Analyzing the Photoprotection Efficiency of Sunscreens Containing Antioxidants under Disinfection Conditions
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Methods
2.2.1. Study Design
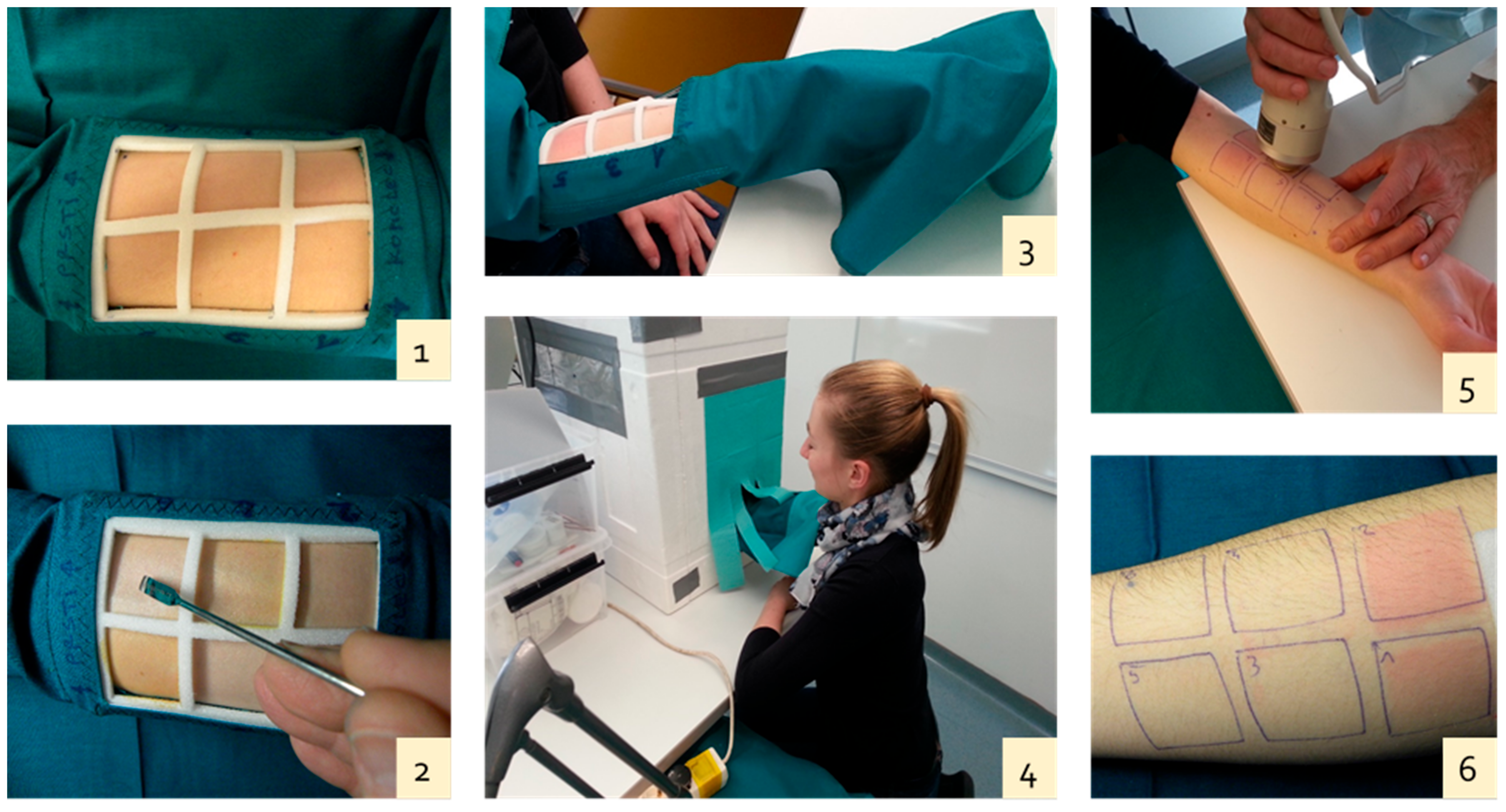
2.2.2. Assay Methods and Conditions
- the first square (positive control): the irradiated area remained free of ointment;
- the second square: a neutral ointment, without a UV filter or antioxidants, was applied;
- the third square: an ointment with a UV filter BP-3 was applied;
- the fourth square: an ointment with a UV filter BP-3 was applied. Before applying the ointment, the skin zone was exposed to disinfection conditions similar to those in swimming pool water for 1 min;
- the fifth square: an ointment with both a UV filter BP-3 and an antioxidant, β-carotene, was applied;
- the sixth square: an ointment with both a UV filter BP-3 and an antioxidant, trans-resveratrol, was applied.
