Psychiatric Disorders and Alcohol Consumption Among Low-Income African Americans:Gender Differences
Abstract
1. Background
2. Aims
3. Methods
3.1. Design and Setting
3.2. Ethics
3.3. Participants and Sampling
3.4. Recruitment
3.5. Data Collection
3.6. Measures
3.6.1. Demographic Factors
3.6.2. Educational Attainment
3.6.3. Household Monthly Income
3.6.4. Number of Psychiatric Disorders
3.6.5. Self-Rated Health (SRH)
3.6.6. Amount of Alcohol Consumption
3.7. Statistical Analysis
4. Results
4.1. Descriptive Statistics
4.2. Bivariate Correlations
4.3. Linear Regressions in the Pooled Sample
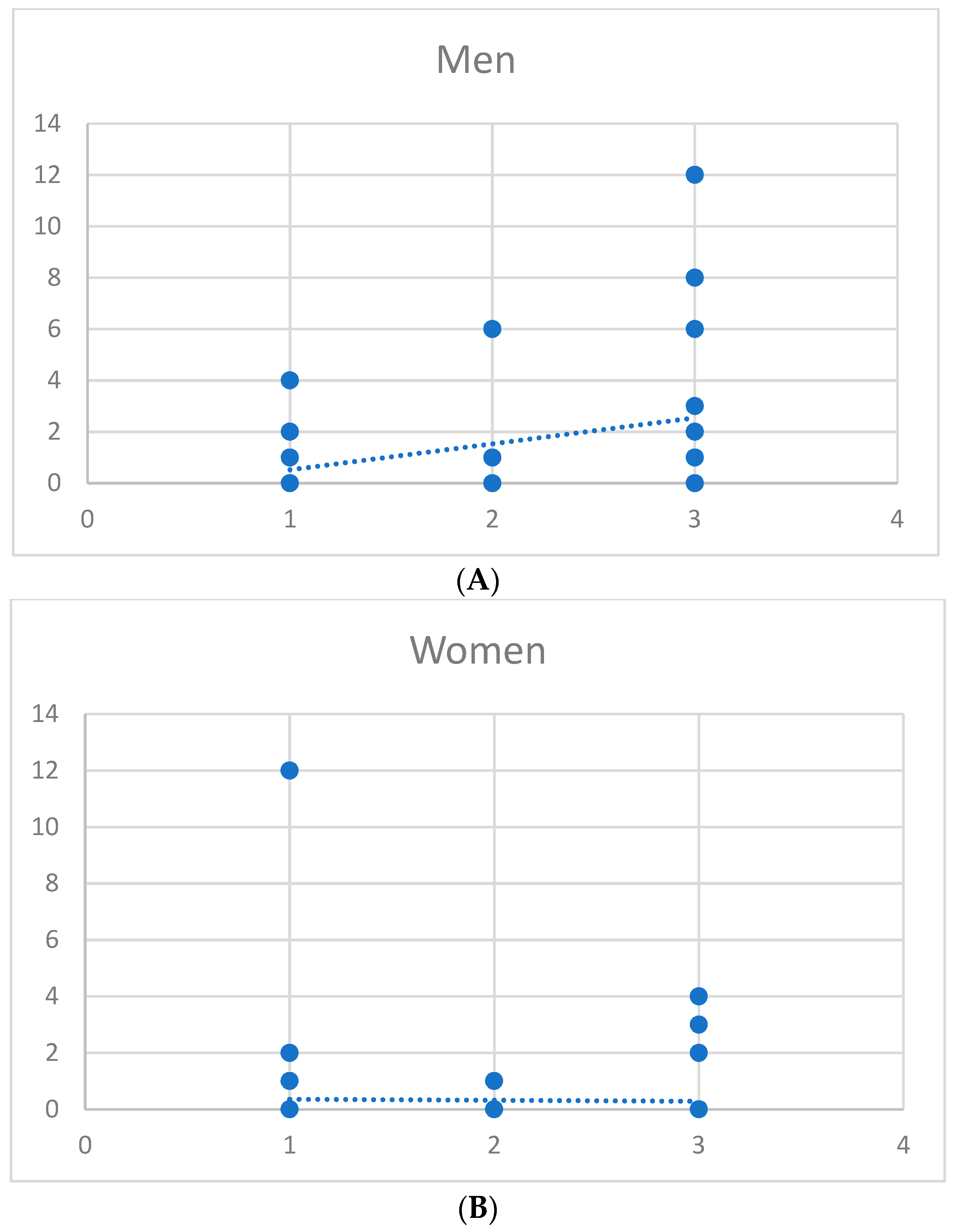
4.4. Linear Regressions by Gender
5. Discussion
5.1. Clinical and Public Health Implications
5.2. Limitations
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Busto, U.E.; Romach, M.K.; Sellers, E.M. Multiple drug use and psychiatric comorbidity in patients admitted to the hospital with severe benzodiazepine dependence. J. Clin. Psychopharmacol. 1996, 16, 51–57. [Google Scholar] [CrossRef]
- Mericle, A.A.; Ta Park, V.M.; Holck, P.; Arria, A.M. Prevalence, patterns, and correlates of co-occurring substance use and mental disorders in the United States: Variations by race/ethnicity. Compr. Psychiatry 2012, 53, 657–665. [Google Scholar] [CrossRef] [PubMed]
- Alvidrez, J.; Havassy, B.E. Racial distribution of dual-diagnosis clients in public sector mental health and drug treatment settings. J. Health Care Poor Underserved 2005, 16, 53–62. [Google Scholar] [CrossRef]
- Goldstick, J.E.; Bohnert, K.M.; Davis, A.K.; Bonar, E.E.; Carter, P.M.; Walton, M.A.; Cunningham, R.M. Dual Trajectories of Depression/Anxiety Symptoms and Alcohol Use, and their Implications for Violence Outcomes Among Drug-Using Urban Youth. Alcohol. Alcohol. 2018, 53, 659–666. [Google Scholar] [CrossRef] [PubMed]
- Hartley, S.; Haddock, G.; Barrowclough, C. Anxiety and depression and their links with delusions and hallucinations in people with a dual diagnosis of psychosis and substance misuse: A study using data from a randomised controlled trial. Behav. Res. Ther. 2012, 50, 65–71. [Google Scholar] [CrossRef]
- Manley, D. Dual diagnosis: Co-existence of drug, alcohol and mental health problems. Br. J. Nurs. 2005, 14, 100–106. [Google Scholar] [CrossRef] [PubMed]
- Manley, D. Dual diagnosis: Approaches to the treatment of people with dual mental health and drug abuse problems. Ment. Health Care 1998, 1, 190–192. [Google Scholar] [PubMed]
- Reilly, J.; McDermott, B.; Dillon, J. Standardized drug and alcohol questions at admission to an acute adult mental health unit: Clarifying the burden of dual diagnoses across a five-year period. Australas Psychiatry 2018. [Google Scholar] [CrossRef]
