Hydrogen Sulfide and Carbon Monoxide Tolerance in Bacteria
Abstract
:1. Introduction
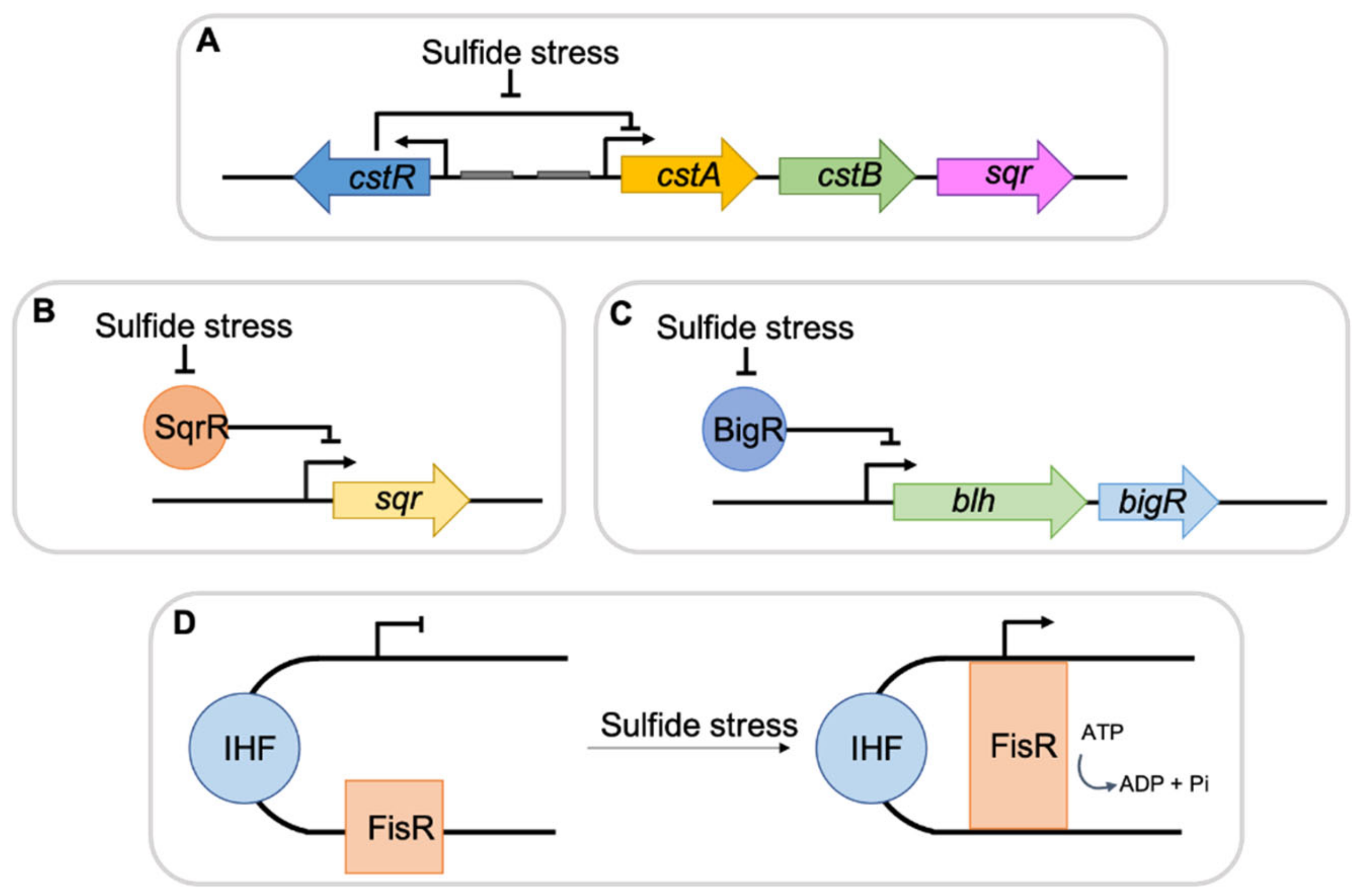
2. Bacterial Responses to H2S
3. H2S Producing Bacteria Confer Self-Protection against Oxidative Stress
4. H2S and Microbial Antibiotic Resistance
5. H2S in Host-Pathogen Interactions
6. CO Utilizing Bacteria
7. Bacterial Responses to Toxic CO
8. CO Producing Bacteria
9. CO and H2S in Host-Pathogen Interactions
10. H2S and CO Interplay
11. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Predmore, B.L.; Lefer, D.J.; Gojon, G. Hydrogen Sulfide in Biochemistry and Medicine. Antioxid. Redox Signal. 2012, 17, 119–140. [Google Scholar] [CrossRef] [Green Version]
- Siracusa, R.; Schaufler, A.; Calabrese, V.; Fuller, P.M.; Otterbein, L.E. Carbon Monoxide: From Poison to Clinical Trials. Trends Pharmacol. Sci. 2021, 42, 329–339. [Google Scholar] [CrossRef]
- Ereño-Orbea, J.; Majtan, T.; Oyenarte, I.; Kraus, J.P.; Martínez-Cruza, L.A. Structural Basis of Regulation and Oligomerization of Human Cystathionine β-Synthase, the Central Enzyme of Transsulfuration. Proc. Natl. Acad. Sci. USA 2013, 110. [Google Scholar] [CrossRef] [Green Version]
- Zuhra, K.; Augsburger, F.; Majtan, T.; Szabo, C. Cystathionine-β-Synthase: Molecular Regulation and Pharmacological Inhibition. Biomolecules 2020, 10, 697. [Google Scholar] [CrossRef]
- Szabo, C. Hydrogen Sulfide, an Endogenous Stimulator of Mitochondrial Function in Cancer Cells. Cells 2021, 10, 220. [Google Scholar] [CrossRef] [PubMed]
- Gullotta, F.; di Masi, A.; Coletta, M.; Ascenzi, P. CO Metabolism, Sensing, and Signaling. BioFactors 2012, 38, 1–13. [Google Scholar] [CrossRef] [Green Version]
- Gullotta, F.; Di Masi, A.; Ascenzi, P. Carbon Monoxide: An Unusual Drug. IUBMB Life 2012, 64, 378–386. [Google Scholar] [CrossRef]
- Kourti, M.; Jiang, W.G.; Cai, J. Aspects of Carbon Monoxide in Form of CO-Releasing Molecules Used in Cancer Treatment: More Light on the Way. Oxid. Med. Cell. Longev. 2017, 2017. [Google Scholar] [CrossRef]
- Ryter, S.W. Therapeutic Potential of Heme Oxygenase-1 and Carbon Monoxide in Acute Organ Injury, Critical Illness, and Inflammatory Disorders. Antioxidants 2020, 9, 1153. [Google Scholar] [CrossRef]
- Ritter, J.M. Human Pharmacology of Hydrogen Sulfide, Putative Gaseous Mediator. Br. J. Clin. Pharmacol. 2010, 69, 573–575. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shatalin, K.; Shatalina, E.; Mironov, A.; Nudler, E. H2S: A Universal Defense Against Antibiotics in Bacteria. Science 2011, 334, 986–990. [Google Scholar] [CrossRef]
- Li, Q.; Lancaster, J.R. Chemical Foundations of Hydrogen Sulfide Biology. Nitric Oxide Biol. Chem. 2013, 35, 21–34. [Google Scholar] [CrossRef] [Green Version]
- Fu, L.H.; Wei, Z.Z.; Hu, K.D.; Hu, L.Y.; Li, Y.H.; Chen, X.Y.; Han, Z.; Yao, G.F.; Zhang, H. Hydrogen Sulfide Inhibits the Growth of Escherichia Coli through Oxidative Damage. J. Microbiol. 2018, 56, 238–245. [Google Scholar] [CrossRef] [PubMed]
- Wu, G.; Wan, F.; Fu, H.; Li, N.; Gao, H. A Matter of Timing: Contrasting Effects of Hydrogen Sulfide on Oxidative Stress Response in Shewanella oneidensis. J. Bacteriol. 2015, 197, 3563–3572. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fu, L.H.; Hu, K.D.; Hu, L.Y.; Li, Y.H.; Hu, L.B.; Yan, H.; Liu, Y.S.; Zhang, H. An Antifungal Role of Hydrogen Sulfide on the Postharvest Pathogens Aspergillus niger and Penicillium italicum. PLoS ONE 2014, 9. [Google Scholar] [CrossRef] [Green Version]
- Ng, S.Y.; Ong, K.X.; Surendran, S.T.; Sinha, A.; Lai, J.J.H.; Chen, J.; Liang, J.; Tay, L.K.S.; Cui, L.; Loo, H.L.; et al. Hydrogen Sulfide Sensitizes Acinetobacter baumannii to Killing by Antibiotics. Front. Microbiol. 2020, 11, 1–9. [Google Scholar] [CrossRef]
- Kolluru, G.K.; Shen, X.; Bir, S.C.; Kevil, C.G. Hydrogen Sulfide Chemical Biology: Pathophysiological Roles and Detection. Nitric Oxide Biol. Chem. 2013, 35, 5–20. [Google Scholar] [CrossRef] [Green Version]
- Aroca, A.; Gotor, C.; Bassham, D.C.; Romero, L.C. Hydrogen Sulfide: From a Toxic Molecule to a Key Molecule of Cell Life. Antioxidants 2020, 9, 621. [Google Scholar] [CrossRef] [PubMed]
- Avalos, M.; van Wezel, G.P.; Raaijmakers, J.M.; Garbeva, P. Healthy Scents: Microbial Volatiles as New Frontier in Antibiotic Research? Curr. Opin. Microbiol. 2018, 45, 84–91. [Google Scholar] [CrossRef] [Green Version]
- Juarez, G.E.; Mateyca, C.; Galvan, E.M. Proteus Mirabilis Outcompetes Klebsiella pneumoniae in Artificial Urine Medium through Secretion of Ammonia and Other Volatile Compounds. Heliyon 2020, 6, e03361. [Google Scholar] [CrossRef]
- Shimizu, T.; Masuda, S. Persulphide-Responsive Transcriptional Regulation and Metabolism in Bacteria. J. Infect. Dis. 2019, 220, 125–132. [Google Scholar] [CrossRef]
- Walsh, B.J.C.; Wang, J.; Edmonds, K.A.; Palmer, L.D.; Zhang, Y.; Trinidad, J.C.; Skaar, E.P.; Giedroc, D.P. The Response of Acinetobacter baumannii to Hydrogen Sulfide Reveals Two Independent Persulfide-Sensing Systems and a Connection to Biofilm Regulation. MBio 2020, 11, 1–18. [Google Scholar] [CrossRef]
