A Computational Model of Deep Brain Stimulation for Parkinson’s Disease Tremor and Bradykinesia
Abstract
1. Introduction
2. Materials and Methods
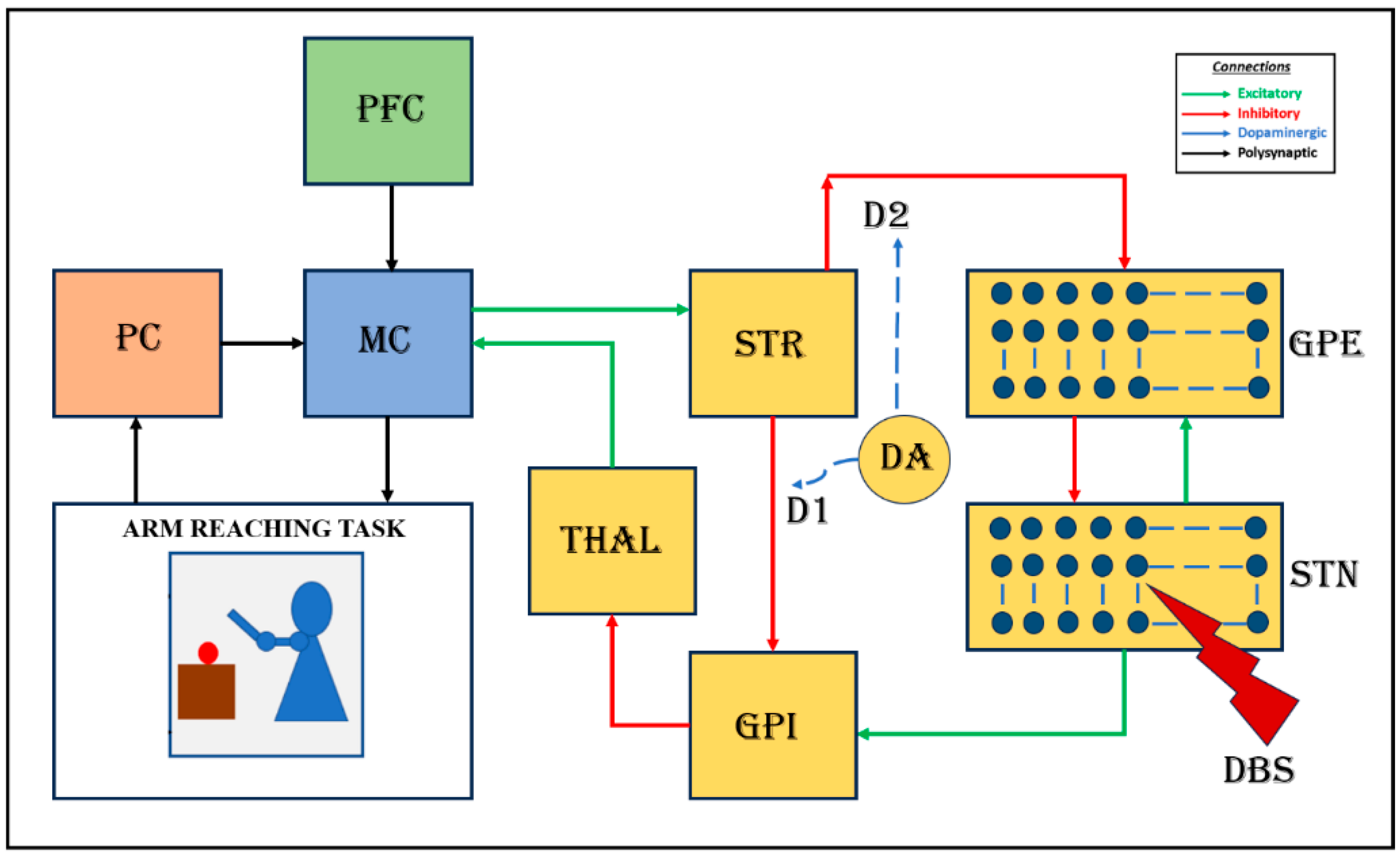
2.1. Cortico-Basal Ganglia Model
2.1.1. MC–BG Interaction
2.1.2. The STN–GPe Subsystem
2.1.3. Simulating the PD Condition
2.1.4. The STN-to-GPi Connection
2.1.5. The BG-to-MC Connection
2.2. Parameter Selection
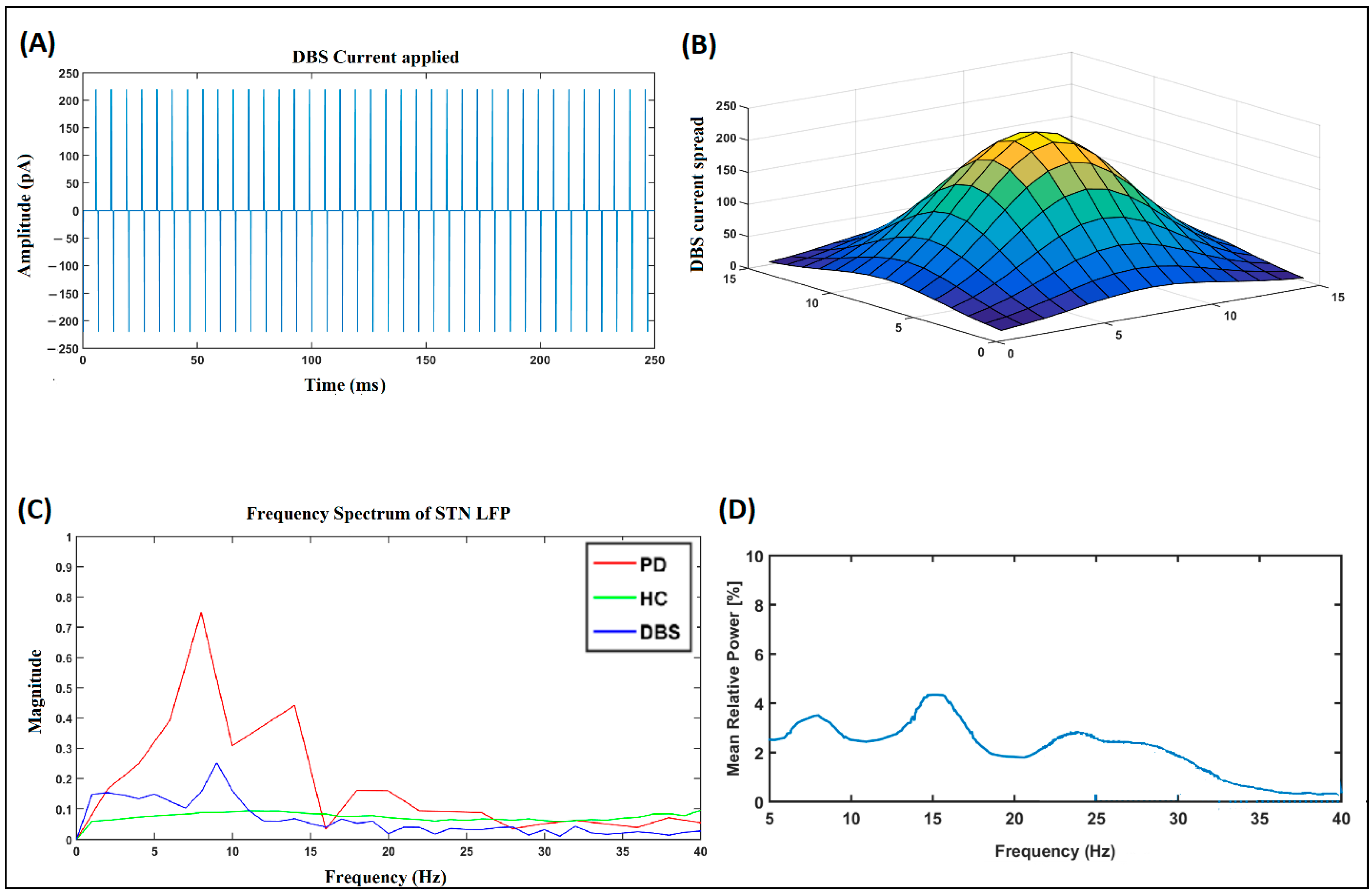
2.3. DBS Effect
2.4. Informing the Model Using Experimental Data
- (i).