- Berking, M.; Wupperman, P. Emotion regulation and mental health: Recent findings, current challenges, and future directions. Curr. Opin. Psychiatry 2012, 25, 128–134. [Google Scholar] [CrossRef]
- Lee, S.H.; Ripke, S.; Neale, B.M.; Faraone, S.V.; Purcell, S.M.; Perlis, R.H.; Mowry, B.J.; Thapar, A.; Goddard, M.E.; Witte, J.S.; et al. Genetic relationship between five psychiatric disorders estimated from genome-wide SNPs. Nat. Genet. 2013, 45, 984–994. [Google Scholar] [CrossRef]
- Najman, J.M.; Hayatbakhsh, M.R.; Clavarino, A.; Bor, W.; O’Callaghan, M.J.; Williams, G.M. Family poverty over the early life course and recurrent adolescent and young adult anxiety and depression: A longitudinal study. Am. J. Public Health 2010, 100, 1719–1723. [Google Scholar] [CrossRef]
- Sweeney, S.; Air, T.; Zannettino, L.; Galletly, C. Psychosis, Socioeconomic Disadvantage, and Health Service Use in South Australia: Findings from the Second Australian National Survey of Psychosis. Front. Public Health 2015, 3, 259. [Google Scholar] [CrossRef]
- Karriker-Jaffe, K.J.; Roberts, S.C.; Bond, J. Income inequality, alcohol use, and alcohol-related problems. Am. J. Public Health 2013, 103, 649–656. [Google Scholar] [CrossRef] [PubMed]
- Stockdale, S.E.; Wells, K.B.; Tang, L.; Belin, T.R.; Zhang, L.; Sherbourne, C.D. The importance of social context: Neighborhood stressors, stress-buffering mechanisms, and alcohol, drug, and mental health disorders. Soc. Sci. Med. 2007, 65, 1867–1881. [Google Scholar] [CrossRef] [PubMed]
- Zlotnick, C.; Johnson, J.; Kohn, R.; Vicente, B.; Rioseco, P.; Saldivia, S. Childhood trauma, trauma in adulthood, and psychiatric diagnoses: Results from a community sample. Compr. Psychiatry 2008, 49, 163–169. [Google Scholar] [CrossRef] [PubMed]
- Farb, N.A.; Anderson, A.K.; Segal, Z.V. The mindful brain and emotion regulation in mood disorders. Can. J. Psychiatry 2012, 57, 70–77. [Google Scholar] [CrossRef] [PubMed]
- Cisler, J.M.; Olatunji, B.O.; Feldner, M.T.; Forsyth, J.P. Emotion Regulation and the Anxiety Disorders: An Integrative Review. J. Psychopathol. Behav. Assess. 2010, 32, 68–82. [Google Scholar] [CrossRef]
- Petit, G.; Luminet, O.; Maurage, F.; Tecco, J.; Lechantre, S.; Ferauge, M.; Gross, J.J.; de Timary, P. Emotion Regulation in Alcohol Dependence. Alcohol. Clin. Exp. Res. 2015, 39, 2471–2479. [Google Scholar] [CrossRef]
- Simning, A.; van Wijngaarden, E.; Conwell, Y. Anxiety, mood, and substance use disorders in United States African-American public housing residents. Soc. Psychiatry Psychiatr. Epidemiol. 2011, 46, 983–992. [Google Scholar] [CrossRef]
- Compton, W.M.; Conway, K.P.; Stinson, F.S.; Grant, B.F. Changes in the prevalence of major depression and comorbid substance use disorders in the United States between 1991-1992 and 2001-2002. Am. J. Psychiatry 2006, 163, 2141–2147. [Google Scholar] [CrossRef]