- Walsh, B.J.C.; Giedroc, D.P. H2S and Reactive Sulfur Signaling at the Host-Bacterial Pathogen Interface. J. Biol. Chem. 2020, 295, 13150–13168. [Google Scholar] [CrossRef] [PubMed]
- Forte, E.; Borisov, V.B.; Falabella, M.; Colaço, H.G.; Tinajero-Trejo, M.; Poole, R.K.; Vicente, J.B.; Sarti, P.; Giuffre, A. The Terminal Oxidase Cytochrome bd Promotes Sulfide-Resistant Bacterial Respiration and Growth. Sci. Rep. 2016, 6, 23788. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tanous, C.; Soutourina, O.; Raynal, B.; Hullo, M.F.; Mervelet, P.; Gilles, A.M.; Noirot, P.; Danchin, A.; England, P.; Martin-Verstraete, I. The CymR Regulator in Complex with the Enzyme CysK Controls Cysteine Metabolism in Bacillus subtilis. J. Biol. Chem. 2008, 283, 35551–35560. [Google Scholar] [CrossRef] [Green Version]
- Peng, H.; Zhang, Y.; Palmer, L.D.; Kehl-Fie, T.E.; Skaar, E.P.; Trinidad, J.C.; Giedroc, D.P. Hydrogen Sulfide and Reactive Sulfur Species Impact Proteome S-Sulfhydration and Global Virulence Regulation in Staphylococcus aureus. ACS Infect. Dis. 2017, 3, 744–755. [Google Scholar] [CrossRef] [Green Version]
- Soutourina, O.; Poupel, O.; Coppée, J.Y.; Danchin, A.; Msadek, T.; Martin-Verstraete, I. CymR, the Master Regulator of Cysteine Metabolism in Staphylococcus aureus, Controls Host Sulphur Source Utilization and Plays a Role in Biofilm Formation. Mol. Microbiol. 2009, 73, 194–211. [Google Scholar] [CrossRef]
- Shen, J.; Peng, H.; Zhang, Y.; Trinidad, J.C.; Giedroc, D.P. Staphylococcus aureus sqr Encodes a Type II Sulfide:Quinone Oxidoreductase and Impacts Reactive Sulfur Speciation in Cells. Biochemistry 2016, 55, 6524–6534. [Google Scholar] [CrossRef] [Green Version]
- Luebke, J.L.; Shen, J.; Bruce, K.E.; Kehl-Fie, T.E.; Peng, H.; Skaar, E.P.; Giedroc, D.P. The CsoR-like Sulfurtransferase Repressor (CstR) Is a Persulfide Sensor in Staphylococcus aureus. Mol. Microbiol. 2014, 94, 1343–1360. [Google Scholar] [CrossRef] [Green Version]
- Peng, H.; Shen, J.; Edmonds, K.A.; Luebke, J.L.; Hickey, A.K.; Palmer, L.D.; Chang, F.-M.J.; Bruce, K.A.; Kehl-Fie, T.E.; Skaar, E.P.; et al. Sulfide Homeostasis and Nitroxyl Intersect via Formation of Reactive Sulfur Species in Staphylococcus aureus. mSphere 2017, 2, 1–21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weikum, J.; Ritzmann, N.; Jelden, N.; Klockner, A.; Herkersdorf, S.; Josten, M.; Sahl, H.-G.; Grein, F. Sulfide Protects Staphylococcus aureus from Aminoglycoside Antibiotics but Cannot Be Regarded as a General Defense Mechanism against Antibiotics. Antimicrob. Agents Chemother. 2018, 62, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Mironov, A.; Seregina, T.; Nagornykh, M.; Luhachack, L.G.; Korolkova, N.; Lopes, L.E.; Kotova, V.; Zavilgelsky, G.; Shakulov, R.; Shatalin, K.; et al. Mechanism of H2S-Mediated Protection against Oxidative Stress in Escherichia coli. Proc. Natl. Acad. Sci. USA 2017, 114, 6022–6027. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ono, K.; Kitamura, Y.; Zhang, T.; Tsutsuki, H.; Rahman, A.; Ihara, T.; Akaike, T.; Sawa, T. Cysteine Hydropersulfide Inactivates β-Lactam Antibiotics with Formation of Ring-Opened Carbothioic S-Acids in Bacteria. ACS Chem. Biol. 2021, 16, 731–739. [Google Scholar] [CrossRef] [PubMed]
- Rahman, M.A.; Glasgow, J.N.; Nadeem, S.; Reddy, V.P.; Sevalkar, R.R.; Lancaster, J.R.; Steyn, A.J.C. The Role of Host-Generated H2S in Microbial Pathogenesis: New Perspectives on Tuberculosis. Front. Cell. Infect. Microbiol. 2020, 10, 586923. [Google Scholar] [CrossRef]
- Pal, V.K.; Bandyopadhyay, P.; Singh, A. Hydrogen Sulfide in Physiology and Pathogenesis of Bacteria and Viruses. IUBMB Life 2018, 70, 393–410. [Google Scholar] [CrossRef] [PubMed]
- Xie, Z.Z.; Liu, Y.; Bian, J.S. Hydrogen Sulfide and Cellular Redox Homeostasis. Oxid. Med. Cell. Longev. 2016, 2016. [Google Scholar] [CrossRef] [Green Version]
- Benedetti, F.; Curreli, S.; Krishnan, S.; Davinelli, S.; Cocchi, F.; Scapagnini, G.; Gallo, R.C.; Zella, D. Anti-Inflammatory Effects of H2S during Acute Bacterial Infection: A Review. J. Transl. Med. 2017, 15, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Sun, F.; Luo, J.H.; Yue, T.T.; Wang, F.X.; Yang, C.L.; Zhang, S.; Wang, X.Q.; Wang, C.Y. The Role of Hydrogen Sulphide Signalling in Macrophage Activation. Immunology 2021, 162, 3–10. [Google Scholar] [CrossRef]
- Wallace, J.L.; Ferraz, J.G.P.; Muscara, M.N. Hydrogen Sulfide: An Endogenous Mediator of Resolution of Inflammation and Injury. Antioxid. Redox Signal. 2012, 17, 58–67. [Google Scholar] [CrossRef]
- Rivers-Auty, J. An Evolutionary Perspective on the Immunomodulatory Role of Hydrogen Sulphide. Med. Hypotheses 2015, 85, 612–617. [Google Scholar] [CrossRef]
