7 [0.5; 1.1] | 1.1 [0.7; 1.4] | <0.001 | 0.115 | <0.001 | 0.005 |
| Dynamic pieces Median [IQR] | 0 [0; 1] | 1 [0; 4] | 2.5 [1; 5] | <0.001 | 0.014 | <0.001 | 0.034 |
| Static pieces Median [IQR] | 21.5 [12; 38] | 32.5 [22.5; 59] | 58.5 [39; 76] | <0.001 | 0.019 | <0.001 | 0.004 |
| Dynamic/static ratio Median [IQR] | 0 [0; 0] | 0 [0; 0.1] | 0.1 [0; 0.1] | 0.019 | 0.018 | <0.001 | 0.229 |
| Coeff | 95% CI | |
|---|---|---|
| Time of execution | ||
| AD | −155.13 | −234.33; −109.25 |
| MCI | −181.63 | −310.6; −60.85 |
| Latency time | ||
| AD | 0.93 | 0.11; 1.41 |
| MCI | 0.89 | 0.32; 1.56 |
| Village area | ||
| AD | −2142.68 | −2522.46; −1101.65 |
| MCI | −1314.76 | −2054.6; −488.97 |
| % used pieces/total | ||
| AD | −22.9 | −28.98; −15.62 |
| MCI | −16.26 | −18.93; −6.52 |
| Human figures | ||
| AD | −4.89 | −7.86; −3.88 |
| MCI | −3.97 | −7.74; −1.36 |
| Living pieces | ||
| AD | −23.86 | −29.25; −19.6 |
| MCI | −15.76 | −20.27; −8.43 |
| Non-living pieces | ||
| AD | −20.2 | −31.35; −11.78 |
| MCI | −13.6 | −24.17; −3.1 |
| Living/non-living ratio | ||
| AD | −0.68 | −0.78; −0.33 |
| MCI | −0.45 | −0.62; −0.10 |
| Dynamic pieces | ||
| AD | −2 | −3.5; −1.13 |
| MCI | −1 | −2.6; 0.43 |
| Static pieces | ||
| AD | −37.26 | −41.01; −25.85 |
| MCI | −23.36 | −31.14; −10.01 |
| Dynamic/static ratio | ||
| AD | −0.1 | −0.1; −0.01 |
| AD | MCI | Controls | p-Value | p-Value | p-Value | p-Value | |
|---|---|---|---|---|---|---|---|
| n = 50 | n = 28 | n = 38 | AD vs. MCI | AD vs. Ctrl | MCI vs. Ctrl | ||
| MMSEc | |||||||
| Mean (SD) | 18.7 (5.2) | 24.5 (3.5) | 27.9 (1.4) | <0.001 | <0.001 | <0.001 | <0.001 |
| Median [IQR] | 19 [16; 22.7] | 25.4 [22.5; 27.6] | 28.1 [27.1; 29] | ||||
| BBDM Final Result | |||||||
| Mean (SD) | −0.7 (1.3) | 1.1 (0.9) | 2.4 (0.5) | <0.001 | <0.001 | <0.001 | <0.001 |
| Median [IQR] | −1 [−1.4; 0.4] | 1.2 [0.8; 1.6] | 2.4 [1.9; 2.7] | ||||
| Rey’s 15 Words imm_c | |||||||
| Mean (SD) | 21.6 (5.6) | 33.6 (6.9) | 43.3 (6.7) | <0.001 | <0.001 | <0.001 | <0.001 |
| Median [IQR] | 21.2 [17.1; 26.2] | 33 [30.4; 37.6] | 44.2 [36.4; 49.1] | ||||
| Rey’s 15 Words del_c | |||||||
| Mean (SD) | 2.4 (1.4) | 5.6 (2.5) | 8.8 (2.1) | <0.001 | <0.001 | <0.001 | <0.001 |
| Median [IQR] | 2.8 [1.6; 3.3] | 5.5 [4; 7.2] | 8.3 [7.3; 10.4] | ||||
| Imm Visual Mem_c | |||||||
| Mean (SD) | 15.3 (4.5) | 19 (2.5) | 20 (1.9) | <0.001 | 0.001 | <0.001 | 0.074 |
| Median [IQR] | 14.9 [12.3; 18.9] | 19.2 [17.7; 20.5] | 20 [19.5; 21.4] | ||||
| Digit Span Forward_c | |||||||
| Mean (SD) | 4.9 (1.2) | 5.4 (1) | 6.3 (1) | <0.001 | 0.066 | <0.001 | 0.001 |
| Median [IQR] | 5.1 [4.1; 5.8] | 5.6 [4.8; 6.3] | 6.2 [5.7; 6.8] | ||||
| Corsi Block-tapping_c | |||||||
| Mean (SD) | 4.2 (4.3) | 4.8 (0.8) | 5.3 (1.2) | <0.001 | <0.001 | <0.001 | 0.109 |
| Median [IQR] | 3.6 [2.9; 4.2] | 4.7 [4.3; 5.4] | 5.1 [4.4; 6] | ||||
| Rey Fig delayed rec_c | |||||||
| Mean (SD) | 7 (4) | 13.8 (8.2) | 20 (5.8) | <0.001 | <0.001 | <0.001 | <0.001 |
| Median [IQR] | 6.6 [4.5; 9.5] | 11.6 [7.9; 19.8] | 19.2 [16.3; 21.8] | ||||
| Barrage time | |||||||
| Mean (SD) | 109.7 (50.6) | 64 (33) | 46.5 (10.6) | <0.001 | <0.001 | <0.001 | 0.006 |
| Median [IQR] | 100 [65; 164] | 58 [43; 66.5] | 45 [38; 54] | ||||
| Digit Span Back_c | |||||||