- Solberg, B.S.; Halmoy, A.; Engeland, A.; Igland, J.; Haavik, J.; Klungsoyr, K. Gender differences in psychiatric comorbidity: A population-based study of 40 000 adults with attention deficit hyperactivity disorder. Acta Psychiatr. Scand. 2018, 137, 176–186. [Google Scholar] [CrossRef] [PubMed]
- Latimer, W.W.; Stone, A.L.; Voight, A.; Winters, K.C.; August, G.J. Gender differences in psychiatric comorbidity among adolescents with substance use disorders. Exp. Clin. Psychopharmacol. 2002, 10, 310–315. [Google Scholar] [CrossRef] [PubMed]
- Idler, E.L.; Benyamini, Y. Self-rated health and mortality: A review of twenty-seven community studies. J. Health Soc. Behav. 1997, 38, 21–37. [Google Scholar] [CrossRef] [PubMed]
- Schnittker, J.; Bacak, V. The increasing predictive validity of self-rated health. PLoS ONE 2014, 9, e84933. [Google Scholar] [CrossRef] [PubMed]
- Nery Guimaraes, J.M.; Chor, D.; Werneck, G.L.; Carvalho, M.S.; Coeli, C.M.; Lopes, C.S.; Faerstein, E. Association between self-rated health and mortality: 10 years follow-up to the Pro-Saude cohort study. BMC Public Health 2012, 12, 676. [Google Scholar] [CrossRef] [PubMed]
- Thong, M.S.; Kaptein, A.A.; Benyamini, Y.; Krediet, R.T.; Boeschoten, E.W.; Dekker, F.W.; Netherlands Cooperative Study on the Adequacy of Dialysis Study Group. Association between a self-rated health question and mortality in young and old dialysis patients: A cohort study. Am. J. Kidney Dis. 2008, 52, 111–117. [Google Scholar] [CrossRef]
- Williams, G.D.; Aitken, S.S.; Malin, H. Reliability of self-reported alcohol consumption in a general population survey. J. Stud. Alcohol. 1985, 46, 223–227. [Google Scholar] [CrossRef] [PubMed]
- Russell, M.; Welte, J.W.; Barnes, G.M. Quantity-frequency measures of alcohol consumption: Beverage-specific vs global questions. Br. J. Addict. 1991, 86, 409–417. [Google Scholar] [CrossRef]
- Williams, G.D.; Proudfit, A.H.; Quinn, E.A.; Campbell, K.E. Variations in quantity-frequency measures of alcohol consumption from a general population survey. Addiction 1994, 89, 413–420. [Google Scholar] [CrossRef]
- Midanik, L.T. Comparing usual quantity/frequency and graduated frequency scales to assess yearly alcohol consumption: Results from the 1990 US National Alcohol Survey. Addiction 1994, 89, 407–412. [Google Scholar] [CrossRef]
- Abbey, A.; Smith, M.J.; Scott, R.O. The relationship between reasons for drinking alcohol and alcohol consumption: An interactional approach. Addict. Behav. 1993, 18, 659–670. [Google Scholar] [CrossRef]