- Li, L.; Bhatia, M.; Zhu, Y.Z.; Zhu, Y.C.; Ramnath, R.D.; Wang, Z.J.; Anuar, F.B.M.; Whiteman, M.; Salto-Tellez, M.; Moore, P.K. Hydrogen Sulfide Is a Novel Mediator of Lipopolysaccharide-induced Inflammation in the Mouse. FASEB J. 2005, 19, 1196–1198. [Google Scholar] [CrossRef]
- Whiteman, M.; Li, L.; Rose, P.; Tan, C.H.; Parkinson, D.B.; Moore, P.K. The Effect of Hydrogen Sulfide Donors on Lipopolysaccharide-Induced Formation of Inflammatory Mediators in Macrophages. Antioxid. Redox Signal. 2010, 12, 1147–1154. [Google Scholar] [CrossRef]
- Aslami, H.; Pulskens, W.P.; Kuipers, M.T.; Bos, A.P.; van Kuilenburg, A.B.P.; Wanders, R.J.A.; Roelofsen, J.; Roelofs, J.J.T.H.; Kerindongo, R.P.; Beurskens, C.J.P.; et al. Hydrogen Sulfide Donor NaHS Reduces Organ Injury in a Rat Model of Pneumococcal pneumosepsis, Associated with Improved Bio-Energetic Status. PLoS ONE 2013, 8. [Google Scholar] [CrossRef]
- Bazhanov, N.; Ansar, M.; Ivanciuc, T.; Garofalo, R.P.; Casola, A. Hydrogen Sulfide: A Novel Player in Airway Development, Pathophysiology of Respiratory Diseases, and Antiviral Defenses. Am. J. Respir. Cell Mol. Biol. 2017, 57, 403–410. [Google Scholar] [CrossRef]
- Citi, V.; Martelli, A.; Brancaleone, V.; Brogi, S.; Gojon, G.; Montanaro, R.; Morales, G.; Testai, L.; Calderone, V. Anti-Inflammatory and Antiviral Roles of Hydrogen Sulfide: Rationale for Considering H2S Donors in COVID-19 Therapy. Br. J. Pharmacol. 2020, 177, 4931–4941. [Google Scholar] [CrossRef] [PubMed]
- Yang, G. MINI-REVIEW H2S as a Potential Defense against COVID-19? J Physiol Cell Physiol 2020, 319, 244–249. [Google Scholar] [CrossRef] [PubMed]
- Garg, S.; Vitvitsky, V.; Gendelman, H.E.; Banerjee, R. Monocyte Differentiation, Activation, and Mycobacterial Killing Are Linked to Transsulfuration-Dependent Redox Metabolism. J. Biol. Chem. 2006, 281, 38712–38720. [Google Scholar] [CrossRef] [Green Version]
- Benedetti, F.; Davinelli, S.; Krishnan, S.; Gallo, R.C.; Scapagnini, G.; Zella, D.; Curreli, S. Sulfur Compounds Block MCP-1 Production by Mycoplasma Fermentans-Infected Macrophages through NF-κB Inhibition. J. Transl. Med. 2014, 12, 1–11. [Google Scholar] [CrossRef] [Green Version]
- Gemici, B.; Wallace, J.L. Anti-Inflammatory and Cytoprotective Properties of Hydrogen Sulfide. Methods Enzymol. 2015, 555, 169–193. [Google Scholar] [CrossRef]
- Sen, N.; Paul, B.D.; Gadalla, M.M.; Mustafa, A.K.; Sen, T.; Xu, R.; Kim, S.; Snyder, S.H. Hydrogen Sulfide-Linked Sulfhydration of NF-κB Mediates Its Antiapoptotic Actions. Mol. Cell 2012, 45, 13–24. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saini, V.; Chinta, K.C.; Reddy, V.P.; Glasgow, J.N.; Stein, A.; Lamprecht, D.A.; Rahman, M.A.; Mackenzie, J.S.; Truebody, B.E.; Adamson, J.H.; et al. Hydrogen Sulfide Stimulates Mycobacterium tuberculosis Respiration, Growth and Pathogenesis. Nat. Commun. 2020, 11, 1–17. [Google Scholar] [CrossRef]
- Rowan, F.E.; Docherty, N.G.; Coffey, J.C.; O’Connell, P.R. Sulphate-Reducing Bacteria and Hydrogen Sulphide in the Aetiology of Ulcerative Colitis. Br. J. Surg. 2009, 96, 151–158. [Google Scholar] [CrossRef] [PubMed]
- Toliver-kinsky, T.; Cui, W.; Lee, S.; Shatalin, K.; Nudler, E.; Szabo, C. H2S, a Bacterial Defense Mechanism against the Host Immune Response. Infect. Immun. 2018, 87, 1–11. [Google Scholar] [CrossRef] [Green Version]
- Hampelska, K.; Jaworska, M.M.; Babalska, Z.Ł.; Karpiński, T.M. The Role of Oral Microbiota in Intra-Oral Halitosis. J. Clin. Med. 2020, 9, 2484. [Google Scholar] [CrossRef]
- Diender, M.; Stams, A.J.M.; Sousa, D.Z. Pathways and Bioenergetics of Anaerobic Carbon Monoxide Fermentation. Front. Microbiol. 2015, 6, 1275. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, Z.Y.; Jia, D.C.; Zhang, K.D.; Zhu, H.F.; Zhang, Q.; Jiang, W.H.; Gu, Y.; Li, F.L. Erratum for Liu et al., “Ethanol Metabolism Dynamics in Clostridium ljungdahlii Grown on Carbon Monoxide.”. Appl. Environ. Microbiol. 2020, 86, 2376. [Google Scholar] [CrossRef]
- Abrini, J.; Naveau, H.; Nyns, E.J. Clostridium autoethanogenum, sp. Nov., an Anaerobic Bacterium That Produces Ethanol from Carbon Monoxide. Arch. Microbiol. 1994, 161, 345–351. [Google Scholar] [CrossRef]
- Robb, F.T.; Techtmann, S.M. Life on the Fringe: Microbial Adaptation to Growth on Carbon Monoxide. F1000Research 2018, 7, 1981. [Google Scholar] [CrossRef]
- Ragsdale, S.W. Life with Carbon Monoxide. Crit. Rev. Biochem. Mol. Biol. 2004, 39, 165–195. [Google Scholar] [CrossRef]
- Fukuyama, Y.; Inoue, M.; Omae, K.; Yoshida, T.; Sako, Y. Anaerobic and Hydrogenogenic Carbon Monoxide-Oxidizing Prokaryotes: Versatile Microbial Conversion of a Toxic Gas into an Available Energy, 1st ed.; Elsevier Inc.: Amsterdam, The Netherlands, 2020; Volume 110, ISBN 9780128207031. [Google Scholar]