2.2.3. UVB Irradiation and Measurement Techniques
2.2.4. Skin Color Measurements
2.2.5. Statistical Analysis
3. Results
3.1. Determination of the Minimal Erythema Dose (MED)
3.2. Comparison of the Effect of the Applied UV Filter and Antioxidants
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Narayanan, D.L.; Saladi, R.N.; Fox, J.L. Ultraviolet radiation and skin cancer. Int. J. Dermatol. 2010, 49, 978–986. [Google Scholar] [CrossRef] [PubMed]
- Poljšak, B.; Dahmane, R. Free radicals and extrinsic skin aging. Dermatol. Res. Pract. 2012, 2012, 135206. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lim, J.; Cho, E.; Lee, K.; Choi, Y.; Seo, Y.; Jeon, H.; Choi, J. Current immunotherapy approaches for malignant melanoma. BioChip J. 2019, 13, 105–114. [Google Scholar] [CrossRef]
- Shaath, N.A. Ultraviolet filters. Photochem. Photobiol. Sci. 2010, 9, 464–469. [Google Scholar] [CrossRef]
- Sobek, A.; Bejgarn, S.; Rudén, C.; Molander, L.; Breitholtz, M. In the shadow of the cosmetic directive—Inconsistencies in EU environmental hazard classification requirements for UV-filters. Sci. Total Environ. 2013, 461–462, 706–711. [Google Scholar] [CrossRef]
- Piérard, G.E. EEMCO guidance for the assessment of skin color. J. Eur. Acad. Dermatol. Venereol. 1998, 10, 1–11. [Google Scholar] [CrossRef]
- Taylor, S.; Westerhof, W.; Im, S.; Lim, J. Noninvasive techniques for evaluation of skin color. J. Am. Acad. Dermatol. 2006, 54, 282–290. [Google Scholar] [CrossRef]
- Calafat, A.M.; Wong, L.Y.; Ye, X.; Reidy, J.A.; Needham, L.L. Concentrations of the sunscreen agent benzophenone-3 in residents of the United States: National Health and Nutrition Examination Survey 2003–2004. Environ. Health Perspect. 2008, 116, 893–897. [Google Scholar] [CrossRef] [Green Version]
- Fediuk, D.J.; Wang, T.; Raizman, J.E.; Parkinson, F.E.; Gu, X. Tissue deposition of the insect repellent DEET and the sunscreen oxybenzone from repeated topical skin applications in rats. Int. J. Toxicol. 2010, 29, 594–603. [Google Scholar] [CrossRef]
- Fediuk, D.J.; Wang, T.; Chen, Y.; Parkinson, F.E.; Namaka, M.P.; Simons, K.J.; Burczynski, F.J.; Gu, X. Tissue disposition of the insect repellent DEET and the sunscreen oxybenzone following intravenous and topical administration in rats. Biopharm. Drug Dispos. 2011, 32, 369–379. [Google Scholar] [CrossRef] [PubMed]
- Freitas, J.V.; Praça, F.S.G.; Bentley, M.V.L.B.; Gaspar, L.R. Trans-resveratrol and β-carotene from sunscreens penetrate viable skin layers and reduce cutaneous penetration of UV-filters. Int. J. Pharm. 2015, 484, 131–137. [Google Scholar] [CrossRef]
- Kockler, J.; Oelgemöller, M.; Robertson, S.; Glass, B.D. Photostability of sunscreens. J. Photochem. Photobiol. C Photochem. Rev. 2012, 13, 91–110. [Google Scholar] [CrossRef]
- Kim, S.; Choi, K. Occurrences, toxicities, and ecological risks of benzophenone-3, a common component of organic sunscreen products: A mini-review. Environ. Int. 2014, 70, 143–157. [Google Scholar] [CrossRef]
- Fent, K.; Kunz, P.Y.; Zenker, A.; Rapp, M. A tentative environmental risk assessment of the UV-filters 3-(4-methylbenzylidene-camphor), 2-ethyl-hexyl-4-trimethoxycinnamate, benzophenone-3, benzophenone-4 and 3-benzylidene camphor. Mar. Environ. Res. 2010, 69, S4–S6. [Google Scholar] [CrossRef]