- Data Source: The experimental reaching performance data from [61] was used for behavior modeling.
- (ii).
- Experimental Task: The participants were asked to reach and grasp a ball that was placed a certain distance away from them as quickly as possible.
- (iii).
- Parameter Tuning for HC and PD Groups: Model parameters were adjusted to replicate the reaching performance of healthy controls (HC).
- (iv).
- (v).
- (vi).
- The network dynamics were then correlated with the symptoms.
3. Results
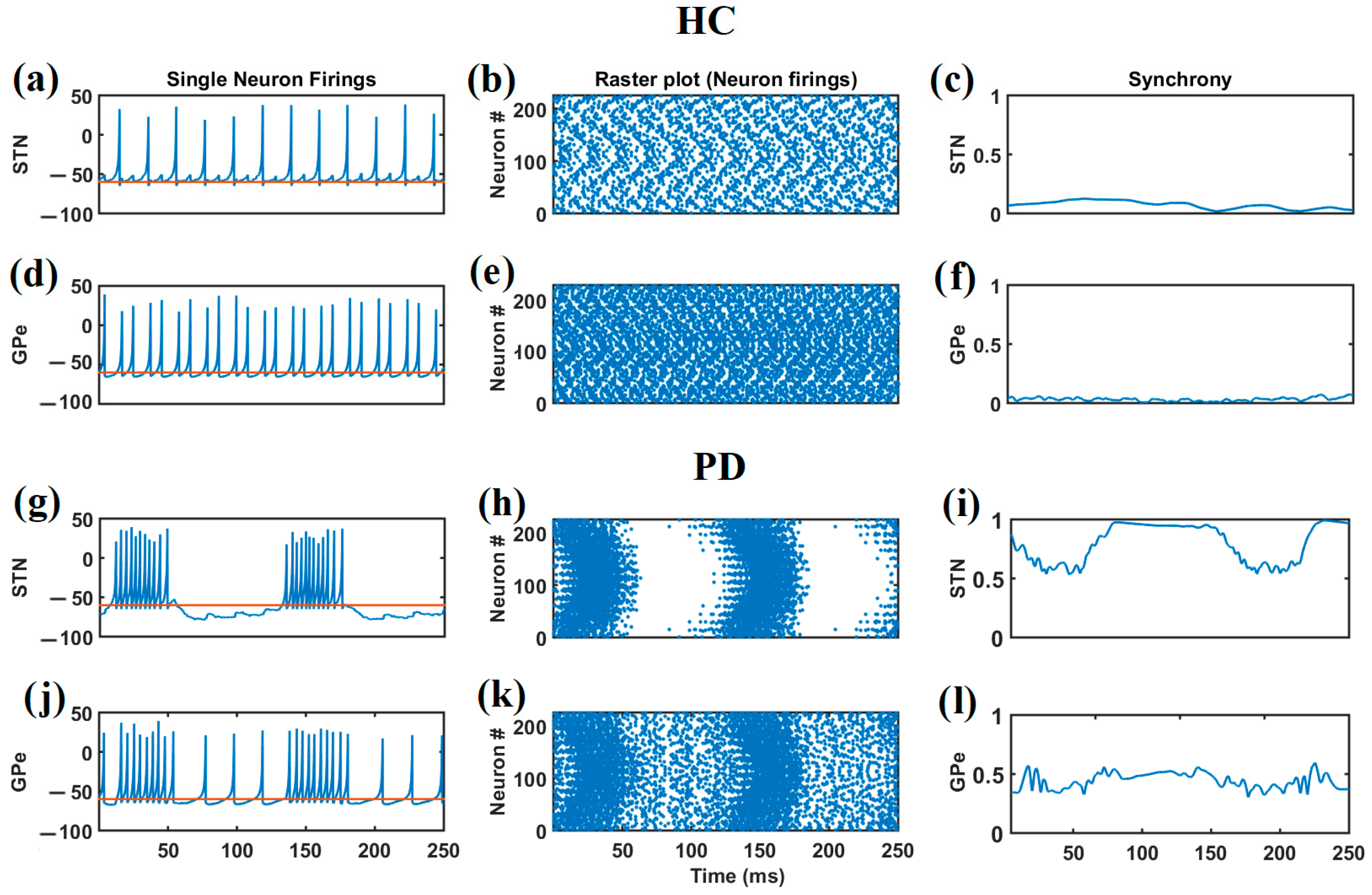
3.1. Parameters Controlling the Firing Patterns and Synchrony in STN–GPe
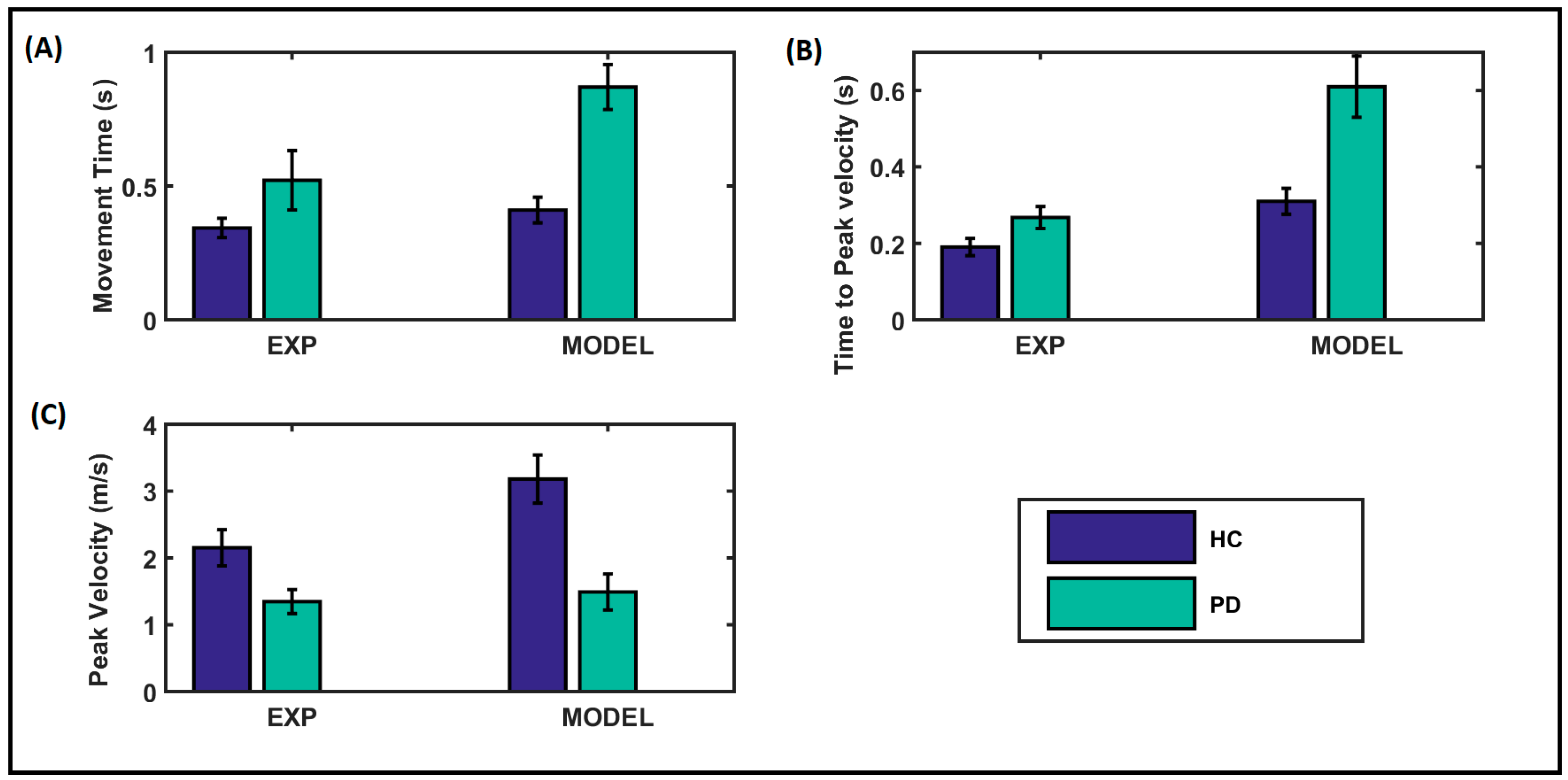
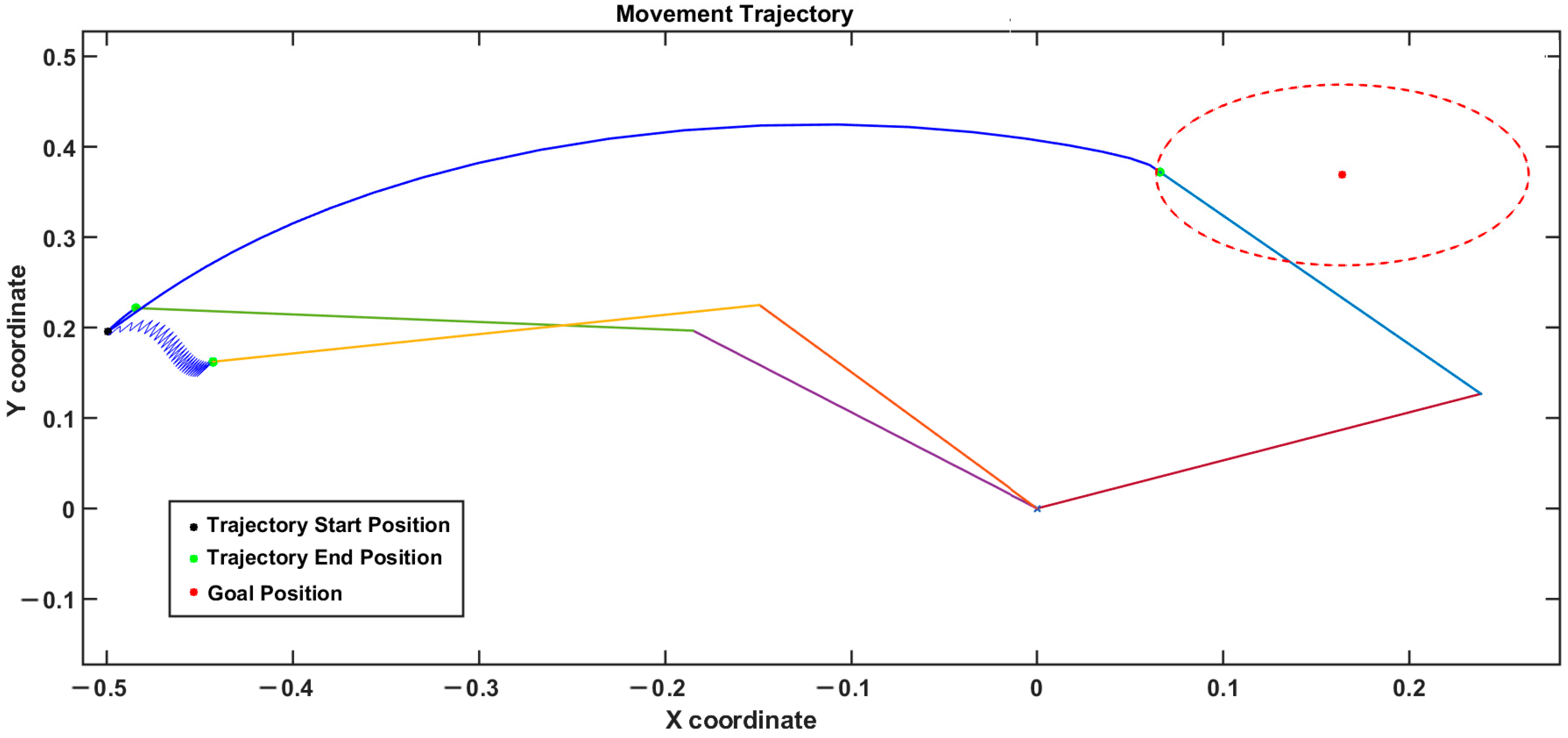
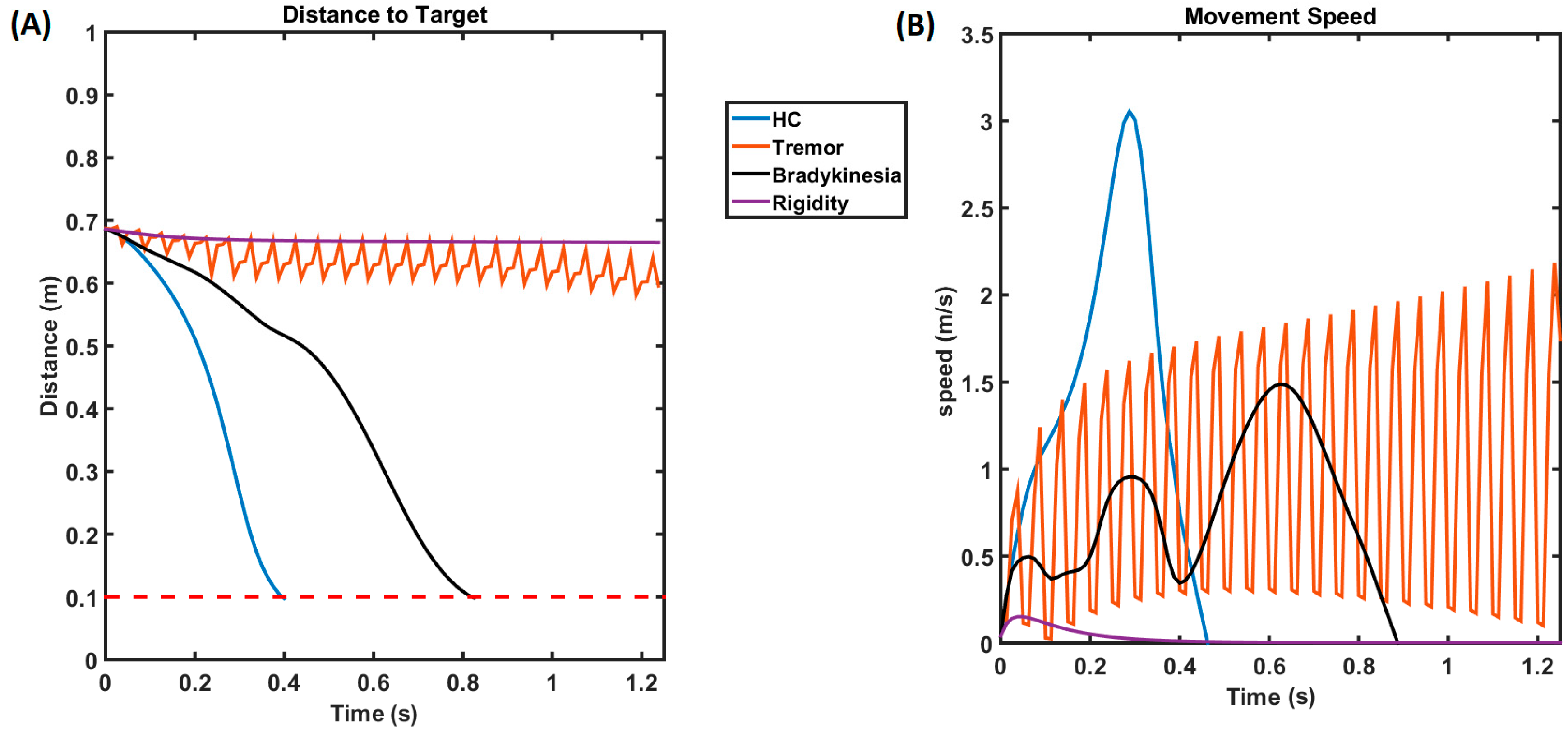
3.2. Kinematic Performance of Arm Reaching
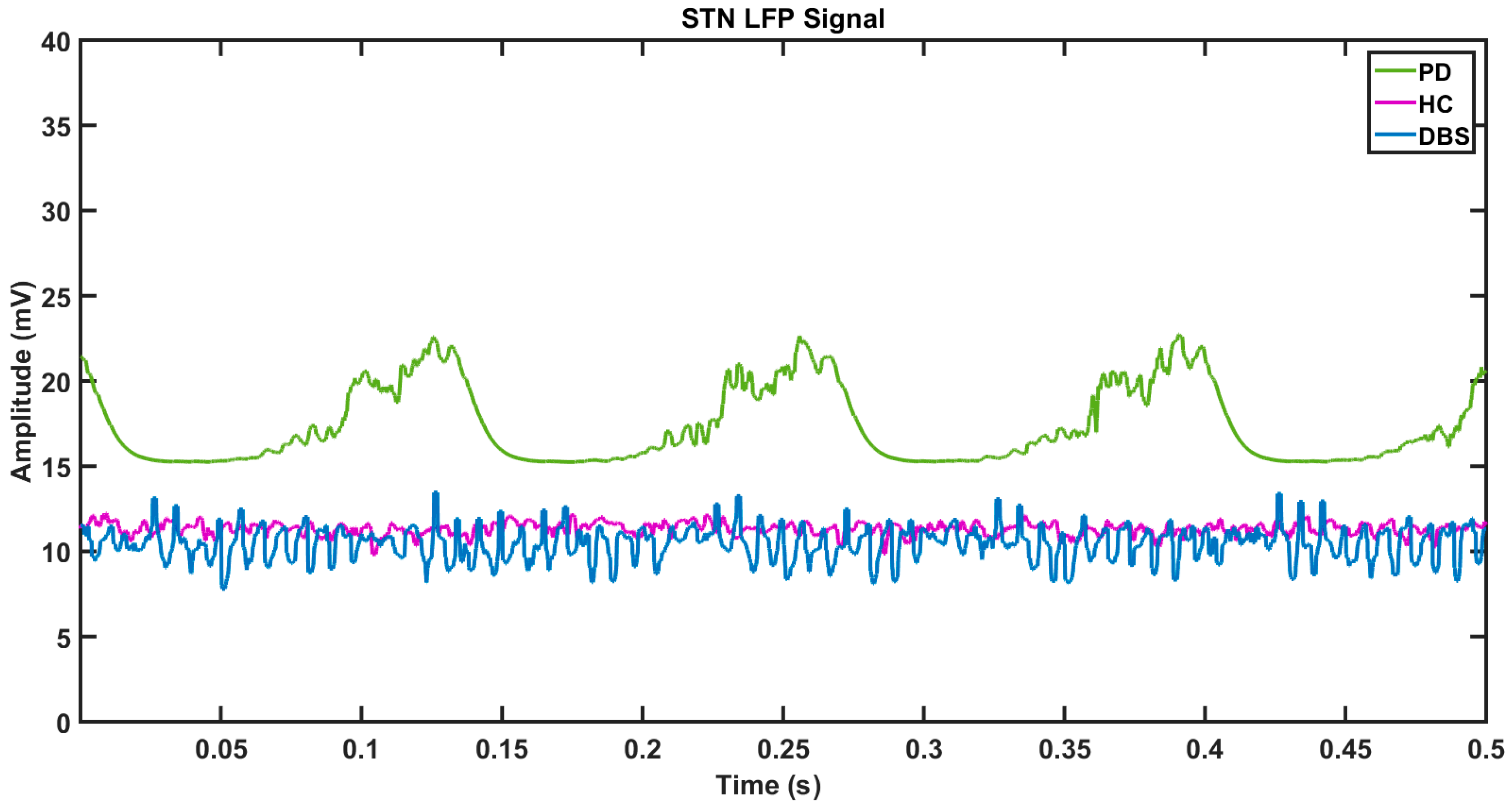
3.3. Neuronal Firings and Synchrony during Healthy and PD Conditions
3.4. Arm Reaching Performance under Healthy and PD Conditions
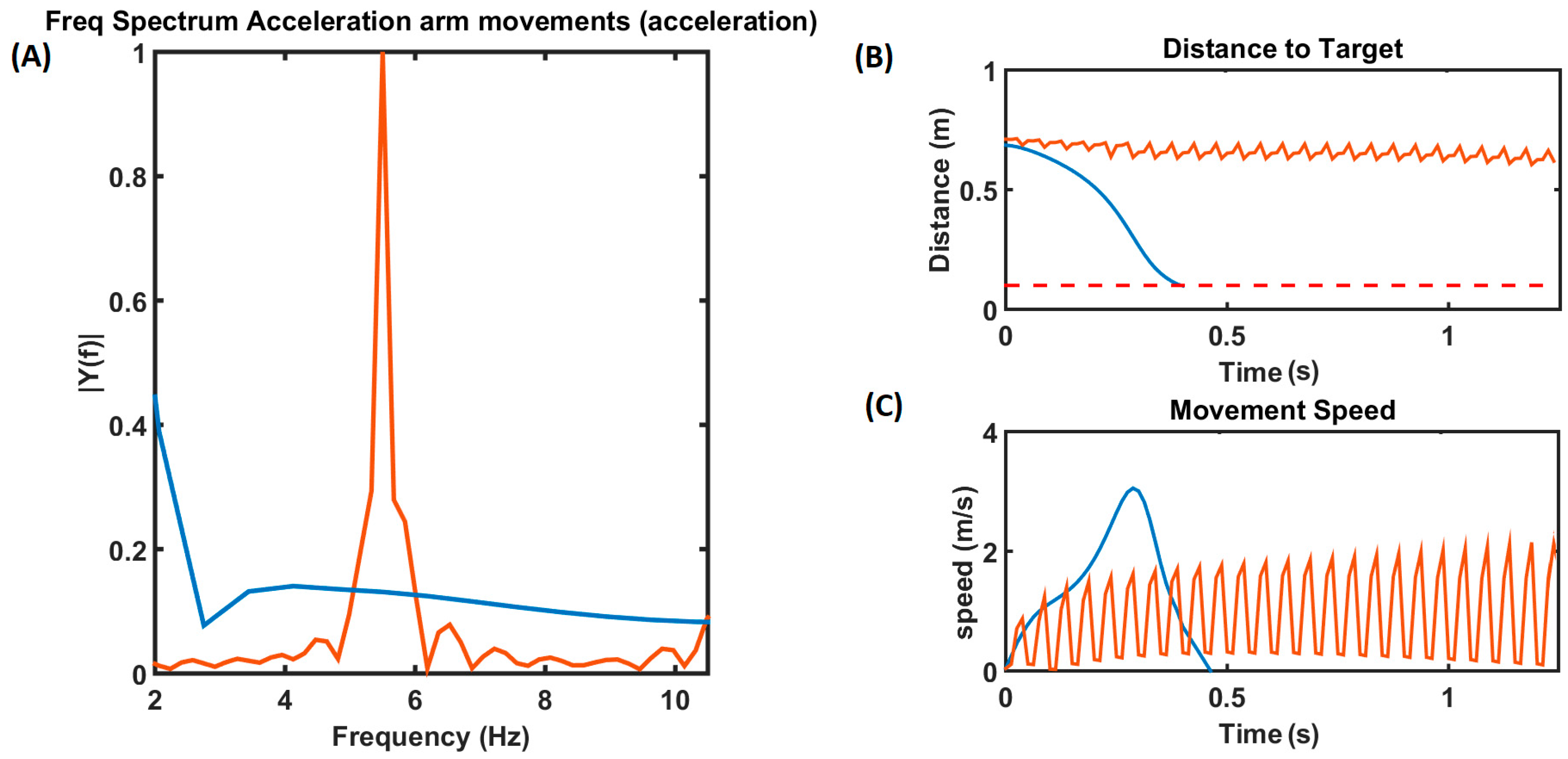
3.5. Simulating Deep Brain Stimulation (DBS) Effect
3.6. Effect of DBS on PD Symptoms (Tremor and Bradykinesia)
3.7. Comparison with Experimental Data
4. Discussion
5. Conclusions and Future Work
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Muddapu, V.R.; Chakravarthy, V.S. Influence of energy deficiency on the subcellular processes of substantia nigra pars compacta cell for understanding Parkinsonian neurodegeneration. Sci. Rep. 2021, 11, 1754. [Google Scholar] [CrossRef]
- Gonzalez-Rodriguez, P.; Zampese, E.; Surmeier, D.J. Selective neuronal vulnerability in Parkinson’s disease. In Progress in Brain Research; Elsevier B.V.: Amsterdam, The Netherlands, 2020; Volume 252, pp. 61–89. [Google Scholar] [CrossRef]
- Marino, B.L.; de Souza, L.R.; Sousa, K.P.; Ferreira, J.V.; Padilha, E.C.; da Silva, C.H.; Taft, C.A.; Hage-Melim, L.I. Parkinson’s Disease: A review from pathophysiology to treatment. Mini-Rev. Med. Chem. 2020, 20, 754–767. [Google Scholar] [CrossRef]
- Morley, J.F.; Duda, J.E. Olfaction as a biomarker in Parkinson’s disease. Biomarkers Med. 2010, 4, 661–670. [Google Scholar] [CrossRef] [PubMed]
- Fullard, M.E.; Morley, J.F.; Duda, J.E. Olfactory dysfunction as an early biomarker in Parkinson’s disease. Neurosci. Bull. 2017, 33, 515–525. [Google Scholar] [CrossRef] [PubMed]
- Balestrino, R.; Schapira, A.H.V. Parkinson disease. Eur. J. Neurol. 2020, 27, 27–42. [Google Scholar] [CrossRef] [PubMed]
- Goldman, J.G.; Guerra, C.M. Treatment of nonmotor symptoms associated with Parkinson disease. Neurol. Clin. 2020, 38, 269–292. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, M.J.; Okun, M.S. Diagnosis and treatment of Parkinson disease: A Review. JAMA—J. Am. Med. Assoc. 2020, 323, 548–560. [Google Scholar] [CrossRef] [PubMed]
- Muddapu, V.R.; Dharshini, S.A.P.; Chakravarthy, V.S.; Gromiha, M.M. Neurodegenerative Diseases—Is Metabolic Deficiency the Root Cause? Front. Neurosci. 2020, 14, 213. [Google Scholar] [CrossRef] [PubMed]
- Surmeier, D.J. Determinants of dopaminergic neuron loss in Parkinson’s disease. FEBS J. 2018, 285, 3657–3668. [Google Scholar] [CrossRef] [PubMed]
- Michel, P.P.; Hirsch, E.C.; Hunot, S. Understanding dopaminergic cell death pathways in Parkinson disease. Neuron 2016, 90, 675–691. [Google Scholar] [CrossRef] [PubMed]
- Cotzias, G.C.; Van Woert, M.H.; Schiffer, L.M. Aromatic amino acids and modification of Parkinsonism. N. Engl. J. Med. 1967, 276, 374–379. [Google Scholar] [CrossRef] [PubMed]