- Svetlitchnyi, V.; Peschel, C.; Acker, G.; Meyer, O. Two Membrane-Associated NiFeS-Carbon Monoxide Dehydrogenases from the Anaerobic Carbon-Monoxide-Utilizing Eubacterium Carboxydothermus hydrogenoformans. J. Bacteriol. 2001, 183, 5134–5144. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Youn, H.; Kerby, R.L.; Conrad, M.; Roberts, G.P. Functionally Critical Elements of CooA-Related CO Sensors. J. Bacteriol. 2004, 186, 1320–1329. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, Y.M.; Park, S.W. Microbiology and Genetics of CO Utilization in Mycobacteria. Antonie Van Leeuwenhoek 2012, 101, 685–700. [Google Scholar] [CrossRef] [PubMed]
- King, G.M.; Weber, C.F. Distribution, Diversity and Ecology of Aerobic CO-Oxidizing Bacteria. Nat. Rev. Microbiol. 2007, 5, 107–118. [Google Scholar] [CrossRef] [PubMed]
- Henstra, A.M.; Dijkema, C.; Stams, A.J.M. Archaeoglobus fulgidus Couples CO Oxidation to Sulfate Reduction and Acetogenesis with Transient Formate Accumulation. Environ. Microbiol. 2007, 9, 1836–1841. [Google Scholar] [CrossRef]
- Plugge, C.M.; Sousa, J.A.B.; Christel, S.; Dopson, M.; Bijmans, M.F.M.; Stams, A.J.M.; Diender, M. Syngas as Electron Donor for Sulfate and Thiosulfate Reducing Haloalkaliphilic Microorganisms in a Gas-Lift Bioreactor. Microorganisms 2020, 8, 1451. [Google Scholar] [CrossRef]
- Oelgeschläger, E.; Rother, M. Carbon Monoxide-Dependent Energy Metabolism in Anaerobic Bacteria and Archaea. Arch. Microbiol. 2008, 190, 257–269. [Google Scholar] [CrossRef]
- Wilson, J.L.; Jesse, H.E.; Poole, R.K.; Davidge, K.S. Antibacterial Effects of Carbon Monoxide. Curr. Pharm. Biotechnol. 2012, 13, 760–768. [Google Scholar] [CrossRef]
- Romão, C.C.; Blättler, W.A.; Seixas, J.D.; Bernardes, G.J.L. Developing Drug Molecules for Therapy with Carbon Monoxide. Chem. Soc. Rev. 2012, 41, 3571–3583. [Google Scholar] [CrossRef]
- Zegdi, R.; Perrin, D.; Burdin, M.; Boiteau, R.; Tenaillon, A. Increased Endogenous Carbon Monoxide Production in Severe Sepsis. Intensive Care Med. 2002, 28, 793–796. [Google Scholar] [CrossRef]
- Foresti, R.; Bani-Hani, M.G.; Motterlini, R. Use of Carbon Monoxide as a Therapeutic Agent: Promises and Challenges. Intensive Care Med. 2008, 34, 649–658. [Google Scholar] [CrossRef]
- Nobre, L.S.; Seixas, J.D.; Romão, C.C.; Saraiva, L.M. Antimicrobial Action of Carbon Monoxide-Releasing Compounds. Antimicrob. Agents Chemother. 2007, 51, 4303–4307. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chin, B.Y.; Otterbein, L.E. Carbon Monoxide Is a Poison... to Microbes! CO as a Bactericidal Molecule. Curr. Opin. Pharmacol. 2009, 9, 490–500. [Google Scholar] [CrossRef] [PubMed]
- Chaves-Ferreira, M.; Albuquerque, I.S.; Matak-Vinkovic, D.; Coelho, A.C.; Carvalho, S.M.; Saraiva, L.M.; Romão, C.C.; Bernardes, G.J.L. Spontaneous CO Release from RuII(CO)2-Protein Complexes in Aqueous Solution, Cells, and Mice. Angew. Chemie Int. Ed. 2015, 54, 1172–1175. [Google Scholar] [CrossRef] [Green Version]
- Motterlini, R.; Mann, B.E.; Foresti, R. Therapeutic Applications of Carbon Monoxide-Releasing Molecules. Expert Opin. Investig. Drugs 2005, 14, 1305–1318. [Google Scholar] [CrossRef] [PubMed]
- Nobre, L.S.; Jeremias, H.; Romão, C.C.; Saraiva, L.M. Examining the Antimicrobial Activity and Toxicity to Animal Cells of Different Types of CO-Releasing Molecules. Dalt. Trans. 2016, 45, 1455–1466. [Google Scholar] [CrossRef]
- Tavares, A.F.; Parente, M.R.; Justino, M.C.; Oleastro, M.; Nobre, L.S.; Saraiva, L.M. The Bactericidal Activity of Carbon Monoxide-Releasing Molecules against Helicobacter Pylori. PLoS ONE 2013, 8. [Google Scholar] [CrossRef] [Green Version]
- Desmard, M.; Davidge, K.S.; Bouvet, O.; Morin, D.; Roux, D.; Foresti, R.; Ricard, J.D.; Denamur, E.; Poole, R.K.; Montravers, P.; et al. A Carbon Monoxide-releasing Molecule (CORM-3) Exerts Bactericidal Activity against Pseudomonas aeruginosa and Improves Survival in an Animal Model of Bacteraemia. FASEB J. 2009, 23, 1023–1031. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Murray, T.S.; Okegbe, C.; Gao, Y.; Kazmierczak, B.I.; Motterlini, R.; Dietrich, L.E.P.; Bruscia, E.M. The Carbon Monoxide Releasing Molecule CORM-2 Attenuates Pseudomonas aeruginosa Biofilm Formation. PLoS ONE 2012, 7, e35499. [Google Scholar] [CrossRef]
- Sahlberg Bang, C.; Kruse, R.; Johansson, K.; Persson, K. Carbon Monoxide Releasing Molecule-2 (CORM-2) Inhibits Growth of Multidrug-Resistant Uropathogenic Escherichia coli in Biofilm and Following Host Cell Colonization. BMC Microbiol. 2016, 16, 64. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bang, C.S.; Kruse, R.; Demirel, I.; Önnberg, A.; Söderquist, B.; Persson, K. Multiresistant Uropathogenic Extended-Spectrum β-Lactamase (ESBL)-Producing Escherichia coli Are Susceptible to the Carbon Monoxide Releasing Molecule-2 (CORM-2). Microb. Pathog. 2014, 66, 29–35. [Google Scholar] [CrossRef]
- Bang, C.S.; Demirel, I.; Kruse, R.; Persson, K. Global Gene Expression Profiling and Antibiotic Susceptibility after Repeated Exposure to the Carbon Monoxide-Releasing Molecule-2 (CORM-2) in Multidrug-Resistant ESBL-Producing Uropathogenic Escherichia coli. PLoS ONE 2017, 12, e0178541. [Google Scholar] [CrossRef] [Green Version]