- DiNardo, J.C.; Downs, C.A. Dermatological and environmental toxicological impact of the sunscreen ingredient oxybenzone/benzophenone-3. J. Cosmet. Dermatol. 2016, 17, 15–19. [Google Scholar] [CrossRef]
- WHO. Guidelines for Safe Recreational Waters. Volume 2. Swimming Pools and Similar Recreational-Water Environments; WHO: Geneve, Switzerland, 2006; p. 118. [Google Scholar]
- Sakkas, V.A.; Giokas, D.L.; Lambropoulou, D.A.; Albanis, T.A. Aqueous photolysis of the sunscreen agent octyl-dimethyl-p-aminobenzoic acid. Formation of disinfection byproducts in chlorinated swimming pool water. J. Chromatogr. A 2003, 1016, 211–222. [Google Scholar] [CrossRef]
- Negreira, N.; Canosa, P.; Rodríguez, I.; Ramil, M.; Rubí, E.; Cela, R. Study of some UV filter stability in chlorinated water and identification of halogenated byproducts by gas chromatography-mass spectrometry. J. Chromatogr. A 2008, 1178, 206–214. [Google Scholar] [CrossRef]
- Lebedev, A.T. Mass spectrometry in the study of the mechanism of aquatic chlorination of organic substrates. Eur. J. Mass Spectrom. 2007, 13, 51–56. [Google Scholar] [CrossRef]
- Lebedev, A.T.; Bavcon Kralj, M.; Polyakova, O.V.; Detenchuk, E.A.; Pokryshkin, S.A.; Trebše, P. Identification of avobenzone by-products formed by various disinfectants in different types of swimming pool waters. Environ. Int. 2020, 137, 105495. [Google Scholar] [CrossRef]
- Grbović, G.; Trebše, P.; Dolenc, D.; Lebedev, A.T.; Sarakha, M. LC/MS study of the UV filter hexyl 2-[4-(diethylamino)-2-hydroxybenzoyl]-benzoate (DHHB) aquatic chlorination with sodium hypochlorite. J. Mass Spectrom. 2013, 48, 1232–1240. [Google Scholar] [CrossRef]
- Zhuang, R.; Žabar, R.; Grbović, G.; Dolenc, D.; Yao, J.; Tišler, T.; Trebše, P. Stability and toxicity of selected chlorinated benzophenone-type UV filters in waters. Acta Chim. Slov. 2013, 60, 826–832. [Google Scholar]
- Santos, A.J.M.; Crista, D.M.A.; Miranda, M.S.; Almeida, I.F.; e Silva, J.P.S.; Costa, P.C.; Amaral, M.H.; Lobao, P.A.; Lobo, J.M.S.; da Silva, J.C.E. Degradation of UV filter 2-ethylhexyl-4-methoxycinnamate and 4-tert-butyl-4-methoxy-dibenzoyl methane in chlorinated water. Environ. Chem. 2013, 10, 127–134. [Google Scholar] [CrossRef] [Green Version]
- Crista, D.M.A.; Miranda, M.S.; Esteves da Silva, J.C.G. Degradation in chlorinated water of the UV filter 4-tert-butyl-4’-methoxy-dibenzoyl methane present in commercial sunscreens. Environ. Technol. 2015, 36, 1319–1326. [Google Scholar] [CrossRef]
- Trebše, P.; Polyakova, O.V.; Baranova, M.; Kralj, M.B.; Dolenc, D.; Sarakha, M.; Kutin, A.; Lebedev, A.T. Transformations of avobenzone in conditions of aquatic chlorination and UV irradiation. Water Res. 2016, 101, 95–102. [Google Scholar] [CrossRef]
- Detenchuk, E.A.; Trebše, P.; Marjanović, A.; Kosyakov, D.S.; Ul’yanovskii, N.V.; Kralj, M.B.; Lebedev, A.T. Transformation of resveratrol under disinfection conditions. Chemosphere 2020, 260, 1–11. [Google Scholar] [CrossRef]
- Joll, C.A.; Alessandrino, M.J.; Heitz, A. Disinfection by-products from halogenation of aqueous solutions of terpenoids. Water Res. 2010, 44, 232–242. [Google Scholar] [CrossRef] [Green Version]