- Nagatsu, T.; Sawada, M. L-dopa therapy for Parkinson’s disease: Past, present, and future. Park. Relat. Disord. 2009, 15, S3–S8. [Google Scholar] [CrossRef]
- Pollak, P.; Benabid, A.L.; Gross, C.; Gao, D.M.; Laurent, A.; Benazzouz, A.; Hoffmann, D.; Gentil, M.; Perret, J. Effects of the stimulation of the subthalamic nucleus in Parkinson disease. Rev. Neurol. 1993, 149, 175–176. [Google Scholar] [PubMed]
- Bechtereva, N.; Bondartchuk, A.; Smirnov, V.; Meliutcheva, L.; Shandurina, A. Method of electrostimulation of the deep brain structures in treatment of some chronic diseases. Ster. Funct. Neurosurg. 1975, 37, 136–140. [Google Scholar] [CrossRef] [PubMed]
- Andrade, P.; Carrillo-Ruiz, J.D.; Jiménez, F. A systematic review of the efficacy of globus pallidus stimulation in the treatment of Parkinson’s disease. J. Clin. Neurosci. 2009, 16, 877–881. [Google Scholar] [CrossRef] [PubMed]
- Ng, J.H.; See, A.A.Q.; Xu, Z.; King, N.K.K. Longitudinal medication profile and cost savings in Parkinson’s disease patients after bilateral subthalamic nucleus deep brain stimulation. J. Neurol. 2020, 267, 2443–2454. [Google Scholar] [CrossRef] [PubMed]
- Welter, M.L.; Houeto, J.L.; du Montcel, S.T.; Mesnage, V.; Bonnet, A.M.; Pillon, B.; Arnulf, I.; Pidoux, B.; Dormont, D.; Cornu, P.; et al. Clinical predictive factors of subthalamic stimulation in Parkinson’s disease. Brain 2002, 125, 575–583. [Google Scholar] [CrossRef] [PubMed]
- Muthuraman, M.; Koirala, N.; Ciolac, D.; Pintea, B.; Glaser, M.; Groppa, S.; Tamás, G.; Groppa, S. Deep brain stimulation and L-DOPA therapy: Concepts of action and clinical applications in Parkinson’s disease. Front. Neurol. 2018, 9, 711. [Google Scholar] [CrossRef]
- Lozano, A.M.; Dostrovsky, J.; Chen, R.; Ashby, P. Deep brain stimulation for Parkinson’s disease: Disrupting the disruption. Lancet Neurol. 2002, 1, 225–231. [Google Scholar] [CrossRef]
- Hefti, F.; Melamed, E. l-DOPA’s mechanism of action in Parkinson’s disease. Trends Neurosci. 1980, 3, 229–231. [Google Scholar] [CrossRef]
- Chakravarthy, V.S.; Moustafa, A.A. Computational neuroscience models of the basal ganglia. In Cognitive Science and Technology; Springer: Singapore, 2018; Volume 15. [Google Scholar] [CrossRef]
- Wang, Z.; Hu, B.; Zhu, L.; Lin, J.; Xu, M.; Wang, D. The possible mechanism of direct feedback projections from basal ganglia to cortex in beta oscillations of Parkinson’s disease: A theoretical evidence in the competing resonance model. Commun. Nonlinear Sci. Numer. Simul. 2023, 120, 107142. [Google Scholar] [CrossRef]
- Brown, P. Oscillatory nature of human basal ganglia activity: Relationship to the pathophysiology of Parkinson’s disease. Mov. Disord. 2003, 18, 357–363. [Google Scholar] [CrossRef]
- Hammond, C.; Bergman, H.; Brown, P. Pathological synchronization in Parkinson’s disease: Networks, models and treatments. Trends Neurosci. 2007, 30, 357–364. [Google Scholar] [CrossRef]
- Engel, A.K.; Fries, P. Beta-band oscillations—Signalling the status quo? Curr. Opin. Neurobiol. 2010, 20, 156–165. [Google Scholar] [CrossRef] [PubMed]
- Kang, G.; Lowery, M.M. Interaction of oscillations, and their suppression via deep brain stimulation, in a model of the cortico-basal ganglia network. IEEE Trans. Neural Syst. Rehabil. Eng. 2013, 21, 244–253. [Google Scholar] [CrossRef]
- Karmon, B.; DeLong, M.R.; Sanabria, D.E.; Johnson, L.A.; Nebeck, S.D.; Zhang, J.; Johnson, M.D.; Baker, K.B.; Molnar, G.F.; Vitek, J.L.; et al. The primate subthalamic nucleus. II. Neuronal activity in the MPTP model of parkinsonism. J. Neurophysiol. 1994, 72, 507–520. [Google Scholar] [CrossRef]