- Desmard, M.; Foresti, R.; Morin, D.; Dagoussat, M.; Berdeaux, A.; Denamur, E.; Crook, S.H.; Mann, B.E.; Scapens, D.; Montravers, P.; et al. Differential Antibacterial Activity against Pseudomonas aeruginosa by Carbon Monoxide-Releasing Molecules. Antioxid. Redox Signal. 2012, 16, 153–163. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wilson, J.L.; Jesse, H.E.; Hughes, B.; Lund, V.; Naylor, K.; Davidge, K.S.; Cook, G.M.; Mann, B.E.; Poole, R.K. Ru(CO)3Cl(Glycinate) (CORM-3): A Carbon Monoxide-Releasing Molecule with Broad-Spectrum Antimicrobial and Photosensitive Activities against Respiration and Cation Transport in Escherichia coli. Antioxid. Redox Signal. 2013, 19, 497–509. [Google Scholar] [CrossRef] [Green Version]
- Davidge, K.S.; Sanguinetti, G.; Yee, C.H.; Cox, A.G.; McLeod, C.W.; Monk, C.E.; Mann, B.E.; Motterlini, R.; Poole, R.K. Carbon Monoxide-Releasing Antibacterial Molecules Target Respiration and Global Transcriptional Regulators. J. Biol. Chem. 2009, 284, 4516–4524. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rana, N.; McLean, S.; Mann, B.E.; Poole, R.K. Interaction of the Carbon Monoxide-Releasing Molecule Ru(CO)3Cl(glycinate) (CORM-3) with Salmonella enterica Serovar Typhimurium: In Situ Measurements of Carbon Monoxide Binding by Integrating Cavity Dual-Beam Spectrophotometry. Microbiology 2014, 160, 2771–2779. [Google Scholar] [CrossRef]
- Ward, J.S.; Lynam, J.M.; Moir, J.; Fairlamb, I.J.S. Visible-Light-Induced CO Release from a Therapeutically Viable Tryptophan-Derived manganese(I) Carbonyl (TryptoCORM) Exhibiting Potent Inhibition against E. coli. Chem. A Eur. J. 2014, 20, 15061–15068. [Google Scholar] [CrossRef]
- Ward, J.S.; Morgan, R.; Lynam, J.M.; Fairlamb, I.J.S.; Moir, J.W.B. Toxicity of Tryptophan Manganese(I) Carbonyl (Trypto-CORM), against Neisseria Gonorrhoeae. Medchemcomm 2017, 8, 346–352. [Google Scholar] [CrossRef] [PubMed]
- Tinajero-Trejo, M.; Rana, N.; Nagel, C.; Jesse, H.E.; Smith, T.W.; Wareham, L.K.; Hippler, M.; Schatzschneider, U.; Poole, R.K. Antimicrobial Activity of the Manganese Photoactivated Carbon Monoxide-Releasing Molecule [Mn(CO)3(tpa-κ3N)]+ Against a Pathogenic Escherichia coli That Causes Urinary Infections. Antioxid. Redox Signal. 2016, 24, 765–780. [Google Scholar] [CrossRef] [Green Version]
- Betts, J.; Nagel, C.; Schatzschneider, U.; Poole, R.; La Ragione, R.M. Antimicrobial Activity of Carbon Monoxide-Releasing Molecule [Mn(CO)3(tpa-κ3N)]Br versus Multidrug-Resistant Isolates of Avian Pathogenic Escherichia coli and Its Synergy with Colistin. PLoS ONE 2017, 12, e0186359. [Google Scholar] [CrossRef] [Green Version]
- Nagel, C.; McLean, S.; Poole, R.K.; Braunschweig, H.; Kramer, T.; Schatzschneider, U. Introducing [Mn(CO)3(tpa-κ3N)]+ as a Novel Photoactivatable CO-Releasing Molecule with Well-Defined iCORM Intermediates-Synthesis, Spectroscopy, and Antibacterial Activity. Dalt. Trans. 2014, 43, 9986–9997. [Google Scholar] [CrossRef] [PubMed]
- Simpson, P.V.; Nagel, C.; Bruhn, H.; Schatzschneider, U. Antibacterial and Antiparasitic Activity of Manganese(I) Tricarbonyl Complexes with Ketoconazole, Miconazole, and Clotrimazole Ligands. Organometallics 2015, 34, 3809–3815. [Google Scholar] [CrossRef]
- Klinger-Strobel, M.; Gläser, S.; Makarewicz, O.; Wyrwa, R.; Weisser, J.; Pletz, M.W.; Schiller, A. Bactericidal Effect of a Photoresponsive Carbon Monoxide-Releasing Nonwoven against Staphylococcus aureus Biofilms. Antimicrob. Agents Chemother. 2016, 60, 4037–4046. [Google Scholar] [CrossRef] [Green Version]
- Flanagan, L.; Steen, R.R.; Saxby, K.; Klatter, M.; Aucott, B.J.; Winstanley, C.; Fairlamb, I.J.S.; Lynam, J.M.; Parkin, A.; Friman, V.P. The Antimicrobial Activity of a Carbon Monoxide Releasing Molecule (EBOR-CORM-1) Is Shaped by Intraspecific Variation within Pseudomonas aeruginosa Populations. Front. Microbiol. 2018, 9, 195. [Google Scholar] [CrossRef] [Green Version]
- Kaczara, P.; Motterlini, R.; Rosen, G.M.; Augustynek, B.; Bednarczyk, P.; Szewczyk, A.; Foresti, R.; Chlopicki, S. Carbon Monoxide Released by CORM-401 Uncouples Mitochondrial Respiration and Inhibits Glycolysis in Endothelial Cells: A Role for mitoBKCa Channels. Biochim. Biophys. Acta Bioenerg. 2015, 1847, 1297–1309. [Google Scholar] [CrossRef] [Green Version]
- Smith, H.; Mann, B.E.; Motterlini, R.; Poole, R.K. The Carbon Monoxide-Releasing Molecule, Corm-3 (Ru(CO) 3Cl(Glycinate)), Targets Respiration and Oxidases in Campylobacter jejuni, Generating Hydrogen Peroxide. IUBMB Life 2011, 63, 363–371. [Google Scholar] [CrossRef]
- Tavares, A.F.N.; Nobre, L.S.; Saraiva, L.M. A Role for Reactive Oxygen Species in the Antibacterial Properties of Carbon Monoxide-Releasing Molecules. FEMS Microbiol. Lett. 2012, 336, 1–10. [Google Scholar] [CrossRef]