- Freitas, J.V.; Lopes, N.P.; Gaspar, L.R. Photostability evaluation of five UV-filters, trans-resveratrol and beta-carotene in sunscreens. Eur. J. Pharm. Sci. 2015, 78, 79–89. [Google Scholar] [CrossRef]
- Nedorost, S.T. Facial erythema as a result of benzophenone allergy. J. Am. Acad. Dermatol. 2003, 49 (Suppl. S5), 259–261. [Google Scholar] [CrossRef]
- Burnet, M.E.; Wang, S.Q. Current sunscreen controversies: A critical review. Photodermatol. Photoimmunol. Photomed. 2011, 27, 58–67. [Google Scholar] [CrossRef]
- Fitzpatrick, T.B. The validity and practicality of sun-reactive skin types I through VI. Arch. Dermatol. 1988, 124, 869–871. [Google Scholar] [CrossRef]
- Maibach, H.; Honari, G. Photoirritation (Phototoxicity): Clinical Aspects. In Applied Dermatotoxicology: Clinical Aspects, 1st ed.; Elsevier Inc.; Academic Press: San Francisco, CA, USA, 2014; pp. 41–56. [Google Scholar]
- Fullerton, A.; Fischer, T.; Lahti, A.; Wilhelm, K.P.; Takiwaki, H.; Serup, J. Guidelines for measurement skin color and erythema A report from the standardization group of the European society of contact dermatitis. Contact Dermat. 1996, 35, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Weatherall, I.L.; Coombs, B.D. Skin Color measurements in terms of CIELAB color space values. J. Investig. Dermatol. 1992, 99, 468–473. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Clarys, P.; Alewaeters, K.; Lambrecht, R.; Barel, A.O. Skin color measurements: Comparison between three instruments: The Chromameter®, the DermaSpectrometer® and the Mexameter®. Ski. Res. Technol. 2000, 6, 230–238. [Google Scholar] [CrossRef]
- Gaspar, L.R.; Campos, P.M.B.G.M. Photostability and efficacy studies of topical formulations containing UV-filters combination and vitamins A, C, and E. Int. J. Pharm. 2007, 343, 181–189. [Google Scholar] [CrossRef] [PubMed]
- Sherwood, V.F.; Kennedy, S.; Zhang, H.; Purser, G.H.; Sheaff, R.J. Altered UV absorbance and cytotoxicity of chlorinated sunscreen agents. Cutan. Ocul. Toxicol. 2012, 31, 273–279. [Google Scholar] [CrossRef] [PubMed]
- Berbicz, F.; Nogueira, A.C.; Neto, A.M.; Natali, M.R.M.; Baesso, M.L.; Matioli, G. Use of photoacoustic spectroscopy in the characterization of inclusion complexes of benzophenone-3-hydroxypropyl-β-cyclodextrin and ex vivo evaluation of the percutaneous penetration of sunscreen. Eur. J. Pharm. Biopharm. 2011, 79, 449–457. [Google Scholar] [CrossRef] [PubMed]
- Siqueira, N.M.; Contri, R.V.; Paese, K.; Beck, R.C.R.; Pohlmann, A.R.; Guterres, S.S. Innovative sunscreen formulation based on benzophenone-3-loaded chitosan-coated polymeric nanocapsules. Ski. Pharmacol. Physiol. 2011, 24, 166–174. [Google Scholar] [CrossRef]
- Vilela, F.M.P.; Oliveira, F.M.; Vicentini, F.T.M.C.; Casagrande, R.; Verri, W.A., Jr.; Cunha, T.M.; Fonseca, M.J. Commercial sunscreen formulations: UVB irradiation stability and effect on UVB irradiation-induced skin oxidative stress and inflammation. J. Photochem. Photobiol. B Biol. 2016, 163, 413–420. [Google Scholar] [CrossRef]