- Bergman, H.; Feingold, A.; Nini, A.; Raz, A.; Slovin, H.; Abeles, M.; Vaadia, E. Physiological aspects of information processing in the basal ganglia of normal and parkinsonian primates. Trends Neurosci. 1998, 21, 32–38. [Google Scholar] [CrossRef] [PubMed]
- Hansel, D.; Mato, G.; Meunier, C. Synchrony in excitatory neural networks. Neural Comput. 1995, 7, 307–337. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.-J.; Rinzel, J. Spindle rhythmicity in the reticularis thalami nucleus: Synchronization among mutually inhibitory neurons. Neuroscience 1993, 53, 899–904. [Google Scholar] [CrossRef] [PubMed]
- Terman, D.; Rubin, J.E.; Yew, A.C.; Wilson, C.J. Activity patterns in a model for the subthalamopallidal network of the basal ganglia. J. Neurosci. 2002, 22, 2963–2976. [Google Scholar] [CrossRef] [PubMed]
- Rubin, J.E.; Terman, D. High frequency stimulation of the subthalamic nucleus eliminates pathological thalamic rhythmicity in a computational model. J. Comput. Neurosci. 2004, 16, 211–235. [Google Scholar] [CrossRef] [PubMed]
- Hurtado, J.M.; Gray, C.M.; Tamas, L.B.; Sigvardt, K.A. Dynamics of tremor-related oscillations in the human globus pallidus: A single case study. Proc. Natl. Acad. Sci. USA 1999, 96, 1674–1679. [Google Scholar] [CrossRef] [PubMed]
- Nini, A.; Feingold, A.; Slovin, H.; Tamtè, M.; Brys, I.; Richter, U.; Ivica, N.; Halje, P.; Petersson, P.; McCairn, K.W.; et al. Neurons in the globus pallidus do not show correlated activity in the normal monkey, but phase-locked oscillations appear in the MPTP model of parkinsonism. J. Neurophysiol. 1995, 74, 1800–1805. [Google Scholar] [CrossRef] [PubMed]
- Levy, R.; Ashby, P.; Hutchison, W.D.; Lang, A.E.; Lozano, A.M.; Dostrovsky, J.O. Dependence of subthalamic nucleus oscillations on movement and dopamine in Parkinson’s disease. Brain 2002, 125, 1196–1209. [Google Scholar] [CrossRef] [PubMed]
- Park, C.; Worth, R.M.; Rubchinsky, L.L.; Ahn, S.; Solfest, J.; Cruz, A.V.; Mallet, N.; Magill, P.J.; Brown, P.; Averbeck, B.B. Fine temporal structure of beta oscillations synchronization in subthalamic nucleus in Parkinson’s disease. J. Neurophysiol. 2010, 103, 2707–2716. [Google Scholar] [CrossRef] [PubMed]
- Bevan, M. Move to the rhythm: Oscillations in the subthalamic nucleus–external globus pallidus network. Trends Neurosci. 2002, 25, 525–531. [Google Scholar] [CrossRef] [PubMed]
- Mandali, A.; Rengaswamy, M.; Chakravarthy, V.S.; Moustafa, A.A. A spiking basal ganglia model of synchrony, exploration and decision making. Front. Neurosci. 2015, 9, 191. [Google Scholar] [CrossRef]
- Mandali, A.; Chakravarthy, V.S.; Rajan, R.; Sarma, S.; Kishore, A. Electrode position and current amplitude modulate impulsivity after subthalamic stimulation in Parkinsons disease—A computational study. Front. Physiol. 2016, 7, 585. [Google Scholar] [CrossRef][Green Version]
- Fitts, P.M. The information capacity of the human motor system in controlling the amplitude of movement. J. Exp. Psychol. 1954, 47, 381–391. [Google Scholar] [CrossRef]
- Morasso, P. Spatial control of arm movements. Exp. Brain Res. 1981, 42, 223–227. [Google Scholar] [CrossRef]
- Knill, D.C.; Pouget, A. The Bayesian brain: The role of uncertainty in neural coding and computation. Trends Neurosci. 2004, 27, 712–719. [Google Scholar] [CrossRef]
- Körding, K.P.; Wolpert, D.M. Bayesian integration in sensorimotor learning. Nature 2004, 427, 244–247. [Google Scholar] [CrossRef]