- Bailey, R.K.; Blackmon, H.L.; Stevens, F.L.; Bailey, R.K.; Blackmon, H.L.; Stevens, F.L. Major depressive disorder in the African American population: Meeting the challenges of stigma, misdiagnosis, and treatment disparities. J. Natl. Med. Assoc. 2009, 101, 1084–1089. [Google Scholar] [CrossRef]
- Samson, M.E.; Porter, N.G.; Hurley, D.M.; Adams, S.A.; Eberth, J.M. Disparities in Breast Cancer Incidence, Mortality, and Quality of Care among African American and European American Women in South Carolina. Southern Med. J. 2016, 109, 24–30. [Google Scholar] [CrossRef]
- Galea, S.; Ahern, J.; Nandi, A.; Tracy, M.; Beard, J.; Vlahov, D. Urban neighborhood poverty and the incidence of depression in a population-based cohort study. Ann. Epidemiol. 2007, 17, 171–179. [Google Scholar] [CrossRef] [PubMed]
- Assari, S. Suicide Attempts in Michigan HealthCare System; Racial Differences. Brain Sci. 2018, 8, 124. [Google Scholar] [CrossRef] [PubMed]
- Assari, S. Race, Depression, and Financial Distress in a Nationally Representative Sample of American Adults. Brain Sci. 2019, 9, 29. [Google Scholar] [CrossRef]
- Assari, S.; Dejman, M.; Neighbors, H.W. Ethnic Differences in Separate and Additive Effects of Anxiety and Depression on Self-rated Mental Health Among Blacks. J. Racial Ethn. Health Disparities 2016, 3, 423–430. [Google Scholar] [CrossRef]
- Carter, J.D.; Assari, S. Sustained Obesity and Depressive Symptoms over 6 Years: Race by Gender Differences in the Health and Retirement Study. Front. Aging Neurosci. 2016, 8, 312. [Google Scholar] [CrossRef]
- Assari, S.; Caldwell, C.H. Gender and Ethnic Differences in the Association Between Obesity and Depression Among Black Adolescents. J. Racial Ethn. Health Disparities 2015, 2, 481–493. [Google Scholar] [CrossRef]
- Assari, S.; Caldwell, C.H.; Zimmerman, M.A. Sex differences in the association between testosterone and violent behaviors. Trauma Mon. 2014, 19, e18040. [Google Scholar] [CrossRef] [PubMed]
- Assari, S. The link between mental health and obesity: Role of individual and contextual factors. Int. J. Prev. Med. 2014, 5, 247–249. [Google Scholar]
- Boyd, R.C.; Joe, S.; Michalopoulos, L.; Davis, E.; Jackson, J.S. Prevalence of mood disorders and service use among US mothers by race and ethnicity: Results from the National Survey of American Life. J. Clin. Psychiatry 2011, 72, 1538–1545. [Google Scholar] [CrossRef]
- Assari, S. Combined Racial and Gender Differences in the Long-Term Predictive Role of Education on Depressive Symptoms and Chronic Medical Conditions. J. Racial Ethn. Health Disparities 2017, 4, 385–396. [Google Scholar] [CrossRef]
- Assari, S.; Gibbons, F.X.; Simons, R. Depression among Black Youth; Interaction of Class and Place. Brain Sci. 2018, 8, 108. [Google Scholar] [CrossRef]