- Geoffrey, K.; Mwangi, A.N.; Maru, S.M. Sunscreen products: Rational of use, formulation development and regulatory considerations. Saudi Pharm. J. 2019, 27, 1009–1018. [Google Scholar] [CrossRef]
- Lee, Y.M.; Lee, G.; Kim, M.K.; Zoh, K.D. Kinetics and degradation mechanism of Benzophenone-3 in chlorination and UV/chlorination reactions. Chem. Eng. J. 2020, 393, 124780. [Google Scholar] [CrossRef]
| Time of Exposure [min] | Hue Angle–Mean Value [°] | Std. Deviation [°] |
|---|---|---|
| 0 | 56.0 | 6.3 |
| 4 | 56.5 | 7.6 |
| 6 | 54.5 | 7.7 |
| 8 | 48.5 | 8.0 |
| Comparisons | F-Ratio | Significance |
|---|---|---|
| Observation at 0 min vs. 4 min | 0.145 | 0.706 |
| Observation at 4 min vs. 6 min | 4.503 | 0.041 |
| Observation at 6 min vs. 8 min | 27.912 | 0.000 |
| Descriptve Analyses | Mean (Hue Angle) | Std. Deviation |
|---|---|---|
| Covered skin | 56.1 | 6.0 |
| Positive control | 51.9 | 8.2 |
| Neutral ointment without additives | 49.6 | 7.2 |
| UV filter–benzophenone 3 | 57.6 | 5.9 |
| UV filter–benzophenone 3 + chlorinated water | 57.4 | 7.1 |
| UV filter–benzophenone 3 + β-carotene | 58.7 | 6.4 |
| UV filter–benzophenone 3 + trans-resveratrol | 58.0 | 5.9 |
| Comparisons | Mean ± Std. Dev. | 95% Confidence | Sig. (2-Tailed) | |
|---|---|---|---|---|
| Lower | Upper | |||
| 1st Pair: Controls comparison | ||||
| Uncovered–Covered skin | −4.1 ± 7.0 | −7.0 | −1.3 | 0.006 |
| 2nd Pair: Neutral ointment without additives | ||||
| Covered skin | −6.5 ± 7.6 | −9.5 | −3.4 | 0.000 |
| Uncovered skin | −2.3 ± 3.9 | −3.9 | −0.7 | 0.005 |
| 3rd Pair: BP-3 | ||||
| Covered skin | 1.5 ± 4.1 | −0.2 | 3.1 | 0.075 |
| Uncovered skin | 5.6 ± 5.9 | 3.2 | 8.0 | 0.000 |
| 4th Pair BP-3 with the addition of chlorinated water | ||||
| Covered skin | 1.3 ± 4.9 | −0.7 | 3.3 | 0.188 |
| Uncovered skin | 5.4 ± 6.5 | 2.8 | 8.1 | 0.000 |
| 5th Pair BP-3 with the addition of β-carotene | ||||
| Covered skin | 2.6 ± 3.8 | 1.1 | 4.1 | 0.002 |
| Uncovered skin | 6.7 ± 6.7 | 4.0 | 9.5 | 0.000 |
| 6th Pair BP-3 − trans-resveratrol | ||||
| Covered skin | 2.0 ± 4.4 | 0.2 | 3.7 | 0.031 |
| Uncovered skin | 6.1 ± 6.3 | 3.6 | 8.6 | 0.000 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sotler, R.; Adamič, M.; Jarni, K.; Dahmane, R.; Trebše, P.; Kralj, M.B. Analyzing the Photoprotection Efficiency of Sunscreens Containing Antioxidants under Disinfection Conditions. Antioxidants 2021, 10, 1720. https://doi.org/10.3390/antiox10111720
Sotler R, Adamič M, Jarni K, Dahmane R, Trebše P, Kralj MB. Analyzing the Photoprotection Efficiency of Sunscreens Containing Antioxidants under Disinfection Conditions. Antioxidants. 2021; 10(11):1720. https://doi.org/10.3390/antiox10111720
Chicago/Turabian StyleSotler, Robert, Metka Adamič, Kristjan Jarni, Raja Dahmane, Polonca Trebše, and Mojca Bavcon Kralj. 2021. "Analyzing the Photoprotection Efficiency of Sunscreens Containing Antioxidants under Disinfection Conditions" Antioxidants 10, no. 11: 1720. https://doi.org/10.3390/antiox10111720
APA StyleSotler, R., Adamič, M., Jarni, K., Dahmane, R., Trebše, P., & Kralj, M. B. (2021). Analyzing the Photoprotection Efficiency of Sunscreens Containing Antioxidants under Disinfection Conditions. Antioxidants, 10(11), 1720. https://doi.org/10.3390/antiox10111720