- Todorov, E. Optimality principles in sensorimotor control. Nat. Neurosci. 2004, 7, 907–915. [Google Scholar] [CrossRef]
- Doya, K. What are the computations of the cerebellum, the basal ganglia and the cerebral cortex? Neural Netw. 1999, 12, 961–974. [Google Scholar] [CrossRef] [PubMed]
- Nakahara, H.; Doya, K.; Hikosaka, O. Parallel cortico-basal ganglia mechanisms for acquisition and execution of visuomotor sequences—A computational approach. J. Cogn. Neurosci. 2001, 13, 626–647. [Google Scholar] [CrossRef] [PubMed]
- Hikosaka, O.; Nakamura, K.; Sakai, K.; Nakahara, H. Central mechanisms of motor skill learning. Curr. Opin. Neurobiol. 2002, 12, 217–222. [Google Scholar] [CrossRef] [PubMed]
- Izawa, J.; Kondo, T.; Ito, K. Biological arm motion through reinforcement learning. Biol. Cybern. 2004, 91, 10–22. [Google Scholar] [CrossRef] [PubMed]
- Sridharan, D.; Prashanth, P.S.; Chakravarthy, V.S. The role of the basal ganglia in exploration in a neural model based on reinforcement learning. Int. J. Neural Syst. 2006, 16, 111–124. [Google Scholar] [CrossRef] [PubMed]
- Muralidharan, V.; Mandali, A.; Balasubramani, P.P.; Mehta, H.; Chakravarthy, V.S.; Jahanshahi, M. A Corti-Co-Basal Ganglia Model to Understand the Neural Dynamics of Targeted Reaching in Normal and Parkinson’s Conditions BT—Computational Neuroscience Models of the Basal Ganglia; Chakravarthy, V.S., Moustafa, A.A., Eds.; Springer: Singapore, 2018; pp. 167–195. [Google Scholar] [CrossRef]
- Nair, S.S.; Muddapu, V.R.; Chakravarthy, V.S. A Multiscale, Systems-Level, Neuropharmacological Model of Cortico-Basal Ganglia System for Arm Reaching Under Normal, Parkinsonian, and Levodopa Medication Conditions. Front. Comput. Neurosci. 2022, 15, 756881. [Google Scholar] [CrossRef]
- Gurney, K.; Prescott, T.J.; Redgrave, P. A computational model of action selection in the basal ganglia. I. A new functional anatomy. Biol. Cybern. 2001, 84, 401–410. [Google Scholar] [CrossRef] [PubMed]
- Humphries, M.D.; Stewart, R.D.; Gurney, K.N. A physiologically plausible model of action selection and oscillatory activity in the basal ganglia. J. Neurosci. 2006, 26, 12921–12942. [Google Scholar] [CrossRef]
- Narayanamurthy, R.; Jayakumar, S.; Elango, S.; Muralidharan, V.; Chakravarthy, V.S. A Cortico-Basal Ganglia Model for choosing an optimal rehabilitation strategy in Hemiparetic Stroke. Sci. Rep. 2019, 9, 13472. [Google Scholar] [CrossRef] [PubMed]
- Benabid, A.L.; Benazzouz, A.; Hoffmann, D.; Limousin, P.; Krack, P.; Pollak, P. Long-term electrical inhibition of deep brain targets in movement disorders. Mov. Disord. 1998, 13, 119–125. [Google Scholar] [CrossRef] [PubMed]
- Volkmann, J. Deep brain stimulation for the treatment of Parkinson’s disease. J. Clin. Neurophysiol. 2004, 21, 6–17. [Google Scholar] [CrossRef]
- Garcia, L.; D’Alessandro, G.; Bioulac, B.; Hammond, C. High-frequency stimulation in Parkinson’s disease: More or less? Trends Neurosci. 2005, 28, 209–216. [Google Scholar] [CrossRef] [PubMed]
- Hauptmann, C.; Tass, P.A. Therapeutic rewiring by means of desynchronizing brain stimulation. Biosystems 2007, 89, 173–181. [Google Scholar] [CrossRef]
- Foutz, T.J.; McIntyre, C.C. Evaluation of novel stimulus waveforms for deep brain stimulation. J. Neural Eng. 2010, 7, 066008. [Google Scholar] [CrossRef]
- Majsak, M.J.; Kaminski, T.; Gentile, A.M.; Flanagan, J.R. The reaching movements of patients with Parkinson’s disease under self- determined maximal speed and visually cued conditions. Brain 1998, 121, 755–766. [Google Scholar] [CrossRef]