- Assari, S. Social Determinants of Depression: The Intersections of Race, Gender, and Socioeconomic Status. Brain Sci. 2017, 7, 156. [Google Scholar] [CrossRef] [PubMed]
- Assari, S.; Lankarani, M.M.; Caldwell, C.H. Does Discrimination Explain High Risk of Depression among High-Income African American Men? Behav. Sci. 2018, 8, 40. [Google Scholar] [CrossRef]
- Assari, S.; Caldwell, C.H. High Risk of Depression in High-Income African American Boys. J. Racial Ethn. Health Disparities 2018, 5, 808–819. [Google Scholar] [CrossRef]
- Assari, S.; Lapeyrouse, L.M.; Neighbors, H.W. Income and Self-Rated Mental Health: Diminished Returns for High Income Black Americans. Behav. Sci. 2018, 8, 50. [Google Scholar] [CrossRef]
- Assari, S. Educational Attainment Better Protects African American Women than African American Men Against Depressive Symptoms and Psychological Distress. Brain Sci. 2018, 8, 182. [Google Scholar] [CrossRef]
- Assari, S. Separate and Combined Effects of Anxiety, Depression and Problem Drinking on Subjective Health among Black, Hispanic and Non-Hispanic White Men. Int. J. Prev. Med. 2014, 5, 269–279. [Google Scholar]
- Assari, S.; Moazen-Zadeh, E. Ethnic Variation in the Cross-sectional Association between Domains of Depressive Symptoms and Clinical Depression. Front. Psychiatry 2016, 7, 53. [Google Scholar] [CrossRef] [PubMed]
- Watkins, D.C.; Abelson, J.M.; Jefferson, S.O. “Their depression is something different …it would have to be”: Findings from a qualitative study of black women’s perceptions of depression in black men. Am. J. Mens. Health 2013, 7, 45S–57S. [Google Scholar] [CrossRef] [PubMed]
- Watkins, D.C.; Johnson, N.C. Age and Gender Differences in Psychological Distress among African Americans and Whites: Findings from the 2016 National Health Interview Survey. Healthcare 2018, 6, 6. [Google Scholar] [CrossRef] [PubMed]
- Assari, S. Association Between Self-Esteem and Depressive Symptoms Is Stronger Among Black than White Older Adults. J. Racial Ethn. Health Disparities 2017, 4, 687–695. [Google Scholar] [CrossRef]
- Smith, D.T.; Mouzon, D.M.; Elliott, M. Reviewing the Assumptions About Men’s Mental Health: An Exploration of the Gender Binary. Am. J. Mens. Health 2018, 12, 78–89. [Google Scholar] [CrossRef] [PubMed]
- Corbie-Smith, G.; Thomas, S.B.; St George, D.M. Distrust, race, and research. Arch. Intern. Med. 2002, 162, 2458–2463. [Google Scholar] [CrossRef] [PubMed]
- Corbie-Smith, G.; Thomas, S.B.; Williams, M.V.; Moody-Ayers, S. Attitudes and beliefs of African Americans toward participation in medical research. J. Gen. Intern. Med. 1999, 14, 537–546. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, B.R.; Mathis, C.C.; Woods, A.K. African Americans and their distrust of the health care system: Healthcare for diverse populations. J. Cult. Divers. 2007, 14, 56–60. [Google Scholar]