| Mean (SD) | 3.1 (1.2) | 3.9 (1.3) | 5.5 (6) | <0.001 | 0.021 | <0.001 | 0.005 |
| Median [IQR] | 3.1 [2.7; 3.6] | 3.7 [3; 4.6] | 4.6 [3.7; 5.3] | ||||
| Stroop time_c | |||||||
| Mean (SD) | 47.9 (51.3) | 60.5 (148.5) | 15.9 (7.9) | <0.001 | 0.499 | <0.001 | <0.001 |
| Median [IQR] | 38.4 [14.3; 56.3] | 36.1 [19.8; 46.9] | 15.3 [9.8; 21.3] | ||||
| Stroop err_c | |||||||
| Mean (SD) | 14.4 (9.9) | 2.1 (5.2) | −1 (2.2) | <0.001 | <0.001 | <0.001 | 0.034 |
| Median [IQR] | 14.4 [4.6; 23.8] | 0.6 [−1.7; 3.2] | −1 [−1.5; −0.5] | ||||
| Analogies_c | |||||||
| Mean (SD) | 9.4 (5.1) | 14.1 (4.4) | 18.2 (1.7) | <0.001 | 0.001 | <0.001 | <0.001 |
| Median [IQR] | 9.8 [5.7; 13.1] | 14.8 [12.2; 17.4] | 18.1 [16.7; 19.1] | ||||
| Phonemic fluency_c | |||||||
| Mean (SD) | 15.7 (8.8) | 26.2 (10.9) | 34 (7.8) | <0.001 | <0.001 | <0.001 | 0.001 |
| Median [IQR] | 16 [11.2; 22.4] | 24.9 [16.2; 33.4] | 32.8 [28.3; 40.3] | ||||
| Semantic fluency_c | |||||||
| Mean (SD) | 20.1 (6.8) | 31.7 (11.2) | 43.2 (6.2) | <0.001 | <0.001 | <0.001 | <0.001 |
| Median [IQR] | 21 [17; 24] | 32 [25; 38.5] | 42.5 [39; 47] | ||||
| Copy Design_c | |||||||
| Mean (SD) | 9.3 (2.4) | 11.1 (1.8) | 11.6 (1) | <0.001 | 0.001 | <0.001 | 0.116 |
| Median [IQR] | 9.8 [7.9; 11.1] | 11.6 [10.1; 12.3] | 11.7 [11.1; 12.4] | ||||
| Rey Fig copy_c | |||||||
| Mean (SD) | 21.5 (11.3) | 32.1 (5.9) | 36.5 (1.7) | <0.001 | 0.001 | <0.001 | 0.001 |
| Median [IQR] | 24 [10.9; 31.5] | 33.7 [31.4; 36] | 36.8 [36; 37.3] | ||||
| Judg of Line Orient_c | |||||||
| Mean (SD) | 16 (8.8) | 22.7 (4.2) | 27.5 (3.7) | <0.001 | 0.007 | <0.001 | <0.001 |
| Median [IQR] | 18 [6; 23] | 23.5 [19.5; 25.5] | 28 [25; 30] | ||||
| Street’s Completion_c | |||||||
| Mean (SD) | 4.1 (2) | 5.6 (2) | 7.3 (1.7) | <0.001 | 0.003 | <0.001 | 0.002 |
| Median [IQR] | 4 [2.8; 5.3] | 5.8 [4.6; 6.9] | 7.3 [6.5; 8.5] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stanzani-Maserati, M.; De Matteis, M.; Bosco, L.; Baccari, F.; Zenesini, C.; Mitolo, M.; La Morgia, C.; Gallassi, R.; Capellari, S. “Build Your Village”—Conducting the Village Test on Cognitively Impaired Patients: A First Journey into Alzheimerland. Brain Sci. 2024, 14, 523. https://doi.org/10.3390/brainsci14060523
Stanzani-Maserati M, De Matteis M, Bosco L, Baccari F, Zenesini C, Mitolo M, La Morgia C, Gallassi R, Capellari S. “Build Your Village”—Conducting the Village Test on Cognitively Impaired Patients: A First Journey into Alzheimerland. Brain Sciences. 2024; 14(6):523. https://doi.org/10.3390/brainsci14060523
Chicago/Turabian StyleStanzani-Maserati, Michelangelo, Maddalena De Matteis, Luca Bosco, Flavia Baccari, Corrado Zenesini, Micaela Mitolo, Chiara La Morgia, Roberto Gallassi, and Sabina Capellari. 2024. "“Build Your Village”—Conducting the Village Test on Cognitively Impaired Patients: A First Journey into Alzheimerland" Brain Sciences 14, no. 6: 523. https://doi.org/10.3390/brainsci14060523
APA StyleStanzani-Maserati, M., De Matteis, M., Bosco, L., Baccari, F., Zenesini, C., Mitolo, M., La Morgia, C., Gallassi, R., & Capellari, S. (2024). “Build Your Village”—Conducting the Village Test on Cognitively Impaired Patients: A First Journey into Alzheimerland. Brain Sciences, 14(6), 523. https://doi.org/10.3390/brainsci14060523