- Tavares, A.F.N.; Teixeira, M.; Romão, C.C.; Seixas, J.D.; Nobre, L.S.; Saraiva, L.M. Reactive Oxygen Species Mediate Bactericidal Killing Elicited by Carbon Monoxide-Releasing Molecules. J. Biol. Chem. 2011, 286, 26708–26717. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Seixas, J.D.; Chaves-Ferreira, M.; Montes-Grajales, D.; Gonçalves, A.M.; Marques, A.R.; Saraiva, L.M.; Olivero-Verbel, J.; Romão, C.C.; Bernardes, G.J.L. An N-Acetyl Cysteine Ruthenium Tricarbonyl Conjugate Enables Simultaneous Release of CO and Ablation of Reactive Oxygen Species. Chem. A Eur. J. 2015, 21, 14708–14712. [Google Scholar] [CrossRef] [Green Version]
- Wilson, J.L.; McLean, S.; Begg, R.; Sanguinetti, G.; Poole, R.K. Analysis of Transcript Changes in a Heme-Deficient Mutant of Escherichia coli in Response to CORM-3 [Ru(CO)3Cl(glycinate)]. Genomics Data 2015, 5, 231–234. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carvalho, S.M.; Marques, J.; Romão, C.C.; Saraiva, L.M. Metabolomics of Escherichia coli Treated with the Antimicrobial Carbon Monoxide-Releasing Molecule CORM-3 Reveals Tricarboxylic Acid Cycle as Major Target. Antimicrob. Agents Chemother. 2019, 63, 1–18. [Google Scholar] [CrossRef]
- Santos-Silva, T.; Mukhopadhyay, A.; Seixas, J.D.; Bernardes, G.J.; Romao, C.C.; Romao, M.J. Towards Improved Therapeutic CORMs: Understanding the Reactivity of CORM-3 with Proteins. Curr. Med. Chem. 2011, 18, 3361–3366. [Google Scholar] [CrossRef] [Green Version]
- Kung, Y.; Doukov, T.I.; Seravalli, J.; Ragsdale, S.W.; Drennan, C.L. Crystallographic Snapshots of Cyanide- and Water-Bound C-Clusters from Bifunctional Carbon Monoxide Dehydrogenase/acetyl-CoA Synthase. Biochemistry 2009, 48, 7432–7440. [Google Scholar] [CrossRef] [Green Version]
- Stripp, S.T.; Goldet, G.; Brandmayr, C.; Sanganas, O.; Vincent, K.A.; Haumann, M.; Armstrong, F.A.; Happe, T. How Oxygen Attacks [FeFe] Hydrogenases from Photosynthetic Organisms. Proc. Natl. Acad. Sci. USA 2009, 106, 17331–17336. [Google Scholar] [CrossRef] [Green Version]
- Tsai, A.L.; Martin, E.; Berka, V.; Olson, J.S. How Do Heme-Protein Sensors Exclude Oxygen? Lessons Learned from Cytochrome c′, Nostoc Puntiforme Heme Nitric Oxide/oxygen-Binding Domain, and Soluble Guanylyl Cyclase. Antioxid. Redox Signal. 2012, 17, 1246–1263. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Roberts, G.P.; Youn, H.; Kerby, R.L. CO-Sensing Mechanisms. Microbiol. Mol. Biol. Rev. 2004, 68, 453–473. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Salman, B.I.; Ali, M.F.B.; Marzouq, M.A.; Hussein, S.A. Utility of the Fluorogenic Characters of Benzofurazan for Analysis of Tigecycline Using Spectrometric Technique; Application to Pharmacokinetic Study, Urine and Pharmaceutical Formulations. Luminescence 2019, 34, 175–182. [Google Scholar] [CrossRef]
- Kerby, R.L.; Youn, H.; Roberts, G.P. RcoM: A New Single-Component Transcriptional Regulator of CO Metabolism in Bacteria. J. Bacteriol. 2008, 190, 3336–3343. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gilles-Gonzalez, M.A.; Gonzalez, G.; Perutz, M.F.; Kiger, L.; Marden, M.C.; Poyart, C. Heme-Based Sensors, Exemplified by the Kinase FixL, Are a New Class of Heme Protein with Distinctive Ligand Binding and Autoxidation. Biochemistry 1994, 33, 8067–8073. [Google Scholar] [CrossRef]
- Chang, A.L.; Tuckerman, J.R.; Gonzalez, G.; Mayer, R.; Weinhouse, H.; Volman, G.; Amikam, D.; Benziman, M.; Gilles-Gonzalez, M.A. Phosphodiesterase A1, a Regulator of Cellulose Synthesis in Acetobacter xylinum, Is a Heme-Based Sensor. Biochemistry 2001, 40, 3420–3426. [Google Scholar] [CrossRef]
- Zhang, W.; Olson, J.S.; Phillips, G.N. Biophysical and Kinetic Characterization of HemAT, an Aerotaxis Receptor from Bacillus subtilis. Biophys. J. 2005, 88, 2801–2814. [Google Scholar] [CrossRef] [Green Version]
- Delgado-Nixon, V.M.; Gonzalez, G.; Gilles-Gonzalez, M.A. Dos, a Heme-Binding PAS Protein from Escherichia coli, Is a Direct Oxygen Sensor. Biochemistry 2000, 39, 2685–2691. [Google Scholar] [CrossRef] [PubMed]
- Shiloh, M.U.; Manzanillo, P.; Cox, J.S. Mycobacterium tuberculosis Senses Host-Derived Carbon Monoxide during Macrophage Infection. Cell Host Microbe 2008, 3, 323–330. [Google Scholar] [CrossRef] [Green Version]
- Sivaramakrishnan, S.; De Montellano, P.R.O. The DosS-DosT/DosR Mycobacterial Sensor System. Biosensors 2013, 3, 259–282. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wareham, L.K.; Begg, R.; Jesse, H.E.; Van Beilen, J.W.A.; Ali, S.; Svistunenko, D.; McLean, S.; Hellingwerf, K.J.; Sanguinetti, G.; Poole, R.K. Carbon Monoxide Gas Is Not Inert, but Global, in Its Consequences for Bacterial Gene Expression, Iron Acquisition, and Antibiotic Resistance. Antioxid. Redox Signal. 2016, 24, 1013–1028. [Google Scholar] [CrossRef] [Green Version]
- Nobre, L.S.; Al-Shahrour, F.; Dopazo, J.; Saraiva, L.M. Exploring the Antimicrobial Action of a Carbon Monoxide-Releasing Compound through Whole-Genome Transcription Profiling of Escherichia coli. Microbiology 2009, 155, 813–824. [Google Scholar] [CrossRef] [Green Version]