- Gamble, V.N. Under the shadow of Tuskegee: African Americans and health care. Am. J. Public Health 1997, 87, 1773–1778. [Google Scholar] [CrossRef]
- Jenks, S. Patient Consent: Defining Control of Genetic Information. J. Natl. Cancer Inst. 2017, 109, 4–5. [Google Scholar] [CrossRef][Green Version]
- Bell, C.C.; Mehta, H. The misdiagnosis of black patients with manic depressive illness. J. Natl. Med. Assoc. 1980, 72, 141–145. [Google Scholar] [PubMed]
- Bell, C.C.; Mehta, H. Misdiagnosis of black patients with manic depressive illness: Second in a series. J. Natl. Med. Assoc. 1981, 73, 101–107. [Google Scholar] [PubMed]
- Akinhanmi, M.O.; Biernacka, J.M.; Strakowski, S.M.; McElroy, S.L.; Balls Berry, J.E.; Merikangas, K.R.; Assari, S.; McInnis, M.G.; Schulze, T.G.; LeBoyer, M.; et al. Racial disparities in bipolar disorder treatment and research: A call to action. Bipolar Disord. 2018, 20, 506–514. [Google Scholar] [CrossRef] [PubMed]
- Roukema, R.; Fadem, B.; James, B.; Rayford, F. Bipolar disorder in a low socioeconomic population. Difficulties in diagnosis. J. Nerv. Ment. Dis. 1984, 172, 76–79. [Google Scholar] [CrossRef]
- Jones, B.E.; Gray, B.A. Problems in diagnosing schizophrenia and affective disorders among blacks. Hosp. Community Psychiatry 1986, 37, 61–65. [Google Scholar] [CrossRef] [PubMed]
- Wald, P.; Jonathan, M. Metzl, the Protest Psychosis: How Schizophrenia Became a Black Disease. Soc. Hist. Med. 2011, 24, 194–195. [Google Scholar] [CrossRef]
- Broome, B. Research and under represented groups. J. Cult Divers. 2007, 14, 55. [Google Scholar] [PubMed]
- Williams, D.R.; Gonzalez, H.M.; Neighbors, H.; Nesse, R.; Abelson, J.M.; Sweetman, J.; Jackson, J.S. Prevalence and distribution of major depressive disorder in African Americans, Caribbean blacks, and non-Hispanic whites: Results from the National Survey of American Life. Arch. Gen. Psychiatry 2007, 64, 305–315. [Google Scholar] [CrossRef] [PubMed]
- Geronimus, A.T.; Hicken, M.; Keene, D.; Bound, J. “Weathering” and age patterns of allostatic load scores among blacks and whites in the United States. Am. J. Public Health 2006, 96, 826–833. [Google Scholar] [CrossRef] [PubMed]
- Ward, E.C.; Wiltshire, J.C.; Detry, M.A.; Brown, R.L. African American men and women’s attitude toward mental illness, perceptions of stigma, and preferred coping behaviors. Nurs. Res. 2013, 62, 185–194. [Google Scholar] [CrossRef] [PubMed]
- Alang, S.M. Mental health care among blacks in America: Confronting racism and constructing solutions. Health Serv. Res. 2019. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, E.A.; Rolle, I.; Ferrans, C.E.; Whitaker, E.E.; Warnecke, R.B. Understanding African Americans’ views of the trustworthiness of physicians. J. Gen. Intern. Med. 2006, 21, 642–647. [Google Scholar] [CrossRef]