- Hoehn, M.M.; Yahr, M.D. Parkinsonism: Onset, progression, and mortality. Neurology 1967, 17. [Google Scholar] [CrossRef]
- Baraduc, P.; Thobois, S.; Gan, J.; Broussolle, E.; Desmurget, M. A common optimization principle for motor execution in healthy subjects and parkinsonian patients. J. Neurosci. 2013, 33, 665–677. [Google Scholar] [CrossRef]
- Munoz, M.J.; Arora, R.; Rivera, Y.M.; Drane, Q.H.; Pal, G.D.; Metman, L.V.; Sani, S.B.; Rosenow, J.M.; Goelz, L.C.; Corcos, D.M.; et al. Medication only improves limb movements while deep brain stimulation improves eye and limb movements during visually-guided reaching in Parkinson’s disease. Front. Hum. Neurosci. 2023, 17, 1224611. [Google Scholar] [CrossRef] [PubMed]
- Benazzouz, A.; Breit, S.; Koudsie, A.; Pollak, P.; Krack, P.; Benabid, A.-L. Intraoperative microrecordings of the subthalamic nucleus in Parkinson’s disease. Mov. Disord. 2002, 17 (Suppl. S3), S145–S149. [Google Scholar] [CrossRef] [PubMed]
- Magnin, M.; Morel, A.; Jeanmonod, D. Single-unit analysis of the pallidum, thalamus and subthalamic nucleus in parkinsonian patients. Neuroscience 2000, 96, 549–564. [Google Scholar] [CrossRef]
- Sinclair, N.C.; McDermott, H.J.; Fallon, J.B.; Perera, T.; Brown, P.; Bulluss, K.J.; Thevathasan, W. Deep brain stimulation for Parkinson’s disease modulates high-frequency evoked and spontaneous neural activity. Neurobiol. Dis. 2019, 130, 104522. [Google Scholar] [CrossRef] [PubMed]
- Kühn, A.A.; Kempf, F.; Brücke, C.; Doyle, L.G.; Martinez-Torres, I.; Pogosyan, A.; Trottenberg, T.; Kupsch, A.; Schneider, G.-H.; Hariz, M.I.; et al. High-frequency stimulation of the subthalamic nucleus suppresses oscillatory β activity in patients with Parkinson’s disease in parallel with improvement in motor performance. J. Neurosci. 2008, 28, 6165–6173. [Google Scholar] [CrossRef]
- Tsui, A.; Aziz, T.; Ray, N.; Brücke, C.; Kupsch, A.; Schneider, G.-H.; Brown, P. Pathological synchronisation in the subthalamic nucleus of patients with Parkinson’s disease relates to both bradykinesia and rigidity. Exp. Neurol. 2009, 215, 380–387. [Google Scholar] [CrossRef]
- Sirica, D.; Hewitt, A.L.; Tarolli, C.G.; Weber, M.T.; Zimmerman, C.; Santiago, A.; Wensel, A.; Mink, J.W.; Lizárraga, K.J. Neurophysiological biomarkers to optimize deep brain stimulation in movement disorders. Neurodegener. Dis. Manag. 2021, 11, 315–328. [Google Scholar] [CrossRef]
- Rački, V.; Hero, M.; Rožmarić, G.; Papić, E.; Raguž, M.; Chudy, D.; Vuletić, V. Cognitive Impact of Deep Brain Stimulation in Parkinson’s Disease Patients: A Systematic Review. Front. Hum. Neurosci. 2022, 16, 867055. [Google Scholar] [CrossRef]
- Massano, J.; Garrett, C. Deep brain stimulation and cognitive decline in Parkinson’s disease: A clinical review. Front. Neurol. 2012, 3, 66. [Google Scholar] [CrossRef]
- Broen, M.; Duits, A.; Visser-Vandewalle, V.; Temel, Y.; Winogrodzka, A. Impulse control and related disorders in Parkinson’s disease patients treated with bilateral subthalamic nucleus stimulation: A review. Park. Relat. Disord. 2011, 17, 413–417. [Google Scholar] [CrossRef]
- Balarajah, S.; Cavanna, A.E. The pathophysiology of impulse control disorders in Parkinson disease. Behav. Neurol. 2013, 26, 237–244. [Google Scholar] [CrossRef] [PubMed]