- Forte, E.; Borisov, V.B.; Siletsky, S.A.; Petrosino, M.; Giuffrè, A. In the Respiratory Chain of Escherichia coli Cytochromes bd-I and bd-II Are More Sensitive to Carbon Monoxide Inhibition than Cytochrome bo3. Biochim. Biophys. Acta Bioenerg. 2019, 1860, 148088. [Google Scholar] [CrossRef] [PubMed]
- Kajimura, M.; Fukuda, R.; Bateman, R.M.; Yamamoto, T.; Suematsu, M. Interactions of Multiple Gas-Transducing Systems: Hallmarks and Uncertainties of CO, NO, and H2S Gas Biology. Antioxid. Redox Signal. 2010, 13, 157–192. [Google Scholar] [CrossRef] [Green Version]
- Pazicni, S.; Cherney, M.M.; Lukat-Rodgers, G.S.; Oliveriusová, J.; Rodgers, K.R.; Kraus, J.P.; Burstyn, J.N. The Heme of Cystathionine β-Synthase Likely Undergoes a Thermally Induced Redox-Mediated Ligand Switch. Biochemistry 2005, 44, 16785–16795. [Google Scholar] [CrossRef] [PubMed]
- Hou, S.; Larsen, R.W.; Boudko, D.; Riley, C.W.; Karatan, E.; Zimmer, M.; Ordal, G.W.; Alam, M. Myoglobin-like Aerotaxis Transducers in Archaea and Bacteria. Nature 2000, 403, 540–544. [Google Scholar] [CrossRef]
- Hirotsu, S.; Chu, G.C.; Unno, M.; Lee, D.S.; Yoshida, T.; Park, S.Y.; Shiro, Y.; Ikeda-Saito, M. The Crystal Structures of the Ferric and Ferrous Forms of the Heme Complex of HmuO, a Heme Oxygenase of Corynebacterium diphtheriae. J. Biol. Chem. 2004, 279, 11937–11947. [Google Scholar] [CrossRef] [Green Version]
- Ridley, K.A.; Rock, J.D.; Li, Y.; Ketley, J.M. Heme Utilization in Campylobacter jejuni. J. Bacteriol. 2006, 188, 7862–7875. [Google Scholar] [CrossRef] [Green Version]
- Guo, Y.; Guo, G.; Mao, X.; Zhang, W.; Xiao, J.; Tong, W.; Liu, T.; Xiao, B.; Liu, X.; Feng, Y.; et al. Functional Identification of HugZ, a Heme Oxygenase from Helicobacter pylori. BMC Microbiol. 2008, 8. [Google Scholar] [CrossRef] [Green Version]
- Zhu, W.; Wilks, A.; Stojiljkovic, I. Degradation of Heme in Gram-Negative Bacteria: The Product of the hemO Gene of Neisseriae Is a Heme Oxygenase. J. Bacteriol. 2000, 182, 6783–6790. [Google Scholar] [CrossRef] [Green Version]
- Nambu, S.; Matsui, T.; Goulding, C.W.; Takahashi, S.; Ikeda-Saito, M. A New Way to Degrade Heme: The Mycobacterium tuberculosis Enzyme MhuD Catalyzes Heme Degradation without Generating CO. J. Biol. Chem. 2013, 288, 10101–10109. [Google Scholar] [CrossRef] [Green Version]
- Matsui, T.; Nambu, S.; Ono, Y.; Goulding, C.W.; Tsumoto, K.; Ikeda-Saito, M. Heme Degradation by Staphylococcus aureus IsdG and IsdI Liberates Formaldehyde rather than Carbon Monoxide. Biochemistry 2013, 52, 3025–3027. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Videira, M.A.M.; Lobo, S.A.L.; Silva, L.S.O.; Palmer, D.J.; Warren, M.J.; Prieto, M.; Coutinho, A.; Sousa, F.L.; Fernandes, F.; Saraiva, L.M. Staphylococcus aureus Haem Biosynthesis and Acquisition Pathways Are Linked through Haem Monooxygenase IsdG. Mol. Microbiol. 2018, 109, 385–400. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wegiel, B.; Larsen, R.; Gallo, D.; Chin, B.Y.; Harris, C.; Mannam, P.; Kaczmarek, E.; Lee, P.J.; Zuckerbraun, B.S.; Flavell, R.; et al. Macrophages Sense and Kill Bacteria through Carbon Monoxide-Dependent Inflammasome Activation. J. Clin. Investig. 2014, 124, 4926–4940. [Google Scholar] [CrossRef] [Green Version]
- Su, W.C.; Liu, X.; Macias, A.A.; Baron, R.M.; Perrella, M.A. Heme Oxygenase-1-Derived Carbon Monoxide Enhances the Host Defense Response to Microbial Sepsis in Mice. J. Clin. Investig. 2008, 118, 239–247. [Google Scholar] [CrossRef] [Green Version]
- Morse, D.; Pischke, S.E.; Zhou, Z.; Davis, R.J.; Flavell, R.A.; Loop, T.; Otterbein, S.L.; Otterbein, L.E.; Choi, A.M.K. Suppression of Inflammatory Cytokine Production by Carbon Monoxide Involves the JNK Pathway and AP-1. J. Biol. Chem. 2003, 278, 36993–36998. [Google Scholar] [CrossRef] [Green Version]
- Jeney, V.; Ramos, S.; Bergman, M.L.; Bechmann, I.; Tischer, J.; Ferreira, A.; Oliveira-Marques, V.; Janse, C.J.; Rebelo, S.; Cardoso, S.; et al. Control of Disease Tolerance to Malaria by Nitric Oxide and Carbon Monoxide. Cell Rep. 2014, 8, 126–136. [Google Scholar] [CrossRef] [Green Version]
- Pamplona, A.; Ferreira, A.; Balla, J.; Jeney, V.; Balla, G.; Epiphanio, S.; Chora, Â.; Rodrigues, C.D.; Gregoire, I.P.; Cunha-Rodrigues, M.; et al. Heme Oxygenase-1 and Carbon Monoxide Suppress the Pathogenesis of Experimental Cerebral Malaria. Nat. Med. 2007, 13, 703–710. [Google Scholar] [CrossRef] [PubMed]
- Scharn, C.R.; Collins, A.C.; Nair, V.R.; Stamm, C.E.; Marciano, D.K.; Graviss, E.A.; Shiloh, M.U. Heme Oxygenase-1 Regulates Inflammation and Mycobacterial Survival in Human Macrophages during Mycobacterium tuberculosis Infection. J. Immunol. 2016, 196, 4641–4649. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Giuffrè, A.; Vicente, J.B. Review Article Hydrogen Sulfide Biochemistry and Interplay with Other Gaseous. Oxid. Med. Cell. Longev. 2018, 2018, 31. [Google Scholar] [CrossRef]