- Hall, M.A.; Dugan, E.; Zheng, B.; Mishra, A.K. Trust in physicians and medical institutions: What is it, can it be measured, and does it matter? Milbank Q. 2001, 79, 613–639. [Google Scholar] [CrossRef]
- Kelly, T.M.; Daley, D.C. Integrated treatment of substance use and psychiatric disorders. Soc. Work Public Health 2013, 28, 388–406. [Google Scholar] [CrossRef] [PubMed]
- Gouzoulis-Mayfrank, E. Comorbidity of substance use and other psychiatric disorders--theoretical foundation and evidence based therapy. Fortschr. Neurol. Psychiatr. 2008, 76, 263–271. [Google Scholar] [CrossRef] [PubMed]
- Drake, R.E.; Mueser, K.T. Psychosocial approaches to dual diagnosis. Schizophr. Bull. 2000, 26, 105–118. [Google Scholar] [CrossRef]
| All N = 150 | African American Women n = 101 | African American Men n = 49 | ||||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | |
| Age * | 55.78 | 7.40 | 54.87 | 7.40 | 57.65 | 7.10 |
| Educational Attainment | 3.61 | 1.40 | 3.53 | 1.51 | 3.76 | 1.13 |
| Household Income | 1.37 | 1.50 | 1.39 | 1.41 | 1.35 | 1.67 |
| Self-Rated Health (Poor) | 3.61 | 1.01 | 3.59 | 1.03 | 3.65 | 0.97 |
| Number of Psychiatric Disorders | 2.07 | 0.89 | 2.09 | 0.88 | 2.02 | 0.90 |
| Amount Alcohol Use * | 0.72 | 2.11 | 0.32 | 1.38 | 1.55 | 2.98 |
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
|---|---|---|---|---|---|---|---|
| All (N = 105) | |||||||
| 1 Gender (Male) | 1.00 | 0.18 * | 0.07 | −0.01 | 0.03 | −0.04 | 0.28 ** |
| 2 Age | 1.00 | 0.08 | 0.05 | 0.11 | −0.11 | 0.02 | |
| 3 Educational Attainment | 1.00 | 0.17 * | −0.07 | −0.11 | −0.07 | ||
| 4 Household Income | 1.00 | −0.23 ** | −0.24 ** | −0.02 | |||
| 5 Self-Rated Health (poor) | 1.00 | 0.20 * | 0.01 | ||||
| 6 Number of Psychiatric Disorders | 1.00 | 0.12 | |||||
| 7 Amount Alcohol Use | 1.00 | ||||||
| African American Men (n = 49) | |||||||
| 2 Age | 1.00 | 0.02 | −0.05 | 0.07 | −0.20 * | 0.01 | |
| 3 Educational Attainment | 1.00 | 0.13 | −0.06 | −0.07 | −0.04 | ||
| 4 Household Income | 1.00 | −0.30 ** | −0.31 ** | −0.10 | |||
| 5 Self-Rated Health (Poor) | 1.00 | 0.36 ** | 0.06 | ||||
| 6 Number of Psychiatric Disorders | 1.00 | −0.02 | |||||
| 7 Amount Alcohol Use | 1.00 | ||||||
| African American Women (n = 101) | |||||||
| 2 Age | 1.00 | 0.21 | 0.25 | 0.18 | 0.10 | −0.08 | |
| 3 Educational Attainment | 1.00 | 0.28 | −0.12 | −0.22 | −0.18 | ||
| 4 Household Income | 1.00 | −0.10 | −0.12 | 0.04 | |||
| 5 Self-Rated Health (Poor) | 1.00 | −0.13 | −0.06 | ||||
| 6 Number of Psychiatric Disorders | 1.00 | 0.31 * | |||||