- Cavanagh, J.F.; Wiecki, T.V.; Cohen, M.X.; Figueroa, C.M.; Samanta, J.; Sherman, S.J.; Frank, M.J. Subthalamic nucleus stimulation reverses mediofrontal influence over decision threshold. Nat. Neurosci. 2011, 14, 1462–1467. [Google Scholar] [CrossRef] [PubMed]
- Combs, H.L.; Folley, B.S.; Berry, D.T.R.; Segerstrom, S.C.; Han, D.Y.; Anderson-Mooney, A.J.; Walls, B.D.; van Horne, C. Cognition and depression following deep brain stimulation of the subthalamic nucleus and globus pallidus pars internus in Parkinson’s disease: A meta-analysis. Neuropsychol. Rev. 2015, 25, 439–454. [Google Scholar] [CrossRef] [PubMed]
- Evens, R.; Stankevich, Y.; Dshemuchadse, M.; Storch, A.; Wolz, M.; Reichmann, H.; Schlaepfer, T.E.; Goschke, T.; Lueken, U. The impact of Parkinson’s disease and subthalamic deep brain stimulation on reward processing. Neuropsychologia 2015, 75, 11–19. [Google Scholar] [CrossRef] [PubMed]
- Pham, U.; Solbakk, A.-K.; Skogseid, I.-M.; Toft, M.; Pripp, A.H.; Konglund, A.E.; Andersson, S.; Haraldsen, I.R.; Aarsland, D.; Dietrichs, E.; et al. Personality changes after deep brain stimulation in Parkinson’s disease. Park. Dis. 2015, 2015, 490507. [Google Scholar] [CrossRef] [PubMed]
- Moum, S.J.; Price, C.C.; Limotai, N.; Oyama, G.; Ward, H.; Jacobson, C.; Foote, K.D.; Okun, M.S. Effects of STN and GPi deep brain stimulation on impulse control disorders and dopamine dysregulation syndrome. PLoS ONE 2012, 7, e29768. [Google Scholar] [CrossRef] [PubMed]
- Scherrer, S.; Smith, A.H.; Gowatsky, J.; Palmese, C.A.; Jimenez-Shahed, J.; Kopell, B.H.; Mayberg, H.S.; Figee, M. Impulsivity and compulsivity after subthalamic deep brain stimulation for Parkinson’s disease. Front. Behav. Neurosci. 2020, 14, 47. [Google Scholar] [CrossRef] [PubMed]
- Ardouin, C.; Voon, V.; Worbe, Y.; Abouazar, N.; Czernecki, V.; Hosseini, H.; Pelissolo, A.; Moro, E.; Lhommée, E.; Lang, A.E.; et al. Pathological gambling in Parkinson’s disease improves on chronic subthalamic nucleus stimulation. Mov. Disord. 2006, 21, 1941–1946. [Google Scholar] [CrossRef]
- Bandini, F.; Primavera, A.; Pizzorno, M.; Cocito, L. Using STN DBS and medication reduction as a strategy to treat pathological gambling in Parkinson’s disease. Park. Relat. Disord. 2007, 13, 369–371. [Google Scholar] [CrossRef]
- Phokaewvarangkul, O.; Auffret, M.; Groppa, S.; Markovic, V.; Petrovic, I.; Bhidayasiri, R. What was first and what is next in selecting device-aided therapy in Parkinson’s disease? Balancing evidence and experience. J. Neural Transm. 2024. [Google Scholar] [CrossRef]
- Hikosaka, O.; Nakahara, H.; Rand, M.K.; Sakai, K.; Lu, X.; Nakamura, K.; Miyachi, S.; Doya, K. Parallel neural networks for learning sequential procedures. Trends Neurosci. 1999, 22, 464–471. [Google Scholar] [CrossRef] [PubMed]
- Iorio-Morin, C.; Fomenko, A.; Kalia, S.K. Deep-brain stimulation for essential tremor and other tremor syndromes: A narrative review of current targets and clinical outcomes. Brain Sci. 2020, 10, 925. [Google Scholar] [CrossRef] [PubMed]
- Groiss, S.; Wojtecki, L.; Südmeyer, M.; Schnitzler, A. Review: Deep brain stimulation in Parkinson’s disease. Ther. Adv. Neurol. Disord. 2009, 2, 379–391. [Google Scholar] [CrossRef] [PubMed]
- Hariz, M.I.; Krack, P.; Alesch, F.; Augustinsson, L.-E.; Bosch, A.; Ekberg, R.; Johansson, F.; Johnels, B.; Meyerson, B.A.; N’Guyen, J.-P.; et al. Multicentre European study of thalamic stimulation for parkinsonian tremor: A 6 year follow-up. J. Neurol. Neurosurg. Psychiatry 2008, 79, 694–699. [Google Scholar] [CrossRef] [PubMed]