- Xie, L.; Gu, Y.; Wen, M.; Zhao, S.; Wang, W.; Ma, Y.; Meng, G.; Han, Y.; Wang, Y.; Liu, G.; et al. Hydrogen Sulfide Induces Keap1 S-Sulfhydration and Suppresses Diabetes-Accelerated Atherosclerosis via Nrf2 Activation. Diabetes 2016, 65, 3171–3184. [Google Scholar] [CrossRef] [Green Version]
- Matsui, T.; Sugiyama, R.; Sakanashi, K.; Tamura, Y.; Iida, M.; Nambu, Y.; Higuchi, T.; Suematsu, M.; Ikeda-Saito, M. Hydrogen Sulfide Bypasses the Rate-Limiting Oxygen Activation of Heme Oxygenase. J. Biol. Chem. 2018, 293, 16931–16939. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Majid, A.S.A.; Majid, A.M.S.A.; Yin, Z.Q.; Ji, D. Slow Regulated Release of H2S Inhibits Oxidative Stress Induced Cell Death by Influencing Certain Key Signaling Molecules. Neurochem. Res. 2013, 38, 1375–1393. [Google Scholar] [CrossRef] [PubMed]

| CORM | Organism | Concentration (µM) | Atmosphere | Observations |
|---|---|---|---|---|
| CORM-2 | H. pylori [77] | 195–390 | Microaerobic | Parental strain (26695) and six clinical isolates (5599, 5611, 5846, 4597, 4574 and 5587) |
| E. coli ATCC 23716 [72] | 250 | Anaerobic, aerobic | --- | |
| E. coli MG1655 [76] | 350 | Microaerobic | --- | |
| E. coli MG1655 [81] | 500 | Aerobic | --- | |
| E. coli UPEC J96 [81] | 500 | Aerobic | --- | |
| E. coli ESBL 7 [81] | 500 | Aerobic | ESBL clinical isolate 7 | |
| E. coli ESBL 1, E. coli UPEC 2, E. coli MG1655 TG1 [80] | 500 | Aerobic | ESBL and non-producing (UPEC) UPEC isolates | |
| E. coli ESBL7, E. coli UPEC2, E. coli K12 [82] | 500 | Aerobic | ESBL-producing ESBL and non-producing UPEC isolates | |
| S. aureus NCTC8325 [72] | 250 | Aerobic, microaerobic | --- | |
| P. aeruginosa [83] | 10 | Aerobic | --- | |
| P. aeruginosa PAO1 biofilms [79] | 25–200 | Microaerobic | Static growth wells | |
| CORM-3 | E. coli MG1655 [84] | 100 | Aerobic | 25% air saturation |
| E. coli ATCC 23716 [72] | 200–400 | Anaerobic | --- | |
| E. coli MG1655 [85] | 30–400 100–200 | Aerobic Anaerobic | --- | |
| S. aureus NCTC8325 [72] | 400 | Microaerobic | --- | |
| P. aeruginosa PAO1 ATCC 15692 [78,83] | 10, 500 | Aerobic | --- | |
| S. typhimurium ATCC 14028s [86] | 150 | n/a | --- | |
| ALF850 | E. coli MG1655 [76] | 650 | Microaerobic | --- |
| ALF021 | E. coli K12 ATCC 23716 [72] | 200 | Anaerobic | |
| S. aureus NCTC 8325 [72] | 500 | Aerobic | ||
| 600 | Microaerobic | |||
| TryptoCORM | E. coli W3110 [87,88] | 100 | Aerobic | With irradiation |
| N. gonorrhoeae MS11 [88] | 100 | 5% CO2 | In the dark | |
| S. aureus 8325-4 [88] | 100 | Aerobic | With irradiation and in the dark | |
| PhotoCORM | E. coli EC958 [89] | 350 | Aerobic | Pre-exposed to UV light |
| USC-CN028-31 | ||||
| (Mn(CO)3(tpa-k3N)Br) | ||||
| Avian pathogenic E. coli [90] | 2000 | Microaerobic | --- | |
| E. coli K12 MG1655 [91] | 250–500 | Aerobic | Glucose or succinate as carbon source; Transient to severe reduction of growth | |
| [Mn(CO)3(bpy)(mcz)]PF6 | S. aureus, S. epidermidis | 1.25 | n/a | --- |
| E. faecium, | ||||
| L. major, | 1.8 | n/a | --- | |
| T. brucei [92] | 0.4 | n/a | --- | |
| [Mn(CO)3(bpy)(ktz)]PF6 | S. aureus, S. epidermidis, | 2.5 | n/a | --- |
| L. major, | 2 | n/a | --- | |
| T. brucei [92] | 0.7 | n/a | --- | |
| [Mn(CO)3(bpy)(ctz)]PF6 | S. aureus, S. epidermidis, | 0.6 | n/a | --- |
| E. faecium, E. faecalis | 2.5 | n/a | --- | |
| L. major, | 2.2 | n/a | --- | |
| T. brucei [92] | 0.5 | n/a | --- | |
| CORM-371 | P. aeruginosa [83] | 10 | Aerobic | --- |
| CORM-1 nonwoven | S. aureus MRSA (biofilms) [93] | < 3 µmol CO/mg nonwoven | n/a | 70% inhibition after irradiation at 405 nm |
| EBOR-CORM-1 | P. aeruginosa [94] | 500 | Microaerobic | Tested in planktonic and biofilms of PAO1 |
| CORM-401 | E. coli K12 [95] | 500 | n/a | --- |
| ALF062 | E. coli ATCC 23716 [72] | 50 | Aerobic, anaerobic | --- |
| E. coli MG1655 [76] | 450 | Microaerobic | --- | |
| S. aureus NCTC 8325 [72] | 50 | Microaerobic, aerobic | --- | |
| ALF186 | E. coli MG1655 [76] | 2000 | Microaerobic | --- |
| CORM-A1 | P. aeruginosa [83] | 10-500 | Aerobic | Bacteriostatic |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mendes, S.S.; Miranda, V.; Saraiva, L.M. Hydrogen Sulfide and Carbon Monoxide Tolerance in Bacteria. Antioxidants 2021, 10, 729. https://doi.org/10.3390/antiox10050729
Mendes SS, Miranda V, Saraiva LM. Hydrogen Sulfide and Carbon Monoxide Tolerance in Bacteria. Antioxidants. 2021; 10(5):729. https://doi.org/10.3390/antiox10050729
Chicago/Turabian StyleMendes, Sofia S., Vanessa Miranda, and Lígia M. Saraiva. 2021. "Hydrogen Sulfide and Carbon Monoxide Tolerance in Bacteria" Antioxidants 10, no. 5: 729. https://doi.org/10.3390/antiox10050729
APA StyleMendes, S. S., Miranda, V., & Saraiva, L. M. (2021). Hydrogen Sulfide and Carbon Monoxide Tolerance in Bacteria. Antioxidants, 10(5), 729. https://doi.org/10.3390/antiox10050729