| 7 Amount Alcohol Use | 1.00 |
| Unstandardized B | Std. Error | Standardized Beta | t | p | |
|---|---|---|---|---|---|
| Model 1 (All; N = 150) | |||||
| Gender (Male) | 1.29 | 0.36 | 0.29 | 3.56 | 0.00 |
| Age | 0.00 | 0.02 | −0.01 | −0.12 | 0.91 |
| Educational Attainment | −0.12 | 0.12 | −0.08 | −0.97 | 0.34 |
| Monthly Household Income | 0.02 | 0.12 | 0.02 | 0.21 | 0.84 |
| Self-Rated Health | −0.06 | 0.18 | −0.03 | −0.35 | 0.73 |
| Number of Psychiatric Disorders | 0.31 | 0.20 | 0.13 | 1.58 | 0.12 |
| Constant | 0.42 | 1.51 | 0.27 | 0.78 | |
| Model 2 (All; N = 150) | |||||
| Gender (Male) | −0.93 | 0.91 | −0.21 | −1.03 | 0.31 |
| Age | −0.01 | 0.02 | −0.05 | −0.61 | 0.54 |
| Educational Attainment | −0.09 | 0.12 | −0.06 | −0.77 | 0.44 |
| Monthly Household Income | 0.01 | 0.12 | 0.01 | 0.11 | 0.91 |
| Self-Rated Health | 0.06 | 0.18 | 0.03 | 0.33 | 0.74 |
| Number of Psychiatric Disorders | −0.09 | 0.25 | −0.04 | −0.36 | 0.72 |
| Number of Psychiatric Disorders * Gender | 1.10 | 0.41 | 0.56 | 2.66 | 0.01 |
| Constant | 1.38 | 1.53 | 0.91 | 0.37 | |
| Model 1 (African American Women; n = 101) | |||||
| Age | 0.00 | 0.02 | −0.02 | −0.18 | 0.858 |
| Educational Attainment | −0.03 | 0.09 | −0.03 | −0.31 | 0.758 |
| Monthly Household Income | −0.11 | 0.11 | −0.11 | −1.00 | 0.318 |
| Self-Rated Health | 0.07 | 0.15 | 0.05 | 0.46 | 0.649 |
| Number of Psychiatric Disorders | −0.13 | 0.18 | −0.08 | −0.71 | 0.481 |
| Constant | 0.78 | 1.32 | 0.59 | 0.556 | |
| Model 1 (African American Men; n = 49) | |||||
| Age | −0.05 | 0.07 | −0.12 | −0.75 | 0.457 |
| Educational Attainment | −0.35 | 0.41 | −0.13 | −0.84 | 0.406 |
| Monthly Household Income | 0.26 | 0.27 | 0.15 | 0.95 | 0.345 |
| Self-Rated Health | 0.00 | 0.46 | 0.00 | 0.00 | 0.998 |
| Number of Psychiatric Disorders | 1.01 | 0.50 | 0.31 | 2.02 | 0.050 |
| Constant | 3.29 | 3.88 | 0.85 | 0.401 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cobb, S.; Assari, S. Psychiatric Disorders and Alcohol Consumption Among Low-Income African Americans:Gender Differences. Brain Sci. 2019, 9, 86. https://doi.org/10.3390/brainsci9040086
Cobb S, Assari S. Psychiatric Disorders and Alcohol Consumption Among Low-Income African Americans:Gender Differences. Brain Sciences. 2019; 9(4):86. https://doi.org/10.3390/brainsci9040086
Chicago/Turabian StyleCobb, Sharon, and Shervin Assari. 2019. "Psychiatric Disorders and Alcohol Consumption Among Low-Income African Americans:Gender Differences" Brain Sciences 9, no. 4: 86. https://doi.org/10.3390/brainsci9040086
APA StyleCobb, S., & Assari, S. (2019). Psychiatric Disorders and Alcohol Consumption Among Low-Income African Americans:Gender Differences. Brain Sciences, 9(4), 86. https://doi.org/10.3390/brainsci9040086