- Wu, T.; Hallett, M. The cerebellum in Parkinson’s disease. Brain 2013, 136, 696–709. [Google Scholar] [CrossRef] [PubMed]
- Welniarz, Q.; Worbe, Y.; Gallea, C. The forward model: A unifying theory for the role of the cerebellum in motor control and sense of agency. Front. Syst. Neurosci. 2021, 15, 644059. [Google Scholar] [CrossRef] [PubMed]
- Caligiore, D.; Pezzulo, G.; Baldassarre, G.; Bostan, A.C.; Strick, P.L.; Doya, K.; Helmich, R.C.; Dirkx, M.; Houk, J.; Jörntell, H.; et al. Consensus paper: Towards a systems-level view of cerebellar function: The Interplay between cerebellum, basal ganglia, and cortex. Cerebellum 2017, 16, 203–229. [Google Scholar] [CrossRef] [PubMed]
- Wolpert, D.M.; Ghahramani, Z. Computational principles of movement neuroscience. Nat. Neurosci. 2000, 3, 1212–1217. [Google Scholar] [CrossRef]
- Collomb-Clerc, A.; Welter, M.-L. Effects of deep brain stimulation on balance and gait in patients with Parkinson’s disease: A systematic neurophysiological review. Neurophysiol. Clin. 2015, 45, 371–388. [Google Scholar] [CrossRef]
- Duncan, R.P.; Van Dillen, L.R.; Garbutt, J.M.; Earhart, G.M.; Perlmutter, J.S. Physical therapy and deep brain stimulation in Parkinson’s Disease: Protocol for a pilot randomized controlled trial. Pilot Feasibility Stud. 2018, 4, 54. [Google Scholar] [CrossRef]
- Nardo, A.; Anasetti, F.; Servello, D.; Porta, M. Quantitative gait analysis in patients with Parkinson treated with deep brain stimulation: The effects of a robotic gait training. NeuroRehabilitation 2014, 35, 779–788. [Google Scholar] [CrossRef] [PubMed]
- Tassorelli, C.; Buscone, S.; Sandrini, G.; Pacchetti, C.; Furnari, A.; Zangaglia, R.; Bartolo, M.; Nappi, G.; Martignoni, E. The role of rehabilitation in deep brain stimulation of the subthalamic nucleus for Parkinson’s disease: A pilot study. Park. Relat. Disord. 2009, 15, 675–681. [Google Scholar] [CrossRef] [PubMed]




| MODEL/EXP | Category | MT (s) | PV (m/s) | TPV (s) |
|---|---|---|---|---|
| MODEL | HC | 0.41 ± 0.048 | 3.18 ± 0.36 | 0.31 ± 0.034 |
| PD/DBS OFF | 0.837 ± 0.084 | 1.49 ± 0.27 | 0.62 ± 0.008 | |
| DBS ON | 0.44 ± 0.028 | 2.89 ± 0.02 | 0.35 ± 0.016 | |
| EXP1 [61] | HC | 0.343 ± 0.004 | 2.15 ± 0.27 | 0.19 ± 0.02 |
| PD/DBS OFF | 0.52 ± 0.063 | 1.35 ± 0.18 | 0.27 ± 0.003 | |
| DBS ON | NA | NA | NA | |
| EXP2 [63] | HC | ~0.8 ± 0.1 | ~0.33 ± 0.06 | ~0.446 |
| PD/DBS OFF | ~1.35 ± 0.18 | ~0.175 ± 0.033 | ~0.756 | |
| DBS ON | ~1.05 ± 0.16 | ~0.25 ± 0.05 | ~0.637 | |
| EXP3 [64] | HC | NA | NA | NA |
| PD/DBS OFF | 0.505 ± 0.017 | 0.34 ± 0.018 | NA | |
| DBS ON | 0.46 ± 0.015 | 0.35 ± 0.005 | NA |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nair, S.S.; Chakravarthy, S. A Computational Model of Deep Brain Stimulation for Parkinson’s Disease Tremor and Bradykinesia. Brain Sci. 2024, 14, 620. https://doi.org/10.3390/brainsci14060620
Nair SS, Chakravarthy S. A Computational Model of Deep Brain Stimulation for Parkinson’s Disease Tremor and Bradykinesia. Brain Sciences. 2024; 14(6):620. https://doi.org/10.3390/brainsci14060620
Chicago/Turabian StyleNair, Sandeep Sathyanandan, and Srinivasa Chakravarthy. 2024. "A Computational Model of Deep Brain Stimulation for Parkinson’s Disease Tremor and Bradykinesia" Brain Sciences 14, no. 6: 620. https://doi.org/10.3390/brainsci14060620
APA StyleNair, S. S., & Chakravarthy, S. (2024). A Computational Model of Deep Brain Stimulation for Parkinson’s Disease Tremor and Bradykinesia. Brain Sciences, 14(6), 620. https://doi.org/10.3390/brainsci14060620









